Abstract
Background:
There is a paucity of research on the management of partial-thickness tears of the distal bicep tendon, and even less is known about the long-term outcomes of this condition.
Purpose:
To identify patients with partial-thickness distal bicep tendon tears and determine (1) patient characteristics and treatment strategies, (2) long-term outcomes, and (3) any identifiable risk factors for progression to surgery or complete tear.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A fellowship-trained musculoskeletal radiologist identified patients diagnosed with a partial-thickness distal bicep tendon tear on magnetic resonance imaging between 1996 and 2016. Medical records were reviewed to confirm the diagnosis and record study details. Multivariate logistic regression models were created using baseline characteristics, injury details, and physical examination findings to predict operative intervention.
Results:
In total, 111 patients met inclusion criteria (54 treated operatively, 57 treated nonoperatively), with 53% of tears in the nondominant arm and a mean follow-up time after surgery of 9.7 ± 6.5 years. Only 5% of patients progressed to full-thickness tears during the study period, at a mean of 35 months after the initial diagnosis. Patients who were nonoperatively treated were less likely to miss time from work (12% vs 61%; P < .001) and missed fewer days (30 vs 97 days; P < .016) than those treated surgically. Multivariate regression analyses demonstrated increased risk of progression to surgery with older age at initial consult (unit odds ratio [OR], 1.1), tenderness to palpation (OR, 7.5), and supination weakness (OR, 24.8). Supination weakness at initial consult was a statistically significant predictor for surgical intervention (OR, 24.8; P = .001).
Conclusion:
Clinical outcomes were favorable for patients regardless of treatment strategy. Approximately 50% of patients were treated surgically; patients with supination weakness were 24 times more likely to undergo surgery than those without. Progression to full-thickness tear was a relatively uncommon reason for surgical intervention, with only 5% of patients progressing to full-thickness tears during the study period and the majority occurring within 3 months of initial diagnosis.
Keywords: distal biceps, bicep tears, long-term outcome, partial-thickness distal bicep tendon tear
Distal bicep tendon tear occurs most commonly in the dominant arms of men between the ages of 30 and 50 years. 13 These injuries may be more common than once appreciated, occurring at a rate of 2.5 per 100,000 patient-years. 13 Launonen et al 14 recently reported an incidence of 10.0 per 100,000 person-years from 2001 to 2016 in the Swedish population. Tears can be either full or partial thickness in nature. Partial-thickness tears typically involve the distal tendon of the short head. 17 While the characteristics, outcomes, and complications of full-thickness distal bicep injuries and surgical repair have been extensively reported in the literature, there remains a paucity of research focusing on partial-thickness distal bicep tendon tears.1,13,20 Accordingly, the true incidence, long-term outcomes, and risk factors for progression to surgery of these partial-thickness bicep tears are not fully understood, and further clinical guidance is needed.
Patients with a partial distal bicep tendon tear may be evaluated with nonspecific pain or dysfunction localized to the anterior arm and antecubital fossa. 23 Delay in diagnosis is quite common, with some patients commonly experiencing symptoms for 8 to 10 months before formal diagnosis.8,19,23 Previous reports on partial-thickness tears of the distal bicep tendon have been largely limited to case reports or small series.5,9,15,16 A recent systematic review identified 19 studies reporting on the operative management of partial-thickness distal bicep tears. Despite the wide scope and inclusive methodology of this review, the authors were only able to report on 86 patients treated operatively and 5 patients treated nonoperatively for partial distal bicep tendon tears. 4 Additionally, because there are little to no long-term data published on treatment outcomes of partial-thickness tears, the fate of these injuries is not well understood.
While risk factors for complete distal bicep tendon tear, such as smoking and elevated body mass index (BMI), have been reported,7,13,18 risk factors for progression of a partial-thickness tear to surgical intervention or full-thickness tear have not been fully elucidated. Therefore, the primary purpose of this study was to determine the long-term outcomes of patients with magnetic resonance imaging (MRI)–confirmed partial-thickness distal bicep tendon tears. More specifically, we sought to describe (1) patient characteristics, (2) treatment strategies, (3) long-term outcomes, and (4) any identifiable risk factors for progression to surgery or tear completion.
Methods
Study Design
This study was determined to be exempt from institutional review board approval. Patients who had been diagnosed with partial-thickness distal bicep tendon tear confirmed on MRI between 1996 and 2016 were identified by a musculoskeletal radiologist (A.C.J.) through review of institutional radiographic records. Patients were included if they had complete medical records and had been seen at least once on follow-up after their diagnosis. Patients with inflammatory arthritis and enthesitis, polytrauma, or incidental findings without clinical symptomatology attributable to the bicep tendon were excluded. Patients who were documented to have MRI evidence of a full-thickness distal bicep tendon tear were also excluded. Those who met criteria were then cross-referenced in the Rochester Epidemiology Project (REP) to minimize the risk of missing patients. The REP is an electronic collection system of complete medical records involving a US-based geographic cohort of >600,000 patients, all of whom were residents in Olmsted County, Minnesota, and neighboring counties in southeast Minnesota and western Wisconsin. The methodology and generalizability of the REP have been previously described in detail.21,22
Medical records were reviewed to confirm the diagnosis and obtain patient characteristics and details relevant to the study, including patient symptomatology and injury characteristics. Patient characteristics recorded included age at diagnosis, sex, BMI, laborer status, dominant hand involvement, anabolic steroid usage, and associated chronic medical conditions. Components of the physical examination included the hook test, range of motion (ROM), supination/flexion weakness, tenderness to palpation (TTP), description of injury, and pain at initial consult. Treatment strategies were nonoperative and operative, with the latter defined as surgical intervention at any time point. Surgical details, such as repair methodology and incisional technique (1 vs 2 incisions), were also recorded.
Outcomes of interest for all patients included both physical and work function after injury. This included flexion, extension, supination, and pronation ROM, in addition to flexion and supination strength through manual testing. These data were gathered from documented physical examination findings during review of patient medical records. Progression from partial-thickness to full-thickness tear and progression to surgery were also investigated. Return-to-work status, if time was missed, and exact time missed from work were obtained from the medical records.
Statistical Analysis
Collected data were stored in Microsoft Excel (2010; Microsoft Corp) and analyzed with JMP Pro (Version 14.1.0; SAS Institute). Patient characteristics are presented with descriptive statistics using means, medians, percentages, and 95% confidence intervals of the mean when appropriate. After analyzing data for parametric/nonparametric assumptions, continuous variables were compared between groups utilizing Student t tests or Wilcoxon rank-sum tests, and categorical variables were similarly compared utilizing chi-square analysis or Fisher exact tests. Statistical differences in the survival analysis were reported with a log-rank P value, and proportional odds ratio (OR). P values <.05 were considered to represent statistical significance.
Multivariate logistic regression models were created using baseline characteristics, injury details, and physical examination findings to predict progression to operative intervention. Predictor screening with a bootstrap forest model with 100 trees was used to identify predictors for inclusion in the initial logistic regression model. The following top 10 predictors identified by predictor screening were included: supination weakness; age at initial consultation; TTP at the distal bicep tendon; sex; sensation of pop, rip, or tear at injury event; flexion weakness; BMI; supination motion; supination pain; and hook test results. After initial inclusion, the predictors with the lowest log worth were removed from the model in a stepwise fashion until the model stabilized. The final model included 3 variables: supination weakness, age at initial consultation, and TTP.
Results
Study Population
Overall, 308 patients were evaluated with distal bicep tears, confirmed by MRI, during the study period. A total of 207 individuals demonstrated full-thickness tear on MRI and were thus excluded; the final cohort included 111 MRI-confirmed partial-thickness bicep tears, of which 54 were treated operatively and 57 nonoperatively (Table 1). The mean age at evaluation was 53.6 years (range, 15.1-102.6 years); 80% of the patients were men, 56.7% worked as laborers, and 53.2% injured their nondominant arm. Men were significantly younger at evaluation than women (51.5 vs 62.5 years; P < .001). No patients had undergone previous ipsilateral biceps surgery. The mean follow-up time from initial consultation to most recent clinical contact was 10.1 years for all patients, with 95% (105/111) having >24-month follow-up. The mean follow-up time after surgery was 9.7 ± 6.5 years.
Table 1.
Patient and Clinical Characteristics a
| Treatment | ||||
|---|---|---|---|---|
| Characteristic | Study Cohort (N = 111) |
Operative (n = 54) |
Nonoperative (n = 57) |
P |
| Age, y | 53.6 ± 13 (15.1-102.6) | Mean 51.5 | Mean 55.7 | .088 |
| Sex | .002 | |||
| Male | 80.2 (89) | 93 (50) | 68 (39) | .001 |
| Female | 19.8 (22) | 7 (4) | 32 (18) | .003 |
| BMI, kg/m2 | 32.0 ± 6.3 (21.38-65.3) | Mean 31.6 | Mean 32.3 | .578 |
| Dominant arm involved | 46.8 (52) | 46 (25) | 47 (27) | .91 |
| Smoking status | .3 | |||
| Current | 18.1 (20) | 18.5 (10) | 17.5 (10) | |
| Former | 34.2 (38) | 40.7 (22) | 28.1 (16) | |
| Never | 47.7 (53) | 40.7 (22) | 54.4 (31) | |
| Diabetes mellitus | 8.1 (9) | 9.3 (5) | 7.0 (4) | .738 |
| Laborer | 56.7 (63) | 63 (34) | 51 (29) | .198 |
| Corticosteroid use | 5.4 (6) | 3.7 (2) | 7.0 (4) | .366 |
| Anabolic steroid use | 0.9 (1) | 1.8 (1) | 0 (0) | NA |
| Chronic renal disease | 0.9 (1) | 0 (0) | 1.8 (1) | NA |
| Follow-up from initial consult, y | Mean 10.1 | 10.3 ± 6.3 (0.7-24) | 9.7 ± 5.8 (0.5-21) | .601 |
| Follow-up after surgery, y | NA | 9.7 ± 6.5 (0.1-24) | NA | NA |
Data are reported as mean ± SD (range) or % (n) unless otherwise indicated. Bolded P values indicate a statistically significant difference between treatment types (P < .05). BMI, body mass index; NA, not applicable.
Six (5%) patients experienced progression from a partial- to a full-thickness tear at a mean of 34.9 months (range, 0-205 months) from the time of their index partial-tear diagnosis. Notably, the majority (5/6) progressed within 3 months of the initial diagnosis. Importantly, 4 of these 6 progressions to full tear were not identified until the time of surgery, which was recommended for persistent pain despite nonoperative management. Only 2% of patients were indicated for surgical intervention for documented preoperative progression to a full-thickness tear. All 6 patients were men with pain at evaluation, and 5 of the 6 reported a pop, rip, or tear at the time of injury; none of these patients reported a new inciting event after the initial consultation. These 6 patients had a mean age of 46.7 ± 8.1 years (range, 31-53 years), and 50% were laborers. All 6 patients underwent operative repair, despite 5 (83.5%) initially attempting nonoperative management. One patient developed scarring of the tendon remnants to the median nerve, which was discovered during an initial repair attempt at an outside hospital; this patient underwent successful repair.
For the 54 patients treated operatively, the median time from injury to surgery was 100 days (IQR, 22-256 days), with 46 patients undergoing operative repair within 1 year (Table 2). Compared with nonoperatively treated patients, operatively treated patients were more likely to be men (68% vs 93%; P > .001); experience a sensation of popping, ripping, or tearing at the time of injury (P = .009); and demonstrate the following physical examination findings: abnormal hook test (P = .018), TTP at tendon insertion (P = .001), weakness of elbow flexion (P = .035), and supination weakness (P = .011). More than half of the operatively treated patients (59%) underwent repair with a double-incision technique, and cortical button fixation was the most common method of fixation (35% of patients) (Table 2).
Table 2.
Operative Treatment Course (n = 54) a
| Variable | Value |
|---|---|
| Days from injury to surgery, median [IQR], mean | 100 [22–256], 387 |
| Days from consult to surgery, median [IQR], mean | 35 [11–112], 218 |
| Surgical approach | |
| Single incision | 41 (22) |
| Double incision | 59 (32) |
| Tear observed intraoperatively | |
| Complete | 9 (5) |
| Partial | 89 (48) |
| No tear observed | 2 (1) |
| Percentage of bicep tendon torn in partial tears | |
| <50% | 13 (6) |
| 50%-75% | 23 (11) |
| >75% | 35 (17) |
| Unknown | 29 (20) |
| Repair technique | |
| Suture through bone tunnel | 13 (9) |
| Button + screw | 23 (14) |
| Button only | 35 (17) |
| Anchor only | 29 (14) |
| Formal postoperative physical therapy | 26 |
Data are reported as % (n) unless otherwise indicated. IQR, interquartile range.
Postintervention mechanical and functional outcomes are recorded in Table 3. Patients in the nonoperative group demonstrated a mean extension-flexion arc of 1° to 139° and a mean pronation-supination arc of 80° to 80° at final follow-up. They were less likely to miss time from work compared with patients treated operatively (12% vs 61%; P < .001) and averaged fewer days missed (30 vs 97 days; P < .016). Patients treated nonoperatively demonstrated no statistically significant differences in ability to return to work without limitations, motion loss, flexion strength, or supination strength when compared with patients treated operatively at long-term follow-up (Table 3).
Table 3.
Postintervention Outcomes a
| Treatment | ||||
|---|---|---|---|---|
| Variable | Overall (N = 111) |
Operative (n = 54) |
Nonoperative (n = 57) |
P |
| Days missed from work since surgery or initial consult, median [IQR], mean | 97 [74–153], 136 b | 30 [0–98], 47 c | .016 | |
| Return to work without modifications | 88 (44/50) | 88 (29/33) | 88 (15/17) | >.999 |
| Weakness of elbow flexion (<5/5) d | 11 (4/38) | 8 (2/24) | 14 (2/14) | .616 |
| Weakness of forearm supination (<5/5) d | 21 (7/34) | 17 (4/24) | 30 (3/10) | .394 |
Data are reported as % (n/N) unless otherwise indicated. Bolded P value indicates a statistically significant difference between treatment courses (P < .05). IQR, interquartile range.
n = 33 patients.
n = 7 patients.
Not performed/recorded in all patients.
Multivariate logistic regression models were created to predict progression to operative treatment (Table 4). The factors that most strongly correlated with surgical intervention were supination weakness (OR, 24.8; 95% CI, 2.3-264.2; P = .001), increased age at initial consultation (unit OR, 1.06; 95% CI, 0.99-1.1; P = .098), and pain with palpation of the bicep tendon (OR, 7.49; 95% CI, 0.4-132.8; P = .154) (Table 5). Although the 3-variable model was statistically significant (P = .004), supination weakness was the only statistically significant predictor when considered individually (P = .001) (Table 4). The receiver operating characteristic curve generated from the logistic regression model demonstrated an optimal cutoff point with a sensitivity of 0.76, specificity of 0.89, and area under the curve of 0.869 (Figure 1).
Table 4.
Univariate Logistic Regression Factors for Operative and Nonoperative Treatment a
| Factor | Operative | Nonoperative | Odds Ratio (95% CI) | P |
|---|---|---|---|---|
| Days from injury to consult, median [IQR] | 38 [7–149] | 44 [6–165] | 1.0 b | .475 |
| Age at initial consult, y, median [IQR] | 50 [45–58] | 53 [46–68] | 0.97 b | .092 |
| Pain at time of consult, % yes | 98 (53/54) | 95 (54/57) | 2.9 (0.3–29.1) | .619 |
| Pop/rip/tear | 77 (37/48) | 51 (23/45) | 3.2 (1.3–7.9) | .009 |
| Traumatic mechanism | 85 (46/54) | 75 (43/57) | 1.8 (0.72–4.9) | .198 |
| Visible deformity | 20 (11/54) | 14 (8/57) | 1.5 (0.58–4.3) | .376 |
| Pronation pain | 52 (15/29) | 42 (10/24) | 1.5 (0.5–4.4) | .465 |
| Supination pain | 84 (36/43) | 81 (29/36) | 1.2 (0.4–3.9) | .714 |
| Weakness of elbow flexion (<5/5) c | 61 (19/31) | 29 (5/17) | 3.8 (1.0–13.5) | .035 |
| Weakness of forearm supination (<5/5) c | 84 (26/31) | 43 (6/14) | 6.9 (1.7–28.9) | .011 |
| Hook test abnormal | 96 (27/28) | 71 (17/24) | 0.09 (0.01–0.80) | .018 |
| TTP at distal biceps | 95 (42/44) | 69 (29/42) | 9.4 (2.0–44.1) | .001 |
| Bruising | 11 (6/54) | 7 (4/57) | 1.6 (0.4–6.2) | .452 |
| Neurological involvement | 4 (2/53) | 15 (7/47) | 0.26 (0.05–1.3) | .161 |
Data are reported as % (n/N) unless otherwise indicated. Bolded P values indicate statistical significance (P < .05). IQR, interquartile range; TTP, tenderness to palpation.
Presented as unit odds ratio.
Not performed/recorded in all patients.
Table 5.
Multivariate Logistic Regression Factors a
| Predictor | Odds Ratio (95% CI) | P |
|---|---|---|
| Supination weakness | 24.8 (2.33–264.20) | .001 |
| Age at initial consult | 1.06 b (0.99–1.14) | .098 |
| TTP at bicep tendon | 7.49 (0.41–132.76) | .154 |
Bolded P value indicates statistical significance (P < .05). TTP, tenderness to palpation.
Presented as unit odds ratio.
Figure 1.
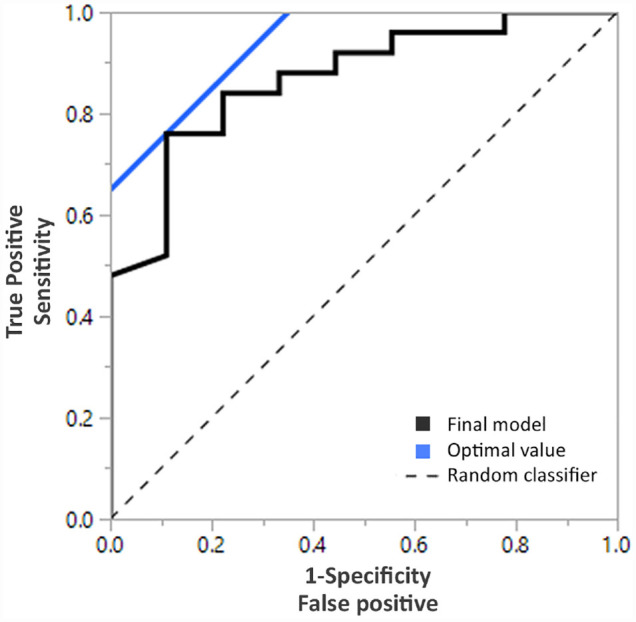
Receiver operating curve demonstrating predictive modeling of operative intervention. The final model included supination weakness, age at initial consult, and tenderness to palpation at bicep tendon as variables for surgical intervention (overall model, P = .004). The optimal cutoff point (the intersection of the final model and optimal value) was determined to have a sensitivity of 0.76, specificity of 0.89, and area under the curve of 0.869.
Discussion
The primary findings of this long-term study of partial-thickness distal bicep tendon tears were that only 5% of patients progressed to full-thickness tears at a mean of 35 months, approximately 50% of patients ultimately required surgery, and supination weakness (OR, 24.8) at initial evaluation was the strongest predictor for progression to surgery. Overall, patients were most often men, were laborers in their 50s, and were without significant associated risk factors. Just >50% of tears occurred in the nondominant extremity. Regardless of treatment (surgical or nonoperative) patient outcomes were very favorable, with nearly all patients achieving full motion, adequate strength, and the ability to return to work without modifications.
Partial-thickness distal bicep tendon tear characteristics and treatment strategies are incompletely reported in the literature to date. The true incidence of partial-thickness distal bicep tendon tears is unknown, as many cases may not be formally evaluated. The age at evaluation for a partial tear has been previously reported to be in the mid-50s, which is consistent with our study.10,23 This patient cohort included 20% female patients, which is a significantly higher proportion than has been previously reported in patients with distal bicep injury. Although nonsurgical treatment has been considered a staple of care for partial distal bicep tendon tears, there are mixed data on the overall efficacy of nonsurgical interventions.2,3,23 Historical treatments with plaster splinting and/or bracing are reported but not commonly utilized in contemporary practice.5,9 Successful surgical treatment of partial-thickness tears has been reported in numerous previous case series and reports and is further validated by our study.6,11,12,17 Our cohort that was treated nonoperatively was met with good clinical and functional results. A recent systematic review by Behun et al 4 identified only 5 patients with nonoperative management in the current literature. Our study reported on the outcomes of a larger number of partial tears treated (N = 111), and the long-term outcomes were quite favorable for those treated nonoperatively and those treated surgically.
In the current literature, little is known about the factors that are associated with the risk of progression from a partial tear to a complete tear or for the need for surgical intervention. Because of the limited number of patients (n = 6), this study was unable to draw statistical conclusions regarding risk factors for progression to full-thickness tears. However, it is notable that only a small minority (5%) of partial-thickness tears progressed to full-thickness tears, and only 2 of those that did progress exhibited signs or symptoms concerning for progression before surgical intervention. This information should be helpful in clinical discussion and decision-making with patients.
There were several risk factors correlated with progression to surgery for this cohort. Univariate analysis risk factors included supination weakness (OR, 24.8), younger age at initial consultation (unit OR, 1.1), and pain with palpation of the bicep tendon (OR, 7.5). During multivariate modeling, supination weakness was shown to be the greatest predictor of conversion to surgical intervention. Because the biceps are the primary supinator of the forearm, loss of supination strength is difficult to compensate for. Although these symptoms were present in our nonoperatively treated patients, the statistical significance of their contribution to operative treatment cannot be overlooked. To our knowledge, this is the first study to report a significant, multifactorial risk model for progression to operative treatment in patients with partial-thickness distal bicep tendon tears.
Limitations
There are several limitations in our study that merit discussion. This study was performed in a retrospective fashion and was subject to the common limitations of retrospective research. Not all data were initially collected in a uniform and consistent way at the time of initial patient evaluation, and as such the model may be slightly underpowered because of missing data. Additionally, strength measurement is an area of the physical examination that lacks rigorous standardization and, as such, is a limitation. Treatment and postoperative course were not standardized across all patients and providers. Only patients with MRI-confirmed partial tears were included in the study. While this strict definition of a partial tear substantially increased diagnostic accuracy, there were likely patients who may have had partial tears but never received advanced imaging and were not included in the study.
Conclusion
In this long-term study of patients with partial-thickness distal bicep tendon tears, clinical outcomes were favorable for patients treated either nonoperatively or surgically. Approximately 50% of patients were treated surgically; patients with supination weakness were 24 times more likely to undergo surgery than those without. Progression to full-thickness tear was a relatively uncommon reason for surgical intervention, with only 5% of patients progressing to full-thickness tears during the study period and the majority occurring within 3 months of initial diagnosis. These data should be helpful in counseling patients diagnosed with partial-thickness tears of the distal bicep tendon.
Footnotes
Final revision submitted January 25, 2023; accepted February 13, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study used the Rochester Epidemiology Project (REP) medical records linkage system, which is supported by the National Institute on Aging (NIA; AG 058738), by the Mayo Clinic Research Committee, and by fees paid annually by REP users. This study was partially funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). Support was received from the Foderaro-Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund. A.J.T. has received hospitality payments from Stryker and Zimmer Biomet. A.C.J. has received hospitality payments from Zimmer Biomet. J.S.-S. has received consulting fees from Acumed, Exactech, and Stryker; speaking fees from Acumed; and royalties from Stryker. J.D.B. has received education payments from Arthrex, consulting fees from Stryker, speaking fees from Arthrex, and hospitality payments from Wright Medical. C.L.C. has received consulting fees and nonconsulting fees from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto. This study was partially funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors would like to acknowledge the support from the Foderaro-Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund.
Ethical approval for this study was waived by Mayo Clinic (reference No. 20-002302).
References
- 1.Amarasooriya M, Bain GI, Roper T, et al. Complications after distal biceps tendon repair: a systematic review. Am J Sports Med. 2020;48(12):3103-3111. [DOI] [PubMed] [Google Scholar]
- 2.Bain GI, Johnson LJ, Turner PC. Treatment of partial distal biceps tendon tears. Sports Med Athrosc Rev. 2008;16(3):154-161. [DOI] [PubMed] [Google Scholar]
- 3.Bauer TM, Wong JC, Lazarus MD. Is nonoperative management of partial distal biceps tears really successful? J Shoulder and Elbow Surg. 2018;27(4):720-725. [DOI] [PubMed] [Google Scholar]
- 4.Behun MA, Geeslin AG, O’Hagan EC, King JC. Partial tears of the distal biceps brachii tendon: a systematic review of surgical outcomes. J Hand Surg Am. 2016;41(7):e175-189. [DOI] [PubMed] [Google Scholar]
- 5.Bourne MH, Morrey BF. Partial rupture of the distal biceps tendon. Clin Orthop Relat Res. 1991;271:143-148. [PubMed] [Google Scholar]
- 6.Cho CH, Song KS, Lee SM. Isolated short head component rupture of a bifurcated distal biceps tendon mimicking as a complete rupture. J Hand Surg Eur Vol. 2011;36(4):333-334. [DOI] [PubMed] [Google Scholar]
- 7.Del Buono A, Battery L, Denaro V, Maccauro G, Maffulli N. Tendinopathy and inflammation: some truths. Int J Immunopathol. 2011;24(1 suppl 2):45-50. [DOI] [PubMed] [Google Scholar]
- 8.Dellaero DT, Mallon WJ. Surgical treatment of partial biceps tendon ruptures at the elbow. J Shoulder Elbow Surg. 2006;15(2):215-217. [DOI] [PubMed] [Google Scholar]
- 9.Dürr HR, Stäbler A, Pfahler M, Matzko M, Refior HJ. Partial rupture of the distal biceps tendon. Clin Orthop Relat Res. 2000;(374):195-200. [DOI] [PubMed] [Google Scholar]
- 10.Eames MH, Bain GI, Fogg QA, van Riet RP. Distal biceps tendon anatomy: a cadaveric study. J Bone Joint Surg Am. 2007;89(5):1044-1049. [DOI] [PubMed] [Google Scholar]
- 11.Fajardo MR, Rosenberg Z, Christoforou D, Grossman JA. Multiple nerve injuries following repair of a distal biceps tendon rupture. Bull Hosp Jt Dis. 2013;71(2):166-169. [PubMed] [Google Scholar]
- 12.Frazier MS, Boardman MJ, Westland M, Imbriglia JE. Surgical treatment of partial distal biceps tendon ruptures. J Hand Surg Am. 2010;35(7):1111-1114. [DOI] [PubMed] [Google Scholar]
- 13.Kelly MP, Perkinson SG, Ablove RH, Tueting JL. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43(8):2012-2017. [DOI] [PubMed] [Google Scholar]
- 14.Launonen AP, Huttunen TT, Lepola V, et al. Distal biceps tendon rupture surgery: changing incidence in Finnish and Swedish men between 1997 and 2016. J Hand Surg Am. 2020;45(11):1022-1028. [DOI] [PubMed] [Google Scholar]
- 15.Nielsen K. Partial rupture of the distal biceps brachii tendon: a case report. Acta Orthop Scand. 1987;58(3):287-288. [DOI] [PubMed] [Google Scholar]
- 16.Rokito AS, McLaughlin Ja, Gallagher MA, Zuckerman JD. Partial rupture of the distal biceps tendon. J Should Elbow Surg. 1996;5(1):73-75. [DOI] [PubMed] [Google Scholar]
- 17.Ruch DS, Watters TS, Wartinbee DA, et al. Anatomic findings and complications after surgical treatment of chronic, partial distal biceps tendon tears: a case cohort comparison study. J Hand Surg Am. 2014;39(8):1572-1577. [DOI] [PubMed] [Google Scholar]
- 18.Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275-283. [PubMed] [Google Scholar]
- 19.Seiler JG, III, Parker LM, Chamberland PD, Sherbourne GM, Carpenter WA. The distal biceps tendon: two potential mechanisms involved in its rupture: arterial supply and mechanical impingement. J Should Elbow Surg. 1995;4(3):149-156. [DOI] [PubMed] [Google Scholar]
- 20.Srinivasan RC, Pederson WC, Morrey BF. Distal biceps tendon repair and reconstruction. J Hand Surg Am. 2020;45(1):48-56. [DOI] [PubMed] [Google Scholar]
- 21.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614-1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, III, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011;173(9):1059-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vardakas DG, Musgrave DS, Varitimidis SE, Goebel F, Sotereanos DG. Partial rupture of the distal biceps tendon. J Should Elbow Surg. 2001;10(4):377-379. [DOI] [PubMed] [Google Scholar]


