Abstract
The Affordable Care Act aimed to increase use of preventive services by eliminating cost-sharing to consumers. However, patients may be unaware of this benefit or they may not seek preventive services if they anticipate that the cost of potential diagnostic or treatment services will be too high, both more likely among those in high deductible health plans. We used nationally representative private health insurance claims (100% sample of IBM® MarketScan®) for the United States from 2006 to 2018, restricting the data to enrollment and claims for non-elderly adults who were enrolled for the full plan year. The cross-sectional sample (185 million person-years) is used to describe trends in preventive service use and costs from 2008 through 2016. The cohort sample (9 million people) focuses on the elimination of cost-sharing for certain high-value preventive services in late 2010, requiring continuous enrollment across 2010 and 2011. We examine whether HDHP enrollment is associated with use of eligible preventive services using semi-parametric difference-in-differences to account for endogenous plan selection. Our preferred model implies that HDHP enrollment was associated with a reduction of the post-ACA change in any use of eligible preventive services by 0.2 percentage points or 12.5%. Cancer screenings were unaffected but HDHP enrollment was associated with smaller increases in wellness visits, immunizations, and screening for chronic conditions and sexually transmitted infections. We also find that the policy was ineffective at reducing out-of-pocket costs for the eligible preventive services, likely due to implementation issues.
Keywords: health insurance, affordable care act, high deductible, preventive services, cost-sharing
What do we already know about this topic?
● Prior studies have assessed how the ACA provision to eliminate cost-sharing has affected preventive service use for specific services or types of services, finding mixed results
How does your research contribute to the field?
● Enrollment in a high deductible health plan was associated with a smaller increase in use of eligible preventive services for which cost-sharing was eliminated by the ACA
What are your research’s implications toward theory, practice, or policy?
● The policy was unsuccessful in reducing out-of-pocket costs for consumers in the early years of implementation, creating potential frustration for consumers
Introduction
Less than one-tenth of adults in the United States aged 35 and older are up-to-date with all recommended preventive services, falling well short of many Healthy People 2020 goals.1-3 Prevention is often incentivized in alternative payment models as a way to improve population health and reduce spending growth, but the number needed to screen or treat to effectively reduce morbidity and mortality through prevention can vary widely across conditions, risk profiles, and transmission potential.4-9 The Patient Protection and Affordable Care Act of 2010 (ACA) aimed to increase use of certain preventive services by eliminating cost-sharing for consumers, making eligible services exempt from plan deductibles, copayments, and coinsurance. 10 Specifically, the ACA required all new and “substantially” modified commercial health insurance plans sold after September 23, 2010 (non-grandfathered plans) to cover certain high-value preventive services with no out-of-pocket cost to consumers. 11 Grandfathered plans, or plans originally sold before this date that did not “substantially cut benefits or increase plan costs” were not subject to this requirement, though many such plans already included, or were amended to include first dollar coverage for some preventive services.12,13
High deductible health plans (HDHP) require consumers to pay first dollar up to a certain amount, providing a disincentive against the use of preventive services and health care generally, and have grown to make up more than one-third of the commercial health insurance market.14-18 Today, many enrollees in employer-sponsored insurance and the ACA exchanges are in HDHPs with large cost-sharing responsibilities before their plans actually meet their stated actuarial values.19,20 HDHPs decrease use of both high- and low-value health care and generally do not meet the goal of promoting more engaged consumer behavior.15,21-29 If patients were able to discriminate in how they reducing health care use, then HDHPs would be an effective remedy against moral hazard, but they often delay, or forego, both high and low-value care instead.14,27,30-33
Consumer understanding of health insurance terminology and benefit design is generally poor so this added benefit could get lost in more salient plan features, like deductibles, meaning that patients may respond to that incentive not fully understanding how they interact.34-39 Prior studies have assessed how the ACA provision to eliminate cost-sharing has affected preventive service use for specific services, finding mixed results.40-45 In this study, we focus on whether HDHP enrollment is associated with a differential response in the use of eligible preventive services, a previously noted gap, 16 employing a quasi-experimental approach with a national cohort of continuously enrolled non-elderly adults.
Methods
Data
This study uses the 100% sample of commercial health insurance claims from the IBM® MarketScan® Commercial Database for the years 2008 through 2016. These data represent a national multi-insurer set of commercially enrolled individuals, including tens of millions of covered lives each year who are enrolled in either employer-sponsored or non-group health insurance plans. 46 MarketScan® data includes self-insured employers, third party administrators, and health insurers, providing one of the largest samples of privately insured individuals in the United States.
We restricted the data to enrollment and claims for non-elderly adults (18-64 years of age) who were enrolled for the full plan year (at least 360 days) as we would not be able to observe preventive service use and type of other coverage held during out-of-sample periods. Over 70% of age-eligible enrollees (71.1%) met this inclusion criterion during the study period. We chose not to include children as they are subject to varying requirements for immunizations and other preventive services for school entry at the state and/or local levels that may attenuate any effect of the reduction in out-of-pocket costs (eg, potential ceiling effects).47,48 Another inclusion criterion was consistency of plan type within the calendar year to ensure that the benefit design and other coverage characteristics (ie, network, gatekeeping) were constant. Nearly 95% of person-years (94.8%) meeting the age and plan days criteria maintained a consistent plan type within the plan year. In total, more than two-thirds of age-eligible person-years (67.4%) in the MarketScan® data for the years 2008 through 2016 met all of these inclusion criteria.
We created 2 samples from the MarketScan® annual enrollment files for use in this analysis, a cross-sectional sample and a cohort sample. The cross-sectional sample is used to describe trends in preventive service use and costs over the years 2008 through 2016, beginning before the ACA was passed. Each person-year meeting all of the inclusion criteria was included, yielding a sample of nearly 185 million person-years. The cohort sample focuses on the time period surrounding the exogenous price change, the elimination of cost-sharing for certain high-value preventive services in late 2010, by requiring continuous enrollment across 2010 and 2011. The elimination of cost-sharing took effect on September 23, 2010 but would not apply to anyone in our continuously enrolled cohort sample until the 2011 plan year. For the cohort sample, the plan consistency criterion was extended to cover both years (2010 and 2011) instead of each plan year individually as in the cross-sectional sample. Of those age-eligible and enrolled for the full plan years in 2010 and 2011, nearly 95% had a consistent plan type across both years. We also required additional continuous enrollment for a 6-month look-back period to quantify comorbidity burden prior to observing preventive service use, yielding a cohort of over 9 million enrollees.
Measures
Prior studies have tended to focus on a single or narrow set of preventive services that were subject to the elimination of cost-sharing under the Affordable Care Act. Our goal was to be as inclusive as possible among eligible services relevant to the non-elderly adult population, focusing on any use and use of specific categories of preventive services. Eligible services were identified and grouped into categories similar to those defined by KFF, 12 yielding 5 categories of preventive services use: (1) health promotion, (2) cancer, (3) chronic conditions, (4) immunizations, and (5) reproductive health and pregnancy (Table 1 and Supplemental Appendix Table 1). Several reproductive health services, such as contraception, breastfeeding supports, and gestational diabetes screenings, were not covered without cost-sharing until August 2012 and therefore are not included in our analysis. Medications or supplements that are also available over the counter (eg, aspirin, folic acid) were not included because they do not require a prescription and would not be observed in pharmacy claims. Our chosen populations for each service in Table 1 broadly reflect the population likely recommended to use these services, they are not meant to summarize USPSTF recommendations, which have changed over time, or reflect specific plan-level guidelines for receiving each preventive service without cost-sharing, which vary by age, gender, risk factors, etc.
Table 1.
Preventive Services Covered Without Cost-Sharing by Non-Grandfathered Plans.
| Service | Population included in analysis (by sex and age) |
|---|---|
| Health promotion | |
| Wellness visit | All |
| Cancer | |
| Breast cancer screening | Women, 40 and older |
| Breast cancer genetic screening and counseling, chemoprevention | Women |
| Cervical cancer screening | Women, 21 and older |
| Colorectal cancer screening | All, 50 and older |
| Lung cancer screening | All, 55 and older |
| Chronic conditions | |
| Lipid disorder screening | All |
| Diabetes screening | All |
| Hepatitis B screening | All |
| Hepatitis C screening | All, 40 and older |
| Obesity screening and counseling | All |
| Osteoporosis screening | Women |
| Immunizations | |
| Flu | All |
| Other immunizations | All |
| Reproductive health and pregnancy | |
| Sexually transmitted infection (STI) screening | All |
| Anemia screening | Pregnant women |
| Bacteriurea screening | Pregnant women |
Eligible preventive services were identified using the MarketScan® annual outpatient services files. Each outpatient service claim has up to 4 diagnosis codes and a single procedure code, all of which were used to identify relevant services. We obtained preventive service coding guidelines from UnitedHealthcare, Cigna, Kaiser Permanente (of Washington), Blue Cross Blue Shield (of North Dakota), and the Centers for Disease Control and Prevention, which were used to identify the specific underlying preventive services using both diagnosis (International Classification of Disease [ICD] 9th and 10th edition codes) and procedure (Current Procedural Terminology [CPT] and Healthcare Common Procedure Coding System [HCPCS]) codes.13,49-52 A harmonized code set from all 5 sources was developed and used to identify preventive services eligible for elimination of cost-sharing, with individual claims flagged as an enrollee having received the service if at least one applicable diagnosis and procedure code were listed (Supplemental Appendix Table 2). We excluded preventive services that took place during an emergency department (ED) visit (approximately 2% of outpatient preventive services) or inpatient admission (approximately 7% of non-ED outpatient preventive services included; nearly all of which were lipid disorder, diabetes, and obesity screening) as we were seeking to identify preventive services used in a primary care or outpatient setting, not those incidental to an acute event where patients may not be making decisions themselves. The out-of-pocket costs for claims occurring on the same day (eg, an HPV vaccine without cost-sharing as part of an office visit subject to cost-sharing) would not be considered out-of-pocket costs for preventive care unless they also were a preventive service (ie, wellness visit). We also identified and aggregated costs for eligible preventive services to the person-year level, capturing realized out-of-pocket costs for these services, by summing across the eligible preventive service claims within a given person-year. A small number of person-years with negative summed values for total, plan, or out-of-pocket costs for eligible preventive services were dropped, representing approximately three-tenths of 1% (0.3%) of the observations in each sample. HDHP enrollment is defined as an indicator equal to one if the plan type corresponds to either a high deductible plan with or without a saving option, and zero otherwise (non-HDHP EPO, HMO, POS, or PPO plan types). We excluded those with plan types of “basic/major medical,” “comprehensive,” and “POS with capitation,” representing approximately 3% of the person-years in the cross-sectional sample and persons in the cohort sample.
Our models include controls for demographic characteristics, including a cubic spline of age (age, age squared, and age cubed each interacted with indicators for being aged 35-49 and 50-64), sex, relationship to policy holder (self, spouse, dependent), employment status of policy holder (full-time, part-time, other, or unknown), employment classification of policy holder (salary, hourly, other, or unknown), and geographic location, including living in a metropolitan statistical area (MSA) and state fixed effects. Those with missing state identifiers and those who moved states were excluded (less than 1% of enrollees). We accounted for prior health status by deriving several measures of comorbidity burden, using diagnoses observed in either inpatient or outpatient service claims in 2009. We calculated both Charlson (17 underlying conditions) and Elixhauser (31 underlying conditions) comorbidity indices and defined indicators for the underlying conditions within each index.53,54 We tested the performance of both indices and sets of condition indicators with our sample, finding that using the set of Elixhauser condition indicators provided the greatest explanatory power. We also calculated the number of inpatient admissions and number of prescriptions (unique generic drug names) in each person-year to capture contemporaneous changes in health status. We also control for the source of the underlying data, from either an employer or health plan. We also created a subsample with 3 years of continuous enrollment to construct a 12-month comorbidity look-back period for comparison with the 6-month measure.
Statistical Analysis
Using the cross-sectional sample, we first described the trend in HDHP enrollment over the study period. We then compared trends in use of and real average per capita annual costs (total and out-of-pocket) for eligible preventive services by plan type (HDHP or not). We inflated nominal dollar values to 2016 dollars using the Consumer Price Index for Medical Care. Using the cohort sample, we estimated difference-in-differences models to isolate whether those enrolled in HDHPs have a differential response to the elimination of cost-sharing for certain high-value preventive services in late 2010.
We used both parametric (DID) and semi-parametric (SDID) difference-in-differences models to estimate the average treatment effect on the treated, the differential change in use of preventive services from 2010 to 2011 among those continuously enrolled in a HDHP versus not. We also explored whether heterogeneous treatment effects were present by sex or tertiles of the Elixhauser comorbidity index. The full cohort sample was used to model any use of an eligble preventive service while the appropriate subsamples were used to estimate category- and service-level use (as specified in Table 1). The parametric difference-in-differences model assumes parallel counterfactual trends between the treatment and control groups, which can be difficult to justify empirically and theoretically, particularly when endogenous selection into treatment occurs. Those choosing to enroll in and remain in HDHPs, given the option, have varying reasons for doing so. Income plays a role, as those of higher income may be willing to bear the risk of reaching the out-of-pocket maximum and those of low income are often forced to risk higher potential out-of-pocket costs in exchange for lower premiums. Health status and expected health care use also play a role, as both those who expect costs well above the out-of-pocket maximum and those who expect very low costs may be incentivized to choose HDHPs.30,55-57
As such, our preferred approach in this context is to employ a semi-parametric difference-in-differences estimator, which uses a propensity score for the probability of treatment to reweight observations based on the distribution of the observable characteristics at baseline within each group.58,59 The parametric model is identified off of the assumption that “average outcomes for treated and controls would have followed parallel paths in absence of treatment” and that selection into treatment is not dependent on “individual-transitory shocks,” 58 which may not be plausible when selection into endogenous treatment is occurring. The semi-parametric approach imposes the same distribution of observables across groups and thus relaxes the strong parallel trends assumption with quasi-random treatment by explicitly accounting for selection into treatment. The weights used by the Abadie estimator are different from standard propensity score-based inverse probability of treatment weights and the estimation explicitly relies on the within-person change in outcome rather than treating it as a 2-period cross-section or panel.58,59 SDID also treats the propensity scores as estimated rather than as given, as the latter can potentially result in artificially small standard errors. 59 Recent work has highlighted issues with matching methods used with difference-in-difference estimators60-62; however, unlike propensity score matching approaches, the Abadie estimator reweights observations rather than performing explicit matches of observations between groups.
The MarketScan® annual enrollment files and inpatient, outpatient, and pharmacy claims data were processed using SAS® 9.4 for Linux and analyses were subsequently conducted in Stata® 13.0 for Linux. The Abadie semi-parametric difference-in-differences models were estimated using the user-written absdid package for Stata® with the sle (logistic regression) option specified to force the propensity scores to be bounded between 0 and 1. 63 We modified the program to output the propensity scores generated using our preferred specification to test for covariate balance between the reweighted treatment (HDHP) and control (non-HDHP) groups. We perform multiple comparisons using the same sample for multiple outcomes and estimators, which increases the likelihood of false positives in terms of statistical significance. Though there is considerable disagreement about the need to adjust for multiple comparions,64,65 we indicate statistical significance based on unadjusted p-values and note which are no longer significant based on a Bonferroni correction, using n = 50 for the number of unique outcome-estimator combinations. This study was approved as exempt by the Non-Biomedical Institutional Review Board at the University of North Carolina at Chapel Hill.
Results
Cross-Sectional Sample
In our cross-sectional sample, consisting of nearly 185 million person-years (n = 184 976 384), HDHP enrollment rose steadily from 2.9% in 2008 to 21.6% in 2016. Those enrolled in a HDHP were approximately 1 year younger on average (41.2 vs 42.2) and female representation was slightly lower (51.9% vs 52.6%). Policy holders (60.7% vs 62.4%) were less prevalent and dependents (12.6% vs 11.1%) were more prevalent in HDHPs. Part-time employment (of the policy holder) representation in HDHPs was low but approximately double that of non-HDHPs (1.7% vs 0.9%). Hourly paid employment (of the policy holder) was more prevalent in the HDHP group (18.9% vs 14.6%). HDHP enrollees were also more likely to live in a metropolitan statistical area (86.5% vs 84.5%).
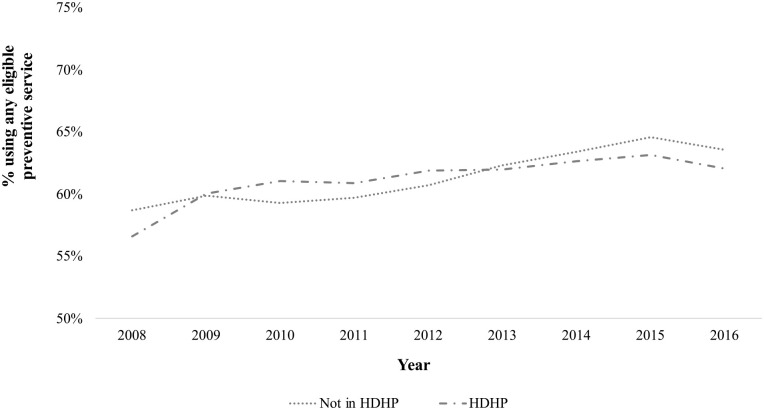
Use of any of the preventive services covered under this Affordable Care Act provision increased from 2008 to 2016 (Figure 1). Those in HDHPs had lower rates of using any of the eligible preventive services than those in non-HDHPs at the beginning (56.6% vs 58.8%) and end (62.1% vs 63.6%) of the study period with the difference in use between the groups narrowing somewhat from 2008 (2.1 percentage points lower) to 2016 (1.5 percentage points lower). Similarly, real average annual per capita total (Supplemental Appendix Figure 1) and out-of-pocket costs (Supplemental Appendix Figure 2) incurred for eligible preventive services also increased during this time period. HDHP enrollees incurred lower real average annual per capita total costs for eligible preventive services initially ($435.08 vs $509.41 in 2008) than those not in a HDHP and the difference increased by one-third during the study period ($615.39 vs $714.67 in 2016). The groups incurred very similar out-of-pocket costs initially ($62.47 for HDHP and $65.49 for non-HDHP in 2008) but cost-sharing grew faster for the HDHP group during the study period ($103.21 for HDHP vs $79.83 for non-HDHP in 2016). These results show that at a population level, any use of eligible preventive services increased during this time period with a corresponding increase in average per capita total costs. There were no obvious changes in use or total costs coincidental with the timing of the policy change between 2010 and 2011. Our conclusions about the effect, or lack thereof, of the policy in substantially reducing or eliminating out-of-pocket costs for eligible preventive services do not change if we condition on any use of a preventive service. However, changes in the composition of the MarketScan® sample over the study period and endogenous plan selection make drawing strong conclusions from cross-sectional findings difficult.
Figure 1.
Use of Any Eligible Preventive Service by HDHP Enrollment, Cross-sectional Sample.
Cohort Sample
In our cohort sample, consisting of 9 253 241 non-elderly adults continuously enrolled from the second half of 2009 through 2011, approximately 6% (6.3%) were enrolled in HDHPs. This is slightly lower than the prevalence of HDHP enrollment in the cross-sectional sample during these years (7.8% in 2010 and 8.1% in 2011) as the continuous enrollment required tends toward higher representation of more generous employer sponsored coverage as a result of lower churn in group versus non-group markets. 66 Table 2 contains unweighted and weighted baseline (2010) descriptive statistics for the cohort sample by HDHP enrollment. In the unweighted results, the average age and distribution of sex were similar across groups. Spouses were present at a higher percentage in the HDHP group (30.3%vs 28.4%), indicating that spousal and family coverage may be more prevalent in that group. Part-time employment (of the policy holder) representation in HDHPs was nearly than fivefold that of non-HDHPs (3.9% vs 0.8%). Hourly paid employment (of the policy holder) was also overrepresented in the HDHP group (17.4% vs 16.7%) with the caveat of a large other or unknown group. HDHP enrollees were slightly less likely to live in a metropolitan statistical area (85.5% vs 86.4%). HDHP enrollees used fractionally more unique prescriptions (11.3 vs 11.0) but showed only small differences in number of inpatient admissions (0.05 vs 0.06) and Elixhauser comorbidity index (0.26 vs 0.29). From this, we observe weak evidence of possible advantageous selection into HDHPs on average but also that price sensitivity on premium costs may be driving selection (ie, higher spousal representation and part-time employment). In comparing the performance of 6- and 12-month Elixhauser comorbidity indices in the subsample with both available, we find a wider gap between the HDHP (0.41) and non-HDHP (0.48) groups that maintains the same rank order of the 6-month measure (0.26 for HDHP and 0.30 for non-HDHP), again indicating potentially slightly healthier individuals on average sorting into the HDHP group. After weighting, the differences in distributions of employment status of the policy holder (ie, full-time, part-time), employment classification of policy holder (ie, salary, hourly), data from health plan, and number of inpatient admissions narrowed considerably between groups.
Table 2.
Unweighted and Weighted Baseline (2010) Sample Characteristics by HDHP Enrollment, Cohort Sample.
| Mean or % (SE) |
||||
|---|---|---|---|---|
| Characteristic |
Unweighted
|
Weighted
|
||
| Not in HDHP | HDHP | Not in HDHP | HDHP | |
| Age | 43.6 (0.004) | 43.7** (0.02) | 43.7 (0.004) | 42.2** (0.05) |
| Female | 52.7% (0.02%) | 53.3%** (0.1%) | 52.8% (0.02%) | 51.9%** (0.2%) |
| Relationship to policy holder | ||||
| Self | 65.7% (0.02%) | 63.5%** (0.1%) | 65.5% (0.02%) | 63.2%** (0.2%) |
| Spouse | 28.4% (0.02%) | 30.3%** (0.1%) | 28.5% (0.02%) | 30.1%** (0.2%) |
| Dependent | 6.0% (0.01%) | 6.2%** (0.03%) | 6.0% (0.01%) | 6.6%** (0.1%) |
| Employment status of policy holder | ||||
| Full-time | 53.9% (0.02%) | 85.0%** (0.05%) | 55.9% (0.02%) | 47.9%** (0.2%) |
| Part-time | 0.8% (0.003%) | 3.9%** (0.03%) | 1.0% (0.004%) | 1.1%** (0.01%) |
| Other, unknown | 45.3% (0.02%) | 11.1%** (0.04%) | 43.1% (0.02%) | 51.0** (0.2%) |
| Employment classification of policy holder | ||||
| Salary | 18.6% (0.01%) | 53.9%** (0.1%) | 21.1% (0.01%) | 22.2%** (0.1%) |
| Hourly | 16.7% (0.01%) | 17.4%** (0.05%) | 16.7% (0.01%) | 18.5%** (0.1%) |
| Other, unknown | 64.7% (0.02%) | 28.7%** (0.1%) | 62.2% (0.02%) | 59.4%**(0.2%) |
| In MSA | 86.4% (0.01%) | 85.5%** (0.05%) | 86.4% (0.01%) | 92.1%** (0.1%) |
| Data from health plan (versus employer) |
40.6% (0.02%) | 2.7%** (0.02%) | 38.1% (0.02%) | 46.3%** (0.2%) |
| Number of unique prescriptions |
11.0 (0.01) | 11.3** (0.02) | 11.0 (0.01) | 8.2** (0.1) |
| Number of inpatient admissions | 0.06 (0.0001) | 0.05** (0.0004) | 0.06 (0.0001) | 0.06 (0.002) |
| Elixhauser comorbidity index (6-month lookback, 2009) |
0.29 (0.001) | 0.26** (0.002) | 0.29 (0.001) | 0.26**(0.01) |
HDHP = high deductible or consumer-driven health plan, MSA = metropolitan statistical area.
P < .01.
Any use of eligible preventive services among the cohort sample shows that HDHP enrollees were somewhat more likely than the non-HDHP group to use preventive services in 2010, and that gap widened slightly in 2011 from 1.3 to 1.6 percentage points (Supplemental Appendix Table 3). Any use increased significantly among both groups from 2010 to 2011 with a slightly larger absolute increase for the HDHP group. Real average annual per capita total costs incurred for eligible preventive services grew during this time period (Supplemental Appendix Table 3). Real per capita total costs increased on average by $51 for the non-HDHP group (from $628.08 to $678.61, P < .01) and by $58 for the HDHP group (from $562.99 to $621.44, P < .01). HDHP enrollees had higher average real per capita out-of-pocket costs for potentially eligible preventive services in both years and experienced a larger year-over-year increase than the non-HDHP enrollees (Supplemental Appendix Table 3). The increases in preventive service use, whether caused by the policy or incidental to the policy change as part of a secular increasing trend, were not met with the promised elimination or even a reduction in average out-of-pocket costs realized for the services targeted by the provision.
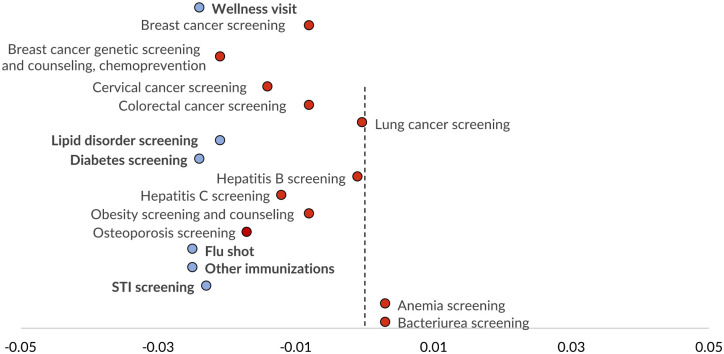
Table 3 shows the difference-in-difference estimates of the average treatment effect on the treated with the DID and SDID estimators. Our preferred SDID results imply that HDHP enrollment was associated with a reduction in the post-ACA change in any use of eligible preventive services by 0.2 percentage points, which corresponds to 12.5% of the observed year-over-year change of 1.6 percentage points among HDHP enrollees (Supplemental Appendix Table 3) and an 11.1% decrease based on the implied counterfactual year-over-year change (of 1.8 percentage points). This 0.2 percentage point effect is 33.3% of the implied policy effect of a 0.6 percentage point increase in any use year-over-year from the full DID model (Table 3, column 4). We find significant heterogenous treatment effects of HDHP enrollment by age (50-64: +0.5 percentage points) and sex (female: +0.3 percentage points), but not by tertiles of the Elixhauser comorbidity index in the SDID model for any use (not shown). Category-specific estimates (health promotion, cancer, chronic conditions, immunizations, reproductive health, and pregnancy) of the average treatment effect on the treated are shown in Supplemental Appendix Table 4. Our SDID estimates imply negative effects of HDHP enrollment on responsiveness to the policy change for 4 of the 5 categories, including health promotion (−0.2 percentage points), chronic conditions (−0.5 percentage points), immunizations (−0.6 percentage points), and reproductive health and pregnancy (−0.4 percentage points), relative to non-HDHP enrollees. Service-specific estimates are shown in Figure 2 and Supplemental Appendix Table 5, with negative estimated effects of HDHP enrollment indicated for 11 of 17 services included compared to 4 null and 2 positive effects. We ran several alternate sets of models to confirm the robustness of our findings (not shown), including dropping those aged 18 to 26 (those potentially eligible for the dependent coverage provision that was implemented coincident to this policy change) and using the subsample with a 12-month comorbidity look-back period (36 months of continuous enrollment rather than 30), yielding qualitatively similar findings. We also used 2 subsamples of our cohort—1) those with at least one claim of any kind during first 6 months of 2010 and 2) those with at least one claim during first 6 months of 2010 and none for preventive care—to assess how this relationship changes when focusing on those with known interactions with the health care system (Supplemental Appendix Table 6). We found that our results generally got larger in magnitude (negatively) and maintained or gained statistical significance, indicating that the depressive association of HDHPs with use of preventive care was more even pronounced.
Table 3.
Difference-In-Differences Estimates of the Effect of HDHP Enrollment on Any Use of Eligible Preventive Services.
| Model, b (SE) | ||||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Any preventive service use | ||||
| DID | ||||
| HDHP | −0.004** (0.001) | −0.007** (0.001) | 0.001*^ (0.001) | 0.003** (0.001) |
| Post | 0.004** (0.0002) | 0.004** (0.0002) | 0.003** (0.0002) | 0.006** (0.0002) |
| HDHP × Post | 0.002**^ (0.001) | 0.002**^ (0.001) | 0.001 (0.001) | 0.002 (0.001) |
| Adjusted R 2 | 0.123 | 0.127 | 0.173 | 0.194 |
| SDID | ||||
| HDHP × Post | 0.001 (0.001) | −0.0001 (0.001) | −0.002*^ (0.001) | −0.002*^ (0.001) |
| Demographic controls | X | X | X | X |
| Geographic controls | X | X | X | |
| # of inpatient admissions and unique prescriptions | X | X | ||
| Comorbidity indicators
(6-month lookback) |
X | |||
| N (persons) | 9253 241 | 9253 241 | 9253 241 | 9253 241 |
DID = parametric difference-in-difference (OLS); SDID = semi-parametric difference-in-differences (Abadie).
P < .05. **P < .01.
^No longer statistically significant after Bonferroni correction for multiple comparisons.
Figure 2.
Difference-In-Differences Estimates of the Effect of HDHP Enrollment on Use of Eligible Preventive Services.
Blue: P < .05, red: not significant; reflecting SDID average treatment effects on the treated shown in Supplemental Appendix Table 5.
Discussion
Our results suggest that enrollment in a high deductible health plan was associated with a smaller increase, by approximately one-eighth, in use of eligible preventive services for which cost-sharing was eliminated by the ACA. These findings build upon prior research showing that consumers respond to higher cost-sharing burdens by reducing use of all care, regardless of its inherent clinical value, 14 which only becomes more meaningful as enrollment in HDHPs continue to rise.14-18 Unlike prior research, which has focused on a single or smaller set of preventive services,41-45 we incorporate nearly all of the billable services that were subject to the late 2010 provision. Other studies have found null or positive effects of the cost-sharing exemption for cancer screening among HDHP enrollees after the policy change and encouragingly,41,42,45 we also find that cancer screenings were seemingly unaffected by the disincentive imposed by higher deductibles to not use medical care. We do, however, find that high deductible health plan enrollment was associated with smaller increases in use of wellness visits, immunizations, and screening for chronic conditions and sexually transmitted infections.
Our study has several limitations. Though our approach can arguably support causal claims, the potential for residual confounding in this specific context is not trivial and therefore we are choosing to describe our findings as associations. The potential endogeneous selection into HDHPs, assuming several plan options were available, is problematic given that we do not observe income, plan choice set, and other characteristics that could be used to model plan choice. 67 Others have addressed this problem by using forced switches into a HDHP at the employer level with similar non-switching employers serving as a control group.33,45,68,69 We chose a more generalizable sample with a semi-parametric approach that does not assume quasi-random group assignment, estimating an underlying propensity score for selection into treatment and using these to reweight the sample for estimation. 58 With only state identifiers available, we were unable to account for local differences in primary care provider availability that could play a role as a supply constraint. We are, however, able to isolate the utilization response conditional on the physician supply environment that each enrollee faces by using a cohort of adults continuously enrolled before and after the policy change who do not move between states. We are also unable to identify which plans were modified to comply with this and other ACA provisions versus those that were grandfathered for the 2011 plan year, as this information is not provided in the MarketScan® data. Grandfathered plans have largely disappeared from the individual (non-group) market, now estimated to be less than 7% of total enrollment. 70 In the group market, there is a similar downward trend with grandfathered plan enrollment falling from a base of just over half (56%) in 2011 to just over a third (36%) just 2 years later. 71 As long as grandfathered plan status was not associated with whether a plan had a high deductible or not (eg, plan modification decisions being made at the insurer-rating area level or employer level), this concern is minimized for our analysis. Also, insurers were responsible for creating their own coding guidelines to operationalize the ACA provision that eliminated cost-sharing for eligible preventive services, with providers needing to adhere specifically in order for enrollees to be billed (or not, in this case) appropriately. Consumers and providers alike ended up being confused by this, with patients receiving surprise bills for so-called “free” preventive services.72-74 As we cannot identify specific insurers in our data, it is not possible to match the applicable coding guidelines exactly to each enrollee. Therefore, we created a comprehensive list of covered diagnosis and procedure code combinations provided by the federal government and several large insurers to capture the services that were supposed to be exempt from cost-sharing. The small amount of revenue involved also calls into question whether providers would be quick to adapt to coding changes given that prior evidence found that only about half of hospitals responded to a change in Medicare coding that would have resulted in a 2% revenue gain.75,76 Also, MarketScan® skews heavily toward large employer plans in its composition, which may have been more likely to cover preventive care at zero out-of-pocket cost before the ACA, meaning our results may be conservative relative to all commercially insured Americans generally.
Plan choice and understanding the nuances of benefit design is challenging for consumers, often resulting in less than optimal choices of plans (eg, choosing dominated plans), and use of care (eg, failing to use high-value preventive care available without cost-sharing), suggesting that more can be done during open enrollment and early in the plan year to support decision making.75,77-84 There are also potential mismatches between ex ante and ex post expectations of cost-sharing for preventive services. An extreme but common example is that a patient goes in for a screening colonoscopy, not subject to cost-sharing, but a polyp is found and removed causing the service to be billed as a diagnostic colonoscopy instead, now subject to cost-sharing. This change in cost-sharing based on the outcome of the preventive service itself is far from consumer-friendly and has yielded a lot of confusion.85-87 Unfortunately, our results also suggest that the provision of the ACA that eliminated cost-sharing for eligible preventive services was unsuccessful in reducing out-of-pocket costs for consumers, the linchpin incentive for consumers to increase their use of preventive services. Future research can help us understand whether there is heterogeneity in the out-of-pocket cost experience with specific services covered by this ACA provision. If use of preventive services is less than optimal and out-of-pocket costs continue to be a barrier, then how the policy is operationalized may need to be reconsidered.
Supplemental Material
Supplemental material, sj-docx-1-inq-10.1177_00469580231182512 for High Deductible Health Plans and Use of Free Preventive Services Under the Affordable Care Act by Paul R. Shafer, Stacie B. Dusetzina, Lindsay M. Sabik, Timothy F. Platts-Mills, Sally C. Stearns and Justin G. Trogdon in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
The authors would like to thank seminar attendees at the University of North Carolina at Chapel Hill, University of Utah, Boston University, and Harvard University, and attendees of the 2019 AcademyHealth Annual Research Meeting and American Society of Health Economists Annual Conference for their helpful comments. The data infrastructure used for this project was funded by the Department of Epidemiology in the Gillings School of Global Public Health, School of Medicine, Cecil G. Sheps Center for Health Services Research, and CER Strategic Initiative under a Clinical and Translational Science Award (UL1TR001111) to the University of North Carolina at Chapel Hill from the National Center for Advancing Translational Sciences at the National Institutes of Health.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from the Robert Wood Johnson Foundation (73923) and Horowitz Foundation for Social Policy to Dr. Shafer.
ORCID iD: Paul R. Shafer  https://orcid.org/0000-0003-0654-5821
https://orcid.org/0000-0003-0654-5821
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Borsky A, Zhan C, Miller T, Ngo-Metzger Q, Bierman AS, Meyers D.Few Americans receive all high-priority, appropriate clinical preventive services. Health Aff. 2018;37(6):925-928. doi: 10.1377/hlthaff.2017.1248 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Healthy People – Healthy People 2020. Published November 6, 2015. Accessed May 9, 2018. https://www.cdc.gov/nchs/healthy_people/hp2020.htm
- 3.Healthy People 2020. Midcourse review: LHIs. n.d. Accessed October 17, 2018. https://www.healthypeople.gov/2020/data-search/midcourse-review/lhi [DOI] [PMC free article] [PubMed]
- 4.Carroll AE.Preventive care saves money? Sorry, it’s too good to be true. New York Times, January29, 2018. [Google Scholar]
- 5.Hashim A, Dang V, Bolotin S, Crowcroft NS.How and why researchers use the number needed to vaccinate to inform decision making—a systematic review. Vaccine. 2015;33(6):753-758. doi: 10.1016/j.vaccine.2014.12.033 [DOI] [PubMed] [Google Scholar]
- 6.Kristiansen IS, Gyrd-Hansen D.Cost-effectiveness analysis based on the number-needed-to-treat: common sense or non-sense? Health Econ. 2004;13(1):9-19. doi: 10.1002/hec.797 [DOI] [PubMed] [Google Scholar]
- 7.Rossignol M, Labrecque M, Cauchon M, Breton M-C, Poirier P.Number of patients needed to prescribe statins in primary cardiovascular prevention: mirage and reality. Fam Pract. 2018;35(4):376-382. doi: 10.1093/fampra/cmx124 [DOI] [PubMed] [Google Scholar]
- 8.Taylor FC, Huffman M, Ebrahim S.Statin therapy for primary prevention of cardiovascular disease. J Am Med Assoc. 2013;310(22):2451-2452. doi: 10.1001/jama.2013.281348 [DOI] [PubMed] [Google Scholar]
- 9.Tuite AR, Fisman DN.Number-needed-to-vaccinate calculations: fallacies associated with exclusion of transmission. Vaccine. 2013;31(6):973-978. doi: 10.1016/j.vaccine.2012.11.097 [DOI] [PubMed] [Google Scholar]
- 10.Patient Protection and Affordable Care Act. 42 U.S.C. § 18001 et seq, 2010. [Google Scholar]
- 11.healthcare.gov. Marketplace options for grandfathered health insurance plans. n.d. Accessed October 17, 2018. https://www.healthcare.gov/health-care-law-protections/grandfathered-plans/
- 12.Kaiser Family Foundation. Preventive services covered by private health plans under the affordable care act. Published August 4, 2015. Accessed October 17, 2018. https://www.kff.org/health-reform/fact-sheet/preventive-services-covered-by-private-health-plans/
- 13.UnitedHealthcare. Preventive care services. 2018. Accessed October 15, 2018. https://www.uhcprovider.com/content/dam/provider/docs/public/policies/comm-medical-drug/preventive-care-services.pdf
- 14.Agarwal R, Mazurenko O, Menachemi N.High-deductible health plans reduce health care cost and utilization, including use of needed preventive services. Health Aff. 2017;36(10):1762-1768. doi: 10.1377/hlthaff.2017.0610 [DOI] [PubMed] [Google Scholar]
- 15.Beeuwkes Buntin M, Haviland AM, McDevitt R, Sood N.Healthcare spending and preventive care in high-deductible and consumer-directed health plans. Am J Manag Care. 2011;17(3):222-230. [PubMed] [Google Scholar]
- 16.Mazurenko O, Buntin MJB, Menachemi N.High-deductible health plans and prevention. Annu Rev Public Health. 2019;40:411-421. doi: 10.1146/annurev-publhealth-040218-044225 [DOI] [PubMed] [Google Scholar]
- 17.Cohen RA, Zammitti EP, Martinez ME.Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey. National Center For Health Statistics; 2018. [Google Scholar]
- 18.Kaiser Family Foundation. 2016Employer health benefits survey. Publisher September14, 2016. Accessed October 17, 2018. https://www.kff.org/report-section/ehbs-2016-summary-of-findings/
- 19.Dolan R.High-deductible health plans. Publisher February 4, 2016. Accessed October 29, 2018. https://www.healthaffairs.org/do/10.1377/hpb20160204.950878/full/
- 20.Polyakova M, Hua LM, Bundorf MK.Marketplace plans provide risk protection, but actuarial values overstate realized coverage for most enrollees. Health Aff. 2017;36(12):2078-2084. doi: 10.1377/hlthaff.2017.0660 [DOI] [PubMed] [Google Scholar]
- 21.Agarwal R, Gupta A, Fendrick AM.Value-based insurance design improves medication adherence without an increase in total health care spending. Health Aff. 2018;37(7):1057-1064. doi: 10.1377/hlthaff.2017.1633 [DOI] [PubMed] [Google Scholar]
- 22.Aron-Dine A, Einav L, Finkelstein A.The RAND Health Insurance Experiment, three decades later. J Econ Perspect. 2013;27(1):197-222. doi: 10.1257/jep.27.1.197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brot-Goldberg ZC, Chandra A, Handel BR, Kolstad JT.What does a deductible do? The impact of cost-sharing on health care prices, quantities, and spending dynamics. Q J Econ. 2017;132(3):1261-1318. doi: 10.1093/qje/qjx013 [DOI] [Google Scholar]
- 24.Gupta N, Polsky D.High deductible health plans: does cost sharing stimulate increased consumer sophistication? Health Expect. 2015;18(3):335-343. doi: 10.1111/hex.12031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kullgren JT, Cliff EQ, Krenz C, et al. Consumer behaviors among individuals enrolled in high-deductible health plans in the United States. JAMA Intern Med. 2018;178(3):424-426. doi: 10.1001/jamainternmed.2017.6622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A, Marquis MS.Health insurance and the demand for medical care: evidence from a randomized experiment. Am Econ Rev. 1987;77(3):251-277. [PubMed] [Google Scholar]
- 27.Newhouse JP.Consumer-directed health plans and the RAND health insurance experiment. Health Aff. 2004;23(6):107-113. doi: 10.1377/hlthaff.23.6.107 [DOI] [PubMed] [Google Scholar]
- 28.Sinaiko AD, Mehrotra A, Sood N.Cost-sharing obligations, high-deductible health plan growth, and shopping for health care: enrollees with skin in the game. JAMA Intern Med. 2016;176(3):395-397. doi: 10.1001/jamainternmed.2015.7554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waters TM, Chang CF, Cecil WT, Kasteridis P, Mirvis D.Impact of high-deductible health plans on health care utilization and costs. Health Serv Res. 2011;46(1 Pt 1):155-172. doi: 10.1111/j.1475-6773.2010.01191.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Einav L, Finkelstein A, Ryan S, Schrimpf P, Cullen MR.Selection on moral hazard in health insurance. Am Econ Rev. 2013;103(1):178-219. doi: 10.1257/aer.103.1.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galbraith AA, Soumerai SB, Ross-Degnan D, Rosenthal MB, Gay C, Lieu TA.Delayed and forgone care for families with chronic conditions in high-deductible health plans. J Gen Intern Med. 2012;27(9):1105-1111. doi: 10.1007/s11606-011-1970-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reid RO, Rabideau B, Sood N.Impact of consumer-directed health plans on low-value healthcare. Am J Manag Care. 2017;23(12):741-748. [PMC free article] [PubMed] [Google Scholar]
- 33.Wharam JF, Zhang F, Lu CY, et al. Breast Cancer Diagnosis and treatment after high-deductible insurance enrollment. J Clin Oncol. 2018;36(11):1121-1127. doi: 10.1200/JCO.2017.75.2501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Politi MC, Kaphingst KA, Kreuter M, Shacham E, Lovell MC, McBride T.Knowledge of health insurance terminology and details among the uninsured. Med Care Res Rev. 2014;71(1):85-98. doi: 10.1177/1077558713505327 [DOI] [PubMed] [Google Scholar]
- 35.Reed M, Benedetti N, Brand R, Newhouse JP, Hsu J.Perspectives from deductible plan enrollees: plan knowledge and anticipated care-seeking changes. BMC Health Serv Res. 2009;9:244. doi: 10.1186/1472-6963-9-244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reed ME, Graetz I, Fung V, Newhouse JP, Hsu J.In consumer-directed health plans, a majority of patients were unaware of free or low-cost preventive care. Health Aff. 2012;31(12):2641-2648. doi: 10.1377/hlthaff.2012.0059 [DOI] [PubMed] [Google Scholar]
- 37.Tipirneni R, Politi MC, Kullgren JT, Kieffer EC, Goold SD, Scherer AM.Association between health insurance literacy and avoidance of health care services owing to cost. JAMA Netw Open. 2018;1(7):e184796. doi: 10.1001/jamanetworkopen.2018.4796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Binder S, Nuscheler R.Risk-taking in vaccination, surgery, and gambling environments: evidence from a framed laboratory experiment. Health Econ. 2017;26(suppl. 3):76-96. doi: 10.1002/hec.3620 [DOI] [PubMed] [Google Scholar]
- 39.Robinson LA, Hammitt JK.Valuing reductions in fatal illness risks: implications of recent research. Health Econ. 2016;25(8):1039-1052. doi: 10.1002/hec.3214 [DOI] [PubMed] [Google Scholar]
- 40.Eisenberg MD, Haviland AM, Mehrotra A, Huckfeldt PJ, Sood N.The long term effects of “Consumer-Directed” health plans on preventive care use. J Health Econ. 2017;55:61-75. doi: 10.1016/j.jhealeco.2017.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fedewa SA, Goodman M, Flanders WD, et al. Elimination of cost-sharing and receipt of screening for colorectal and breast cancer. Cancer. 2015;121(18):3272-3280. doi: 10.1002/cncr.29494 [DOI] [PubMed] [Google Scholar]
- 42.Han X, Robin Yabroff K, Guy GP, Jr, Zheng Z, Jemal A.Has recommended preventive service use increased after elimination of cost-sharing as part of the Affordable Care Act in the United States? Prev Med. 2015;78:85-91. doi: 10.1016/j.ypmed.2015.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mehta SJ, Polsky D, Zhu J, et al. ACA-mandated elimination of cost sharing for preventive screening has had limited early impact. Am J Manag Care. 2015;21(7):511-517. [PMC free article] [PubMed] [Google Scholar]
- 44.Sabik LM, Adunlin G.The ACA and cancer screening and diagnosis. Cancer J. 2017;23(3):151-162. doi: 10.1097/PPO.0000000000000261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wharam JF, Zhang F, Landon BE, LeCates R, Soumerai S, Ross-Degnan D.Colorectal cancer screening in a nationwide high-deductible health plan before and after the affordable care act. Med Care. 2016;54(5):466-473. doi: 10.1097/MLR.0000000000000521 [DOI] [PubMed] [Google Scholar]
- 46.IBM Watson Health. The Truven Health MarketScan Databases for Health Services Researchers. Publisher December 2017. Accessed October 16, 2018. https://truvenhealth.com/portals/0/assets/2017_MarketScan_Databases_Health_Services_Researchers.pdf
- 47.Hedden EM, Jessop AB, Field RI.An education in contrast: state-by-state assessment of school immunization records requirements. Am J Public Health. 2014;104(10):1993-2001. doi: 10.2105/AJPH.2014.302078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shaw J, Mader EM, Bennett BE, Vernyi-Kellogg OK, Yang YT, Morley CP.Immunization mandates, vaccination coverage, and exemption rates in the United States. Open Forum Infect Dis. 2018;5(6):ofy130. doi: 10.1093/ofid/ofy130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blue Cross Blue Shield of North Dakota. Preventive health benefits and coding. Published May 2014. Accessed 29, 2018. http://www.bcbsnd.com/documents/10181/324765/preventivehealthservicesandcodingguidelines/bb1bb7b3-f1f9-49c4-9abc-489f108226f4.pdf
- 50.Centers for Disease Control and Prevention. Billing codes. Published September 4, 2014. Accessed October 29, 2018. https://www.cdc.gov/prevention/billingcodes.html
- 51.Cigna. A guIde to Cigna’s preventive health coverage. Published August 2015. Accessed October 29, 2018. http://www.cigna.com/assets/docs/health-care-professionals/807467h-Preventive-Health-Cov-Guide.pdf
- 52.Kaiser Permanente Washington. Coding guidelines for preventive care services commercial (Non-Medicare) Kaiser permanente plans. n.d. Accessed October 29, 2018. https://provider.ghc.org/open/coverageAndEligibility/groupHealthPlans/preventive-services-guidelines.pdf
- 53.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 54.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ.A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626-633. doi: 10.1097/MLR.0b013e31819432e5 [DOI] [PubMed] [Google Scholar]
- 55.Dowd B, Feldman R, Cassou S, Finch M.Health plan choice and the utilization of health care services. Rev Econ Stat. 1991;73(1):85. doi: 10.2307/2109690 [DOI] [Google Scholar]
- 56.Fowles JB, Kind EA, Braun BL, Bertko J.Early experience with employee choice of consumer-directed health plans and satisfaction with enrollment. Health Serv Res. 2004;39(4 Pt 2):1141-1158. doi: 10.1111/j.1475-6773.2004.00279.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Parente ST, Feldman R, Christianson JB.Employee choice of consumer-driven health insurance in a multiplan, multiproduct setting. Health Serv Res. 2004;39(4p2):1091-1112. doi: 10.1111/j.1475-6773.2004.00275.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abadie A.Semiparametric difference-in-differences estimators. Rev Econ Stud. 2005;72(1):1-19. doi: 10.1111/0034-6527.00321 [DOI] [Google Scholar]
- 59.Houngbedji K.Abadie’s semiparametric difference-in-differences estimator. Stata J. 2016;16:482-490. [Google Scholar]
- 60.Daw JR, Hatfield LA.Matching and regression to the mean in difference-in-differences analysis. Health Serv Res. 2018;53(6):4138-4156. doi: 10.1111/1475-6773.12993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Daw JR, Hatfield LA.Matching in difference-in-differences: between a rock and a hard Place. Health Serv Res. 2018;53:4111-4117. doi: 10.1111/1475-6773.13017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lindner S, McConnell KJ.Difference-in-differences and matching on outcomes: a tale of two unobservables. Health Serv Outcomes Res Methodol. 2019;19:127-144. doi: 10.1007/s10742-018-0189-0 [DOI] [Google Scholar]
- 63.Houngbedji K.ABSDID: Stata Module to Estimate Treatment Effect With Abadie Semiparametric DID Estimator (Statistical Software Components S458134). Computer Software, Boston College Department of Economics; 2016. [Google Scholar]
- 64.Rothman KJ.No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43-46. [PubMed] [Google Scholar]
- 65.Gelman A, Hill J, Yajima M.Why We (Usually) don’t have to worry about multiple comparisons. J Res Educ Eff. 2012;5(2):189-211. [Google Scholar]
- 66.Klein K, Glied S, Ferry D.Entrances and exits: health insurance churning, 1998-2000. Issue Brief. 2005;855:1-12. [PubMed] [Google Scholar]
- 67.Crown WH.Specification issues in a big data context: controlling for the endogeneity of consumer and provider behaviours in healthcare treatment effects models. PharmacoEconomics. 2016;34(2):95-100. doi: 10.1007/s40273-015-0362-z [DOI] [PubMed] [Google Scholar]
- 68.Wharam JF, Graves AJ, Landon BE, Zhang F, Soumerai SB, Ross-Degnan D.Two-year trends in colorectal cancer screening after switch to a high-deductible health plan. Med Care. 2011;49(9):865-871. doi: 10.1097/MLR.0b013e31821b35d8 [DOI] [PubMed] [Google Scholar]
- 69.Wharam JF, Graves AJ, Zhang F, Soumerai SB, Ross-Degnan D, Landon BE.Two-year trends in cancer screening among low socioeconomic status women in an HMO-based high-deductible health plan. J Gen Intern Med. 2012;27(9):1112-1119. doi: 10.1007/s11606-012-2057-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Altman D. The ACA stability “crisis” in perspective. Published August 10, 2017. Accessed October 29, 2018. https://www.axios.com/the-aca-stability-crisis-in-perspective-1513304736-b21bb11c-04a8-49e1-a47f-37b0d9fdf7aa.html
- 71.Seiler N, Malcarney M-B, Horton K, Dafflitto S.Coverage of clinical preventive services under the affordable care act: from law to access. Public Health Rep. 2014;129(6):526-532. doi: 10.1177/003335491412900611.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Andrews M. Getting charged for ‘free’ preventive care. January20, 2014. Accessed October 28, 2018. https://www.washingtonpost.com/national/health-science/getting-charged-for-free-preventive-care/2014/01/17/98fbd1fa-7ec2-11e3-95c6-0a7aa80874bc_story.html?noredirect=on&utm_term=.e4ccbae8bc45
- 73.Konrad W.Co-payments or not? Affordable Care Act May Puzzle Patients. New York Times, September19, 2011. [Google Scholar]
- 74.LaMontagne C. Billed for “Free” preventive care. Publisher March9, 2015. Accessed October 29, 2018. https://www.forbes.com/sites/christinalamontagne/2015/03/09/billed-for-free-preventive-care/#374245db3bbb
- 75.Bhargava S, Loewenstein G, Sydnor J.Do Individuals Make Sensible Health Insurance Decisions? Evidence From a Menu With Dominated Options. National Bureau of Economic Research; 2015. [Google Scholar]
- 76.Sacarny A.Adoption and learning across hospitals: the case of a revenue-generating practice. J Health Econ. 2018;60:142-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sinaiko AD, Hirth RA.Consumers, health insurance and dominated choices. J Health Econ. 2011;30(2):450-457. doi: 10.1016/j.jhealeco.2010.12.008 [DOI] [PubMed] [Google Scholar]
- 78.Sinaiko AD, Ross-Degnan D, Soumerai SB, Lieu T, Galbraith A.The experience of Massachusetts shows that consumers will need help in navigating insurance exchanges. Health Aff. 2013;32(1):78-86. doi: 10.1377/hlthaff.2012.0124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wong CA, Kulhari S, McGeoch EJ, et al. Shopping on the public and private health insurance marketplaces: consumer decision aids and plan presentation. J Gen Intern Med. 2018;33(8):1400-1410. doi: 10.1007/s11606-018-4483-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wong CA, Polsky DE, Jones AT, Weiner J, Town RJ, Baker T.For third enrollment period, marketplaces expand decision support tools to assist consumers. Health Aff. 2016;35(4):680-687. doi: 10.1377/hlthaff.2015.1637 [DOI] [PubMed] [Google Scholar]
- 81.Feher A, Menashe I.Using email and letters to reduce choice errors among ACA marketplace enrollees. Health Aff. 2021;40(5):812-819. doi: 10.1377/hlthaff.2020.02099 [DOI] [PubMed] [Google Scholar]
- 82.Yagi BF, Luster JE, Scherer AM, Farron MR, Smith JE, Tipirneni R.Association of health insurance literacy with health care utilization: a systematic review. J Gen Intern Med. 2022;37(2):375-389. doi: 10.1007/s11606-021-06819-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Anderson DM, Rasmussen PW, Drake C.Estimated Plan enrollment outcomes after changes to US health insurance marketplace automatic renewal rules. JAMA Health Forum. 2021;2(7):e211642. doi: 10.1001/jamahealthforum.2021.1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Handel BR, Kolstad RJT. Health insurance for “Humans”: information frictions, plan choice, and consumer welfare. Am Econ Rev. 2015;105(8):2449-2500. doi: 10.1257/aer.20131126 [DOI] [PubMed] [Google Scholar]
- 85.American Cancer Society. Insurance coverage for colorectal cancer screening. Published May 30, 2018. Accessed January 11, 2019. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/screening-coverage-laws.html
- 86.Andrews M. Colonoscopy costs can change for diagnosis vs. screening. Published January 30, 2018. Accessed January 10, 2019. https://www.npr.org/sections/health-shots/2018/01/30/581545006/after-a-polyp-is-found-patients-may-have-to-chip-in-for-colonoscopies
- 87.Colorectal Cancer Alliance. The mystery of cost sharing for colon cancer screening. Published November 4, 2016. Accessed January 11, 2019. https://www.ccalliance.org/news/get-involved/the-mystery-of-cost-sharing-for-colon-cancer-screening
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-inq-10.1177_00469580231182512 for High Deductible Health Plans and Use of Free Preventive Services Under the Affordable Care Act by Paul R. Shafer, Stacie B. Dusetzina, Lindsay M. Sabik, Timothy F. Platts-Mills, Sally C. Stearns and Justin G. Trogdon in INQUIRY: The Journal of Health Care Organization, Provision, and Financing