Abstract
During the early stages of the COVID-19 pandemic, healthcare workers (HcWs) reported having high levels of psychological stress caused by the risk of being infected and infecting their families, social isolation, and inadequate protective equipment. This study aimed to determine the level of anxiety and related factors in HcWs and their children during the first phase of the Covid-19 pandemic in Turkey. Online questionnaires were sent to HcWs with children aged 8-18 years via e-mail and WhatsApp messages. In total, 144 HcWs and 135 of their children participated in this study.
HcWs completed the State-Trait Anxiety Inventory state subscale (STAI-S) and the COVID-19 Risk Perception Scale. Their children completed the Screen for Child Anxiety-Related Emotional Disorders (SCARED). STAI-S and COVID-19 Risk Perception Scale scores of the HcWs in direct contact with COVID-19 patients were significantly higher than of those not in direct contact. Moreover, the children of HcWs that were in direct contact with COVID-19 patients had significantly higher SCARED subscale scores than those whose parents were not in direct contact. There was a significant correlation between the SCARED somatic/panic subscale scores and HcW STAI-S scores. The presence of a mental illness and direct contact with COVID-19 patients were the 2 main predictors of COVID-19 risk perception and the level of anxiety in HcWs. During the Covid-19 pandemic the children of HcWs were observed to be a mentally sensitive group, and preventive mental health programs should be developed.
Keywords: Covıd-19, healthcare workers, children, anxiety
1. Introduction
The COVID- 19 pandemic that emerged in Wuhan China in December 2019 spread rapidly all over the world (Wang et al. 2020). On 11 March 2020 the Turkish Ministry of Health reported the first COVID-19 case in Turkey (RTMH 2019). Then, the Turkish government closed schools, mandated flexible working or working from home, cancelled public events, and put into effect many more pandemic prevention measures. A strict nationwide lockdown procedure was implemented 1 d after the first death from COVID-19 on 15 March 2020, which lasted until 17 May 2021 (RTMH 2021). As of March 2023, the number of deaths in Turkey due to COVID-19 was 102,174 and the number of cases was approximately 17,000,000 (RTMH 2023). In Turkey a health army of approximately 165,000 doctors, 200,000 nurses, and 175,000 other healthcare workers (HcWs) were involved in the fight against COVID-19. The World Health Organization (WHO) estimates that worldwide between 80,000 and 180,000 HcWs died from COVID-19 between January 2020 and May 2021 (WHO 2021), during which time approximately 506 HcWs in Turkey died from COVID-19 (Sant'Ana et al. 2020).
Along with the Covid-19 pandemic's rapid increase in the number of cases, the psychological and physical burden on HcWs increased significantly. In addition to the psychological burden of societal lockdown, HcWs were faced with increased working hours in risky environments (hospitals and home visits for severe cases). Many HcWs were separated from their children for long periods of time due to the risk of infection and fear of transmitting COVID-19. At a time when the number of cases in Wuhan was significantly higher than in other provinces, HcWs in Wuhan reported much higher rates of psychological stress than HcWs in other provinces of China (Dai et al. 2020). Moreover, HcWs had concerns about the risk of infection to themselves and family, social isolation, and inadequate protective equipment, which are associated with depression and anxiety (Dai et al. 2020). HCWs’ children were physically separated from their parents and had negative thoughts about their parents getting infected with COVID-19 and dying (Skokauskas et al. 2022).
A study on the psychological effect of the COVID-19 pandemic on adults and children in Italy observed that HcWs in direct contact with COVID-19 patients reported more psychological distress than those not in direct contact with COVID-19 patients. Moreover, the level of psychological distress and the severity of behavioral problems in the children of HcWs directly involved in healthcare services related to COVID-19 were higher than in children whose HcW parents didn't have direct contact with Covid-19 patients (Davico et al. 2021). To the best of our knowledge whereas there are much data on the mental health of HcWs during the COVID-19 pandemic, little is known about that of their children. The present study aimed to determine the perception of risk and level of anxiety in HcWs during the first months of the Covid-19 pandemic in Turkey, and determine the relationship between the level of anxiety in HcWs and that in their children.
2. Materials and Methods
2.1. Design and participants
An online questionnaire was distributed to HcWs and those with children aged 8-18 years completed the questionnaire with their children via email and WhatsApp. HcWs completed a sociodemographic form, the State-Trait Anxiety Inventory state subscale (STAI-S) and COVID-19 Exposure and Risk Perception Scale, and their children completed the Screen for Child Anxiety-Related Emotional Disorders (SCARED). Among the 144 HcWs participating in the study, 9 of their children did not complete SCARED. The study protocol was approved by the ethics committee, and all the participants provided informed consent. Data were collected between April and June 2020. Ethics committee approval was obtained from XXXXX (19.08.2020-9176).
2.2. Assessments and sociodemographic data
A sociodemographic form was used to collect such data as HCWs’ age, gender, marital status, and income, and who they live with, how many children they have, and their occupation. In addition, HCWs were asked to report if they had direct contact with COVID-19 patients, if they had a chronic illness or a medical condition that could be a risk factor for COVID-19, if they had a psychiatric illness, if they had been infected with COVID-19, and who took care of their children during the COVID-19 pandemic. Direct contact with COVID-19 patients was defined as being responsible for the care, follow-up, and treatment of active COVID-19 patients.
2.3. Covid-19 Exposure and Risk Perception Scale
In order to evaluate the risk perception of HcWs this study used a Turkish version of the 6-item 5-point Likert-type Covid-19 Exposure and Risk Perception Scale used by Dai et al. (2020). After the scale was translated into Turkish, it was back-translated into English and validated. The scale's 6 items are as follows: 1. Are you worried about being infected with Covid-19? 2. Are you worried that your family members will be infected by you? 3. Are you worried that you may be abused by COVID-19 patients or their relatives? 4. Are you worried about your colleagues that have direct contact with Covid-19 patients? 5. Are you worried about the lack of preventive measures? 6. Are you worried about current COVID-19 control and prevention strategies? Lower scores indicate higher levels of concern related to Covid-19.
2.4. State-Trait Anxiety Inventory (STAI)
STAI was developed by Spielberger et al. (1970) and has 2 subscales: state (STAI-S) and trait (STAI-T). There are 40 items in total; 20 items on each subscale. STAI-S measures how an individual feels at a certain point in time and under certain conditions. STAI-T measures how an individual generally feels, regardless of time and circumstances. Items are answered using a 4-point Likert-type scale (1-4) and higher scores indicate higher levels of anxiety. The Turkish version was reported to be valid and reliable by Öner and Le Compte (1983). The internal consistency coefficients for the scale range from 0.86 to 0.95, and the test-retest reliability coefficients range from 0.65 to 0.75 over a 2-month period (Spielberger, Gorsuch, Lushene, Vagg, and Jacobs 1983). Some researchers used a cut-off score of 40 to define possible clinical anxiety (Ercan et al. 2015; Vigneau and Cormier 2008). In the present study only the STAI-S was used to assess the level of anxiety associated with stress experienced during the COVID-19 pandemic.
2.5. Screen for Child Anxiety-Related Emotional Disorders (SCARED)
SCARED was developed by Birmaher et al. (1997) for screening anxiety disorders in children. The Turkish version was reported to be valid and reliable by Çakmakcı et al. (2004). This scale consists of 41 items and the following 5 subscales: somatic/panic; generalized anxiety; social anxiety; separation anxiety; school anxiety. In this study a 30-item version was used (items on the social anxiety and school anxiety subscales were removed) and the items were answered using a 3-point Likert-type scale (1: incorrect or rarely true; 2: sometimes or partially true; 3: very true or mostly true). The internal consistency coefficients for the scale range from 0.74 to 0.89 and the test-retest reliability coefficients range from 0.70 to 0.90 over a 5-week period.
2.6. Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows v.22.0 (IBM Corp., Armonk, NY). To verify that the study sample size was sufficient for the analyses a power calculation was performed based on G × power. The power was set at 99% and the significance level at α = 0.01, with an effect size of d = 0.5; a sample size of n = 68 was suggested. The chi-square (χ2) test was used for between-group comparison of categorical variables. Student's t-test was applied for between-group comparison of continuous variables. Correlations between age of the children, Covid-19 Exposure and Risk Perception Scale score, STAI-S score, and SCARED subscale scores were assessed using Pearson's correlation analysis. Multiple linear regression tests were performed to identify the predictors of Covid-19 Exposure and Risk Perception Scale and STAI-S scores. The level of statistical significance was set at P < 0.05.
3. Results
The study included 144 HcWs (14 [9.7%] male and 130 [90.3%] female) and 135 of their children aged 8-18 years. In all, 129 (89.6%) of the HcWs were married, 87.5% lived with their spouses and children, 11.1% lived with their children only, and 1.4% lived alone. Among the HcWs, there were 99 medical doctors, 14 dentists, 14 nurses, 4 cleaning staff, 3 child development specialists, 3 dietitians, 2 psychologists, 2 emergency medicine technicians, 1 midwife, 1 medical secretary, and 1 laboratory technician. In total, 61.1% of the HcWs had direct contact with Covid-19 patients. Among the HcWs, 27.8% had a medical disease or used a medication that could aggravate Covid-19 infection. Only 1 of the HcWs was diagnosed with COVID-19. During the pandemic, 95.1% of the HcWs slept at home, whereas 3.5% slept at hotels or guesthouses. HcW demographic data are summarized in Table 1 .
Table 1.
HcW demographic variables.
| N | % | |
|---|---|---|
| Participants | ||
| Medical doctor | 99 | 68.7 |
| Dentist | 14 | 9.7 |
| Nurse | 14 | 9.7 |
| Others | 17 | 11.8 |
| Dealing with a child during the Covid-19 pandemic | ||
| Partners | 44 | 30.8 |
| Childminder | 30 | 21.0 |
| Grandfather | 24 | 16.8 |
| Be alone at home | 45 | 31.5 |
| Psychiatric illness | ||
| No disease | 124 | 86.1 |
| Previous | 11 | 7.6 |
| Ongoing | 5 | 3.5 |
| Newly diagnosed | 4 | 2.8 |
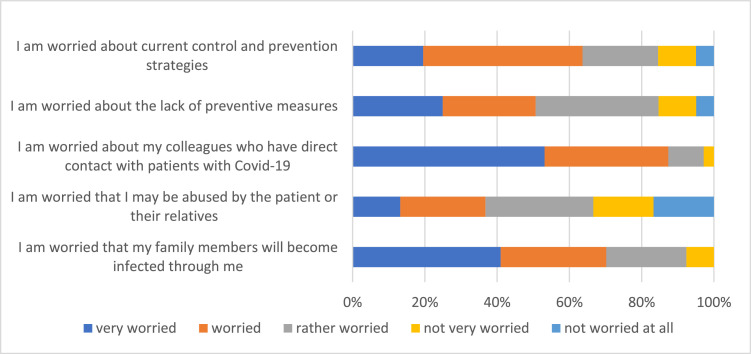
The risk perceptions of the HcWs regarding the COVID-19 pandemic are summarized in Figure 1 and were rated from 1 to 5. The mean Covid-19 Exposure and Risk Perception Scale score was 13.82 ± 4.64. The mean STAI-S score was 47.94 ± 11.29 and 76.4% of the HcWs scored above the cut-off point of 40. As the Covid-19 Exposure and Risk Perception Scale score decreased, which means higher risk perception, the STAI-S score also increased (r = –0.617, P ˂ 0.001).
Figure 1.
Risk perception of HcWs related to the COVID-19 pandemic.
The study included 135 children with a mean age of 12.36 ± 3.29 years, and 50.4% were female. The children's mean SCARED subscale scores were as follows: panic/somatic: 7.23 ± 5.71; general anxiety: 6.89 ± 4.25; separation anxiety: 6.88 ± 3.94. The correlation between the SCARED subscale scores, and age of the children, and their parents’ Covid-19 Expopsure and Risk Perception Scale and STAI-S scores are shown in Table 2 . STAI-S scores, Covid-19 Exposure and Risk Perception Scale scores (higher scores mean lower risk perception), the SCARED somatic/panic subscale scores, the SCARED generalized anxiety subscale scores, and the SCARED separation anxiety scores were significantly higher in the HcWs (and their children) that had direct contact with Covid-19 patients than that did not (Table 3 ).
Table 2.
The relationship between the level of anxiety in HcWs’ and their children.
| Age of Children | Covid-19 Risk Perception | STAI-S Score | |
|---|---|---|---|
| SCARED somatic/panic | r = –0.083, P = 0.345 |
r = –0.157, P = 0.070 |
r = 0.190, P = 0.028 |
| SCARED general anxiety |
r = 0.178, P = 0.040 |
r = –0.126, P = 0.149 |
r = 0.145, P = 0.093 |
| SCARED separation anxiety |
r = –0.490, P ˂ 0.001 |
r = –0.134, P = 0.124 |
r = 0.134, P = 0.122 |
Pearson's correlation analysis: bold text indicates statistically significant differences.
Table 3.
The anxiety scores of HcWs and their children according to HcW direct contact with COVID-19 patients.
| Direct contact with Covid-19 direct patients | No direct contact with Covid-19 direct patients | Statistical analysis | |
|---|---|---|---|
| STAI-S | 50.10 ± 10.34 | 45.82 ± 11.68 | t = 2.354, P = 0.020 |
| Covid-19 Exposure and Risk Perception | 13.19 ± 4 .24 | 14.94 ± 5.12 | t = –2.262, P = 0.025 |
| SCARED somatic/panic | 7.96 ± 5.86 | 5.85 ± 5.20 | t = 2.073, P = 0.040 |
| SCARED generalized anxiety | 7.42 ± 4 .39 | 5.91 ± 3.84 | t = 1.980, P = 0.050 |
| SCARED separation anxiety | 7.37 ± 4.05 | 5.95 ± 3.59 | t = 2.084, P = 0.040 |
Student's t-test: bold text indicates statistically significant differences.
To evaluate the variables that might have affected the STAI-S score and Covid-19 Exposure and Risk Perception Scale score, HcW gender, monthly income, direct contact with COVID-19 patients, and the presence of mental illness were examined via multiple linear regression analysis. Gender, direct contact with COVID-19 patients, and the presence of mental illness were observed to be predictors of the Covid-19 Exposure and Risk Perception Scale score (Table 4 ). In addition, direct contact with COVID-19 patients and the presence of mental illness were predictors of the STAI-S score (Table 5 ).
Table 4.
Predictors of the Covid-19 Exposure and Risk Perception scorea.
| Non-standardized coefficients | Standardized coefficients | P | t | ||
|---|---|---|---|---|---|
| Beta | Standard error | Beta | |||
| (Constant) | 9.567 | 2.648 | 0.000 | 3.613 | |
| Gender | 3.994 | 1.246 | 0.249 | 0.002 | 3.205 |
| Monthly income | 0.031 | 0.062 | 0.039 | 0.616 | 0.502 |
| Direct contact with Covid-19 patients | 1.725 | 0.736 | 0.179 | 0.021 | 2.342 |
| Presence of mental illness | 1.499 | 0.569 | 0.204 | 0.009 | 2.636 |
| R = 0.389 | R2 = 0.151 | F = 6.544 | P ˂ 0.001 | ||
Multiple linear regression: bold text indicates statistically significant differences.
Covid-19 risk perception scale; higher scores mean lower risk perception.
Table 5.
Predictors of the STAI-S score.
| Non-standardized coefficients | Standardized coefficients | P | t | ||
|---|---|---|---|---|---|
| Beta | Standard error | Beta | |||
| (Constant) | 28.087 | 6.191 | 0.000 | 4.537 | |
| Gender | 4.297 | 2.835 | 0.119 | 0.132 | 1.516 |
| Monthly income | -0.053 | 0.150 | -0.028 | 0.725 | -0.353 |
| Direct contact with Covid-19 patients | 4.570 | 1.779 | 0.199 | 0.011 | 2.569 |
| Presence of mental illness | 4.360 | 1.371 | 0.250 | 0.002 | 3.180 |
| R = 0.346 | R2 = 0.120 | F = 5.027 | P = 0.001 | ||
Multiple linear regression: bold text indicates statistically significant differences.
4. Discussion
The present study's data were collected between April 2020 and June 2020, during the first few months of the COVID-19 pandenic in Turkey. The main findings of this study are: 1. 76.4% of HcWs scored above the STAI-S clinical cut-off of score of 40; 2. female gender, the presence of mental illness, and direct contact with COVID-19 patients predicted the perception of a high risk of COVID-19; 3. direct contact with COVID-19 patients and the presence of mental illness predicted the HcW level of anxiety; 4. the SCARED somatic/panic subscale score in the children of HcWs was associated with their parents’ level of anxiety (While the symptoms of separation anxiety are in the foreground as the age decreases in children, the prevalence of common anxiety symptoms increases as the age increases in children.); 5. Children of the HcWs that had direct contact with Covid-19 patients had higher levels of anxiety than the children of the HcWs that did not.
The present findings emphasize the augmented psychiatric symptoms, which are frequently mentioned after the COVID-19 pandemic, both in HcWs and their children, and dual relations between COVID-19 related concerns of HcWs and their children's anxiety. Moreover, the HcWs in the present study had high levels of anxiety, as reported earlier (Davico et al. 2021; Muller et al. 2020). Furthermore, the present findings show that direct contact with COVID-19 patients and the presence of mental illness strongly predicted the COVID-19 risk perceptions and the level of anxiety in the HcWs. The onset of the COVID-19 pandemic was a period when uncertainty about the process was felt clearly. During this period when most of society was protected from infection by quarantine, the inadequacy of protective equipment and the fact that a vaccine against the infection had not yet been developed, the workload of HcWs increased to a much greater degree than for other professions. Death of colleagues from COVID-19, increased work load, the risk of contracting the disease, and the possibility of transmitting COVID-19 infection to their families might have been causes for the increase in the level of anxiety among HcWs (Hacimusalar et al. 2020). Furthermore, with the unpredictable outbreak of the pandemic, the inadequacy of social support in basic areas, such as childcare for HcWs, came to the fore. The sustainability of the healthcare system depends entirely on the ability to protect the health of HcWs; yet, recent findings related to psychological distress among HcWs indicate that the healthcare system is currently unable to effectively do so.
Both the risk perception and level of anxiety were higher in the female HcWs than in the male HcWs. Similarly, a study from China reported that female HcWs were significantly more worried about being infected with COVID-19 and infecting their families than male HcWs (Dai et al. 2020). As females worldwide are the primary caregivers responsible for childcare, their concern that their children might be infected with COVID-19 may be greater than that of males.
The factors affecting the level of anxiety in the children of HcWs was also examined in the present study. To the best of our knowledge the literature includes only a few studies on the mental health of HcWs’ children with during the COVID-19 pandemic. The worldview of children, including depictions of anxiety, is shaped by their primary caregiver (Hoagwood 2005). This was shown in a study conducted in Spain that observed that psychological changes in children were closely related to the level of parental exposure to the COVID-19 pandemic (Romero et al. 2020). A recent study reported that there is a relationship between the burden of illness and mental health of parents as well as children's perception of stress (Russell et al. 2020). A large-scale population-based study noted that female HcWs employed in COVID-19 wards had higher levels of stress than HcWs not in direct contact with COVID-19 patients and non-HcWs (Davico et al. 2021). That study also observed that COVID-19-related symptoms of trauma, such as avoidance, intrusion, and hyperarousal, in HcWs and their children are correlated (Chen et al. 2020; Davico et al. 2021). As reported by Davico et al. (2021), in the present study SCARED somatic/panic anxiety symptoms in the children of HcWs were related to the state anxiety of their parents, and the level of anxiety in the children of HcWs that had direct contact with COVID-19 patients was significantly higher than in the children of HcWs not in direct contact with COVID-19 patients. Children of HcWs might have been highly susceptible to stress and trauma during the COVID-19 pandemic because their parents had a high level of stress and they were acutely aware of the risks posed by COVID-19 (Skokauskas et al. 2022). In the light of these results, it is thought that the interventions for the psychological effects of the pandemic will have long-term intergenerational repercussions.
The present findings should be evaluated in consideration of the study's strengths and limitations. The study was performed at the start of the COVID-19 pandemic in Turkey before many of the confounding factors emerged and when the country was in full lockdown, which could be considered a limitation. A strength of the study is that both HcWs and their children were assessed; however, the assessments are limited due to the small number of participants and online data collection. The short-term psychological effects of COVID-19 on HcWs and their children should be reviewed once the long-term psychological consequences become apparent. Understanding the psychological symptoms of the children of HcWs during the COVID-19 pandemic will guide the development of interventions that aim to maintain psychological health.
Ethical approval
This study was conducted at the child and adolescent psychiatry outpatient clinic of the Marmara University School of Medicine in Istanbul, Turkey. The study protocol was approved by the Ethics Committee of Mus Alparslan University (19.08.2020-9176).
Author Statement
Leyla Ezgi Tugen contributed to the overall design, data collection, article selection, review and manuscript preparation. Muhsine Goksu contributed to data collection, statistical analysis and review. Ayşe Burcu Erdoğdu contributed to overall design, review and manuscript preparation. All other authors contributed to editing, and submission.
Uncited References
Spielberger, 1970, Cakmakcı, 2004, COVID-19 Normalleşme Süreci ve Alınacak Tedbirler [WWW Document] n.d., Davico et al., 2021b
Declaration of Competing Interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. No potential conflict of interest was reported by the authors.
References
- Birmaher B., Khetarpal S., Brent D., Cully M., Balach L., Kaufman J., Neer S.M.K. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Cakmakcı, F., 2004. Çocuklarda Anksiyete Bozukluklarını Tarama Ölçeği Geçerlik Ve Güvenirlik Çalışması [WWW Document]. Tıpta Uzmanlık tezi. URL https://tez.yok.gov.tr/UlusalTezMerkezi/
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J., Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Normalleşme Süreci ve Alınacak Tedbirler [WWW Document], n.d. URL https://shgm.saglik.gov.tr/TR,65901/covid-19-normallesme-sureci-ve-alinacak-tedbirler.html (accessed 5.5.23).
- Dai, Y., Hu, G., Xiong, H., Qiu, H., Yuan, X., 2020. Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. medRxiv 2020.03.03.20030874. https://doi.org/10.1101/2020.03.03.20030874
- Davico C., Ghiggia A., Marcotulli D., Ricci F., Amianto F., Vitiello B. Psychological Impact of the COVID-19 Pandemic on Adults and Their Children in Italy. Front Psychiatry. 2021;12:1–8. doi: 10.3389/fpsyt.2021.572997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ercan I., Hafizoglu S., Ozkaya G., Kirli S., Yalcintas E., Akkaya C. Examining Cut-Off Values For The State-Trait Anxiety Inventory. Revista Argentina De Clinica Psicologica. 2015;24:143–148. [Google Scholar]
- Hacimusalar Y., Kahve A.C., Yasar A.B., Aydin M.S. Anxiety and hopelessness levels in COVID-19 pandemic: A comparative study of healthcare professionals and other community sample in Turkey. J Psychiatr Res. 2020;129:181–188. doi: 10.1016/J.JPSYCHIRES.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoagwood K.E. Family-based services in children's mental health: a research review and synthesis. J Child Psychol Psychiatry. 2005;46:690–713. doi: 10.1111/J.1469-7610.2005.01451.X. [DOI] [PubMed] [Google Scholar]
- Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø., Stroobants S., Van de Velde S., Vist G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020;293 doi: 10.1016/J.PSYCHRES.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oner N., Le Compte A. Bogazici Universitesi Yayinlari; 1983. Durumluk Surekli Kaygi Envanteri El Kitabi [WWW Document]https://www.scirp.org/(S(i43dyn45teexjx455qlt3d2q))/reference/ReferencesPapers.aspx?ReferenceID=1959191 URL. [Google Scholar]
- Romero E., López-Romero L., Domínguez-álvarez B., Villar P., Gómez-Fraguela J.A. Testing the Effects of COVID-19 Confinement in Spanish Children: The Role of Parents’ Distress, Emotional Problems and Specific Parenting. Int J Environ Res Public Health. 2020;17:1–23. doi: 10.3390/IJERPH17196975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RTMH, 2023. COVID-19 Information Platform [WWW Document]. T.R. Ministry of Health COVID-19 Information Platform online website.
- RTMH, 2021. COVID-19 normalization process [WWW Document]. Official website of the Ministry of Health of Türkiye. URL (accessed 5.13.23).
- RTMH, 2019. COVID-19 [WWW Document]. Republic of Türkiye Ministry of Health online official site.
- Russell B.S., Hutchison M., Tambling R., Tomkunas A.J., Horton A.L. Initial Challenges of Caregiving During COVID-19: Caregiver Burden, Mental Health, and the Parent-Child Relationship. Child Psychiatry Hum Dev. 2020;51:671–682. doi: 10.1007/S10578-020-01037-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sant'Ana G., Imoto A.M., Amorim F.F., Taminato M., Peccin M.S., Santana L.A., Göttems L.B.D., Camargo E.B. Infection and death in healthcare workers due to COVID-19: a systematic review. ACTA Paulista de Enfermagem. 2020;33 doi: 10.37689/ACTA-APE/2020AO0107. [DOI] [Google Scholar]
- Skokauskas N., Leventhal B., Cardeli E.L., Belfer M., Kaasbøll J., Cohen J. Supporting children of healthcare workers during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. 2022;31:203–204. doi: 10.1007/S00787-020-01604-6/METRICS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger, C.D., 1970. STAI manual. Calf : Consulting Psychologist.
- Spielberger C.D., Gorsuch R.L., Lushene R., Vagg P.R., Jacobs G.A. Consulting Psychologists Press; Palo Alto: 1983. Manual for the State-Trait Anxiety Inventory. [WWW Document]https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/referencespapers.aspx?referenceid=1824137 URL. [Google Scholar]
- Vigneau F., Cormier S. The factor structure of the State-Trait Anxiety Inventory: an alternative view. J Pers Assess. 2008;90:280–285. doi: 10.1080/00223890701885027. [DOI] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA - Journal of the American Medical Association. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2021. The impact of COVID-19 on health and care workers: a closer look at deaths [WWW Document] URL (accessed 5.5.23. [Google Scholar]