Abstract
Background
Enhanced recovery programmes are associated with improved short-term outcomes following liver surgery. The impact of enhanced recovery programmes on medium- and long-term outcomes is incompletely understood. This study aimed to assess the impact of an enhanced recovery programme on long-term survival in patients undergoing surgery for colorectal liver metastases.
Methods
At a tertiary hepatobiliary centre, we analysed short-, medium- and long-term outcomes in consecutive patients undergoing liver resection for colorectal liver metastases. A five-year retrospective review was carried out comparing the enhanced recovery programme to standard care.
Results
A total of 172 patients were included in the analysis: 87 on standard care and 85 on an enhanced recovery programme. Open surgery was performed in 122 patients: 74 (85.1%) and 48 (56.5%) patients in the standard care and enhanced recovery programme, respectively (p < 0.001). There was a significant reduction in the median (IQR) length of hospital stay in the enhanced recovery programme compared with standard care (7 (5) days vs. 8 (3) days, p = 0.0009). There was no significant difference in survival between standard care and the Enhanced Recovery Programme at one (p = 0.818), three (p = 0.203), and five years (p = 0.247).
Conclusion
An enhanced recovery programme was associated with a reduced length of hospital stay. There was no effect on the one-, three- and five-year survival.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00423-023-02968-4.
Keywords: Enhanced recovery programme, ERP, Colorectal cancer
Introduction
Enhanced recovery programmes (ERP) have demonstrated improved patient outcomes and length of stay following surgery by optimising the perioperative period [1]. Successful experiences with ERPs were reported as early as 1999 with the benefit of early and safe discharge of patients following major abdominal aneurysm surgery [2], and their use has since expanded into other specialities such as colorectal surgery [3]. It is a key peri-operative care recommendation by the National Institute for Clinical Excellence (NICE) [4] and is now the gold standard in many surgical specialties [5–9]. Through its successes, ERP has paved the way for contemporary prehabilitation strategies [10]. The use of ERPs following liver surgery began in 2008 following successful trials that showed earlier oral intake, a better postoperative period and a reduction in hospital stay [11]. A recent systematic review of patient outcomes following major liver surgery with ERP showed hospital stay to be reduced by 5–7 days without compromising morbidity and mortality [12]. Further, a recent randomised clinical trial comparing the ERP to standard care in open liver resection surgery showed a reduction in the incidence of medical complications and an improvement in quality of life [13]. The positive short-term effects of ERP have also been supported by other studies suggesting that such programmes are safe, cost-effective and acceptable to patients [14]
To date, although there have been reports on the effect of ERP on long-term survival of patients having surgery for colorectal cancer, there have been no reports on the effect of ERP on long-term survival in liver resection solely for colorectal liver metastases. The aim of this study was to clarify whether the well-established benefits of ERP may translate to reduced time to chemotherapy or increased likelihood of completing chemotherapy, thereby offering an overall survival benefit.
Materials and methods
We evaluated retrospective data from a prospectively maintained database for patients who had undergone liver resection for colorectal liver metastasis (CRLM) between January 2011 and December 2016 at a regional hepatobiliary referral centre. Health Research Authority (HRA) guidelines on the use of NHS patient data for research purposes were adhered to [15]. All patients having liver resection for CRLM with curative intent were included regardless of the operative modality (laparoscopic or open). The ERP was introduced in January 2014 and patients were stratified into two groups based on time periods: Pre-ERP, hereafter referred to as control (CON) & ERP. We aimed to compare CON and ERP for an equivalent time period in years with a minimum 5-year follow-up. Patients were classified as ERP if they received at least 50% of the components in each of four domains (Appendix 1) of the ERP programme. CON patients received no components of ERP.
Data collection
The data collated included patient demographics, details of surgical and oncological treatments, histology of resection specimens, duration of hospital stay, 90-day readmission, details of complications, compliance with individual ERP components and post-treatment survival (one-year, three-year and five-year mortality). The information was gathered from electronic records, clinic letters and operative notes. A multidisciplinary team of doctors, nurses, anaesthetists and allied health professionals contemporaneously completed an ERP document (Appendix 1). This document was developed through prior consultation with the multidisciplinary team (MDT). The primary outcome measured was posttreatment survival. One-, three- and five-year survival was scrutinised to determine whether there was any effect of ERP during this period. The secondary outcomes included hospital length of stay, post-operative complications using the Clavien-Dindo (CD) classification and 90-day readmission rates. The data was then reviewed and validated by all the investigators before being subjected to statistical analysis.
Components of the ERP for liver surgery
ERP protocols involve a range of peri-operative strategies to promote recovery, facilitate safe and early discharge and improve patients’ overall peri-operative experience. All patients undergoing elective liver resection for CRLM were enrolled on to a standardised enhanced recovery programme from January 2014. The programme (Appendix 1) contained a series of strategies delivered by a specialist team as part of standard peri-operative care. The programme was assembled into four distinct but inter-related domains namely (i) Pre-operative Assessment & Information (ii) Day of Surgery Interventions (iii) Anaesthesia Protocols (iv) Post-operative Assessment, Information & Interventions. Each domain contained several components focussed on a particular aspect of patient optimisation, best clinical practice, and holistic patient care.
Statistical analysis
Normality of data were assessed using Shapiro–Wilk tests. Univariate analyses (Mann–Whitney-U and chi2 tests) were used to detect significant differences in patient demographics and clinical case-mix between the CON and ERP cohorts (Table 1). Furthermore, patient demographics and clinical case mix features were analysed for significant associations with the one-, three- and five-year survival cohorts (Table 3). To achieve the primary aim of the study, survival analysis was applied to calculate one-, three- and five-year survival (postliver resection CON vs. ERP cohorts). Kaplan Meier survival curves were plotted and analysed using the log-rank test to determine significant differences in survival. All statistical analysis was performed using STATA statistical package version 15 (Stata Corp LLC4905 Lakeway Drive, College Station, Texas 77845-4512, USA) and figures were constructed in GraphPad Prism v 9.4.1 (GraphPad Software, San Diego, CA, USA). Significance was defined as p < 0.05.
Table 1.
Patient demographics
| Characteristic | Total | CON | ERP | P-value |
|---|---|---|---|---|
| Patient factors | 172 | 87 | 85 | |
| Mean age (years) | 64.1 | 63.9 | 64.4 | 0.39 |
| SD | 10.1 | 9.4 | 10.8 | |
| Male sex | 125 (72.7%) | 66 (75.9%) | 59 (69.4%) | 0.34 |
| Mean BMI (kg/m2) | 27.4 | 27.9 | 26.9 | 0.10 |
| Risk stratification | ||||
| Mean Charlson Index | 8.4 | 8.3 | 8.4 | 0.58 |
| ASA I | 12 (7.0%) | 6 (6.9%) | 6 (7.1%) | 0.22 |
| ASA II | 94 (54.7%) | 53 (60.9%) | 41 (48.2%) | |
| ASA III | 66 (38.4%) | 28 (32.2%) | 38 (44.7%) | |
| Surgical & oncological factors | ||||
| Open surgery | 122 (70.9%) | 74 (85.1%) | 48 (56.5%) | < 0.001 |
| Mean number of metastases | 2.3 | 2.1 | 2.5 | 0.48 |
| Mean number of liver segments | 2.5 | 2.4 | 2.5 | 0.75 |
| Major resection | 94 (54.7%) | 46 (52.9%) | 48 (56.5%) | 0.64 |
| Neo-adjuvant chemotherapy | 89 (51.7%) | 44 50.6% | 45 (52.9%) | 0.76 |
SD, standard deviation; BMI, body mass index; ASA, American Society of Anaesthesiologist Classification; ICU, intensive care unit
Table 3.
Factors associated with overall survival in both CON & ERP groups
| Variables | 1-year survival | 3-year survival | 5-year survival |
|---|---|---|---|
| P-value | P-value | P-value | |
| Age (years) | 0.90 | 0.40 | 0.10 |
| Sex | 0.72 | 0.90 | 0.86 |
| BMI (kg/m2) | 0.60 | 0.41 | 0.88 |
| Charlson Index | 0.42 | 0.11 | 0.18 |
| Open surgery | 0.43 | 0.80 | 0.50 |
| Number of metastases | 0.12 | 0.26 | 0.47 |
| Number of segments | 0.02 | 0.10 | 0.79 |
| Neo-adjuvant chemotherapy | 0.19 | 0.33 | 0.17 |
| Length of stay (days) | 0.70 | 0.08 | 0.06 |
| Days in ICU | 0.23 | 0.74 | 0.92 |
| ASA | 0.82 | 0.47 | 0.47 |
Bold indicates p < 0.05
Anaesthesiologist Classification; ICU, intensive care unit, BMI, body mass index; ASA, American Association of Anaesthesiology
Results
A total of 172 patients were included in the analysis, 87 CON and 85 ERP (Table 1). Sufficient data could not be retrieved for 19 patients (21.8%) in the CON and 10 patients (11.7%) in the ERP group. The median follow-up time was 58 months. One hundred and twenty-two patients had open surgery: 74 and 48 patients in the CON and ERP groups, respectively. Fifty patients had laparoscopic surgery: 13 and 37 in the CON and ERP groups, respectively. There was no significant difference in survival between CON and ERP at one, three and five years (Table 3). Although the median survival was greater in the ERP group compared to the CON group at three years, this was not significant (p > 0.05, Fig. 1). Furthermore, there was no significant difference in survival at five years (Fig. 2). We further assessed the determinants of survival (Table 3). The main determinant of 1-year survival was number of resected segments. The number of segments being inversely proportional to survival within the first year post-operatively. This effect was not observed at three and five years.
Fig. 1.
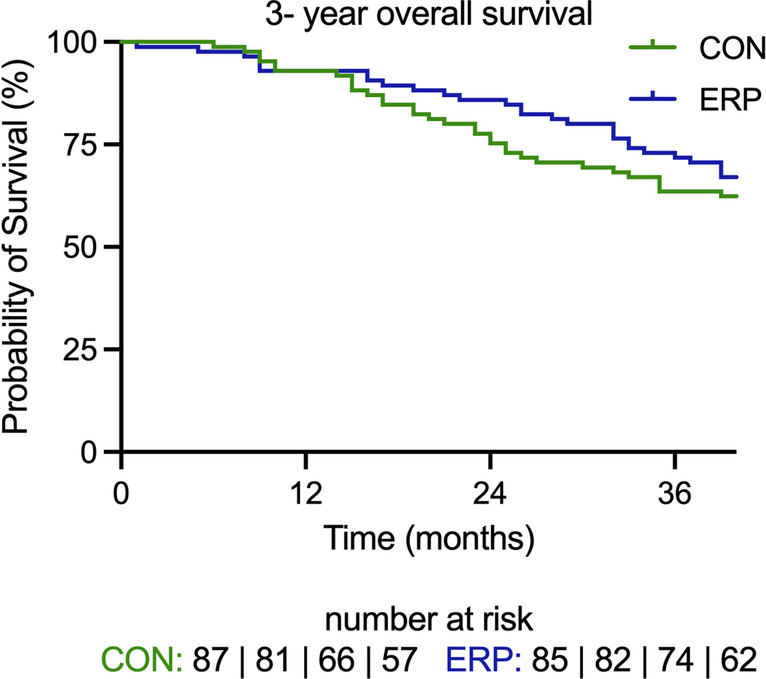
There was no effect of ERP on 3-year survival p = 0.203
Fig. 2.
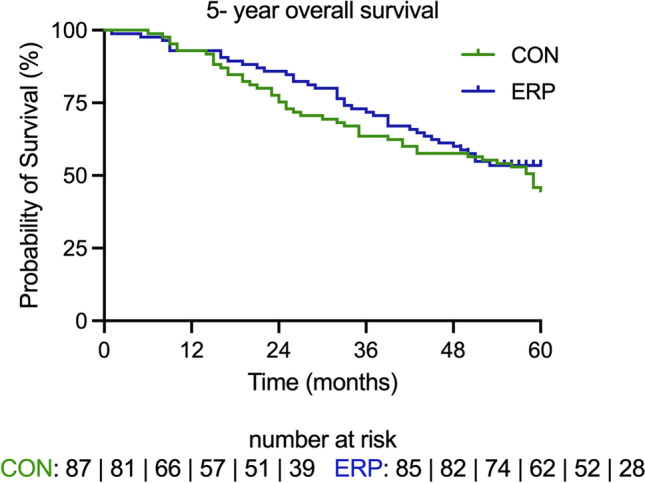
There was no effect of ERP on 5-year survival, p = 0.274
Over the five-year study period, the CON group had significantly more patients who underwent open surgery as compared to the ERP group; 74 (85.1%) vs. 48 (56.5%), p < 0.001. There was a significant reduction in the median (IQR) length of hospital stay in the ERP group as compared to the CON group (7 (5) vs. 8 (3) days, p = 0.0009). Open liver surgery was associated with a longer hospital stay compared with a laparoscopic approach (Table 2). Complications were grouped into minor (CD I-II) and major (CD III-IV). There was a statistical trend for differences in minor and major complications (data for CON vs. ERP, p = 0.088). However, re-admission rates between the groups were similar: CON 5 (0.05%) vs. ERP 9 (0.10%), p = 0.247 (Table 2). Interestingly, there were significantly more patients in the ERP group that experienced no complications; CON 33 (37.9%) vs. ERP 58 (68.2%), p < 0.001 (Table 3).
Table 2.
Secondary outcomes
| Length of hospital stay (days) | Total | CON | ERP | P-value |
|---|---|---|---|---|
| Median length of stay (IQR) | 8.0 (3) | 8.0 (3) | 7.0 (5) | 0.0009 |
| Median ICU stay (IQR) | 2.0 (2) | 2.0 (2) | 2.0 (2) | 0.76 |
| Complication rates | ||||
| No complications | 91 (52.9%) | 33 (37.9%) | 58 (68.2%) | 0.001 |
|
Clavien-Dindo I Clavien-Dindo II |
33 (19.2%) | 22 (25.3%) | 11 (12.9%) |
CD I-II vs. III-IV 0.08 |
| 34 (19.8%) | 26 (29.9%) | 8 (9.4%) | ||
|
Clavien-Dindo III Clavien-Dindo IV |
10 (5.8%) | 4 (4.6%) | 6 (7.1%) | |
| 2 (1.2%) | 1 (1.2%) | 1 (1.2%) | ||
| Readmission rates | 172 | 5 (0.05%) | 9 (0.10%) | 0.2471 |
ICU, intensive care unit
Discussion
Over the last decade, enhanced recovery programmes have become integrated as part of standard surgical perioperative practice [16]. Studies have cited a reduced length of hospital stay [17, 18], ICU stay [19], peri-operative complications [13] and improved patient experiences [20] as the main benefits of ERP. It is well estabished that the short-term benefits of improved functional recovery after major surgery translate into savings of bed-days and reduced cost to healthcare systems [21, 22]. Our study is consistent with the literature regarding length of hospital stay. This association was recently corroborated by Noba et al., in their meta-analysis of 3739 patients undergoing liver resections [23].
In elective cancer surgery, the effect of ERP on improving short- and medium-term outcomes such as functional recovery and hospital stay has been well established [16]. However, there is a paucity of literature on the effect of ERP on long-term outcomes such as survival. Curtis et al. assessed the effect of ERP on 5-year survival in a colorectal cancer cohort of 854 patients and demonstrated improved survival when combined with a laparoscopic approach [24]. To our knowledge, this is the first study that has attempted to assess the effect of ERP on medium and long-term survival in curative liver resection for CRLM. In our series, ERP was found to be associated with a significant reduction in the median length of hospital stay. This finding was consistent with other studies that have analysed ERP in the context of elective hepatopancreatobiliary [5, 25], colorectal [6, 26, 27], oesophagogastric [7, 28] urological [8, 29] and breast surgery [9]. Although length of stay may be influenced by other administrative and social factors outside of ERP [30], most investigators believe this observation to be weighted in favour of ERP.
We found no significant relationship between the ERP and survival at one, three, or five years. This was not an unexpected finding, considering that ERP interventions are more likely to influence homeostatic and physiological factors than the biology of the disease [31]. More importantly, within a cancer context, it may also be that ERP has limited influence on reducing time to adjuvant chemotherapy or chances of completion. In one colorectal cancer study, ERP was associated with ‘on time’ initiation of adjuvant chemotherapy; however, long-term survival was not studied [32]. We would expect that interventions that lead to quicker functional recovery may offer an increased opportunity for patients to shorten their time to commencing adjuvant therapy. Some studies have alluded to this effect and have shown improved survival as a function of a reduced time to completion of adjuvant chemo or radiotherapy [33, 34]. This effect was not investigated in our study and provides an avenue for further analysis.
We analysed several factors to determine those common to both groups that may have influenced survival. We found that independent of ERP, the number of resected segments had a significant association with survival at one year. A greater number of resected segments was associated with poorer survival at one year. This finding was not dissimilar to work done by Fromer et al. who demonstrated poorer survival with > 3 resected lesions [35]. Evidence has suggested that the number of metastases may be directly related to tumour burden. The number of metastases and their their anatomical distribution (uni/bi lobar) may serve as a marker for overall disease burden and may suggest more aggressive tumour biology, hence poorer survival [36].
Concerning length of stay, the ERP group showed a statistically significant reduction when compared to the CON group. The clinical importance of a reduction in LoS by a day must be viewed within the wider context of patient satisfaction and the cost reduction in total number of bed days. This was beyond the scope of this study. It is possible that this observation could be related to smaller numbers of patients in the CON group (13 patients) who also had laparoscopic surgery. Reduced length of stay in ERP has been extensively investigated by several authors. While authors suggest that hospital stay may be influenced by other factors such as social care provision, administrative protocols and patient-related factors [30], there appears to be a genuine effect of accelerated hospital recovery with ERP that seems to be consistent with a wide range of ERP protocols [16].
In our series, there was no difference in the incidence of major complications (CD III-IV) between the groups. However, significantly more patients in the ERP group had no complications when compared with the CON group. While this could be a genuine effect, it is also plausible that this observation could be explained by the higher proportion of patients having open surgery in the CON group and having complications related to this. Contrary to this assumption, a study by Jones et al. found ERP to be associated with reduced complication rates when investigating a cohort of patients undergoing open liver resections [13]. Another series of primary liver resections found reduced complication rates with ERP; however, this was confined to patients with the highest compliance [37]. Additionally, a recent meta-analysis of 27 comparative liver resection studies showed a significant reduction in both length of stay and complication rates [23]. It is our opinion that while ERP may have no influence on surgical factors (such as technical failures) that may lead to complications; peri-operative optimisation with better glycaemic control and anaemia correction and maintaining intra-operative haemostasis along with postoperative strategies may reduce the risk of complications.
ERPs have evolved in step with other improvements in perioperative care such as multi-modal analgesia, patient-tailored anaesthesia and more widespread use of objective operative risk stratification tools such as cardiopulmonary exercise testing (CPET) [38]. In light of these improvements over the last decade and the multi-modal nature of ERP, delineating what may be the most important components of these pathways can be challenging due to wide variations in adherence rates and number ERP components [39]. It is widely accepted that observed improvements may be due to the collective implementation of several components and that the effectiveness of ERPs are enshrined in the multimodal nature of their delivery [31].
Strengths and limitations
This study is the first of its kind to address the impact of ERP on medium and long-term survival for the curative resection of CRLM. Due to the wide variability in content and implementation of ERPs, coupled with demographic differences and care pathways across NHS Trusts, we concluded that a single site observational study was most appropriate in addressing this issue. Data was collected using robust reporting and recording systems and was verified for accuracy by all authors. Our findings supplement the existing literature on ERP and provides evidential basis for further larger controlled studies powered to detect improvements in long-term survival. We believe this to be a pertinent area for further investigation due to the evolving nature of ERP and the more widespread uptake of minimally invasive stragegies such as laparoscopic and robotic surgery [40].
Inherent biases within our study design meant that findings should be interpreted within the limitations of a retrospective study. The nature of ERP and the advent of its implementation at our institution may have been associated with recall and reporting biases that may have over-estimated the beneficial effects of ERP. We concede that within the period that ERP commenced, data may have been more fastidiously recorded and reported especially within the context of being a nationally recognised quality indicator of peri-operative patient care. Additionally, the ERP programme coincided with an increased uptake of laparoscopic liver resection. We are aware that minimally invasive techniques are associated with reduced complication rates and length of hospital stay in some series [41]. We recognise that inadequate numbers of study patients are likely to preclude revealing significant differences in low incidence secondary outcomes. In most surgical units within the National Health Service, ERP is now standard practice[42]. Further studies within this field may provide more clarity on medium and long-term survival by probing larger databases. As the components within ERP are improved and evolve further, so too will oncological and surgical techniques. Improving survival in patients with CRLM may depend on a range of strategies deployed via a multimodal, multidisciplinary platform.
Conclusion
An enhanced recovery programme accelerates recovery and reduces hospital stay in patients undergoing curative resection for CRLM. We found ERP to have no effect on long-term survival .
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank the ERP and Hepatopancreatobiliary Teams at East Lancashire Hospitals NHS Trust for providing detailed protocols, electronic and physical data in the production of this manuscript.
Authors’ contributions
J.L. and D.S. conceived the study. J.L., T.M., K.A., A.S., H.U., A.L., R.A., and G.S. collected data. All authors were involved in data analysis or interpretation. J.L, C.G. and D.S. drafted the manuscript. Critical revisions involved all authors and the final manuscript was approved by all authors.
Data availability
The data are available from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wilmore DW. Recent advances: management of patients in fast track surgery. BMJ. 2001;322:473–476. doi: 10.1136/bmj.322.7284.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Podore PC, Throop EB. Infrarenal aortic surgery with a 3-day hospital stay: a report on success with a clinical pathway. J Vasc Surg. 1999;29:787–792. doi: 10.1016/S0741-5214(99)70204-1. [DOI] [PubMed] [Google Scholar]
- 3.Scharfenberg M, Raue W, Junghans T, Schwenk W. “Fast-track” rehabilitation after colonic surgery in elderly patients—is it feasible? Int J Colorectal Dis. 2007;22:1469–1474. doi: 10.1007/s00384-007-0317-8. [DOI] [PubMed] [Google Scholar]
- 4.National Institute of Clinical Excellence https://www.nice.org.uk/guidance/ng180/evidence/b-enhanced-recovery-programmes-pdf-8833151055. https://www.nice.org.uk/guidance/ng180/evidence/b-enhanced-recovery-programmes-pdf-8833151055. Accessed 3 Jul 2022
- 5.Coolsen MME, van Dam RM, van der Wilt AA, et al. Systematic review and meta-analysis of enhanced recovery after pancreatic surgery with particular emphasis on pancreaticoduodenectomies. World J Surg. 2013;37:1909–1918. doi: 10.1007/s00268-013-2044-3. [DOI] [PubMed] [Google Scholar]
- 6.Greco M, Capretti G, Beretta L, et al. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38:1531–1541. doi: 10.1007/s00268-013-2416-8. [DOI] [PubMed] [Google Scholar]
- 7.Underwood TJ, Noble F, Madhusudan N, et al. The development, application and analysis of an enhanced recovery programme for major oesophagogastric resection. J Gastrointest Surg. 2017;21:614–621. doi: 10.1007/s11605-017-3363-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arumainayagam N, McGrath J, Jefferson KP, Gillatt DA. Introduction of an enhanced recovery protocol for radical cystectomy. BJU Int. 2008;101:698–701. doi: 10.1111/j.1464-410X.2007.07319.x. [DOI] [PubMed] [Google Scholar]
- 9.Dumestre DO, Webb CE, Temple-Oberle C. Improved recovery experience achieved for women undergoing implant-based breast reconstruction using an enhanced recovery after surgery model. Plast Reconstr Surg. 2017;139:550–559. doi: 10.1097/PRS.0000000000003056. [DOI] [PubMed] [Google Scholar]
- 10.Lambert JE, Hayes LD, Keegan TJ et al (2021) The impact of prehabilitation on patient outcomes in hepatobiliary, colorectal, and upper gastrointestinal cancer surgery. Ann Surg 274:70–77. 10.1097/SLA.0000000000004527 [DOI] [PubMed]
- 11.van Dam RM, Hendry PO, Coolsen MME, et al. Initial experience with a multimodal enhanced recovery programme in patients undergoing liver resection. Br J Surg. 2008;95:969–975. doi: 10.1002/bjs.6227. [DOI] [PubMed] [Google Scholar]
- 12.Coolsen MME, Wong-Lun-Hing EM, van Dam RM, et al. A systematic review of outcomes in patients undergoing liver surgery in an enhanced recovery after surgery pathways. HPB. 2013;15:245–251. doi: 10.1111/j.1477-2574.2012.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones C, Kelliher L, Dickinson M, et al. Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg. 2013;100:1015–1024. doi: 10.1002/bjs.9165. [DOI] [PubMed] [Google Scholar]
- 14.Schultz NA, Larsen PN, Klarskov B, et al. Evaluation of a fast-track programme for patients undergoing liver resection. Br J Surg. 2012;100:138–143. doi: 10.1002/bjs.8996. [DOI] [PubMed] [Google Scholar]
- 15.Health Research Authority (2022) Guidance for using patient data. https://www.hra.nhs.uk/covid-19-research/guidance-using-patient-data/. Accessed 30 Aug 2022
- 16.Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery. JAMA Surg. 2017;152:292. doi: 10.1001/jamasurg.2016.4952. [DOI] [PubMed] [Google Scholar]
- 17.Wahl TS, Goss LE, Morris MS, et al. Enhanced recovery after surgery (ERAS) eliminates racial disparities in postoperative length of stay after colorectal surgery. Ann Surg. 2018;268:1026–1035. doi: 10.1097/SLA.0000000000002307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balvardi S, Pecorelli N, Castelino T, et al. Measuring in-hospital recovery after colorectal surgery within a well-established enhanced recovery pathway: a comparison between hospital length of stay and time to readiness for discharge. Dis Colon Rectum. 2018;61:854–860. doi: 10.1097/DCR.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 19.Giacopuzzi S, Weindelmayer J, Treppiedi E, et al. Enhanced recovery after surgery protocol in patients undergoing esophagectomy for cancer: a single center experience. Dis Esophagus. 2017;30:1–6. doi: 10.1093/dote/dow024. [DOI] [PubMed] [Google Scholar]
- 20.Bernard H, Foss M. Patient experiences of enhanced recovery after surgery (ERAS) Br J Nurs. 2014;23:100–106. doi: 10.12968/bjon.2014.23.2.100. [DOI] [PubMed] [Google Scholar]
- 21.Adamina M, Kehlet H, Tomlinson GA, et al. Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery. 2011;149:830–840. doi: 10.1016/j.surg.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Luzuy-Guarnero V, Gronnier C, Figuereido S, et al. Cost-benefit analysis of an enhanced recovery program for gastrectomy a retrospective controlled analysis. World J Surg. 2021;45:3249–3257. doi: 10.1007/s00268-021-06220-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noba L, Rodgers S, Chandler C, et al. Enhanced recovery after surgery (ERAS) reduces hospital costs and improve clinical outcomes in liver surgery: a systematic review and meta-analysis. J Gastrointest Surg. 2020;24:918–932. doi: 10.1007/s11605-019-04499-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Curtis NJ, Taylor M, Fraser L, et al. Can the combination of laparoscopy and enhanced recovery improve long-term survival after elective colorectal cancer surgery? Int J Colorectal Dis. 2018;33:231–234. doi: 10.1007/s00384-017-2935-0. [DOI] [PubMed] [Google Scholar]
- 25.Hughes MJ, McNally S, Wigmore SJ. Enhanced recovery following liver surgery: a systematic review and meta-analysis. HPB. 2014;16:699–706. doi: 10.1111/hpb.12245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramírez JM, Blasco JA, Roig JV, et al. Enhanced recovery in colorectal surgery: a multicentre study. BMC Surg. 2011;11:9. doi: 10.1186/1471-2482-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller TE, Thacker JK, White WD, et al. Reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesth Analg. 2014;118:1052–1061. doi: 10.1213/ANE.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 28.Tang J, Humes D, Gemmil E, et al. Reduction in length of stay for patients undergoing oesophageal and gastric resections with implementation of enhanced recovery packages. Annal Royal Coll Surg Engl. 2013;95:323–328. doi: 10.1308/003588413X13629960046039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin C, Wan F, Lu Y, et al. Enhanced recovery after surgery protocol for prostate cancer patients undergoing laparoscopic radical prostatectomy. J Int Med Res. 2019;47:114–121. doi: 10.1177/0300060518796758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiao J, Douglas D, Lee AH, Vemuri SR. A Delphi evaluation of the factors influencing length of stay in Australian hospitals. Int J Health Plann Manage. 1997;12:207–218. doi: 10.1002/(SICI)1099-1751(199707/09)12:3<207::AID-HPM480>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 31.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–641. doi: 10.1016/S0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 32.Hassinger TE, Mehaffey JH, Martin AN, et al. Implementation of an enhanced recovery protocol is associated with on-time initiation of adjuvant chemotherapy in colorectal cancer. Dis Colon Rectum. 2019;62:1305–1315. doi: 10.1097/DCR.0000000000001486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nelson DB, Mehran RJ, Mitchell KG, et al. Enhanced recovery after thoracic surgery is associated with improved adjuvant chemotherapy completion for non–small cell lung cancer. J Thorac Cardiovasc Surg. 2019;158:279–286.e1. doi: 10.1016/j.jtcvs.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Pang Q, Duan L, Jiang Y, Liu H. Oncologic and long-term outcomes of enhanced recovery after surgery in cancer surgeries — a systematic review. World J Surg Oncol. 2021;19:191. doi: 10.1186/s12957-021-02306-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fromer MW, Scoggins CR, Egger ME, et al. Preventing futile liver resection: a risk-based approach to surgical selection in major hepatectomy for colorectal cancer. Ann Surg Oncol. 2022;29:905–912. doi: 10.1245/s10434-021-10761-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sasaki K, Morioka D, Conci S, et al. The tumor burden score. Ann Surg. 2018;267:132–141. doi: 10.1097/SLA.0000000000002064. [DOI] [PubMed] [Google Scholar]
- 37.Feng J, Li K, Xu R, et al. Association between compliance with enhanced recovery after surgery (ERAS) protocols and postoperative outcome in patients with primary liver cancer undergoing hepatic resection. J Cancer Res Clin Oncol. 2022 doi: 10.1007/s00432-021-03891-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parasuraman S, Schwarz K, Gollop ND et al (2015) Healthcare professional’s guide to cardiopulmonary exercise testing. Br J Cardiol 22:156. 10.5837/bjc.2015.042
- 39.Fagard K, Wolthuis A, D’Hoore A, et al. A systematic review of the intervention components, adherence and outcomes of enhanced recovery programmes in older patients undergoing elective colorectal surgery. BMC Geriatr. 2019;19:157. doi: 10.1186/s12877-019-1158-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shugaba A, Lambert JE, Bampouras TM et al (2022) Should all minimal access surgery be robot-assisted? A systematic review into the musculoskeletal and cognitive demands of laparoscopic and robot-assisted laparoscopic surgery. J Gastrointest Surg 26:1520–1530. 10.1007/s11605-022-05319-8 [DOI] [PMC free article] [PubMed]
- 41.Nigri GR, Rosman AS, Petrucciani N, et al. Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc. 2011;25:1642–1651. doi: 10.1007/s00464-010-1456-5. [DOI] [PubMed] [Google Scholar]
- 42.NHS England https://www.nhs.uk/conditions/enhanced-recovery/. https://www.nhs.uk/conditions/enhanced-recovery/. Accessed 3 Jul 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are available from the corresponding author upon reasonable request.


