Abstract
Background:
Exercise is an effective nonpharmaceutical therapy for knee osteoarthritis (KOA).
Purpose:
To identify the most effective type of exercise therapy for KOA with regard to pain, stiffness, joint function, and quality of life.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
The PubMed, Web of Science, Embase, and Cochrane Library databases were searched, from inception to April 4, 2022. Included were randomized controlled trials that assessed the efficacy on KOA among 5 different exercise therapy groups (aquatic exercise [AE], stationary cycling [CY], resistance training [RT], traditional exercise [TC], and yoga [YG]) and compared with the control group. Outcomes among the groups were assessed with the Western Ontario and McMaster University Osteoarthritis Index (WOMAC), 6-minute walk test (6-MWT), visual analog scale (VAS) for pain, and Knee injury and Osteoarthritis Outcome Score (KOOS); weighted mean differences (WMDs) and 95% confidence intervals were calculated. Network meta-analyses comparing outcomes between all groups and with controls were performed, and group rankings were calculated using the surface under the cumulative ranking curve (SUCRA).
Results:
A total of 39 studies (N = 2646 participants) were included. Most of the studies failed to blind participants and researchers, resulting in a high risk of performance bias. Significantly worse WOMAC-Pain scores were seen in controls compared with all exercise interventions except AE (WMD [95% CI]: CY, –4.45 [–5.69 to –3.20]; RT, –4.28 [–5.48 to –3.07]; TC, –4.20 [–5.37 to –3.04]; and YG, –0.57 [–1.04 to –1.04]), and worse scores were seen in controls compared with YG regarding WOMAC-Stiffness (WMD, –1.40 [95% CI, –2.45 to –0.34]) and WOMAC-Function (WMD, –0.49 [95% CI, –0.95 to –0.02]). According to the SUCRA, CY was the most effective for improving WOMAC-Pain (80.8%) and 6-MWT (76.1%); YG was most effective for improving WOMAC-Stiffness (90.6%), WOMAC-Function (77.4%), KOOS–Activities of Daily Living (72.0%), and KOOS–Quality of Life (79.1%); AE was the most effective regarding VAS pain (77.2%) and KOOS-Pain (64.0%); and RT was the most effective regarding KOOS-Symptoms (84.5%).
Conclusion:
All 5 types of exercise were able to ameliorate KOA. AE (for pain relief) and YG (for joint stiffness, limited knee function, and quality of life) were the most effective approaches, followed by RT, CY, and TC.
Keywords: knee osteoarthritis, exercise therapy, systematic review, network meta-analysis
Knee osteoarthritis (KOA) is a chronic degenerative disease that most frequently affects middle-aged and elderly people. It is mainly characterized by articular cartilage degeneration and bone hyperplasia. The common clinical manifestations include knee swelling and pain with motion restrictions, and even joint deformity in severe cases. Relevant studies have indicated that the prevalence of KOA reached 23% in people older than 60 years of age.15,49 Some studies have reported that the proportion of middle-aged and elderly population will more than double by 2050, and the number of patients with KOA is likely to soar accordingly. 10 KOA causes adverse impacts on the work and life of the elderly population, increases medical costs, and places a heavy burden on society. Therefore, it is of great significance to explore effective treatment for KOA.
There are many options for the treatment of KOA, including pharmacotherapy, physical therapy, surgery, and rehabilitation therapy. 33 However, pharmacotherapy is correlated with multiple adverse effects such as congestive heart failure, hypertension, and renal toxicity. 22 Physical therapy has some limitations as well, such as being inappropriate for terminal patients. Terminal patients are those who need surgery and physical therapy is not appropriate for them. Patients with early KOA do not need surgery and can be treated nonoperatively. 16 It is necessary to find an effective nonsurgical approach to alleviate the symptoms in patients with KOA in that surgery is not indicated for patients at the early stage. A systematic review regarding therapeutic exercise for KOA has revealed that exercise could significantly alleviate joint pain and improve patients’ bodily function and quality of life. 12 Exercise therapy aims to achieve functional improvements in any part of the human body by virtue of the patient’s own strength, therapist assistance, or rehabilitation equipment. 44 Additionally, exercise could improve cardiac and pneumonic functions, enhance muscular strength, increase body stability, and promote psychological well-being. 14 Therefore, exercise is an effective complementary therapy and plays a critical role in KOA treatment.
Studies have demonstrated that traditional exercise (TC) therapies (tai chi, qi gong, ba duan jin, yi jin jing), yoga (YG), Pilates, aquatic exercise (AE) and muscle strengthening were found to be significantly effective in alleviating KOA-related symptoms, 62 while there is evidence showing that the therapeutic effect of exercise varies by type of exercise (such as resistance training [RT] and aerobics). 21 However, the relative effects of different exercises on different outcomes remain elusive.
Most randomized controlled trials (RCTs) on exercise therapy for KOA have focused on comparing exercise interventions with nonexercise interventions rather than a direct comparison of different exercise types. Given this situation, a network meta-analysis (NMA) could be performed to compare different types of exercise indirectly. 9 It could make full use of all available evidence, either direct or indirect, to enhance the assessment performance. 7 The aim of the current study was to use NMA to assess RCTs so as to identify the most effective exercise therapy for KOA.
Methods
Literature Search
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews incorporating Network Meta-Analyses (PRISMA-NMA) guidelines and was registered on PROSPERO (CRD42022335738). The Web of Science, PubMed, Embase, and Cochrane Central Register of Controlled Trials databases were searched from inception to April 2022. The International Clinical Trials Registry Platform of the World Health Organization (ClinicalTrials.gov) was also searched for eligible studies. Finally, the reference lists of systematic reviews published in the past 3 years were screened and searched for potential eligible studies. The search strategy was reviewed by experts in exercise and health to ensure its comprehensiveness and accuracy. Details of the search strategies for each database are presented in Supplemental Table S1.
Study Selection
The titles and abstracts of the retrieved articles were screened by 2 reviewers (L.M. and B.J.) independently to identify relevant studies. Studies meeting the inclusion criteria were confirmed and evaluated by the same 2 reviewers. Disagreements were settled via discussion or, if necessary, consultation with a third reviewer (T.M.).
The inclusion criteria were as follows:
RCTs;
Participants older than 50 years who were diagnosed with KOA; diagnosis could be based on the American Rheumatism Association criteria for osteoarthritis classification, 2 imaging, or laboratory indicators;
Exercise-based interventions, such as AE, YG, RT, tai-chi, or stationary cycling (CY);
Control group in which patients received either no intervention, routine care, health education, or sham exercise;
Outcome measures including the Western Ontario and McMaster University Osteoarthritis Index (WOMAC), 6-minute walk test (6-MWT), visual analog scale (VAS) for pain, or Knee injury and Osteoarthritis Outcome Score (KOOS);
Reported and published in the English language.
The exclusion criteria were as follows:
Animal studies;
Data unavailable;
Full text unavailable;
Meta-analyses, review articles, conference summaries, case reports, or abstracts.
Duplicate studies were removed. If >1 article reported the same study and the same results, the article with the latest published results was included.
Data Extraction
Data extraction was conducted by 2 reviewers (L.M. and B.J.) independently and included study characteristics (first author, country, publication information), participant characteristics (sample size, mean age, sex distribution), interventions (type, frequency, intensity, time of each regimen, duration, comparisons), control group characteristics, and outcomes. We divided exercise interventions into the following 5 categories: AE (all types of AE), RT (exercises aiming to enhance muscular strength), TC (exercises such as tai chi, qi gong, and ba duan jin), CY, and YG, and compared the effects of different types of exercise according to the Physical Activity Guidelines for Americans 38 and previous systematic reviews on exercise intervention classification.55,62
Outcome Measures
The primary outcome measure was the WOMAC (Pain, Stiffness, and Function subscales). Secondary outcomes included the 6-MWT, VAS pain, and KOOS (Pain, Symptoms, Activities of Daily Living [ADL], Sports, and Quality of Life [QoL] subscales). Outcomes were compared between the exercise interventions and with the control group.
Risk of Bias Assessment
Study quality was evaluated by 2 reviewers (B.J. and D.Z.) using the risk of bias assessment tool in the Cochrane Handbook. 17 Disagreements were settled by a third reviewer. Review Manager 5.4 was adopted for risk of bias assessment for studies. Seven domains of bias were assessed: randomization sequence generation (selection bias), allocation concealment (performance bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete data (withdrawal bias), selective reporting (reporting bias), and other sources of bias. Each domain was graded as high risk, low risk, or unclear risk. Studies with no direct evidence indicating selective bias or other sources of bias were graded as low risk or unclear risk.
Data Analysis
For interrater reliability of study selection and data extraction, we calculated the proportion of the consistent data extracted by the 2 reviewers to the total extracted data.
NMA was performed on the primary and secondary outcomes using the frequentist framework of Stata software (Version 15.0; Stata Corp), which assembled the results of every study. It combined direct evidence from the RCTs with head-to-head comparison and indirect evidence, allowing 2 intervention groups to be compared separately with a common control group. A network diagram for each outcome measure was generated in which each node represented a group (including the control group), and the line between every 2 nodes represented one or more RCTs in which the 2 groups were directly compared. The size of each node was weighted based on the number of participants in the group, and the thickness of the lines connecting the 2 nodes was weighted according to the number of studies that applied the connected interventions. Inconsistency within a network, which occurs when the direct and indirect evidence conflict, was tested for each outcome measure.
Random-effects models were applied to interpret the heterogeneity caused by clinical and other study factors, and 95% confidence intervals were provided for pooled point estimation. For each outcome measure, weighted mean differences (WMDs) and 95% confidence intervals between groups were calculated by subtracting the baseline data from endpoint data to estimate the effects of the outcomes, with a statistically significant difference indicated when the 95% confidence interval did not cross zero.
For each outcome measure, the intervention and control groups were ranked using the surface under the cumulative ranking curve (SUCRA). The SUCRA values ranged from 0% to 100%, with higher values indicating a more effective intervention. Finally, for outcome measures involved in ≥10 studies, a funnel plot analysis was performed to identify potential publication bias and small-sample effects.
Results
Included Studies
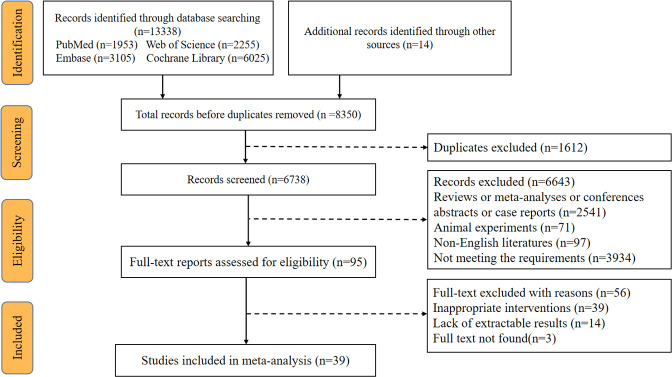
A total of 13,338 articles were initially identified, and 6738 remained after removal of duplicates. After applying inclusion and exclusion criteria, 39 RCTs § (2646 participants) on exercise therapy for KOA were included. A flow diagram of the study selection process is shown in Figure 1, and the characteristics of the included studies are presented in Supplemental Table S2.
Figure 1.
Flowchart of study selection.
All included articles were published between 2002 and 2022. Sample size in included studies ranged from 6 to 134. The proportion of female patients (82%) was higher than that of male patients (12%). For the intervention group, 13 studies ∥ applied AE, 14 studies ¶ applied RT, 17 studies # applied TC, 3 studies1,28,43 applied CY, and 3 studies8,23,37 applied YG. There were 11 studies ** that compared the effects of different exercise interventions. Control groups included attention control (n = 3), health education (n = 8), and no intervention (n = 28). Among the 39 studies, 11 were conducted in China, 10 in the United States, 3 in Australia, and 1 or 2 in South Korea, Iran, Canada, Greece, Malaysia, Finland, the Netherlands, Denmark, Brazil, and Thailand. The consistency rates of study selection and data extraction between the 2 reviewers were 83.7% and 80.8%, respectively.
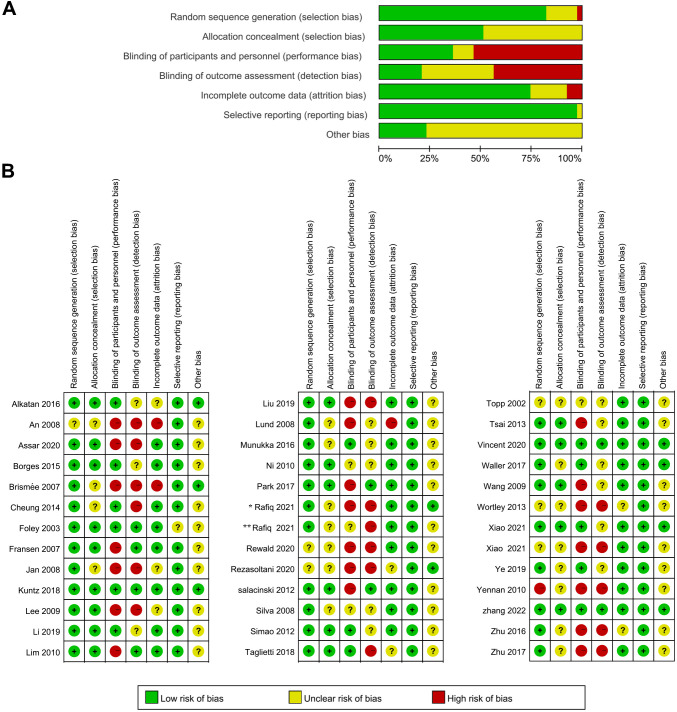
Results of Risk of Bias Assessment
Regarding the overall risk of bias assessment, the percentages of low, medium, and high risk of bias for each evaluated domain are shown in Figure 2A.
Figure 2.
(A) Overall risk of bias of the included studies. For each domain evaluated, the percentages of low, medium, and high risk of bias were as follows: randomization sequence generation (79%, 19%, and 2%), allocation concealment (52%, 48%, and 0%), blinding of participants and personnel (32%, 15%, and 53%), blinding of outcome assessment (24%, 33%, and 43%), incomplete outcome data (74%, 17%, and 9%), selective reporting (97%, 3%, and 0%), and other source of bias (24%, 6%, and 0%). (B) Risk of bias for each included study. *Reference 39. **Reference 40.
The results of the risk of bias assessment by study are shown in Figure 2B. All included studies used simple randomization; 32 studies described the process of randomization and the generation of randomization sequences (eg, computer numerical randomization or random number tables). Studies that included details of the randomization process were deemed to have a low risk of bias in allocation concealment. Most of the studies failed to blind participants and researchers because of the implementation of exercise intervention, resulting in a high risk of bias. There were 29 studies that provided information on patients who withdrew and the corresponding reasons.
Results of NMAs
Primary Outcome Measure: WOMAC Score
Forest plots, cumulative probability graphs, and network diagrams of the intervention and control group comparisons for the WOMAC are shown in Figure 3, and SUCRA rankings based on the cumulative probability diagrams are shown in Table 1. The network analysis–based inconsistency test showed no significant global inconsistencies for the WOMAC.
Figure 3.
Forest plots (left), cumulative probability graphs (middle), and network diagrams (right) for (A) WOMAC–Pain, (B) WOMAC-Stiffness, and (C) WOMAC-Function. On the forest plots, for treatment effect 1 vs 2, a negative WMD favors 1 and a positive WMD favors 2. On the network diagrams, the size of each node is weighted based on the number of participants receiving a certain intervention, and the thickness of the lines connecting 2 nodes is weighted according to the number of studies that applied the connected interventions. A and AE, aquatic exercise; B and CG, health education (control); C and CY, stationary cycling; D and RT, resistance training; E and TC, traditional exercise; F and YG, yoga; WMD, weighted mean difference; WOMAC, Western Ontario and McMaster University Osteoarthritis Index.
Table 1.
WOMAC Efficacy Ranking Table (Treatment-Relative Ranking) a
| Intervention | SUCRA, % | Probable Best b | Mean Rank c |
|---|---|---|---|
| WOMAC-Pain | |||
| AE | 67.9 | 9.5 | 2.6 |
| Control | 0.2 | 0.0 | 6.0 |
| CY | 80.8 | 50.2 | 2.0 |
| RT | 68.6 | 24.7 | 2.6 |
| TC | 62.7 | 15.6 | 2.9 |
| YG | 19.8 | 0.0 | 5.0 |
| WOMAC-Stiffness | |||
| AE | 63.6 | 5.2 | 2.8 |
| Control | 15.6 | 0.0 | 5.2 |
| CY | 64.3 | 18.5 | 2.8 |
| RT | 44.5 | 1.8 | 3.8 |
| TC | 21.4 | 2.1 | 4.9 |
| YG | 90.6 | 72.5 | 1.5 |
| WOMAC-Function | |||
| AE | 67.2 | 12.9 | 2.6 |
| Control | 18.0 | 0.0 | 5.1 |
| CY | 32.4 | 9.3 | 4.4 |
| RT | 48.3 | 7.5 | 3.6 |
| TC | 56.8 | 21.0 | 3.2 |
| YG | 77.4 | 49.2 | 2.1 |
a AE, aquatic exercise; CY, stationary cycling; RT, resistance training; SUCRA, surface under the cumulative ranking curve; TC, traditional exercise; WOMAC, Western Ontario and McMaster University Osteoarthritis Index; YG, yoga.
b The probability of that intervention being the most efficient treatment.
c The evaluation ranking of the intervention.
A total of 25 studies †† (1695 participants) reported WOMAC-Pain scores. Interventions included AE (n = 5), RT (n = 4), TC (n = 4), CY (n = 2), and YG (n = 2). Five studies1,11,13,57,61 performed direct comparisons for various exercise interventions via a 3-arm design. Significantly worse scores were seen in controls compared with all exercise interventions except AE (WMD [95% CI]: CY, –4.45 [–5.69 to –3.20]; RT, –4.28 [–5.48 to –3.07]; TC, –4.20 [–5.37 to –3.04]; YG, –0.57 [–1.04 to –1.04]). Significantly better WOMAC-Pain scores were seen with CY, RT, and TC compared with YG (WMD [95% CI]: CY, 3.88 [2.55 to 5.21]; RT, 3.71 [2.42 to 5.00]; TC, 3.64 [2.38 to 4.90]). Significantly worse WOMAC-Pain scores were seen with AE compared with controls (WMD, –4.28 [95% CI, –5.48 to –3.07]) and CY (WMD, –3.92 [95% CI, –5.10 to –2.74]), and significantly better scores were seen with AE versus RT (WMD, 4.28 [95% CI, 3.24 to 5.31]) and TC (WMD, 5.43 [95% CI, 3.95 to 6.91]). Group rankings based on a cumulative probability diagram and SUCRA showed that CY was the most effective exercise intervention for patients with KOA in terms of WOMAC-Pain score. According to SUCRA ranking, the top 3 most effective exercises were CY (80.8%), RT (68.6%), and AE (67.9%) (Table 1).
WOMAC-Stiffness scores were reported in 21 studies ‡‡ (n = 1261 participants). Interventions included AE (n = 2), RT (n = 5), TC (n = 12), CY (n = 2), and YG (n = 1). Four studies1,4,11,45 performed direct comparison for various types of exercise intervention via a 3-arm design. Controls had significantly worse scores compared with YG (WMD, –1.40 [95% CI, –2.45 to –0.34]). Other pairwise comparisons showed no statistical significance. Group rankings based on a cumulative probability diagram and SUCRA showed that YG was the most effective intervention for improving the WOMAC-Stiffness score. According to SUCRA ranking, the top 3 effective exercises were YG (90.6%) > CY (64.3%) > AE (63.6%) (Table 1).
There were 23 studies §§ (1387 participants) that reported WOMAC-Function score. Interventions included AE (n = 3), RT (n = 6), TC (n = 12), CY (n = 2), and YG (n = 2). Five studies1,11,13,27,57 performed direct comparison for various types of exercise intervention via a 3-arm design. Significantly worse scores were seen in controls versus YG (WMD, –0.49 [95% CI, –0.95 to –0.02]). Other pairwise comparisons showed no statistical significance. Group rankings based on a cumulative probability diagram and SUCRA showed that YG was the most effective type of exercise for improving the WOMAC-Function score. According to SUCRA, the top 3 effective exercises were YG (77.4%) > AE (67.2%) > TC (56.8%) (Table 1).
Secondary Outcome Measures
The network analysis–based inconsistency test showed no significant global inconsistencies regarding the 6-MWT, VAS pain, or KOOS. Forest plots, cumulative probability graphs, and network diagrams comparing the intervention and control groups for all secondary outcome measures are shown in Supplemental Figure S1, and group rankings based on a cumulative probability diagram and SUCRA are shown in Supplemental Tables S3 to S5.
6-MWT
Overall, 14 studies ∥∥ (n = 678 participants) reported a 6-MWT score. Interventions included AE (n = 2), RT (n = 4), TC (n = 8), CY (n = 2), and YG (n = 1). Three studies1,23,57 performed direct comparison for various types of exercise intervention via a 3-arm design. However, other pairwise comparisons showed no significant differences. Group rankings based on a cumulative probability diagram and SUCRA showed that the 3 most effective exercises were CY (76.1%) > YG (59.5%) >AE (58.4%) (Supplemental Table S3).
VAS Pain
Eight studies4,6,20,29,45,48,61,63 (n = 432 participants) reported VAS pain scores. Interventions included AE (n = 4), RT (n = 2), and TC (n = 2). Four studies4,29,45,61 performed direct comparison for various types of exercise intervention via a 3-arm design. However, the pairwise comparisons showed no significant differences. Group rankings based on a cumulative probability diagram and SUCRA showed that the top 3 effective exercises were AE (77.2%) > RT (65.5%) > TC (32.2%) (Supplemental Table S4).
KOOS
There were 8 studies23,28,29,35,41–43,53 (n = 537 participants) that reported KOOS-Pain and 7 studies23,28,29,35,41,43,53 (n = 507 participants) that reported KOOS-Symptoms, KOOS-ADL, KOOS-Sports, and KOOS-QoL. Regarding KOOS-Symptoms, better scores were seen with CY versus AE (WMD, –0.44 [95% CI, –0.73 to –0.15]), and worse scores were seen with TC versus control (WMD, 0.62 [95% CI, 0.13 to 1.10]). Regarding KOOS-QoL, better scores were seen with CY versus AE (WMD, –0.44 [95% CI, –0.73 to –0.15]) and with TC versus RT (WMD, –0.89 [95% CI, –1.75 to –0.02]), and worse scores were seen with RT (WMD, 1.04 [95% CI, 0.36 to 1.71]) and YG (WMD, 1.07 [95% CI, 0.11 to 2.03]) versus the control group.
Group rankings based on a cumulative probability diagram and SUCRA showed that the 3 most effective exercises for improving the KOOS values were as follows: KOOS-Pain, AE (64.0%) > RT (63.4%) > YG (51.7%); KOOS-Symptoms, TC (84.5%) > RT (71.3%) > AE (54.8%); KOOS-ADL, YG (72.0%) > RT (63.6%) > CY (55.8%); KOOS-Sports, AE (65.4%) > RT (61.9%) > TC (45.4%); and KOOS-QoL, YG (79.1%) > RT (79.1%) > TC (67.3%) (Supplemental Table S5).
Publication Bias
The only outcome measure that was included in ≥10 studies was the WOMAC. Publication bias assessment showed that WOMAC-Pain, WOMAC-Stiffness, and WOMAC-Function had symmetric funnel plots, indicating no significant publication bias existed, as shown in Supplemental Figure S2.
Discussion
In this review of 39 studies, we found that all the evaluated exercise interventions were beneficial to patients with KOA for relieving pain, alleviating stiffness, improving function, and improving quality of life when compared with patients who had no intervention. AE (for pain relief) and YG (for joint stiffness, limited knee function, and quality of life) were shown to be the most effective interventions, followed by RT, TC, and CY.
With regard to pain, outcome measures included (in descending order) the WOMAC-Pain subscale, VAS pain, and KOOS-Pain subscale. The ranking results of the WOMAC-Pain subscale were CY> RT > AE > TC > YG; VAS pain, AE > RT > TC; and KOOS-Pain subscale, AE > RT > YG > TC > CY. We found that CY was most effective regarding WOMAC-Pain (SUCRA, 80.8%; WMD vs control, –4.45 [95% CI –5.69 to –3.20]), and AE was the most effective regarding VAS pain (SUCRA, 77.2%; WMD vs control, 0.04 [95% CI, –1.86 to 1.95]) and KOOS-Pain (SUCRA, 64.0%; WMD vs control, 3.10 [95% CI, –6.67 to 12.88]). Thus, AE ranked highly in terms of improving patient pain.
AE typically refers to hydrotherapy or exercise performed in the water, which has been applied to treat diseases for >18 years. 32 Studies have revealed that AE could significantly alleviate pain and improve body function through thermal stimulus and buoyancy. 18 Water temperatures ranging from 33.5°C to 35.5°C would be appropriate in that such temperatures allow patients to soak for long periods of time, ensuring a long enough exercise duration to achieve the therapeutic effect, and patients would not feel cold or overheat. 5 Different water depths could provide different buoyancies. Deeper water could provide more buoyancy to reduce weightbearing of the joint so as to alleviate symptoms in patients with KOA. 24
Alkatan et al 1 found that regular swimming could alleviate joint pain and stiffness and improve muscular function and strength in middle-aged and elderly patients with KOA. The pain-relieving effects of AE are subject to multiple factors, such as exercise regimen, intensity, frequency, and duration, and the optimal regimen and intensity remain to be further elucidated. Various types of AE could alleviate KOA joint pain and improve joint function.47,56 Silva et al 45 compared water-based exercise with land-based exercise and found that at the final follow-up, AE was more effective in relieving pain before and after walking, and was accompanied with fewer adverse effects. However, another study found that increasing the exercise intensity yielded a dissatisfactory effect, 19 which was consistent with results of an RCT conducted to compare the effect of aerobics, high-intensity RT, and low-intensity RT, 30 indicating that more other theories are needed to elucidate the role of exercise intensity in pain relief.
As for improvements in stiffness, limited function, and quality of life, the ranking results of stiffness were YG > AE > CY > RT > TC; limited function,YG > AE > TC > RT > CY; and quality of life, YG > RT > TC > AE > CY. Compared with the control group, we found that YG was the most effective exercise intervention for improving stiffness (WOMAC-Stiffness: WMD, –1.40 [95% CI, 0.–2.45 to –0.34]), function (WOMAC-Function: WMD, –0.49 [95% CI, 0–0.95 to –0.02]), and quality of life [KOOS-QoL: WMD, -1.07 [95% CI, 0.11 to 2.03]). YG is a TC in India and is beneficial to physical and mental health. It alleviates pain via simulating baroreceptors, increasing vagal tone and the serotonin level, and decreasing the generation of cortisol and substance P. 31 An RCT by Moonaz et al 34 found that YG could safely improve body activity, physical and mental health, and health-related quality of life in sedentary patients with arthritis. However, studies regarding YG for KOA differ in many aspects, such as different types of YG, duration, and frequency. Two studies23,37 adopted a comprehensive YG regimen, which included not only body posture (Asanas) but also respiration (Pranayama) and meditation. This makes the identification of the most effective YG type more difficult. According to Cheung et al, 8 Hatha YG training 5 times per week (1-time practice in class and 4 times at home) for 8 weeks showed better effect in pain relief, stiffness alleviation, and function improvement in elderly female patients with KOA, compared with other types of YG. This effect lasted for 20 weeks during the follow-up. 8 A 60-minute “mindfulness” YG training (3 times a week for 12 weeks) could be as effective as traditional YG in alleviating debilitating symptoms in female patients with KOA, whereas AE could be more effective in alleviating pain, improving self-reported body function, and improving quality of life. The effect was also satisfactory during the follow-up. 23 To summarize, YG is an effective treatment for KOA, especially for female patients, while few studies focus on male patients. More studies are needed to fill this gap.
Limitations
One limitation of this review and meta-analysis is that there was a measure of heterogeneity among included studies because of differences in the effects and exercise cycles of different types of exercise. Second, lack of study with a large sample size, missing data, and uneven sex distribution might also be sources of heterogeneity, which remains unresolved in that subgroup analysis could not be performed. Third, un-unified scoring scales could lead to heterogeneity, even though we applied WMD to pool the effects. All included studies failed to perform blinding of participants because of the characteristics of the exercise interventions, which might affect the results of this study. Lastly, we only included studies reported and published in English, which might cause some information loss as well as heterogeneity.
Conclusion
This review and meta-analysis showed that all 5 types of exercise could effectively attenuate KOA. AE (for pain relief) and YG (for joint stiffness, limited knee function, and quality of life) were revealed to be the most effective approaches, followed by RT, CY, and TC. More RCTs with a larger sample size and higher quality are needed to further validate the efficacy of exercise therapy for KOA.
Supplemental material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671231172773.
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671231172773 for Exercise Therapy for Knee Osteoarthritis: A Systematic Review and Network Meta-analysis by Ling Mo, Banghua Jiang, Tao Mei and Daihua Zhou in Orthopaedic Journal of Sports Medicine
Final revision submitted February 7, 2023; accepted February 22, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding was received from the Fundamental Research Funds for the Central University (20165Y5002) and the National Key R&D Program of China (2018 YFC2000602). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1.Alkatan M, Baker JR, Machin DR, et al. Improved function and reduced pain after swimming and cycling training in patients with osteoarthritis. J Rheumatol. 2016;43(3):666–672. [DOI] [PubMed] [Google Scholar]
- 2.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–1049. [DOI] [PubMed] [Google Scholar]
- 3.An B, Dai K, Zhu Z, et al. Baduanjin alleviates the symptoms of knee osteoarthritis. J Altern Complement Med. 2008;14(2):167–174. [DOI] [PubMed] [Google Scholar]
- 4.Assar S, Gandomi F, Mozafari M, Sohaili F. The effect of total resistance exercise vs. aquatic training on self-reported knee instability, pain, and stiffness in women with knee osteoarthritis: a randomized controlled trial. BMC Sports Sci Med Rehabil. 2020;12:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Becker BE. Aquatic therapy: scientific foundations and clinical rehabilitation applications. PM R. 2009;1(9):859–872. [DOI] [PubMed] [Google Scholar]
- 6.Brismée JM, Paige RL, Chyu MC, et al. Group and home-based tai chi in elderly subjects with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2007;21(2):99–111. [DOI] [PubMed] [Google Scholar]
- 7.Caldwell DM. An overview of conducting systematic reviews with network meta-analysis. Syst Rev. 2014;3:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheung C, Wyman JF, Resnick B, Savik K. Yoga for managing knee osteoarthritis in older women: a pilot randomized controlled trial. BMC Complement Altern Med. 2014;14:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Ann Intern Med. 2013;159(2):130–137. [DOI] [PubMed] [Google Scholar]
- 10.Fejer R, Ruhe A. What is the prevalence of musculoskeletal problems in the elderly population in developed countries? A systematic critical literature review. Chiropr Man Therap. 2012;20(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Foley A, Halbert J, Hewitt T, Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis—a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis. 2003;62(12):1162–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015;49(24):1554–1557. [DOI] [PubMed] [Google Scholar]
- 13.Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007;57(3):407–414. [DOI] [PubMed] [Google Scholar]
- 14.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. [DOI] [PubMed] [Google Scholar]
- 15.Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: part I. Caspian J Intern Med. 2011;2(2):205–212. [PMC free article] [PubMed] [Google Scholar]
- 16.Henderson KG, Wallis JA, Snowdon DA. Active physiotherapy interventions following total knee arthroplasty in the hospital and inpatient rehabilitation settings: a systematic review and meta-analysis. Physiotherapy. 2018;104(1):25–35. [DOI] [PubMed] [Google Scholar]
- 17.Higgins JP, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2019. [Google Scholar]
- 18.Hinman RS, Heywood SE, Day AR. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007;87(1):32–43. [DOI] [PubMed] [Google Scholar]
- 19.Jan MH, Lin JJ, Liau JJ, Lin YF, Lin DH. Investigation of clinical effects of high- and low-resistance training for patients with knee osteoarthritis: a randomized controlled trial. Phys Ther. 2008;88(4):427–436. [DOI] [PubMed] [Google Scholar]
- 20.Jorge RT, Souza MC, Chiari A, et al. Progressive resistance exercise in women with osteoarthritis of the knee: a randomized controlled trial. Clin Rehabil. 2015;29(3):234–243. [DOI] [PubMed] [Google Scholar]
- 21.Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66(3):622–636. [DOI] [PubMed] [Google Scholar]
- 22.Kan HS, Chan PK, Chiu KY, et al. Non-surgical treatment of knee osteoarthritis. Hong Kong Med J. 2019;25(2):127–133. [DOI] [PubMed] [Google Scholar]
- 23.Kuntz AB, Chopp-Hurley JN, Brenneman EC, et al. Efficacy of a biomechanically-based yoga exercise program in knee osteoarthritis: a randomized controlled trial. PLoS One. 2018;13(4):e0195653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kutzner I, Richter A, Gordt K, et al. Does aquatic exercise reduce hip and knee joint loading? In vivo load measurements with instrumented implants. PLoS One. 2017;12(3):e0171972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee HJ, Park HJ, Chae Y, et al. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: a pilot, randomized, waiting list controlled trial. Clin Rehabil. 2009;23(6):504–511. [DOI] [PubMed] [Google Scholar]
- 26.Li L, Cheng S, Wang G, Duan G, Zhang Y. Tai chi chuan exercises improve functional outcomes and quality of life in patients with primary total knee arthroplasty due to knee osteoarthritis. Complement Ther Clin Pract. 2019;35:121–125. [DOI] [PubMed] [Google Scholar]
- 27.Lim JY, Tchai E, Jang SN. Effectiveness of aquatic exercise for obese patients with knee osteoarthritis: a randomized controlled trial. PM R. 2010;2(8):723–731. [DOI] [PubMed] [Google Scholar]
- 28.Liu J, Chen L, Tu Y, et al. Different exercise modalities relieve pain syndrome in patients with knee osteoarthritis and modulate the dorsolateral prefrontal cortex: a multiple mode MRI study. Brain Behav Immun. 2019;82:253–263. [DOI] [PubMed] [Google Scholar]
- 29.Lund H, Weile U, Christensen R, et al. A randomized controlled trial of aquatic and land-based exercise in patients with knee osteoarthritis. J Rehabil Med. 2008;40(2):137–144. [DOI] [PubMed] [Google Scholar]
- 30.Mangione KK, McCully K, Gloviak A, et al. The effects of high-intensity and low-intensity cycle ergometry in older adults with knee osteoarthritis. J Gerontol A Biol Sci Med Sci. 1999;54(4):M184–M190. [DOI] [PubMed] [Google Scholar]
- 31.Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971–979. [DOI] [PubMed] [Google Scholar]
- 32.Messier SP, Royer TD, Craven TE, et al. Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the Fitness, Arthritis, and Seniors Trial (FAST). J Am Geriatr Soc. 2000;48(2):131–138. [DOI] [PubMed] [Google Scholar]
- 33.Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int. 2010;107(9):152–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moonaz SH, Bingham CO III, Wissow L, Bartlett SJ. Yoga in sedentary adults with arthritis: effects of a randomized controlled pragmatic trial. J Rheumatol. 2015;42(7):1194–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Munukka M, Waller B, Rantalainen T, et al. Efficacy of progressive aquatic resistance training for tibiofemoral cartilage in postmenopausal women with mild knee osteoarthritis: a randomised controlled trial. Osteoarthritis Cartilage. 2016;24(10):1708–1717. [DOI] [PubMed] [Google Scholar]
- 36.Ni GX, Song L, Yu B, Huang CH, Lin JH. Tai chi improves physical function in older Chinese women with knee osteoarthritis. J Clin Rheumatol. 2010;16(2):64–67. [DOI] [PubMed] [Google Scholar]
- 37.Park J, McCaffrey R, Newman D, Liehr P, Ouslander JG. A pilot randomized controlled trial of the effects of chair yoga on pain and physical function among community-dwelling older adults with lower extremity osteoarthritis. J Am Geriatr Soc. 2017;65(3):592–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Piercy KL, Troiano RP, Ballard RM, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rafiq MT, Hamid MSA, Hafiz E. Short-term effects of strengthening exercises of the lower limb rehabilitation protocol on pain, stiffness, physical function, and body mass index among knee osteoarthritis participants who were overweight or obese: a clinical trial. ScientificWorldJournal. 2021;2021:6672274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rafiq MT, Hamid MSA, Hafiz E. Effect of progressive resistance strength training on body mass index, quality of life and functional capacity in knee osteoarthritis: a randomized controlled trial. J Multidiscip Healthc. 2021;14:2161–2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rewald S, Lenssen AFT, Emans PJ, et al. Aquatic cycling improves knee pain and physical functioning in patients with knee osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101(8):1288–1295. [DOI] [PubMed] [Google Scholar]
- 42.Rezasoltani Z, Sanati E, Mofrad RK, et al. Randomized controlled trial of aquatic cycling for treatment of knee osteoarthritis in elderly people. Top Geriatr Rehabil. 2020;36(2):103–109. [Google Scholar]
- 43.Salacinski AJ, Krohn K, Lewis SF, et al. The effects of group cycling on gait and pain-related disability in individuals with mild-to-moderate knee osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther. 2012;42(12):985–995. [DOI] [PubMed] [Google Scholar]
- 44.Sheikh AM, Vissing J. Exercise therapy for muscle and lower motor neuron diseases. Acta Myol. 2019;38(4):215–232. [PMC free article] [PubMed] [Google Scholar]
- 45.Silva LE, Valim V, Pessanha AP, et al. Hydrotherapy versus conventional land-based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Phys Ther. 2008;88(1):12–21. [DOI] [PubMed] [Google Scholar]
- 46.Simão AP, Avelar NC, Tossige-Gomes R, et al. Functional performance and inflammatory cytokines after squat exercises and whole-body vibration in elderly individuals with knee osteoarthritis. Arch Phys Med Rehabil. 2012;93(10):1692–1700. [DOI] [PubMed] [Google Scholar]
- 47.So BCL, Kong ISY, Lee RKL, et al. The effect of Ai Chi aquatic therapy on individuals with knee osteoarthritis: a pilot study. J Phys Ther Sci. 2017;29(5):884–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taglietti M, Facci LM, Trelha CS, et al. Effectiveness of aquatic exercises compared to patient-education on health status in individuals with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2018;32(6):766–776. [DOI] [PubMed] [Google Scholar]
- 49.Tao J, Liu J, Egorova N, et al. Increased hippocampus-medial prefrontal cortex resting-state functional connectivity and memory function after tai chi chuan practice in elder adults. Front Aging Neurosci. 2016;8:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Topp R, Woolley S, Hornyak J III, Khuder S, Kahaleh B. The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Arch Phys Med Rehabil. 2002;83(9):1187–1195. [DOI] [PubMed] [Google Scholar]
- 51.Tsai PF, Chang JY, Beck C, Kuo YF, Keefe FJ. A pilot cluster-randomized trial of a 20-week Tai Chi program in elders with cognitive impairment and osteoarthritic knee: effects on pain and other health outcomes. J Pain Symptom Manage. 2013;45(4):660–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vincent KR, Vincent HK. Concentric and eccentric resistance training comparison on physical function and functional pain outcomes in knee osteoarthritis: a randomized controlled trial. Am J Phys Med Rehabil. 2020;99(10):932–940. [DOI] [PubMed] [Google Scholar]
- 53.Waller B, Munukka M, Rantalainen T, et al. Effects of high intensity resistance aquatic training on body composition and walking speed in women with mild knee osteoarthritis: a 4-month RCT with 12-month follow-up. Osteoarthritis Cartilage. 2017;25(8):1238–1246. [DOI] [PubMed] [Google Scholar]
- 54.Wang C, Schmid CH, Hibberd PL, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum. 2009;61(11):1545–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang S, Yin H, Wang X, et al. Efficacy of different types of exercises on global cognition in adults with mild cognitive impairment: a network meta-analysis. Aging Clin Exp Res. 2019;31(10):1391–1400. [DOI] [PubMed] [Google Scholar]
- 56.Wang TJ, Belza B, Elaine Thompson F, Whitney JD, Bennett K. Effects of aquatic exercise on flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. J Adv Nurs. 2007;57(2):141–152. [DOI] [PubMed] [Google Scholar]
- 57.Wortley M, Zhang S, Paquette M, et al. Effects of resistance and Tai Ji training on mobility and symptoms in knee osteoarthritis patients. J Sport Health Sci. 2013;2(4):209–214. [Google Scholar]
- 58.Xiao CM, Li JJ, Kang Y, Zhuang YC. Follow-up of a Wuqinxi exercise at home programme to reduce pain and improve function for knee osteoarthritis in older people: a randomised controlled trial. Age Ageing. 2021;50(2):570–575. [DOI] [PubMed] [Google Scholar]
- 59.Xiao Z, Li G. The effect of Wuqinxi exercises on the balance function and subjective quality of life in elderly, female knee osteoarthritis patients. Am J Transl Res. 2021;13(6):6710–6716. [PMC free article] [PubMed] [Google Scholar]
- 60.Ye J, Simpson MW, Liu Y, et al. The effects of baduanjin qigong on postural stability, proprioception, and symptoms of patients with knee osteoarthritis: a randomized controlled trial. Front Med (Lausanne). 2019;6:307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yennan P, Suputtitada A, Yuktanandana PJAB. Effects of aquatic exercise and land-based exercise on postural sway in elderly with knee osteoarthritis. Asian Biomed. 2010;4(5):739–745. [Google Scholar]
- 62.Zeng CY, Zhang ZR, Tang ZM, Hua FZ. Benefits and mechanisms of exercise training for knee osteoarthritis. Front Physiol. 2021;12:794062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang S, Guo G, Li X, et al. The effectiveness of traditional Chinese Yijinjing Qigong exercise for the patients with knee osteoarthritis on the pain, dysfunction, and mood disorder: a pilot randomized controlled trial. Front Med (Lausanne). 2021;8:792436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhu Q, Huang L, Wu X, et al. Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: a randomized controlled trial. J Sport Health Sci. 2016;5(3):297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhu Q, Huang L, Wu X, et al. Effect of Taijiquan practice versus wellness education on knee proprioception in patients with knee osteoarthritis: a randomized controlled trial. J Tradit Chin Med. 2017;37(6):774–781. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671231172773 for Exercise Therapy for Knee Osteoarthritis: A Systematic Review and Network Meta-analysis by Ling Mo, Banghua Jiang, Tao Mei and Daihua Zhou in Orthopaedic Journal of Sports Medicine