Cardiovascular diseases, including heart disease, hypertension and heart failure, along with stroke, continue to be leading causes of death in the United States.1,2 Hypertension currently affects nearly 78 million* adults in the United States and is also a major modifiable risk factor for other cardiovascular diseases and stroke.1 According to data from the National Health and Nutrition Evaluation Survey (NHANES) in 2007–2010, 81.5% of those with hypertension are aware they have it, and 74.9% are being treated but only 52.5% are under control, with significant variation across different patient subgroups.1,3–6 Of those with uncontrolled hypertension, 89.4% reported having a usual source of health care, and 85.2% reported having health insurance.7 This is the current status, despite the fact that therapies to lower blood pressure and associated risks of cardiovascular events and death have been available for decades and various education and quality improvement efforts have been targeted at patients and healthcare providers.
The direct and indirect costs of hypertension are enormous, considering the number of patients and their families impacted as well as the healthcare dollars spent on treatment and blood pressure-related complications.8 Currently, hypertension affects 46% of patients with known cardiovascular disease, 72% of those who have suffered a stroke, and was listed as a primary or contributing cause in approximately 15% of the 2.4 million deaths in 2009.1 In 2008, the total estimated direct and indirect cost of hypertension was estimated at $69.9 billion.8 Thus, it is imperative to identify, disseminate and implement more effective approaches to achieve optimal control of this condition.
High-quality blood pressure management is multifactorial and requires engagement of patients, families, providers and healthcare delivery systems and communities. This includes expanding patient and healthcare provider awareness, appropriate lifestyle modifications, access to care, evidence-based treatment, a high level of medication adherence and adequate follow-up.9 Recognizing the urgent need to address inadequate control, the American Heart Association (AHA) has made hypertension a primary focus area of its 2014–2017 strategic plan as it seeks to improve the cardiovascular health of all Americans by 20% and reduce the death rate from cardiovascular disease and stroke by 20% by 2020.10 Similarly, Million Hearts, a US Department of Health and Human Services initiative spearheaded by the Centers for Disease Control (CDC) and Prevention and the Centers for Medicare & Medicaid Services (CMS) to prevent a million heart attacks and strokes by 2017, has focused its first 2 years on actions to improve and achieve control of hypertension.11
We believe that identification of best practice, evidence–based management algorithms leading to standardization of treatment is a critical element in helping to achieve these ambitious national goals at a population level. In this paper, we describe the value of hypertension treatment algorithms, provide criteria for effective hypertension management algorithms, describe an AHA/American College of Cardiology (ACC)/CDC-recommended treatment algorithm based on current guidelines and describe examples of other specific algorithms that have been associated with improved blood pressure on a large scale.
The Value of Hypertension Treatment Algorithms As Part of a Multifactorial Approach to Improve Blood Pressure Control
As described previously, despite the strong evidence and consensus regarding the treatment and control of high blood pressure,9,12 as well as the availability of many different therapeutic options, achieving success in hypertension control at both the individual patient-level and even more importantly, the population-level, has remained a major challenge nationally.
Although there is no single explanation for the poor hypertension control seen in many patient subgroups, the fragmentation of health care for many patients and the lack of consistent implementation of system-level solutions in clinical practice and healthcare delivery systems appear to be important contributors. Efforts focused primarily on educating patients and providers about hypertension and the benefits of its treatment have not been sufficient in bringing hypertension under control. Similarly, interventions targeting only physicians have not led to consistent and meaningful improvements on a large scale.13 However, there are examples of substantial success that could be emulated and scaled with a high likelihood of important benefit.
To reduce the prevalence of hypertension in the United States,10,14 system-level approaches will be needed. Successful examples from other medical areas where a system-level approach has been taken include reducing medical errors and improving patient safety in the hospital setting15; improving the inpatient treatment and outcomes of acute myocardial infarction, heart failure, stroke and cardiopulmonary resuscitation16; reducing health disparities in the treatment of cardiovascular conditions16; early detection and intervention in sepsis to lower case fatality17,18; and reducing hospital-acquired infections.19,20 In the case of hypertension, system-level methods can address multiple factors in a coordinated manner:
Identifying all patients eligible for management
Monitoring at the practice/population level
Increasing patient and provider awareness
Providing an effective diagnosis and treatment guideline
Systematic follow-up of patients for initiation and intensification of therapy
Clarifying roles of healthcare providers to implement a team approach
Reducing barriers for patients to receive and adhere to medications as well as to implementing lifestyle modifications
Leveraging the electronic medical record systems being established throughout the US to support each of these steps
Several examples of success using a system-level paradigm have been recently reported. For example, within Kaiser Permanente Northern California, a large integrated healthcare delivery system caring for >3 million members, a regional hypertension program was implemented involving five major components: creation and maintenance of a health system-wide electronic hypertension registry, tracking hypertension control rates with regular feedback to providers at a facility- and provider-level, development and frequent updating of an evidence-based treatment guideline, promotion of single-pill combination therapies and using medical assistants for follow-up blood pressure checks to facilitate necessary treatment intensification. Between 2001 and 2009, the number of patients with hypertension increased from 349,937 to 652,763, but the proportion of hypertensive patients meeting target blood pressure goals improved substantially from 44% to >80%, and continued to improve to >87% in 2011.21 Favorable hypertension control rates have been observed in other healthcare delivery systems22 as well as coordinated health systems such as the Veterans Affairs medical system.23–25
Developing, disseminating and implementing an effective hypertension treatment algorithm is a critical part of a multipronged, systematic approach to controlling hypertension, as it facilitates clinical decision-making, provides a default approach with proven benefits, and engages multiple providers in a coordinated manner. We describe next the principles for developing such an algorithm.
Principles for Algorithm Development
The following is a summary of principles recommended by the AHA, ACC, and CDC for creating an effective hypertension management algorithm:
Base algorithm components and processes on the best available science.
Format to be simple to update as better information becomes available.
Create feasible, simple implementation strategy.
Include patient version at appropriate scientific and language literacy level.
Consider costs of diagnosis, monitoring, treatment.
Develop algorithm in format easily used within a team approach to health care.
Develop algorithm in a format able to be incorporated into electronic health records for use as clinical decision support.
Include a disclaimer to ensure that the algorithm is not used to counter the treating healthcare provider’s best clinical judgment.
The purpose of these principles is to establish a common platform for the development and implementation of hypertension management algorithms tailored to different practice settings and populations. We note the last principle supports the notion that treatment guidelines serve to facilitate a systematic approach to the management of hypertension, but provide appropriate modifications based on specific patient characteristics, preferences and other pragmatic factors (eg, cost, pill burden, risks of certain side effects) to optimize a personalized approach to the care of individual patients.9,12,26,27 In addition, ongoing randomized clinical trials (eg, SPRINT28) are addressing optimal blood pressure targets for specific patient subgroups such as the elderly and patient with chronic kidney diseases to maximize net clinical benefit and avoid unnecessary complications.
AHA/ACC/CDC Hypertension Treatment Algorithm
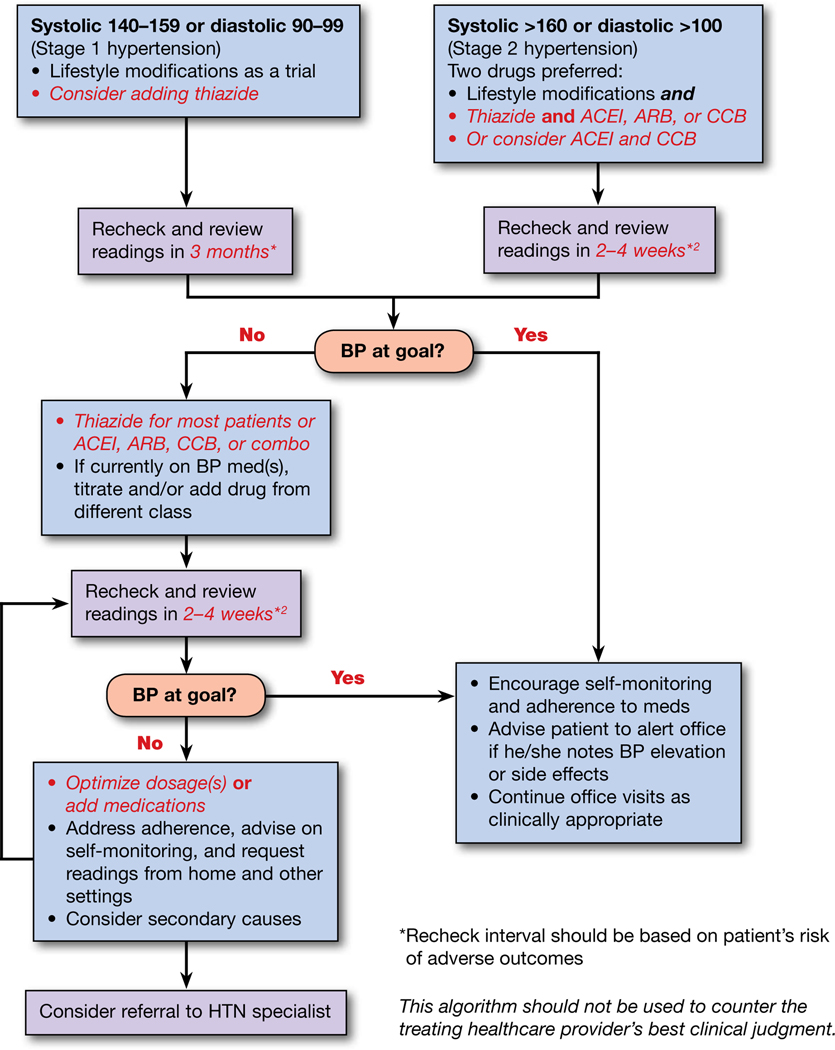
In the Appendix is a template outlining a general approach for an effective treatment algorithm that incorporates the principles described previously and balances applicability the largest number of hypertensive patients with the flexibility and the level of detail to support individualization of therapy.
Several existing algorithms for hypertension treatment in large healthcare settings associated with improved blood pressure in populations21 have also been reviewed, which included a look at both private and public systems, systems with regional reach, as well as an algorithm used by the US Department of Veteran Affairs that are in support of the recommended principles. These algorithms are either attached in the online-only data supplement or are available for public use within the resources and tools section of the Million Hearts initiative Web site at http://millionhearts.hhs.gov/resources.html.
Call-to-Action, Next Steps, and Conclusions
It is critical that the AHA, ACC and CDC, together with other organizations, continue to identify, define, and implement exemplary local, regional, and national programs that facilitate better blood pressure awareness, treatment, and control together with improving other cardiovascular health factors and behaviors.11,15,29–31,31a Arming healthcare providers, health systems, and communities with proven tools, algorithms, strategies, programs, and other best practices along with expertise and technical assistance for improving blood pressure awareness, treatment, and control is essential to reducing the tremendous burden of cardiovascular risk.30,32
This advisory serves as a call to action for broad-based efforts to improve hypertension awareness, treatment, and the proportion of patients treated and controlled. There is a clear need to provide enhanced, evidence-based, blood pressure treatment systems for providers, including standardization of protocols and algorithms, incentives for improved performance based on achieving and maintaining patients at blood pressure goals, and technology-facilitated clinical decision support and feedback.32 As noted previously, health system wide implementation of focused evidence-based hypertension treatment algorithms together with regularly scheduled performance feedback within a coordinated multifactorial management program have been associated with substantially improved hypertension control in large populations and varied clinical practice settings.21,32–34 This approach can facilitate the ability to emphasize existing evidence-based recommendations and integrate new evidence as it becomes available. Successful best practices or innovations can be further identified and then disseminated health system wide.21 Such an approach is scalable, sustainable, and of high value, especially as the use of electronic medical records becomes even more widespread nationally.21,33,34,40 This advisory has provided a number of examples of algorithms from successful programs that can be readily implemented in diverse healthcare settings. Greater participation in innovative programs such as the AHA’s Heart 360 personal health record,35 AHA/ASA’s Get With The Guidelines Program,36 the AHA/ADA/ACS Guideline Advantage Program,37 and the HHS Million Hearts initiative,11,15,30,31 as well as the ACC’s National Cardiovascular Data Registries (NCDR)38 and CDC Coverdell Stroke registry,39 should also be encouraged and incentivized.
Further engaging individuals in the hypertension control process, motivating more proactive management though shared accountability and incentives for blood pressure treatment and control are also essential.30 There are also opportunities for the increased role of pharmacists and other community-based providers in hypertension treatment and control.30,40,41 There is also great potential to apply an innovative mix of health information technology, peer support, feedback, and incentive programs designed to drive actionable, patient-centered blood pressure awareness, treatment and control programs. Workplace and community based wellness programs can also have significant impact.30
It is also vital that these programs are implemented among broader segments of the population. Disparities/inequities in hypertension awareness, treatment, and control continue to exist in a number of patient subgroups.6,42 Intervention programs for hypertension should be specifically targeted to groups with the greatest cardiovascular risk and disease burden based on clinical risk factors and appropriate consideration of sex, race, ethnicity, socioeconomic status, disability, and geographic location.30 Additional research is needed to better define blood pressure treatment goals especially in specific populations including by age, sex, race, ethnicity, and comorbid conditions. It is essential that there be proportionate representation of these patient populations in the study of blood pressure goals as well as new hypertension treatment technologies such as catheter-based renal sympathetic denervation.
The AHA, ACC, CDC, and other organizations should continue to foster effective activities regarding hypertension which include surveillance, education and media, organizational partnerships, and environmental and policy changes.30 Building on such programs as the
AHA’s Life’s Simple 7 program43 with a longitudinal cardiovascular health tracking system, patient-oriented clinical decision support tool, individual patient-oriented cardiovascular health performance measures, and data feedback, and
ACC’s CardioSmart Patient Education Portal44 with a customized patient dashboard for blood pressure management, an interactive workbook to educate and motivate better health, and a patient text messaging program providing heart healthy tips aimed at primary prevention should be considered within a comprehensive system-level management program. This approach may help to facilitate and incentivize improvement in blood pressure control, cardiovascular health, as well as enhance real-time surveillance of cardiovascular health. Further research efforts to enhance specific interventions for improving patient adherence and to identify optimal patient-centered, value oriented systems of care should continue to be supported.
This advisory is intended to complement and support clinical guidelines, providing clinicians and health systems tools to improve treatment and control of hypertension. The prevention of heart disease and stroke mandates a greater emphasis on the population-wide improvement of blood pressure awareness, treatment, and control together with other cardiovascular health factors.15,26,45
Supplementary Material
Appendix
Controlling Hypertension in Adults1
© 2013 The Authors. Hypertension is published on behalf of the American Heart Association, Inc., by Wolters Kluwer; the Journal of the American College of Cardiology is published on behalf of the American College of Cardiology Foundation by Elsevier Inc. This is an open access article under the terms of the Creative Commons Attribution Non-Commercial-NoDervis License, which permits use, distribution, and reproduction in any medium, provided that the Contribution is properly cited, the use is non-commercial, and no modifications or adaptations are made.
The blood pressure (BP) goal for an individual is set by utilizing a combination of factors including scientific evidence, clinical judgment, and patient tolerance. For most people, the goal is <140 and <90;3 however, lower targets may be appropriate for some populations such as African-Americans, the elderly, or patients with LV hypertrophy, systolic or diastolic LV dysfunction, diabetes mellitus or chronic kidney disease. Lifestyle modifications (LM) should be initiated in all patients with hypertension (HTN) and they should be assessed for target organ damage and existing cardiovascular disease. Self-monitoring4 is encouraged for most patients throughout their care, and requesting and reviewing readings from home and community settings can help the provider assist the patient in achieving and maintaining good control. For patients with hypertension in combination with certain clinical conditions, specific medications should be considered first-line treatments.
Suggested Medications for Treatment of Hypertension in Presence of Certain Medical Conditions
Coronary artery disease/Post MI: BB, ACEI
Systolic heart failure: ACEI or ARB, BB, ALDO ANTAG, thiazide
Diastolic heart failure: ACEI or ARB, BB, thiazide
Diabetes: ACEI or ARB, thiazide, BB, CCB
Kidney disease: ACEI or ARB
Stroke or TIA: thiazide, ACEI
Lifestyle Modifications3 (LM)
| Modification | Recommendation | Approximate SBP Reduction (Range)** |
|---|---|---|
| Reduce weight | Maintain normal body weight (body mass index 18.5–24.9 kg/m2) | 5–20 mm Hg/10 kg |
| Adopt DASH * 5 eating plan | Consume a diet rich in fruits, vegetables, and low-fat dairy products with a reduced content of saturated and total fat | 8–14 mm Hg |
| Lower sodium intake 6 | a. Consume no more than 2,400 mg of sodium/day; b. Further reduction of sodium intake to 1,500 mg/day is desirable since it is associated with even greater reduction in BP; and c. Reduce intake by at least 1,000 mg/day since that will lower BP, even if the desired daily sodium intake is not acheived |
2–8 mm Hg |
| Physical activity | Engage in regular aerobic physical activity such as brisk walking (at least 30 min per day, most days of the week) | 4–9 mm Hg |
| Moderation of alcohol consumption | Limit consumption to no more than 2 drinks (e.g., 24 oz beer, 10 oz wine, or 3 oz 80-proof whiskey) per day in most men, and to no more than 1 drink per day in women and lighter weight persons | 2–4 mm Hg |
DASH, dietary approaches to stop hypertension
The effects of implementing these modifications are dose and time dependent, and could be greater for some individuals
Abbreviations
ACEI, angiotensin-converting-enzyme inhibitor; ALDO ANTAG, aldosterone antagonist; ARB, angiotensin II receptor blocker; BB, ß-blocker; BP, blood pressure; CCB, calcium channel blocker; HTN, hypertension; MI, myocardial infarction; SBP, systolic blood pressure; TIA, transient ischemic attack
Writing Group Disclosures
| Writing Group Member | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Alan S. Go | Kaiser Permanente of Northern California; University of California, San Francisco | None | None | None | None | None | None | None |
| Mary Ann Bauman | INTEGRIS Health, Inc | None | None | None | None | None | None | None |
| Sallyann M. Coleman King | CDC | None | None | None | None | None | None | None |
| Gregg C. Fonarow | UCLA | AHRQ†; NIH† | None | None | None | None | Novartis†; Bayer*; Johnson & Johnson*; Medtronic* | None |
| Willie Lawrence | HCA and Midwest Heart and Vascular Associates | No | No | No | No | No | BCBS KC (Credentials Committee, P & T Committee)* | Wife is CFO Childrens’ Mercy Hospital, KC† |
| Eduardo Sanchez | American Heart Association (since 4/15/13); Blue Cross and Blue Shield of Texas (through 4/15/2013) | None | None | None | None | None | None | None |
| Kim A. Williams | Rush University | None | None | None | None | None | None | None |
This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10,000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10,000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Modest.
Significant.
Reviewer Disclosures
| Reviewer | Employment | Research Grant | Other Research Support | Speakers’ Bureau/Honoraria | Expert Witness | Ownership Interest | Consultant/Advisory Board | Other |
|---|---|---|---|---|---|---|---|---|
| Robert M. Carey | University of Virginia Health System | NIH† | None | None | None | None | None | None |
| Gregory D. Fink | Michigan State University | NIH† (money paid to institution); AHA† (money paid to institution); Medtronic* | None | None | None | None | None | None |
| John M. Flack | Wayne State University | NIH*; Novartis*; Medtronic* | None | Novartis† | None | None | Novartis†; NIH*; Medtronic*; Back Beat Hypertension*; NIVasc* | None |
| Daniel W. Jones | University of Mississippi | None | None | None | None | None | None | None |
| Janet Wright | CDC | None | None | None | None | None | None | None |
This table represents the relationships of reviewers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all reviewers are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10,000 or more during any 12-month period, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10,000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.
Modest.
Significant.
Footnotes
The estimate is based on hypertension definition of blood pressure reading ≥140/90 mm Hg, current use of antihypertensive medications, or being told of having hypertension on 2 occasions by a healthcare provider. When the third component of the definition is excluded, the estimated number of prevalence cases among US adults would be 67 million.7
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire D, Mohler E, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy SL, Xu JQ, Kochanek KD. Deaths: final data for 2010. National Vital Statistics Reports; Vol 61 No. 4. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 3.Yoon SS, Burt V, Louis T, Carroll MD. Hypertension among adults in the United States, 2009–2010. NCHS Data Brief. 2012:1–8. [PubMed] [Google Scholar]
- 4.Egan BM, Li J, Qanungo S, Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients: National Health and Nutrition Examination Surveys 1988–2010. Circulation. 2013;128:29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuznik A, Mardekian J, Tarasenko L. Evaluation of cardiovascular disease burden and therapeutic goal attainment in us adults with chronic kidney disease: an analysis of National Health and Nutritional Examination Survey data, 2001–2010. BMC Nephrol. 2013;14:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Racial/ethnic disparities in the awareness, treatment, and control of hypertension - United States, 2003–2010. MMWR Morb Mortal Wkly Rep. 2013;62:351–355. [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Vital signs: prevalence, treatment, and control of hypertension—United States, 2003–2010. MMWR Morb Mortal Wkly Rep. 2012;61:703–709. [PubMed] [Google Scholar]
- 8.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ. Forecasting the future of cardiovascular disease in the united states: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. [DOI] [PubMed] [Google Scholar]
- 9.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 11.Frieden TR, Berwick DM. The “Million Hearts” initiative—preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. [DOI] [PubMed] [Google Scholar]
- 12.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Burnier M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Ferrari R, Hasdai D, Hoes AW, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Gillebert TC, Rosei EA, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Vlachopoulos C, Volpe M, Wood DA. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 13.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010:CD005182. [DOI] [PubMed] [Google Scholar]
- 14.Healthy People 2020. Heart disease and stroke. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=21. Accessed November 11, 2013.
- 15.Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 16.Ellrodt AG, Fonarow GC, Schwamm LH, Albert N, Bhatt DL, Cannon CP, Hernandez AF, Hlatky MA, Luepker RV, Peterson PN, Reeves M, Smith EE. Synthesizing lessons learned from Get With The Guidelines: the value of disease-based registries in improving quality and outcomes. Circulation. 2013: published online before print October 28, 2013, 10.1161/01.cir.0000435779.48007.5c. [DOI] [PubMed] [Google Scholar]
- 17.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. [DOI] [PubMed] [Google Scholar]
- 18.Rivers EP, Coba V, Whitmill M. Early goal-directed therapy in severe sepsis and septic shock: a contemporary review of the literature. Curr Opin Anaesthesiol. 2008;21:128–140. [DOI] [PubMed] [Google Scholar]
- 19.Wheeler DS, Giaccone MJ, Hutchinson N, Haygood M, Bondurant P, Demmel K, Kotagal UR, Connelly B, Corcoran MS, Line K, Rich K, Schoettker PJ, Brilli RJ. A hospital-wide quality-improvement collaborative to reduce catheter-associated bloodstream infections. Pediatrics. 2011;128:e995–e1004; quiz e1004–1007. [DOI] [PubMed] [Google Scholar]
- 20.Morris AC, Hay AW, Swann DG, Everingham K, McCulloch C, McNulty J, Brooks O, Laurenson IF, Cook B, Walsh TS. Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle. Crit Care Med. 2011;39:2218–2224. [DOI] [PubMed] [Google Scholar]
- 21.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.California Department of Managed Healthcare. California health plans vs. national top 10 performance. Right Care Initiative: Selected HEDIS Measures. 2012. Available at: http://www.dmhc.ca.gov/library/reports/news/rci/top10plans.pdf. Accessed. November 11, 2013. [Google Scholar]
- 23.Department of Veterans Affairs, Veterans Health Administration, Office of Quality and Safety. 2009 VHA facility quality and safety report. Available at: http://www.va.gov/health/docs/HospitalReportCard2009.pdf. Accessed November 11, 2013.
- 24.Report to the Appropriations Committee of the US House of Representatives in response to House Appropriations report No. 110–186, accompanying public law 110–161, the Consolidated Appropriations Act. 2008.
- 25.Department of Veterans Affairs, Veterans Health Administration, Office of Quality and Safety. 2010. VHA facility quality and safety report. Available at: http://www.va.gov/health/docs/HospitalReportCard2010.pdf. Accessed November 11, 2013.
- 26.KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2012;2:S388–S397. [DOI] [PubMed] [Google Scholar]
- 27.Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(suppl 1):S11–S66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Systolic Blood Pressure Intervention Trial (SPRINT). 2013. Available at: http://clinicaltrials.gov/ct2/show/NCT01206062. Accessed November 11, 2013.
- 29.Tomaselli GF, Harty MB, Horton K, Schoeberl M. The American Heart Association and the Million Hearts initiative: a presidential advisory from the American Heart Association. Circulation. 2011;124:1795–1799. [DOI] [PubMed] [Google Scholar]
- 30.Pearson TA, Palaniappan LP, Artinian NT, Carnethon MR, Criqui MH, Daniels SR, Fonarow GC, Fortmann SP, Franklin BA, Galloway JM, Goff DC Jr, Heath GW, Frank AT, Kris-Etherton PM, Labarthe DR, Murabito JM, Sacco RL, Sasson C, Turner MB. American Heart Association guide for improving cardiovascular health at the community level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127:1730–1753. [DOI] [PubMed] [Google Scholar]
- 31.Jones DW, Peterson ED, Bonow RO, Masoudi FA, Fonarow GC, Smith SC Jr, Solis P, Girgus M, Hinton PC, Leonard A, Gibbons RJ. Translating research into practice for healthcare providers: the American Heart Association’s strategy for building healthier lives, free of cardiovascular diseases and stroke. Circulation. 2008;118:687–696. [DOI] [PubMed] [Google Scholar]; 31a. Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, Ferdinand KC, Forciea MA, Frishman WH, Jaigobin C, Kostis JB, Mancia G, Oparil S, Ortiz E, Reisin E, Rich MW, Schocken DD, Weber MA, Wesley DJ. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2011;123:2434–2506. [DOI] [PubMed] [Google Scholar]
- 32.Handler J, Lackland DT. Translation of hypertension treatment guidelines into practice: a review of implementation. J Am Soc Hypertens. 2011;5:197–207. [DOI] [PubMed] [Google Scholar]
- 33.Aucott JN, Pelecanos E, Dombrowski R, Fuehrer SM, Laich J, Aron DC. Implementation of local guidelines for cost-effective management of hypertension. A trial of the firm system. J Gen Intern Med. 1996;11:139–146. [DOI] [PubMed] [Google Scholar]
- 34.Choma NN, Huang RL, Dittus RS, Burnham KE, Roumie CL. Quality improvement initiatives improve hypertension care among veterans. Circ Cardiovasc Qual Outcomes. 2009;2:392–398. [DOI] [PubMed] [Google Scholar]
- 35.American Heart Association/American Stroke Association. Heart 360. Available at: http://www.heart360.org. Accessed November 11, 2013.
- 36.American Heart Association. Get With the Guidelines. Available at: http://www.heart.org/GWTG. Accessed November 11, 2013.
- 37.American Cancer Society, American Diabetes Association, and American Heart Association. The Guideline Advantage. Available at: http://www.theguidelineadvantage.org. Accessed November 11, 2013.
- 38.American College of Cardiology. National Cardiovascular Data Registry. Available at: https://www.ncdr.com/webncdr/. Accessed November 11, 2013.
- 39.Centers for Disease Control and Prevention. State Heart Disease and Stroke Prevention Programs. Paul Coverdell National Acute Stroke Registry (PCNASR). Available at: http://www.cdc.gov/dhdsp/programs/stroke_registry.htm. Accessed November 11, 2013. [Google Scholar]
- 40.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, Carrell D, Tyll L, Larson EB, Thompson RS. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The Guide to Community Preventive Services. Cardiovascular disease prevention and control: team-based care to improve blood pressure control. Available at: http://www.thecommunityguide.org/cvd/teambasedcare.html. Accessed November 11, 2013.
- 42.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. [DOI] [PubMed] [Google Scholar]
- 43.American Heart Association. Life’s Simple 7. Available at: http://mylifecheck.heart.org/. Accessed November 11, 2013.
- 44.American College of Cardiology. CardioSmart. Available at: https://www.cardiosmart.org/. Accessed November 11, 2013.
- 45.Smith SC Jr, Chen D, Collins A, Harold JG, Jessup M, Josephson S, Logstrup S, Sacco RL, Vardas PE, Wood DA, Zoghbi WA. Moving from political declaration to action on reducing the global burden of cardiovascular diseases: a statement from the Global Cardiovascular Disease Taskforce. Circulation. 2013: published online before print September 17, 2013, 10.1161/CIR.0b013e3182a93504. [DOI] [PubMed] [Google Scholar]
References
- 1.Go AS, Bauman M, Coleman King SM, Fonarow GC, Lawrence W, Williams K, Sanchez E. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2013: published online before print November 15, 2013, 10.1161/HYP.0000000000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved Blood Pressure Control Associated with a Large-Scale Hypertension Program. JAMA. 2013;310(7);699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Heart, Lung, and Blood Institute, National Institutes of Health. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure — Complete Report. National Heart, Lung, and Blood Institute, National Institutes of Health. NIH Publication No. 04–5230, 2004. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Self-Measured Blood Pressure Monitoring: Action Steps for Public Health Practitioners. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2013. [Google Scholar]
- 5.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 6.Eckel RH, Jakicic JM, Ard JD, Hubbard VS, de Jesus JM, Lee I-M, Lichtenstein AH, Loria CM, Millen BE, Houston Miller N, Nonas CA, Sacks FM, Smith SC Jr, Svetkey LP, Wadden TW, Yanovski SZ. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013: published online before print November 12, 2103, 10.1161/01.cir.0000437740.48606.d1. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.