Abstract
Although evidence exists for an association between income level and diet quality, a causal relationship has not been established. A number of studies find that the price of nutritious food and the time cost to prepare foods are economically driven reasons for this relationship. However, in addition to economic constraints, low-income individuals and families face a number of additional challenges linked with food choice, eating behaviors, and diet-related chronic conditions that contribute to diet quality and health. Low-income individuals have a higher burden of employment and food- and housing-related insecurity that threatens the livelihood of their household. Poverty and exposure to these insecurities are hypothesized to activate biobehavioral and psychological mechanisms—endocrine, immune, and neurologic systems—that influence food choice and consumption. Examples of biobehavioral and psychological factors that influence diet are stress, poor sleep, and diminished cognitive capacity. High levels of stress, poor sleep, and cognitive overload compound the challenges of economic constraints, creating a mentality of scarcity that leads to poor diet quality.
Introduction
Low-income individuals and families face a number of challenges to acquiring enough nutritious foods for a healthy and active life. High costs for nutritious foods are hypothesized as the most compelling challenge to acquiring high diet quality. For example, a report published by the U.S. Department of Agriculture (USDA) examined how the purchase of fruits and vegetables varied across income levels. It was reported that monthly food spending on fruits and vegetables was about $53 for income categories ranging from $10,000-$14,000 to $50,000-$69,999.1 Not until family incomes increased beyond $70,000 was there a significant increase in spending on fruits and vegetables to $76 per month, suggesting a threshold effect. At this higher income level; however, spending on other foods, including calorically dense foods, also increased.
A review of the literature linking SES and diet quality by Darmon and Drewnowski2 makes a case of not only a causal relationship but of a positive dose-response relationship between higher levels of SES linked to improved diet quality. The authors posit two primary reasons for the strong, monotonic relationship between income and diet quality.2 The first is the higher cost in both food price and time to acquire and prepare food; which was highlighted in the IOM report, Supplemental Nutrition Assistance Program: Examining the Evidence to Define Benefit Adequacy.3 The second is the limited access to nutritious foods because of limited availability of grocery stores in low-income neighborhoods.2,4 Both of these mechanisms have been challenged. Using longitudinal data, economists have found that the income differences are weak when other factors are included, namely education and nutrition knowledge.5 Recent studies that focus on the food environment and dietary intake have been inconsistent for adults6 and find moderately strong relationship for children,7 and have highlighted the wide variation in measurement of the food environment. Food price alone does not explain poor dietary intake. Understanding barriers to the purchase and consumption of nutritious foods is important for informing a new generation of interventions targeted at improving diet quality.
The U.S. Dietary Guidelines for Americans are a set of recommendations for a healthy eating pattern associated with decreased risk for diet-related chronic diseases.8 Several studies have highlighted that the majority of Americans eat poorly.9–12 For example, on a given day, only 2% of Americans reported meeting the recommendation for whole grains, 12.5% for fruits, and 13% for vegetables. Thus, suggesting that most Americans, regardless of income, eat poorly.13 A number of cross-sectional and longitudinal analyses have found very modest income inequalities and social disparities in dietary intake,14–16 and at least one study did not find income differences.17 Although reasons for consuming a poor diet may differ between upper- and lower-income Americans, at all income levels, diet quality is much lower than what might indicate a healthy diet quality. Over the life course, a persistent poor-quality diet compounded by stress can adversely impact future dietary intake, eating behaviors, and health outcomes.18
Further compounding economic constraints of acquiring a nutritious diet are the accompanying psychological and biobehavioral factors experienced by low-income individuals and households. The biobehavioral theory of health suggests a complex interplay between social and environmental exposures and human biological responses, which change and shape behavior.19 Stress and emotional responses to poverty and environmental uncertainties such as employment, food, and housing insecurities are regulated by the nervous, endocrine, and immune systems, and can influence health behaviors that play an important role in food choice, consumption, and diet-related chronic disease processes.18–20
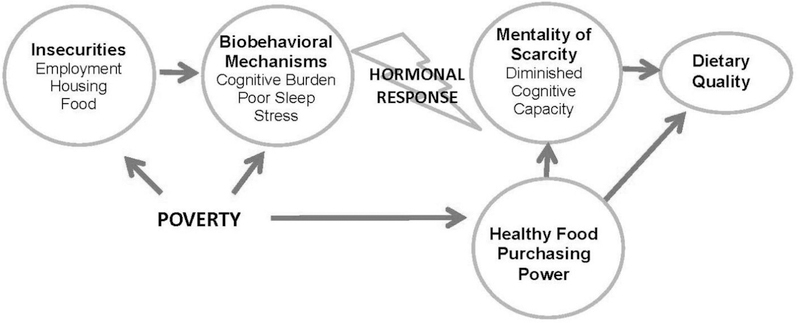
This narrative review discusses several examples of diet-related psychological and biobehavioral challenges that low-income households may face in addition to economic constraints. Living in poverty, especially extreme poverty, may have direct effects on stress, sleep, and one’s cognitive capacity. However, the authors posit that uncertainty and threat to one’s well-being associated with employment, food, and housing insecurities are the main mechanisms of how poverty triggers elevated levels of stress, poor sleep, and cognitive burden (Figure 1). Under conditions of uncertainty and threat, a biological response is mounted activating stress-, appetite-, and hunger-regulating hormones that signal the hypothalamus and shape eating behaviors.21 Together, these contribute to a mentality of scarcity,22 defined as the diminished cognitive capacity to manage challenges, which when combined with decreased purchasing power for healthy food, adversely affects dietary quality.
Figure 1.
Conceptual Framework: how poverty creates environment of scarcity leading to poor dietary quality.
Approach and Findings
The authors identified a set of socioenvironmental inputs for which low-income individuals are at risk—employment, food, and housing insecurity—as well as biobehavioral responses of poor sleep, stress, and cognitive burden, which have all been found to influence dietary intake. This paper reviews the literature focusing only on research studies that assessed the relationship between a source of uncertainty or biobehavioral response and dietary intake among low-income populations. Academic journal articles were prioritized if they:
had a population-based focus;
assessed associations among low-income individuals or households; or
were based on a low-income sample.
Evidence of the Relationship Between Employment Insecurity and Diet
Job insecurity is defined as a “psychosocial stressor at the job level, caused by employment conditions and work organization, and reflecting a worker’s perceptions of fear of job loss or instability.”23 Job insecurity is perhaps most tangibly measured by how “precarious” one’s employment conditions are; assessed with a scale to measure precariousness evaluating temporariness, disempowerment, vulnerability, wages, rights to benefits, and ability to exercise rights.24 There is a preponderance of evidence from studies in the U.S., as well as countries around the world, suggesting that lower SES is linked with greater job insecurity.23 The demands and psychosocial stress associated with insecure employment can have a deleterious effect not only on an individual’s diet, but on the diet of the family as well. One qualitative study with low-wage employed parents described sacrifices and food choice coping strategies that were made in the household, and the researchers described a framework of “spill-over” between work and family.25 This study describes parental behaviors of “food choice coping” to manage stress, by offering “quick meals” (e.g., macaroni and cheese, hot dogs) and using food as a treat to deal with stress. Despite multiple job stressors and lack of control, parents were reluctant to leave undesirable jobs because of their need for the income, low though it might be, and because of their hopes that these suboptimal jobs might lead to more permanent opportunities in the future. One mother described these pressures as follows: “Every day’s pressure, it just wears and tears on you, and a lot of times you do take it home…cause you’re so tired, you can’t do as much with your kids as you should…with me being a single mom, my kids are relying on me, and I’m relying on my job.”25 page 2,596
Individuals in low-income jobs that are insecure not only have greater difficulty feeding their families an optimal diet because of limited finances, but also because of limited capacity due to disproportionate job insecurity.
The relationship between employment and diet among the poor extends beyond the lower ability to purchase healthy food because of lower wages; work organization can influence eating patterns as well. Characteristics such as the length of one’s workweek or the patterns of the hours that they work (e.g., “night shifts”) are referred to as “work organization” factors.26 Though educated, white-collar professionals tend to be working longer, regular hours in a week,27 less educated workers are more likely to have irregular work hours and less flexibility with their work schedules.26,28 A higher percentage of low-income individuals are employed in jobs with irregular schedules, and the lowest-income earners have the most irregular work hours.29 Because of an evolving “24/7” economy, two fifths of Americans work during nights, weekends, or on rotating shifts outside of a standard 9am to 5pm workday, and this burden is disproportionately borne by the working poor, who more typically have these less desirable jobs.30 A review of 21 studies regarding dietary intake among shift workers suggests that though overall total energy intake over 24 hours does not vary between day and shift workers, eating frequency, quality of the dietary intake, and energy distribution over the day is very different.31 Furthermore, shift workers appear to have a higher consumption of refined carbohydrates and animal fat and protein than non-shift workers, and have higher risk for metabolic disorders such as cardiovascular disease and diabetes.31 There are a variety of explanations to describe the lower diet quality of shift workers, including the mismatch between socially determined meal schedules of worker’s friends and families and their own work-determined schedule, less optimal metabolism and digestion during the night when one is biologically “programmed” to be asleep, and availability of cheap, tasty, and energy-dense foods around the clock (e.g., in a vending machine).31
Evidence of the Relationship Between Housing Insecurity and Diet
Housing insecurity, also known as housing instability, has been variably defined as occurring when there are high housing costs in proportion to income, poor housing quality (including problems with electricity and heat), unstable neighborhoods, overcrowding, or homelessness,32 and also when a household makes frequent (e.g., more than two) moves in a year.33 According to respondents in the National Survey of American Families, in 2002, an estimated 23.6% of Americans experienced difficulty paying rent.34 Low-income families are more likely to be homeless, live in single room occupancy hotels, live with crowded conditions, and have unstable housing.35 In 2014, more than 578,000 individuals were homeless.36 Since the economic recession, added financial pressures have led many families to make alternative domestic arrangements to make ends meet, and the prevalence of “doubled-up households,” defined as households including “an adult who is not the householder, spouse, or cohabitating partner of the household” increased from 22.4% in 2008 to 24.1% in 2010.37 These “extra” individuals in the household can be family members (e.g., adult child moving in with parents) and non-family adults living in alternative arrangements, with or without financial compensation.
Housing insecurity among low-income individuals poses unique challenges to acquiring, storing, and preparing nutritious food for the family that are above and beyond the obvious challenge because of limited finances to pay for food. In comparison to families from high-SES backgrounds, low-income families may face unique challenges to preparing meals for all members of their household.38 At the extreme end of household challenges that limit the ability to store and prepare foods, 4.4% of households in the U.S. lack a fully functioning kitchen.39 However, for households that are doubled up, there is an extra demand on the capacity for food storage and preparation. The refrigerator needs to hold food for different households, and the use of the stove needs to be negotiated by two households who may not actually share meals together. Though there are theoretic advantages that can arise from pooled resources and social support, there are health consequences to consider for vulnerable families living in doubled-up arrangements.40 One study of families who had been previously been living doubled up showed that though they were usually able to use the kitchen in the household that took them in, negotiating this use was often difficult and uncomfortable.41
Evidence of the Relationship Between Food Insecurity and Diet
Food insecurity, as defined by the U.S. Department of Agriculture, is the limited or uncertain ability to acquire enough food for an active and healthy life. During 2014, more than 48 million Americans lived in a household that experienced food insecurity.42 Inherent to household food insecurity is the association with anxiety, depression, and stress.43–45 Research on the influence of household food insecurity on mental health, such as maternal depression, suggests that the relationship is bidirectional and that interventions need to address nutrition, food security, and mental health in order to break recursive events.46,47
Food insecurity-induced stress is hypothesized to influence food choice and dietary pattern by activating stress hormones and neuropeptides that favor highly palatable foods.48 Indeed, food insecurity is associated with lower diet quality,49 a lower intake of nutritious foods, and a greater dependence on energy-dense but nutrient-poor foods.50 Food insecurity is also associated with dietary restraint, measured by a scale that captures dieting followed by disinhibited eating or a susceptibility to overeating51 and disordered eating measured by the Eating Attitudes Test.52
Not only is food insecurity associated with higher prevalence of diet-related chronic conditions such as diabetes53,54 and gestational diabetes,55 food insecurity is also associated with poor management of these conditions.56,57 The relationship among food insecurity, stress, and diet-related chronic disease has been characterized as a cyclic and bidirectional process whereby food insecurity and stress can lead to the development of chronic conditions. Chronic conditions, such as diabetes, then exacerbate resource constraints by adding healthcare costs, necessitating a greater need for nutritious foods, and perpetuating food insecurity.58
Evidence of a Relationship Between Stress and Diet
Stress that causes a threat to one’s well-being, compared with stress that presents a surmountable challenge, activates the hypothalamic-pituitary-adrenal axis, often causing a preference for highly palatable foods to dampen the stress response and the increased stress-related hormones shifting metabolism to favor storage of excess calories as central fat.48,59 The American Psychological Association national survey of stress in the U.S. has been an annual poll since 2007.60 The 2014 survey reported that U.S. stress score was 4.9 on a 10-point Likert scale where 1 is little or no stress and 10 is a great deal of stress. Stress scores were higher among women (5.2) than men (4.5) and among individuals in low-income (<$50,000 per year) households (5.2). The leading reason for stress was financial (64%), followed by work-related issues (60%), family responsibilities (47%), and health concerns (46%). The survey asked about eating as a response to stress. More low-income individuals with money concerns (38%) compared with low-income people without money concerns (15%) reported eating too much or eating unhealthy foods because of stress. A recent review study found that upper-income individuals were more likely to have lower stress levels, healthier eating patterns, and lower body weight.61 The opposite was found for lower-income individuals who had higher levels of stress, and who were more likely to have less-healthy dietary behaviors and higher body weight. The findings were more consistent among women than men. The nature of the relationships among level of stress, eating behaviors, and metabolism are multifactorial.61 In a study of 101 women who participated in the Special Supplemental Nutrition Assistance Program for Women, Infants, and Children, perceived stress was assessed with regard to diet quality, eating behaviors, and weight status. An analysis using structural equation modeling showed that higher levels of perceived stress had a direct association with uncontrolled eating, emotional eating, and severe obesity.62 In a larger sample of postpartum women who participated in the program (N=711), anxiety, depression, and perceived stress were strongly associated with emotional eating; depression was associated with dietary restraint.63 Furthermore, stressful events were linked to emotional eating in qualitative study of low-income overweight/obese mothers.64 The consistency of findings in these studies suggests that interventions aimed at improving dietary intake should consider stress and eating behaviors.
Evidence of a Relationship Between Poor Sleep and Diet
More recently, there has been increased interest in understanding the relationship between sleep quality and diet. A short period of decreased sleep duration resulted in signs of impaired glucose tolerance, decreased insulin response, and increased cortisol response, which Spiegel et al.65 concluded demonstrate the harmful impact of short sleep on carbohydrate metabolism and endocrine function through alterations of the hypothalamic-pituitary-adrenal axis. Two important appetite-regulating hormones—leptin and ghrelin—are influenced by sleep duration and are hypothesized to play a direct role in weight gain. Leptin, created in fat (adipose) tissue, signals to the brain to suppress appetite whereas ghrelin, which is created in the stomach, signals to increase appetite. Both leptin and ghrelin travel through blood, cross the blood-brain barrier, and activate the hypothalamus. Shorter sleep duration has been associated with higher BMI levels, and also lower levels of leptin and higher levels of ghrelin, which cause hunger, increased appetite, and potentially increased caloric consumption.66
Low-income individuals disproportionately experience poor sleep duration and face higher levels of stress, which influences food choice and eating behaviors. According to the National Sleep Foundation, adults aged 26–64 years should sleep 7–9 hours/day for optimal health.67 Between 2007 and 2010, 37.3% of U.S. adults reported sleeping on average ≤6 hours.68 Economic and ethnic disparities in sleep exist, such that low-income populations are at increased risk of poor sleep quality in comparison with those from higher-SES backgrounds.69–71 For instance, a cross-sectional analysis of national survey data suggests that after adjusting for age and education, individuals earning <$20,000 annually are more likely to get ≤5 hours of sleep compared with individuals who earn >$75,000 per year.70 Furthermore, discrimination has been associated with poor sleep among African Americans.72,73
Poor sleep has been hypothesized to lead to non-homeostatic eating (eating in the absence of hunger) by being more likely to eat when stimulated by sight or smell of food, and by being more likely to eat in response to negative emotions; this especially occurs with children and women.74,75 A review of epidemiologic studies suggests a positive correlation between short sleep duration (<6 hours) and higher total energy intake, higher fat intake (e.g., total fat and saturated fats), as well as lower fruit and vegetable intake; this is especially concerning given the fact that individuals with lower SES are more likely to have less sleep.76 In addition to macronutrients and particular food types, short sleep duration is also shown to be negatively correlated with eating breakfast and dinner meals, based on an analysis of cross-sectional dietary recall data from the 2005–2010 National Health Examination and Nutrition Examination Survey (NHANES).77 Other measures of sleep quality, such as sleep latency (i.e., length of time to fall asleep) and sleep disruptions (i.e., waking in the middle of the night), are associated with poor diet quality.78 Furthermore, food insecurity is associated with poor sleep quality70,79 and sleep latency.69 According to a cross-sectional analysis of data collected from the 2005–2010 NHANES, women (aged ≥22 years) who experienced very low food security had a shorter duration of sleep than women living with full food security. The study also found that men living with very low food security, low food security, and marginal food security took longer to fall asleep than men who were fully food secure.79
Evidence of a Relationship Between a Mentality of Scarcity and Diet
Mullainathan and Shafir22 describe scarcity as “…more than just the displeasure of having very little. It changes how we think. It imposes itself on our minds.” This mentality of scarcity leads to a depletion of cognitive resources, which diminishes the reasoning center in the prefrontal cortex disrupting food regulation21 and reduces impulse control.80 There have been a number of studies linking a depletion of cognitive resources with preferences of unhealthy foods. In the classic experiment by Shiv and Fedorikhin,81 college students were asked to memorize a seven-digit number or a two-digit number, walk into another room, and choose between a piece of chocolate cake or a serving of fruit salad. Students who memorized the seven-digit number were significantly more likely to choose the chocolate cake than students who memorized the two-digit number. Variations of this experiment have produced similar results, suggesting that impulsive eating and irrational food choices can result when cognitive resources are depleted.82–84
In the presence of poverty, the mentality of scarcity is compounded.85 Low-income individuals are more likely to face uncertainties of many necessities (e.g., housing, food, employment), each of which requires sufficient cognitive resources to manage. Furthermore, it has been well established that energy-dense, processed foods are heavily marketed and widely available in low-income neighborhoods.86,87 Combining the depletion of cognitive resources with marketing of unhealthy foods has been shown to exert an interactive effect on dietary intake. In an experimental study, 351 college students were randomly assigned to four groups:
high cognitive load and food advertising;
low cognitive load and food advertising;
high cognitive load and non-food advertising; and
low cognitive load and non-food advertising.88
The participants were then allowed to eat ad libitum from an array of healthy and unhealthy snacks. Results showed that exposure to food advertising resulted in a 43% increase in unhealthy snacks consumed among students in the high cognitive load group; no effect was observed in the low cognitive load group. Resource scarcity experienced during early life is hypothesized to result in responding to a scarce resource environment as an adult by being more impulsive, taking risks, and responding to temptations. These behaviors can put individuals and households at risk of being focused on decisions based on present need (e.g., cheap, highly caloric, nutrient-poor food) and immediate gratification (e.g., cheap, highly palatable, high-fat, high-sugar food). Short-term decisions that favor high-calorie foods in the presence of uncertainty may be very rational, although not oriented to consequences of future health and well-being.80
Thus, high levels of uncertainties, in the context of the low-income food environment, may inhibit healthy food choices among low-income individuals, even in the presence of healthy food. Combined with the influence of chronic, psychological stress and poor sleep on metabolic health,59 this mentality of scarcity can greatly affect one’s dietary intake and diet quality, contributing to increased risks of chronic conditions over the life course for low-income children and adults.18,19
Discussion
Darmon and Drewnowski2,4 make a case for a causal relationship between income and diet quality; however, several studies refute this link as a number of socioeconomic, health, and biobehavioral factors are also associated in shaping eating behavior and diet quality.5,21 Although the relationship between SES and diet quality may be partially explained by the high cost of nutritious foods and potential inaccessibility of fresh whole foods in some neighborhoods, there are other compelling factors that compound economic constraints and influence food choice among low-income individuals and households. Chief among these factors are the burdens of uncertainty with employment, housing, and food. These uncertainties can threaten one’s well-being and livelihood, lead to an overwhelming psychological and cognitive burden, influence biobehavioral pathways (e.g., psychological distress, short sleep duration), and create a mentality of scarcity that predisposes one to poor diet quality and subsequently cardiometabolic diseases.18,89,90 Therefore, increasing income alone will not necessarily lead to improved diet quality.
Using the proposed conceptual framework, a focus on employment opportunities, housing stability, and food security will assist families with procuring and consuming a nutritious diet in at least three ways. First, stable income, housing, and food will assist individuals by having more purchasing power to be able to afford nutritious foods. Second, stability will decrease stress and improve sleep, which in turn will improve dietary behaviors and diet quality. Third, stability may help to decrease cognitive burden of navigating a poor food environment and lead to improved diet quality.
Future policy and population-level interventions need to be more comprehensive and have a systems-level approach to addressing poverty-related barriers to health eating, which includes providing secure safety-net programs that address employment, housing, and food security as well as providing resources to address mental health.
Conclusions
Low-income individuals and households experience unique challenges to healthy eating and the current review confirms the need for interventions that acknowledge the multiple ways in which poverty influences dietary behaviors. Although cost of food is often cited as a major barrier to purchasing and consuming nutritious foods, this review provides a unique lens to understand how poverty, when exacerbated by uncertainty (i.e., food, employment, and housing insecurities), might trigger a biobehavioral response that alters neuroendocrine function and carbohydrate metabolism, which then leads to poor diet quality. The conceptual framework in this review could be used to inform the design of future interventions that aim to improve eating behaviors among low-income populations.
Acknowledgments
This paper was supported by the University of California Office of the President (UCOP) Multiple-Campus Research Initiative, Stress, Environment and Weight, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development funded study, “Race, stress and dysregulated eating: Maternal to child transmission of obesity” (Principal Investigator, Barbara Laraia, R01HD073568) and by grants 1K99HD84758 (Leung) and 1K23HD075852 (Tester) from NIH. The paper is also supported by funders of article publication, the Physicians Committee for Responsible Medicine.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Frazao E, Smallwood D, Prell M. Food spending patterns of low-income households will increasing purchasing power result in healthier food choices? In: U.S. Department of Agriculture. Economic Information Bulletin. Vol 29. Washington, DC: Economic Research Services; 2007:7. [Google Scholar]
- 2.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. 2008;87(5):1107–1117. [DOI] [PubMed] [Google Scholar]
- 3.Committee on the Examination of the Adequacy of Food Resources and SNAP Allotments, Food and Nutrition Board, Institute of Medicine. Caswell JA, Yaktine AL, eds. Supplemental Nutrition Assistance Program: Examining the Evidence to Define Benefit Adequacy. Washington, D.C.: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 4.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–660. 10.1093/nutrit/nuv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Variyam JN, Blaylock J, Smallwood D. USDA’s Healthy Eating Index and Nutrition Information. Washington, D.C.: USDA; April 1998. No. 1866. [Google Scholar]
- 6.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: A systematic review. Health Place. 2012;18(5):1172–1187. 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engler-Stringer R, Le H, Gerrard A, Muhajarine N. The community and consumer food environment and children’s diet: A systematic review. BMC Public Health. 2014;14:522. 10.1186/1471-2458-14-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.2015–2020 Dietary Guidelines for Americans. U.S. Department of Agriculture, U.S. Department of Health. 8th Ed. Washington, D.C. 2015:144. [Google Scholar]
- 9.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010;140(10):1832–1838. 10.3945/jn.110.124826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rehm CD, Penalvo JL, Afshin A, Mozaffarian D. Dietary Intake Among U.S. Adults, 1999–2012. JAMA 2016;315(23):2542–2553. 10.1001/jama.2016.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to U.S. Dietary Guidelines for children and adolescents in the National Health and Nutrition Examination Survey Population. J Acad Nutr Diet. 2016;116(1):21–27. 10.1016/j.jand.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guenther PM, Kirkpatrick SI, Reedy J, et al. Diet quality of Americans in 2001–02 and 2007–08 as measured by the Healthy Eating Index-2010. Washington, DC: U.S. Department of Agriculture; 2013. [Google Scholar]
- 13.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among U.S. adults and children. J Acad Nutr Diet. 2012;112(5):624–635. 10.1016/j.jand.2011.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI- 2010. J Acad Nutr Diet. 2013;113(4):569–580. http://dx.doi.Org/10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23(4):839–862. 10.1016/j.jhealeco.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Wang DD, Leung CW, Li Y, et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587–1595. 10.1001/jamainternmed.2014.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113(2):297–306. 10.1016/j.jand.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 18.Hemmingsson E A new model of the role of psychological and emotional distress in promoting obesity: Conceptual review with implications for treatment and prevention. Obesity Rev. 2014;15(9):769–779. 10.1111/obr.12197. [DOI] [PubMed] [Google Scholar]
- 19.Committee on Health and Behavior: Research, Practice and Policy;.Board on Neuroscience and Behavioral Health; Institutes of Medicine. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 20.Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress. Does stress account for SES effects on health? Ann N Y Acad Sci. 1999;896:131–144. 10.1111/j.1749-6632.1999.tb08111.x. [DOI] [PubMed] [Google Scholar]
- 21.Alonso-Alonso M, Pascual-Leone A. The right brain hypothesis for obesity. JAMA 2007;297(16):1819–1822. 10.1001/jama.297.16.1819. [DOI] [PubMed] [Google Scholar]
- 22.Mullainathan S, Shafir E. Scarcity: Why having too little means so much. First edition. Time Books, Henry Holt & Company, LLC, New York, NY; 2013. [Google Scholar]
- 23.Landsbergis PA, Grzywacz JG, LaMontagne AD. Work organization, job insecurity, and occupational health disparities. Am J Ind Med. 2014;57(5):495–515. 10.1002/ajim.22126. [DOI] [PubMed] [Google Scholar]
- 24.Vives A, Amable M, Ferrer M, et al. The Employment Precariousness Scale (EPRES): psychometric properties of a new tool for epidemiological studies among waged and salaried workers. Occup Env Med. 2010;67(8):548–555. 10.1136/oem.2009.048967. [DOI] [PubMed] [Google Scholar]
- 25.Devine CM, Jastran M, Jabs J, Wethington E, Farell TJ, Bisogni CA. “A lot of sacrifices”: Work-family spillover and the food choice coping strategies of low-wage employed parents. Soc Sci Med. 2006;63(10):2591–2603. 10.1016/j.socscimed.2006.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson JV, Lipscomb J. Long working hours, occupational health and the changing nature of work organization. Am J Ind Med. 2006;49(11):921–929. 10.1002/ajim.20383. [DOI] [PubMed] [Google Scholar]
- 27.Grosch JW, Caruso CC, Rosa RR, Sauter SL. Long hours of work in the U.S.: associations with demographic and organizational characteristics, psychosocial working conditions, and health. Am J Ind Med. 2006;49(11):943–952. 10.1002/ajim.20388. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs JA, Gerson K. The time divide: work, family, and gender inequality. Cambridge, MA: Harvard University Press; 2004. [Google Scholar]
- 29.Golden L Irregular work scheduling and its consequences. Washington, DC: Economic Policy Institute; April 9, 2015. [Google Scholar]
- 30.Presser HB. Working in a 24/7 economy: challenges for American families. New York: Russell Sage Foundation; 2003. [Google Scholar]
- 31.Lowden A, Moreno C, Holmback U, Lennernas M, Tucker P. Eating and shift work - effects on habits, metabolism and performance. Scand J Work Environ Health. 2010;36(2):150–162. 10.5271/sjweh.2898. [DOI] [PubMed] [Google Scholar]
- 32.Johnson A, Meckstroth A. Ancillary services to support welfare to work. Washington, D C.: U S. DHHS; June 22, 1998. [Google Scholar]
- 33.Cutts DB, Meyers AF, Black MM, et al. U.S. Housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–1514. 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kushel M, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care: Results from the national survey of American families. J Gen Int Med. 2005;20:116–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mundra K, Sharma A. Housing adequacy gap for minorities and immigrants in the U.S.: Evidence from the 2009 American Housing Survey. J Housing Res. 2015;24(1):18. [Google Scholar]
- 36.NAEH. The State of Homelessness in America. An examination of trends in homelessness, homelessness assistance, and at-risk populations at the national and state levels. Washington, D.C.: National Alliance to End Homelessness, 2015. [Google Scholar]
- 37.Mykyta L The effects of recession on household composition:“doubling up” and economic well-being: U.S. Census Bureau; 2011. [Google Scholar]
- 38.Appelhans BM, Waring ME, Schneider KL, Pagoto SL. Food preparation supplies predict children’s family meal and home-prepared dinner consumption in low-income households. Appetite. 2014;76:1–8. 10.1016/j.appet.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 39.U.S. Census Bureau. American Housing Survey for the United States: 2011. Washington, D C.; 2013. [Google Scholar]
- 40.Ahrentzen S Double indemnity or double delight? The health consequences of shared housing and “doubling up”. J Soc Issues. 2003;59(3):547–568. 10.1111/1540-4560.00077. [DOI] [Google Scholar]
- 41.Dehavenon AL. In: Dehavenon AL, ed. There’s no place like home: Anthropological perspectives on housing and homelessness in the United States. Westport, CT.: Bergen & Garvey; 1996:51–66. [Google Scholar]
- 42.Coleman-Jensen A, Rabbitt MP, Gregory C, Singh A. Household Food Security in the United States in 2014. U.S. Department of Agriculture. Vol ERR-194. Washington, DC: Economic Research Service; 2015. [Google Scholar]
- 43.Casey P, Goolsby S, Berkowitz C, et al. Maternal depression, changing public assistance, food security, and child health status. Pediatrics. 2004;113(2):298–304. 10.1542/peds.113.2.298. [DOI] [PubMed] [Google Scholar]
- 44.Black MM, Quigg AM, Cook J, et al. WIC participation and attenuation of stress-related child health risks of household food insecurity and caregiver depressive symptoms. Arch Pediatr Adolesc Med. 2012;166(5):444–451. 10.1001/archpediatrics.2012.1. [DOI] [PubMed] [Google Scholar]
- 45.Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006;136(1):177–182. [DOI] [PubMed] [Google Scholar]
- 46.Huddleston-Casas C, Charnigo R, Simmons LA. Food insecurity and maternal depression in rural, low-income families: A longitudinal investigation. Pub Health Nutr. 2009;12(8):1133–1140. 10.1017/S1368980008003650. [DOI] [PubMed] [Google Scholar]
- 47.Whitaker RC, Phillips SM, Orzol SM. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–868. 10.1542/peds.2006-0239. [DOI] [PubMed] [Google Scholar]
- 48.Laraia BA. Food Insecurity and Chronic Disease. Adv Nutr. 2013;4(2):203–212. 10.3945/an.112.003277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114(12):1943–1953. 10.1016/j.jand.2014.06.353. [DOI] [PubMed] [Google Scholar]
- 50.Widome R, Neumark-Sztainer D, Hannan PJ, Haines J, Story M. Eating when there is not enough to eat: eating behaviors and perceptions of food among food-insecure youths. Am J Pub Health. 2009;99(5):822–828. 10.2105/AJPH.2008.139758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Laraia B, Epel E, Siega-Riz AM. Food insecurity with past experience of restrained eating is a recipe for increased gestational weight gain. Appetite. 2013;65:178–184. 10.1016/j.appet.2013.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Laraia B, Vinikoor-Imler LC, Siega-Riz AM. Food insecurity during pregnancy leads to stress, disordered eating, and greater postpartum weight among overweight women. Obesity. 2015;23(6):1303–1311. 10.1002/oby.21075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Int Med. 2007;22(7):1018–1023. 10.1007/s11606-007-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–310. 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Laraia BA, Siega-Riz AM, Gundersen C. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain, and pregnancy complications. J Am Diet Assoc. 2010;110(5):692–701. 10.1016/j.jada.2010.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Seligman HK, Jacobs EA, Lopez A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233–238. 10.2337/dc11-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Eng J Med. 2010;363(1):6–9. 10.1056/NEJMp1000072. [DOI] [PubMed] [Google Scholar]
- 59.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–458. 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 60.Stress in America: Paying with our health. Washington, DC: American Psychological Association; 2015. [Google Scholar]
- 61.Moore CJ, Cunningham SA. Social position, psychological stress, and obesity: a systematic review. J Acad Nutr Diet. 2012;112(4):518–526. 10.1016/j.jand.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 62.Richardson AS, Arsenault JE, Cates SC, Muth MK. Perceived stress, unhealthy eating behaviors, and severe obesity in low-income women. Nutr J. 2015;14:122. 10.1186/s12937-015-0110-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Emerson JA, Hurley KM, Caulfield LE, Black MM. Maternal mental health symptoms are positively related to emotional and restrained eating attitudes in a statewide sample of mothers participating in a supplemental nutrition program for women, infants and young children. Mater Child Nutr. In press. Online February 22, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chang MW, Nitzke S, Guilford E, Adair CH, Hazard DL. Motivators and barriers to healthful eating and physical activity among low-income overweight and obese mothers. J Am Diet Assoc. 2008;108(6):1023–1028. 10.1016/j.jada.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 65.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435–1439. 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 66.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62. 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hirshkowitz MWK, Albert SM, Alessi C, Bruni O, DonCarlos L, Neubauer DN. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 2015;1(1):4. 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 68.Frenk SM, Chong YN. Sleep Duration* Among Adults Aged >=20 Years, by Race/Ethnicity-National Health and Nutrition Examination Survey, United States, 2007–2010. MMWR Morbid Mortal Wkly Rep. 2013;62(36):755–755. [Google Scholar]
- 69.Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9(9):897–905. 10.5664/jcsm.2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Patel NP, Grandner MA, et al. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Pub Health. 2010;10:475. 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Van Dyke ME, Vaccarino V, Quyyumi AA, Lewis TT. Socioeconomic status discrimination is associated with poor sleep in African-Americans, but not Whites. Soc Sci Med. 2016;153:141–147. 10.1016/j.socscimed.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012;10(4):235–249. 10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Burt J, Dube L, Thibault L, Gruber R. Sleep and eating in childhood: a potential behavioral mechanism underlying the relationship between poor sleep and obesity. Sleep Med. 2014;15(1):71–75. 10.1016/j.sleep.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 75.Dweck JS, Jenkins SM, Nolan LJ. The role of emotional eating and stress in the influence of short sleep on food consumption. Appetite. 2014;72:106–113. 10.1016/j.appet.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 76.Dashti HS, Scheer FA, Jacques PF, Lamon-Fava S, Ordovas JM. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv Nutr. 2015;6(6):648–659. 10.3945/an.115.008623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kant AK, Graubard BI. Association of self-reported sleep duration with eating behaviors of American adults: NHANES 2005–2010. Am J Clin Nutr. 2014;100(3):938–947. 10.3945/ajcn.114.085191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Crispim CA, Zimberg IZ, dos Reis BG, Diniz RM, Tufik S, de Mello MT. Relationship between food intake and sleep pattern in healthy individuals. J Clin Sleep Med. 2011;7(6):659–664. 10.5664/jcsm.1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ding M, Keiley MK, Garza KB, Duffy PA, Zizza CA. Food insecurity is associated with poor sleep outcomes among U.S. adults. J Nutr. 2015;145(3):615–621. 10.3945/jn.114.199919. [DOI] [PubMed] [Google Scholar]
- 80.Kidd C, Palmeri H, Aslin RN. Rational snacking: young children’s decision-making on the marshmallow task is moderated by beliefs about environmental reliability. Cognition. 2013;126(1):109–114. 10.1016/j.cognition.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shiv B, Fedorikhin A. Heart and mind in conflict: The interplay of affect and cognition in consumer decision making. J Consum Res. 1999;26(3):278–292. 10.1086/209563. [DOI] [Google Scholar]
- 82.Lattimore P, Maxwell L. Cognitive load, stress, and disinhibited eating. Eating Behav. 2004;5(4):315–324. 10.1016/j.eatbeh.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 83.Ward A, Mann T. Don’t mind if I do: Disinhibited eating under cognitive load. J Pers Soc Psychol. 2000;78(4):753–763. 10.1037/0022-3514.78.4.753. [DOI] [PubMed] [Google Scholar]
- 84.Friese M, Hofmann W, Wanke M. When impulses take over: moderated predictive validity of explicit and implicit attitude measures in predicting food choice and consumption behaviour. Br J Soc Psychol. 2008;47(Pt 3):397–419. 10.1348/014466607X241540. [DOI] [PubMed] [Google Scholar]
- 85.Spears D Economic decision-making in poverty depletes cognitive control. 2010:38, Princeton, NJ. [Google Scholar]
- 86.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44(3):189–195. 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 87.Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–29. 10.1016/S0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 88.Zimmerman FJ, Shimoga SV. The effects of food advertising and cognitive load on food choices. BMC Pub Health. 2014;14:342. 10.1186/1471-2458-14-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shah AK, Mullainathan S, Shafir E. Some consequences of having too little. Science. 2012;338(6107):682–685. 10.1126/science.1222426. [DOI] [PubMed] [Google Scholar]
- 90.Griskevicius V, Ackerman JM, Cantu SM, et al. When the economy falters, do people spend or save? Responses to resource scarcity depend on childhood environments. Psychol Sci. 2013;24(2): 197–205. 10.1177/0956797612451471. [DOI] [PubMed] [Google Scholar]