Key Clinical Message
We present a case of chemotherapy‐induced hiccups that were alleviated by steroid rotation. Hiccups are often overlooked, but they have an impact on the patient's quality of life. In the COVID‐19 era, web‐based teleworking has become an important tool, hiccups during a teleconference should be noted as a concern for patients.
Keywords: colorectal cancer, dexamethasone, hiccups, prednisolone, steroid rotation, teleworking
Dexamethasone to prednisolone rotation relieved hiccups in colorectal cancer patient during anticancer therapy.
1. INTRODUCTION
Hiccups induced by anticancer therapy occur in approximately 16%–25% of patients receiving chemotherapy. 1 , 2 , 3 Most cases improve within 7 days, 4 but some last longer, significantly decreasing the patient's quality of life (QOL). It is not uncommon for patients to continue working in a web‐based fashion during cancer treatment, especially in the COVID‐19 era. In this case report, we present our experience with a cancer patient undergoing web‐based telework who developed hiccups associated with chemotherapy. The hiccups were well controlled by switching from dexamethasone to prednisolone as an antiemetic regimen. We obtained written informed consent for publication of this case report.
2. CASE HISTORY
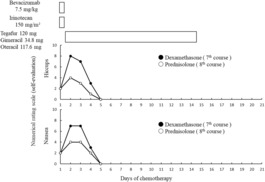
A 49‐year‐old man (weight: 103.9 kg, height: 167.5 cm, body surface area: 2.119 m2) with hypertension was undergoing chemotherapy (7.5 mg/kg bevacizumab and 150 mg/m2 irinotecan on day 1 and combined capsule of 120 mg tegafur/34.8 mg gimeracil/117.6 mg oteracil on days 1–14 of a 21‐day cycle) after surgery for transverse colon cancer with lung metastasis as a second‐line anticancer therapy. 5 Palonosetron and dexamethasone were adopted for chemotherapy‐induced nausea and vomiting (CINV); the patient received an injection of 0.75 mg/day palonosetron and 9.9 mg/day dexamethasone on Day 1 and orally 8 mg/day dexamethasone on Days 2–4 during chemotherapy. 6 At the 7th course of chemotherapy, he complained of severe hiccups during an online meeting for his work, with one hiccup per word during the meeting. Therefore, we started 25 mg chlorpromazine and 2.5 g shakuyakukanzoto as needed for 21 days; however, his hiccups did not improve. To retain his ability to work and his QOL, at the 8th course, we changed the 8 mg dexamethasone to 60 mg prednisolone for 2 days, according to the literature by Kang et al. 7 after obtained informed consent from him as advanced choice considering his QOL. When the patient was receiving dexamethasone, the severity of hiccups and nausea peaked on Day 2 at grades 8 and 7, respectively (0: no symptoms to 10: severe) (Figure 1). However, when he was receiving prednisolone, his symptoms peaked on Day 2 at grade 4 for both hiccups and nausea. He was satisfied that he could smoothly continue his online meetings after changing to prednisolone to prevent CINV. We continued prednisolone during the 9th course of chemotherapy to ensure the patient's QOL but decreased the dose to 30 mg/day for 2 days after chemotherapy. His hiccups and nausea were well controlled at this dose. He was administered pyridoxal (60 mg/day), vonoprazan (20 mg/day), mecobalamin (1.5 mg/day), amlodipine (5 mg/day), ambroxol (45 mg/day), and magnesium oxide (990 mg/day); these were not changed throughout the treatment period.
FIGURE 1.
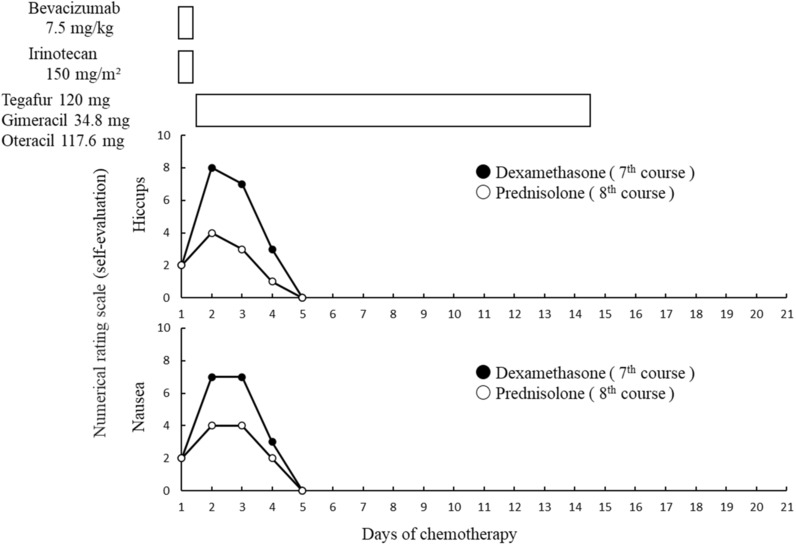
Severity of hiccups and nausea with dexamethasone and prednisolone.
3. DISCUSSION
We presented our experience with severe hiccups associated with chemotherapy that were improved by steroid rotation from dexamethasone to prednisolone for CINV. The patient's nausea was also well controlled after the change. Hiccups are known to occur in patients treated with dexamethasone. 3 In our case, some of the patient's other medicine may have caused hiccups, including irinotecan (frequency of hiccups, <5%), bevacizumab (1%–5%), and palonosetron (<1%–10%). 8 , 9 , 10 Because we did not want to reduce either the anticancer or antiemetic effects of the patient's therapy, we first tried chlorpromazine and shakuyakukanzoto. However, these drugs did not improve his hiccups; therefore, we changed dexamethasone to prednisolone at a 1:7.5 titer (dexamethasone vs. prednisolone: 8 mg vs. 60 mg). 7 , 11
The mechanism of hiccups caused by dexamethasone is reported to be the stimulation of the steroid receptors and the central part of the hiccup reflex arc and a decrease in the synaptic transmission threshold in the midbrain. Steroid receptors are highly expressed in the central part of the hiccup reflex arc. 12 , 13 Dexamethasone has been reported to be more potent than methylprednisolone in inducing hiccups, and steroids have different hiccup‐inducing effects depending on their potency. 14 Dexamethasone when administered in high doses can cross the blood–brain barrier and activate steroid receptors in the hypothalamus, 15 and dexamethasone crosses the blood–brain barrier better than prednisolone. 16 The hiccup reflex arc is also inhibited by γ‐aminobutyric acid (GABA), and GABA antagonists are thought to induce hiccups. It has been suggested that steroids may be potent GABA antagonists at the hiccup reflex arc. 17
Rotation within the same drug class is generally conducted to control adverse events or increase efficacy. 18 Although our patient's hiccups may be partially explained by the rotation in steroids, they cannot be explained solely by differences in steroid potency and blood–brain barrier passage. Further studies are needed to determine the best method for controlling hiccups in cancer patients.
4. CONCLUSION
The present case has afforded us a new perspective on hiccups, an adverse event that is often overlooked due to its seemingly benign nature, despite its negative impact on patients' QOL, particularly in the context of the COVID‐19 pandemic and the shift toward remote work for half of the working population. 19 As a matter of fact, adverse events experienced by cancer patients have been described as a “missing voice” in the literature. 20 This study contributes to the existing body of evidence highlighting the critical importance of medical staff's awareness of overlooked adverse events that can significantly impair patients' QOL.
In conclusion, COVID‐19 has drastically changed to the web‐based working style. In cancer patients, web‐based working is desirable to avoid physical burdens and decrease infection risks. However, randomly occurring hiccups are a considerable concern for those working online especially as videoconferencing becomes an important part of their life. Hiccups will become a primary concern for cancer patients continuing to work online during their treatment. Currently, steroid rotation is not intended to replace standard treatment methods. Effective and high‐quality studies are necessary to reduce hiccups in cancer patients undergoing chemotherapy.
AUTHOR CONTRIBUTIONS
Takuya Nagata: Data curation; investigation; writing – original draft. Ayako Watanabe: Conceptualization; data curation; investigation; writing – original draft. Kenji Momo: Conceptualization; methodology; project administration; supervision; validation; writing – original draft. Yuka Kashiwabara: Project administration; supervision. Misa Saeki: Data curation; investigation; validation. Yuji Oto: Methodology; validation. Takeshi Uchikura: Methodology; validation. Kouji Kobayashi: Data curation; supervision. Hirokazu Toshima: Methodology; supervision. Ken Shimada: Project administration; supervision. Katsumi Tanaka: Project administration; supervision.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The Department of Hospital Pharmaceutics, School of Pharmacy, Showa University received funds from Ono for a contract research project according to a collaborative research agreement. YO's kin is employed from Mitsubishi Tanabe Pharma. KS is a medical adviser of Ono, Taiho, and Sawai. As a potential conflict of interest, Hospital Pharmaceutics received research grants from Daiichi Sankyo, Mochida, Shionogi, Ono, Taiho, Nippon‐kayaku, and Bayer. TN received an honorarium fee for presentations from Sanofi. KM received an honorarium fee for presentations from Nippon‐Kayaku and Abbvie Inc. YK received an honorarium fee for presentations from Daiichi Sankyo. HT received an honorarium fee for presentations from Daiichi Sankyo, Taiho, Bristol‐Myers. KS received an honorarium fee for presentations from Daiichi Sankyo, Ono, Taiho, Yakult, Bristol‐Myers. KT received an honorarium for presentations at AYUMI, Daiichi Sankyo, TERUMO, Chugai, Towa, and Taisho. The other authors declare no conflict of interest associated with this manuscript.
CONSENT
We obtained written informed consent for publication from the patient.
Nagata T, Watanabe A, Momo K, et al. Dexamethasone to prednisolone rotation relieved hiccups in colorectal cancer patient continuing teleworking during anticancer therapy. Clin Case Rep. 2023;11:e7367. doi: 10.1002/ccr3.7367
DATA AVAILABILITY STATEMENT
Author elects to not share data.
REFERENCES
- 1. Wang Z, Liu W, Zhang J, et al. Antiemetic prophylaxis for chemoradiotherapy‐induced nausea and vomiting in locally advanced head and neck squamous cell carcinoma: a prospective phase II trial. Strahlenther Onkol. 2022;198:949‐957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ergen M, Arikan F, Fırat Çetin R. Hiccups in cancer patients receiving chemotherapy: a cross‐sectional study. J Pain Symptom Manage. 2021;62:e85‐e90. [DOI] [PubMed] [Google Scholar]
- 3. Vardy J, Chiew KS, Galica J, Pond GR, Tannock IF. Side effects associated with the use of dexamethasone for prophylaxis of delayed emesis after moderately emetogenic chemotherapy. Br J Cancer. 2006;94:1011‐1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ehret CJ, Almodallal Y, Le‐Rademacher JG, et al. Hiccups in patients with cancer: a multi‐site, single‐institution study of etiology, severity, complications, interventions, and outcomes. BMC Cancer. 2022;22:659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yamada Y, Yamaguchi T, Matsumoto H, et al. Phase II study of oral S‐1 with irinotecan and bevacizumab (SIRB) as first‐line therapy for patients with metastatic colorectal cancer. Invest New Drugs. 2012;30:1690‐1696. [DOI] [PubMed] [Google Scholar]
- 6. Razvi Y, Chan S, McFarlane T, et al. ASCO, NCCN, MASCC/ESMO: a comparison of antiemetic guidelines for the treatment of chemotherapy‐induced nausea and vomiting in adult patients. Support Care Cancer. 2019;27:87‐95. [DOI] [PubMed] [Google Scholar]
- 7. Kang JH, Hui D, Kim MJ, et al. Corticosteroid rotation to alleviate dexamethasone‐induced hiccup: a case series at a single institution. J Pain Symptom Manage. 2012;43:625‐630. [DOI] [PubMed] [Google Scholar]
- 8. Package insert of “CAMPTO®” . Accessed November 7, 2022. https://www.info.pmda.go.jp/go/pack/4240404A1040_1_16/.
- 9. Package insert of “AVASTIN®” . Accessed November 7, 2022. https://www.info.pmda.go.jp/go/pack/4291413A1022_1_24/.
- 10. Package insert of “Aloxi®” . Accessed November 7, 2022. https://www.info.pmda.go.jp/go/pack/2391404A1020_1_07/.
- 11. Melby JC. Drug spotlight program: systemic corticosteroid therapy: pharmacology and endocrinologic considerations. Ann Intern Med. 1974;81:505‐512. [DOI] [PubMed] [Google Scholar]
- 12. Davis JN. An experimental study of hiccup. Brain. 1970;93:851‐872. [DOI] [PubMed] [Google Scholar]
- 13. Dickerman RD, Overby C, Eisenberg M, Hollis P, Levine M. The steroid‐responsive hiccup reflex arc: competitive binding to the corticosteroid‐receptor? Neuro Endocrinol Lett. 2003;24:167‐169. [PubMed] [Google Scholar]
- 14. Hosoya R, Uesawa Y, Ishii‐Nozawa R, Kagaya H. Analysis of factors associated with hiccups based on the Japanese adverse drug event report database. PLoS One. 2017;12:e0172057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. De Kloet ER, Vreugdenhil E, Oitzl MS, Joëls M. Brain corticosteroid receptor balance in health and disease. Endocr Rev. 1998;19:269‐301. [DOI] [PubMed] [Google Scholar]
- 16. Liaw C‐C, Wang C‐H, Chang H‐K, et al. Cisplatin‐related hiccups: male predominance, induction by dexamethasone, and protection against nausea and vomiting. J Pain Symptom Manage. 2005;30:359‐366. [DOI] [PubMed] [Google Scholar]
- 17. Kondo T. Three cases of drug‐induced hiccup: causative drugs and mechanisms‐the relationship with GABA receptor action‐. (in Japanese.) journal of Japanese association for. Acute Medicine. 2019;30:115‐120. [Google Scholar]
- 18. Schuster M, Bayer O, Heid F, Laufenberg‐Feldmann R. Opioid rotation in cancer pain treatment. Deutsch Arztebl Int. 2018;115:135‐142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Karako K, Song P, Chen Y, Tang W. Shifting workstyle to teleworking as a new normal in face of COVID‐19: analysis with the model introducing intercity movement and behavioral pattern. Ann Transl Med. 2020;8(17):1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Basch E. The missing voice of patients in drug‐safety reporting. N Engl J Med. 2010;362(10):865‐869. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Author elects to not share data.


