Abstract
INTRODUCTION:
To evaluate the effect of orthodontic retraction force on thick and thin gingival biotypes of anterior teeth having grade I and II gingival recession with D1 and D2 alveolar bone densities by assessing the displacement of teeth and deformation in gingival tissue, along with evaluating the amount of equivalent stress on teeth and gingiva in finite element model.
MATERIALS AND METHOD:
Based on cone-beam computed tomography datasets, eight models (LC01–LC08) of maxilla with appliance assembly were created. A retraction load of 150 gm was applied on each model during the finite element analysis (FEA), and then values of teeth displacement, gingival deformation, and von Mises stress were evaluated.
RESULT:
All the models with D1 bone density (LC01–04) were showing gingival deformation, whereas models with D2 bone quality (LC05–08) give no significant outcome. The amount of von Mises stress for teeth and gingival tissue in each model was the same for both central and lateral incisors.
CONCLUSION:
All the models having D1 bone quality showed greater gingival deformation after applying retraction force, whereas in models with D2 bone density, deformation was not significant. Changes in gingival tissue are brought about by orthodontic treatment, which also helps to correct the periodontal defects; however, bone density plays a significant role in improving gingival recession.
Keywords: Bone density, finite element analysis, gingival biotype, gingival deformation, gingival recession, orthodontic retraction
Introduction
Tooth migration outside the alveolus increases the risk of bone abnormalities, which may be preceded by gingival recession.[1] Establishment of a root into the alveolar bone can be complimented by an increased bone level and the subsequent improvement in gingival recession.[2] Periodontal alterations and orthodontic therapy can exhibit a strong relationship.[3] Numerous trials have investigated the effect of orthodontic tooth movement on periodontal tissues, primarily those resulting from the buccal migration of the incisors.[4,5] The initiation of periodontal defects, such as the onset of root resorption, as a direct consequence of unrestrained orthodontic forces,[6] the emergence of dehiscence and bone fenestrations,[7] and the recession of the gingival margin are some of the adverse effects of orthodontic treatment.[8] Although gingival recession is among the most frequently reported side effects of fixed orthodontic therapy, it remains a debatable topic.[9]
Some advanced technologies, such as the photoelasticity procedure, strain gauge technique, laser holograms, and the finite element method (FEM), can be used to determine the biological (efficiency) and biomechanical properties (stress and strain patterns) of the tooth and its surrounding structures. FEM is used to evaluate stress and strain through modeling a biological component with the help of computer software.[10] FEM can be used to obtain quantitative data that provide information on physiological processes that occur after the application of load and can help understand particular tissue reactions and physical interactions observed in response to force.[11] Treatment planning for teeth with a compromised periodontium is challenging, particularly in extraction cases. Few studies have investigated the effect of orthodontic tooth movement, such as intrusion and torquing, on gingival recession.[12,13] Moreover, no study has determined the effect of orthodontic force on the periodontium considering the gingival biotype and alveolar bone quality.
The present study investigated the effect of orthodontic retraction force on the thick and thin gingival biotypes of anterior teeth with grade I and II gingival recession and D1 and D2 bone densities. This study assessed the displacement of teeth and deformation in the gingival tissue as well as determined the amount of equivalent stress on the teeth and gingiva by using the FEM.
Materials and Method
A patient of class I bimaxillary protrusion having grade I gingival recession on upper central and lateral incisors was considered for this analysis. All four first premolar extraction treatment plans were followed, and after the leveling-alignment and canine retraction, the patient was referred to CT (computed tomography) scan after removing all the brackets, wires, and trans-palatal archs to avoid any metal artifacts. The CT scan of vertex to manubrium, 130 kV, 81 mA/s, slice increment 0.5 mm, width 512 pixels, height 512 pixels, pixel size 500 mm, gantry tilt 0.00, and algorithm h70s were used to create the CT. The maxillary arch with intact dentition was obtained as DICOM (digital imaging and communications) image. The DICOM CT images were converted to STEP (Standard for the Exchange of Product Data) format using CREO parametric version 2.0 and then imported for geometrical clean-up of maxilla with geometrical modeling.
The modeling of three-dimensional (3D) finite element model was performed using HYPERMESH software. Discretization was performed by dividing the structure into several small elements, connected with nodes. All elements and nodes were numbered so that a setup of matrix connectivity was established. The “4-noded tetrahedral” form was chosen as the finite element to describe the irregular geometry of the teeth for the maxilla, dentition, gingiva, periodontal ligament (PDL), cortical bone, and cancellous bone in this work. There are 290,020 nodes in total, containing the tetrahedron element 179976 [Table 1, Figures 1 and 2].
Table 1.
Number of nodes and elements in the model
| Structure | Elements | Nodes |
|---|---|---|
| Cortical bone | 39901 | 65013 |
| Cancellous bone | 14509 | 21868 |
| Teeth | 99751 | 159534 |
| Periodontal ligament | 9068 | 15230 |
| Bracket | 10882 | 15276 |
| Wire (stainless steel) | 4254 | 10184 |
| Niti coil spring | 1611 | 2915 |
| Total | 179976 | 290020 |
Figure 1.
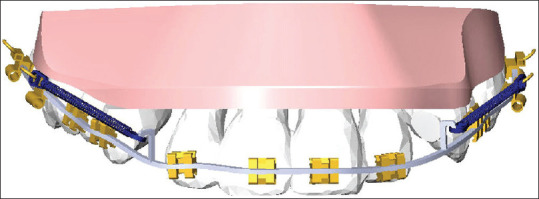
3D geometric model prepared from DICOM file having all the assembled components required for analysis
Figure 2.
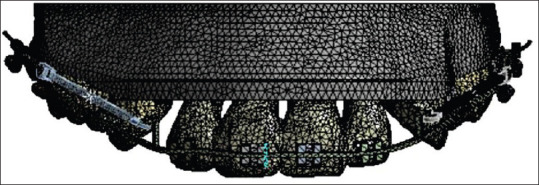
Model with meshing
Boundary conditions and material properties such as Young's modulus and Poisson's ratio were introduced for teeth, gingiva, cortical bone, cancellous bone, and PDL.[14] [Table 2]. The bracket/teeth contact was believed to be firmly bonded, and materials were linear and isotropic. All these components were independently modeled and then integrated to construct 3D finite element models of the maxilla that depicted anterior tooth retraction. The outcome was obtained in the form of cumulative deformation and von Mises stresses using ANSYS 20.1 version which can import models with 100% data transfer or with 0% data loss. The gap between the lateral and retracted canines would be used for anterior retraction. A closed coil spring of 9 mm was stretched and attached to the lever arm of 5 mm length to the hook of the molar tube on both sides. The maxillary model was built with two distinct densities of alveolar bone D1 and D2. Likewise, two different types of gingival biotype were also used, thick with 1.25 mm faciopalatal dimension and thin with 0.8 mm dimension. The evaluation of retraction force and its effect on periodontal tissue was performed in anterior teeth by creating grade I and grade II gingival recession. A total of eight geometries were created for analyzing the outcomes based on bone density, gingival biotype, and recession and assigned as load case number LC01–LC08 [Table 3].
Table 2.
List of the materials with their physical properties
| Materials | Youngs modulus (MPa) | Poisson’s ratio |
|---|---|---|
| Tooth | 20000 | 0.30 |
| Periodontal ligament | 0.059 | 0.49 |
| Alveolar bone | 20000 | 0.30 |
| Bracket | 200000 | 0.33 |
| Arch wire (Stainless steel) | 200000 | 0.33 |
| Cancellous bone | 1500 | 0.30 |
| Cortical bone | 15000 | 0.30 |
| NiTi coil spring | 83000 | 0.33 |
| Buccal mucosa | 8.33 | 0.30 |
| Gingiva | 37.63 | 0.30 |
Table 3.
Grouping based on bone density and recession
| Grouping | Gingival biotype | Gingival recession | Load case number |
|---|---|---|---|
| Group 1 with D1 bone density | Thick | Grade I | LC01 |
| Grade II | LC02 | ||
| Thin | Grade I | LC03 | |
| Grade II | LC04 | ||
| Group 2 with D2 bone density | Thick | Grade I | LC05 |
| Grade II | LC06 | ||
| Thin | Grade I | LC07 | |
| Grade II | LC08 |
Results
Before the simulation, the FEM model is marked with a fixed point at incisal tip passing through the long axis of the central and lateral incisors to accurately determine the displacement of the tooth and deformation in associated gingival tissue. On application of 150 gm retraction force on both sides of the maxillary model, the initial displacement of central and lateral incisors gave different values that are mentioned in table according to load case (LC) numbers. Likewise, the deformation in gingiva due to the displacement of these teeth and von Mises stress values are included in table [Tables 4 and 5].
Table 4.
Displacement of anterior teeth with retraction force (mm) and von Mises stress (MPa)
| Load case number | Displacement value of central incisors (mm) | von Mises stress for central incisors (MPa) | Displacement value of lateral incisors (mm) | von Mises stress for lateral incisors (MPa) |
|---|---|---|---|---|
| LC01 | 0.0015 | 1.09 | 0.0015 | 1.09 |
| LC02 | 0.0012 | 1.05 | 0.0012 | 1.05 |
| LC03 | 0.0013 | 1.22 | 0.0013 | 1.22 |
| LC04 | 0.0012 | 0.90 | 0.0010 | 0.90 |
| LC05 | 0.0004 | 0.80 | 0.0003 | 0.80 |
| LC06 | 0.0002 | 1.05 | 0.0003 | 1.05 |
| LC07 | 0.0003 | 0.90 | 0.0003 | 0.90 |
| LC08 | 0.0002 | 0.85 | 0.0003 | 0.85 |
Table 5.
Deformation of gingival tissue of anterior teeth and von Mises stress
| Load case number | Deformation value of gingival tissue of central incisors (mm) | von Mises stress on gingiva of central incisors (MPa) | Deformation value of gingival tissue of lateral incisors (mm) | von Mises stress on gingiva of lateral incisors (MPa) |
|---|---|---|---|---|
| LC01 | 0.0006 | 1.09 | 0.0006 | 1.09 |
| LC02 | 0.0009 | 1.05 | 0.0004 | 1.05 |
| LC03 | 0.0008 | 1.22 | 0.0008 | 1.22 |
| LC04 | 0.0010 | 0.90 | 0.0005 | 0.90 |
| LC05 | Nil | 0.80 | Nil | 0.80 |
| LC06 | Nil | 1.05 | Nil | 1.05 |
| LC07 | Nil | 2.77 | Nil | 2.77 |
| LC08 | Nil | 2.56 | Nil | 2.56 |
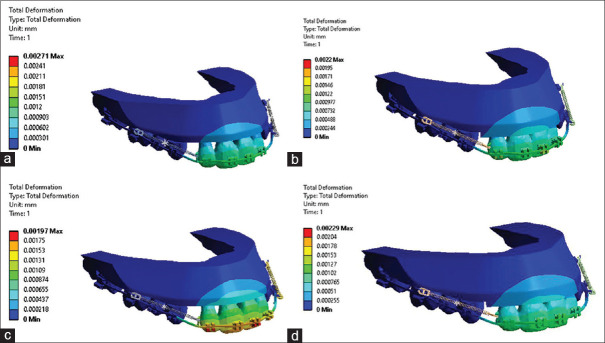
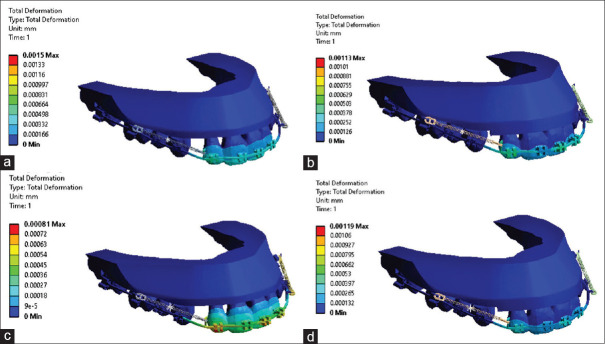
In LC01, the displacement value of central and lateral incisors is 0.0015 mm with 0.0006 mm of gingival deformation [Figure 3a], and LC02 shows that the initial displacement value for central and lateral incisors is 0.0012 mm associated with 0.0009 mm deformation for central incisors and 0.0004 mm deformation for lateral incisors [Figure 3b]. However, in LC03, the initial displacement value of central and lateral incisors is 0.0013 mm, which shows 0.0008 mm deformation in gingival tissue [Figure 3c]. Likewise in LC04, the displacement value of central incisors is 0.0012 mm and that of lateral incisors is 0.0010 mm; however, the gingival deformation for central incisors is 0.0010 and that in lateral incisors is 0.0005 mm [Figure 3d]. In LC05, the initial teeth movement value is 0.0004 mm in central incisors and 0.0003 mm for lateral incisors [Figure 4a]. However, in LC06, the displacement value for central incisors is 0.0002 mm and 0.0003 mm in lateral incisors [Figure 4b]. However, in LC07, the initial displacement values of both central and lateral incisors are 0.0003 mm [Figure 4c]. Likewise in LC08, the displacement is 0.0002 mm and 0.0003 mm in central and lateral incisors, respectively; however, the gingival deformation value is 0 in gingival tissue of both the teeth [Figure 4d]. All the models from LC05 to LC08 show no deformation in gingival tissue of both the teeth.
Figure 3.
(a) Load case LC01 showing teeth displacement and gingival deformation; (b) Load case LC02 showing teeth displacement and gingival deformation; (c) Load case LC03 showing teeth displacement and gingival deformation; (d) Load case LC04 showing teeth displacement and gingival deformation
Figure 4.
(a) Load case LC05 showing teeth displacement and gingival deformation; (b) Load case LC06 showing teeth displacement and gingival deformation; (c) Load case LC07 showing teeth displacement and gingival deformation; (d) Load case LC08 showing teeth displacement and gingival deformation
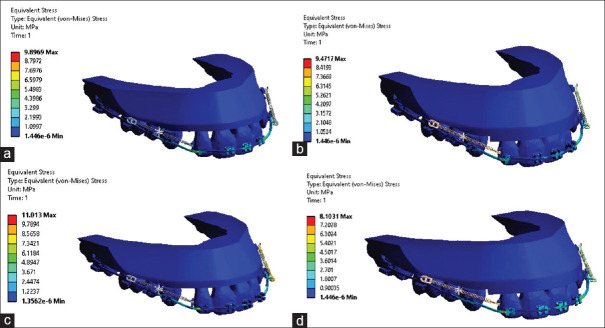
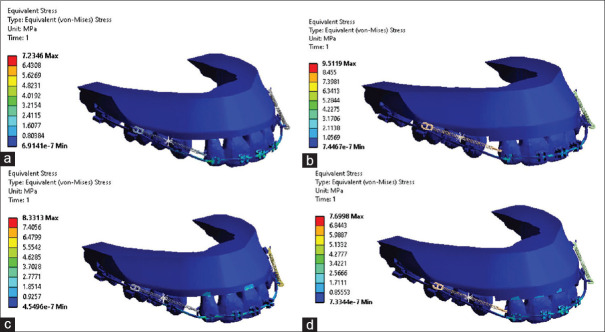
The amount of equivalent stress is the same for both central and lateral incisors and also on gingival tissues of these anterior teeth [Tables 4 and 5; Figures 5a-d, 6a-d].
Figure 5.
(a) Load case LC01 showing von Mises stress; (b) Load case LC02 showing von Mises stress; (c) Load case LC03 showing von Mises stress; (d) Load case LC04 showing von Mises stress
Figure 6.
(a) Load case LC05 showing von Mises stress; (b) Load case LC06 showing von Mises stress; (c) Load case LC07 showing von Mises stress; (d) Load case LC08 showing von Mises stress
The ratio of initial teeth displacement and gingival tissue deformation was calculated after applying the orthodontic retraction force. This ratio makes interpretation easy by determining ‘how much teeth displacement causes what amount of gingival deformation’. All the cases with D1 bone density (LC01–04) show positive results by showing gingival deformation, whereas cases with D2 bone quality (LC05–08) give no outcome. The ratio between teeth displacement and gingival deformation in LC01 is 5:2 for both central and lateral incisors, the ratio is 5:3.75 for central incisors and 5:4 for lateral incisors in LC02, the ratio is 5:3 for both central and lateral incisors in LC03, and in the case of LC04, the ratio is 5:4 and 5:2.5 for central and lateral incisors, respectively [Table 6].
Table 6.
Ratio between displacement of teeth and deformation in gingival tissue
| Load case number | Ratio between teeth displacement and gingival tissue deformation at central incisors | Ratio between teeth displacement and gingival tissue deformation at lateral incisors |
|---|---|---|
| LC01 | 5:2 | 5:2 |
| LC02 | 5:3.75 | 5:4 |
| LC03 | 5:3 | 5:3 |
| LC04 | 5:4 | 5:2.5 |
| LC05 | Nil | Nil |
| LC06 | Nil | Nil |
| LC07 | Nil | Nil |
| LC08 | Nil | Nil |
Discussion
The apical relocation of the gingival margin from the cemento–enamel junction, which exposes the root surface to the oral environment, is the fundamental characteristic of gingival recession. This phenomenon is noted in almost all communities worldwide and is usually limited to the facial aspect of a single rooted tooth.[15] If the root surface is exposed to the oral cavity, clinicians can cover the root surface with the gingival tissue only to some extent after moving the root toward the centre of alveolar bone.[16] Periodontal health can be improved by changing the inclination of a tooth or moving the tooth within alveolar bone housing.[12,13,17,18,19,20,21,22,23,24]
When the anterior teeth are retracted, care should be ensured to apply an optimal force of 150 gm to prevent side effects such as the root resorption, excessive bone loss, and hyalinization of the PDL.[25] Assuming all the boundary conditions and biomechanical efficiency of the FEM, the present study correlated the qualitative findings of previous studies with the quantitative results of the present study.
Previous human studies have reported improvement in gingival recession (mostly performed on the mandibular anterior teeth), and all the studies have considered only the grades of recession but not the quality of the gingival tissue or bone density.[13,17,18,19,20,23,24] However, the present study examined all the features of the periodontium in the finite element model.
In an animal study[19] on maxillary teeth, gingival recession was created after moving the teeth outside the alveolar bone and the teeth were then repositioned to the same position by gaining the half of the original bone but not the soft tissue. The results of the present study concerning the D2 bone did not reveal gingival deformation after the application of retraction force (LC05–08).
Deng et al.[26] suggested that gingival recession is an irreversible process, and clinicians can only prevent the occurrence of gingival recession by maintaining appropriate oral hygiene. The results of simulation performed on D2 bone density in LC05–08 cases having both thick and thin gingiva with grade I or grade II recession are in accordance with those reported by Deng et al.
In their retrospective study, Antanavičienė et al.[27] examined gingival recession in different biotypes (thick or thin) and its improvement after orthodontic treatment without considering bone quality. They observed improvement in gingival recession in half of the participants, particularly in the maxillary anterior teeth.
Gingival recession and root positioning are interdependent entities. The effect of other tooth movements, such as tipping, intrusion, and extrusion, on periodontal health should be evaluated to conclude one of the most debated topics in the fields of orthodontics and periodontics.
Limitation and future aspect
Although we had tried a biomechanical method to obtain the promising results, we cannot ignore the biological oral environment and predisposing factors for gingival recession such as oral hygiene maintenance, brushing technique, person's diet, and so on.
Various orthodontic tooth movements such as complete anterior retraction, intrusion, extrusion, tipping, and root uprighting can be performed to assess the effect on the periodontium.
Conclusion
Although the previous clinical studies include some controversies regarding the gingival recession and orthodontic treatment, based on the findings of the present biomechanical finite element study, it may be concluded that
1- Orthodontic treatment induces changes in gingival tissue and improves the periodontal defect. However, bone density may play an important role in improvement of gingival recession after orthodontic retraction of the teeth.
2- Models having D1 bone quality irrespective of gingival biotype show greater gingival deformation after applying retraction force, whereas in the case of D2 bone density, gingival deformation was not significant.
3- The equivalent stresses generated on central and lateral incisors and gingival tissue associated with these teeth are the same for all the cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Karring T, Nyman S, Thilander B, Magnusson I. Bone regeneration in orthodontically produced alveolar bone dehiscences. J Periodont Res. 1982;17:309–15. doi: 10.1111/j.1600-0765.1982.tb01158.x. [DOI] [PubMed] [Google Scholar]
- 2.Nyman S, Karring T, Bergenholtz G. Bone regeneration in alveolar bone dehiscences produced by jiggling forces. J Periodont Res. 1982;17:316–22. doi: 10.1111/j.1600-0765.1982.tb01159.x. [DOI] [PubMed] [Google Scholar]
- 3.Alfuriji S, Alhazmi N, Alhamlan N, Al-Ehaideb A, Alruwaithi M, Alkatheeri N, et al. The effect of orthodontic therapy on periodontal health: A review of the literature. Int J Dent 2014. 2014 doi: 10.1155/2014/585048. 585048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aziz T, Flores-Mir C. A systematic review of the association between appliance-induced labial movement of mandibular incisors and gingival recession. Aust Orthod J. 2011;27:33–9. [PubMed] [Google Scholar]
- 5.Djeu G, Hayes C, Zawaideh S. Correlation between mandibular central incisor proclination and gingival recession during fixed appliance therapy. Angle Orthod. 2002;72:238–45. doi: 10.1043/0003-3219(2002)072<0238:CBMCIP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Nakada T, Motoyoshi M, Horinuki E, Shimizu N. Cone-beam computed tomography evaluation of the association of cortical plate proximity and apical root resorption after orthodontic treatment. J Oral Sci. 2016;58:231–6. doi: 10.2334/josnusd.15-0566. [DOI] [PubMed] [Google Scholar]
- 7.Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: A retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2005;127:552–61. doi: 10.1016/j.ajodo.2003.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C. Orthodontic therapy and gingival recession: A systematic review. Orthod Craniofac Res. 2010;13:127–41. doi: 10.1111/j.1601-6343.2010.01491.x. [DOI] [PubMed] [Google Scholar]
- 9.Johal A, Katsaros C, Kiliaridis S, Leitao P, Rosa M, Sculean A, et al. State of the science on controversial topics: Orthodontic therapy and gingival recession (a report of the Angle Society of Europe 2013 meeting) Prog Orthod. 2013;14:16. doi: 10.1186/2196-1042-14-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knop L, Gandini LG, Jr, Shintcovsk RL, Gandini MR. Scientific use of the finite element method in Orthodontics. Dental Press J Orthod. 2015;20:119–25. doi: 10.1590/2176-9451.20.2.119-125.sar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grbović A, Mihajlović D. Practical aspects of finite element method applications in dentistry. Balkan J Dent Med. 2017;21:69–77. [Google Scholar]
- 12.Laursen MG, Rylev M, Melsen B. The role of orthodontics in the repair of gingival recessions. Am J Orthod Dentofacial Orthop. 2020;157:29–34. doi: 10.1016/j.ajodo.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 13.Machado AW, MacGinnis M, Damis L, Moon W. Spontaneous improvement of gingival recession after correction of tooth positioning. Am J Orthod Dentofacial Orthop. 2014;145:828–35. doi: 10.1016/j.ajodo.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 14.Moga RA, Cosgarea R, Buru SM, Chiorean CG. Finite element analysis of the dental pulp under orthodontic forces. Am J Orthod Dentofacial Orthop. 2019;155:543–51. doi: 10.1016/j.ajodo.2018.05.018. [DOI] [PubMed] [Google Scholar]
- 15.Jati AS, Furquim LZ, Consolaro A. Gingival recession: Its causes and types, and the importance of orthodontic treatment. Dental Press J Orthod. 2016;21:18–29. doi: 10.1590/2177-6709.21.3.018-029.oin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim J, Amar S. Periodontal disease and systemic conditions: A bidirectional relationship. Odontology. 2006;94:10–21. doi: 10.1007/s10266-006-0060-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dorfman HS. Mucogingival changes resulting from mandibular incisor tooth movement. Am J Orthod. 1978;74:286–97. doi: 10.1016/0002-9416(78)90204-x. [DOI] [PubMed] [Google Scholar]
- 18.Coatoam GW, Behrents RG, Bissada NF. The width of keratinized gingiva during orthodontic treatment: Its significance and impact on periodontal status. J Periodontol. 1981;52:307–13. doi: 10.1902/jop.1981.52.6.307. [DOI] [PubMed] [Google Scholar]
- 19.Engelking G, Zachrisson BU. Effects of incisor repositioning on monkey periodontium after expansion through the cortical plate. Am J Orthod. 1982;82:23–32. doi: 10.1016/0002-9416(82)90542-5. [DOI] [PubMed] [Google Scholar]
- 20.Ngan PW, Burch JG, Wei SH. Grafted and ungrafted labial gingival recession in pediatric orthodontic patients: Effects of retraction and inflammation. Quintessence Int. 1991;22:103–11. [PubMed] [Google Scholar]
- 21.McComb JL. A review orthodontic treatment and isolated gingival recession. Br J Orthod. 1994;21:151–9. doi: 10.1179/bjo.21.2.151. [DOI] [PubMed] [Google Scholar]
- 22.Northway WM. Gingival recession—can orthodontics be a cure? Evidence from a case presentation. Angle Orthod. 2013;83:1093–101. doi: 10.2319/012413-76.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kamak G, Kamak H, Keklik H, Gurel HG. The effect of changes in lower incisor inclination on gingival recession. ScientificWorldJournal 2015. 2015 doi: 10.1155/2015/193206. 193206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanocki G. Gingival recession management in orthodontic treatment – A case report. Orthod Forum. 2017;13:190–201. [Google Scholar]
- 25.Barlow M, Kula K. Factors influencing efficiency of sliding mechanics to close extraction space: A systematic review. Orthod Craniofac Res. 2008;11:65–73. doi: 10.1111/j.1601-6343.2008.00421.x. [DOI] [PubMed] [Google Scholar]
- 26.Deng H, Miao D, Liu J, Meng S, Wu Y. The regeneration of gingiva: Its potential value for the recession of healthy gingiva. Med Hypotheses. 2010;74:76–7. doi: 10.1016/j.mehy.2009.07.051. [DOI] [PubMed] [Google Scholar]
- 27.Antanavičienė G, Zasčiurinskienė E, Smailienė D, Basevičienė N. The impact of orthodontic treatment on pre-existing gingival recessions: A retrospective study. Appl Sci. 2021;11:9036. [Google Scholar]