Abstract
Objective
To describe the prevalence of ‘graded thinness’ in children aged 11, 13 and 15 years in eleven developed countries and to identify trends in the prevalence of ‘thinness’ (BMI < 17 kg/m2 at age 18 years) by age and gender.
Design
Cross-sectional study using data collected through self-reported questionnaires.
Setting
Data were taken from the 1997/1998, 2001/2002 and 2005/2006 surveys of the Health Behaviours in School-aged Children (HBSC) Study.
Subjects
Children and adolescents from ten European countries and the USA (n 158 000).
Results
Prevalence of grades 1, 2 and 3 of thinness was higher among 11-year-old students compared with the 13- and 15-year-olds in all countries. A higher prevalence of thinness was observed in girls than in boys. Since 1998 the prevalence of thinness decreased steadily in Czech boys and girls, while it increased for French girls. In the total European sample of females, thinness decreased from 1998 to 2006 (χ 2 for trend, P < 0·01). Age-adjusted logistic regression analysis showed that Czech boys and girls, and Flemish and American girls were less likely to be thin in 2006 than in 1998; while a noteworthy increment, even if borderline significant, was observed for French girls with a 41 % increase in the likelihood to be thin.
Conclusions
Our findings suggest that thinness is an important overlooked phenomenon with wide variation in prevalence and trends across developed countries. It deserves further longitudinal studies in a multinational context that could increase the understanding of the factors associated with thinness and contribute to developing preventive and nutritional programmes targeted at controlling obesity and chronic diseases, while monitoring thinness.
Keywords: Adolescents, BMI, Graded thinness, Underweight, Trend
Thinness in infants, children and adolescents poses a considerable public health problem internationally and may produce unfavourable outcomes, particularly in young women, because their desire for thinness is greater than that of other age groups( 1 – 3 ). In most European countries, teenagers are under social pressure to pursue an unreal beauty ideal of thinness( 4 ), which may lead to risky weight-management practices and eating disorders. In the developed world, anorexia nervosa is in fact the third most common chronic condition of adolescence( 5 ). Moreover, thinness is frequently associated with nutritional deficiencies, menstrual irregularity, decreased cognitive and work capacity, and increased infections( 6 ).
Nevertheless, while in developed countries the childhood obesity epidemic( 7 ) and related consequences have broadly been investigated, thinness has received less consideration, although overweight and thinness frequently coexist even within a single family. This phenomenon, referred to as ‘dual burden households’( 8 , 9 ), occurs in all countries and presents growing public health concerns for underweight individuals who may inadvertently become the focus of obesity prevention initiatives.
Until 2007, when Cole et al.( 10 ) proposed international age- and sex-specific thinness cut-offs from 2 to 18 years to provide comparable prevalence rates of thinness, trends in thinness among children and adolescents had been seldom described( 11 ) and the comparisons between countries had been difficult due to the use of several cut-off points (Centers for Disease Control and Prevention, WHO and International Obesity Task Force growth references) and different terms (underweight, wasting, thinness, undernutrition), which have a different meaning in adults, adolescents and children( 10 – 20 ). In their paper, Cole et al. ‘tried to avoid potential confusion between the terms wasting and underweight in children by adopting the term thinness, which WHO uses to mean low BMI in adults and adolescents’ and ‘extended the definition to include low BMI for age in children, linked to the adult definition through the fulcrum of BMI 17 at age 18’. Then in addition to the primary cut-off of BMI = 17 kg/m2 they proposed ‘two secondary cut offs: 18·5, long used by WHO in adult studies and for grade 1 thinness, and 16, used for grade 3 thinness’. Thus the ‘three cut offs correspond to the WHO graded definition of thinness’( 20 ).
The objectives of the present study were to: (i) describe the prevalence of graded thinness in ten European countries and the USA, using the three cut-off points proposed by Cole et al. ( 10 ); and (ii) identify trends in the prevalence of grade 2 thinness and below (BMI < 17 kg/m2 at age 18 years) in nationally representative samples of 11-, 13- and 15-year-old children from eleven countries.
To our knowledge, the present study is the first analysis of thinness prevalence and trends over the last 10 years among 11–15-year-olds in several European countries and the USA using a standardized scientific methodology( 21 ) and the international cut-offs( 10 ) recommended by the International Obesity Task Force that are suitable for use with a sample of children and adolescents in comparative studies. Recently some studies have used the international reference cut-offs( 10 ) to describe the trends in thinness at the national level( 19 , 22 – 24 ).
From this point onwards, unless otherwise specified, the term ‘thinness’ as used in the present article refers to the cut-off identified by Cole et al. (‘BMI 17 at age 18’).
Methods
The present analysis uses data from the Health Behaviour in School-aged Children (HBSC) Study, which is an international WHO collaborative study conducted in schools every four years. A detailed description of the study, its historical development and methods are available elsewhere( 25 – 27 ). According to the HBSC international research protocol, appropriate ethical approval was gained from qualified authorities or committees for the study in all countries( 26 , 27 ). The survey instrument is an internationally standardized self-report questionnaire which is administered in the classroom and whose completion takes approximately 50 min. Participants gave their assent and were assured of the confidentiality of their answers. Parental permission to participate was obtained before administration.
Participants
Analyses were based on cross-sectional data from the HBSC surveys, which involved nationally representative samples selected by clustered sampling design where the primary sampling unit was the class or school. The recommended minimum sample size for each of the three age groups was 1536 students to ensure a confidence interval of ±3 % around a proportion of 50 % and an estimated Deft value of 1·2( 25 – 28 ). The specific populations selected for sampling included those in school and aged 11, 13 and 15 years; i.e. in their 12th, 14th and 16th year (Table 1). For the current analyses data from ten European countries and the USA were used, where BMI data were available over the 1997/1998, 2001/2002 and 2005/2006 survey rounds, and for which missing values on BMI-related variables were less than 20 % of the sample surveyed. The sample included 158 000 adolescents from eleven countries in Europe and the USA.
Table 1.
Sample description: number of participants in 1997/1998, 2001/2002 and 2005/2006 surveys, by year of data collection, gender, country† and age; Health Behaviour in School-aged Children (HBSC) Study
| Missing‡ | 11 years | 13 years | 15 years | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | Boys (n) | Girls (n) | Boys (n) | Girls (n) | Boys (n) | Girls (n) | |
| Austria | ||||||||
| 1998 | 222 | 5 | 723 | 690 | 744 | 759 | 604 | 759 |
| 2002 | 371 | 9 | 750 | 777 | 771 | 791 | 643 | 634 |
| 2006 | 276 | 6 | 853 | 841 | 794 | 793 | 693 | 801 |
| Belgium-Flemish | ||||||||
| 1998 | 359 | 8 | 828 | 902 | 781 | 754 | 797 | 762 |
| 2002 | 413 | 7 | 1003 | 1150 | 966 | 1140 | 1027 | 1003 |
| 2006 | 347 | 8 | 670 | 621 | 697 | 707 | 831 | 785 |
| Czech Republic | ||||||||
| 1998 | 77 | 2 | 579 | 588 | 637 | 637 | 596 | 609 |
| 2002 | 22 | 1 | 826 | 865 | 780 | 881 | 806 | 854 |
| 2006 | 56 | 1 | 765 | 744 | 804 | 797 | 842 | 823 |
| Denmark | ||||||||
| 1998 | 540 | 11 | 793 | 842 | 855 | 892 | 737 | 783 |
| 2002 | 578 | 13 | 783 | 867 | 772 | 796 | 656 | 713 |
| 2006 | 951 | 17 | 985 | 1108 | 980 | 1057 | 762 | 790 |
| Finland | ||||||||
| 1998 | 216 | 4 | 796 | 858 | 803 | 824 | 764 | 772 |
| 2002 | 143 | 3 | 952 | 937 | 873 | 845 | 867 | 874 |
| 2006 | 249 | 5 | 850 | 933 | 834 | 891 | 790 | 895 |
| France | ||||||||
| 1998 | 327 | 8 | 736 | 731 | 642 | 779 | 592 | 653 |
| 2002 | 561 | 7 | 1332 | 1339 | 1421 | 1479 | 1301 | 1313 |
| 2006 | 533 | 8 | 1265 | 1228 | 1147 | 1279 | 1139 | 1083 |
| Germany | ||||||||
| 1998 | 275 | 6 | 813 | 756 | 821 | 792 | 795 | 796 |
| 2002 | 757 | 13 | 1056 | 1038 | 879 | 921 | 842 | 899 |
| 2006 | 626 | 9 | 1127 | 1104 | 1234 | 1207 | 1271 | 1281 |
| Greece | ||||||||
| 1998 | 110 | 6 | 788 | 800 | 643 | 653 | 605 | 717 |
| 2002 | 223 | 4 | 627 | 625 | 600 | 631 | 643 | 681 |
| 2006 | 133 | 4 | 543 | 544 | 553 | 634 | 650 | 766 |
| Portugal | ||||||||
| 1998 | 386 | 11 | 446 | 557 | 564 | 632 | 534 | 775 |
| 2002 | 266 | 11 | 579 | 586 | 456 | 507 | 378 | 422 |
| 2006 | 352 | 9 | 623 | 578 | 648 | 687 | 613 | 770 |
| Sweden | ||||||||
| 1998 | 393 | 10 | 656 | 621 | 699 | 647 | 607 | 537 |
| 2002 | 389 | 10 | 743 | 744 | 606 | 585 | 609 | 609 |
| 2006 | 422 | 10 | 772 | 741 | 655 | 698 | 752 | 774 |
| USA | ||||||||
| 1998 | 602 | 12 | 709 | 849 | 873 | 930 | 813 | 995 |
| 2002 | 578 | 12 | 674 | 805 | 894 | 1027 | 754 | 871 |
| 2006 | 375 | 11 | 500 | 594 | 708 | 806 | 649 | 635 |
Only countries or regions included in the trend analysis.
Percentage of 11–15-year-olds who did not respond to one or more self-reported weight and height items, by country/region and year of data collection.
Variables
BMI
Items on self-reported weight and height were mandatory questions in the 2001/2002 and 2005/2006 surveys for all participating countries. In 1997/1998, fifteen countries (Austria, Belgium-Flanders, Czech Republic, Denmark, Finland, France, Germany, Greece, Israel, Lithuania, Ireland, Portugal, Slovakia, Sweden and USA) included these variables. Weight and height were assessed by asking: ‘How much do you weigh without clothes?’ and ‘How tall are you without shoes?’, respectively. These items remained unchanged for the three survey rounds.
The items were formulated as open-ended questions and thus enabled countries to use whatever measurement system was appropriate. Non-metric measurements were converted into corresponding metric measurements according to the following formulas: centimetres = [(feet × 12) +inches] × 2·54, metres = centimetres/100 and kilograms =[(stones × 14) + pounds] × 0·454. A new variable BMI was computed from the original cleaned data as weight (kg) divided by the square of height (m2).
Graded thinness
The BMI variable was first categorized according to Cole et al., who have proposed a graded definition of thinness in childhood and adolescence based on pooled international data for BMI and linked to the WHO recommended adult cut-off points of 16, 17 and 18·5 kg/m2 at age 18 years( 10 ). Using these international age- and sex-specific cut-offs, the three categories of thinness were determined, coding grades 1, 2 and 3 as cut-offs of BMI = 17 to <18·5 kg/m2, BMI = 16 to <17 kg/m2 and BMI < 16 kg/m2, respectively.
Thinness
The primary variable for trend analyses was a dichotomous variable, used to describe the proportion of children with BMI corresponding to the cut-off of <17 kg/m2 at age 18 years.
Year trend
The key independent variable was an ordered variable representing the survey time. It was coded 0 for the 1997/1998 survey, 1 for the 2001/2002 survey and 2 for the 2005/2006 survey.
Sociodemographic characteristics
Sociodemographic characteristics analysed were age and country or region of residence of the children.
Missing values
A large number of height and/or weight values were missing in the three HBSC surveys (about 10 % on average, Table 1), with the percentage of missing values being higher than 20 % in some countries resulting in their exclusion from the analysis (43 % in Ireland, 31 % in Lithuania and 20 % in Israel). The extreme values of height, weight and BMI (recoded as ‘out-of-range’) in the three HBSC surveys have been cleaned according to the same criteria using the range estimates of the US Centers for Disease Control and Prevention's website under the Growth Chart Site.
Statistical analysis
The data were analysed using the statistical software package SPSS for Windows version 16·0 and a more conservative two-sided level of significance of P = 0·01 was applied in the present study to account for the cluster sampling. Trends were assessed using unweighted prevalence of thinness from countries that had data at every time point. Temporal trends in graded-thinness prevalence were plotted by age category, gender and country (Figs 1 and 2).
Fig. 1.
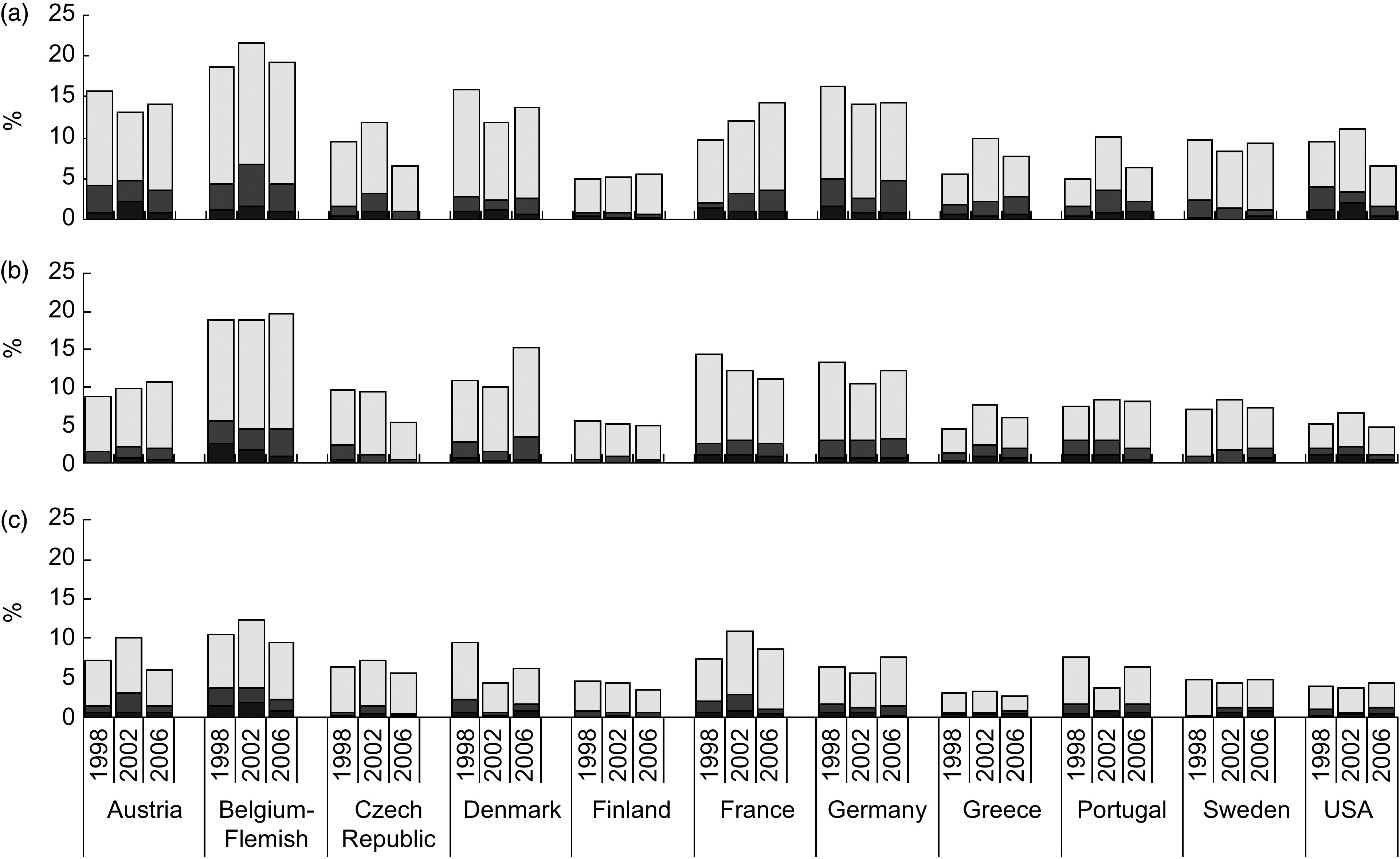
Prevalences of thinness grade 1 ( ), thinness grade 2 (
), thinness grade 2 ( ) and thinness grade 3 (
) and thinness grade 3 ( ) in (a) 11-year-old, (b) 13-year-old and (c) 15-year-old boys, by country and year of data collection; Health Behaviour in School-aged Children (HBSC) Study
) in (a) 11-year-old, (b) 13-year-old and (c) 15-year-old boys, by country and year of data collection; Health Behaviour in School-aged Children (HBSC) Study
Fig. 2.
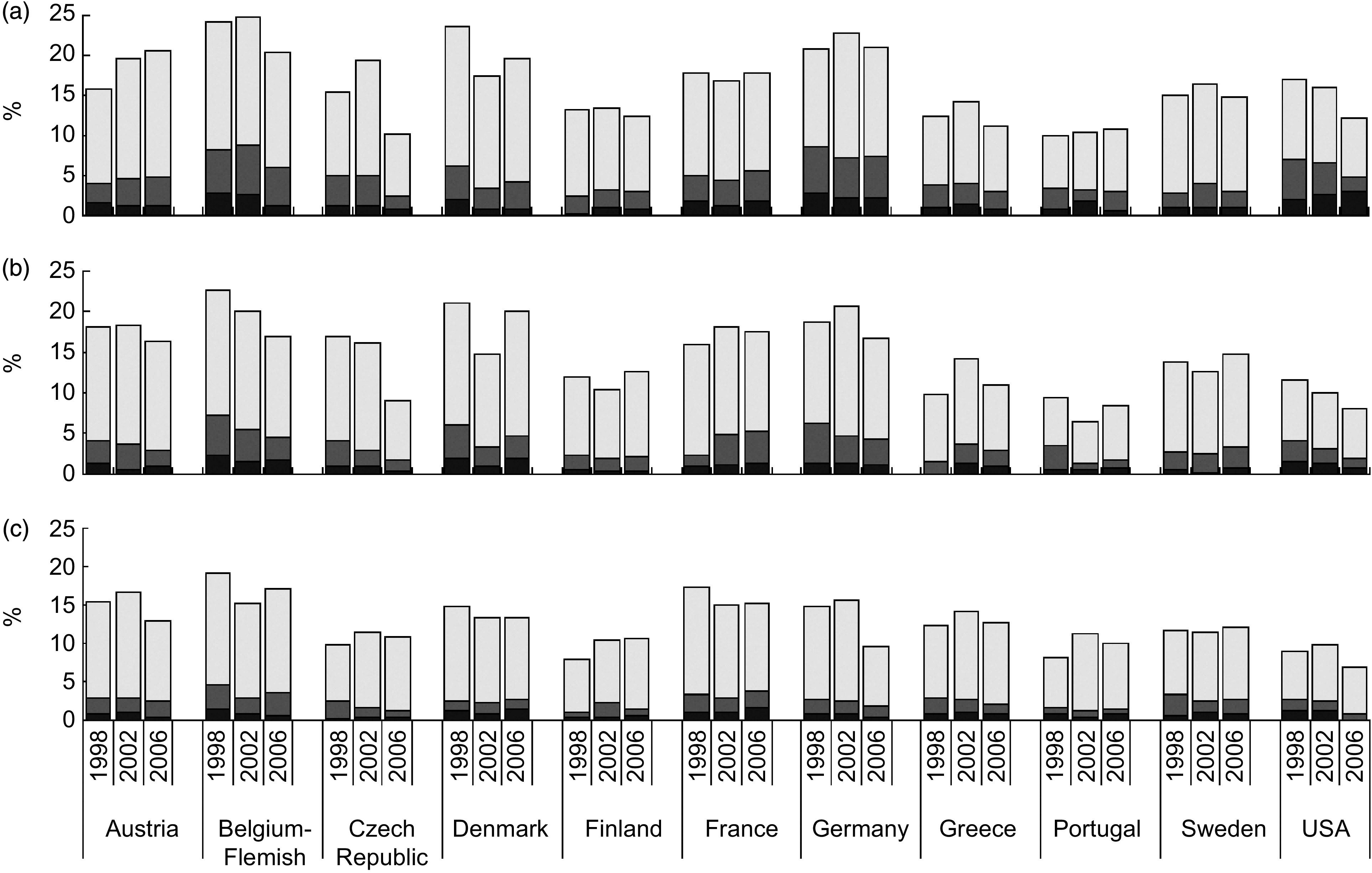
Prevalences of thinness grade 1 ( ), thinness grade 2 (
), thinness grade 2 ( ) and thinness grade 3 (
) and thinness grade 3 ( ) in (a) 11-year-old, (b) 13-year-old and (c) 15-year-old girls, by country and year of data collection; Health Behaviour in School-aged Children (HBSC) Study
) in (a) 11-year-old, (b) 13-year-old and (c) 15-year-old girls, by country and year of data collection; Health Behaviour in School-aged Children (HBSC) Study
The χ 2 test for trend (Mantel–Haenszel extension) was calculated to assess a significant steady decrease or increase in the prevalence of thinness (BMI < 17 kg/m2 at age 18 years) across age groups within national surveys and across survey years by age.
Logistic regression analyses by gender and country (Table 3) were used to quantify the changes from 1998 to 2006 in the likelihood to be thin. Thinness was used as a dependent variable and the survey period as an independent variable (dummy), while controlling for age. The odds ratios and relative 99 % confidence intervals were calculated with the 1997/1998 survey as the reference category.
Table 3.
Odds ratios and 99 % confidence intervals for thinness (BMI < 17 kg/m2 at age 18 years) by country and gender from age-adjusted logistic regression models; Health Behaviour in School-aged Children (HBSC) Study
| 2001/2002 | 2005/2006 | ||||
|---|---|---|---|---|---|
| Country | 1997/1998† | OR | 99 % CI | OR | 99 % CI |
| Boys‡ | |||||
| Austria | 1·00 | 1·27 | 0·77, 2·09 | 0·97 | 0·58, 1·63 |
| Belgium-Flemish | 1·00 | 1·12 | 0·79, 1·58 | 0·81 | 0·54, 1·21 |
| Czech Republic | 1·00 | 1·25 | 0·67, 2·33 | 0 · 37 § | 0·16, 0·87* |
| Denmark | 1·00 | 0·59 | 0·33, 1·01 | 0·98 | 0·61, 1·60 |
| Finland | 1·00 | 1·07 | 0·46, 2·48 | 0·78 | 0·31, 1·99 |
| France | 1·00 | 1·30 | 0·81, 2·11 | 1·07 | 0·65, 1·77 |
| Germany | 1·00 | 0·75 | 0·48, 1·20 | 0·98 | 0·66, 1·47 |
| Greece | 1·00 | 1·37 | 0·68, 2·73 | 1·53 | 0·76, 3·01 |
| Portugal | 1·00 | 1·27 | 0·66, 1·26 | 0·87 | 0·45, 1·70 |
| Sweden | 1·00 | 1·28 | 0·59, 2·76 | 1·33 | 0·63, 2·82 |
| USA | 1·00 | 0·81 | 0·46, 1·42 | 0·55 | 0·27, 1·06 |
| Girls‡ | |||||
| Austria | 1·00 | 0·99 | 0·64, 1·53 | 0·94 | 0·61, 1·44 |
| Belgium-Flemish | 1·00 | 0·86 | 0·64, 1·15 | 0·68 § | 0·48, 0·97* |
| Czech Republic | 1·00 | 0·85 | 0·55, 1·30 | 0·47 § | 0·28, 0·79** |
| Denmark | 1·00 | 0 · 59 § | 0·39, 0·89** | 0·75 | 0·67, 1·09 |
| Finland | 1·00 | 1·25 | 0·76, 2·08 | 1·13 | 0·67, 1·89 |
| France | 1·00 | 1·12 | 0·77, 1·64 | 1·41 | 0·97, 2·06 |
| Germany | 1·00 | 0·88 | 0·62, 1·24 | 0·76 | 0·54, 1·05 |
| Greece | 1·00 | 1·22 | 0·76, 1·96 | 0·93 | 0·55, 1·55 |
| Portugal | 1·00 | 0·70 | 0·37, 1·32 | 0·65 | 0·36, 1·16 |
| Sweden | 1·00 | 1·05 | 0·62, 1·77 | 1·03 | 0·62, 1·72 |
| USA | 1·00 | 0·78 | 0·54, 1·15 | 0 · 49 § | 0·30, 0·79** |
*P < 0·01, **P < 0·001 (Wald test).
†Reference category.
‡Total samples of 11–15-year-olds.
§Underlined bold characters are used to highlight significant changes in the likelihood to be thin in 2005/2006 compared with 1997/1998 (age-adjusted OR, 99% CI)
Results
Data collected from European and American adolescents during 1997/1998, 2001/2002 and 2005/2006 showed (Figs 1 and 2) that prevalence of thinness grade 1, 2 and 3 was higher among 11-year-old students compared with the 13- and 15-year-olds, with no effect by gender. For all countries similar patterns were observed for prevalence of thinness, with prevalence ranging (Table 2) in boys between 0·2 % in Swedish 15-year-olds (1998) and 6·9 % in Belgian-Flemish 11-year-olds (2002) and in girls between 0·8 % in American 15-year-olds (2002) and 8·8 % in Belgian-Flemish 11-year-olds (2002).
Table 2.
Prevalence of thinness (BMI < 17 kg/m2 at age 18 years) by year of data collection, gender, country† and age; Health Behaviour in School-aged Children (HBSC) Study
| Boys | Girls | |||||||
|---|---|---|---|---|---|---|---|---|
| Country or region | 11 years | 13 years | 15 years | 11 years | 13 years | 15 years | ||
| Austria | 1998‡ | 4 · 3 | 1· 6 | 1·4 | 1998 | 3·9 | 4·1 | 2·7 |
| 2002 | 4·8 | 2·2 | 3·0 | 2002 | 4·6 | 3·7 | 2·9 | |
| 2006‡ | 3 · 6 | 2· 0 | 1· 4 | 2006 | 4·7 | 2·9 | 2·5 | |
| Belgium-Flemish | 1998 | 4·4 | 5·5 | 3·8 | 1998‡ | 8 · 3 | 7· 2 | 4· 5 |
| 2002‡ | 6 · 9 | 4· 4 | 3· 7 | 2002‡ | 8 · 8 | 5· 4 | 2· 9 | |
| 2006 | 4·4 | 4·6 | 2·3 | 2006 | 6·0 | 4·5 | 3·4 | |
| Czech Republic | 1998 | 1·6 | 2·4§ | 0·7 | 1998‡ | 5·0 | 4 · 0 § | 2 · 3 |
| 2002‡ | 3 · 3 | 1 · 2 | 1 · 4 | 2002‡ | 5 · 0 | 3 · 0 | 1 · 6 | |
| 2006 | 1·1 | 0·4 | 0·4 | 2006 | 2·4 | 1 · 8 | 1·2 | |
| Denmark | 1998 | 2·9 | 2·7 | 2·2 | 1998‡ | 6 · 2 | 6· 0 | 2· 5 |
| 2002‡ | 2 · 5 | 1· 6 | 0· 5 | 2002 | 3·5 | 3·3 | 2·2 | |
| 2006 | 2·7 | 2·4 | 1·6 | 2006 | 4·3 | 4·6 | 2·6 | |
| Finland | 1998 | 1·0 | 0·5 | 0·8 | 1998 | 2·5 | 2·4 | 0·9 |
| 2002 | 0·9 | 1·0 | 0·6 | 2002 | 3·2 | 1·8 | 2·2 | |
| 2006 | 0·7 | 0·5 | 0·5 | 2006‡ | 3 · 0 | 2· 2 | 1· 3 | |
| France | 1998 | 2·1 | 2·6 | 2·1 | 1998 | 5·0 | 2·3§ | 3·4 |
| 2002 | 3·1 | 3·1 | 3·0 | 2002 | 4·4 | 4·9 | 2·9 | |
| 2006‡ | 3 · 6 | 2· 5 | 1· 0 | 2006 | 5·7 | 5·3 | 3·6 | |
| Germany | 1998‡ | 5 · 0 | 3· 1 | 1· 6 | 1998‡ | 8 · 5 | 6· 3 | 2· 6 |
| 2002 | 2·7 | 3·0 | 1·3 | 2002‡ | 7 · 1 | 4· 7 | 2· 5 | |
| 2006‡ | 4 · 8 | 3· 2 | 1· 4 | 2006‡ | 7 · 3 | 4· 2 | 1· 8 | |
| Greece | 1998 | 2·0 | 1·3 | 0·5 | 1998 | 3·8 | 1·6 | 2·8 |
| 2002 | 2·3 | 2·5 | 0·6 | 2002 | 4·0 | 3·7 | 2·6 | |
| 2006‡ | 2 · 9 | 1· 9 | 0· 8 | 2006 | 2·9 | 2·8 | 2·0 | |
| Portugal | 1998 | 1·6 | 3·0 | 1·6 | 1998 | 3·4 | 3·5 | 1·7 |
| 2002 | 3·7 | 3·1 | 0·8 | 2002 | 3·3 | 1·3 | 1·3 | |
| 2006 | 2·3 | 1·9 | 1·6 | 2006 | 2·9 | 1·8 | 1·4 | |
| Sweden | 1998‡ | 2·5 | 0·8 | 0·2 | 1998 | 2·8 | 2·7 | 3·2 |
| 2002 | 1·6 | 1·7 | 1·2 | 2002 | 4·0 | 2·5 | 2·5 | |
| 2006 | 1·3 | 2·0 | 1·3 | 2006‡ | 3·0 | 3·3 | 2·6 | |
| USA | 1998‡ | 4 · 1 | 1· 9 | 0· 9 | 1998‡ | 7 · 0 | 4· 0 | 2· 6 |
| 2002‡ | 3 · 5 | 2· 2 | 0· 6 | 2002 | 6 · 6 | 3· 0 | 2· 4 | |
| 2006 | 1·6 | 1·1 | 1·2 | 2006‡ | 4 · 9 | 2· 0 | 0· 8 | |
| Ten European countries combined | 1998‡ | 2 · 8 | 2· 3 | 1· 5 | 1998‡ | 5 · 1 | 4· 1 | 2· 6 |
| 2002‡ | 3 · 2 | 2· 4 | 1· 8 | 2002‡ | 5 · 0 | 3· 7 | 2· 4 | |
| 2006‡ | 2 · 8 | 2· 3 | 1· 2 | 2006‡ | 4 · 4 | 3· 5 | 2· 2 | |
Only countries or regions included in the trend analysis.
Significant linear trend in prevalence across age groups by survey (test for trend, P < 0·01; underlined data).
Significant linear trend in prevalence across survey years by age (test for trend, P < 0·01; data in bold).
Table 2 presents a decreasing trend of thinness (BMI < 17 kg/m2 at age 18 years) by age group but it was not a characteristic of all national surveys. In 1997/1998, 2001/2002 and 2005/2006, thinness decreased steadily with age for both genders only in the Czech Republic, Germany and the USA and for girls in Belgium (χ 2 for linear trend, P < 0·01). If we combine data of the ten European countries, thinness decreased with age in both genders by all years examined. Considering the total samples of 11–15-year-olds by gender, there was a significant decrease from 1998 to 2006 only in females (P < 0·01; data not presented in table).
Although the prevalence of thinness declined in almost all countries, larger age-adjusted reductions were observed in the likelihood to be thin in 2006 compared with 1998 (Table 3) for Czech boys and girls (OR = 0·37, 99 % CI 0·16, 0·87 for boys; OR = 0·47, 99 % CI 0·28, 0·79 for girls) and for American girls (OR = 0·49, 99 % CI 0·30, 0·79 for girls) and Flemish girls (OR = 0·68, 99 % CI 0·48, 0·97 for girls) and for Danish girls, but only from 1998 to 2002 (OR = 0·59, 99 % CI 0·39, 0·89 for girls).
Increments, even if not statistically significant, were observed for both boys and girls in Sweden (OR = 1·33, 99 % CI 0·63, 2·82 for boys; OR = 1·03, 99 % CI 0·62, 1·72 for girls) and for Greek boys (OR = 1·53, 99 % CI 0·76, 3·01) and Finnish girls (OR = 1·13, 99 % CI 0·67, 1·89 for girls). Finally a noteworthy increment, even if borderline significant, was observed for French girls, with a 41 % increase in odds to be thin in 2006 with respect to 1998 (OR = 1·41, 99 % CI 0·97, 2·06).
Discussion
Thinness in children and adolescents poses a considerable public health problem globally and in the developed world, where anorexia nervosa is the third most common chronic condition of adolescence( 5 ). Thinness can also result in problems such as osteoporosis, menstrual irregularity, increased susceptibility to infections, hypothermia, thinning hair and premature mortality( 1 ).
In the present study, ‘the fulcrum of BMI 17 at age 18’, proposed by Cole and colleagues( 10 ) to unify the two WHO definitions of thinness for adults and adolescents, while extending its use to include low BMI for age in children too, was used to explore the direction in prevalence of thinness across developed countries. To our knowledge the current report is the first one on thinness trends among adolescents of ten European countries and the USA, using internationally agreed standards and utilizing international data collected using a standardized protocol. The study found that the frequency of thinness has decreased in almost all countries from 1998 to 2006 and across age groups; however, declines were significant only for Czech boys and girls, and Flemish and American girls. A decline in the frequency of thinness has been forecast for developed countries as a whole, over the period 1990–2015( 29 ), and the present data seem to follow this prediction. The forecast, and indeed the data that follow, are probably due to a shift to the right of the entire distribution of BMI associated with the obesity epidemic( 22 , 29 ). As hand in hand with this overall phenomenon are an increase in obesity and overweight and a decrease in underweight, the reason for this evolution might be linked to a progressive increase in the number of households with a lower standard of living and, consequently, to the change in eating habits. In fact, individuals of lower social status spend a lower percentage of their disposable income on food and tend to cover energy requirements more easily by purchasing high-energy products, which are often cheaper than low-energy products( 30 , 31 ). While the obesity epidemic is receiving considerable attention in terms of both policy and practice, it is important not to forget the public health challenge posed by thinness. Data such as those presented herein are important in order to track prevalence and identify where resources and follow-up may be particularly needed. Up a until few years ago, it appears that only some studies( 23 , 24 , 32 – 34 ) published results using the agreed cut-offs to define thinness in European children and adolescents. Up until then different cut-offs were used, which led to differences in the prevalence of thinness and by gender. It was timely that international data using the same classification system were available on thinness.
In contrast to most countries, the frequency of thinness, although not statistically significant, increased in France, Sweden and Greece. Nevertheless, these data warrant attention and consideration. We cannot explain why the prevalence of thinness seems to have increased among in these countries, but possible reasons include: (i) sociocultural factors associated with standards of beauty, mainly in France where the first signs of thinness increasing had been found in 2002 by Rolland-Cachera et al.( 29 ) and where thinness is more highly valued by women than by those from other West European countries and being slender seems very desirable to them and there is a strong pressure to remain thin( 30 ); (ii) morphological changes during puberty; (iii) low levels of physical activity during leisure time, that a recent Swedish study( 34 ) has confirmed to be a predictor of thinness( 35 , 36 ); (iv) adolescent body dissatisfaction and unhealthy weight-control behaviours and dieting( 3 , 4 ) associated with media exposure to images of ideally thin models, repeatedly demonstrated experimentally in English-speaking Western countries and now confirmed by the first study investigating body image in Southern Europe among French and Italian women( 37 , 38 ). Finally if we were to speculate, the answer also could be the ‘household paradox’, because national policies targeted at controlling obesity and chronic diseases may have had undesirable effects on the thinnest individuals. Paradoxically, the presence of an underweight person together with an overweight individual in the same household underscores the continuing importance of undernutrition( 8 , 22 ). In this respect, nutrition interventions targeting ‘at-risk’ individuals should be cautioned against making recommendations that would alter household diets.
Our results show an overall decline in all grades of thinness, although we cannot conclude that thinness has steadily been reduced, year-on-year, but only that we observed a fluctuating pattern in prevalence like that found by other studies( 23 , 24 ). There is no geographical pattern in this trend and no obvious reason for it, but only some hypotheses to interpret the different direction of the prevalence of thinness in these countries v. the remaining countries in the present study. The mechanism behind the development of thinness is in fact relatively unknown in adolescents and is extremely complex( 24 ). Thus further work that monitors and explores this trend and these particular countries is warranted.
Some limitations of the study must be considered. The current results are based on self-reported data that could be subject to socially desirable reporting bias. However, students’ responses were anonymous and therefore participants had no reason to misreport their height or weight. A study has shown that the BMI based on self-reported data can produce lower prevalence estimates of overweight (preobesity and obesity) than those based on actual height and weight measurements( 39 ), while another has reported high accuracy for classification of youth as obese or non-obese based on self-reported data( 40 ). Furthermore, BMI based on self-reports has been found to be fairly reliable( 40 ) and suitable for identifying valid relationships in epidemiological studies( 40 , 41 ).
There was a large number of missing values for height and/or weight in these three HBSC surveys (about 10 % on average), with the percentage of missing values being high in some countries (43 % in Ireland, 31 % in Lithuania and 20 % in Israel); thus such countries were not included in the current analysis involving eleven countries where the data were available on >80 % of the sample surveyed.
Health problems associated with thinness have rarely been investigated in industrialized countries. There is a need for systematic longitudinal data to provide precise estimates of prevalence and trends for thinness and the presence of health-risk behaviours. Thus the results from the current study add important information on this issue and suggest wide variation in prevalence and trends in thinness across nations. These findings suggest that thinness is also an important overlooked phenomenon in developed countries and deserves further study in a multinational context utilizing longitudinal data as much as possible. Such work would increase understanding of the factors associated with thinness and could contribute to developing optimal preventive programmes and nutritional interventions for both overweight and thin persons.
Acknowledgements
Sources of funding: HBSC is an international study carried out in collaboration with WHO/EURO. Funding from national agencies and from an international subscription system provide financial support: national data collection is funded at national level; international data file production and management are supported by national funding; WHO (as study partner) supports research dissemination, publication of international reports and the HBSC–WHO Forum for policy and practice. Conflicts of interest: The authors have no conflict of interest. Authors’ contributions: G.L. wrote the manuscript; M.V.G. designed the analysis with input from N.A.; S.R. carried out the statistical analysis; G.L., M.V.G., N.A., C.K. and C.V. contributed to drafting of the manuscript and its critical revision; all authors read and approved the final manuscript. Acknowledgements: HBSC is an international study carried out in collaboration with the WHO Regional Office for Europe. The international coordinator of the 1997/1998, 2001/2002 and 2005/2006 surveys was Candace Currie, University of Edinburgh, Scotland; and the databank manager was Oddrun Samdal, University of Bergen, Norway. A complete list of the participating researchers can be found on the HBSC website (www.HBSC.org).
References
- 1. Takimoto H, Yoshiike N, Kaneda F et al. (2004) Thinness among young Japanese women. Am J Public Health 94, 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kaneko K, Kiriike N, Ikenaga K et al. (1999) Weight and shape concerns and dieting behaviors among pre-adolescents and adolescents in Japan. Psychiatry Clin Neurosci 53, Suppl. 3, 365–371. [DOI] [PubMed] [Google Scholar]
- 3. Rozin P & Fallon A (1988) Body image, attitudes to weight, and misperceptions of figure preferences of the opposite sex: a comparison of men and women in two generations. J Abnorm Psychol 97, Suppl. 3, 342–345. [DOI] [PubMed] [Google Scholar]
- 4. Lawrie Z, Sullivan EA, Davies PS et al et al. (2006) Media influence on the body image of children and adolescents. Eat Disord 14, 355–364. [DOI] [PubMed] [Google Scholar]
- 5. Russell JD, Mira M, Allen BJ et al. (1994) Protein repletion and treatment in anorexia nervosa. Am J Clin Nutr 59, 98–102. [DOI] [PubMed] [Google Scholar]
- 6. Misra M, Aggarwal A, Miller KK et al et al. (2004) Effects of anorexia nervosa on clinical, hematologic, biochemical, and bone density parameters in community-dwelling adolescent girls. Pediatrics 114, 1574–1583. [DOI] [PubMed] [Google Scholar]
- 7. Lobstein T, Baur L & Uauy R (2004) Obesity in children and young people: a crisis in public health. Obes Rev 5, Suppl. 1, 4–104. [DOI] [PubMed] [Google Scholar]
- 8. Doak CM, Adair LS, Bentley M et al. (2005) The dual burden household and the nutrition transition paradox. Int J Obes (Lond) 29, 129–136. [DOI] [PubMed] [Google Scholar]
- 9. Florencio TM, Ferreira HS, de Franca AP et al et al. (2001) Obesity and undernutrition in a very low-income population in the city of Maceio, northeastern Brazil. Br J Nutr 86, 277–284. [DOI] [PubMed] [Google Scholar]
- 10. Cole TJ, Flegal KM, Nicholls D et al. (2007) Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 335, 194–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang Y, Monteiro C & Popkin BM (2002) Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr 75, 971–977. [DOI] [PubMed] [Google Scholar]
- 12. Kim E, Hwang JY, Woo EK et al. (2005) Body mass index cutoffs for underweight, overweight, and obesity in South Korean schoolgirls. Obes Res 13, 1510–1514. [DOI] [PubMed] [Google Scholar]
- 13. Oner N, Vatansever U, Sari A et al et al. (2004) Prevalence of underweight, overweight and obesity in Turkish adolescents. Swiss Med Wkly 134, 529–533. [DOI] [PubMed] [Google Scholar]
- 14. Baya Botti A, Perez-Cueto FJ, Vasquez Monllor PA et al et al. (2010) International BMI-for-age references underestimate thinness and overestimate overweight and obesity in Bolivian adolescents. Nutr Hosp 25, 428–436. [PubMed] [Google Scholar]
- 15. Khasnutdinova SL & Grjibovski AM (2010) Prevalence of stunting, underweight, overweight and obesity in adolescents in Velsk district, north-west Russia: a cross-sectional study using both international and Russian growth references. Public Health 124, 392–397. [DOI] [PubMed] [Google Scholar]
- 16. Rosario AS, Kurth BM, Stolzenberg H et al. (2010) Body mass index percentiles for children and adolescents in Germany based on a nationally representative sample (KiGGS 2003–2006). J Clin Nutr 64, 341–349. [DOI] [PubMed] [Google Scholar]
- 17. Bovet P, Kizirian N, Madeleine G et al. (2011) Prevalence of thinness in children and adolescents in the Seychelles: comparison of two international growth references. Nutr J 9, 10–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization (1995) Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Export Committee. WHO Technical Report Series no. 854. Geneva: WHO. [PubMed] [Google Scholar]
- 19. Kelishadi R, Ardalan G, Gheiratmand R et al. (2008) Thinness, overweight and obesity in a national sample of Iranian children and adolescents: CASPIAN Study. Child Care Health Dev 34, 44–54. [DOI] [PubMed] [Google Scholar]
- 20. World Health Organization (1995) Thin adults. In Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Export Committee. WHO Technical Report Series no. 854, pp. 354–374. Geneva: WHO; available at http://whqlibdoc.who.int/trs/WHO_TRS_854.pdf [PubMed]
- 21. Health Behaviour in School-aged Children World Health Organization Collaborative Cross-National Study (2010) HBSC International Protocol 2009/10. http://www.hbsc.org/methods/index.html
- 22. Martínez-Vizcaíno V, Sánchez López M, Moya Martínez P et al et al. (2009) Trends in excess weight and thinness among Spanish schoolchildren in the period 1992–2004: the Cuenca study. Public Health Nutr 12, 1015–1018. [DOI] [PubMed] [Google Scholar]
- 23. Tambalis KD, Panagiotakos DB, Kavouras SA et al et al. (2010) Eleven-year prevalence trends of obesity in Greek children: first evidence that prevalence of obesity is leveling off. Obesity (Silver Spring) 18, 161–166. [DOI] [PubMed] [Google Scholar]
- 24. Boddy LM, Hackett AF & Stratton G (2009) The prevalence of underweight in 9–10-year-old schoolchildren in Liverpool: 1998–2006. Public Health Nutr 12, 953–956. [DOI] [PubMed] [Google Scholar]
- 25. Currie C, Nic Gabhainn S & Godeau E, International HBSC Network Coordinating Committee (2009) The Health Behaviour in School-aged Children: WHO Collaborative Cross-National (HBSC) study: origins, concept, history and development 1982–2008. Int J Public Health 54, Suppl. 2, 131–139. [DOI] [PubMed] [Google Scholar]
- 26. Roberts C, François Y, Batista-Foguet J et al et al. (2000) Methods. In Health and Health Behaviour among Young People. WHO Policy Series: Health for Children and Adolescents, pp. 9–21 [C Currie, K Hurrelmann, W Settertobulte et al., editors]. Geneva: WHO. [Google Scholar]
- 27. Roberts C, Freeman J, Samdal O et al et al. ; International HBSC Network Coordinating Committee (2009) The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. Int J Public Health 54, Suppl. 2, 140–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. King A, Wold B, Smith CT et al. (1996) The Health of Youth. A Cross-National Survey. WHO Regional Publications European Series no. 69. Geneva: WHO. [PubMed] [Google Scholar]
- 29. Rolland-Cachera MF, Castetbon K, Arnault N et al. (2002) Body mass index in 7–9-year-old French children: frequency of obesity, overweight and thinness. Int J Obes Relat Metab Disord 26, Suppl. 12, 1610–1616. [DOI] [PubMed] [Google Scholar]
- 30. de Saint Pol T (2009) Evolution of obesity by social status in France, 1981–2003. Econ Hum Biol 7, 398–404. [DOI] [PubMed] [Google Scholar]
- 31. Drewnowski A & Specter S (2004) Poverty and obesity: the role of energy density and costs. Am J Clin Nutr 79, 6–16. [DOI] [PubMed] [Google Scholar]
- 32. Marques-Vidal P, Ferreira R, Oliveira JM et al et al. (2008) Is thinness more prevalent than obesity in Portuguese adolescents? Clin Nutr 27, 531–536. [DOI] [PubMed] [Google Scholar]
- 33. Villa I, Yngve A, Poortvliet E et al. (2007) Dietary intake among under-, normal- and overweight 9-and 15-year-old Estonian and Swedish schoolchildren. Public Health Nutr 10, 311–322. [DOI] [PubMed] [Google Scholar]
- 34. Elinder Schäfer L & Sundblom E & Rosendahl KI (2011) Low physical activity is a predictor of thinness and low self-rated health: gender differences in a Swedish cohort. J Adolesc Health 48, 481–486. [DOI] [PubMed] [Google Scholar]
- 35. Levin S, Lowry R, Brown DR et al. (2003) Physical activity and body mass index among US adolescents: youth risk behavior survey, 1999. Arch Pediatr Adolesc Med 157, 816–820. [DOI] [PubMed] [Google Scholar]
- 36. Kumar BN, Holmboe-Ottesen G, Lien N et al. (2004) Ethnic differences in body mass index and associated factors of adolescents from minorities in Oslo, Norway: a cross-sectional study. Public Health Nutr 7, 999–1008. [DOI] [PubMed] [Google Scholar]
- 37. Rodgers R & Chabrol H (2009) The impact of exposure to images of ideally thin models on body dissatisfaction in young French and Italian women. Encephale 35, 262–268. [DOI] [PubMed] [Google Scholar]
- 38. Perkins JM, Perkins HW & Craig DW (2010) Peer weight norm misperception as a risk factor for being over and underweight among UK secondary school students. Eur J Clin Nutr 64, 965–971. [DOI] [PubMed] [Google Scholar]
- 39. Himes HJ, Hannan P, Wall M et al. (2005) Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Ann Epidemiol 15, 272–278. [DOI] [PubMed] [Google Scholar]
- 40. Strauss RS (1999) Comparison of measured and self-reported weight and height in a cross-sectional sample of young adolescents. Int J Obes Relat Metab Disord 23, 904–908. [DOI] [PubMed] [Google Scholar]
- 41. Goodman E, Hinden BR & Khandelwal S (2000) Accuracy of teen and parental reports of obesity and body mass index. Pediatrics 106, 52–58. [DOI] [PubMed] [Google Scholar]


