Abstract
Myopericarditis associated with COVID-19 mRNA vaccines has been recognized as an uncommon adverse reaction, especially among young, healthy adult males. Eosinophilic myocarditis is a rare form of inflammation reflecting a hypersensitivity reaction following an inciting event commonly caused by drugs including vaccines. Eosinophilic myocarditis, a subtype of myocarditis, is characterized by eosinophilic myocardial infiltrates. It is usually accompanied by systemic eosinophilia in the form of a drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome and is rarely associated with myocyte fibrosis and/or necrosis. In this report, we present a case of biopsy-proven eosinophilic myocarditis in a 24-year-old male patient, likely secondary to COVID-19 mRNA vaccination. To our knowledge, this is the first report to describe delayed eosinophilic myocarditis following the COVID-19 mRNA vaccine. Clinicians should be aware of possible delayed presentation to avoid associated morbidity.
Introduction
Eosinophilic myocarditis is a rare inflammatory cardiomyopathy associated with other hypereosinophilic syndromes, hypersensitivity myocarditis, eosinophilic granulomatosis with polyangiitis, infections, malignancy, toxins, and idiopathic myocarditis. Driven by hypersensitivity reactions, hypersensitivity myocarditis can be caused by a wide array of inciting events. These may include antibiotics (36.5%), central nervous system agents (21.1%), vaccines including non-mRNA (7.7%), antitubercular drugs (1.9%), and a variety of other drugs (32.8%)1.
Of note, no clear histological pattern is associated with COVID-19 mRNA vaccination-induced myocarditis; nevertheless, eosinophilic myocarditis is a histological diagnosis and requires an endomyocardial biopsy. However, there are only a few case reports of biopsy proved COVID-19-mRNA-vaccination induced EM to date. Nevertheless, there is increasing evidence that COVID-19 mRNA vaccine-induced myocarditis is a hypersensitivity myocarditis with or without systemic eosinophilia2–14. To our knowledge, myocarditis following COVID-19 mRNA vaccination, with subsequent biopsy-proven eosinophilic myocarditis, has been reported in at least 12 patients15–23. Most reported cases describe COVID-19 mRNA vaccine-induced myocarditis occurring in the first 2 weeks following COVID-19 mRNA vaccination15–23. Our case highlights the first case of delayed hypersensitivity reaction consistent with EM 3 months after the second dose of the COVID-19 mRNA vaccine.
Case presentation
A healthy 24-year-old male with history of allergic rhinitis presented with chest tightness, dyspnea, and hemoptysis. He denied recent infections, travel, changes in diet, medications, or alcohol consumption and had two cats at home. He was exposed to his family with COVID-19 infection six months prior to presentation; however, he was asymptomatic and never tested positive. Notably, he received a second dose of the Moderna vaccine (mRNA-1273) three months before presentation.
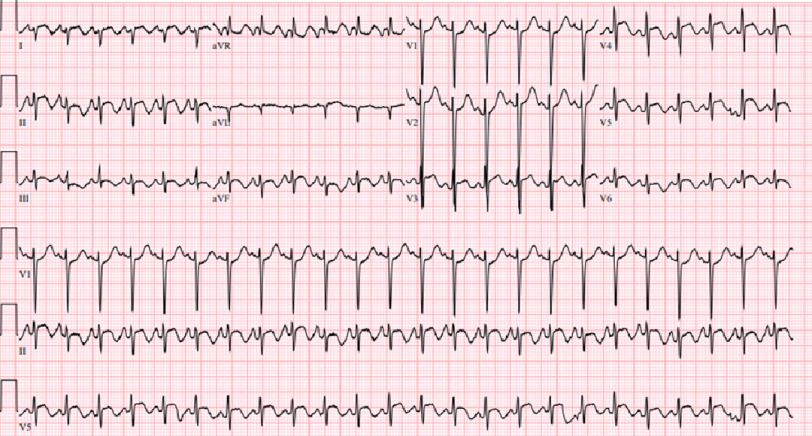
On arrival, the patient was hypoxic to 88% on room air, with a heart rate of 133 bpm, temperature 101.5 F, and blood pressure of 122/68 mmHg. On examination, he was in acute distress, diaphoretic, and tachycardic with a regular rhythm. Pulmonary auscultation revealed diffuse bilateral rhonchi, with the remainder of the examination being negative for rashes and lymphadenopathy. Electrocardiography (ECG) showed sinus tachycardia with diffuse ST-segment elevation and T-wave inversion (Figure 1).
Figure 1. ECG with diffuse ST-segment elevation and T-wave inversion.
Chest radiography revealed a clear lung. Initial troponins were 6629 ng/L (<19 ng/L), pro-BNP 5577 pg/ml ( ≤ 125 pg/ml), and creatine kinase (CK-MB) 1038 IU/L (25–125 IU/L). Other lab work included WBC 16.4 B/L (3.4–10.8x10E3/uL), with 70.6% neutrophils and 0.60 absolute eosinophils, BUN 15 mg/dL (6–20 mg/dL), creatinine 1.23 mg/dL (0.26–1.27 mg/dL), ALP 65 IU/L (29–92 IU/L), AST 137 IU/L (7–42 IU/L), ALT 47 IU/L (<45 IU/L), lactate 1.6 mmol/L.
Inflammatory markers were elevated at ESR 55 mm/h and CRP 8.70 mg/dL. Bedside echocardiography revealed a decreased ejection fraction of approximately 35–40%. In retrospect, he had an abnormal ECG consistent with sinus tachycardia with fusion complexes and T-wave inversions in the inferior and lateral leads two weeks before presentation, during regular physical examination for job application. During that visit, the echocardiogram showed normal LV function with EF 55–60%, and the patient was asymptomatic until the current presentation. He had normal ECGs approximately two years ago, without any known underlying heart disease.
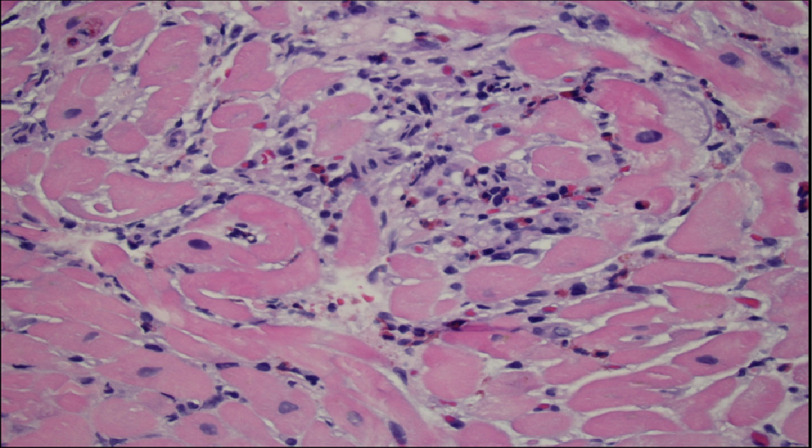
One day after the initiation of IV methylprednisone, a repeat echocardiogram showed a preserved EF of 45–50% with grade 3 diastolic dysfunction. Right heart catheterization was unremarkable, with normal filling pressures and cardiac index, excluding pulmonary embolism. An endomyocardial biopsy was performed, which showed myocarditis with prominent eosinophils (Figure 2). In the interim, due to normal heart filling pressures, suspicion of diffuse alveolar hemorrhage was high, with hemoptysis on presentation. Bronchoscopy ruled this out, and bronchioloalveolar fluid studies were negative.
Figure 2. Myocardial biopsy showing a focal inflammatory area composed predominantly of eosinophils (cells with red granular cytoplasm), admixed with lymphocytes and rare neutrophils.
An extensive workup was performed: infection (HIV, EBV, CMV, COVID, Coxsackie, Giardia, cryptosporidium, aspergillus, histoplasma, strongyloides, trichinella, quantiferon), autoimmune causes (IgE, ANA, ANCA), and hypersensitivity pneumonitis were all ruled out (Table 1). The likely etiology of eosinophilic myocarditis in our patient was a delayed hypersensitivity reaction following the COVID-19 mRNA vaccine. The patient was treated with a pulse dose of methylprednisone (1 g intravenously for three days.
Table 1. Laboratory tests for myocarditis workup.
| Laboratory test | Result |
|---|---|
| Lyme disease antibody | Negative |
| Syphilis antibody, Treponemal pallidum antibody cascade screening test | Negative |
| Mycobacterium TB gold | Negative |
| Chlamydia trachomatis TMA, rectal | Negative |
| HSV 1, 2 DNa | Negative |
| Parvovirus B19 IgM, IgG | Negative |
| Influenza A, B | Negative |
| HIV Ab/Ag | Negative |
| Hepatitis panel | Negative |
| SARs CoV-2 RT PCR | Negative |
| SARS-CoV-2 anti nucleocapsid antibody | Positive |
| SARS-CoV-2 anti spike glycoprotein antibody | Positive |
| Coxsackie B 1-6 antibody | Negative |
| Enterovirus RNA, real-time PCR | Negative |
| Respiratory pathogen panel | Negative |
| Varicella zoster IgG | Negative |
| Giardia Cryptosporidium TIA | Negative |
| Toxoplasma IgM/ IgG antibody | Negative |
| Cryptosporidium antigen | Negative |
| Histoplasma antigen candidate | Negative |
| trichinella antibody IgG | Negative |
| Strongyloides antibody IgG | Negative |
| Thermoactinomyces vulgaris IgG | Negative |
| Hypersensitivity pneumonitis screen | Negative |
| Asperigillus galactomannan antigen | Negative |
| Giardia lamblia | Negative |
| Neisseria gonorrhea TMA, rectal | Negative |
| Streptococcus pneumoniae antigen | Negative |
| Asperigillus fumigatus | Negative |
A repeat echocardiogram on the third day of steroid treatment showed normalization of EF to 60–65%, with an improvement in ECG findings. He was discharged on a steroid taper, 50 mg oral methylprednisone with a decrease in 10 mg dose every seven days for his eosinophilic myocarditis, along with lisinopril and carvedilol. At a follow-up visit a month later, the patient reported improvement in chest tightness and dyspnea. However, he also reported intermittent palpitations. His mobile outpatient telemetry showed a high burden of premature ventricular contraction (PVC) with transient ST-segment and T-wave abnormalities; hence, a loop recorder was placed for prolonged cardiac monitoring.
Discussion
We present a novel case of biopsy-proven EM following COVID-19 mRNA (Moderna) vaccination in a young, healthy male without systemic eosinophilia, highlighting the possibility of delayed hypersensitivity myocarditis following vaccination. Myocarditis is a diverse disease with varying clinical presentations attributed to different etiologies and therapeutic effects caused by an inflammatory reaction to the myocardium without ischemia. Viral infections, including SARS-CoV-2, are the most common triggers of myocarditis, whereas other etiologies may include drug reactions and vaccine exposure24,25.
Eosinophilic myocarditis (EM) is a rare type of inflammatory cardiomyopathy, characterized by eosinophilic infiltration of the myocardium. The incidence of EM is unclear thanks to non-specific diagnostic criteria and a reliance on endomyocardial biopsy for diagnosis. However, the mortality rate seems to be high, at approximately 20%26. Therefore, early recognition and prompt management of EM is vital for reducing the disease burden. Approximately one-third of EM cases are caused by hypersensitivity reactions, with the likely etiology being vaccines and medications26,27. There have been some reported cases of post-vaccination eosinophilic myocarditis after smallpox, diphtheria, tetanus, and pertussis vaccination28,29. Such non-mRNA vaccine-induced EM can also be observed following conjugate meningococcal C and hepatitis B vaccines in children15. Recently, reports of EM secondary to COVID-19 mRNA vaccination have been documented, with few fulminant cases15–23.
To date, myocarditis following a COVID-19 mRNA vaccine has been described in several cases. Among the few patients who underwent endomyocardial biopsy, approximately 11 cases of EM have been reported. The cases were reported following a Pfizer vaccine or for five cases, including our patient, after the Moderna vaccine. Among the reported cases following the Moderna vaccine, all were diagnosed within a week or two of receiving the COVID-19 mRNA vaccine15–23. In contrast, our patient received the vaccine approximately three months before the clinical presentation, indicating a possible delayed hypersensitivity reaction to the COVID-19 mRNA vaccine.
The clinical presentation of EM varies from the typical symptoms of chest pain, dyspnea, syncope, palpitations, and fever to non-specific symptoms, and the spectrum varies from mild asymptomatic disease to cardiogenic shock30,31. Historically, endomyocardial biopsy (EMB) has been the gold standard for diagnosing EM with a sensitivity of approximately 50%32. However, the utilization of EMB has decreased due to the widespread utility of MRI in diagnosing myocarditis and is used only in exceptional cases of rapid clinical deterioration, as in our patient. EM diagnosis depends on the histological pattern of inflammation, which can be revealed only by performing EMB33. In our case, myocarditis was suspected based on the clinical presentation supported by the elevated troponin, CK-MB, and echocardiography findings. However, due to rapid deterioration of the patient, coronary angiography with EMB was performed, which revealed EM. Our patient did not have any exposure to drugs or other vaccines, no evidence of infection, or autoimmune condition, supporting the etiology of the delayed hypersensitivity reaction from the COVID-19 vaccine. The treatment of EM secondary to COVID-19 mRNA vaccines remains unclear. Literature has shown steroids to be useful in cases of COVID-19 mRNA vaccine-induced myocarditis, as it is believed to be secondary to hypersensitivity reaction19.
Conclusion
Early onset hypersensitivity reactions in the form of myocarditis have been reported after administration of the COVID-19 mRNA vaccine. This case highlights the first delayed hypersensitivity reaction in the form of EM in a healthy patient months after administration of the CVOID-19 mRNA vaccine. Clinicians should be aware of the delayed nature of this association, as it may mimic other severe cardiac diseases. Appropriate evaluation and timely intervention are essential in cases of high suspicion for COVID-19 mRNA vaccine-associated myocarditis, as an aggressive strategy warrants survival, as in our case. Despite the reported adverse effects of COVID-19 vaccination, its benefits still outweigh the risks; therefore, vaccination is still recommended with close monitoring.
References
- 1.Kounis NG, Koniari I, Mplani V, Plotas P, Velissaris D. Hypersensitivity myocarditis and the pathogenetic conundrum of COVID 19 Vaccine Related Myocarditis. Cardiology. 2022 doi: 10.1159/000524224. doi: Epub ahead of print. PMID: 35316805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Istampoulouoglou I, Dimitriou G, Späni S, Christ A, Zimmermanns B, Koechlin S, Stoeckmann O, Winterhalder C, Marono D, Toma V, Leuppi-Taegtmeyer AB. Myocarditis and pericarditis in association with COVID-19 mRNA-vaccination: cases from a regional pharmacovigilance centre. Glob Cardiol Sci Pract. 2021;2021(3):e202118. doi: 10.21542/gcsp.2021.18. doi: PMID: 34805376; PMCID: PMC8587334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marshall M, Ferguson ID, Lewis P, Jaggi P, Gagliardo C, Collins JS, Shaughnessy R, Caron R, Fuss C, Corbin KJE, Emuren L, Faherty E, Hall EK, Di Pentima C, Oster ME, Paintsil E, Siddiqui S, Timchak DM, Guzman-Cottrill JA. Symptomatic acute myocarditis in 7 adolescents after Pfizer-BioNTech COVID-19 vaccination. Pediatrics. 2021;148(3):e2021052478. doi: 10.1542/peds.2021-052478. doi: Epub 2021 Jun 4. PMID: 34088762. [DOI] [PubMed] [Google Scholar]
- 4.Rosner CM, Genovese L, Tehrani BN, Atkins M, Bakhshi H, Chaudhri S, Damluji AA, de Lemos JA, Desai SS, Emaminia A, Flanagan MC, Khera A, Maghsoudi A, Mekonnen G, Muthukumar A, Saeed IM, Sherwood MW, Sinha SS, O’Connor CM, deFilippi CR. Myocarditis temporally associated with COVID-19 vaccination. Circulation. 2021;144(6):502–505. doi: 10.1161/CIRCULATIONAHA.121.055891. doi: Epub 2021 Jun 16. PMID: 34133885; PMCID: PMC8340723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abu Mouch S, Roguin A, Hellou E, Ishai A, Shoshan U, Mahamid L, Zoabi M, Aisman M, Goldschmid N, Berar Yanay N. Myocarditis following COVID-19 mRNA vaccination. Vaccine. 2021;39:3790–3793. doi: 10.1016/j.vaccine.2021.05.087. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larson KF, Ammirati E, Adler ED, Cooper LT Jr, Hong KN, Saponara G, Couri D, Cereda A, Procopio A, Cavalotti C, Oliva F, Sanna T, Ciconte VA, Onyango G, Holmes DR, Borgeson DD. Myocarditis after BNT162b2 and mRNA-1273 vaccination. Circulation. 2021;144(6):506–508. doi: 10.1161/CIRCULATIONAHA.121.055913. doi: Epub 2021 Jun 16. PMID: 34133884; PMCID: PMC8340725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ammirati E, Cavalotti C, Milazzo A, Pedrotti P, Soriano F, Schroeder JW, Morici N, Giannattasio C, Frigerio M, Metra M, Camici PG, Oliva F. Temporal relation between second dose BNT162b2 mRNA Covid-19 vaccine and cardiac involvement in a patient with previous SARS-COV-2 infection. Int J Cardiol Heart Vasc. 2021;34:100774. doi: 10.1016/j.ijcha.2021.100774. doi: Epub 2021 Mar 31. PMID: 33821210; PMCID: PMC8011690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bautista GJ, Pena OP, Bonilla Fernandez JA, Cardenes LA, Ramirez BL, Caballero DE. Acute myocarditis after administration of the BNT162b2 vaccine against COVID-19. Rev Esp Cardiol (Engl Ed) 2021 doi: 10.1016/j.rec.2021.04.005. doi: Published online April 27, 2021; S1885–5857(21)00133–X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mclean K, Johnson T. Myopericarditis in a previously healthy adolescent male following COVID-19 vaccination: a case report. Acad Emerg Med. 2021 doi: 10.1111/acem.14322. doi: Published online June 16, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Angelo T, Cattafi A, Carerj ML, Booz C, Ascenti G, Cicero G, Blandino A, Mazziotti S. Myocarditis after SARS-CoV-2 vaccination: a vaccine-induced reaction? Can J Cardiol. 2021 doi: 10.1016/j.cjca.2021.05.010. doi: Published online June 9, 2021; S0828–282X(21)00286–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albert E, Aurigemma G, Saucedo J, Gerson DS. Myocarditis following COVID-19 vaccination. Radiol Case Rep. 2021;16:2142–2145. doi: 10.1016/j.radcr.2021.05.033. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muthukumar A, Narasimhan M, Li QZ, Mahimainathan L, Hitto I, Fuda F, Batra K, Jiang X, Zhu C, Schoggins J, Cutrell JB, Croft CL, Khera A, Drazner MH, Grodin JL, Greenberg BM, Mammen PPA, Morrison SJ, de Lemos JA. In-depth evaluation of a case of presumed myocarditis after the second dose of COVID-19 mRNA vaccine. Circulation. 2021;144(6):487–498. doi: 10.1161/CIRCULATIONAHA.121.056038. doi: Epub 2021 Jun 16. PMID: 34133883; PMCID: PMC8340727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morimoto S, Kubo N, Hiramitsu S, Uemura A, Ohtsuki M, Kato S, Kato Y, Sugiura A, Miyagishima K, Mori N, Yoshida Y, Hishida H. Changes in the peripheral eosinophil count in patients with acute eosinophilic myocarditis. Heart Vessels. 2003;18:193–196. doi: 10.1007/s00380-003-0721-0. [DOI] [PubMed] [Google Scholar]
- 14.Fozing T, Zouri N, Tost A, Breit R, Seeck G, Koch C, Oezbek C. Management of a patient with eosinophilic myocarditis and normal peripheral eosinophil count: case report and literature review. Circ Heart Fail. 2014;7(4):692–4. doi: 10.1161/CIRCHEARTFAILURE.114.001130. doi: PMID: 25028351. [DOI] [PubMed] [Google Scholar]
- 15.Ameratunga R, Woon ST, Sheppard MN, Garland J, Ondruschka B, Wong CX, Stewart RAH, Tatley M, Stables SR, Tse RD. First identified case of fatal fulminant necrotizing eosinophilic myocarditis following the initial dose of the Pfizer-BioNTech mRNA COVID-19 vaccine (BNT162b2, Comirnaty): an extremely rare idiosyncratic hypersensitivity reaction. J Clin Immunol. 2022;42(3):441–447. doi: 10.1007/s10875-021-01187-0. doi: Epub 2022 Jan 3. PMID: 34978002; PMCID: PMC8720536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Otsuka K, Matsuo T, Ishimatsu T, Fukae A, Hamamoto T, Oku K, Ito M. A case of BNT162b2 COVID-19 vaccine-associated fulminant myocarditis in a very elderly woman. Clin Case Rep. 2022;10(9):e6161. doi: 10.1002/ccr3.6161. doi: PMID: 36093466; PMCID: PMC9445258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimura M, Hashimoto T, Noda E, Ishikawa Y, Ishikita A, Fujino T, Matsushima S, Ide T, Kinugawa S, Nagaoka K, Ushijima T, Shiose A, Tsutsui H. Fulminant necrotizing eosinophilic myocarditis after COVID-19 vaccination survived with mechanical circulatory support. ESC Heart Fail. 2022;9(4):2732–2737. doi: 10.1002/ehf2.13962. doi: Epub 2022 May 26. PMID: 35616026; PMCID: PMC9288782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parmar K, Mekraksakit P, Del Rio-Pertuz G, Sethi P, Motes A, Hughes M, Wischmeyer J, Carbajal L, Sosa EA. Myocarditis following COVID-19 mRNA vaccination. Proc (Bayl Univ Med Cent) 2021;35(2):209–213. doi: 10.1080/08998280.2021.1990743. doi: PMID: 35256821; PMCID: PMC8607537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ohtani K, Takahama S, Kato S, Higo T. Acute necrotizing eosinophilic myocarditis after COVID-19 vaccination. Eur Heart J. 2022;43(27):2640. doi: 10.1093/eurheartj/ehac239. doi: [DOI] [PubMed] [Google Scholar]
- 20.Frustaci A, Verardo R, Galea N, Lavalle C, Bagnato G, Scialla R, Chimenti C. Hypersensitivity myocarditis after COVID-19 mRNA vaccination. J Clin Med. 2022;11(6):1660. doi: 10.3390/jcm11061660. doi: PMID: 35329986; PMCID: PMC8949349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verma AK, Lavine KJ, Lin CY. Myocarditis after Covid-19 mRNA vaccination. The New England Journal of Medicine. 2021 doi: 10.1056/NEJMc2109975. doi: Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Witberg G, Barda N, Hoss S, Richter I, Wiessman M, Aviv Y, Grinberg T, Auster O, Dagan N, Balicer RD, Kornowski R. Myocarditis after Covid-19 vaccination in a large health care organization. N Engl J Med. 2021;385(23):2132–2139. doi: 10.1056/NEJMoa2110737. doi: Epub 2021 Oct 6. PMID: 34614329; PMCID: PMC8531986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choi S, Lee S, Seo JW, Kim MJ, Jeon YH, Park JH, Lee JK, Yeo NS. Myocarditis-induced Sudden Death after BNT162b2 mRNA COVID-19 vaccination in Korea: case report focusing on histopathological findings. J Korean Med Sci. 2021;36(40):e286. doi: 10.3346/jkms.2021.36.e286. doi: PMID: 34664804; PMCID: PMC8524235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, Martin I, Nordet P. Report of the 1995 World Health Organization/International Society and Federation of cardiology task force on the definition and classification of cardiomyopathies. Circulation. 1996;93(5):841–2. doi: 10.1161/01.cir.93.5.841. doi: PMID: 8598070. [DOI] [PubMed] [Google Scholar]
- 25.Sawalha K, Abozenah M, Kadado AJ, Battisha A, Al-Akchar M, Salerno C, Hernandez-Montfort J, Islam AM. Systematic review of COVID-19 related myocarditis: insights on management and outcome. Cardiovasc Revasc Med. 2021;23:107–113. doi: 10.1016/j.carrev.2020.08.028. doi: Epub 2020 Aug 18. PMID: 32847728; PMCID: PMC7434380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brambatti M, Matassini MV, Adler ED, Klingel K, Camici PG, Ammirati E. Eosinophilic myocarditis: characteristics, treatment, and outcomes. J Am Coll Cardiol. 2017;70(19):2363–2375. doi: 10.1016/j.jacc.2017.09.023. doi: PMID: 29096807. [DOI] [PubMed] [Google Scholar]
- 27.Séguéla PE, Iriart X, Acar P, Montaudon M, Roudaut R, Thambo JB. Eosinophilic cardiac disease: Molecular, clinical and imaging aspects. Arch Cardiovasc Dis. 2015;108(4):258–268. doi: 10.1016/j.acvd.2015.01.006. doi: [DOI] [PubMed] [Google Scholar]
- 28.Boccara F, Benhaiem-Sigaux N, Cohen A. Acute myopericarditis after diphtheria, tetanus, and polio vaccination. Chest. 2001;120:671–672. doi: 10.1378/chest.120.2.671. [DOI] [PubMed] [Google Scholar]
- 29.Cassimatis DC, Atwood JE, Engler RM, Linz PE, Grabenstein JD, Vernalis MN. Smallpox vaccination and myopericarditis: a clinical review. J Am Coll Cardiol. 2004;43(9):1503–10. doi: 10.1016/j.jacc.2003.11.053. doi: PMID: 15120802. [DOI] [PubMed] [Google Scholar]
- 30.Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, Friedrich MG, Klingel K, Lehtonen J, Moslehi JJ, Pedrotti P, Rimoldi OE, Schultheiss HP, Tschöpe C, Cooper LT Jr, Camici PG. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail. 2020;13(11):e007405. doi: 10.1161/CIRCHEARTFAILURE.120.007405. doi: Epub 2020 Nov 12. PMID: 33176455; PMCID: PMC7673642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sheikh H, Siddiqui M, Uddin SMM, Haq A, Yaqoob U. The clinicopathological profile of eosinophilic myocarditis. Cureus. 2018;10(12):e3677. doi: 10.7759/cureus.3677. doi: Published 2018 Dec 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rizkallah J, Desautels A, Malik A, Zieroth S, Jassal D, Hussain F, Cordova F. Eosinophilic myocarditis: two case reports and review of the literature. BMC Res Notes. 2013;6:538. doi: 10.1186/1756-0500-6-538. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gannon MP, Schaub E, Grines CL, Saba SG. State of the art: evaluation and prognostication of myocarditis using cardiac MRI. J Magn Reson Imaging. 2019;49(7):e122–e131. doi: 10.1002/jmri.26611. doi: Epub 2019 Jan 13. PMID: 30637834. [DOI] [PubMed] [Google Scholar]