Abstract
BACKGROUND
Institutions across the world have observed a decrease in the incidence of preterm births during the coronavirus disease 2019 pandemic. The reason for this reduction remains unknown.
OBJECTIVE
We sought to explore potential causes for the decrease in preterm births by exploring the following 3 hypotheses: (1) do women who are more likely to be able to work from home incur less physical/or emotional stress resulting in longer gestation? (2) Does the effect of the coronavirus disease 2019 pandemic on the incidence of preterm births vary by race? (3) Is this change provider driven?
STUDY DESIGN
Using a retrospective cohort of all singleton deliveries at a single tertiary care center, we compared the deliveries for the period before the coronavirus disease 2019 pandemic (January 1, 2018–January 31, 2020) with those occurring during the pandemic (April 1, 2020–October 27, 2020). Comparisons between the period before and during the pandemic were made using Pearson chi-square or t tests as appropriate. The overall incidence of preterm birth, defined as delivery at <37 weeks’ gestation, was analyzed and then further classified into spontaneous or indicated preterm births. The population was then stratified by the following categories: (1) insurance type and neighborhood disadvantage; (2) race; and (3) provider type. The provider type was classified as delivery occurring within an outpatient care facility, a clinic that provides prenatal care to those eligible for medical assistance, or a nonoutpatient care facility.
RESULTS
In a population of 17,687 pre–coronavirus disease 2019 deliveries, and 5396 deliveries occurring during the coronavirus disease 2019 pandemic, there was a significant decrease in the overall incidence of preterm births (11.1 vs 10.1%; P=.039). Both spontaneous and indicated preterm deliveries decreased across the entire population. When stratified, decreases in the incidence of spontaneous preterm birth before vs during the coronavirus disease 2019 pandemic were limited to deliveries to women from more advantaged neighborhoods (most advantaged, 4.4 vs 3.8%; least advantaged, 7.2 vs 7.4%), white mothers (white, 5.6 vs 4.7%; black, 6.6 vs 7.1%), and those receiving care from nonoutpatient care providers (nonoutpatient care providers, 5.5 vs 4.8%; outpatient care providers, 6.3 vs 6.7%).
CONCLUSION
The incidence of preterm births has decreased during the coronavirus disease 2019 pandemic. Decreases in the rate of spontaneous preterm births were limited to deliveries to white women, living in more advantaged neighborhoods, and deliveries at nonoutpatient care facilities. The coronavirus disease 2019 response regulations may have benefited women with more indicators of advantage disproportionately more.
Key words: coronavirus, disparities, regulations, spontaneous preterm birth
AJOG MFM at a Glance.
Why was this study conducted?
This study explored potential causes for the decrease in the incidence of preterm births (PTBs) during the coronavirus disease 2019 (COVID-19) pandemic through stratification.
Key findings
A decrease in the incidence of PTBs occurred across the entire study population. When evaluating subpopulations, decreases in spontaneous PTBs were limited to women with more indicators of advantage.
What does this add to what is known?
This study not only confirms a decrease in the incidence of PTBs during COVID-19, but further provides the opportunity to assess the differential impact of the COVID-19 response regulations on subpopulations.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has affected specific populations across the globe in a variety of unexpected ways. In the obstetrical realm, there has been an unanticipated decrease in the incidence of preterm births (PTBs) both in the United States1 and internationally.2, 3, 4, 5, 6
Although the decrease in PTBs is interesting and critical for public health, the cause of the decreased incidence is unknown. PTB is clinically and mechanistically heterogeneous and, owing to this complexity, only a limited number of prevention strategies has been proposed. Exploring the effects of the care environment during the COVID-19 pandemic has the potential to identify opportunities for prevention.
The first case of COVID-19 in Pennsylvania was confirmed on March 6, 2020. Subsequently, a statewide shutdown order was enacted, requiring residents to begin social distancing and to close all nonessential businesses. At the University of Pittsburgh Medical Center (UPMC), protocols were enacted, and measures were taken to increase telemedicine opportunities for virtual care and to prepare the system for a potential COVID-19 surge. These necessary safety precautions impacted pregnant women in many ways. Thousands of home blood pressure monitors were disseminated to our population of pregnant women and the majority of routine prenatal care appointments were conducted via video assessment.
Both statewide and UPMC-specific COVID-19 responses were executed quickly, allowing little time for tailoring to distinct subpopulations. At our UPMC delivery hospital, we have access to a large clinical data warehouse, which captures the data of more than 11,000 deliveries annually. We are thus well poised to explore the potential contributors to the decrease in the incidence of PTBs during the COVID-19 pandemic.
To do so, we addressed the following 3 hypotheses: (1) do women who are more likely to be able to work from home incur less physical/or emotional stress, resulting in longer gestation? (2) Does the effect of COVID-19 on PTB vary by race? (3) Is the change provider driven? Stated otherwise, is the decrease in PTB iatrogenic and merely reflective of a trade-off between spontaneous and indicated PTB, and a consequence of provider behavior?
Materials and Methods
We analyzed a retrospective cohort of all singleton deliveries occurring at ≥20 weeks’ gestations at the UPMC Magee-Womens Hospital from January 1, 2018, to October 27, 2020. The Magee-Womens Hospital is the delivery hospital within the UPMC, the largest health system in Pennsylvania. This study was exempt from institutional review board approval because it was conducted under our institution's quality improvement initiative for clinical process assessment and improvement.
Using a clinical data warehouse, we captured both the prenatal and delivery characteristics documented in the electronic health records. Prenatal care was defined as any visit to a UPMC facility between the start of pregnancy, calculated using gestational age, and delivery. The prenatal nonstress test results and biophysical profiles were identified using Current Procedural Terminology codes. Each woman's address (Zone Improvement Plan [ZIP]+4) at the time of delivery was used to classify her neighborhood's area deprivation index (ADI).7 , 8
We defined the period before COVID-19 as January 1, 2018, to January 31, 2020; the period during the COVID-19 pandemic was defined as April 1, 2020, to October 27, 2020. February and March 2020 were excluded as a washout period because no cases were identified in Pennsylvania yet, but regulations were beginning to be rolled out over these 2 months.
Outcome
The gestational age at the time of delivery, calculated using a combination of the last menstrual period and updates from ultrasound measurements, is documented in the clinical data warehouse. Infants with missing gestational age data were excluded (∼1%). We further classified preterm delivery (<37 weeks’ gestation) into early (<34 weeks’ gestation) and very early (<28 weeks’ gestation) and indicated vs spontaneous. Delivery forms completed by the obstetrical staff were used to define inductions and indications for induction. Deliveries with “induced” documented as the cause of labor onset without premature rupture of membranes as the indication for induction were considered indicated. We further classified any preterm cesarean delivery with missing information about the labor onset as indicated. All others were assumed to be spontaneous. The “Induction Indication” field captured the reason for the induction.
Analysis
Because the effect of the COVID-19 pandemic is the exposure and cannot be modified, there were no true confounders for the relationship. We therefore chose to evaluate the effect of the pandemic period in subpopulations to explore whether different groups were affected differently by the COVID-19 responses and regulations. We tested the following 3 stratifications to explore our hypotheses: stratification according to (1) insurance and neighborhood disadvantage, (2) race, and (3) provider type.
Insurance at the time of delivery was classified as either commercial or public (Medicaid or Medicare). Women who indicated that they were self-paying were excluded (n=442). ADI is widely used in the study of health disparities as a measure of the economic and social disadvantage of neighborhoods across the United States.7 Using ADI, each neighborhood was ranked from 1 to 100 with 100 indicating the most disadvantaged areas.7 , 8 Race was self-reported at the time of delivery. Data stratification according to race was limited to black and white to assess the comparison between our 2 largest race groups. At our institution, outpatient care (OPC) clinic types are hospital- and neighborhood-based prenatal clinics that function under the Healthy Beginnings Plus program. Healthy Beginnings Plus is Pennsylvania's effort to assist pregnant women with low incomes, who are eligible for medical assistance (MA), to have a positive prenatal care experience. Healthy Beginnings Plus expands maternity services that can be reimbursed by the MA program. The intent of Healthy Beginnings Plus is to render services that meet women's psychosocial needs in addition to rendering traditional medical and obstetrical services. Federal legislation permits Pennsylvania to extend MA eligibility to pregnant women with family incomes of up to 185% of the federal poverty guidelines. Pregnant clients may elect to participate in Healthy Beginnings Plus or receive their prenatal care in the traditional MA system.
Comparisons between the periods before and during COVID-19 were made in each subgroup using Pearson chi-square and t tests as appropriate. As a sensitivity analysis, all the comparisons were repeated after excluding 120 neonatal deaths and then excluding 7 women who tested positive for COVID-19 during admission for delivery.
Results
Our retrospective cohort of 23,083 singleton deliveries comprised 17,687 deliveries that occurred before the pandemic (January 2018–January 2020) and 5396 deliveries that occurred during the pandemic (April 2020–October 2020). A total of 1454 deliveries that occurred during the washout period were not included, along with 270 deliveries with missing data about the gestational age and 1 delivery that occurred at less than 20 weeks’ gestation.
Across all subgroups and stratifications, there were less biophysical profiles completed prenatally and an increase in the number of inductions during the COVID-19 period (Table 1, Table 2, Table 3, Table 4, Table 5 ). The Figure displays the gestational age in weeks at the time of delivery for all deliveries. The notably higher percentage of deliveries at 39 weeks’ gestation during the COVID-19 period was likely caused by an increase in the number of elective inductions of labor aimed at controlling patient flow and in accordance with the' a randomized trial of induction vs expectant management procedures' (ARRIVE).
Table 1.
Delivery characteristics of singleton deliveries at Magee-Womens Hospital before and during the COVID-19 pandemic (n=23,083)a
| Demographics | Pre–COVID-19 regulations (January 1, 2018–January 31, 2020) (n=17,687) | During COVID-19 pandemic (April 1, 2020–October 27, 2020) (n=5396) | P valued |
|---|---|---|---|
| Self-reported race, n (%) Other White Black |
1800 (10.2) 12,246 (69.2) 3641 (20.6) |
536 (9.9) 3845 (71.3) 1015 (18.8) |
.011 |
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
10,642 (60.2) 6526 (36.9) 178 (1.0) 341 (1.9) |
3406 (63.1) 1851 (34.3) 38 (0.7) 101 (1.9) |
<.001 |
| Prenatal care, n (%) | 16,989 (96.1) | 5173 (95.9) | .54 |
| Prenatal NST, n (%) | 3536 (20.0) | 1158 (21.5) | .019 |
| Prenatal biophysical profile, n (%) | 3362 (19.0) | 835 (15.5) | <.001 |
| Last PNV with OPC clinic, n (%) | 3066 (17.3) | 786 (14.6) | <.001 |
| Cesarean delivery, n (%) | 5410 (30.6) | 1615 (29.9) | .36 |
| Obstetrician, gynecologist, or midwife attending, n (%) | 17,066 (96.5) | 5217 (96.7) | .50 |
| Outcomes, n (%) | |||
| PTB (<37 wk) | 1963 (11.1) | 545 (10.1) | .039 |
| EPTB (<34 wk) | 639 (3.6) | 169 (3.1) | .092 |
| VEPTB (<28 wk) | 176 (1.0) | 45 (0.8) | .29 |
| Indicated PTB | 959 (5.4) | 273 (5.1) | .30 |
| Spontaneous PTB | 1004 (5.7) | 272 (5.0) | .074 |
| Overall inductions | 6079 (34.4) | 2098 (38.9) | <.001 |
| Preterm induction indicationb Preeclampsia Gestational HTN GDM FGR |
237 (24.7) 21 (2.2) 11 (1.1) 21 (2.2) |
61 (22.3) 7 (2.6) 3 (1.1) 2 (0.7) |
.42 .71 .95 .12 |
| ADI, mean (SD)c | 57.6 (26.6) | 56.5 (26.4) | .014 |
ADI, area deprivation index; COVID-19, coronavirus disease 2019; EPTB, early preterm birth; FGR, fetal growth restriction; GDM, gestational diabetes mellitus; HTN, hypertension; NST, nonstress test; OPC, outpatient care; PNV, prenatal visit; PTB, preterm birth; SD, standard deviation; VEPTB, very early preterm birth.
February and March were considered a washout period and excluded
Percentage of preterm inductions
ADI is missing for 7% (n=1520) of deliveries
Pearson chi-square or 2-sample t test as appropriate.
Lemon. Differential decreases in spontaneous preterm birth during coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Table 2.
Delivery characteristics of singleton deliveries at Magee-Womens Hopital before and during the COVID-19 pandemic stratified according to insurance type (n=22,641)a
| Factor | Pre–COVID-19 regulations (January 1, 2018–January 31, 2020) | During COVID-19 pandemic (April 1, 2020–October 27, 2020) | P valueb |
|---|---|---|---|
| Commercial (n=14,048) | |||
| n | 10,642 | 3406 | |
| Self-reported race, n (%) Other White Black |
1193 (11.2) 8591 (80.7) 858 (8.1) |
344 (10.1) 2809 (82.5) 253 (7.4) |
.075 |
| Prenatal care, n (%) | 10,422 (97.9) | 3343 (98.2) | .43 |
| Prenatal NST, n (%) | 2660 (25.0) | 868 (25.5) | .57 |
| Prenatal biophysical profile, n (%) | 1894 (17.8) | 517 (15.2) | <.001 |
| Last PNV with OPC clinic, n (%) | 407 (3.8) | 131 (3.8) | .95 |
| Cesarean delivery, n (%) | 3232 (30.4) | 1044 (30.7) | .76 |
| Obstetrician, gynecologist, or midwife attending, n (%) | 10,467 (98.4) | 3325 (97.6) | .005 |
| PTB (<37 wk), n (%) | 910 (8.6) | 290 (8.5) | .95 |
| EPTB (<34 wk), n (%) | 276 (2.6) | 92 (2.7) | .73 |
| VEPTB (<28 wk), n (%) | 66 (0.6) | 21 (0.6) | .98 |
| Indicated PTB, n (%) | 445 (4.2) | 163 (4.8) | .13 |
| Spontaneous PTB, n (%) | 465 (4.4) | 127 (3.7) | .11 |
| Overall inductions, n (%) | 3679 (34.6) | 1372 (40.3) | <.001 |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
108 (24.3) 12 (2.7) 7 (1.6) 6 (1.3) |
39 (23.9) 3 (1.8) 1 (0.6) 1 (0.6) |
.93 .55 .36 .45 |
| ADI, mean (SD)d | 47.5 (24.3) | 47.3 (24.1) | .60 |
| Medicare or Medicaid (n=8593) | |||
| n | 6704 | 1889 | |
| Self-reported race, n (%) Other White Black |
555 (8.3) 3419 (51.0) 2730 (40.7) |
173 (9.2) 964 (51.0) 752 (39.8) |
.44 |
| Insurance, n (%) Medicaid Medicare |
6526 (97.3) 178 (2.7) |
1851 (98.0) 38 (2.0) |
.115 |
| Prenatal care, n (%) | 6278 (93.6) | 1750 (92.6) | .12 |
| Prenatal NST, n (%) | 824 (12.3) | 271 (14.3) | .018 |
| Prenatal biophysical profile, n (%) | 1415 (21.1) | 305 (16.1) | <.001 |
| Last PNV with OPC clinic, n (%) | 2604 (38.8) | 644 (34.1) | <.001 |
| Cesarean delivery, n (%) | 2112 (31.5) | 550 (29.1) | .047 |
| Obstetrician, gynecologist, or attending midwife, n (%) | 6280 (93.7) | 1795 (95.0) | .030 |
| PTB (<37 weeks), n (%) | 1000 (14.9) | 242 (12.8) | .022 |
| EPTB (<34 weeks), n (%) | 345 (5.1) | 72 (3.8) | .017 |
| VEPTB (<28 weeks), n (%) | 102 (1.5) | 23 (1.2) | .33 |
| Indicated PTB, n (%) | 492 (7.3) | 107 (5.7) | .012 |
| Spontaneous PTB, n (%) | 508 (7.6) | 135 (7.1) | .53 |
| Overall inductions, n (%) | 2278 (34.0) | 692 (36.6) | .032 |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
122 (24.8) 8 (1.6) 4 (0.8) 15 (3.0) |
21 (19.6) 4 (3.7) 2 (1.9) 1 (0.9) |
.26 .16 .32 .22 |
| ADI, mean (SD)d | 74.1 (21.6) | 73.8 (21.3) | .61 |
ADI, area deprivation index; COVID-19, coronavirus disease 2019; EPTB, early preterm birth; FGR, fetal growth restriction; GDM, gestational diabetes mellitus; HTN, hypertension; NST, nonstress test; OPC, outpatient care; PNV, prenatal visit; PTB, preterm birth; SD, standard deviation; VEPTB, very early preterm birth.
February and March were considered a washout period and excluded
Pearson chi-square or 2-sample t test as appropriate
Percentage of preterm inductions
ADI is missing for 7% (n=1520) of deliveries.
Lemon. Differential decreases in spontaneous preterm birth during coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Table 3.
Delivery characteristics of singleton deliveries at Magee-Womens Hospital before and during the COVID-19 pandemic stratified according to ADI tertile (n=21,563)a
| Factor | Pre–COVID-19 regulations(January 1, 2018–January 31, 2020) | During COVID-19 pandemic (April 1, 2020–October 27, 2020) | P valueb |
|---|---|---|---|
| ADI tertile 1 (1–52) | |||
| n | 7034 | 2163 | |
| Self-reported race, n (%) Other White Black |
844 (12.0) 5923 (84.2) 267 (3.8) |
222 (10.3) 1865 (86.2) 76 (3.5) |
.066 |
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
5902 (83.9) 970 (13.8) 32 (0.5) 130 (1.8) |
1851 (85.6) 266 (12.3) 3 (0.1) 43 (2.0) |
.050 |
| Prenatal care, n (%) | 6850 (97.4) | 2114 (97.7) | .36 |
| Prenatal NST, n (%) | 1745 (24.8) | 558 (25.8) | .35 |
| Prenatal biophysical profile, n (%) | 1246 (17.7) | 313 (14.5) | <.001 |
| Last PNV with OPC clinic, n (%) | 309 (4.4) | 74 (3.4) | .048 |
| Cesarean delivery, n (%) | 2071 (29.4) | 653 (30.2) | .51 |
| Obstetrician, gynecologist, or midwife attending, n (%) | 6887 (97.9) | 2118 (97.9) | .98 |
| PTB (<37 wk), n (%) | 565 (8.0) | 170 (7.9) | .80 |
| EPTB (<34 wk), n (%) | 161 (2.3) | 46 (2.1) | .66 |
| VEPTB (<28 wk), n (%) | 40 (0.6) | 14 (0.6) | .68 |
| Indicated PTB, n (%) | 259 (3.7) | 88 (4.1) | .41 |
| Spontaneous PTB, n (%) | 306 (4.4) | 82 (3.8) | .26 |
| Overall inductions, n (%) | 2346 (33.4) | 829 (38.3) | <.001 |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
56 (21.6) 5 (1.9) 3 (1.2) 4 (1.5) |
18 (20.5) 3 (3.4) 1 (1.1) 0 (0.0) |
.82 .42 .99 .24 |
| ADI, mean (SD) | 31.8 (13.2) | 31.9 (13.3) | .67 |
| ADI teritile 2 (53–75) | |||
| n | 4442 | 1385 | |
| Self-reported race, n (%) Other White Black |
410 (9.2) 3401 (76.6) 631 (14.2) |
139 (10.0) 1075 (77.6) 171 (12.3) |
.17 |
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
2690 (60.6) 1603 (36.1) 41 (0.9) 108 (2.4) |
870 (62.8) 476 (34.4) 7 (0.5) 32 (2.3) |
.26 |
| Prenatal care, n (%) | 4252 (95.7) | 1329 (96.0) | .71 |
| Prenatal NST, n (%) | 905 (20.4) | 300 (21.7) | .30 |
| Prenatal biophysical profile, n (%) | 838 (18.9) | 208 (15.0) | .001 |
| Last PNV with OPC clinic, n (%) | 672 (15.1) | 160 (11.6) | <.001 |
| Cesarean delivery, n (%) | 1373 (30.9) | 408 (29.5) | .31 |
| Obstetrician, gynecologist or midwife attending, n (%) | 4290 (96.6) | 1349 (97.4) | .13 |
| PTB (<37 wk), n (%) | 532 (12.0) | 140 (10.1) | .057 |
| EPTB (<34 wk), n (%) | 166 (3.7) | 46 (3.3) | .47 |
| VEPTB (<28 wk), n (%) | 51 (1.1) | 7 (0.5) | .035 |
| Indicated PTB, n (%) | 277 (6.2) | 75 (5.4) | .26 |
| Spontaneous PTB, n (%) | 255 (5.7) | 65 (4.7) | .14 |
| Overall inductions, n (%) | 1584 (35.7) | 576 (41.6) | <.001 |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
71 (25.6) 9 (3.2) 3 (1.1) 10 (3.6) |
18 (24.0) 2 (2.7) 1 (1.3) 1 (1.3) |
.77 .80 .86 .31 |
| ADI, mean (SD) | 64.1 (6.7) | 63.9 (6.7) | .26 |
| ADI tertile 3 (75–100) | |||
| n | 5130 | 1409 | |
| Self-reported race, n (%) Other White Black |
382 (7.4) 2264 (44.1) 2484 (48.4) |
118 (8.4) 614 (43.6) 677 (48.0) |
.51 |
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
1500 (29.2) 3475 (67.7) 88 (1.7) 67 (1.3) |
435 (30.9) 928 (65.9) 25 (1.8) 21 (1.5) |
.60 |
| Prenatal care, n (%) | 4879 (95.1) | 1317 (93.5) | .015 |
| Prenatal NST, n (%) | 688 (13.4) | 206 (14.6) | .24 |
| Prenatal biophysical profile, n (%) | 1069 (20.8) | 249 (17.7) | .009 |
| Last PNV with OPC clinic, n (%) | 1858 (36.2) | 478 (33.9) | .11 |
| Cesarean delivery, n (%) | 1631 (31.8) | 411 (29.2) | .060 |
| Obstetrician, gynecologist, or midwife attending, n (%) | 4844 (94.4) | 1333 (94.6) | .79 |
| PTB (<37 wk), n (%) | 715 (13.9) | 187 (13.3) | .52 |
| EPTB (<34 wk), n (%) | 251 (4.9) | 59 (4.2) | .27 |
| VEPTB (<28 wk), n (%) | 68 (1.3) | 17 (1.2) | .73 |
| Indicated PTB, n (%) | 347 (6.8) | 83 (5.9) | .24 |
| Spontaneous PTB, n (%) | 368 (7.2) | 104 (7.4) | .79 |
| Overall inductions, n (%) | 1767 (34.4) | 523 (37.1) | .062 |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
95 (27.4) 5 (1.4) 5 (1.4) 7 (2.0) |
21 (25.3) 2 (2.4) 0 (0.0) 1 (1.2) |
.70 .53 .27 .62 |
| ADI, mean (SD) | 88.5 (7.2) | 88.6 (7.1) | .50 |
ADI, area deprivation index; COVID-19, coronavirus disease 2019; EPTB, early preterm birth; FGR, fetal growth restriction; GDM, gestational diabetes mellitus; HTN, hypertension; NST, nonstress test; OPC, outpatient care; PNV, prenatal visit; PTB, preterm birth; SD, standard deviation; VEPTB, very early preterm birth.
February and March were considered a washout period and excluded
Pearson chi-square or 2-sample t test as appropriate
Percentage of preterm inductions.
Lemon. Differential decreases in spontaneous preterm birth during coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Table 4.
Delivery characteristics of singleton deliveries at Magee-Womens Hospital before and during the COVID-19 pandemic stratified according to race (n=20,748)a
| Factor | Pre–COVID-19 regulations(January 1, 2018–January 31, 2020) | During COVID-19 pandemic(April 1, 2020–October 27, 2020) | P valueb | |
|---|---|---|---|---|
| White (n=16,092) | ||||
| n | 12,247 | 3845 | ||
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
8591 (70.1) 3319 (27.1) 100 (0.8) 237 (1.9) |
2809 (73.1) 945 (24.6) 19 (0.5) 72 (1.9) |
.002 | |
| Prenatal care, n (%) | 11,837 (96.7) | 3714 (96.6) | .86 | |
| Prenatal NST, n (%) | 2857 (23.3) | 940 (24.4) | .15 | |
| Prenatal biophysical profile, n (%) | 2309 (18.9) | 577 (15.0) | <.001 | |
| Last PNV with OPC clinic, n (%) | 1021 (8.3) | 240 (6.2) | <.001 | |
| Cesarean delivery, n (%) | 3714 (30.3) | 1137 (29.6) | .37 | |
| Obstetrician, gynecologist, or midwife attending, n (%) | 11,958 (97.6) | 3763 (97.9) | .41 | |
| PTB (<37 wk), n (%) | 1323 (10.8) | 378 (9.8) | .087 | |
| EPTB (<34 wk), n (%) | 416 (3.4) | 115 (3.0) | .22 | |
| VEPTB (<28 wk), n (%) | 100 (0.8) | 28 (0.7) | .59 | |
| Indicated PTB, n (%) | 642 (5.2) | 196 (5.1) | .72 | |
| Spontaneous PTB, n (%) | 681 (5.6) | 182 (4.7) | .047 | |
| Overall inductions, n (%) | 4324 (35.3) | 1569 (40.8) | <.001 | |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
165 (25.7) 17 (2.6) 6 (0.9) 15 (2.3) |
43 (21.9) 7 (3.6) 2 (1.0) 2 (1.0) |
.29 .50 .91 .25 |
|
| ADI, mean (SD) | 51.5 (24.6) | 50.4 (24.2) | .020 | |
| Black (n=4656) | ||||
| n | 3641 | 1015 | ||
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
858 (23.6) 2653 (72.9) 77 (2.1) 53 (1.5) |
253 (24.9) 737 (72.6) 15 (1.5) 10 (1.0) |
.31 |
|
| Prenatal care, n (%) | 3506 (96.3) | 969 (95.5) | .23 | |
| Prenatal NST, n (%) | 342 (9.4) | 103 (10.1) | .47 | |
| Prenatal biophysical profile, n (%) | 772 (21.2) | 181 (17.8) | .019 | |
| Last PNV with OPC clinic, n (%) | 1784 (49.0) | 465 (45.8) | .073 | |
| Cesarean delivery, n (%) | 1135 (31.2) | 299 (29.5) | .30 | |
| Obestetrician, gynecologist, or midwife attending, n (%) | 3421 (94.0) | 953 (93.9) | .94 | |
| PTB (<37 wk), n (%) | 487 (13.4) | 130 (12.8) | .64 | |
| EPTB (<34 wk), n (%) | 174 (4.8) | 46 (4.5) | .74 | |
| VEPTB (<28 wk), n (%) | 63 (1.7) | 15 (1.5) | .58 | |
| Indicated PTB, n (%) | 247 (6.8) | 58 (5.7) | .22 | |
| Spontaneous PTB, n (%) | 240 (6.6) | 72 (7.1) | .57 | |
| Overall inductions, n (%) | 1232 (33.8) | 358 (35.3) | .39 | |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
62 (25.1) 4 (1.6) 4 (1.6) 6 (2.4) |
15 (25.9) 0 (0.0) 1 (1.7) 0 (0.0) |
.90 .33 .95 .23 |
|
| ADI, mean (SD) | 81.3 (19.0) | 81.2 (19.67) | .83 | |
ADI, area deprivation index; COVID-19, coronavirus disease 2019; EPTB, early preterm birth; FGR, fetal growth restriction; GDM, gestational diabetes mellitus; HTN, hypertension; NST, nonstress test; OPC, outpatient care; PNV, prenatal visit; PTB, preterm birth; SD, standard deviation; VEPTB, very early preterm birth.
February and March were considered a washout period and excluded
Pearson chi-square or 2-sample t test as appropriate
Percentage of preterm inductions.
Lemon. Differential decreases in spontaneous preterm birth during coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Table 5.
Delivery characteristics of singleton deliveries at Magee-Womens Hospital before and during the COVID-19 pandemic stratified according to provider clinic type (n=23,083)a
| Factor | Pre–COVID-19 regulations(January 1, 2018–January 31, 2020) | During COVID-19 pandemic(April 1, 2020–October 27, 2020) | P valueb |
|---|---|---|---|
| Non-OPC clinic (n=19,232) | |||
| n | 14,622 | 4610 | |
| Self-reported race, n (%) Other White Black |
1539 (10.5) 11,226 (76.8) 1857 (12.7) |
455 (9.9) 3605 (78.2) 550 (11.9) |
.13 |
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
10,235 (70.0) 3992 (27.3) 109 (0.7) 286 (2.0) |
3275 (71.0) 1219 (26.4) 26 (0.6) 90 (2.0) |
.37 |
| Prenatal NST, n (%) | 3526 (24.1) | 1157 (25.1) | .18 |
| Prenatal biophysical profile, n (%) | 2713 (18.6) | 712 (15.4) | <.001 |
| Cesarean delivery, n (%) | 4487 (30.7) | 1394 (30.2) | .56 |
| Obstetrician, gynecologist, or midwife attending, n (%) | 14,109 (96.5) | 4472 (97.0) | .092 |
| PTB (<37 wk), n (%) | 1580 (10.8) | 458 (9.9) | .094 |
| EPTB (<34 wk), n (%) | 528 (3.6) | 143 (3.1) | .10 |
| VEPTB (<28 wk), n (%) | 135 (0.9) | 38 (0.8) | .53 |
| Indicated PTB, n (%) | 770 (5.3) | 239 (5.2) | .83 |
| Spontaneous PTB, n (%) | 810 (5.5) | 219 (4.8) | .038 |
| Overall inductions, n (%) | 4974 (34.0) | 1808 (39.2) | <.001 |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
187 (24.3) 20 (2.6) 8 (1.0) 14 (1.8) |
50 (20.9) 7 (2.9) 3 (1.3) 2 (0.8) |
.28 .78 .78 .29 |
| ADI, mean (SD) | 53.4 (25.8) | 52.8 (25.4) | .17 |
| OPC clinic (n=3851) | |||
| n | 3065 | 786 | |
| Self-reported race, n (%) Other White Black |
260 (8.5) 1021 (33.3) 1784 (58.2) |
81 (10.3) 240 (30.5) 465 (59.2) |
.14 |
| Insurance, n (%) Commercial Medicaid Medicare Self-pay and other |
407 (13.3) 2534 (82.7) 69 (2.3) 55 (1.8) |
131 (16.7) 632 (80.4) 12 (1.5) 11 (1.4) |
.054 |
| Prenatal NST, n (%) | 10 (0.3) | 1 (0.1) | .35 |
| Prenatal biophysical profile, n (%) | 649 (21.2) | 123 (15.6) | <.001 |
| Cesarean delivery, n (%) | 923 (30.1) | 221 (28.1) | .27 |
| Obstetrician, gynecologist, or midwife attending, n (%) | 2957 (96.5) | 745 (94.8) | .028 |
| PTB (<37 wk), n (%) | 383 (12.5) | 87 (11.1) | .28 |
| EPTB (<34 wk), n (%) | 111 (3.6) | 26 (3.3) | .67 |
| VEPTB (<28 wk), n (%) | 41 (1.3) | 7 (0.9) | .31 |
| Indicated PTB, n (%) | 189 (6.2) | 34 (4.3) | .049 |
| Spontaneous PTB, n (%) | 194 (6.3) | 53 (6.7) | .67 |
| Overall inductions, n (%) | 1105 (36.1) | 290 (36.9) | .66 |
| Preterm induction indication,c n (%) Preeclampsia Gestational HTN GDM FGR |
50 (26.5) 1 (0.5) 3 (1.6) 7 (3.7) |
11 (32.4) 0 (0.0) 0 (0.0) 0 (0.0) |
.48 .67 .46 .25 |
| ADI, mean (SD) | 78.1 (19.7) | 79.2 (19.6) | .19 |
ADI, area deprivation index; COVID-19, coronavirus disease 2019; EPTB, early preterm birth; FGR, fetal growth restriction; GDM, gestational diabetes mellitus; HTN, hypertension; NST, nonstress test; OPC, outpatient care; PNV, prenatal visit; PTB, preterm birth; SD, standard deviation; VEPTB, very early preterm birth.
February and March were considered a washout period and excluded
Pearson chi-square or 2-sample t test as appropriate
Percentage of preterm inductions.
Lemon. Differential decreases in spontaneous preterm birth during coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Figure.
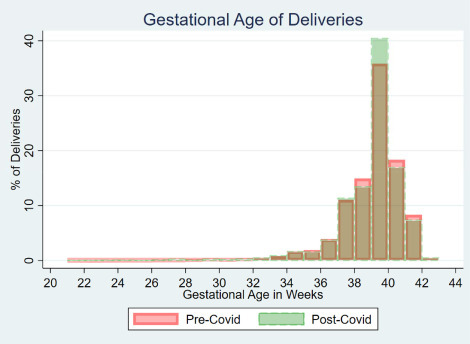
Gestational age at delivery
Singleton deliveries at Magee-Womens Hospital before and during the COVID-19 pandemic (n=23,083).
COVID-19, coronavirus disease 2019.
Lemon. Differential decreases in spontaneous preterm birth during coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Across the entire population, there was a decrease in the incidence of PTBs (11.1 vs 10.1%; P=.039), early PTBs (3.6 vs 3.1%; P=.092), and both indicated and spontaneous PTBs (Table 1). In the period during the COVID-19 pandemic, there were more deliveries to white women and commercially insured patients, with a corresponding reduction in deliveries at OPC clinic providers and in areas with lower ADI scores, indicating more deliveries to patients from more advantaged neighborhoods.
When stratifying by commercial (n=14,048; pre–COVID-19=10,642; during COVID-19=3406) vs public (n=8593; pre–COVID-19=6704; during COVID-19=1889) insurance as a surrogate of socioeconomic status, there was no significant decrease in PTBs in the cohort of commercially insured deliveries despite a trend toward a reduction in spontaneous PTB (4.4 vs 3.7%; P=.11) (Table 2). In the Medicaid and Medicare population, there was a significant decrease in PTBs (14.9 vs 12.8%; P=.022), which was driven by indicated PTB (7.3 vs 5.7%; P=.017). The spontaneous PTB rate slightly decreased in the Medicaid and Medicare population (7.6 vs 7.1%; P=.53).
The ADI was classified into 3 equal groups with tertile 1 representing the most advantaged neighborhoods (ADI, 1–52) and tertile 3 including the most disadvantaged (ADI, 76–100). A total of 21,563 (T1=9197; T2=5827; T3=6539) were included in this analysis with exclusion of 1520 deliveries with missing data about the neighborhood ADI. Although the pattern of statistically insignificant decreases in PTBs overall was similar in the most and least disadvantaged neighborhoods, the most disadvantaged areas demonstrated an increase in spontaneous PTB (7.2 vs 7.4%; P=.79), whereas the more advantaged areas experienced a decrease (tertile 1, 4.4 vs 3.8%; P=.68; tertile 2, 5.7 vs 4.7%; P=.14) (Table 3).
The entire population comprised 16,092 deliveries to white women (pre–COVID-19=12,247; during COVID-19=3845) and 4656 to black women (pre–COVID-19=3641; during COVID-19=1015). The patterns for all types of PTBs were similar for each race, both demonstrating a decrease in overall PTBs (Table 4). However, white women demonstrated a significant decrease in spontaneous PTB (5.6 vs 4.7%; P=.047) as opposed to nearly equal rates in the black women before and during the pandemic (6.6 vs 7.1%; P=.57).
Finally, 19,232 deliveries were performed by non-OPC providers (pre–COVID-19=14,622; during COVID-19=4610) and 3851 deliveries were performed by OPC clinic providers (pre–COVID-19=3065; during COVID-19=786). When stratified by clinic type, the trends were consistent for each clinic type with statistically insignificant decreases in PTBs before and during the pandemic (Table 5). Similar to the trends observed for stratification by race, those delivering in non-OPC clinics had a marked decrease in spontaneous PTBs (5.5 vs 4.8%; P=.038), whereas the rate of spontaneous PTB at OPC clinics remained almost unchanged (6.3 vs 6.7%; P=.67).
The results were consistent when excluding 120 neonatal deaths that occurred before delivery discharge and when excluding the 7 deliveries of women who tested positive for COVID-19 during admission.
Discussion
Principal findings
The decrease in the incidence of births at <37 weeks’ gestation was consistent for all insurance types, neighborhood disadvantages, races, and provider clinic types. Interestingly, the trend of decreasing spontaneous PTBs, although not statistically significant, was limited to the more advantaged neighborhoods, white patients, and deliveries by non-OPC provider subpopulations. Black women, living in the most disadvantaged neighborhoods, or those who delivered at OPC providers demonstrated no change or increase in the rate of spontaneous PTB.
Results
Our findings are consistent with recent studies identifying a decrease in PTB in the United States during the COVID-19 pandemic (Table 6).1 The magnitude of the decreased incidence at our institution, UPMC Magee-Womens Hospital, which went from 11.1% before the pandemic to 10.1% during the pandemic, was similar to that reported for Thomas Jefferson University Hospital, which went from 12.6% before the pandemic to 9.9% during the pandemic1. These authors also demonstrated a similar decreasing trend in the incidence of both indicated and spontaneous PTB. Interestingly, a second study in the United States found a decrease in the incidence of spontaneous PTB that was similarly confined to white women.9 A third paper supporting this disparity, conducted in the Netherlands, observed that the reductions in PTBs were limited to neighborhoods with higher socioeconomic indicators.4 Of the studies that thus far found no significant reduction in PTBs, the first demonstrated a decrease in deliveries at <28 weeks2; the second examined a population of only 127 PTBs during the COVID-19 pandemic11; the third took place in Nepal, a dramatically different care environment, in which they experienced a 50% overall reduction in the number of deliveries at a hospital, which could have significantly impacted the results.10
Table 6.
Summary of literature to date evaluating PTB rates during the COVID-19 pandemic
| Study, year | Country | Pre–COVID-19 | During COVID-19 | Spont | Singletons | Method | Results | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Time frame(PTB/total) | Time frame(PTB/total) | |||||||
| Been et al,4 2020a | The Netherlands | March 9, 2010–July 16, 2019; X/1,010,152 |
March 9, 2020–July 16, 2020; X/56,720 |
No | Yes | Difference in difference approach. | Unadj OR, 0.84 (0.73–0.97) | Reductions in PTB, limited to neighborhoods of higher socioeconomic status. |
| Berghella et al,1 2020 | United States | March 1–July 31, 2019; 115/911; spontaneous: 59/911 |
March 1, 2020–July 31, 2020; 118/1197; spontaneous: 57/1197 |
Yes | No | Multivariate logistic regression. Adjusted for race or ethnicity. | Adj OR, 0.75 (0.57–0.99); spontaneous: adj OR, 0.75 (0.52–1.10) |
25% decrease in odds of PTB. No statistically significant difference in spontaneous PTB. |
| Handley et al,9 2020 | United States | March 1, 2018–June 30, 2019; 617/5907; spontaneous: 315/5907 |
March 1, 2020–June 30, 2020; 283/3007; spontaneous: 135/3007 |
Yes | Yes | Marginal effects models. Adjusted for birth month, age, parity, BMI, race or ethnicity, marital status, smoking and insurance status. Stratified by race. | Adj RD, −1.1 (−2.4 to 0.2); spontaneous: adj RD, −0.8 (−1.8 to 0.2) |
No significant decrease in overall PTB. Significant decrease in spontaneous PTB in white women only. [adjusted RD, −1.4 (−2.8 to −0.1)]. |
| Hedermann et al,2 2021 | Denmark | March 12, 2015–April 14, 2019; 1317/26,018 |
March 12, 2020–April 14, 2020; 249/5162 |
No | Yes | Prevalence proportion study. | Unadj OR, 0.95b | No significant decrease in overall PTB. Decrease in births at <28 wk (unadjusted OR, 0.09 [0.01–0.40]). |
| KC et al,10 2020 | Nepal | Jan. 1–March 20, 2020; 2125/13,189 |
March 21, 2020–May 30, 2020; 1342/7165 |
No | Yes | Adjusted for complication during admission, ethnicity, and maternal age. | Adj OR, 1.30 (1.20–1.40); unadju OR, 1.198 (1.113–1.125) |
Significant increase in overall PTB. Significant decline in births at a hospital. |
| Khalil et al,11 2020 | United Kingdom | Oct. 1, 2019–Jan. 31, 2020; 113/1655 |
Feb. 1, 2020–June 14, 2020; 127/1692 |
No | No | Mann-Whitney and Fisher's exact tests. | Unadj RD, −0.68 (−2.43 to 1.07) | No significant decrease in overall PTB. |
| Philip et al,3 2020 | Ireland | Jan. 1, 2001–April 30, 2019; 210/29,324 VLBW |
Jan. 1, 2020–April 30, 2020; 3/1381 VLBW |
No | No | Poisson regression analysis. | Rate ratio,c 3.77 (1.21–11.75) | Significant 73% decrease in the incidence of VLBW infants (used as a surrogate of PTB and gestational age). |
Adj, adjusted; COVID-19, coronavirus disease 2019; OR, odds ratio; PTB, preterm birth (<37 weeks’ gestation); RD, risk difference; spont, spontaneous; unadj, unadjusted; VLBW, very low birthweight.
Referring to a primary analysis using March 9, 2020, regulation cutoffs with 4-month follow-up. Crude counts of PTBs before and after March 9, 2020, are not available in this manuscript;
No confidence interval because OR was calculated by hand;
VLBW using 2020 as referent.
Lemon. Differential decreases in spontaneous preterm birth during coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
With a nearly 4-fold increase in the number of deliveries during the COVID-19 pandemic, our findings not only strengthen previous work that demonstrated a decrease in PTB, but also allow us to explore possible explanations through stratification.
Clinical implications
The decreased incidence of spontaneous PTB in only the white, advantaged populations addresses the above hypotheses that certain COVID-19 responses may be more likely to benefit those populations. Using the broad implementation of work-from-home mandates as an example, we speculate that the decreased stress of not commuting or not being exposed to other people and infections in the workplace toward the end of pregnancy is desirable. Assuming that women with more indicators of advantages are more likely to work from home, it is possible they are reaping these benefits disproportionately more.
Importantly, it is also possible that working from home leads to more emotional stress, particularly for those caring for a family while quarantined. Moreover, much of the extant literature encourages increased physical activity during pregnancy12 because it is not associated with an increased risk for preterm delivery.13 Thus, differences in leisure time or work-related physical activities are unlikely contributors to our observed effect.
As more births continue during the pandemic, the differential rates in these subpopulations more likely will become clearer.
Research implications
Regarding work-from-home policies, additional research with more accurate quantification of the employment requirements and the associated physical and emotional stress is needed. Our classifications are broad markers and may not truly reflect those with the ability to work from home, nor can we differentiate between physical vs emotional stressors.
We also propose assessing other stress-related obstetrical complications during the pandemic. Comorbidities like preeclampsia, anxiety, and depression can be evaluated as indicators of changes in stress levels that could be contributing to this PTB decline. The role of COVID-19 infection itself must also be explored because we only had 7 positive cases during delivery admission at our institution during the study period. Across the UPMC system, nearly 2000 patients were hospitalized after testing positive for COVID-19 during the study period; 57 of these were admitted to the Magee-Womens Hospital.
Strengths and limitations
A notable strength is our ability to employ an existing clinical data warehouse, but this has inherent limitations. First, the retrospective nature of the design prohibits us from establishing the causality of the association. We were also forced to rely on surrogates of advantage that were captured in the electronic health record, based on ZIP+4 and census tract level data. We also did not have access to fetal death and miscarriage rate data and therefore included only live births. The documentation and missingness of the measures used in this study did not vary for the period before and during the pandemic.
The shift in the racial composition of deliveries at our institution is also noteworthy. There is a slight trend toward more deliveries to white women than to black women over the 3-year period. This may reflect changes in the population demographics of the service area or use of other hospital networks. Importantly, this change would not impact our findings. Finally, some of our results may be redundant across strata because there is overlap and collinearity between subpopulations. Black women are more likely to be insured by Medicaid, live in more disadvantaged neighborhoods, and undergo delivery by an OPC provider. We included each stratification because the individual qualifiers may have had differential impacts. There are other factors, not directly represented in our dataset, that may have causal implications for our observed findings. For example, the issues associated with a more disadvantaged neighborhood could represent an effect of the associated phenomenon, such as greenspace access or environmental pollution.
Conclusions
The frequency of PTBs is decreasing during the COVID-19 pandemic. The decreases could not be attributed to provider behavior but could perhaps be attributed to COVID-19 responses that differentially benefit women who reside in more advantaged neighborhoods.
Footnotes
The authors report no conflict of interest.
The authors report no source of funding.
Cite this article as: Lemon L, Edwards RP, Simhan HN. What is driving the decreased incidence of preterm birth during the coronavirus disease 2019 pandemic? Am J Obstet Gynecol MFM 2021;XX:x.ex–x.ex.
References
- 1.Berghella V, Boelig R, Roman A, Burd J, Anderson K. Decreased incidence of preterm birth during coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hedermann G, Hedley PL, Bækvad-Hansen M, et al. Danish premature birth rates during the COVID-19 lockdown. Arch Dis Child Fetal Neonatal Ed. 2021;106:93–95. doi: 10.1136/archdischild-2020-319990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Philip RK, Purtill H, Reidy E, et al. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: a ‘natural experiment’ allowing analysis of data from the prior two decades. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-003075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Been JV, Burgos Ochoa L, Bertens LCM, Schoenmakers S, Steegers EAP, Reiss IKM. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health. 2020;5:e604–e611. doi: 10.1016/S2468-2667(20)30223-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meyer R, Bart Y, Tsur A, et al. A marked decrease in preterm deliveries during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol. 2021;224:234–237. doi: 10.1016/j.ajog.2020.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maeda Y, Nakamura M, Ninomiya H, Ogawa K, Sago H, Miyawaki A. Trends in intensive neonatal care during the COVID-19 outbreak in Japan. Arch Dis Child Fetal Neonatal Ed. 2020 doi: 10.1136/archdischild-2020-320521. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. 2018;378:2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Medicine, School of Medicine and Public Health, University of Wisconsin. Neighborhood Atlas. 2015. Available at: https://www.neighborhoodatlas.medicine.wisc.edu/. Accessed December 16, 2020.
- 9.Handley SC, Mullin AM, Elovitz MA, et al. Changes in preterm birth phenotypes and stillbirth at 2 Philadelphia Hospitals during the SARS-CoV-2 pandemic, March-June 2020. JAMA. 2021;325:87–89. doi: 10.1001/jama.2020.20991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.KC A, Gurung R, Kinney MV, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. 2020;8:e1273–e1281. doi: 10.1016/S2214-109X(20)30345-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khalil A, von Dadelszen P, Draycott T, Ugwumadu A, O'Brien P, Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.12746. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ACOG committee opinion no. 650: physical activity and exercise during pregnancy and the postpartum period. Obstet Gynecol. 2015;126:e135–e142. doi: 10.1097/AOG.0000000000001214. [DOI] [PubMed] [Google Scholar]
- 13.Di Mascio D, Magro-Malosso ER, Saccone G, Marhefka GD, Berghella V. Exercise during pregnancy in normal-weight women and risk of preterm birth: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2016;215:561–571. doi: 10.1016/j.ajog.2016.06.014. [DOI] [PubMed] [Google Scholar]


