Abstract
Most patients undergo just one type of gender-affirming top surgery, but some will have a double-incision mastectomy after reduction mammaplasty. We describe a 46-year-old transgender man who requested a flatter chest after undergoing reduction mammoplasty the previous year. We also provide three considerations to guide surgical decision-making in this situation.
Keywords: Double-incision mastectomy, breast reduction, reduction mammaplasty, gender-affirming surgery, gender dysphoria, shared decision-making
Background
In the United States, an estimated 11,000 transgender patients undergo gender-affirming procedures annually [1]. Of these procedures, gender-affirming top surgery is the most commonly performed [2,3] and ranges from reduction mammaplasty with preservation of the nipple areolar complex (NAC), to mastectomy with and without NAC preservation [4,5]. Among the various mastectomy incision types, the double-incision is the most commonly performed; however, for patients with smaller chests and good skin quality, alternatives can be used [3].
Transgender patients who do not necessarily desire a flat chest seek reduction mammaplasty, whereas patients who desire a flat, masculine chest undergo a mastectomy [5]. Ideally, patients undergo just one type of top surgery, but some who undergo reduction mammaplasty later decide to undergo subsequent mastectomy. In this situation, little guidance is available to inform surgical decision-making. We present a case of a transgender man with a prior history of Wise-pattern reduction mammaplasty who underwent a double-incision mastectomy for persistent gender dysphoria and highlight important considerations.
Case
A 46-year-old transgender man with history of Wise-pattern reduction mammaplasty presented to our clinic requesting a flatter chest for persistent gender dysphoria. The patient met World Professional Association for Transgender Health (WPATH) criteria and had been consistently living in his chosen gender for several years. He received testosterone cypionate injections for two years. There was a significant family history of breast cancer in his maternal aunt, grandmother and cousin; his preoperative mammogram was unremarkable. He underwent reduction mammaplasty with a superior-based pedicle and Wise-pattern incision in 2014. Subsequent revision surgery with autologous fat grafting and areola resizing took place three months later at the same outside hospital.
Nine months after his reduction mammaplasty, the patient had persistent gender dysphoria due to chest contour deformity, ‘female-appearing’ breasts, and residual breast tissue. His residual breast tissue presented as an A-cup breast size with limited excess skin to perform a double-incision mastectomy. He also felt dysphoric about his Wise-pattern scars and sought to have double-incision scars. The decision was thus made to perform a double-incision mastectomy with free nipple grafts to revise the chest contour deformity and achieve a flat chest. The preoperative markings and intraoperative techniques of the double-incision mastectomy were done in accordance with the senior author’s published steps [6].
At his one and two-week follow-up appointments, the patient was happy with his results. He later underwent an in-office procedure to revise small bilateral ‘dog ears’ at the lateral chest, larger left nipple and right inferior lateral chest concavity. Four years after his mastectomy, the patient returned for another in-office revision of a small dog ear on the right lateral chest. The patient was pleased with his outcome and had no additional concerns.
Discussion
Mastectomy after a Wise-pattern mammaplasty for gender dysphoria was described in a case series of five patients who had a history of either a concentric circular or Wise-pattern reduction mammaplasty who later underwent subsequent mastectomy [7]. The reasons for undergoing the initial reduction mammaplasty included prior gender identification as nonbinary that later changed to male with desire for a more masculine chest, not being aware of a subcutaneous mastectomy as an option, and desire to preserve nipple sensation [7]. There were no hematomas, seromas, or NAC necrosis after an average of 12 months of follow-up. One patient required revision for a painful right nipple at 11 months postoperatively. Although postoperative outcomes for the various mastectomy incision types were discussed, little surgical guidance was provided for the conversion of reduction mammaplasty to subcutaneous mastectomy.
In contrast, more studies have focused on this surgical transition for oncologic resection in cisgender women [8,9]. Staged oncologic reconstruction with nipple-sparing mastectomy can be performed for cisgender women with large or ptotic breasts [8,10]. This two-stage approach entails a reduction mammaplasty followed by nipple-sparing mastectomy and direct-to-implant reconstruction [10]. Previous outcome studies of this two-stage approach show low complication rates and successful reconstruction [8–10]. However, we do not recommend it as the routine standard for gender-affirming top surgery. Ideally, only one chest surgery should be performed. Therefore, preoperative patient selection and shared decision-making are critical when deciding on the appropriate chest surgery. For patients unsure whether to pursue reduction mammaplasty or mastectomy, we suggest patients and providers understand the aesthetic challenges of having a mastectomy after a breast reduction.
There are several reasons why a transgender patient may choose to undergo a reduction mammaplasty versus a double-incision mastectomy. Patients who desire smaller, A-cup breasts and/or preservation of NAC sensation, may prefer breast reduction. NAC resizing may not be necessary for these patients. Nonbinary patients are more likely than transgender male patients to undergo reduction mammaplasty [5]. Patients who desire a flat chest and/or resizing of the NACs usually undergo double-incision mastectomy [11,12]. Our patient initially requested a double-incision mastectomy, but was only offered reduction mammaplasty. Although gender-affirming top surgery, such as the double-incision mastectomy, was less common than reduction mammaplasty in earlier years [10], as the demand for gender-affirming top surgery increases, more surgeons will become experienced with the double-incision technique, enabling more patients to undergo double-incision mastectomy as a surgical option.
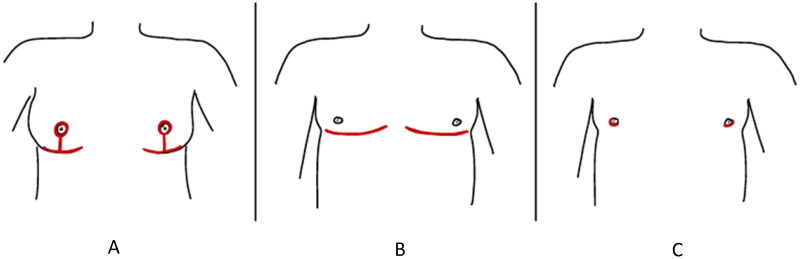
For patients with persistent gender dysphoria after Wise-pattern reduction mammaplasty, we highlight three considerations when transitioning to a mastectomy: (1) the amount of chest skin remaining after the breast reduction, (2) chest contour and (3) NAC position and size. To achieve an aesthetic reduction mammaplasty result, excess skin and tissue are usually excised [13]. However, with limited skin after a breast reduction, it can be challenging to place the final double-incision scar at what is considered to be the ideal location – the inferior border of the pectoralis major muscle (Figure 1). Instead, the scar usually results in a superior location.
Figure 1.
Mastectomy scar patterns. (A) Scars from a Wise-pattern reduction. (B) Scars from a double-incision mastectomy with free nipple grafts. (C) Scars from a periareolar mastectomy.
Chest contour irregularity also needs to be considered when deciding on which surgery to perform next. Theoretically, a periareolar incision, instead of a double-incision, could be performed for patients with limited chest skin and breast tissue. Previous studies have shown low complication rates for both surgical techniques [14,15]. However, the periareolar incision has a limited window of access, which is less reliable in correcting chest contour irregularities [7]. Although our patient presented with limited breast tissue, he felt dysphoric about his Wise- pattern scars and chest contour. Thus, a double-incision mastectomy seemed most appropriate to remove his prior scars and correct the contour irregularities, as contour revisions are usually more frequent with periareolar and concentric circular techniques [16].
Finally, in terms of NAC position and size, if the NAC is in the proper location on the chest with appropriate distance from the intramammary fold (IMF) and there is minimal residual breast tissue, then an IMF incision is another option for reconstruction. However, the IMF incision may be less ideal for patients who desire resizing of the NACs.
Although there are several options to achieve a flat chest after reduction mammaplasty, we recommend that patients and their providers understand the outcomes of each gender-affirming chest procedure before deciding on a chest surgery. Shared decision-making can help with appropriate patient selection.
Conclusions
This is a case report of a transgender man who underwent a double-incision mastectomy after a Wise-pattern reduction mammaplasty for persistent gender dysphoria. We illustrate several considerations when transitioning from reduction mammaplasty to mastectomy. With shared decision-making, optimal patient outcomes and satisfaction can be achieved.
Ethical approval
This study was approved by the University of California, San Francisco Institutional Review Board and conforms to the Declaration of Helsinki.
Funding Statement
No funding was received for this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.U.S. Sex Reassignment Surgery Market Report, 2020-2027 ; [cited 2021. Nov 1]. Available from: https://www.grandviewresearch.com/industry-analysis/us-sex-reassignment-surgery-market
- 2.Lane M, Ives GC, Sluiter EC, et al. Trends in gender-affirming surgery in insured patients in the United States. Plast Reconstr Surg Glob Open. 2018;6(4):e1738. doi: 10.1097/GOX.0000000000001738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ammari T, Sluiter EC, Gast K, et al. Female-to-male gender-affirming chest reconstruction surgery. Aesthet Surg J. 2019;39(2):150–163. doi: 10.1093/asj/sjy098. [DOI] [PubMed] [Google Scholar]
- 4.Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast Reconstr Surg. 2008;121(3):849–859. doi: 10.1097/01.prs.0000299921.15447.b2. [DOI] [PubMed] [Google Scholar]
- 5.McTernan M, Yokoo K, Tong W.. A comparison of gender-affirming chest surgery in nonbinary versus transmasculine patients. Ann Plast Surg. 2020;84(5S Suppl 4):S323–S328. doi: 10.1097/SAP.0000000000002254. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen A, Alcon A, Parmeshwar N, et al. A technique for optimizing symmetry in gender-affirming mastectomy. Plast Reconstr Surg Glob Open. 2021;9(6):e3622. doi: 10.1097/GOX.0000000000003622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salim A, Metz E, Constant JS, et al. Does previous breast reduction affect the outcome of gender-affirming subcutaneous mastectomy? Ann Plast Surg. 2018;80(5S Suppl 5):S279–S284. doi: 10.1097/SAP.0000000000001414. [DOI] [PubMed] [Google Scholar]
- 8.Frederick MJ, Lin AM, Neuman R, et al. Nipple-sparing mastectomy in patients with previous breast surgery: comparative analysis of 775 immediate breast reconstructions. Plast Reconstr Surg. 2015;135(6):954e–962e. doi: 10.1097/PRS.0000000000001283. [DOI] [PubMed] [Google Scholar]
- 9.Alperovich M, Tanna N, Samra F, et al. Nipple-sparing mastectomy in patients with a history of reduction mammaplasty or mastopexy: how safe is it? Plast Reconstr Surg. 2013;131(5):962–967. doi: 10.1097/PRS.0b013e3182865ad2. [DOI] [PubMed] [Google Scholar]
- 10.Gunnarsson GL, Bille C, Reitsma LC, et al. Prophylactic nipple-sparing mastectomy and direct-to-Implant reconstruction of the large and ptotic breast: is preshaping of the challenging breast a key to success? Plast Reconstr Surg. 2017;140(3):449–454. doi: 10.1097/PRS.0000000000003621. [DOI] [PubMed] [Google Scholar]
- 11.Salibian AA, Gonzalez E, Frey JD, et al. Tips and tricks in gender-affirming mastectomy. Plast Reconstr Surg. 2021;147(6):1288–1296. doi: 10.1097/PRS.0000000000007997. [DOI] [PubMed] [Google Scholar]
- 12.Etemad SA, Furuyama WM, Winocour JS.. Double incision mastectomy with free nipple graft for masculinizing chest wall surgery. Plast Reconstr Surg Glob Open. 2020;8(11):e3184. doi: 10.1097/GOX.0000000000003184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall-Findlay EJ, Shestak KC.. Breast reduction. Plast Reconstr Surg. 2015;136(4):531e–544e. doi: 10.1097/PRS.0000000000001622. [DOI] [PubMed] [Google Scholar]
- 14.Kamali A, Sigurjónsson H, Gran I, et al. Improved surgical outcome with double incision and free nipple graft in gender confirmation mastectomy. Plast Reconstr Surg Glob Open. 2021;9(7):e3628. doi: 10.1097/GOX.0000000000003628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rifkin WJ, Robinson IS, Kloer C, et al. Gender-affirming mastectomy: comparison of periareolar and double incision patterns. Plast Reconstr Surg Glob Open. 2022;10(5):e4356. doi: 10.1097/GOX.0000000000004356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kääriäinen M, Salonen K, Helminen M, et al. Chest-wall contouring surgery in female-to-male transgender patients: a one-center retrospective analysis of applied surgical techniques and results. Scand J Surg. 2017;106(1):74–79. doi: 10.1177/1457496916645964. [DOI] [PubMed] [Google Scholar]