Abstract
Background.
Repeated binge drinking is associated with reduced microvascular function. However, microvascular responses to pathophysiological stimulus such as high pressure as well as potential mechanisms that underlie binge-induced microvascular dysfunction are unknown. Therefore, using an ex vivo experimental model, we examined microvascular responses following a brief period of high intraluminal pressure in isolated arterioles from young adults who have a history of repeated binge drinking. In addition, we examined if the application of the endothelial nitric oxide synthase cofactor, tetrahydrobiopterin, would restore microvascular function in response to flow and high intraluminal pressure in young adult binge drinkers.
Methods.
Isolated subcutaneous adipose arterioles were obtained from young adult binge drinkers (BD; n=14), moderate drinkers (MODs; n=10), and alcohol abstainers (ABs; n=12; mean age: 23.7±0.5 yrs and body mass index: 23.4±0.4 kg m−2). Arteriolar flow-induced dilation (FID, pressure gradient: Δ10-100 cm H2O) was measured before and after acute high intraluminal pressure with and without tetrahydrobiopterin.
Results.
Before high pressure, FID at Δ60 and Δ100 cm H2O pressure gradient in BDs was 14% lower and 18% lower respectively than ABs (P<0.05), while MODs and ABs had similar FID across all pressure gradients (P≥0.2). After high pressure, FID in BDs was further reduced by 10% (P<0.0005) and this impairment was ameliorated by the treatment of tetrahydrobiopterin (4-26% higher, P<0.005). In contrast, FID after high pressure did not change in MODs and ABs (P≥0.5).
Conclusions.
Microvascular dysfunction in young adult binge drinkers may be exacerbated with acute pathophysiological stimulus. These binge-induced dysfunctions may be reversed by tetrahydrobiopterin, which suggests a role of oxidative stress and/or uncoupled endothelial nitric oxide synthase in binge drinking.
Keywords: alcohol use, cardiovascular risk, endothelial function, heavy episodic drinking, vascular function
Introduction
Repeated binge drinking in young adults is associated with signs of premature cardiovascular disease such as elevated blood pressure (Wellman et al., 2016, Piano et al., 2018), increased coronary artery calcification (Pletcher et al., 2005) and microvascular dysfunction (Bian et al., 2018). Microvascular dysfunction is defined as inadequate or abnormal microvascular vasodilator or constrictor responses to physiologic stimuli (e.g., flow, acetylcholine) and pathophysiologic stimuli (e.g., high pressure). Microvascular dysfunction precedes the development of several cardiovascular diseases including hypertension (Yannoutsos et al., 2014) and arises due to reduced production or bioavailability of nitric oxide (Gutterman et al., 2016).
Nitric oxide (NO), a potent vasodilator, is synthesized by the enzyme endothelial NO synthase (eNOS) and tetrahydrobiopterin (BH4) is a critical cofactor for eNOS production (Bendall et al., 2014). Reduced BH4 bioavailability, for example, during aging or disease states, contributes to reduced bioavailability of NO, thus decreasing NO-dependent vasodilation. Using different experimental approaches, others have demonstrated that increasing BH4 levels acutely ameliorates the impaired microvascular NO-dependent vasodilation in older adults (Stanhewicz et al., 2013, Stanhewicz et al., 2012) and in patients with atherosclerosis (Tiefenbacher et al., 2000). Reduced BH4 levels have been reported after alcohol consumption (Yoshimoto et al., 1997). Data from animal models demonstrate that alcohol administration (via intraperitoneal injection) reduces BH4 levels in brains of mice (Yoshimoto et al., 1997), while BH4 treatment ameliorates impaired NO-dependent dilation in arterioles isolated from rats chronically administered alcohol (liquid diet, 2-3 months) (Sun et al., 2001).
We have previously established that repeated binge drinking in young adults is associated with reduced microvascular flow-induced vasodilation (FID) which may be due to decreased bioavailability of NO (Bian et al., 2018). To the best of our knowledge, there have been no investigations examining mechanisms that may mediate the adverse effects of repeated binge drinking on microvascular function in young adults. In addition, there are no investigations examining responses of the microvasculature to a pathophysiologic stimulus such as high pressure. We hypothesized that exposure to high pressure would further reduce FID and that treatment of BH4 would reverse the FID in arterioles isolated from young adult binge drinkers (BDs). Therefore, using an ex vivo experimental model of isolated arterioles from young adults who have a history of repeated binge drinking, moderate alcohol drinking, and alcohol abstention, the first aim of this study was to examine microvascular function, measured as FID in isolated arterioles, following a pathophysiologic stress, that is, acute high intraluminal pressure. The second aim was to determine if the application of the cofactor BH4 improves microvascular function in response to flow and high intraluminal pressure in BDs.
Materials and Methods
Study design.
Using a cross-sectional design, participants were recruited from the community and a university campus. The study was conducted in accordance with the Declaration of Helsinki and was approved by the University of Illinois at Chicago Office of Protection of Research Subjects and Institutional Review Board. Written informed consent was obtained from all participants prior to study procedures.
Study participants.
Men and women (18-30 years) were screened based on self-reported medical history, physical examination, and fasting venous blood analysis. Exclusion criteria included: 1) body mass index ≥ 30 kg m−2; 2) total cholesterol > 230 mg dl−1 and/or low-density lipoprotein cholesterol > 160 mg dl−1; 3) blood pressure > 140/90 mm Hg; 4) history of diabetes, cardiovascular disease, or renal disease; 5) current or history of cigarette smoking and illicit drug use; 6) active infection (2 months prior); 7) a history of seizure disorder, cancer, and inflammatory disease (i.e., gout or rheumatoid); 8) pregnancy.
Study procedures.
Clinical measurements
Anthropometric measures (body weight, height, and waist and hip circumferences) were measured prior to obtaining fasting venous samples. Venous blood was collected into either serum separator tubes or tubes containing sodium citrate for measurement of total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, and glucose. Using the oscillometric technique (HEM-907XL, Omron Corporation, Japan), seated blood pressure was obtained, and we calculated the average of 3 blood pressure measures (with a 1-min interval between measures).
Alcohol use measurements
As described previously, we determined levels of alcohol intake and patterns of drinking using the alcohol intake questionnaire (AIQ), Alcohol Use Disorders Test (AUDIT), and dried blood spot phosphatidylethanol levels (Piano et al., 2015). Briefly, AIQ included questions on alcohol use frequency (e.g., how often), amount (e.g., how many drinks in one occasion, on a typical day, or over 2 hours), and history (e.g., how long in years) and was used for classifying alcohol use pattern (i.e., alcohol abstention and moderate or binge drinking). The AUDIT includes 10 questions (Babor, 2001), and total AUDIT and AUDIT-C (i.e., first three questions) scores were calculated to assess the risk of high-risk drinking.
Binge drinking was defined as the consumption of 5 or more standard drinks if male and 4 or more standard drinks if female, either on one occasion or within a two-hour period (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015). Binge drinkers (BDs) were defined as those who had at least 2 binge drinking episodes in the last month and a history of more than two years of repeated binge drinking. Moderate drinkers (MODs) were defined as follows: for males, the consumption of no more than 3 standard drinks per sitting with no more than 1-2 times per week, and for females, the consumption of no more than 2 standard drinks per sitting with no more than 1-2 times in a given week in the last five years. Alcohol abstainers (ABS) were defined as those that consumed no more than 1 standard drink per month in the last 2-3 years (and abstention could not be due to a medical illness or prior alcohol abuse). One standard drink contains 14 g of pure alcohol such as 12 oz. beer, 5 oz. wine, 1.5 oz. of 80-proof spirits, 8-9 oz. of malt liquor (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015).
Microvascular function assessments
Using previously described methods, microvascular function was determined by FID in isolated adipose arterioels (Bian et al., 2018, Robinson et al., 2017). Briefly, after a 12-hour fast and abstinence of caffeine, alcohol, and medication use, a gluteal subcutaneous adipose biopsy was obtained from participants. The adipose tissue was transferred and stored in HEPES buffer to dissect and isolate arterioles for microvascular function assessments by study personnel who were unaware of participant alcohol pattern. For BDs, the time from last binge drinking episode was a minimum of 48 hours.
Isolated arterioles were cannulated with glass micropipettes and pressurized (60 cm H2O or 44 mm Hg) in an organ perfusion chamber (37°C) circulated with KREBS solution (pH ~7.40) bubbled with air (5% CO2 and 21% O2) by a peristaltic pump for at least 30 minutes. Lumen diameters were measured by a video microscopy and image measurement system calibrated for horizontal measurements (model VIA-100, Boekeler) during responses to flow (pressure gradients of Δ10-Δ100 cm H2O) before and after high intraluminal pressure (150 cm H2O or 110 mm Hg) (Robinson et al., 2017) in the presence or absence of BH4 (10−5 M).
For each protocol, baseline diameter was recorded before pre-constricting the vessel to ~50% of baseline diameter with endothelin-1 (100 to 200 pM). The arterioles were exposed to each step increase in flow for 3 minutes, and the diameter was recorded. The flow was induced by simultaneously raising and lowering the reservoirs connected to two sides of arterioles to elicit a pressure gradient. At the end of each protocol, papaverine (10−4 M) was applied to induce endothelial-independent vasodilation. If the endothelin-1 pre-constriction was lower than 40% of baseline diameter, arterioles were not used for further experiments. In the high pressure experiments, high intraluminal pressure was maintained at 150 cm H2O (~135 mmHg) for 60 min followed by 15 min of re-equilibration at 60 cm H2O after which BH4 was added to the organ chamber 30 min prior to repeat FID measurements. FID at each pressure gradient was calculated as the percentage change from the endothelin-1 induced pre-constricted diameter relative to the baseline.
Materials.
Endothelin-1, papaverine, BH4, and other chemical reagents for buffer solutions were obtained from Sigma-Aldrich Corporation (St. Louis, MO) and Fisher Scientific (San Jose, CA).
Covariates.
Physical activity was determine by asking the question, “Do you have a usual exercise routine (y/n)?” and cardiorespiratory fitness was measured as peak oxygen consumption using a graded treadmill exercise test with Bruce protocol (Bruce et al., 1973). Based upon the completion of a diet questionnaire, we calculated the Dietary Approaches to Stop Hypertension (DASH) adherence score (Kim and Andrade, 2016) and assessed sleep quality using the Pittsburgh Sleep Quality (PSQ) Index (Buysse et al., 1989).
Statistics analyses.
Statistical analyses were conducted using IBM SPSS Statistics (Essentials, Version 22). Data are presented as mean±SE or n (%). Data normality and outliers were examined by scatter plots and the Shapiro-Wilk statistic. To examine group differences in participant characteristics, a one-way ANOVA was used for continuous variables, and χ2 was used for categorical variables. The nonparametric Kruskal–Wallis test was used for phosphatidylethanol levels, AUDIT and AUDIT-C score, internal diameter of adipose arterioles, and concentration of endothelin-1 among groups. To examine the effect of drinking pattern on FID, a two-way mixed ANOVA was used with a between-subject factor (BDs, MODs, and ABs) and a within-subject factor (pressure gradients of Δ10-Δ100 cm H2O). To examine the effect of high pressure/BH4 on FID within each group, two-way repeated-measures ANOVA with two within-subject factors: 1) presence or absence of high pressure/BH4 and 2) pressure gradients of Δ10-Δ100 cm H2O. When the interaction between the two factors was significant, then Bonferroni post hoc pairwise comparisons were performed. Main effect of high pressure/BH4 was examined if no interaction was found.
Results
Subject characteristics and alcohol use.
A total of 36 young adults (age: 23.7±0.5 yrs and body mass index: 23.4±0.4 kg/m2) were included and classified as ABs (n=12), MODs (n=10), and BDs (n=14). No differences were found in body mass index, waist and hip circumference, blood pressure, lipids, and glucose among the groups (Table 1). Phosphatidylethanol levels and scores of the AUDIT and AUDIT-C were significantly greater in BDs compared with MODs and ABs (Table 1).
TABLE 1.
Participant characteristics
| ABs (n=12) |
MODs (n=10) |
BDs (n=14) |
P | |
|---|---|---|---|---|
| Age (y) | 22±1 | 24±1 | 24±1 | 0.09 |
| Sex | 0.6 | |||
| Male | 7 (58) | 7 (70) | 7 (50) | |
| Female | 5 (42) | 3 (30) | 7 (50) | |
| Body weight (kg) | 62.6±2.7 | 70.6±3.8 | 71.2±2.5 | 0.08 |
| Body height (cm) | 166.9±2.3 | 169.0±3.0 | 173.8±1.8 | 0.09 |
| Body mass index (kg/m2) | 22.4±0.8 | 24.6±0.8 | 23.5±0.6 | 0.2 |
| Waist circumference (cm) | 78.2±2.5 | 83.7±2.4 | 81.1±1.9 | 0.3 |
| Waist to hip ratio | 0.87±0.02 | 0.91±0.02 | 0.87±0.02 | 0.2 |
| Systolic BP (mmHg) | 108±2 | 110±2 | 113±2 | 0.2 |
| Diastolic BP (mmHg) | 64±2 | 67±3 | 65±2 | 0.6 |
| Total cholesterol (mg/dL) | 156±10 | 167±10 | 159±11 | 0.8 |
| LDL cholesterol (mg/dL) | 85±8 | 98±8 | 85±8 | 0.5 |
| HDL cholesterol (mg/dL) | 52±2 | 53±4 | 60±5 | 0.3 |
| Triglycerides (mg/dL) | 88±10 | 77±13 | 66±8 | 0.3 |
| Glucose (mg/dL) | 89±1 | 93±3 | 87±2 | 0.1 |
| Peth (ng/mL) | 0±0 | 2.4±1.6 | 59.2±16.2* | <0.0005 |
| AUDIT score | 0.3±0.1 | 3.5±0.5† | 8.8±1.3* | <0.0005 |
| AUDIT-C score | 0.2±0.4 | 2.7±0.4† | 5.0±0.4* | <0.0005 |
| VO2peak (mL/min/kg) | 44.9±3.5 | 41.1±2.8 | 43.4±2.5 | 0.7 |
| DASH score | 1.5±0.2 | 2.1±0.4 | 2.3±0.2 | 0.1 |
| PSQ index | 4.5±0.5 | 5.3±0.6 | 5.1±0.4 | 0.6 |
Date are mean±SE or n (%). ABs, alcohol abstainers; AUDIT, Alcohol Use Disorders Identification Test; BDs, binge drinkers; BP, blood pressure; DASH, Dietary Approaches to Stop Hypertension; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MODs, moderate drinkers; Peth, phosphatidylethanol; PSQ, Pittsburgh Sleep Quality; VO2peak, peak oxygen consumption.
Statistically significant different from ABs and MODs.
Statistically significant different from ABs.
Nine ABs, 6 MODs, and 12 BDs reported engagement in a usual exercise routine (P=0.4). There was no difference among groups in peak oxygen consumption, the DASH score, and PSQ index (Table 1).
Microvascular function among ABs, MODs, and BDs.
FID before high intraluminal pressure
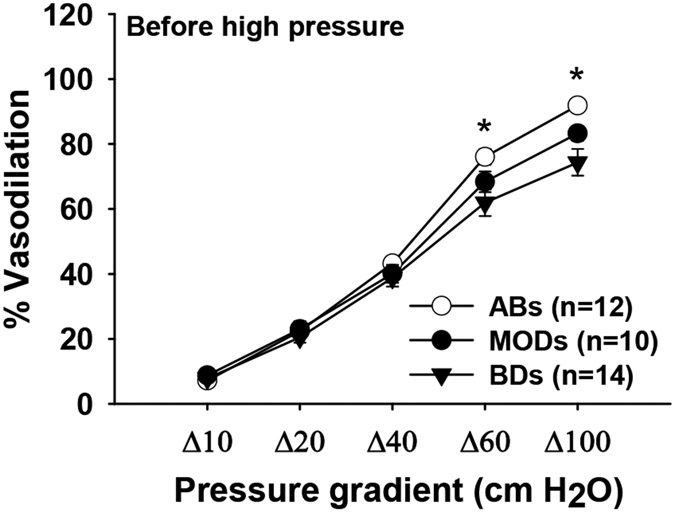
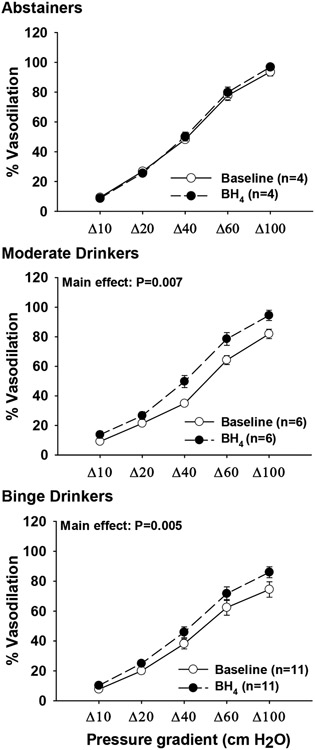
The internal diameter of adipose arterioles ranged from 48.6 to 312.5 μm with no differences among BDs, ABs, and MODs (P=0.07). Across all pressure gradients, no differences were found in FID between MODs and ABs (P≥0.2; Figure 1). At Δ60 cm H2O pressure gradient, vasodilation in BDs was 14% less than ABs (P=0.02), and at Δ100 cmH2O pressure gradient, vasodilation in BDs was 18% less than ABs (P=0.001; Figure 1). BH4 did not have effect on FID in ABs (P=0.5 for main effect) while it increased overall FID in MODs by 10 % and BDs by 7% (P≥0.005 for main effect; Figure 2). The dose of endothelin-1 used for the pre-constriction of arterioles was not different among the groups (BDs: 120±2 pM; MODs: 118±4 pM; ABs: 124±4 pM; P=0.3).
Fig. 1.
Baseline flow-induced dilation in arterioles from young adult alcohol abstainers (ABs), moderate drinkers (MODs), and binge drinkers (BDs). *P<0.05 for ABs vs. BDs.
Fig. 2.
Effect of tetrahydrobiopterin (BH4) on baseline flow-induced dilation in arterioles from young adult alcohol abstainers (ABs), moderate drinkers (MODs), and binge drinkers (BDs).
FID after high intraluminal pressure
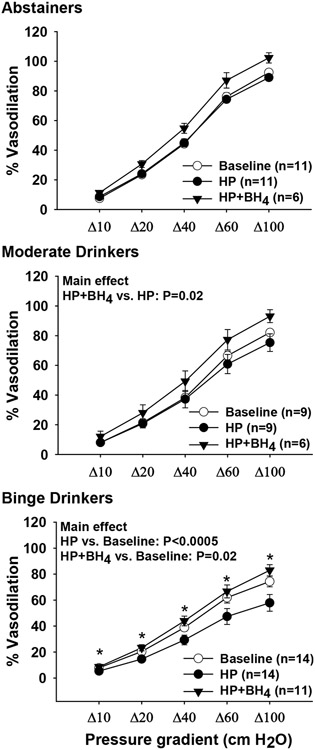
In ABs and MODs, no differences were found in FID responses before and after high pressure (P=0.6 and P=0.5 for main effect respectively; Figure 3, top and middle panels), while overall FID was reduced in BDs by 10% (P<0.0005 for main effect of high pressure; bottom panel). There was no effect of BH4 on FID after high pressure in ABs (P=0.1 for main effect of BH4; Figure 3, top panel), however, overall FID response to high pressure in MODs with BH4 increased by 9% (P=0.02 for main effect of BH4; Figure 3, middle panel). BH4 increased FID at all pressure gradients in BDs (4-26% higher, P<0.005 for post-hoc pairwise comparison at the pressure gradient; P=0.02 for interaction; Figure 3, bottom panel). The FID response in BDs with BH4 was greater than FID before high pressure (P=0.02 for main effect; Figure 3, bottom panel).
Fig. 3.
Effect of acute high intraluminal pressure (HP) and tetrahydrobiopterin (BH4) on FID in arterioles from young adult abstainers (ABs), moderate drinkers (MODs), and binge drinkers (BDs). Baseline data are used as a reference to compare with HP data and, except 1 in ABs and 1 in MODs, are the same as in Figure 1. * P<0.005 for after HP+BH4 vs. after HP at the pressure gradient.
Discussion
In this study, we investigated mechanisms underlying microvascular dysfunction as well as the responses to the pathophysiologic stimulus of high intraluminal pressure in arterioles isolated from young adults who have a history of repeated binge drinking, moderate alcohol drinking, and alcohol abstention. The major findings are: (1) acute high intraluminal pressure induced further FID impairments in BDs; (2) the impaired FID after acute high pressure in BDs was ameliorated by the treatment of BH4; (3) FID in MODs and ABs were similar and both remained unchanged after acute high pressure. Our findings suggest that microvascular responses to pathophysiological stimulus such as high pressure are altered in binge drinking and that binge-induced microvascular dysfunction is related to BH4 bioavailability.
Microvascular dysfunction is present in patients with cardiovascular diseases including hypertension (Antony et al., 1995, Esen et al., 2014, Farkas et al., 2004, Smith et al., 2011) and coronary artery disease (Phillips et al., 2007). In this study, all BD participants had no history of cardiovascular disease and systolic blood pressure within normal limits (<120 mmHg), yet microvascular function measured as FID in arterioles was reduced in BDs compared with ABs. Our findings suggest that microvascular dysfunction may occur at an early stage of binge drinking-induced pathophysiological changes and may potentially contribute to the development of hypertension and cardiovascular disease later in life. Consistent with this possibility, using both the new and old classifications for high blood pressure, Hayibor and colleagues recently reported binge drinking (e.g., consuming five or more drinks in a row) during adolescence and young adulthood was associated with a greater odds of high blood pressure in young adulthood (Hayibor et al., 2019). In the Coronary Artery Risk Development in Young Adults Study with a 15-year follow-up, binge drinking was associated with increased risks of coronary calcification (Pletcher et al., 2005).
This is the first study to demonstrate that the impaired FID in BDs was further reduced by exposing arterioles to high intraluminal pressure, while FID did not change following a high-pressure exposure in ABs. These novel findings suggest that after reduced microvascular function is present (e.g., in BDs), the response to acute physiological stressors (e.g., high pressure) leads to further reductions in microvascular function. This response in binge drinkers may represent an increased susceptibility of the microcirculation to dysfunction following acute stressors that raise blood pressure and may aggravate the progression to hypertension or cardiovascular disease (Yannoutsos et al., 2014). Further, these findings in adipose arteries may be applied to other microvasculature, e.g., coronary or retinal arteries, which are likely to experience high pressure during exertion. We have previously demonstrated that acute high intraluminal pressure increases superoxide in human adipose arterioles (Durand et al., 2014). Previous studies demonstrated that binge drinking increases reactive oxygen species (Tian et al., 2016, Yang et al., 2014, Gonzaga et al., 2014, Simplicio et al., 2016, Yogi et al., 2012). Therefore, it is possible that high intraluminal pressure aggravates the existing oxidative environment in BDs, which further reduces NO bioavailability and disturbs the compensatory mechanisms, leading to deceased FID.
Prior studies demonstrated that the treatment of BH4 restores the reduced NO-dependent vasodilation or NO bioavailability in microvasculature (Stanhewicz et al., 2013, Stanhewicz et al., 2012, Tiefenbacher et al., 2000, Sun et al., 2001). In agreement with previous studies, we show that the impaired FID before and after high pressure in arterioles from BDs were ameliorated by BH4. We have previously found no differences between ABs and BDs in microvascular responsiveness to sodium nitroprusside (Goslawski et al., 2013), suggesting the effect of binge drinking is endothelium-specific. Animal studies have demonstrated that BH4 decreases superoxide (Mayhan and Arrick, 2017, Franco Mdo et al., 2004) and increases eNOS activity (Franco Mdo et al., 2004), eNOS dimer-to-monomer ratios (eNOS coupling), and NO levels (Dikalova et al., 2016). While this study did not measure BH4, BH4:BH2 ratio, reactive oxygen species within the adipose/arterioles, and/or use eNOS inhibitor (LNAME) or stereoisomer BH4, future studies to further dissect the mechanisms by which BH4 improves microvascular dysfunction in binge drinking appears warranted.
We found no difference between MODs and ABs in arteriolar FID at baseline, as well as in systolic or diastolic blood pressure. To our knowledge, there are no studies that have examined the effects of repeated moderate drinking on microvascular function. Few studies have examined the effects of moderate or light drinking levels on blood pressure in young adults. In young adults (18-30 years) enrolled in the Coronary Artery Risk Development in Young Adults Study, Dyer et al. (1990) found that alcohol intake at moderate levels over the last 12 months (~1-2 drinks/day) was positively but not significantly associated with increases in blood pressure. In a cross-sectional study, Gillman et al. (1995) found that young adults (18-26 years of age) consuming no alcohol and <1 drink/day over the 30 days had a 4 mm Hg higher in systolic blood pressure compared with those who consumed 1 to < 2 drinks/day . In young adults (26-36 years) enrolled in the 2004-2006 follow-up of the Childhood Determinants of Adult Heath, Du et al. (2017) found systolic blood pressure was similar among non-drinkers (116±13 mmHg), light drinkers (>0-1 drink/day; 117±12 mmHg) and moderate drinkers (>1-2 drinks/day; 120±13 mmHg). Collectively, these findings suggest that low-to-moderate levels of alcohol consumption in young adults do not increase the risk for elevated blood pressure. Interestingly, while FID following high pressure did not change in both MODs and ABs, in MODs but not ABs it was increased with the treatment of BH4 suggesting that moderate drinking may alter the vasodilatory mechanisms following high pressure.
Our study had some strengths and limitations. Our ex vivo model to assess microvascular function allowed us to investigate the mechanisms of vascular dysfunction using pharmacologic and physiologic approaches. On the other hand, it was difficult to isolate enough vessels to examine all the potential mechanisms or measure protein and perform molecular biology while also obtaining tissue for corresponding measures of microvasculature reactivity. We used endothelin-1 for pre-constriction. In our experience, pre-constriction by potassium chloride reduces the response of human vessels to endothelium-dependent agonists or flow (Bosnjak et al., 2003, Phillips et al., 2007). Since high concentrations of potassium chloride act to prevent potassium channel opening and potassium channels are implicated in FID, the blockade of potassium channels would confound our results. Given the numbers of participants and vessels obtained, our study was not powerful enough to fully examine differences in microvascular function between men and women. We did not include in vivo measures such as brachial flow-mediated dilation in this current study, although microvascular NO-dependent dilation in isolated arterioles is correlated with brachial flow-mediated dilation (Dharmashankar et al., 2012). Microvascular function may also be affected by other factors, such as physical activity, fitness levels, diet, sleep quality, and depression. In this study, we found no differences in physical activity, fitness levels, diet, and sleep quality among our groups; however, we did not include quantitative measures of physical activity and assessments of depression.
We categorized young adult moderate and binge drinkers based upon self-report (via AIQ and AUDIT questionnaire) as well as objective measures (phosphatidylethanol levels). We included a moderate drinking group in order to test the idea that a ‘binge’ pattern is harmful (Piano et al., 2017). Ideally, having a moderate group that consumes the same amount of alcohol (e.g., g/week) comparable to the BD group, but on a daily basis, would more strongly establish if indeed a binge pattern is more harmful than consuming high doses and volumes of alcohol. Finally, our findings may not be generalizable to all age groups and socio-economic settings. On the other hand, our participants were recruited mainly from college campuses, given the current study’s high relevance to the college culture of binge drinking. Therefore, the study findings provide important insights into vascular changes in binge drinking and have important public health implications in early counseling on the risks of binge drinking in young adults to prevent microvascular dysfunction and potential development of hypertension.
In conclusion, moderate drinking seems to not provide benefits on the microvascular function measured as FID in arterioles from young adults. On the other hand, reduced FID is observed in young adults who repeatedly engage in binge drinking and can be further reduced by acute high intraluminal pressure and ameliorated by tetrahydrobiopterin. These findings suggest the vascular response in binge drinking is altered, which may be due to oxidative stress and/or uncoupled eNOS.
ACKNOWLEDGMENTS
We would like to thank all study participants for their time and participation. We would also like to thank Maryann Holtcamp, MS, APN and the rest of the staff at the Center for Clinical and Translational Science for their support with the study.
Grants:
National Institutes of Health grants R01HL130513 (SAP), R21AA024535 (SAP and MRP), and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR002003.
Footnotes
CONFLICTS OF INTEREST
None was declared.
REFERENCES
- ANTONY I, LEREBOURS G & NITENBERG A 1995. Loss of flow-dependent coronary artery dilatation in patients with hypertension. Circulation, 91, 1624–8. [DOI] [PubMed] [Google Scholar]
- BABOR TF H.-B. JC; SAUNDERS JB; MONTEIRO MG 2001. the Alcohol Use Disorders Identification Test : guidelines for use in primary health care 2nd ed ed. Geneva: World Health Organization. [Google Scholar]
- BENDALL JK, DOUGLAS G, MCNEILL E, CHANNON KM & CRABTREE MJ 2014. Tetrahydrobiopterin in cardiovascular health and disease. Antioxid Redox Signal, 20, 3040–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BIAN JT, PIANO MR, KOTLO KU, MAHMOUD AM & PHILLIPS SA 2018. MicroRNA-21 Contributes to Reduced Microvascular Function in Binge Drinking Young Adults. Alcohol Clin Exp Res, 42, 278–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BOSNJAK JJ, TERATA K, MIURA H, SATO A, NICOLOSI AC, MCDONALD M, MANTHEI SA, SAITO T, HATOUM OA & GUTTERMAN DD 2003. Mechanism of thrombin-induced vasodilation in human coronary arterioles. Am J Physiol Heart Circ Physiol, 284, H1080–6. [DOI] [PubMed] [Google Scholar]
- BRUCE RA, KUSUMI F & HOSMER D 1973. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J, 85, 546–62. [DOI] [PubMed] [Google Scholar]
- BUYSSE DJ, REYNOLDS CF 3RD, MONK TH, BERMAN SR & KUPFER DJ 1989. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res, 28, 193–213. [DOI] [PubMed] [Google Scholar]
- DHARMASHANKAR K, WELSH A, WANG J, KIZHAKEKUTTU TJ, YING R, GUTTERMAN DD & WIDLANSKY ME 2012. Nitric oxide synthase-dependent vasodilation of human subcutaneous arterioles correlates with noninvasive measurements of endothelial function. Am J Hypertens, 25, 528–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DIKALOVA A, ASCHNER JL, KAPLOWITZ MR, SUMMAR M & FIKE CD 2016. Tetrahydrobiopterin oral therapy recouples eNOS and ameliorates chronic hypoxia-induced pulmonary hypertension in newborn pigs. Am J Physiol Lung Cell Mol Physiol, 311, L743–L753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DU D, BRUNO R, DWYER T, VENN A & GALL S 2017. Associations between alcohol consumption and cardio-metabolic risk factors in young adults. Eur J Prev Cardiol, 24, 1967–1978. [DOI] [PubMed] [Google Scholar]
- DURAND MJ, PHILLIPS SA, WIDLANSKY ME, OTTERSON MF & GUTTERMAN DD 2014. The vascular renin-angiotensin system contributes to blunted vasodilation induced by transient high pressure in human adipose microvessels. Am J Physiol Heart Circ Physiol, 307, H25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DYER AR, CUTTER GR, LIU KQ, ARMSTRONG MA, FRIEDMAN GD, HUGHES GH, DOLCE JJ, RACZYNSKI J, BURKE G & MANOLIO T 1990. Alcohol intake and blood pressure in young adults: the CARDIA Study. J Clin Epidemiol, 43, 1–13. [DOI] [PubMed] [Google Scholar]
- ESEN F, ATA N & ESEN H 2014. Comparative study of the upper and lower limb skin blood flow control mechanisms in patients with essential hypertension. Anadolu Kardiyol Derg, 14, 3–8. [DOI] [PubMed] [Google Scholar]
- FARKAS K, KOLOSSVARY E, JARAI Z, NEMCSIK J & FARSANG C 2004. Non-invasive assessment of microvascular endothelial function by laser Doppler flowmetry in patients with essential hypertension. Atherosclerosis, 173, 97–102. [DOI] [PubMed] [Google Scholar]
- FRANCO MDO C, FORTES ZB, AKAMINE EH, KAWAMOTO EM, SCAVONE C, DE BRITTO LR, MUSCARA MN, TEIXEIRA SA, TOSTES RC, CARVALHO MH & NIGRO D 2004. Tetrahydrobiopterin improves endothelial dysfunction and vascular oxidative stress in microvessels of intrauterine undernourished rats. J Physiol, 558, 239–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GILLMAN MW, COOK NR, EVANS DA, ROSNER B & HENNEKENS CH 1995. Relationship of alcohol intake with blood pressure in young adults. Hypertension, 25, 1106–10. [DOI] [PubMed] [Google Scholar]
- GONZAGA NA, CALLERA GE, YOGI A, MECAWI AS, ANTUNES-RODRIGUES J, QUEIROZ RH, TOUYZ RM & TIRAPELLI CR 2014. Acute ethanol intake induces mitogen-activated protein kinase activation, platelet-derived growth factor receptor phosphorylation, and oxidative stress in resistance arteries. J Physiol Biochem, 70, 509–23. [DOI] [PubMed] [Google Scholar]
- GOSLAWSKI M, PIANO MR, BIAN JT, CHURCH EC, SZCZUREK M & PHILLIPS SA 2013. Binge drinking impairs vascular function in young adults. J Am Coll Cardiol, 62, 201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GUTTERMAN DD, CHABOWSKI DS, KADLEC AO, DURAND MJ, FREED JK, AIT-AISSA K & BEYER AM 2016. The Human Microcirculation: Regulation of Flow and Beyond. Circ Res, 118, 157–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HAYIBOR LA, ZHANG J & DUNCAN A 2019. Association of binge drinking in adolescence and early adulthood with high blood pressure: findings from the National Longitudinal Study of Adolescent to Adult Health (1994-2008). J Epidemiol Community Health, 73, 652–659. [DOI] [PubMed] [Google Scholar]
- KIM H & ANDRADE FC 2016. Diagnostic status of hypertension on the adherence to the Dietary Approaches to Stop Hypertension (DASH) diet. Prev Med Rep, 4, 525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAYHAN WG & ARRICK DM 2017. Tetrahydrobiopterin rescues impaired responses of cerebral resistance arterioles during type 1 diabetes. Diab Vasc Dis Res, 14, 33–39. [DOI] [PubMed] [Google Scholar]
- PHILLIPS SA, HATOUM OA & GUTTERMAN DD 2007. The mechanism of flow-induced dilation in human adipose arterioles involves hydrogen peroxide during CAD. Am J Physiol Heart Circ Physiol, 292, H93–100. [DOI] [PubMed] [Google Scholar]
- PIANO MR, BURKE L, KANG M & PHILLIPS SA 2018. Effects of Repeated Binge Drinking on Blood Pressure Levels and Other Cardiovascular Health Metrics in Young Adults: National Health and Nutrition Examination Survey, 2011-2014. J Am Heart Assoc, 7, e008733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PIANO MR, MAZZUCO A, KANG M & PHILLIPS SA 2017. Binge Drinking Episodes in Young Adults: How Should We Measure Them in a Research Setting? J Stud Alcohol Drugs, 78, 502–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PIANO MR, TIWARI S, NEVORAL L & PHILLIPS SA 2015. Phosphatidylethanol Levels Are Elevated and Correlate Strongly with AUDIT Scores in Young Adult Binge Drinkers. Alcohol Alcohol, 50, 519–25. [DOI] [PubMed] [Google Scholar]
- PLETCHER MJ, VAROSY P, KIEFE CI, LEWIS CE, SIDNEY S & HULLEY SB 2005. Alcohol consumption, binge drinking, and early coronary calcification: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol, 161, 423–33. [DOI] [PubMed] [Google Scholar]
- ROBINSON AT, FANCHER IS, SUDHAHAR V, BIAN JT, COOK MD, MAHMOUD AM, ALI MM, USHIO-FUKAI M, BROWN MD, FUKAI T & PHILLIPS SA 2017. Short-term regular aerobic exercise reduces oxidative stress produced by acute in the adipose microvasculature. Am J Physiol Heart Circ Physiol, 312, H896–H906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SIMPLICIO JA, HIPOLITO UV, VALE GT, CALLERA GE, PEREIRA CA, TOUYZ RM, TOSTES RC & TIRAPELLI CR 2016. Acute Ethanol Intake Induces NAD(P)H Oxidase Activation and Rhoa Translocation in Resistance Arteries. Arq Bras Cardiol, 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SMITH CJ, SANTHANAM L, BRUNING RS, STANHEWICZ A, BERKOWITZ DE & HOLOWATZ LA 2011. Upregulation of inducible nitric oxide synthase contributes to attenuated cutaneous vasodilation in essential hypertensive humans. Hypertension, 58, 935–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STANHEWICZ AE, ALEXANDER LM & KENNEY WL 2013. Oral sapropterin acutely augments reflex vasodilation in aged human skin through nitric oxide-dependent mechanisms. J Appl Physiol (1985), 115, 972–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STANHEWICZ AE, BRUNING RS, SMITH CJ, KENNEY WL & HOLOWATZ LA 2012. Local tetrahydrobiopterin administration augments reflex cutaneous vasodilation through nitric oxide-dependent mechanisms in aged human skin. J Appl Physiol (1985), 112, 791–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SUN H, PATEL KP & MAYHAN WG 2001. Tetrahydrobiopterin, a cofactor for NOS, improves endothelial dysfunction during chronic alcohol consumption. Am J Physiol Heart Circ Physiol, 281, H1863–9. [DOI] [PubMed] [Google Scholar]
- TIAN H, YE X, HOU X, YANG X, YANG J & WU C 2016. SVCT2, a potential therapeutic target, protects against oxidative stress during ethanol-induced neurotoxicity via JNK/p38 MAPKs, NF-kappaB and miRNA125a-5p. Free Radic Biol Med, 96, 362–73. [DOI] [PubMed] [Google Scholar]
- TIEFENBACHER CP, BLEEKE T, VAHL C, AMANN K, VOGT A & KUBLER W 2000. Endothelial dysfunction of coronary resistance arteries is improved by tetrahydrobiopterin in atherosclerosis. Circulation, 102, 2172–9. [DOI] [PubMed] [Google Scholar]
- WELLMAN RJ, VAUGHN JA, SYLVESTRE MP, O'LOUGHLIN EK, DUGAS EN & O'LOUGHLIN JL 2016. Relationships Between Current and Past Binge Drinking and Systolic Blood Pressure in Young Adults. J Adolesc Health, 58, 352–7. [DOI] [PubMed] [Google Scholar]
- YANG L, ROZENFELD R, WU D, DEVI LA, ZHANG Z & CEDERBAUM A 2014. Cannabidiol protects liver from binge alcohol-induced steatosis by mechanisms including inhibition of oxidative stress and increase in autophagy. Free Radic Biol Med, 68, 260–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YANNOUTSOS A, LEVY BI, SAFAR ME, SLAMA G & BLACHER J 2014. Pathophysiology of hypertension: interactions between macro and microvascular alterations through endothelial dysfunction. J Hypertens, 32, 216–24. [DOI] [PubMed] [Google Scholar]
- YOGI A, CALLERA GE, MECAWI AS, BATALHAO ME, CARNIO EC, ANTUNES-RODRIGUES J, QUEIROZ RH, TOUYZ RM & TIRAPELLI CR 2012. Acute ethanol intake induces superoxide anion generation and mitogen-activated protein kinase phosphorylation in rat aorta: a role for angiotensin type 1 receptor. Toxicol Appl Pharmacol, 264, 470–8. [DOI] [PubMed] [Google Scholar]
- YOSHIMOTO K, SORIMACHI Y, LI YJ, UEMURA K, YAYAMA K, TANI J, UEDA S & KOMURA S 1997. Effects of ethanol on the levels of brain 6R-L-erythro-5, 6, 7, 8-tetrahydrobiopterin in the inbred strains of mice. DBA/2J, C3H/HeJ and C57BL/6J with different alcohol preferences. Nihon Arukoru Yakubutsu Igakkai Zasshi, 32, 139–48. [PubMed] [Google Scholar]