Abstract
Background
Marked ethnic inequalities in COVID-19 infection and its consequences have been documented. The aim of this paper is to identify the range and nature of evidence on potential pathways which lead to ethnic inequalities in COVID-19 related health outcomes in the United Kingdom (UK).
Methods
We searched six bibliographic and five grey literature databases from 1st December 2019 to 23rd February 2022 for research on pathways to ethnic inequalities in COVID-19 health outcomes in the UK. Meta-data were extracted and coded, using a framework informed by a logic model. Open Science Framework Registration: DOI 10.17605/OSF.IO/HZRB7.
Results
The search returned 10,728 records after excluding duplicates, with 123 included (83% peer-reviewed). Mortality was the most common outcome investigated (N = 79), followed by infection (N = 52). The majority of studies were quantitative (N = 93, 75%), with four qualitative studies (3%), seven academic narrative reviews (6%), nine third sector reports (7%) and five government reports (4%), and four systematic reviews or meta-analyses (3%). There were 78 studies which examined comorbidities as a pathway to mortality, infection, and severe disease. Socioeconomic inequalities (N = 67) were also commonly investigated, with considerable research into neighbourhood infrastructure (N = 38) and occupational risk (N = 28). Few studies examined barriers to healthcare (N = 6) and consequences of infection control measures (N = 10). Only 11% of eligible studies theorised racism to be a driver of inequalities and 10% (typically government/third sector reports and qualitative studies) explored this as a pathway.
Conclusion
This systematic map identified knowledge clusters that may be amenable to subsequent systematic reviews, and critical gaps in the evidence-base requiring additional primary research. Most studies do not incorporate or conceptualise racism as the fundamental cause of ethnic inequalities and therefore the contribution to literature and policy is limited.
Keywords: Ethnicity, Health inequalities, COVID-19, Racism, Systematic map
Background
There have been over 600 million confirmed cases of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection since the virus was identified in December 2019 (Ritchie et al., 2022; Wu et al., 2020), and an estimated 6.5 million deaths from Coronavirus Disease (COVID-19) (Ritchie et al., 2022). Evidence from the United Kingdom (UK) and the United States (US) suggests that minoritised racial and ethnic groups have been disproportionately affected by SARS-CoV-2 infection and COVID-19 disease (Khunti et al., 2020; Pareek et al., 2020; Patel et al., 2020). During the first wave of the pandemic, there were higher rates of SARS-CoV-2 infection, severe COVID-19 disease (hospitalisation, intensive care unit (ICU) admission), and mortality among Black, Asian, and Mixed ethnic groups, compared to White British groups in the UK (Mathur et al., 2021). The evidence on the level of the global extent of ethnic inequalities in COVID-19 health outcomes has been synthesised in previous systematic reviews (Irizar et al., 2023; Pan et al., 2020; Raharja et al., 2020; Siddiq et al., 2022; Sze et al., 2020). However, a greater understanding of the pathways that have led to ethnic inequalities is necessary to know where additional resources are needed to prevent further worsening of these inequalities and their reoccurrence in a future pandemic.
The COVID-19 pandemic has exposed and exacerbated existing inequalities that disproportionately affect the health of minoritised racial and ethnic groups (Bambra et al., 2020; Haque et al., 2020; Kapadia and Bradby, 2021; Keys et al., 2021; Mishra et al., 2021; Nazroo and Bécares, 2020). These inequalities are driven racism, where racism is theorised as the processes by which structures, systems, policies, actions and attitudes interrelate to discriminate and disadvantage minoritised racial and ethnic groups, whilst unfairly advantaging the majority group (Jones, 2000)). Racism is operationalised as the interconnectedness of structural, institutional, and interpersonal racism for the purpose of this paper (Nazroo, 2022; Nazroo et al., 2020). Structural racism refers to the way in which discrimination is embedded within and between societal and structural systems (e.g., housing, education, employment, healthcare, criminal justice) (Bailey et al., 2017), as a result of historical colonialism, and its continuing effects (Saito, 2020), generating and reinforcing inequalities in accessing economic, physical, and social resources (Krieger, 2021; Nazroo and Bécares, 2021). Institutional racism refers specifically to discriminatory ideologies or processes within sectors that amplify rather than redress pre-existing inequalities (Jones, 2000). Institutional racism within one sector (e.g., criminal justice) influences racism in other sectors (e.g., education), creating an interconnected system of structural racism (Bailey et al., 2017). Structural and institutional racism allow individual biases to be embedded in processes, which can result in interpersonal racism. Interpersonal racism refers to discriminatory interactions between people, e.g., harmful attitudes or behaviours towards minoritised racial and ethnic groups, and is associated with poor mental and physical health outcomes (Berger and Sarnyai, 2015; Karlsen and Nazroo, 2002; McKenzie, 2006; Paradies et al., 2015; Priest et al., 2013; Richman et al., 2017; Wallace et al., 2016). Experiences of racism and racial discrimination have a direct negative impact on the health of minoritised racial and ethnic groups (Nazroo, 2003; Wallace et al., 2016; Williams et al., 2019), with known increases in racist hate crimes during the pandemic (Schumann and Moore, 2022).
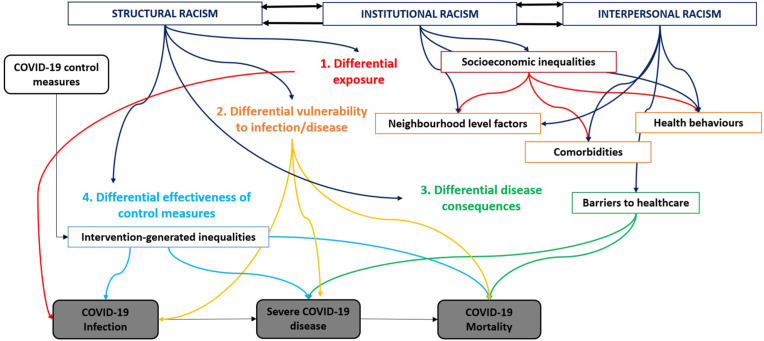
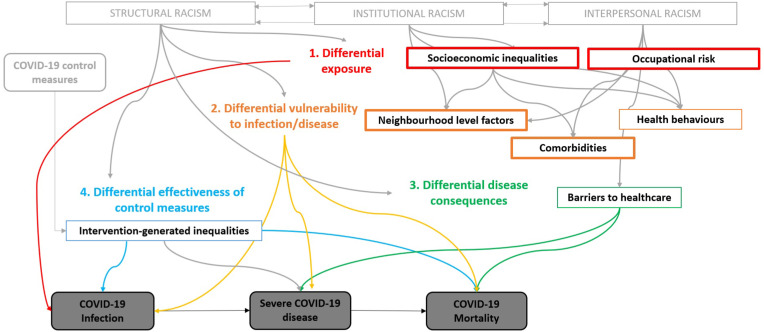
We present a conceptual model hypothesising several pathways that contribute to ethnic inequalities in COVID-19 health outcomes (Fig. 1 ). The conceptual model was developed through consultations with researchers and clinicians, and guided by the theoretical framework proposed by Bécares and colleagues (Bécares et al., 2022), Katikireddi and colleagues (Katikireddi et al., 2021) and Nazroo and colleagues (Nazroo and Bécares, 2020). The following outcomes were included in the conceptual model: SARS-CoV-2 infection, severe COVID-19 disease (e.g., hospital admission, ICU admission/mechanical ventilation required), and mortality. We sought to include post-COVID-19 conditions and access to healthcare as outcomes, however, consultations with an information professional (PD) highlighted that these outcomes would require distinct search strategies, and therefore, these outcomes were excluded.
Fig. 1.
A conceptual model outlining potential pathways that could contribute to ethnic inequalities in COVID-19 health outcomes (infection, severe disease, mortality), developed in line with the theoretical frameworks hypothesised by Bécares et al. (2022) , Katikireddi et al. (2021), and Nazroo and Becares (2020).
The conceptual model depicts the ways in which racism is the fundamental driver of each pathway that leads to ethnic inequalities in health outcomes. Racism results in direct harm as well as leading to the accumulation of socioeconomic disadvantage across the life course (Bécares et al., 2015; Phelan and Link, 2015; Williams et al., 2019). The first pathway relates to differential exposure to infection, partly due to socioeconomic inequalities, such as financial insecurity and insecure employment which may prevent the ability to self-isolate due to fears of income or job loss (Wachtler et al., 2020). In addition, minoritised racial and ethnic groups are over-represented in many keyworker occupations (e.g., healthcare, transport), and were on the frontline during the pandemic, increasing their risk of exposure (Mikolai et al., 2020; Platt and Warwick, 2020). Economic insecurity and overrepresentation in certain keyworker occupations relate to the ethnicity pay gap and unequal access to education and training (Longhi et al., 2017) – consequences of structural and institutional racism. The second pathway represents differential vulnerability to disease, such as having comorbidities (e.g., physical or mental health problems) (Kabarriti et al., 2020), with evidence demonstrating that interpersonal racism and transgenerational trauma directly lead to stress which increases the risk of developing comorbidities, as well as structural and institutional racism driving social inequalities that result in poor health (Bécares et al., 2015; Stopforth et al., 2022). Neighbourhood-level factors (e.g., poor transport, lack of green/open spaces, pollution, overcrowding) that are related to structural and institutional racism, driving racial segregation and inequalities in housing, increase vulnerability to infection and severe disease (Byrne et al., 2020; Hong et al., 2021; Lymperopoulou and Finney, 2017).
Once infected, minoritised racial and ethnic groups experience differential disease consequences, relating to barriers to healthcare resulting in delayed diagnosis and treatment, in addition to underlying comorbidities. Barriers to healthcare are a consequence of institutional racism (e.g., language barriers due to a lack of interpretation facilities which result in miscommunication and a misunderstanding of health conditions and treatment; restrictions to healthcare eligibility based on migrant status) and interpersonal racism (e.g., previous experiences of racial discrimination within healthcare which can result in medical distrust) (Germain and Yong, 2020; Kapadia et al., 2022). The final pathway is the differential effectiveness of control measures (i.e., intervention-generated inequalities), as interventions designed to limit the spread of COVID-19 may cause inequitable adverse consequences in health outcomes, e.g., minoritised racial and ethnic groups were overrepresented in many keyworker occupations (risking exposure to the virus, due to being unable to work from home during government-mandated lockdown). This can result from institutional racism, for example, unequal access to higher education (Boliver, 2018) and discrimination within the labour market (Heath and Di Stasio, 2019) (that is not protected by educational attainment (Zwysen et al., 2021)). In addition, minoritised racial and ethnic groups had differential access to affordable, adequate and/or culturally appropriate personal protective equipment (PPE) for minoritised racial and ethnic groups (Hoernke et al., 2021; Martin et al., 2022; Nguyen et al., 2020), with qualitative research showing that this was perceived to be due to institutional and structural racism (Qureshi et al., 2022).
We conducted a systematic map to identify the available evidence regarding the pathways that have led to ethnic inequalities in COVID-19 health outcomes. Systematic mapping is a useful method for narratively synthesising and categorising available evidence (James et al., 2016). This systematic map will identify the number of studies that are available, the study designs that have been utilised, and the pathways that have been tested. Using these outputs, we aim to describe knowledge clusters, by identifying well-represented research areas that are amenable to full synthesis via systematic review. In addition, we aim to identify relative evidence-gaps that require additional primary research, thereby informing policy-making decisions on the effective direction of resources. Finally, we will evaluate how included studies have measured ethnicity and operationalised ethnicity in analyses. Ethnicity is a complex concept describing a shared social and/or cultural identity, and ethnic groups are ever-changing, varying by place, time, and context (Kapadia and Bradby, 2021). Ethnicity matters for health inequalities as it is a medium that captures the processes of racism and racialisation (Goldberg and Solomos, 2002). There are inconsistencies as to how ethnicity has been theorised, which leads to poor measurement and operationalisation and can result in misperceptions of the extent of ethnic inequalities (Møllersen and Holte, 2008; Ross et al., 2020).
Objectives of the review
The primary research question this study aims to address is:
-
1.
What evidence exists regarding the pathways leading to ethnic inequalities in COVID-19 health outcomes in the UK?
This systematic map also aims to answer the following secondary research questions:
-
1.
How have existing studies measured and conceptualised ethnicity?
-
2.
To what extent have existing studies considered and captured the role of racism in leading to ethnic inequalities?
-
3.
Where are the evidence gaps in data and knowledge, where further primary research is needed?
Methods
Systematic map methodology involves establishing the scope and research questions; searching for evidence; screening evidence; coding; describing and visualising the findings (using a table); and producing a report (James et al., 2016). This map is reported in line with the RepOrting standards for Systematic Evidence Syntheses (ROSES) (Haddaway et al., 2018). The conceptual model, research questions and protocol for this systematic map were developed through consultations with academic researchers, medical clinicians, an information professional (PD), and an expert in evidence synthesis methodologies (DK). The conceptual model informed eligibility decisions and the coding and synthesis of the included studies. The protocol was registered with Open Science Framework on the 28th February 2022: DOI 10.17605/OSF.IO/HZRB7.
Search strategy
An information professional (PD) developed the search strategy, with consultation from the review team members. The search strategy was developed after screening the results of scoping searches undertaken in MEDLINE and after examining existing frameworks and reviews for relevant search terms. The search aimed to identify a wide range of evidence from bibliographic databases, COVID-19 specific databases, and grey literature databases (Table 1 ). Pre-prints were included, though if peer-reviewed publications were available upon data extraction, they were used instead. We searched for articles available in English only, from 1st December 2019 to 23rd February 2022. An example search string is presented in supplementary materials.
Table 1.
Information sources used to identify relevant research.
| Database | |
|---|---|
| Bibliographic databases | MEDLINE, EMBASE, CINAHL, PsycINFO, ASSIA |
| COVID-19 specific databases | EPPI Centre Living Systematic Map of Evidence |
| Pre-print databases | MedRXiv |
| Grey literature databases | Health Management Information Centre, Social Care Institute for Excellence, Social Policy and Practice, North Grey Literature Collection |
Inclusion and exclusion criteria
The conceptual model (Fig. 1) was used to guide the inclusion and exclusion of studies identified through the search, outlined in Table 2 .
Table 2.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population |
|
|
| Outcomes |
|
|
|
|
|
|
|
|
|
||
| ||
| Study designs |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Population
Studies were eligible if they presented findings relating to COVID-19 health outcomes for minoritised racial and ethnic groups in the UK. Studies which compare minoritised racial and ethnic groups with the majority racial/ethnic group (e.g., White British or an aggregated White group depending on how this was defined in the study) were included, as were studies which included only participants from minoritised racial and ethnic groups (i.e., no comparison group). The review only included studies of individuals living in the UK. However, studies which included participants from the UK and other countries were included if the findings were separated by country.
Outcomes
The COVID-19 health outcomes of interest were infection, severe disease (hospitalisation, ICU admission/ventilation required), and mortality. Studies reporting on multiple outcomes were included. Studies were excluded if they focused on health outcomes other than SARS-CoV-2 infection, severe COVID-19 disease, and mortality. For the purpose of this map, we excluded studies which included post-COVID-19 conditions and access to healthcare (e.g., accessing the COVID-19 vaccine) as outcomes.
Study designs
Primary research studies including observational studies, intervention studies, qualitative studies, and mixed methods studies were included. Systematic reviews, rapid reviews, scoping reviews, and other types of reviews with a systematic nature were also included. Studies were included if they examined the pathways that have led to ethnic inequalities in these outcomes, such as, but not only, those which are presented in the conceptual model. Studies which presented data on ethnic inequalities in the COVID-19 health outcomes without investigating potential pathways (e.g., through moderation, mediation, sub-group analyses, covariate adjustment, qualitatively or narratively within reports) were excluded. Studies were excluded if potential pathways were mentioned in the introduction or discussion but were not the focus of the paper (with the exception of studies that mentioned racism without empirically testing it, as racism is conceptualised as the driver of the pathways).
Article screening
Search records identified through the information sources were exported to EndNote and then to EPPI-Reviewer 4 (Thomas et al., 2020), a web-based software program for managing and analysing data in literature reviews. Both EndNote and EPPI-Reviewer were used to de-duplicate the records. Following de-duplications, the articles were screened against inclusion and exclusion criteria, which were first applied to titles and abstracts, followed by full texts. First, a proportion (10%) of records (titles and abstracts, then full texts) were screened by both reviewers to assess the replicability of the selection criteria, using inter-rater agreement statistics calculated in EPPI-Reviewer 4 (91% inter-rater agreement for title and abstract screening and 82% inter-rater agreement for full text screening). If there was any doubt of the relevance of an article during the title and abstract screening, it was retained for full text screening. Any disagreements at full text screening were resolved through discussion with the review team. One reviewer (PI) conducted 70% of the remaining screening (titles and abstracts, then full texts) against the inclusion and exclusion criteria. A second reviewer (DK) screened the final 30% (titles and abstracts, then full texts).
Critical evaluation
No formal critical appraisal tools were used for the systematic map, as the findings were not synthesised. However, we critically evaluated how the included studies have theorised, conceptualised, and measured ethnicity (prioritising self-reported ethnicity and disaggregated ethnic groups). Reviewers who had authored articles to be considered within the review were not involved in the critical evaluation, data extraction, or data synthesis of those specific articles.
Meta-data extraction & coding strategy
One reviewer (PI) completed 100% of the data extraction for the included studies. A coding framework was developed based on the conceptual model and employed when extracting the meta-data. Coding reflects the following information: bibliographic information (e.g., names of authors, publication type, date of publication), study aims, study design (e.g., qualitative, RCT, mixed methods), study characteristics (e.g., setting, region), participant ethnicity (and how it was measured and conceptualised), COVID-19 health outcomes, and pathways or covariates/moderators/mediators that were investigated. The pathways were coded in line with the conceptual model, with additional pathways being included through inductive coding.
Data synthesis and presentation
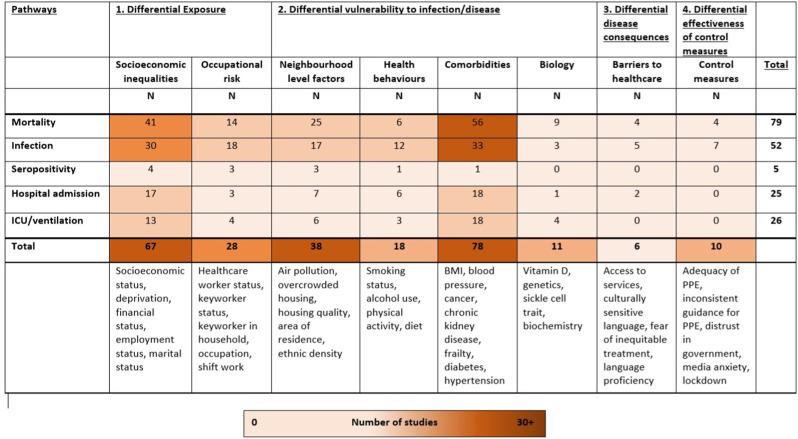
Following the coding of the meta-data, we developed a table, which is a graphical illustration of the number of studies that have explored each of the pathways, and for which outcomes (Fig. 5). Evidence for each COVID-19 health outcome (in rows) was mapped onto the different pathways (in columns), and each cell representing the number of studies. The table documents the existing knowledge clusters (i.e., areas with a considerable number of studies that are amenable to full synthesis via systematic review) and the knowledge gaps (i.e., under-represented areas that require primary research).
Fig. 5.
table of the number of included studies for each pathway to ethnic inequalities and the COVID-19 health outcome investigated.
Results
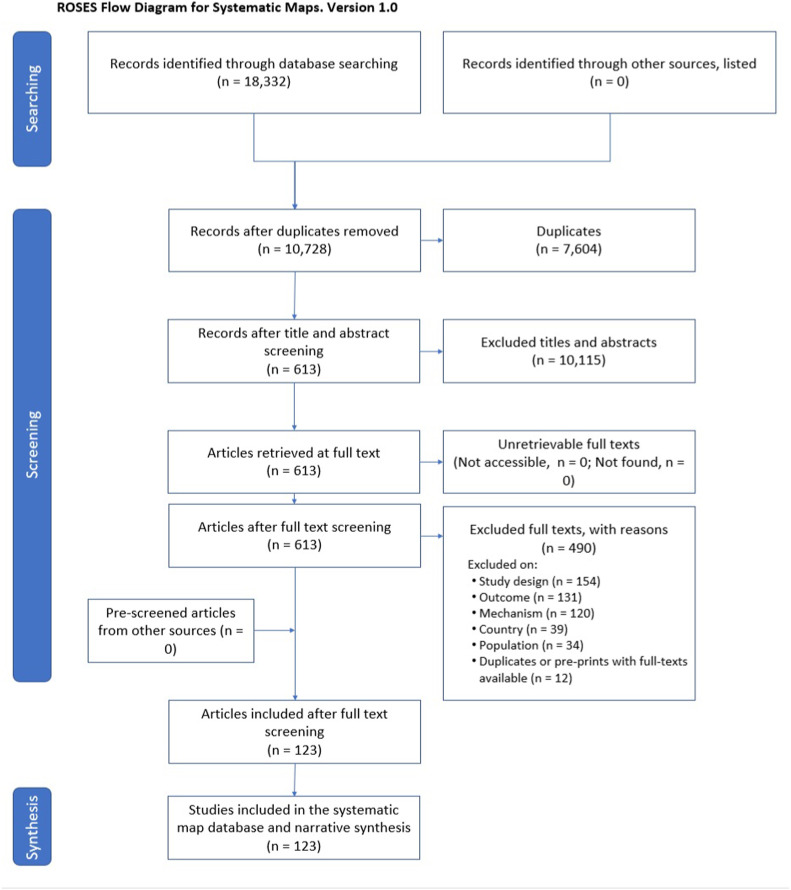
Search results
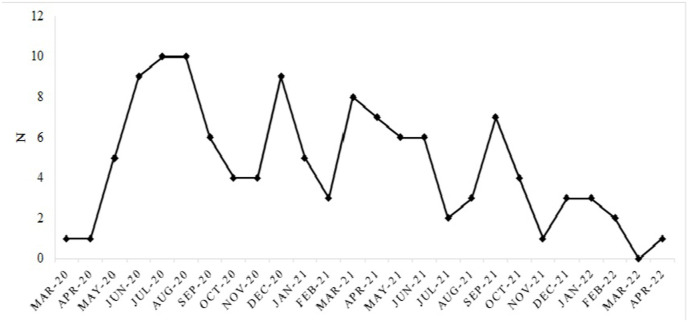
The search returned a total of 10,728 records after excluding duplicates (Fig. 2 ). After title and abstract screening, 613 full texts were assessed against eligibility criteria, with 123 being included in the final systematic map. Of the 123 records, most were peer-reviewed (N = 102, 82.9%), with only five being pre-prints (4.1%). There were nine third sector reports (7.3% and five government reports (4.1%). Two records were conference abstracts (1.6%). The number of studies published each month (date of publication in peer-reviewed journal or date of pre-print) since the start of the pandemic are presented in Fig. 3 . In addition to the pathways described in the conceptual model, we identified several studies that explored ‘occupational risk’ and ‘biology’ as pathways to ethnic inequalities, that are described below. All included studies are presented in a supplementary table (Table S1), listing the pathways that each study investigated.
Fig. 2.
Roses flow diagram for the evidence map screening process (Haddaway et al., 2017).
Fig. 3.
Number of studies investigating pathways to ethnic inequalities in COVID-19 health outcomes published each month.
Where were studies published?
Most records included data from all four UK nations (N = 65), with 20 records focusing on England only. Three records included data for England, Scotland, and Wales, and three included data for England and Wales only. Scotland and Wales were the focus of one record each. In total, 15 studies being conducted in London, five in Birmingham, and two in the West Midlands. Some cities were covered by only one record (e.g., Bradford, Leicester, Middlesex, Newport, Wolverhampton), with one record covering Merseyside and one covering the Northern Powerhouse (Manchester, Leeds, Liverpool, Sheffield, Newcastle).
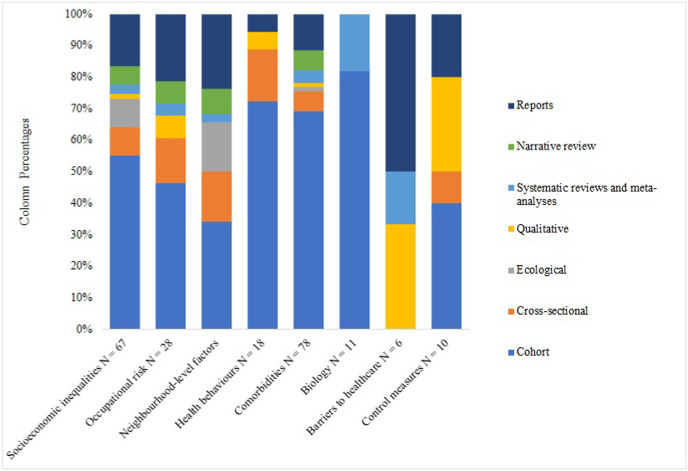
Study designs
Most of the eligible records were cohort studies (N = 76). Of the remaining quantitative studies, nine were cross-sectional and nine were ecological. There were four qualitative studies, four systematic reviews/meta-analyses, seven academic narrative reviews, nine third sector reports and five government reports (i.e., no new empirical evidence is used). An overview of the study designs of included studies for each pathway are presented in Fig. 4 . Studies investigating health behaviours, comorbidities, and biology as pathways were typically cohort studies. In contrast, qualitative study designs were often used to explore barriers to healthcare and effectiveness of control measures.
Fig. 4.
Overview of the study designs of included studies for each pathway to ethnic inequalities in COVID-19 health outcomes.
Outcomes investigated
A table of studies which have explored each of the pathways and the outcomes investigated are presented in Fig. 5. Studies could include multiple outcomes. Most records investigated COVID-19 mortality as an outcome (N = 79), and infection (current infection through PCR or LFT N = 52; seropositivity N = 5). Several records examined severe disease (hospital admission N = 25; ICU admission or ventilation required N = 26). Mortality was the most commonly investigated outcome (followed by infection) for studies which tested socioeconomic inequalities, comorbidities, neighbourhood-level factors, and biology as pathways. Current infection was the most measured outcome for studies which explored occupational risk and health behaviours as pathways. Of the studies exploring barriers to healthcare as a pathway, current infection was the outcome in five studies, and mortality and hospital admission were each investigated as outcomes in four studies. For studies which explored the effectiveness of control measures, the only outcomes investigated were infection (N = 7) and mortality (N = 4).
Conceptualisation of ethnicity
For 18 records (14.6%), it was not applicable to state how ethnicity data were recorded because they did not present original data (e.g., government or third sector reports). Of the remaining records, 56 (45.5%) stated that ethnicity was self-reported and seven (5.7%) stated that ethnicity was obtained through medical records. The way in which ethnicity was recorded was not reported or unclear for 42 studies (34.1%).
Five studies explored pathways within one minoritised racial/ethnic group only. In total, 37 studies (30.1%) aggregated all minoritised racial and ethnic groups into one category, e.g., “Black, Asian or Minoritised Ethnic groups” (BAME) or non-White. There were 81 records (65.9%) that examined outcomes across various racial/ethnic groups, with 60 (74.1%) focusing on broader racial/ethnic groups (e.g., Black, Asian, Mixed), whilst 21 (25.9%) included more granular data (e.g., Black African, Black Caribbean, Indian, Pakistani, Bangladeshi). However, sometimes studies use a combination of broader categories and more granular categories depending on statistical power to investigate the outcome of interest.
Differences in the measurement of race/ethnicity and treatment of racial/ethnic groups for each pathway are presented in Table 3 . Studies which explored health behaviours and the effectiveness of control measures as pathways often recorded race/ethnicity through self-report, and 8% of studies which investigated comorbidities as a pathway used medical records. Approximately one third of studies within each pathway did not report how race/ethnicity was recorded, or it was unclear, despite all studies assessing ethnic inequalities. This was more common in studies which examined comorbidities and biological factors as pathways. Across the pathways, over half of studies utilised disaggregated racial/ethnic groups, with over 80% of studies that explored comorbidities as a pathway using disaggregated racial/ethnic groups (and almost 70% of studies that assessed socioeconomic inequalities and occupational risk as pathways).
Table 3.
The number and percentage of studies that have used each method to record race/ethnicity and aggregate racial/ethnic groups for each pathway to ethnic inequalities in COVID-19 health outcomes.
| Pathway | Recording of race and ethnicity |
Aggregation of racial and ethnic groups |
|||||
|---|---|---|---|---|---|---|---|
| Self-reported N (%) | Medical records N (%) |
NR/unclear N (%) |
N/A N (%) |
One group N (%) |
Aggregateda N (%) |
Disaggregatedb N (%) |
|
| Socioeconomic inequalities | 32 (37.8) | 2 (3.0) | 19 (28.4) | 14 (20.9) | 2 (3.0) | 19 (28.4) | 46 (68.7) |
| Occupational risk | 14 (50.0) | 0 (0.0) | 8 (28.6) | 6 (21.4) | 1 (3.6) | 8 (28.6) | 19 (67.9) |
| Comorbidities | 33 (42.3) | 6 (7.7) | 27 (34.6) | 12 (15.4) | 2 (2.6) | 19 (24.4) | 57 (73.1) |
| Health behaviours | 11 (61.1) | 1 (5.6) | 5 (27.8) | 1 (5.6) | 1 (5.6) | 2 (11.1) | 15 (83.3) |
| Neighbourhood-level factors | 18 (47.4) | 0 (0.0) | 10 (26.3) | 10 (26.3) | 1 (2.6) | 13 (34.2) | 24 (63.2) |
| Biology | 5 (45.5) | 0 (0.0) | 4 (36.4) | 2 (18.2) | 1 (9.1) | 4 (36.4) | 6 (54.5) |
| Barriers to healthcare | 3 (50.0) | 0 (0.0) | 2 (33.3) | 1 (16.7) | 0 (0.0) | 3 (50.0) | 3 (50.5) |
| Effectiveness of control measures | 6 (60.0) | 0 (0.0) | 3 (30.0) | 1 (10.0) | 0 (0.0) | 4 (40.0) | 6 (60.0) |
NR: not reported; N/A: not applicable (for studies which did not present primary data, e.g., systematic reviews).
Aggregated into one broad category (e.g., BAME).
Disaggregated into either broader racial/ethnic groups (e.g., Black, Asian, Mixed) or more granular race/ethnicity data (e.g., Black African, Black Caribbean, Indian, Pakistani, Bangladeshi). Some studies used a combination of broader categories and more granular categories depending on statistical power to investigate the outcome of interest.
Consideration of racism
Approximately 11% (N = 13) theorised racism to be the driver of ethnic inequalities in COVID-19 health outcomes. The study designs were mostly third sector reports (N = 7), with one government report from Public Health England, two qualitative studies, one systematic review/meta-analysis, and one academic narrative review. These findings highlight the lack of empirical quantitative data, which may reflect difficulties in collecting such data (with one cohort study theorising the role of structural racism in the background without explicitly exploring how it relates to the factors tested as pathways). As presented in the conceptual model, we hypothesise racism to be a fundamental cause of each pathway to ethnic inequalities. Within each pathway, we describe the number of studies that also considered the role of racism. However, it should be noted that although some studies did explicitly make the link between racism and the respective pathway (e.g., structural racism leading to socioeconomic inequalities), others reported the role of racism without stating how it is related to the other pathways being investigated.
Pathway 1: differential exposure
Socioeconomic inequalities
The search identified 67 studies which investigated socioeconomic inequalities, such as socioeconomic status, deprivation, and employment status, as a pathway to ethnic inequalities. In terms of how pathways were tested, covariate adjustment was the most common method (N = 43), followed by exploration through qualitative themes or narratively within academic reviews or government/third sector reports (N = 12). A total of six studies tested pathways through moderation or mediation (e.g., fitting interaction terms, structural equation modelling, causal mediation analyses) and six used sub-group analyses to test for socioeconomic pathways. Of these 67 studies, 11 theorised the role of racism, for example, deprivation resulting from structural racism.
Occupational risk
We identified 28 studies which investigated occupational risk (e.g., healthcare worker status, keyworker status, shift work). Again, covariate adjustment was the most common method used to test pathways (N = 16). No studies tested the role of occupational risk through moderation or mediation, though three studies utilised sub-group analyses. Nine records identified occupational risk as a pathway through qualitative research or narratively described occupational risk within reports. Of the 28 studies investigating occupational risk, seven theorised racism as the cause of ethnic inequalities (e.g., working in high-risk occupations, driven by structural racism).
Pathway 2: differential vulnerability to infection/disease
Comorbidities
Comorbidities (e.g., diabetes, hypertension, chronic kidney disease) were the most commonly investigated factor (N = 78), and this was typically done in cohort studies (N = 54). Most studies adjusted for comorbidities as a covariate (N = 45). There were 11 studies which used moderation/mediation analyses, 11 which used sub-group analyses, and 11 which narratively reported the role of comorbidities through reports, reviews, or qualitative research. Despite the large number of studies investigating comorbidities as a pathway, only eight theorised that racism leads to ethnic inequalities, though these were mostly government or third sector reports (with one cohort study).
Neighbourhood-level factors
A total of 38 studies investigated the impact of neighbourhood-level factors, such as air pollution, overcrowded housing, housing quality, and ethnic density, on ethnic inequalities in COVID-19 health outcomes. Most studies tested neighbourhood-level factors as a pathway through covariate adjustment (N = 27). A further three used sub-group analyses, two utilised moderation/mediation, and six narratively explored this pathway through reviews or reports. Seven of these studies theorised the role of racism (e.g., housing conditions driven by racial marginalisation).
Health behaviours
Some studies included health behaviours (e.g., smoking status, alcohol use, physical activity, diet) as a potential contributing factor (N = 18). Adjusting for covariates was the most commonly used method for testing this pathway (N = 15), with one study using mediation, one qualitatively exploring themes and one reporting this pathway in a review. Two of the 18 studies investigating health behaviours conceptualised the role of structural and institutional racism as a driver of inequalities.
Biology
We identified 11 studies that explored the contribution of biology (e.g., vitamin D, genetics) in ethnic inequalities in COVID-19 health outcomes. This pathway was tested through covariate adjustment in seven studies, mediation/moderation in two studies, sub-group analyses for one study, and narratively reported in one study. Only one study investigating biology also theorised racism (marginality) as a cause of inequalities, however, this study did not establish a link between racism and biological susceptibility.
Pathway 3: differential disease consequences
Barriers to healthcare
Pathway three was under-investigated in comparison to the other pathways. Six studies explored barriers to healthcare (e.g., access to services, culturally sensitive language, fear of inequitable treatment) as a contributing factor to ethnic inequalities in COVID-19 health outcomes. As all studies were qualitative (N = 2), reports (N = 3), or systematic reviews (N = 1), five reported this pathway narratively or explored it qualitatively (e.g., interviews with minoritised racial and ethnic groups) and one included language proficiency as a covariate. Of the six studies exploring barriers to healthcare, most (N = 5) theorised the role of racism (e.g., institutional racism creating barriers to accessing services).
Pathway 4: differential effectiveness of control measures
Few studies investigated the differential effectiveness of control measures (N = 10). Those that did explored factors such as adequacy of PPE, inconsistent guidance surrounding PPE, and distrust in the government. As with barriers to healthcare, three studies were qualitative and two were government/third sector reports, meaning this pathway was typically explored through themes or narratively reported (N = 5). Covariate adjustment was used for three studies, moderation or mediation was used for one study, as was sub-group analysis. Three studies exploring the effectiveness of control measures conceptualised racism as the driver of inequalities (e.g., insufficient PPE for those working in high-risk occupations, which is driven by structural racism).
Conceptual model
An updated conceptual model is presented in Fig. 6 , demonstrating where there is considerable evidence relating to each pathway (indicated by the boldness of the boxes). Comorbidities were most commonly tested, followed by socioeconomic inequalities, occupational risk, and neighbourhood-level factors. Very few studies investigated biological factors, barriers to healthcare, or the differential effectiveness of control measures as pathways. Structural, institutional, and interpersonal racism were also under-theorised as the cause of ethnic inequalities in COVID-19 health outcomes, and very few studies measured racism.
Fig. 6.
Updated conceptual model showing the available literature on pathways to ethnic inequalities in COVID-19 health outcomes.
Discussion
We aimed to determine what evidence exists regarding the pathways leading to ethnic inequalities in COVID-19 health outcomes in the UK. This map identified knowledge clusters that may be amenable to further investigation through systematic reviews or meta-analyses and critical gaps in data and knowledge, where further primary research is needed. In addition, we evaluated how included studies measured race/ethnicity and treated racial/ethnic groups, and the extent to which existing studies considered and captured the role of racism in leading to ethnic inequalities. The map identified 123 eligible records, most of which investigated mortality as the outcome, with almost half examining infection, and one-fifth assessing each of the domains of severe disease. Early in the pandemic, there were reports of the disproportionate impact of COVID-19 on minoritised racial and ethnic groups (Khunti et al., 2020; Pareek et al., 2020; Public Health England, 2020), which resulted in a sharp increase in the number of studies published investigating the pathways to these inequalities, though the number of studies published each month steadily declined following widespread vaccination roll-out.
Comorbidities were the most investigated pathway, though most of these studies failed to explore the role of racism on the development of comorbid diseases, for example, through the accumulation of socioeconomic disadvantage, barriers to adequate healthcare, and stress pathways (arising from interpersonal racism and long-standing disadvantage) (Gee et al., 2012; Miller et al., 2021; Stopforth et al., 2022). We also identified a small number of studies which tested biological pathways, though this was not included as a pathway in our conceptual model, as early hypotheses such as vitamin D deficiency and genetics were not supported by evidence (Lee et al., 2020; Raisi-Estabragh et al., 2020). The second most commonly investigated pathway was socioeconomic inequalities, followed by neighbourhood-level factors. Racism is a fundamental cause of racial/ethnic differences in socioeconomic position (Nazroo, 2003; Williams, 1999), which is related to neighbourhood-level factors and residential segregation, as people from minoritised racial and ethnic groups tend to live in more deprived regions, have poorer housing quality, and insecure housing tenures (Finney and Harries, 2013). Several studies examined occupational risk as a pathway, and although we did not specifically outline this in our conceptual model, it aligns with the first pathway, ‘differential exposure’. Few studies investigated the third and fourth pathways, ‘differential disease consequences’ and ‘differential effectiveness of control measures’, and most studies which explored these pathways were qualitative or reports. This meant these studies were able to capture important pathways that are often not covered in quantitative health datasets, such as fear of inequitable treatment, lack of culturally sensitive language, adequacy of PPE, and government mistrust.
The most important gap identified through this systematic map, is the lack of research that considered the role of racism. It has been suggested that the intersection between ethnicity and health is the product of discrimination, in which racism, not ethnicity, is the cause of health inequalities (Razai et al., 2021; Stopforth et al., 2022), yet only 13 studies considered racism as a driver of ethnic inequalities. This may reflect political pressure, under-recognition, or difficulties in collecting empirical data on racism, particularly when racism is embedded within and between societal and structural systems (e.g., housing, education, employment, healthcare, criminal justice) (Bailey et al., 2017; Gee and Ford, 2011; Jones, 2000). It may be that authors explored the role of variables that indicate processes of structural and institutional racism, such as deprivation and housing quality, which many studies did investigate, yet authors rarely made the explicit link between these factors and racism. One cohort study did highlight structural racism as a cause of ethnic inequalities, and subsequently explored socioeconomic inequalities as covariates (e.g., household deprivation, social grade), yet did not infer how structural racism may lead to socioeconomic inequalities (Nafilyan et al., 2021). Although we decided to exclude studies of vaccine hesitancy, we are aware of some UK studies which have empirically tested the role of interpersonal racism on vaccine hesitancy (Bécares et al., 2022; Woolf et al., 2021).
This systematic map highlights the limited use of theory and limited understanding and lack of acknowledgement of how racism leads to health inequalities. Without theorising the role racism, which most of the included studies failed to do, these studies are limited in their conceptualisation of the causal pathways to ethnic inequalities in COVID-19 health outcomes. The findings of this systematic map advance scholarship on the theorisations of ethnicity, racialisation and racism in health research, by evidencing the paucity of discussions around the reasons for severe health inequalities in COVID-19 outcomes. We recommend that future research in ethnic inequalities in health must theorise and consider the role of racism, and where possible, investigate the impact of interpersonal racism (e.g., self-reports of experiences of harassment) and institutional racism (e.g., self-reports of discrimination within sectors) on health outcomes. In addition, researchers must more meaningfully consider the impacts structural and institutional racism that may be more subtle and indirect, perhaps by considering their effects on measurable consequences of such racism (e.g., socioeconomic disadvantage), otherwise we remain limited in our understanding of the drivers of ethnic inequalities in health outcomes and risk repeating racist patterns within health research (Powell et al., 2022).
Despite ethnic inequalities being the focus of most records, it was not reported or unclear how race/ethnicity was recorded for over 30% of studies. Over a quarter of studies aggregated participants from minoritised racial and ethnic groups into one broad category, such as ‘BAME’ or “non-White” – preventing the identification of differences in the extent of inequalities in COVID-19 health outcomes across individual ethnic groups. A large UK study found differences in the risk of outcomes when further disaggregating racial/ethnic groups, for example, finding an increased risk of infection for South Asian people, but when further disaggregated, there was no increased risk for Bangladeshi people (Mathur et al., 2021). Differences in the risk of outcomes indicate that there are differences in the pathways which contribute to them. For example, there is evidence to suggest that Pakistani and Bangladeshi people tend to live in more deprived areas and occupy the lowest socioeconomic positions (Bécares et al., 2011), and socioeconomic deprivation is associated with higher risk of COVID-19 infection (Niedzwiedz et al., 2020). Studies which utilise more granular race/ethnicity data are necessary to determine the extent of, and pathways to, inequalities in COVID-19 health outcomes, and how they differ across racial/ethnic groups, as aggregated data obscures and masks important differences between groups.
This systematic map has its limitations. We included only UK literature, due to variation in racial and ethnic composition and because pathways may differ across countries. Though access to and uptake of the vaccine, and post-COVID conditions were included in our pre-registered conceptual model, we decided to exclude them, as they are both distinct outcomes which would require additional search terms or a separate search strategy to ensure all studies were captured. In addition, post-COVID conditions, i.e., long COVID, are currently a broad and heterogenous group of patients, with wide ranging symptoms (Pan and Pareek, 2023; Rando et al., 2021). However, future systematic reviews should examine pathways to ethnic inequalities in accessing and accepting the vaccine, and post-COVID conditions. Despite these limitations, we generated a comprehensive systematic map of available UK evidence regarding the pathways to ethnic inequalities in COVID-19 health outcomes. We conducted an extensive and rigorous search of multiple databases, including grey literature databases. Our search strategy and protocol were developed through consultations with academic researchers, medical clinicians, an information professional (PD), and an expert in evidence synthesis methods (DK).
This systematic map has identified knowledge clusters which may be amenable to subsequent systematic review and meta-analysis, as well as clear gaps in the evidence base, with very few studies exploring differential disease consequences (e.g., barriers to healthcare) and differential effectiveness of control measures, which may be more difficult to empirically test compared to the other pathways. For future research into ethnic inequalities in health, we recommend the inclusion of studies which utilise disaggregated racial/ethnic groups (to the most granular level possible whilst maintaining statistical power), to determine differences in the pathways to inequalities, and we argue against the use of one uninformative aggregated group (i.e., BAME), which disguise unique experiences (GOV.UK, 2021). Importantly, we recommend theorising how racism drives ethnic inequalities in health, and researchers should conceptualise the relationship between racism and more measurable variables that can be included in quantitative analyses, as well as utilising qualitative research to enable a deeper exploration of experiences of racism.
Credit author statement
Patricia Irizar: Conceptualisation, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft. Dharmi Kapadia: Conceptualisation, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. Sarah Amele: Conceptualisation, Writing – review & editing. Laia Bécares: Conceptualisation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. Pip Dival: Conceptualisation, Data curation, Resources. Srinivasa Vittal Katikireddi: Conceptualisation, Investigation, Methodology, Supervision, Validation, Writing – review & editing. Eliud Kibuchi: Conceptualisation, Writing – review & editing. Dylan Kneale: Conceptualisation, Methodology, Writing – review & editing. Ronan McCabe: Conceptualisation, Writing – review & editing. James Nazroo: Conceptualisation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. Laura B Nellums: Conceptualisation, Investigation, Methodology, Supervision, Validation, Writing – review & editing. Harry Taylor: Conceptualisation, Writing – review & editing. Shirley Sze: Conceptualisation, Writing – review & editing. Danial Pan: Conceptualisation, Investigation, Methodology, Validation, Writing – review & editing. Manish Pareek: Conceptualisation, Investigation, Methodology, Supervision, Validation, Writing – review & editing.
Data sharing
All extracted data and analytical codes are available from the corresponding author are available upon request.
Role of funding source
This work was supported by the ESRC (grant number ES/W000849/1). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. DP is supported by a NIHR Doctoral Research Fellowship (NIHR302338). MP is supported by a NIHR Development and Skills Enhancement Award, by the NIHR Leicester Biomedical Research Centre (BRC), and by the NIHR Applied Research Collaboration East Midlands (ARC EM). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. SVK acknowledges funding from a NRS Senior Clinical Fellowship (SCAF/15/02), the Medical Research Council (MC_UU_00022/2) and the Scottish Government Chief Scientist Office (SPHSU17). LBN is supported by an Academy of Medical Sciences Springboard Award (SBF005/1047).
Declaration of competing interest
SVK was co-chair of the Scottish Government's Expert Reference Group on Ethnicity and COVID-19 and a member of the UK Scientific Advisory Group on Emergencies (SAGE) subgroup on ethnicity. All other authors report no conflicts of interest.
Handling Editor: Medical Sociology Office
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2023.116044.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
No data was used for the research described in the article.
References
- Bailey Z.D., Krieger N., Agénor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health. 2020;74(11):964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L., Nazroo J., Kelly Y. A longitudinal examination of maternal, family, and area-level experiences of racism on children's socioemotional development: patterns and possible explanations. Soc. Sci. Med. 2015;142:128–135. doi: 10.1016/j.socscimed.2015.08.025. [DOI] [PubMed] [Google Scholar]
- Bécares L., Shaw R.J., Katikireddi S.V., Irizar P., Amele S., Kapadia D., Nazroo J., Taylor H. SSM-Population Health; 2022. Racism as the Fundamental Cause of Ethnic Inequities in COVID-19 Vaccine Hesitancy: A Theoretical Framework and Empirical Exploration Using the UK Household Longitudinal Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bécares L., Stafford M., Laurence J., Nazroo J. Composition, concentration and deprivation: exploring their association with social cohesion among different ethnic groups in the UK. Urban Stud. 2011;48(13):2771–2787. doi: 10.1177/0042098010391295. [DOI] [PubMed] [Google Scholar]
- Berger M., Sarnyai Z. “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress. 2015;18(1):1–10. doi: 10.3109/10253890.2014.989204. [DOI] [PubMed] [Google Scholar]
- Boliver V. Ethnic inequalities in admission to highly selective universities. Dismantling race in higher education: Racism, whiteness and decolonising the academy. 2018:67–85. [Google Scholar]
- Byrne B., Alexander C., Khan O., Nazroo J., Shankley W. Policy Press; 2020. Ethnicity, Race and Inequality in the UK: State of the Nation. [Google Scholar]
- Finney N., Harries B. 2013. Understanding Ethnic Inequalities in Housing: Analysis of the 2011 Census (Better Housing Briefing Paper 23, Issue. [Google Scholar]
- Gee G.C., Ford C.L. Structural racism and health inequities: old issues, New Directions1. Du. Bois Rev.: Social Science Research on Race. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Walsemann K.M., Brondolo E. A life course perspective on how racism may be related to health inequities. Am. J. Publ. Health. 2012;102(5):967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germain S., Yong A. COVID-19 highlighting inequalities in access to healthcare in England: a case study of ethnic minority and migrant women. Fem. Leg. Stud. 2020;28(3):301–310. doi: 10.1007/s10691-020-09437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg D.T., Solomos J. Blackwell; Malden, MA: 2002. A Companion to Racial and Ethnic Studies. [Google Scholar]
- GOV.UK . 2021. Writing about Ethnicity.https://www.ethnicity-facts-figures.service.gov.uk/style-guide/writing-about-ethnicity [Google Scholar]
- Haddaway N.R., Macura B., Whaley P., Pullin A.S. 2017. ROSES Flow Diagram for Systematic Maps. [Google Scholar]
- Haddaway N.R., Macura B., Whaley P., Pullin A.S. ROSES RepOrting standards for Systematic Evidence Syntheses: pro forma, flow-diagram and descriptive summary of the plan and conduct of environmental systematic reviews and systematic maps. Environ. Evid. 2018;7(1):1–8. [Google Scholar]
- Haque Z., Becares L., Treloar N. London: Runnymede. 2020. Over-exposed and under-protected: the devastating impact of COVID–19 on Black and minority ethnic communities in great britain. A runnymede trust and icm survey (London, runnymede)https://www.runnymedetrust.org/uploads/Runnymede [Google Scholar]
- Heath A.F., Di Stasio V. Racial discrimination in Britain, 1969–2017: a meta‐analysis of field experiments on racial discrimination in the British labour market. Br. J. Sociol. 2019;70(5):1774–1798. doi: 10.1111/1468-4446.12676. [DOI] [PubMed] [Google Scholar]
- Hoernke K., Djellouli N., Andrews L., Lewis-Jackson S., Manby L., Martin S., Vanderslott S., Vindrola-Padros C. Frontline healthcare workers' experiences with personal protective equipment during the COVID-19 pandemic in the UK: a rapid qualitative appraisal. BMJ Open. 2021;11(1) doi: 10.1136/BMJOPEN-2020-046199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong B., Bonczak B.J., Gupta A., Thorpe L.E., Kontokosta C.E. Exposure density and neighborhood disparities in COVID-19 infection risk. Proc. Natl. Acad. Sci. USA. 2021;118(13) doi: 10.1073/pnas.2021258118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irizar P., Pan D., Kapadia D., Becares L., Sze S., Taylor H., Amele S., Divall P., Gray L.J., Nellums L.B., Katikireddi S.V., Pareek M. EClinicalMedicine; 2023. Examining Ethnic Inequalities in COVID-19 Infection, Hospitalisation, Intensive Care Admission, and Death: a Global Systematic Review and Meta-Analysis of 200 Million Participants. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James K.L., Randall N.P., Haddaway N.R. A methodology for systematic mapping in environmental sciences. Environ. Evid. 2016;5(1):1–13. doi: 10.1186/s13750-016-0059-6. [DOI] [Google Scholar]
- Jones C.P. Levels of racism: a theoretic framework and a gardener's tale. Am. J. Publ. Health. 2000;90(8):1212. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabarriti R., Brodin N.P., Maron M.I., Guha C., Kalnicki S., Garg M.K., Racine A.D. Association of race and ethnicity with comorbidities and survival among patients with COVID-19 at an urban medical center in New York. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapadia D., Bradby H. Routledge International Handbook of Critical Issues in Health and Illness. Routledge; 2021. Ethnicity and health; pp. 183–196. [Google Scholar]
- Kapadia D., Zhang J., Salway S., Nazroo J., Booth A., Villarroel-Williams N., Becares L., Esmail A. 2022. Ethnic Inequalities in Healthcare: a Rapid Evidence Review.https://www.nhsrho.org/wp-content/uploads/2022/02/RHO-Rapid-Review-Final-Report_Summary_v.4.pdf [Google Scholar]
- Karlsen S., Nazroo J.Y. Relation between racial discrimination, social class, and health among ethnic minority groups. Am. J. Publ. Health. 2002;92(4):624–631. doi: 10.2105/AJPH.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katikireddi S.V., Lal S., Carrol E.D., Niedzwiedz C.L., Khunti K., Dundas R., Diderichsen F., Barr B. Unequal impact of the COVID-19 crisis on minority ethnic groups: a framework for understanding and addressing inequalities. J. Epidemiol. Community Health. 2021;75(10):970–974. doi: 10.1136/jech-2020-216061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keys C., Nanayakkara G., Onyejekwe C., Sah R.K., Wright T. Health inequalities and ethnic vulnerabilities during COVID-19 in the UK: a reflection on the PHE Reports. Fem. Leg. Stud. 2021;29(1):107–118. doi: 10.1007/s10691-020-09446-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khunti K., Singh A.K., Pareek M., Hanif W. British Medical Journal Publishing Group; 2020. Is Ethnicity Linked to Incidence or Outcomes of Covid-19? [DOI] [PubMed] [Google Scholar]
- Krieger N. Structural racism, health inequities, and the two-edged sword of data: structural problems require structural solutions. Front. Public Health. 2021;9:301. doi: 10.3389/fpubh.2021.655447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee I.-H., Lee J.-W., Kong S.W. A survey of genetic variants in SARS-CoV-2 interacting domains of ACE2, TMPRSS2 and TLR3/7/8 across populations. Infect. Genet. Evol. 2020;85 doi: 10.1016/j.meegid.2020.104507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longhi S., Brynin M.J.E., Commission H.R. 2017. The Ethnicity Pay Gap.https://www.equalityhumanrights.com/sites/default/files/research-report-108-the-ethnicity-pay-gap.pdf [Google Scholar]
- Lymperopoulou K., Finney N. Socio-spatial factors associated with ethnic inequalities in districts of England and Wales, 2001–2011. Urban Stud. 2017;54(11):2540–2560. doi: 10.1177/0042098016653725. [DOI] [Google Scholar]
- Martin C.A., Pan D., Nazareth J., Aujayeb A., Bryant L., Carr S., Gray L.J., Gregary B., Gupta A., Guyatt A.L. Access to personal protective equipment in healthcare workers during the COVID-19 pandemic in the United Kingdom: results from a nationwide cohort study (UK-REACH) BMC Health Serv. Res. 2022;22(1):1–13. doi: 10.1186/s12913-022-08202-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur R., Rentsch C.T., Morton C.E., Hulme W.J., Schultze A., MacKenna B., Eggo R.M., Bhaskaran K., Wong A.Y., Williamson E.J. Ethnic differences in SARS-CoV-2 infection and COVID-19-related hospitalisation, intensive care unit admission, and death in 17 million adults in England: an observational cohort study using the OpenSAFELY platform. Lancet. 2021;397(10286):1711–1724. doi: 10.1016/S0140-6736(21)00634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie K. Racial discrimination and mental health. Psychiatry. 2006;5(11):383–387. doi: 10.1053/j.mppsy.2006.08.002. [DOI] [Google Scholar]
- Mikolai J., Keenan K., Kulu H. Intersecting household-level health and socio-economic vulnerabilities and the COVID-19 crisis: an analysis from the UK. SSM-Population Health. 2020;12 doi: 10.1016/j.ssmph.2020.100628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller H.N., LaFave S., Marineau L., Stephens J., Thorpe R.J., Jr. The impact of discrimination on allostatic load in adults: an integrative review of literature. J. Psychosom. Res. 2021;146 doi: 10.1016/j.jpsychores.2021.110434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra V., Seyedzenouzi G., Almohtadi A., Chowdhury T., Khashkhusha A., Axiaq A., Wong W.Y.E., Harky A. Health inequalities during COVID-19 and their effects on morbidity and mortality. J. Healthc. Leader. 2021;13:19. doi: 10.2147/JHL.S270175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Møllersen S., Holte A. Ethnicity as a variable in mental health research: a systematic review of articles published 1990–2004. Nord. J. Psychiatr. 2008;62(4):322–328. doi: 10.1080/08039480802044414. [DOI] [PubMed] [Google Scholar]
- Nafilyan V., Islam N., Mathur R., Ayoubkhani D., Banerjee A., Glickman M., Humberstone B., Diamond I., Khunti K. Ethnic differences in COVID-19 mortality during the first two waves of the Coronavirus Pandemic: a nationwide cohort study of 29 million adults in England. Eur. J. Epidemiol. 2021;36(6):605–617. doi: 10.1007/s10654-021-00765-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazroo J. Tackling racism: moving beyond rhetoric to turn theory into practice. Br. Med. J. 2022;378 doi: 10.1136/bmj.o1597. [DOI] [PubMed] [Google Scholar]
- Nazroo J., Bécares L. Evidence for ethnic inequalities in mortality related to COVID-19 infections: findings from an ecological analysis of England. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-041750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazroo J., Bécares L. Runnymede/CoDE COVID Briefings; Issue: 2021. Ethnic Inequalities in COVID-19 Mortality: a Consequence of Persistent Racism. [Google Scholar]
- Nazroo J.Y. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am. J. Publ. Health. 2003;93(2):277–284. doi: 10.2105/AJPH.93.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazroo J.Y., Bhui K.S., Rhodes J. Where next for understanding race/ethnic inequalities in severe mental illness? Structural, interpersonal and institutional racism. Sociol. Health Illness. 2020;42(2):262–276. doi: 10.1111/1467-9566.13001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.-G., Ma W., Mehta R.S., Warner E.T., Sikavi D.R., Lo C.-H. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedzwiedz C.L., O'Donnell C.A., Jani B.D., Demou E., Ho F.K., Celis-Morales C., Nicholl B.I., Mair F.S., Welsh P., Sattar N. Ethnic and socioeconomic differences in SARS-CoV-2 infection: prospective cohort study using UK Biobank. BMC Med. 2020;18(1):1–14. doi: 10.1186/s12916-020-01640-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan D., Pareek M. Towards a universal definition of post-COVID-19 condition - how do we proceed? JAMA Netw. Open. 2023;6(4) doi: 10.1001/jamanetworkopen.2023.5779. [DOI] [PubMed] [Google Scholar]
- Pan D., Sze S., Minhas J.S., Bangash M.N., Pareek N., Divall P., Williams C.M., Oggioni M.R., Squire I.B., Nellums L.B. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020;23 doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y., Ben J., Denson N., Elias A., Priest N., Pieterse A., Gupta A., Kelaher M., Gee G. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9) doi: 10.1371/journal.pone.0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pareek M., Bangash M.N., Pareek N., Pan D., Sze S., Minhas J.S., Hanif W., Khunti K. Ethnicity and COVID-19: an urgent public health research priority. Lancet. 2020;395(10234):1421–1422. doi: 10.1016/S0140-6736(20)30922-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P., Hiam L., Sowemimo A., Devakumar D., McKee M. British Medical Journal. Publishing Group; 2020. Ethnicity and covid-19. [DOI] [PubMed] [Google Scholar]
- Phelan J.C., Link B.G. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 2015;41:311–330. [Google Scholar]
- Platt L., Warwick R. COVID‐19 and ethnic inequalities in England and Wales. Journal of Fiscal Studies. 2020;41(2):259–289. doi: 10.1111/1475-5890.12228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell R.A., Njoku C., Elangovan R., Sathyamoorthy G., Ocloo J., Thayil S., Rao M. Tackling racism in UK health research. Br. Med. J. 2022;376 doi: 10.1136/bmj-2021-065574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priest N., Paradies Y., Trenerry B., Truong M., Karlsen S., Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc. Sci. Med. 2013;95:115–127. doi: 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- Public Health England . P. H. England; 2020. Disparities in the Risk and Outcomes of COVID-19.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf [Google Scholar]
- Qureshi I., Gogoi M., Wobi F., Chaloner J., Al-Oraibi A., Hassan O., Pan D., Nellums L.B., Pareek M. Healthcare workers from diverse ethnicities and their perceptions of risk and experiences of risk management during the COVID-19 pandemic: qualitative insights from the UK-REACH study. Front. Med. 2022:1872. doi: 10.3389/fmed.2022.930904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raharja A., Tamara A., Kok L.T. Association between ethnicity and severe COVID-19 disease: a systematic review and meta-analysis. Journal of racial & ethnic health disparities. 2020:1–10. doi: 10.1007/s40615-020-00921-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raisi-Estabragh Z., McCracken C., Bethell M.S., Cooper J., Cooper C., Caulfield M.J., Munroe P.B., Harvey N.C., Petersen S.E. Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25 (OH)-vitamin D status: study of 1326 cases from the UK Biobank. J. Publ. Health. 2020;42(3):451–460. doi: 10.1093/pubmed/fdaa095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rando H.M., Bennett T.D., Byrd J.B., Bramante C., Callahan T.J., Chute C.G., Davis H.E., Deer R., Gagnier J., Koraishy F.M. 2021. Challenges in Defining Long COVID: Striking Differences across Literature, Electronic Health Records, and Patient-Reported Information. medRxiv. [DOI] [Google Scholar]
- Razai M.S., Majeed A., Esmail A. Structural racism is a fundamental cause and driver of ethnic disparities in health. Br. Med. J. 2021;373 doi: 10.1136/bmj.n938. [DOI] [PubMed] [Google Scholar]
- Richman L.S., Pascoe E., Lattaner M. 2017. Interpersonal Discrimination and Physical Health. [Google Scholar]
- Ritchie H., Mathieu E., Rodés-Guirao L., Appel C., Giattino C., Ortiz-Ospina E., Hasell J., Macdonald B., Beltekian D., Roser M. 2022. Coronavirus Pandemic (COVID-19)https://ourworldindata.org/coronavirus-data [Google Scholar]
- Ross P.T., Hart-Johnson T., Santen S.A., Zaidi N.L.B. Considerations for using race and ethnicity as quantitative variables in medical education research. Perspectives on Medical Education. 2020;9(5):318–323. doi: 10.1007/s40037-020-00602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito N.T. vol. 2. NYU Press; 2020. (Settler Colonialism, Race, and the Law: Why Structural Racism Persists). [Google Scholar]
- Schumann S., Moore Y. The COVID-19 outbreak as a trigger event for sinophobic hate crimes in the United Kingdom. Br. J. Criminol. 2022 doi: 10.1093/bjc/azac015. [DOI] [Google Scholar]
- Siddiq S., Ahmed S., Akram I. Public health; 2022. A Systematic Review and Meta-Analysis of Clinical Outcomes Following COVID-19 Infection in Ethnic Minority Groups in the UK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stopforth S., Kapadia D., Nazroo J., Bécares L. SSM-Population Health; 2022. The Enduring Effects of Racism on Health: Understanding Direct and Indirect Effects over Time. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sze S., Pan D., Nevill C.R., Gray L.J., Martin C.A., Nazareth J., Minhas J.S., Divall P., Khunti K., Abrams K.R. EClinicalMedicine; 2020. Ethnicity and Clinical Outcomes in COVID-19: a Systematic Review and Meta-Analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas J., Graziosi S., Brunton J., Ghouze Z., O’Driscoll P., Bond M. EPPI-Reviewer: advanced software for systematic reviews, maps and evidence synthesis. EPPI-Centre Software. UCL Social Research Institute; London: 2020. [Google Scholar]
- Wachtler B., Michalski N., Nowossadeck E., Diercke M., Wahrendorf M., Santos-Hövener C., Lampert T., Hoebel J. 2020. Socioeconomic Inequalities and COVID-19–A Review of the Current International Literature. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace S., Nazroo J., Bécares L. Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. Am. J. Publ. Health. 2016;106(7):1294–1300. doi: 10.2105/AJPH.2016.303121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R. Race, socioeconomic status, and health the added effects of racism and discrimination. Ann. N. Y. Acad. Sci. 1999;896(1):173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: evidence and needed research. Annu. Rev. Publ. Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf K., McManus I.C., Martin C.A., Nellums L.B., Guyatt A.L., Melbourne C., Bryant L., Gogoi M., Wobi F., Al-Oraibi A. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: results from the UK-REACH prospective nationwide cohort study. The Lancet Regional Health-Europe. 2021;9 doi: 10.1016/j.lanepe.2021.100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu F., Zhao S., Yu B., Chen Y.-M., Wang W., Song Z.-G., Hu Y., Tao Z.-W., Tian J.-H., Pei Y.-Y. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwysen W., Di Stasio V., Heath A. Ethnic penalties and hiring discrimination: comparing results from observational studies with field experiments in the UK. Sociology. 2021;55(2):263–282. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data was used for the research described in the article.