Abstract
Objective
Environmental factors may be very important in the development of disordered weight-control behaviours (DWCB) among youth, yet no study to date has conducted a review that synthesizes these findings. The purpose of the present study was to systematically review existing literature on environmental influences on DWCB among youth and to identify conceptual and methodological gaps in the literature.
Design
Systematic review.
Setting
Studies were identified through a systematic search using PubMed, PsycINFO, Google Scholar and secondary references. Inclusion criteria included observational studies published in peer-reviewed journals from 1994 to 2012 that examined environmental exposure(s) associated with DWCB among youth.
Subjects
Ninety-three studies, the majority of which utilized a cross-sectional design (75 %; n 70), were identified. Longitudinal studies’ follow-up time ranged from 8 months to 10 years.
Results
Parental, peer and media influences have been extensively studied as factors associated with DWCB among youth. Fewer studies have examined behavioural settings (i.e. homes, schools, neighbourhoods) or sectors of influence other than the media on DWCB. No studies utilized multilevel methods to parse out environmental influences on DWCB. Most studies (69 %, n 64) did not explicitly utilize a theory or model to guide the research.
Conclusions
Findings indicate that exploring a wider range of environmental influences on DWCB, specifically behavioural settings and sectors of influence, using diverse study samples and multilevel methodology is needed to advance the field and to inform the design of comprehensive prevention programmes that target DWCB and other weight-related behaviours.
Keywords: Environment, Disordered weight control, Youth
Disordered weight-control behaviours (DWCB), such as vomiting, taking laxatives and taking diet pills without a prescription, are a growing concern among youth and have been found to be more common than clinical eating disorders. Among 9th–12th grade females, 9·4 % reported taking diet pills, 8·8 % reported self-induced vomiting and 1·9 % reported taking laxatives. Among males of the same age, 2·3 % reported taking diet pills, 1·6 % reported self-induced vomiting and 1·7 % reported using laxatives( 1 ). These types of DWCB often precede the development of clinical eating disorders and are associated with numerous detrimental outcomes, including oesophagitis, gastric rupture and impairment of digestive functioning( 2 , 3 ), menstrual dysregulation in girls( 4 ), low self-esteem and depression( 5 ). Identifying and understanding risk and protective factors of DWCB are essential to inform future prevention and intervention efforts.
DWCB are broadly considered to be behaviours intended for weight loss and/or weight management that are unhealthy, extreme or disordered. Currently, there is no one universal definition of DWCB. Many other similar terms are used in the literature, such as disordered eating, disordered eating symptomatology, eating disorder symptoms, unhealthy weight-control behaviours, extreme weight-control behaviours, excessive dieting, compulsive exercising, bulimic tendencies and bulimic symptomatology. Each of these terms has distinct definitions and operationalizations depending on the discipline, study and/or scale used. The American College of Sports Medicine defines disordered eating as ‘a wide spectrum of harmful and often ineffective eating behaviours used in attempts to lose weight or achieve a lean appearance’( 6 , 7 ). Some studies have used the terminology DWCB to distinguish unhealthy methods with the intention of losing or maintaining weight, such as taking laxatives, taking diet pills or self-induced vomiting( 8 – 11 ), compared with definitions of disordered eating, which have included binge eating( 12 – 14 ). Cigarette smoking and fasting for the purposes of losing weight have also been included as examples of harmful weight-control behaviours( 1 , 15 – 18 ).
Environmental influences have been explored as one set of factors associated with DWCB. While there is no one universal definition of the environment, the environment broadly refers to factors external to the individual that may shape individual attitudes, perceptions and behaviours. An adaptation of the social-ecological model by the Institute of Medicine identified specific behavioural settings (i.e. common settings in which individuals are exposed to and that shape health behaviours, such as homes, schools, neighbourhoods) and sectors of influence (i.e. established industries and institutions, such as government, agriculture, education, transportation, health care) relevant for childhood obesity prevention efforts( 19 ). These conceptualizations may be helpful in examining specific environmental influences on DWCB, as DWCB are part of the range of weight-related behaviours that contribute to multiple adverse outcomes, including obesity and eating disorders.
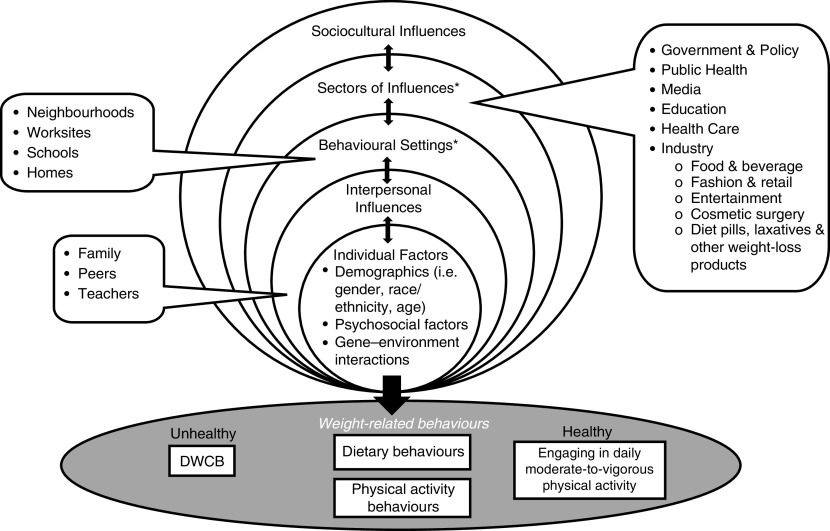
We developed a modified version of the Institute of Medicine's social-ecological model( 19 , 20 ) specific to examining environmental influences on DWCB (Fig. 1). Within the spectrum of weight-related behaviours, DWCB, unlike increasing physical activity or decreasing intake of energy-dense foods, are considered unhealthy and harmful ways to lose and/or maintain weight and are not recommended by clinicians. Factors that shape the development of weight-related behaviours include individual factors (i.e. demographics, psychosocial factors), interpersonal factors (i.e. relationships with parents, peers and teachers), behavioural settings in which individuals engage in various weight-related behaviours (i.e. homes, schools, neighbourhoods), sectors of influence that shape weight-related behaviours (i.e. media, education, government, and fashion, entertainment and cosmetic surgery industries) and the overarching sociocultural context (i.e. social and cultural norms and values around ideal body sizes and shapes) in which individuals and populations live. Interactions between levels of influence may contribute to the development of DWCB and/or other weight-related behaviours; for example, the exposure and internalization of sociocultural expectations of ideal body shapes and sizes for males and females, channelled through media, fashion and entertainment industries, may in turn be perpetuated and reinforced in the home and school settings and through interpersonal influences with parents and peers.
Fig. 1.
Adaptation of the social-ecological model (modified from the Institute of Medicine( 132 )) in understanding environmental influences on disordered weight-control behaviours (DWCB). *Behavioural settings include a wide range of common settings to which individuals are exposed. ‘Homes’ are often included in this level of influence. Sectors of influence include established institutions, industries or markets in society
The environment has been well conceptualized for obesity prevention efforts, which focus primarily on establishing healthy dietary and physical activity behaviours( 21 – 23 ). A wealth of literature exists on the role of interpersonal influences, such as child feeding practices and parental modelling of dietary behaviours( 24 – 26 ), behavioural settings, such as the built food and physical activity environment( 21 , 22 , 27 ), and sectors of influence, such as policy and the food and beverage industry( 28 ), in driving the obesity epidemic. A recent conceptual review emphasized that there are many opportunities for integrating the prevention of obesity and eating disorders, particularly through environmental approaches( 29 ). However, there has been considerably less research on conceptualizing and measuring the full range of potentially important environmental influences on DWCB. Addressing this gap will be essential to advancing research on DWCB and informing the development of comprehensive and integrative programmes and policies.
Studies to date on DWCB have tended to focus on individual-level risk factors, such as body image and dissatisfaction, self-esteem and depression( 5 , 30 – 32 ), interpersonal factors, such as parent and peer influences( 16 , 33 – 35 ), and/or media influences( 36 – 39 ), whereas studies on behavioural settings and sectors of influence on DWCB have been sparse. No study to date to our knowledge has systematically reviewed the empirical literature on how various aspects of the environment may shape or prevent DWCB among youth. The present study aims to address this gap by reviewing studies’ examination of environmental influences on DWCB among youth over the past several years. Specific aims of the study were to: (i) examine the range of environmental domains that have been explored; (ii) compare studies’ participants, use of theory, measures and design; and (iii) review studies’ findings on the association between environmental influences and DWCB among youth.
Methods
Literature search
The process for identifying relevant articles was based on the Cochrane Handbook of Systematic Review of Interventions version 5·0·2( 40 ) and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines( 41 ). We first searched PubMed, PsycINFO and Google Scholar for relevant articles published from 1994 to December 2012 using the following search terms: ‘disordered weight control’ or ‘disordered eating’, ‘environment’ and ‘youth’. After eliminating duplicates and obtaining the initial set of relevant articles, reference lists of these articles were screened to acquire further relevant studies.
Selection criteria
Inclusion criteria for articles were: publication in English in peer-reviewed journals; research conducted with child or adolescent samples; utilization of an observational epidemiological study design; and examination of an environmental variable as an exposure and DWCB as an outcome. For the purpose of the review, an environmental variable was defined as any type of physical and/or social factor or relationship that is or takes place external to the individual, including levels and settings defined by the social-ecological model (Fig. 1). Media exposure and use were included as an environmental factor, as media is one way of assessing sociocultural influences. Individual attitudes, perceptions, cognitions and behaviours other than media use were not considered environmental variables.
Criteria for DWCB included any type of intentional weight-control behaviour that is considered extreme, disordered or unhealthy. Examples include: vomiting, taking laxatives or diuretics, taking diet pills without a prescription, skipping meals, fasting, smoking cigarettes for weight control and excessive exercising (i.e. exercising to the point that it interferes significantly with important activities, occurs at inappropriate times or settings, or continues despite injury and other medical complications)( 42 ). Binge eating was not considered a DWCB. Additionally, studies that defined DWCB or related terms using measures that focus only on eating disordered attitudes, body dissatisfaction, thoughts or intentions of engaging in DWCB or a composite score of eating disorder symptomatology that includes cognitions, attitudes and behaviours as outcomes were excluded, as the outcome of interest for the current review focuses exclusively on behaviours. We further excluded studies using clinical samples or samples of youth who have been clinically diagnosed with eating disorders, as individual behaviours concerning weight and eating among clinical samples are likely to be influenced by diagnosis and treatment interventions( 43 ). Intervention studies were excluded as there are very few preventive interventions specifically targeting environmental factors related to DWCB.
Methodological critique
As longitudinal studies are methodologically stronger than cross-sectional studies, the longitudinal studies were further evaluated for methodological rigour using a modified version of the Methodological Quality Rating Scale (MQRS) initially developed for evaluation of randomized controlled trials( 44 , 45 ) (see Supplemental Table 1 in the online supplementary material). The original scale consisted of twelve attributes, with a maximum score of 17( 44 ). We adapted the scale to include eight attributes (length of follow-up; attrition rate; theoretical basis; measures; statistical analyses; sample size; number of sites; and generalizability) appropriate for critiquing longitudinal, observational studies. Higher scores correspond to a more rigorous study design (maximum score of 20 for the studies in the present review). See Supplemental Table 1 (online supplementary material) for rating criteria. Studies that specifically discussed the application or use of a theory or conceptual model in guiding the research, tested a specific theory or model, and/or discussed assumptions of a theoretical model in order to justify the analysis were classified as studies explicitly guided by the theory or model identified.
Quality assessment
To examine inter-rater reliability of article coding, the first author (M.L.W.) coded all of the studies and a second coder (S.B.A.) independently reviewed a subset of articles (n 18) that were randomly selected without replacement using a coding scheme developed for the subset of studies.
Results
A total of 262 articles were identified through PubMed (n 22), PsycINFO (n 177) and Google Scholar (n 63), of which twenty-four were duplicates. After reviewing the full texts and reference lists of the remaining 238 articles, we identified as relevant ninety-three studies (seventy cross-sectional; twenty-three longitudinal) for review. Inter-rater reliability for coding of articles was 0·73, which demonstrates moderate to substantial agreement( 46 , 47 ). Supplemental Table 2 (online supplementary material) presents the characteristics (study sample, environmental exposure measure(s), DWCB measure, relevant survey instruments) of the cross-sectional studies. Supplemental Table 3 (online supplementary material) presents study characteristics, MQRS scores and findings of the longitudinal studies.
Range of environmental exposures/constructs examined
Table 1 presents common environmental constructs and corresponding examples that emerged from the articles reviewed organized by level of influence (interpersonal, behavioural settings, sectors of influence and sociocultural context). As several studies examined more than one type of environmental exposure, Fig. 2 presents the frequency and percentage of major categories of environmental exposures that were examined in the literature. Studies that analysed multiple environmental constructs were counted multiple times, with ninety-three studies and a total of 297 constructs counted. Family (51·5 %), peer (22·9 %) and media influences (9·4 %) represented the most commonly studied environmental exposures. Family- and peer-related influences had the greatest number and range regarding type of environmental construct examined in association with DWCB. Behavioural settings, including the school and home environment, were much less frequently examined as an exposure (5·4 %). Of the many sectors that may influence weight-related behaviours( 20 ), only media was examined in association with DWCB. General sociocultural influences represented 4·4 % of environmental exposures, and no studies were conducted on the built environment or policy influences (i.e. legislation regarding sale of diet pills and laxatives to minors) as exposures related to DWCB.
Table 1.
Common environmental constructs examined by level of influence
| Level of influence | Environmental constructs | |
|---|---|---|
| Interpersonal influences | ||
| Family influences | 1. | Attitudes and perceptions (importance of thinness to parents, approval or criticism of focal youth's current body weight or size, parents’ body dissatisfaction and weight concerns, parental pressures and expectations)( 13 , 14 , 33 , 35 , 37 , 49 , 62 , 67 , 79 , 82 , 98 , 105 , 108 , 114 , 115 , 118 , 133 , 134 ) |
| 2. | Modelling and reinforcement (parental modelling of dieting and other weight-related behaviours, parental encouragement or pressure for their children to diet, parental or sibling discussion of weight loss, parental expression of negative verbal messages regarding weight and shape)( 13 , 15 , 33 , 62 , 70 , 73 , 82 , 84 , 87 , 101 , 109 , 135 ) | |
| 3. | Quality of family relationships (family communication, family connectedness, family stress, parent–child relationship, cohesion, support, trust and conflict)( 33 , 35 , 48 , 49 , 51 , 57 , 60 , 63 , 65 , 69 , 73 , 82 , 84 , 87 – 89 , 101 , 103 , 104 , 107 , 108 , 112 , 114 – 116 , 136 – 138 ) | |
| 4. | Family practices and behaviours (appearance- or weight-related teasing from family members, family criticism, parental supervision and monitoring, parental promotion of their children's autonomy, parent involvement in schooling, parental alcohol problems)( 33 , 35 , 48 , 51 , 60 , 61 , 76 , 84 , 85 , 87 – 89 , 98 , 105 , 108 , 113 , 114 , 115 , 137 – 139 ) | |
| 5. | Family composition and history (one- or two-parent household, marital status of parents, family history of eating disorders, history of physical and/or sexual abuse from a family member)( 1 , 49 , 92 , 103 , 104 , 108 , 110 , 112 – 115 ) | |
| Peer influences | 1. | Attitudes and perceptions (importance of thinness to peers, approval or criticism of current body weight from peers)( 14 , 36 , 37 , 82 , 94 , 140 ) |
| 2. | Modelling and reinforcement (friends’ modelling of or engagement in dieting behaviours and/or DWCB, peer encouragement or pressure related to appearance and/or dieting, friends’ discussion of or interest in dieting methods, romantic partner or friend providing social reinforcement of thinness)( 35 , 49 , 70 , 79 , 81 , 82 , 89 , 101 , 109 , 118 , 133 , 134 , 141 ) | |
| 3. | Quality of peer relationships (peer support, peer connectedness, intimacy of friend relationships, level of communication and caring from peers, perceived popularity and acceptance among peers, social support)( 1 , 35 , 69 , 81 , 82 , 89 , 103 , 106 , 112 , 114 , 115 , 117 , 140 , 142 ) | |
| 4. | Peer practices and behaviours (appearance- or weight-related teasing from peers)( 35 , 36 , 51 , 85 , 86 , 89 , 94 , 137 , 138 , 141 , 143 ) | |
| 5. | Peer characteristics (friends who have been clinically diagnosed with an eating disorder)( 69 ) | |
| 6. | Peer experiences (dating violence)( 92 ) | |
| Other interpersonal influences | 1. | Connectedness to non-family members, non-family member adult support( 104 , 108 , 112 , 116 , 142 ) |
| Behavioural settings | 1. | Home food environment (family meal atmosphere, priority of family meals, family meal frequency, structure/rules during family meals, healthy food availability)( 33 , 35 , 48 , 51 , 87 – 89 , 144 ) |
| 2. | School-related perceptions (perception of school atmosphere)( 117 ) | |
| 3. | School characteristics and norms (school SES, type of ballet school attended, school-wide dieting norm, percentage of students eligible for free or reduced-price school lunch)( 9 , 18 , 52 , 120 ) | |
| 4. | School experiences (being bullied at school)( 117 ) | |
| 5. | School connectedness( 1 ) | |
| 6. | Neighbourhood poverty level( 9 ) | |
| Sectors of influence | 1. | TV viewing and exposure (overall TV viewing per week, amount of TV watched, thin-ideal TV exposure, physical appearances of TV characters)( 35 , 75 , 89 , 97 , 114 , 115 ) |
| 2. | Magazine use and exposure (frequency of reading thin-ideal, fitness and/or sports magazines)( 35 , 74 , 75 , 89 , 91 , 97 , 99 , 105 , 128 , 145 ) | |
| 3. | Selective exposure (exposure to specific types of media content based on interest in that content, such as fitness, dieting and sports)( 74 ) | |
| 4. | Perception and interpretation of media messages (perceived pressure from media to be thin, lose weight or build muscle, perception that media communicated a strong message that thinness was important, acceptance of thin stereotypes)( 67 , 78 , 95 , 106 , 134 ) | |
| 5. | Media influences on ideal body shape (importance of articles in influencing ideal body shape, interest in emulating models or looking like girls/women or boys/men in the media)( 93 , 105 ) | |
| Sociocultural context | 1. | Sociocultural ideals and norms related to thinness, body size and appearance( 72 , 76 , 80 , 119 ) |
| 2. | Sociocultural pressures related to weight and appearance( 14 , 118 ) | |
| 3. | Acculturation( 119 ) | |
| 4. | Cultural pride( 113 ) | |
| 5. | Perception of gender role prescriptions (appearance and gender role norms)( 66 ) | |
| 6. | Religion and religiosity (importance and attendance of religious events)( 63 , 71 , 116 ) | |
DWCB, disordered weight-control behaviours; SES, socio-economic status; TV, television.
Fig. 2.
Frequency of environmental constructs* ( , family, n 153;
, family, n 153;  , peers, n 68;
, peers, n 68;  , other interpersonal influences, n 9;
, other interpersonal influences, n 9;  , behavioural settings, n 16;
, behavioural settings, n 16;  , media, n 28;
, media, n 28;  , sociocultural influences, n 13;
, sociocultural influences, n 13;
 , environmental influences (from twin studies), n 10;
, environmental influences (from twin studies), n 10;  , built environment (BM), n 0;
, built environment (BM), n 0;  , policy, n 0) examined as exposure variables to disordered weight-control behaviours among youth. *Studies that examined multiple environmental constructs were counted multiple times, with ninety-three studies and a total of 297 constructs counted (grouped by the categories shown); n refers to the number of times a particular construct was examined, not the number of studies
, policy, n 0) examined as exposure variables to disordered weight-control behaviours among youth. *Studies that examined multiple environmental constructs were counted multiple times, with ninety-three studies and a total of 297 constructs counted (grouped by the categories shown); n refers to the number of times a particular construct was examined, not the number of studies
Theoretical basis
Most studies (69 %; n 64) did not explicitly identify a theoretical framework guiding the research. Over half of longitudinal studies (52 %; n 12) identified a theory or conceptual framework compared with 24 % (n 17) of cross-sectional studies. The following theories or constructs were cited as explicitly guiding the research: Social Cognitive Theory, gene–environment theory, socialization theory, achievement goal theory, social support, self-discrepancy theory, cumulative risk model, ecodevelopmental perspective, biosocial model, biopsychosocial model, the Catalyst Theory, feminist theory of conflicting gender roles, and thin-ideal internalization. Four studies developed and tested a specific conceptual model of the development of DWCB( 48 – 51 ).
Study populations
About half of the studies (n 45) were conducted with all-female samples, with no studies conducted on all-male samples. Less than half of the studies (46 %; n 43) included diverse or representative populations with respect to race/ethnicity and socio-economic status (SES). Most studies (61 %; n 57) had sample sizes of youth under 1000; twenty-six studies had 1000–9999 participants and ten studies had 10 000 or more participants. Two studies specifically recruited youth who participated in an aesthetic physical activity (i.e. gymnastics or ballet)( 52 , 53 ). Five studies examined genetic and environmental influences on DWCB using twin samples( 54 – 58 ), and nine studies included parent/caregivers of adolescents in the study( 13 , 15 , 37 , 59 – 64 ) to obtain multiple methods of data collection on measures of interest.
Study measures
The majority of environmental exposures and DWCB were assessed by various self-report surveys completed by youth with diverse measures used to assess the various environmental exposures of interest (see Supplemental Tables 2 and 3, online supplementary material). Commonly validated measures for DWCB assessment included scales or subscales such as the Eating Attitudes Test (EAT-26, EAT-40)( 65 – 68 ), the Bulimia Test and Bulimia Test Revised (BUILT, BUILT-R)( 53 , 69 , 70 ) and various subscales of the Eating Disorders Inventory (EDI)( 12 , 50 , 54 , 55 , 71 – 82 ), as well as validated items on DWCB used in study questionnaires, such as the Project Eating Among Teens (Project EAT) survey( 15 , 35 , 51 , 64 , 83 – 91 ), and items adapted from the Youth Risk Behavior Surveillance (YRBS) survey( 36 , 37 , 92 – 94 ). A number of studies (n 19) used items or surveys developed specifically for the study to assess DWCB.
Study design
The majority of studies (75 %; n 70) used a cross-sectional design. Figure 3 presents the length of follow-up and MQRS scores (mean = 10·8, range 5·7–20·0) of the twenty-three longitudinal studies. Average length of follow-up time was 3·6 years, with eleven studies having follow-up periods of 8 months to 2 years( 36 , 50 , 67 , 68 , 70 , 77 , 94 – 98 ) and the remaining twelve studies with follow-up periods ranging from 4 to 10 years( 17 , 35 , 37 , 48 , 56 , 57 , 58 , 83 , 88 , 89 , 99 , 100 ). Ten longitudinal studies had attrition rates under 20 %.
Fig. 3.

Length of study ( ) and methodological rigour (Methodological Quality Rating Scale (MQRS) score,
) and methodological rigour (Methodological Quality Rating Scale (MQRS) score,  ) of the longitudinal studies reviewed (n 23)
) of the longitudinal studies reviewed (n 23)
Overall results across studies
The wide range of definitions, operationalizations, measurement and analysis of environmental exposures in association with DWCB across studies limited our ability to standardize comparisons of studies’ effect size estimates; thus, we first describe general patterns in associations between environmental exposures and DWCB across all ninety-three studies, followed by a methodological critique of the longitudinal studies and synthesis of their findings.
Overall, the following family, peer and media influences were found to be positively associated with DWCB: negative weight-related comments and/or teasing from family members and peers( 13 , 34 , 35 , 37 , 67 , 79 , 83 , 90 , 101 ); parental and peer modelling and social reinforcement of dieting behaviours( 13 , 67 , 70 , 95 , 102 ); peer acceptance concerns( 103 , 104 ); parent and peer attitudes on dieting and weight concerns( 60 , 105 , 106 ); poor parental–child communication and/or relationships( 59 , 60 , 107 ); high parental supervision and monitoring( 108 ); family conflict( 59 , 65 ); lack of trust in parents( 59 ); fewer family meals( 1 , 33 , 35 , 87 , 88 , 89 , 107 ); high use of media (particularly content that portrays thin ideals)( 14 , 35 – 38 , 74 , 75 , 78 , 83 , 89 , 94 , 97 , 105 ); perceived pressure to be thin from various sources( 14 , 67 , 70 , 78 , 95 , 101 , 106 , 109 ); thin-ideal internalization( 70 , 74 , 75 , 95 ); and traumatic experiences, such as history of physical and/or sexual abuse or being bullied by peers( 49 , 92 , 103 , 104 , 110 – 117 ). One study found that negative comments from parents regarding body shape, eating, importance of physical appearance, or comparisons of shape and weight of other people explained a larger amount of the variance in girls’ disordered eating compared with boys( 79 ).
Environmental exposures that were protective against DWCB included: family connectedness and support( 1 , 89 , 108 , 116 ); positive family communication( 84 , 108 , 116 ); frequent family meals or dinners( 33 , 35 , 48 , 51 , 84 , 87 , 88 ); positive family meal environment (i.e. high priority for family meals, a positive atmosphere at family meals and a structured family meal environment)( 84 , 87 ); and connectedness to adults (non-family members from school or church)( 104 , 116 ). Family connectedness and positive family communication were strong protective factors for girls, and high perceived parental expectations were a strong protective factor for boys( 108 ). One study of a large co-gender sample( 94 ) found that parental, peer and media influences independently predicted constant dieting, with no one factor emerging as the primary source of influence.
In terms of behavioural settings, school-wide prevalence of trying to lose weight was associated with unhealthy weight-control behaviours among healthy-weight females and marginally associated among overweight females, adjusting for friends’ dieting behaviours( 17 ). Studies that examined the broader sociocultural environment or overall sociocultural influences found that perceived sociocultural or societal pressures related to appearance( 72 , 118 ), stronger identification with the Anglo culture among Latino youth living in the USA( 119 ) and higher agreement with socially sanctioned standards of beauty and thinness( 119 ) were associated with DWCB. One study that explored percentage of students eligible for free or reduced-priced school lunch and percentage of residents living at or below poverty in the student's neighbourhood found that the latter was positively associated with DWCB among boys( 9 ). School SES was not found to be associated with DWCB among adolescent females( 120 ). No studies that examined the built environment, neighbourhood/community influences, industries such as those promoting fashion, weight loss, diet pills, laxatives or cosmetic surgery, or policy influences on DWCB were found.
Gene–environment studies using twin samples examined shared and non-shared environmental influences on DWCB. According to Klump et al.( 54 – 56 ), non-shared environmental influences are those that are ‘unique to individuals reared in the same family and contribute to differences among family members’, whereas shared environmental influences are ‘those that are common to individuals reared in the same family and that contribute to familial similarity’. However, most of these studies did not specify or measure shared and non-shared environment factors; shared environmental influence was inferred if both monozygotic and dizygotic twin correlations were similar in magnitude and statistically significant, whereas non-shared environmental influence was suggested if these correlations were small. Thus, the specific type of environmental influence that contributed significantly to DWCB was often unclear from these studies.
Longitudinal studies’ findings
Finally, we examined longitudinal studies’ findings within the context of their MQRS scores, which were heavily correlated with study length of follow-up (see Fig. 3). Similar to cross-sectional studies, parental, peer and media influences emerged as the most frequent exposures examined in relation to DWCB (see Supplemental Table 3, online supplementary material). Studies varied in their presentation of outcome effects, including odds ratios, mean scores on various DWCB instruments, percentage of participants who engaged in DWCB at various time points, correlations and percentage of variance explained. The following findings across studies scoring in the top 50th percentile (MQRS ≥ 12) were significant in predicting DWCB for males and females: friend/peer dieting behaviours as a risk factor (1·4–3·7 times increase in the percentage participating in DWCB( 17 ); OR = 1·2–1·6)( 35 , 89 ); weight-related teasing as a risk factor (OR = 1·4–1·8)( 35 , 83 ); exposure to weight-loss magazines (OR = 1·4–1·6)( 35 , 89 ); and family connectedness as protective factors (OR = 0·8–0·9)( 89 ). Several gender differences emerged in studies’ findings: parental weight concerns and behaviours were a risk factor for females (OR = 1·2–1·3)( 35 ); frequent family meals were protective against DWCB among females (OR = 0·7–0·9) but increased risk for skipping meals and eating very little food among males (OR = 1·8)( 35 , 88 ); positive family atmosphere was protective for females (OR = 0·6–0·8)( 35 , 89 ); maternal history of an eating disorder (OR = 2·8) and trying to look like females in the media were risk factors for females (OR = 1·5)( 37 ); and importance of weight to peers (OR = 3·4)( 37 ), friend connectedness (OR = 1·7)( 35 ) and low social support from family and friends (β = 0·2) were risk factors among males( 100 ). A dose–response association was observed between frequency of reading diet/weight-loss magazine articles and DWCB among females (OR = 2·0–3·2 for those who often read these types of articles v. those who never read these articles)( 99 ).
Two longitudinal studies conducted with twins explicitly measured specific types of environmental influence (parent–child conflict( 56 ); maternal warmth, school problems and media use( 58 )) in the gene–environment analysis. Results indicated that differences in parent–child conflict between identical adolescent twins were a consequence, rather than a predictor, of disordered eating (r s = 0·1–0·3)( 57 ) and that media use was associated with reduced DWCB (β = −0·3) among dizygotic twins( 58 ). Franko and colleagues’ 10-year longitudinal study, consisting of annual assessments of family meal frequency, family cohesion, extreme weight-control behaviours and bulimia among 2379 white and black females (age 9·5 years at baseline), yielded the highest MQRS score (20). This particular study demonstrated that the protective association between family meal frequency during years 1 and 3 and scores on a bulimia scale at year 10 (score = 2·1 for never/almost have family meals v. score = 1·4 always/usually have family meals) was mediated by greater family cohesion (β = 0·05). Guided by a clear conceptual model, Franko et al.'s longitudinal study provided the strongest evidence for family cohesion, promoted through eating together as a family, as protective against DWCB 10 years later among female youth( 48 ).
Discussion
The aim of the present paper was to review the literature on environmental influences on DWCB among youth. Studies primarily examined parental influences, peer influences and the media in association with DWCB. The focus on observational, epidemiological studies included in our review allowed us to examine the range of environmental influences on DWCB at the population level and to identify behavioural settings and sectors where preventive measures can be implemented. The following subsections highlight key patterns observed in the studies reviewed with corresponding recommendations to guide future research and interventions on DWCB.
Study design and methodology
The large majority of the research reviewed utilized cross-sectional designs, and over half of the longitudinal studies reviewed had follow-up periods of two or fewer years.
Recommendation #1
Additional longitudinal studies with longer follow-up periods (i.e. longer than 2 years) are needed to establish the trajectory of the magnitude and significance of the protective or risk effects of environmental exposures over time. For example, to what extent do frequent family meals remain protective against DWCB over time? At what age(s) are parental modelling of weight-related behaviours, peer dieting behaviours, weight-related teasing and exposure to diet/weight-loss media most critical? Lengthier follow-up time frames will allow investigators to identify sensitive periods or developmental stages during which risk or protective factors exert the most influence.
No studies in the current review applied multilevel design and analysis in examining environmental influences on DWCB. A recent study by Austin and colleagues (published outside the year range specified for the review) used multilevel modelling to estimate odds of DWCB and school-level variation in DWCB among a large sample of middle-school youth( 121 ). Results indicated that the prevalence of DWCB varied widely across schools (<1 % to 12 % of the student population) and that school-neighbourhood poverty was associated with higher odds of DWCB among males. However, multilevel methodology remains largely underutilized in the DWCB literature, and further multilevel research is warranted on the role of school-level influences on DWCB. Several multilevel studies in the obesity literature have demonstrated the unique contribution of environmental characteristics, such as fast-food density, proximity to fast-food outlets and neighbourhood walkability, in influencing obesity risk over and above individual characteristics and behaviours( 122 – 125 ). These studies provide a strong evidence base for the development of environmental and ecological interventions as part of comprehensive efforts to address obesity. Similar approaches can be undertaken to prevent DWCB, as obesity and DWCB are influenced by similar environmental characteristics.
Recommendation #2
To advance the field, methods appropriate for multilevel study design and analysis are necessary to better identify and disentangle levels of influence that are associated with DWCB. Given that obesity and DWCB have shared risk and protective factors at the individual and interpersonal level( 35 , 83 ), and the higher odds of DWCB observed among overweight and obese adolescents than their healthy-weight peers( 11 ), it may be possible that obesogenic environments also promote DWCB. Multilevel analysis of environmental influences (including the built food and physical activity environment, as well as the media environment) on DWCB will be important to demonstrate which environmental factors affect both obesity and DWCB, thus providing stronger justification for policy and environmental changes that create not only a non-obesogenic environment, but also a health-promoting environment.
Exposures of interest
Most studies in the current review, both cross-sectional and longitudinal, have focused on family influences, followed by peer and media influences, as exposures associated with DWCB or predictors of DWCB. However, very few studies examined school- and neighbourhood-level factors, the built environment, industry or policy influences on DWCB. Addressing this conceptual gap in the literature is essential, as various behavioural settings and sectors of influence may provide different magnitudes of influence throughout child and adolescent development. For example, as youth transition from childhood to adolescence, the role of peer and school environment influences may increase in shaping or preventing the development of DWCB( 126 ). Advances in technology, including the globalization of media, are outpacing the rate at which science can understand their effects, both short-term and long-term, on weight-related behaviours as well as other health behaviours and outcomes. It is imperative to change this trend by addressing current gaps in the DWCB literature, moving beyond existing measures of the environment and examining novel ways of measuring environmental exposures, and to be aware of new exposures that emerge.
Recommendation #3
To better understand the development of DWCB, future studies should examine behavioural settings (i.e. schools, neighbourhoods, the built environment), sectors of influence (i.e. industry, policy) and overarching sociocultural influences, as these domains have not been well explored in the literature. For example, developing a measure to assess the globalization and spread of media, specifically the sociocultural ideals of body size and shape, may be used to examine sociocultural influences on DWCB across countries and cultures. Additionally, examining density and frequency of exposure to thin-ideal media (i.e. billboards, subway advertisements) or unhealthy weight-loss products (i.e. diet pill and laxative product placement and/or promotion in stores) will be important to assess, as findings on the role of advertising from these underexplored sectors of influence (fashion, cosmetic, diet pill and laxative industries) on DWCB among youth may provide evidence for policy regulations and restrictions on advertising and sale of diet pills, laxatives and other weight-loss products from these industries to minors( 127 ).
Study samples
With regard to study samples, the majority of articles reviewed focused on all-female participants and/or primarily white participants. Previous articles have justified the homogeneity of their study samples with the argument that disordered eating behaviours, DWCB and/or eating disorders occur primarily among white females of middle to high SES( 128 , 129 ). However, the literature does not support this argument, and some studies have found that youth from certain non-white racial/ethnic groups (i.e. blacks, Hispanics, Native Americans, Hawaiian/Pacific Islanders) may be at similar or increased risk for engaging in DWCB compared with their white peers( 9 , 130 ). Given the fast rate at which health behaviours and outcomes change (as seen with the rapid growth of overweight and obesity among youth over the past three decades)( 131 ), it is important to avoid assumptions about health behaviours and outcomes associated with certain genders, racial/ethnic groups and/or SES that may prevent the identification of populations who are at risk and who would benefit from medical and public health intervention and prevention efforts. Another example is the protective effect of frequent family meals on DWCB consistently observed among females but not among males, which may be partially attributed to the greater number of studies examining family meals and DWCB on all-female participants.
Recommendation #4
Future quantitative and qualitative studies should include males, racially/ethnically diverse samples and socio-economically diverse samples in order to capture all populations that may potentially engage in DWCB, better understand mechanisms driving disparities in DWCB and develop gender- and/or culturally tailored interventions. For example, family-based interventions that encourage family cohesion and connectedness through frequent family meals may be highly effective among females, whereas another type of family-based strategy that promotes family cohesion and connectedness may be needed to prevent DWCB among males.
Twin studies
Another pattern that emerged was that studies examining twin samples broadly categorized and analysed the environment as ‘shared’ and ‘non-shared’ or ‘unique’ environmental influences( 12 , 54 – 57 ). Although examples of shared and non-shared environmental influences were sometimes specified in the introduction (i.e. non-shared environmental influences included differential treatment by parents, siblings and peers and unique life events; shared environmental influences included SES and general child-rearing practices), most of these studies did not distinguish or measure different types of shared and non-shared environmental influences in their study design and analysis and inferred shared and/or non-shared environmental influences based on the magnitude and statistical significance of monozygotic and dizygotic twin correlations( 54 – 56 ). Furthermore, the one twin study that identified specific environmental factors with an effect estimate calculated (as opposed to percentage of the variance explained) reported that media use (frequency of television and computer game use) was associated with reduced DWCB( 58 ), which is inconsistent with other studies’ findings among larger, more general study samples that utilized a more specific measure of media in relation to DWCB (i.e. media exposure to dieting/weight-loss magazines; influence of thinness in media)( 35 – 37 , 89 , 94 , 99 ).
Recommendation #5
Future studies that aim to disentangle genetic and environmental influences on DWCB using twin samples should clearly define, measure and analyse shared and non-shared aspects of the environment. The explicit measurement and operationalization of environmental factors, guided by a theoretical framework that clearly conceptualizes the role of the environment and its relation to genetics in influencing risk for DWCB, is essential to better understand gene–environment interactions, particularly as there are numerous environmental levels of influence that are as interrelated and complex as individual-level factors.
Strengths and limitations
To date, no study to the authors’ knowledge has systematically reviewed the use of theoretical frameworks and constructs in guiding the development of research of environmental factors on DWCB among youth. The present results highlight conceptual and methodological gaps in the literature. Furthermore, findings from the present review can guide future research, such as further exploring certain environmental domains that are not well studied and the use of analytic methods designed for the study of multilevel and environmental influences. The inclusion and exclusion criteria used for the current review of the literature may limit the generalizability of the study's findings to other literature (i.e. studies with adults, youth clinically diagnosed with eating disorders), symptom types (i.e. binge eating, disordered eating attitudes) and cultures (i.e. non-English speaking) that were not included.
Conclusions
Findings from the current review indicate that multiple aspects of the environment can be critical in shaping and preventing the development of DWCB among youth. Future research on DWCB can address conceptual gaps in the literature by examining unexplored or understudied environmental influences and target methodological gaps by utilizing multilevel design and analysis. Findings from multilevel studies can parse out the relative contributions of environmental v. individual-level influences on DWCB and thus guide the development of intervention strategies (i.e. counselling, family-based or peer-based behavioural programmes, changes in the social or physical environment, or a combination of these) that would be most effective in preventing DWCB and promoting healthy eating and physical activity behaviours among youth. Additionally, clinicians, nurses, programme planners and researchers in public health and medicine should recognize that DWCB are not limited to white female adolescents but are a growing concern for both boys and girls and for youth across racial/ethnic and SES groups. The growing incidence of DWCB among youth, compounded by the increase in obesity and overweight among youth over the past few decades, demands multidisciplinary and collaborative efforts to promote healthy ways to lose or maintain weight.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980013001407
Acknowledgements
Sources of funding: M.L.W. is supported by the Ellen Feldberg Gordon Fund for Eating Disorders Research, the Strategic Training Initiative for the Prevention of Eating Disorders Dissertation Research Award, and the Maternal and Child Health Bureau grant MCHB 5T76 MC 00001. S.B.A. is supported by the Leadership Education in Adolescent Health project, Maternal and Child Health Bureau, HRSA grant 6T71-MC00009. Conflicts of interest: The authors do not have any conflicts of interest or any financial interests to disclose. Ethics: Ethical approval was not required. Authors’ contributions: M.L.W. conducted the systematic review and wrote the manuscript. S.B.A. served as an independent rater of a subset of studies included in the review. S.B.A., K.E.P. and M.C.M. contributed to the study design methodology and revision of the manuscript.
References
- 1. Croll J, Neumark-Sztainer D, Story M et al. (2002) Prevalence and risk and protective factors related to disordered eating behaviors among adolescents: relationship to gender and ethnicity. J Adolesc Health 31, 166–175. [DOI] [PubMed] [Google Scholar]
- 2. Herzog W, Deter HC, Fiehn W et al. (1997) Medical findings and predictors of long-term physical outcome in anorexia nervosa: a prospective, 12-year follow-up study. Psychol Med 27, 269–279. [DOI] [PubMed] [Google Scholar]
- 3. Mitchell JE (1995) Medical complications of bulimia nervosa. In Eating Disorders and Obesity: A Comprehensive Handbook, pp. 271–275 [KD Brownell and CG Fairburn, editors]. New York: Guilford Press. [Google Scholar]
- 4. Austin SB, Ziyadeh NJ, Vohra S et al. (2008) Irregular menses linked to vomiting in a nonclinical sample: findings from the National Eating Disorders Screening Program in high schools. J Adolesc Health 42, 450–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Santos M, Richards CS & Bleckley MK (2007) Comorbidity between depression and disordered eating in adolescents. Eating Behav 8, 440–449. [DOI] [PubMed] [Google Scholar]
- 6. Nattiv A, Loucks AB, Manore MM et al. (2007) American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc 39, 1867–1882. [DOI] [PubMed] [Google Scholar]
- 7. Otis CL, Drinkwater B, Johnson M et al. (1997) American College of Sports Medicine position stand. The female athlete triad. Med Sci Sports Exerc 29, i–ix. [DOI] [PubMed] [Google Scholar]
- 8. Austin SB, Field AE, Wiecha J et al. (2005) The impact of a school-based obesity prevention trial on disordered weight-control behaviors in early adolescent girls. Arch Pediatr Adolesc Med 159, 225–230. [DOI] [PubMed] [Google Scholar]
- 9. Austin SB, Spadano-Gasbarro J, Greaney ML et al. (2011) Disordered weight control behaviors in early adolescent boys and girls of color: an under-recognized factor in the epidemic of childhood overweight. J Adolesc Health 48, 109–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Austin SB, Kim J, Wiecha J et al. (2007) School-based overweight preventive intervention lowers incidence of disordered weight-control behaviors in early adolescent girls. Arch Pediatr Adolesc Med 161, 865–869. [DOI] [PubMed] [Google Scholar]
- 11. Wang ML, Walls CE, Peterson KE et al. (2013) Dietary and physical activity factors related to eating disorder symptoms among middle school youth. J Sch Health 83, 14–20. [DOI] [PubMed] [Google Scholar]
- 12. Baker JH, Maes HH, Lissner L et al. (2009) Genetic risk factors for disordered eating in adolescent males and females. J Abnorm Psychol 118, 576–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Keel PK, Heatherton TF, Harnden JL et al. (1997) Mothers, fathers and daughters: dieting and disordered eating. Eat Disord 5, 216–228. [Google Scholar]
- 14. Grigg M, Bowman J & Redman S (1996) Disordered eating and unhealthy weight reduction practices among adolescent females. Prev Med 25, 748–756. [DOI] [PubMed] [Google Scholar]
- 15. Fulkerson JA, McGuire MT, Neumark-Sztainer D et al. (2002) Weight-related attitudes and behaviors of adolescent boys and girls who are encouraged to diet by their mothers. Int J Obes Relat Metab Disord 26, 1579–1587. [DOI] [PubMed] [Google Scholar]
- 16. Eisenberg ME, Berge JM, Fulkerson JA et al. (2012) Associations between hurtful weight-related comments by family and significant other and the development of disordered eating behaviors in young adults. J Behav Med 35, 500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eisenberg ME & Neumark-Sztainer D (2010) Friends’ dieting and disordered eating behaviors among adolescents five years later: findings from Project EAT. J Adolesc Health 47, 67–73. [DOI] [PubMed] [Google Scholar]
- 18. Eisenberg ME, Neumark-Sztainer D, Story M et al. (2005) The role of social norms and friends’ influences on unhealthy weight-control behaviors among adolescent girls. Soc Sci Med 60, 1165–1173. [DOI] [PubMed] [Google Scholar]
- 19. Institute of Medicine (2005) Preventing Childhood Obesity: Health in the Balance [JP Koplan, CT Liverman and VI Kraak, editors]. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- 20. Swinburn BA, Sacks G, Hall KD et al. (2011) The global obesity pandemic: shaped by global drivers and local environments. Lancet 378, 804–814. [DOI] [PubMed] [Google Scholar]
- 21. Sallis JF & Glanz K (2006) The role of built environments in physical activity, eating, and obesity in childhood. Future Child 16, 89–108. [DOI] [PubMed] [Google Scholar]
- 22. Millstein RA, Strobel J, Kerr J et al. (2011) Home, school, and neighborhood environment factors and youth physical activity. Pediatr Exerc Sci 23, 487–503. [DOI] [PubMed] [Google Scholar]
- 23. Norman GJ, Schmid BA, Sallis JF et al. (2005) Psychosocial and environmental correlates of adolescent sedentary behaviors. Pediatrics 116, 908–916. [DOI] [PubMed] [Google Scholar]
- 24. Campbell KJ, Crawford DA & Ball K (2006) Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. Int J Obes (Lond) 30, 1272–1280. [DOI] [PubMed] [Google Scholar]
- 25. Campbell KJ, Crawford DA, Salmon J et al. (2007) Associations between the home food environment and obesity-promoting eating behaviors in adolescence. Obesity (Silver Spring) 15, 719–730. [DOI] [PubMed] [Google Scholar]
- 26. Birch LL & Fisher JO (2000) Mothers’ child-feeding practices influence daughters’ eating and weight. Am J Clin Nutr 71, 1054–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nichol M, Janssen I & Pickett W (2010) Associations between neighborhood safety, availability of recreational facilities, and adolescent physical activity among Canadian youth. J Phys Act Health 7, 442–450. [DOI] [PubMed] [Google Scholar]
- 28. Kim D & Kawachi I (2006) Food taxation and pricing strategies to ‘thin out’ the obesity epidemic. Am J Prev Med 30, 430–437. [DOI] [PubMed] [Google Scholar]
- 29. Sanchez-Carracedo D, Neumark-Sztainer D & Lopez-Guimera G (2012) Integrated prevention of obesity and eating disorders: barriers, developments and opportunities. Public Health Nutr 15, 2295–2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Katsounari I (2009) Self-esteem, depression and eating disordered attitudes: a cross-cultural comparison between Cypriot and British young women. Eur Eat Disord Rev 17, 455–461. [DOI] [PubMed] [Google Scholar]
- 31. Littleton HL & Ollendick T (2003) Negative body image and disordered eating behavior in children and adolescents: what places youth at risk and how can these problems be prevented? Clin Child Fam Psychol Rev 6, 51–66. [DOI] [PubMed] [Google Scholar]
- 32. Ackard DM, Croll JK & Kearney-Cooke A (2002) Dieting frequency among college females: association with disordered eating, body image, and related psychological problems. J Psychosom Res 52, 129–136. [DOI] [PubMed] [Google Scholar]
- 33. Fulkerson JA, Story M, Mellin A et al. (2006) Family dinner meal frequency and adolescent development: relationships with developmental assets and high-risk behaviors. J Adolesc Health 39, 337–345. [DOI] [PubMed] [Google Scholar]
- 34. Haines J, Kleinman KP, Rifas-Shiman SL et al. (2010) Examination of shared risk and protective factors for overweight and disordered eating among adolescents. Arch Pediatr Adolesc Med 164, 336–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Neumark-Sztainer DR, Wall MM, Haines JI et al. (2007) Shared risk and protective factors for overweight and disordered eating in adolescents. Am J Prev Med 33, 359–369. [DOI] [PubMed] [Google Scholar]
- 36. Field AE, Camargo CA Jr, Taylor CB et al. (1999) Relation of peer and media influences to the development of purging behaviors among preadolescent and adolescent girls. Arch Pediatr Adolesc Med 153, 1184–1189. [DOI] [PubMed] [Google Scholar]
- 37. Field AE, Javaras KM, Aneja P et al. (2008) Family, peer, and media predictors of becoming eating disordered. Arch Pediatr Adolesc Med 162, 574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McCabe MP, Ricciardelli L, Mellor D et al. (2005) Media influences on body image and disordered eating among indigenous adolescent Australians. Adolescence 40, 115–127. [PubMed] [Google Scholar]
- 39. Tiggemann M & Pickering AS (1996) Role of television in adolescent women's body dissatisfaction and drive for thinness. Int J Eat Disord 20, 199–203. [DOI] [PubMed] [Google Scholar]
- 40. Higgins JPT & Green S (editors) (2009) Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration. http://www.cochrane.org/training/cochrane-handbook
- 41. Liberati A, Altman DG, Tetzlaff J et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339, b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. American Psychiatric Association (2000) Diagnostic and Statistical Manual for Mental Disorders, 4th ed. Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Association. [Google Scholar]
- 43. Rodgers R & Chabrol H (2009) Parental attitudes, body image disturbance and disordered eating amongst adolescents and young adults: a review. Eur Eat Disord Rev 17, 137–151. [DOI] [PubMed] [Google Scholar]
- 44. Miller WR, Brown JM, Simpson TL et al. (1995) What works? A methodological analysis of the alcohol treatment outcome literature. In Handbook of Alcoholism Treatment Approaches: Effective Alternatives, 2nd ed., pp. 12–44 [RK Hester and WR Miller, editors]. Needham Heights, MA: Allyn & Bacon. [Google Scholar]
- 45. Sung-Chan P, Sung YW, Zhao X et al. (2012) Family-based models for childhood-obesity intervention: a systematic review of randomized controlled trials. Obes Rev (Epublication ahead of print version). [DOI] [PubMed] [Google Scholar]
- 46. Grove WM, Andreasen NC, McDonald-Scott P et al. (1981) Reliability studies of psychiatric diagnosis. Theory and practice. Arch Gen Psychiatry 38, 408–413. [DOI] [PubMed] [Google Scholar]
- 47. Rietveld T & van Hout R (1993) Statistical Techniques for the Study of Language and Language Behavior. Berlin: Mouton de Gruyter. [Google Scholar]
- 48. Franko DL, Thompson D, Affenito SG et al. (2008) What mediates the relationship between family meals and adolescent health issues. Health Psychol 27, 2 Suppl., S109–S117. [DOI] [PubMed] [Google Scholar]
- 49. Neumark-Sztainer D, Story M, Toporoff E et al. (1996) Psychosocial predictors of binge eating and purging behaviors among adolescents with and without diabetes mellitus. J Adolesc Health 19, 289–296. [DOI] [PubMed] [Google Scholar]
- 50. Wertheim EH, Koerner J & Paxton SJ (2001) Longitudinal predictors of restrictive eating and bulimic tendencies in three different age groups of adolescent girls. J Youth Adolesc 30, 69–81. [Google Scholar]
- 51. Neumark-Sztainer D, Hannan PJ, Story M et al. (2003) Family meal patterns: associations with sociodemographic characteristics and improved dietary intake among adolescents. J Am Diet Assoc 103, 317–322. [DOI] [PubMed] [Google Scholar]
- 52. Thomas JJ, Keel PK & Heatherton TF (2005) Disordered eating attitudes and behaviors in ballet students: examination of environmental and individual risk factors. Int J Eat Disord 38, 263–268. [DOI] [PubMed] [Google Scholar]
- 53. de Bruin AP Bakker FC & Oudejans RRD (2009) Achievement goal theory and disordered eating: disordered eating with goal orientations and motivational climate in female gymnasts and dancers. Psychol Sport Exerc 10, 72–79. [Google Scholar]
- 54. Klump KL, McGue M & Iacono WG (2000) Age differences in genetic and environmental influences on eating attitudes and behaviors in preadolescent and adolescent female twins. J Abnorm Psychol 109, 239–251. [PubMed] [Google Scholar]
- 55. Klump KL, McGue M & Iacono WG (2002) Genetic relationships between personality and eating attitudes and behaviors. J Abnorm Psychol 111, 380–389. [DOI] [PubMed] [Google Scholar]
- 56. Klump KL, Burt SA, McGue M et al. (2007) Changes in genetic and environmental influences on disordered eating across adolescence: a longitudinal twin study. Arch Gen Psychiatry 64, 1409–1415. [DOI] [PubMed] [Google Scholar]
- 57. Spanos A, Klump KL, Burt SA et al. (2010) A longitudinal investigation of the relationship between disordered eating attitudes and behaviors and parent–child conflict: a monozygotic twin differences design. J Abnorm Psychol 119, 293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Ferguson CJ MM, Winegard B & Winegard B (2012) Influence of heritability, neuroticism, maternal warmth and media use on disordered eating behaviors: a prospective analysis of twins. Psychiatr Q 83, 353–360. [DOI] [PubMed] [Google Scholar]
- 59. Maharaj SI, Rodin GM, Olmsted MP et al. (1998) Eating disturbances, diabetes and the family: an empirical study. J Psychosom Res 44, 479–490. [DOI] [PubMed] [Google Scholar]
- 60. Maharaj SI, Rodin GM, Olmsted MP et al. (2003) Eating disturbances in girls with diabetes: the contribution of adolescent self-concept, maternal weight and shape concerns and mother–daughter relationships. Psychol Med 33, 525–539. [DOI] [PubMed] [Google Scholar]
- 61. Maharaj S, Rodin G, Connolly J et al. (2001) Eating problems and the observed quality of mother–daughter interactions among girls with type 1 diabetes. J Consult Clin Psychol 69, 950–958. [PubMed] [Google Scholar]
- 62. Benedikt R, Wertheim EH & Love A (1998) Eating attitudes and weight-loss attempts in female adolescents and their mothers. J Youth Adolesc 27, 43–57. [Google Scholar]
- 63. Hill AJ & Franklin JA (1998) Mothers, daughters and dieting: investigating the transmission of weight control. Br J Clin Psychol 37, 3–13. [DOI] [PubMed] [Google Scholar]
- 64. Keery H, Eisenberg ME, Boutelle K et al. (2006) Relationships between maternal and adolescent weight-related behaviors and concerns: the role of perception. J Psychosom Res 61, 105–111. [DOI] [PubMed] [Google Scholar]
- 65. Lee AM & Lee S (1996) Disordered eating and its psychosocial correlates among Chinese adolescent females in Hong Kong. Int J Eat Disord 20, 177–183. [DOI] [PubMed] [Google Scholar]
- 66. Mensinger JL, Bonifazi DZ & LaRosa J (2007) Perceived gender role prescriptions in schools, the superwoman ideal, and disordered eating among adolescent girls. Sex Roles 57, 557–568. [Google Scholar]
- 67. Shomaker LB & Furman W (2009) Interpersonal influences on late adolescent girls’ and boys’ disordered eating. Eat Behav 10, 97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Espinoza P, Penelo E & Raich RM (2010) Disordered eating behaviors and body image in a longitudinal pilot study of adolescent girls: what happens 2 years later? Body Image 7, 70–73. [DOI] [PubMed] [Google Scholar]
- 69. Pike KM (1995) Bulimic symptomatology in high school girls. Psychol Women Q 19, 373–396. [Google Scholar]
- 70. Stice E (1998) Modeling of eating pathology and social reinforcement of the thin-ideal predict onset of bulimic symptoms. Behav Res Ther 36, 931–944. [DOI] [PubMed] [Google Scholar]
- 71. Borjorquez I & Unikel C (2004) Presence of disordered eating among Mexican teenage women from a semi-urban area: its relation to the cultural hypothesis. Eur Eat Disord 12, 197–202. [Google Scholar]
- 72. Griffiths JA & McCabe MP (2000) The influence of significant others on disordered eating and body dissatisfaction among early adolescent girls. Eur Eat Disord 8, 301–314. [Google Scholar]
- 73. Hanna AC & Bond MJ (2006) Relationships between family conflict, perceived maternal verbal messages, and daughters’ disturbed eating symptomatology. Appetite 47, 205–211. [DOI] [PubMed] [Google Scholar]
- 74. Harrison K (2000) Television viewing, fat stereotyping, body shape standards, and eating disorder symptomatology in grade school children. Commun Res 27, 617–640. [Google Scholar]
- 75. Harrison K (2001) Ourselves, our bodies: thin-ideal medial, self-discrepancies, and eating disorder symptomatology in adolescents. J Soc Clin Psychol 20, 289–323. [Google Scholar]
- 76. Keery H, Boutelle K, van den Berg P et al. (2005) The impact of appearance-related teasing by family members. J Adolesc Health 37, 120–127. [DOI] [PubMed] [Google Scholar]
- 77. McCabe MP & Ricciardelli LA (2004) A longitudinal study of pubertal timing and extreme body change behaviors among adolescent boys and girls. Adolescence 39, 145–166. [PubMed] [Google Scholar]
- 78. Peterson KA, Paulson SE & Williams KK (2007) Relations of eating disorder symptomology with perceptions of pressures from mother, peers, and media in adolescent girls and boys. Sex Roles 57, 629–639. [Google Scholar]
- 79. Rodgers RF, Faure K & Chabrol H (2009) Gender differences in parental influences on adolescent body dissatisfaction and disordered eating. Sex Roles 61, 837–849. [Google Scholar]
- 80. Sanderson CA, Wallier JM & Stockdale JE (2008) Who feels discrepant and how does feeling discrepant matter? Examining the presence and consequences of feeling discrepant from personal and social norms related to thinness in American British high school girls. J Soc Clin Psychol 27, 995–1020. [Google Scholar]
- 81. Schutz HK & Paxton SJ (2007) Friendship quality, body dissatisfaction, dieting and disordered eating in adolescent girls. Br J Clin Psychol 46, 67–83. [DOI] [PubMed] [Google Scholar]
- 82. Vincent M & McCabe MP (2000) Gender differences among adolescents in family, and peer influences on body dissatisfaction, weight loss, and binge eating behaviors. J Youth Adolesc 29, 205–221. [Google Scholar]
- 83. Haines J & Neumark-Sztainer D (2006) Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res 21, 770–782. [DOI] [PubMed] [Google Scholar]
- 84. Fulkerson JA, Strauss J, Neumark-Sztainer D et al. (2007) Correlates of psychosocial well-being among overweight adolescents: the role of the family. J Consult Clin Psychol 75, 181–186. [DOI] [PubMed] [Google Scholar]
- 85. Libbey HP, Story MT, Neumark-Sztainer DR et al. (2008) Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity (Silver Spring) 16, Suppl. 2, S24–S29. [DOI] [PubMed] [Google Scholar]
- 86. Neumark-Sztainer D, Story M, Hannan PJ et al. (2002) Weight-related concerns and behaviors among overweight and nonoverweight adolescents: implications for preventing weight-related disorders. Arch Pediatr Adolesc Med 156, 171–178. [DOI] [PubMed] [Google Scholar]
- 87. Neumark-Sztainer D, Wall M, Story M et al. (2004) Are family meal patterns associated with disordered eating behaviors among adolescents? J Adolesc Health 35, 350–359. [DOI] [PubMed] [Google Scholar]
- 88. Neumark-Sztainer D, Eisenberg ME, Fulkerson JA et al. (2008) Family meals and disordered eating in adolescents: longitudinal findings from Project EAT. Arch Pediatr Adolesc Med 162, 17–22. [DOI] [PubMed] [Google Scholar]
- 89. Neumark-Sztainer D, Wall M, Story M et al. (2009) Five-year longitudinal predictive factors for disordered eating in a population-based sample of overweight adolescents: implications for prevention and treatment. Int J Eat Disord 42, 664–672. [DOI] [PubMed] [Google Scholar]
- 90. Neumark-Sztainer D, Bauer KW, Friend S et al. (2010) Family weight talk and dieting: how much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health 47, 270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Utter J, Neumark-Sztainer D, Wall M et al. (2003) Reading magazine articles about dieting and associated weight control behaviors among adolescents. J Adolesc Health 32, 78–82. [DOI] [PubMed] [Google Scholar]
- 92. Ackard DM & Neumark-Sztainer D (2002) Date violence and date rape among adolescents: associations with disordered eating behaviors and psychological health. Child Abuse Negl 26, 455–473. [DOI] [PubMed] [Google Scholar]
- 93. Austin SB, Ziyadeh N, Kahn JA et al. (2004) Sexual orientation, weight concerns, and eating-disordered behaviors in adolescent girls and boys. J Am Acad Child Adolesc Psychiatry 43, 1115–1123. [DOI] [PubMed] [Google Scholar]
- 94. Field AE, Camargo CA Jr, Taylor CB et al. (2001) Peer, parent, and media influences on the development of weight concerns and frequent dieting among preadolescent and adolescent girls and boys. Pediatrics 107, 54–60. [DOI] [PubMed] [Google Scholar]
- 95. Stice E & Agras WS (1998) Predicting onset and cessation of bulimic behaviors during adolescence: a longitudinal grouping analyses. Behav Ther 29, 257–276. [Google Scholar]
- 96. McCabe MP & Ricciardelli LA (2005) A prospective study of pressures from parents, peers, and the media on extreme weight change behaviors among adolescent boys and girls. Behav Res Ther 43, 653–668. [DOI] [PubMed] [Google Scholar]
- 97. Harrison KH & Hefner V (2006) Media exposure, current and future body ideals, and disordered eating among preadolescent girls: a longitudinal panel study. J Youth Adolesc 32, 153–163. [Google Scholar]
- 98. Haines J, Gillman MW, Rifas-Shiman S et al. (2010) Family dinner and disordered eating behaviors in a large cohort of adolescents. Eat Disord 18, 10–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. van den Berg P, Neumark-Sztainer D, Hannan PJ et al. (2007) Is dieting advice from magazines helpful or harmful? Five-year associations with weight-control behaviors and psychological outcomes in adolescents. Pediatrics 119, e30–e37. [DOI] [PubMed] [Google Scholar]
- 100. Ferreiro F, Seoane G & Senra C (2012) Gender-related risk and protective factors for depressive symptoms and disordered eating in adolescence: a 4-year longitudinal study. J Youth Adolesc 41, 607–622. [DOI] [PubMed] [Google Scholar]
- 101. Tremblay L & Lariviere M (2009) The influence of puberty onset, body mass index, and pressure to be thin on disordered eating behaviors in children and adolescents. Eat Behav 10, 75–83. [DOI] [PubMed] [Google Scholar]
- 102. Eisenberg ME, Wall M, Shim JJ et al. (2012) Associations between friends’ disordered eating and muscle-enhancing behaviors. Soc Sci Med 75, 2242–2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. French SA, Story M, Neumark-Sztainer D et al. (1997) Ethnic differences in psychosocial and health behavior correlates of dieting, purging, and binge eating in a population-based sample of adolescent females. Int J Eat Disord 22, 315–322. [DOI] [PubMed] [Google Scholar]
- 104. Story M, French SA, Neumark-Sztainer D et al. (1997) Psychosocial and behavioral correlates of dieting and purging in Native American adolescents. Pediatrics 99, E8. [DOI] [PubMed] [Google Scholar]
- 105. Levine MP, Smolak L & Hayden H (1994) The relation of sociocultural factors to eating attitudes and behaviors among middle school girls. J Early Adolesc 14, 471–490. [Google Scholar]
- 106. Paxton SJ, Schutz HK, Wertheim EH et al. (1999) Friendship clique and peer influences on body image concerns, dietary restraint, extreme weight-loss behaviors, and binge eating in adolescent girls. J Abnorm Psychol 108, 255–266. [DOI] [PubMed] [Google Scholar]
- 107. Hautala LA, Junnila J, Helenius H et al. (2008) Towards understanding gender differences in disordered eating among adolescents. J Clin Nurs 17, 1803–1813. [DOI] [PubMed] [Google Scholar]
- 108. Fonseca H, Ireland M & Resnick MD (2002) Familial correlates of extreme weight control behaviors among adolescents. Int J Eat Disord 32, 441–448. [DOI] [PubMed] [Google Scholar]
- 109. Goodwin H, Haycraft E & Meyer C (2011) Sociocultural correlates of compulsive exercise: is the environment important in fostering a compulsivity towards exercise among adolescents? Body Image 8, 390–395. [DOI] [PubMed] [Google Scholar]
- 110. Ackard DM, Neumark-Sztainer D, Hannan PJ et al. (2001) Binge and purge behavior among adolescents: associations with sexual and physical abuse in a nationally representative sample. Child Abuse Negl 6, 771–785. [DOI] [PubMed] [Google Scholar]
- 111. Fonseca H, Matos MG, Guerra A et al. (2009) Are overweight adolescents at higher risk of engaging in unhealthy weight-control behaviours? Acta Paediatr 98, 847–852. [DOI] [PubMed] [Google Scholar]
- 112. French SA, Story M, Downes B et al. (1995) Frequent dieting among adolescents: psychosocial and health behavior correlates. Am J Public Health 85, 695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Hodson C, Newcomb MD, Locke TF et al. (2006) Childhood adversity, poly-substance use, and disordered eating in adolescent Latinas: mediated and indirect paths in a community sample. Child Abuse Negl 30, 1017–1036. [DOI] [PubMed] [Google Scholar]
- 114. Neumark-Sztainer D, Story M, Falkner NH et al. (1998) Disordered eating among adolescents with chronic illness and disability: the role of family and other social factors. Arch Pediatr Adolesc Med 152, 871–878. [DOI] [PubMed] [Google Scholar]
- 115. Neumark-Sztainer D, Story M, Hannan PJ et al. (2000) Disordered eating among adolescents: associations with sexual/physical abuse and other familial/psychosocial factors. Int J Eat Disord 28, 249–258. [DOI] [PubMed] [Google Scholar]
- 116. Perkins DF & Luster T (1999) The relationship between sexual abuse and purging: findings from community-wide surveys of female adolescents. Child Abuse Negl 23, 371–382. [DOI] [PubMed] [Google Scholar]
- 117. Kaltiala-Heino R, Rissanen A, Rimpela M et al. (1999) Bulimia and bulimic behaviour in middle adolescence: more common than thought? Acta Psychiatr Scand 100, 33–39. [DOI] [PubMed] [Google Scholar]
- 118. White J & Halliwell E (2010) Examination of a sociocultural model of excessive exercise among male and female adolescents. Body Image 7, 227–233. [DOI] [PubMed] [Google Scholar]
- 119. Ayala GX, Mickens L, Galindo P et al. (2007) Acculturation and body image perception among Latino youth. Ethn Health 12, 21–41. [DOI] [PubMed] [Google Scholar]
- 120. Kaluski DN, Natamba BK, Goldsmith R et al. (2008) Determinants of disordered eating behaviors among Israeli adolescent girls. Eat Disord 16, 146–159. [DOI] [PubMed] [Google Scholar]
- 121. Austin SB, Richmond TK, Spadano-Gasbarro J et al. (2013) The contribution of school environmental factors to individual and school variation in disordered weight control behaviors in a statewide sample of middle schools. Eat Disord 21, 91–108. [DOI] [PubMed] [Google Scholar]
- 122. Rundle A, Diez Roux AV, Free LM et al. (2007) The urban built environment and obesity in New York City: a multilevel analysis. Am J Health Promot 21, 326–334. [DOI] [PubMed] [Google Scholar]
- 123. Li F, Harmer P, Cardinal BJ et al. (2009) Built environment and 1-year change in weight and waist circumference in middle-aged and older adults: Portland Neighborhood Environment and Health Study. Am J Epidemiol 169, 401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Li F, Harmer P, Cardinal BJ et al. (2009) Obesity and the built environment: does the density of neighborhood fast-food outlets matter? Am J Health Promot 23, 203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Oreskovic NM, Winickoff JP, Kuhlthau KA et al. (2009) Obesity and the built environment among Massachusetts children. Clin Pediatr (Phila) 48, 904–912. [DOI] [PubMed] [Google Scholar]
- 126. Brown B (2004) Adolescents’ Relationships with Peers. Handbook of Adolescent Psychology, 2nd ed. New York: Wiley. [Google Scholar]
- 127. Pomeranz JL, Taylor LM & Austin SB (2013) Over-the-counter and out-of-control: legal strategies to protect youths from abusing products for weight control. Am J Public Health 103, 220–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Thomsen SR, Weber MM & Brown LB (2002) The relationship between reading beauty and fashion magazines and the use of pathogenic dieting methods among adolescent females. Adolescence 37, 1–18. [PubMed] [Google Scholar]
- 129. Bissell K & Zhou P (2004) Must-See TV or ESPN: entertainment and sports media exposure and body-image distortion in college women. J Commun 54, 5–21. [Google Scholar]
- 130. Story M, French SA, Resnick MD et al. (1995) Ethnic/racial and socioeconomic differences in dieting behaviors and body image perceptions in adolescents. Int J Eat Disord 18, 173–179. [DOI] [PubMed] [Google Scholar]
- 131. Eaton DK, Kann L, Kinchen S et al. (2012) Youth risk behavior surveillance – United States, 2011. MMWR Surveill Summ 61, issue 4, 1–162. [PubMed] [Google Scholar]
- 132. Institute of Medicine (2005) Progress in Preventing Childhood Obesity: How Do We Measure Up? Washington, DC: National Academies Press. [Google Scholar]
- 133. Neumark-Sztainer D, Butler R & Palti H (1996) Personal and socioenvironmental predictors of disordered eating among adolescent females. J Nutr Educ 28, 195–201. [Google Scholar]
- 134. Stice E, Mazotti L, Krebs M et al. (1998) Predictors of adolescent dieting behaviors: a longitudinal study. Psychol Addict Behav 12, 195–205. [Google Scholar]
- 135. Dixon R, Adair V & O'Connor S (1996) Parental influences on the dieting beliefs and behaviors of adolescent females in New Zealand. J Adolesc Health 19, 303–307. [DOI] [PubMed] [Google Scholar]
- 136. Blodgett Salafia EH & Lemer JL (2012) Associations between multiple types of stress and disordered eating among girls and boys in middle school. J Child Fam Stud 21, 148–157. [Google Scholar]
- 137. Neumark-Sztainer D, Falkner N, Story M et al. (2002) Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes Relat Metab Disord 26, 123–131. [DOI] [PubMed] [Google Scholar]
- 138. Neumark-Sztainer D, Wall MM, Story M et al. (2003) Correlates of unhealthy weight-control behaviors among adolescents: implications for prevention programs. Health Psychol 22, 88–98. [DOI] [PubMed] [Google Scholar]
- 139. Unikel C, Von Holle A, Bulik CM et al. (2012) Disordered eating and suicidal intent: the role of thin ideal internalisation, shame and family criticism. Eur Eat Disord Rev 20, 39–48. [DOI] [PubMed] [Google Scholar]
- 140. Gerner B & Wilson PH (2005) The relationship between friendship factors and adolescent girls’ body image concern, body dissatisfaction, and restrained eating. Int J Eat Disord 37, 313–320. [DOI] [PubMed] [Google Scholar]
- 141. Lieberman M, Gauvin L, Bukowski WM et al. (2001) Interpersonal influence and disordered eating behaviors in adolescent girls: the role of peer modeling, social reinforcement, and body-related teasing. Eat Behav 2, 215–236. [DOI] [PubMed] [Google Scholar]
- 142. French SA, Story M, Downes B et al. (1995) Frequent dieting among adolescents: psychosocial and health behavior correlates. Am J Public Health 85, 695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Shisslak CM, Crago M, McKnight KM et al. (1998) Potential risk factors associated with weight control behaviors in elementary and middle school girls. J Psychosom Res 44, 301–313. [DOI] [PubMed] [Google Scholar]
- 144. Fulkerson JA, Strauss J, Neumark-Sztainer D et al. (2007) Correlates of psychosocial well-being among overweight adolescents: the role of the family. J Consult Clin Psychol 75, 181–186. [DOI] [PubMed] [Google Scholar]
- 145. Thomsen SR, Weber MM & Brown LB (2001) The relationship between health and fitness magazine reading and eating-disordered weight-loss methods among high school girls. Am J Health Educ 32, 133–138. [Google Scholar]
- 146. McCabe MP & Ricciardelli LA (2001) The structure of the Perceived Sociocultural Influences on Body Image and Body Change Questionnaire. Int J Behav Med 8, 19–41. [Google Scholar]
- 147. Procidano ME & Heller K (1983) Measures of perceived social support from friends and from family: three validation studies. Am J Community Psychol 11, 1–24. [DOI] [PubMed] [Google Scholar]
- 148. Levine MP, Smolak L & Hayden H (1994) The relation of sociocultural factors to eating attitudes and behaviors among middle school girls. J Early Adoles 14, 471–490. [Google Scholar]
- 149. Unikel C & Gómez-Peresmitré G (2004) Validez de constructo de un instrumento para la deteccio′n de factores de riesgo en los trastornos de la conducta alimentaria en mujeres mexicanas. Salud Mental 27, 38–49. [Google Scholar]
- 150. Unikel C, Villatoro J, Medina-Mora ME et al. (2000) Conductas alimentarias de riesgo en adolescentes mexicanos. Datos en población estudiantil del Distrito Federal. Rev Invest Clin 52, 140–147. [PubMed] [Google Scholar]
- 151. Taranis L, Touyz S & Meyer C (2011) Disordered eating and exercise: development and preliminary validation of the Compulsive Exercise Test (CET). Eur Eat Disord Rev 19, 256–268. [DOI] [PubMed] [Google Scholar]
- 152. Paxton SJ, Wertheim EH, Gibbons K et al. (1991) Body image satisfaction, dieting beliefs, and weight loss behaviors in adolescent girls and boys. J Youth Adolesc 20, 361–379. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
To view supplementary material for this article, please visit https://doi.org/10.1017/S1368980013001407