Key Teaching Points.
-
•
There exists a well-established relationship between sleep-disordered breathing and arrhythmias. The mechanisms of this interaction are not clear.
-
•
The improvement in atrial fibrillation burden following treatment of sleep apnea is well described. Early data suggest improvement in sleep apnea after atrial fibrillation ablation.
-
•
There appears to be an association between sleep-disordered breathing and premature ventricular contractions (PVCs), which is not well described in the literature.
-
•
We describe an unexpected finding of dramatic immediate improvement in periodic breathing after successful PVC ablation.
Introduction
The relationship between cardiac arrhythmias and both obstructive sleep apnea (OSA) and central sleep apnea (CSA) is increasingly being recognized. This association is especially well established between sleep apnea and atrial fibrillation.1,2 The interaction seems to go beyond the coexistence of the 2 disorders owing to shared risk factors. The mechanism between ventricular arrhythmias and sleep apnea is less well described and is restricted mostly to observations about OSA contributing to ventricular arrhythmias.3
Case report
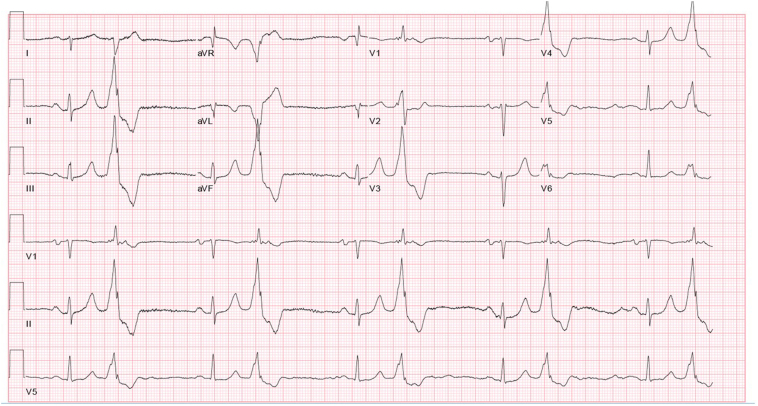
A 63-year-old male patient with history of coronary artery bypass graft surgery with decreased left ventricular ejection fraction (LVEF) of 45% was noted to have frequent monomorphic premature ventricular contractions (PVCs), with a burden of 40% (on amiodarone and metoprolol). In addition, he also was diagnosed with severe OSA and had complaints of fatigue and nonrestorative sleep. The electrocardiogram before ablation is shown in Figure 1. He underwent PVC mapping and ablation procedure. The PVCs were mapped and ablated with immediate suppression at the interleaflet triangle below the left and right coronary cusps. The PVC burden 3 months post ablation on a repeat 2-week event recorder was noted to be 2%, corresponding to improved symptoms. Notably, there was no change in LVEF. The patient’s amiodarone was stopped at this point. After 1 year, the LVEF continued to remain in the initial range.
Figure 1.
The preablation electrocardiogram of the patient.
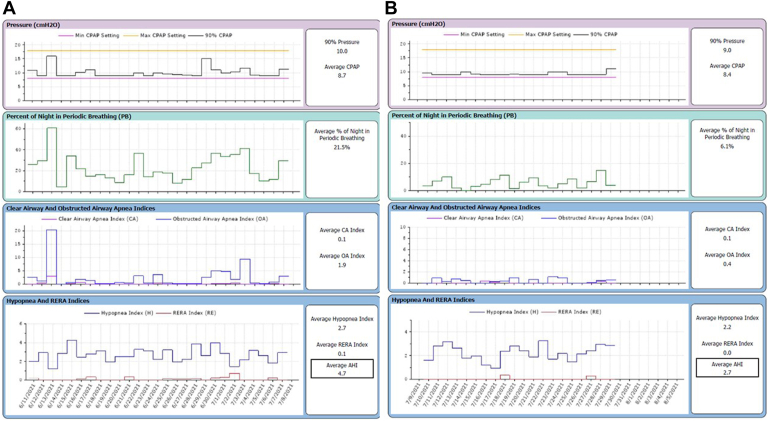
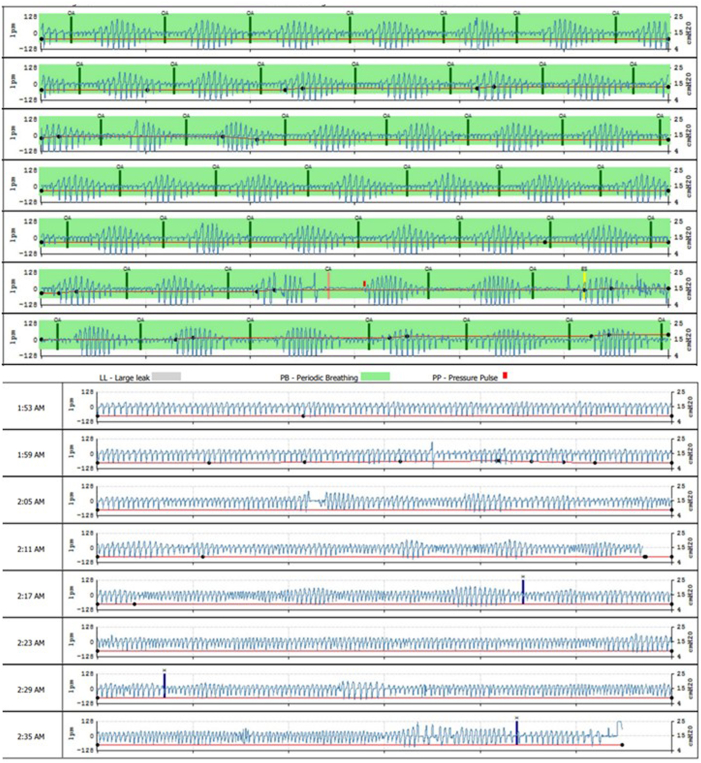
Before the ablation procedure, downloads from the patient’s continuous positive airway pressure (CPAP) machine revealed significant elevation in periodic breathing, as noted in Figure 2 (left), with subsequent improvement, as seen in Figure 2 (right). The percentage of periodic breathing was 21.5%, which decreased to 6.1% after ablation. Before ablation, apnea-hypopnea index (AHI) was 4.7, which reduced to 2.2 after ablation in the 4-week period post ablation (before CPAP prescription, the AHI was 31.5). The AHI at 1 year was 1.5, with continued patient-reported improvement in sleep quality. The representative periodic Cheyne-Stokes breathing pattern prior to ablation on PAP waveform review can be seen in the top tracing shown in Figure 3. The improvement in the periodic breathing pattern post ablation is seen in the corresponding representative tracing in the bottom portion of Figure 3. The patient reported improvement in quality of sleep, fatigue, and daytime functioning. Other risk factors for OSA during follow-up, such as neck circumference, sleep position, and alcohol intake, were unchanged.
Figure 2.
Waveform data obtained from the patient’s continuous positive airway pressure machine. The x-axis is the timeline. Waveforms on left show sleep parameters in the 1 month immediately before premature ventricular complex (PVC) ablation. Waveforms on right show sleep parameters 1 month immediately after PVC ablation.
Figure 3.
The sample waveforms before premature ventricular complex (PVC) ablation (top) show periodic breathing / Cheyne-Stokes pattern and after PVC ablation (bottom) show an improvement in periodic breathing. Note the background is marked as green when periodic breathing is detected.
Discussion
Our patient was being treated for OSA with CPAP, and the machine downloads revealed episodes of periodic breathing concerning for coexisting central sleep events. CSA diagnosis was not made on a formal sleep study, but waveform download (top tracing in Figure 3) was highly concerning for Cheyne-Stokes ventilation pattern. CSA is diagnosed in patients with Cheyne-Stokes breathing who meet polysomnogram criteria and have the classic crescendo-decrescendo pattern. Therefore, periodic breathing could be considered a surrogate for CSA. The periodic breathing improved significantly in our patient immediately after PVC ablation, as evidenced by improved AHI and percent of periodic breathing.
Ablation of atrial fibrillation has been shown to improve CSA, and treating sleep apnea is associated with decreased atrial fibrillation burden.4,5 A similar reciprocal therapeutic association between ventricular arrhythmias and sleep apnea has not been described.
The improvement in sleep apnea after PVC ablation is likely due to factors unrelated to LVEF, as this parameter had not improved in our patient. The immediate improvement in sleep apnea following PVC ablation also suggests a mechanism related to improved acute hemodynamics positively affecting sleep apnea.
CSA is closely associated with heart failure and elevated pulmonary capillary wedge pressure.6 PVCs also are known to increase pulmonary capillary wedge pressure, and their elimination may result in an acute improvement in this parameter.7 The fact that the patient’s PVCs were associated with ventriculoatrial dissociation could lead to exacerbation of this phenomenon. Other possible mechanisms to explain the improvement could be related to improved cardiac output after PVC ablation. Interventions that improve cardiac output in congestive heart failure patients do seem to improve exercise oscillatory ventilation, and a similar mechanism could potentially influence periodic breathing too.8
It is likely that multiple mechanisms mediating the interaction between PVCs and periodic breathing may be at play, and this area would require continuing research. While the exact pathways of the interaction between PVCs and CSA are still being worked out, the clinical benefits of PVC treatment on CSA should be explored in larger studies. Our isolated case report showing a dramatic improvement in periodic breathing after successful PVC ablation is a provocative finding and, to our knowledge, has not been described before.
Conclusion
The improvement of periodic breathing following successful ablation of PVCs is an intriguing finding. This suggests a possible causal relationship between the two. It will require more studies to confirm the association between sleep-disordered breathing and PVCs. For now, it adds another possible indication for ablation in patients with PVCs and CSA.
Footnotes
Funding Sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures: The authors have no conflicts to disclose.
References
- 1.Gami A.S., Pressman G., Caples S.M., et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364–367. doi: 10.1161/01.CIR.0000136587.68725.8E. [DOI] [PubMed] [Google Scholar]
- 2.Linz D., Hendriks J. Central sleep apnea in atrial fibrillation: risk factor or marker of untreated underlying disease? Int J Cardiol Heart Vasc. 2020;30 doi: 10.1016/j.ijcha.2020.100650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marinheiro R., Parreira L., Amador P., et al. Ventricular arrhythmias in patients with obstructive sleep apnea. Curr Cardiol Rev. 2019;15:64–74. doi: 10.2174/1573403X14666181012153252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naruse Y., Tada H., Satoh M., et al. Radiofrequency catheter ablation of persistent atrial fibrillation decreases a sleep-disordered breathing parameter during a short follow-up period. Circ J. 2012;76:2096–2103. doi: 10.1253/circj.cj-12-0014. [DOI] [PubMed] [Google Scholar]
- 5.Kohno T., Kimura T., Fukunaga K., et al. Prevalence and clinical characteristics of obstructive- and central-dominant sleep apnea in candidates of catheter ablation for atrial fibrillation in Japan. Int J Cardiol. 2018;260:99–102. doi: 10.1016/j.ijcard.2018.01.103. [DOI] [PubMed] [Google Scholar]
- 6.Solin P., Bergin P., Richardson M., Kaye D.M., Walters E.H., Naughton M.T. Influence of pulmonary capillary wedge pressure on central apnea in heart failure. Circulation. 1999;99:1574–1579. doi: 10.1161/01.cir.99.12.1574. [DOI] [PubMed] [Google Scholar]
- 7.Kuroki K., Tada H., Seo Y., et al. Prediction and mechanism of frequent ventricular premature contractions related to haemodynamic deterioration. Eur J Heart Fail. 2012;14:1112–1120. doi: 10.1093/eurjhf/hfs095. [DOI] [PubMed] [Google Scholar]
- 8.Murphy R.M., Shah R.V., Malhotra R., et al. Exercise oscillatory ventilation in systolic heart failure: an indicator of impaired hemodynamic response to exercise. Circulation. 2011;124:1442–1451. doi: 10.1161/CIRCULATIONAHA.111.024141. [DOI] [PMC free article] [PubMed] [Google Scholar]