Abstract
Duodenal stump fistula is a rare but dangerous complication of gastric cancer surgery. Reinforcement of the duodenal stump was suggested as a useful method to prevent the occurrence of duodenal stump fistula. Although laparoscopic surgery has been established as a safe procedure for gastric cancer, it is acknowledged that the application of duodenal stump reinforcement is a demanding process in laparoscopic radical gastrectomy. This review aims to provide a concise description of the proposed reinforcement methods of duodenal stump after laparoscopic radical gastrectomy for gastric cancer by summarizing the relevant literature written in English. The thorough knowledge of these reinforcement techniques may help surgeons to find the most suitable reinforcement method of duodenal stump for patients.
Keywords: Laparoscopic gastrectomy, Gastric cancer, Duodenal stump reinforcement, Duodenal stump fistula
1. Introduction
With an estimated 1,089,103 new cases and 768,793 deaths from cancer worldwide, gastric cancer is projected to be the fifth most common malignancy and the fourth leading cause of cancer-related mortality [1]. Although significant advances have been achieved in the diagnosis and treatment of gastric cancer, curative resection as part of a comprehensive therapy still provides the only radical treatment for resectable disease [2,3]. In the field of surgery, laparoscopic gastrectomy is now regarded as a standard option for early-stage gastric cancer [4]. The application of laparoscopic gastrectomy in advanced gastric cancer, although still subject to debate, has proved to be a safe and effective technique compared to open approaches in terms of both short- and long-term outcomes for locally advanced gastric cancer according to several high-quality studies [[5], [6], [7]].
However, in contrast to open approach, the laparoscopic approach could increase the incidence of postoperative duodenal stump fistula (DSF) [[8], [9], [10]]. DSF, or duodenal stump leakage, is a relatively uncommon but highly serious complication after gastrectomy using Roux-en-Y or Billroth-II digestive reconstruction. The incidence of DSF was reported to be between 1 and 5% [11,12], while it has a morbidity rate of 75% and a mortality rate of up to 40% [13,14]. A number of causes of DSF have been proposed, including inadequate closure and postoperative distension of the duodenum [15]. One potential pathogenesis mechanism is that increased pressure in the lumen of duodenal stump exceeds tissue and staple-line tension [16]. The risk factors for DSF include duodenal ulcer, bio-humoral nutritional status impairment intraoperative contamination, multiple comorbidities and gastric outlet obstruction [15,17,18]. However, not all surgeons routinely perform the reinforcement of duodenal stump [19], and unreinforced duodenal stump was found to be a risk factor for DSF in several studies [11,12]. Therefore, it is reasonable to reinforce the staple line, as commonly done in open surgery. Meanwhile, laparoscopic surgery is more demanding and laparoscopic suturing is not as easily performed as suturing in open operation. Thus far, several different methods of duodenal stump reinforcement have been proposed, but no optimal method has yet been established as no direct comparisons among the described methods.
In this article, we presented a review of the reported duodenal stump reinforcement methods after laparoscopic gastric cancer in literature.
2. Methods
This study is a scoping review conducted according to the PRISMA 2020 guidelines and the extension for scoping systematic review [20]. This study was not registered in the public database.
2.1. Literature research
A comprehensive literature research was conducted utilizing MEDLINE/PubMed and Web of Science with the latest end of search date on 12 September 2022. In PubMed, the terms “laparoscopic” “gastrectomy,” and “duodenal stump” were searched to identify articles regarding the reinforcement of the duodenal stump following laparoscopic gastrectomy for gastric cancer. The most relevant and informative citations were identified for inclusion.
2.2. Eligibility criteria
Only studies in English with a detailed description of the reinforcement technique of duodenal stump were included. Reinforcement not performed laparoscopically were excluded. Case reports/series with less than ten patients were also eliminated. After the establishment of the search strategy, two reviewers (XL and WK) independently performed the study selection, and data extraction. Disagreements were solved by consultation with a third reviewer (GY).
2.3. Data charting
The study characteristics extracted from the included articles included the following: first author, publication year, country, total number of patients in the study, detailed description of reinforcement method, and DSF rate. Due to the high heterogeneity among the different reinforcement methods and the nature of the scoping review, the evaluation of evidence quality was not conducted. Instead of a meta-analysis, basic numeric analysis was presented.
3. Results
A total of 190 records were extracted from the databases of PubMed/Medline and Web of Science. Finally, 9 articles were retained for analysis (Fig. 1) [12,13,16,18,[21], [22], [23], [24], [25]]. All of the articles provided schemes or illustrations for the reinforcement techniques.
Fig. 1.
Flow chart of literature search.
A total of 6 types of duodenal stump reinforcement methods were described by the 9 included studies (Table 1). All of these 9 included articles came from East Asia and were published between 2016 and 2021. The majority of the articles adopted a retrospective study design [12,13,16,18,22,24,25]. With the exception of two [21,24], all studies were performed in a single institution. The sample size ranged from 40 to 895 patients, and the DSF rate ranged from 0 to 2.0%.
Table 1.
Summary of duodenal stump reinforcement techniques.
| Methods | Author | Year | Country | Study design | No. of patients | DSF rate |
|---|---|---|---|---|---|---|
| BPA method | ||||||
| BPA sheet + fibrin sealant | Paik et al. [18] | 2016 | Korea | Retrospective | 316 | 1.6% |
| BPA sheet | Misawa et al. [21] | 2019 | Japan | Multi-institutional, prospective | 100 | 2.0% |
| Lembert Suture | Inoue et al. [16] | 2016 | Japan | Retrospective | 121 | 0% |
| Barbed suture | Kim MC [22] | 2017 | Korea | Retrospective | 62 | 0% |
| Kim SY et al. [24] | 2017 | Korea | Bi-institutional, retrospective | 99 | 0% | |
| Kim MC et al. [23] | 2017 | Korea | Prospective | 100 | 0% | |
| Single Purse-String Suture | He et al. [25] | 2019 | China | Retrospective | 183 | 0% |
| Handover method | Du et al. [13] | 2021 | China | Retrospective | 40 | 0% |
| Buried suture | Ri et al. [12] | 2019 | Japan | Retrospective | 895 | 0.7% |
BPA: bioabsorbable polyglycolic acid, DSF: duodenal stump fistula.
4. Discussion
DSF is a rare but serious complication after laparoscopic gastrectomy for gastric cancer using Billroth II or Roux-en-Y reconstruction. However, no consensus on the management of duodenal stump has yet been reached. This scoping review identified a total of six methods to reinforce the duodenal stump during laparoscopic gastrectomy. Except for the BPA methods, although each of the suturing reinforcement methods for duodenal stump has its special features and characteristics, they are mainly based on the pursing-string suture and inverted the Lembert suture.
4.1. Bioabsorbable polyglycolic acid (BPA) method
Paik et al. investigated the utility of a bioabsorbable polyglycolic acid (BPA) felt in combination with a fibrin sealant in preventing postoperative DSF [18]. After duodenal transection with a laparoscopic linear stapler, the fibrin sealant was applied onto the duodenal stump and the BPA felt was then used to seal over the duodenal stump, followed by fibrin sealant reapplication. They found that 5 out of 311 patients who underwent laparoscopic gastric cancer surgery developed DSF. Among these 5 patients, 3 patients who were treated conservatively and 1 patient who underwent percutaneous drainage showed satisfactory recovery, and the remaining 1 patient deceased due to complications from DSF despite undergoing percutaneous transhepatic biliary drainage.
In another study, Misawa et al. conducted a multicenter, single-arm, phase II study to evaluate the safety and feasibility of a stapler with BPA sheet for laparoscopic duodenal stump closure and reinforcement in gastric surgery [21]. In this method, BPA sheets were pre-attached on the inner surface of both the anvil and cartridge arms of the linear stapling. During surgery, when the duodenum was transected using a linear stapler with BPA sheet, the staple line was simultaneously reinforced. Among the 100 included patients, 44 patients underwent laparoscopic surgery and one patient developed DSF. This patient underwent drainage surgery for the DSF and recovered well.
BPA was also used to reinforce Billroth I gastroduodenostomy or Roux-en-Y gastrojejunostomy in gastrectomy [26], and to reinforce the pancreatic stump after distal pancreatectomy [27]. The use of BPA sheet is probably the most convenient method for reinforcement of the duodenal staple line, which eliminates the need for suturing and provides the advantage of great generalizability for application. For example, it can be used if the duodenal stump is short or the duodenum has a history of disease, while other methods require a relative long duodenal stump.
4.2. Lembert suture
Inoue et al. described a stump reinforcement procedure with Lembert sutures [16]. After transection of the duodenum with a 60-mm endoscopic linear stapler (Echelon 60, white cartridge; Ethicon Endo Surgery Co.), the staple line of the duodenal stump was reinforced using hand-sewn Lembert sutures with seromuscular interrupted absorbable 3-0 sutures (Fig. 2(A–C)). Following the reinforcement step, the staple line of the duodenum stump was inverted. In their retrospective study on 223 patients, none of the 121 patients who received laparoscopic Lembert sutures reinforcement of duodenal stump developed DSF, while DSF occurred in 2 of the 102 patients who did not receive this reinforcement. This technique has the disadvantage of leaving the corners of the stapled line unreinforced and unwrapped.
Fig. 2.
Illustration of the Lembert suture technique. (A–B) The duodenal staple line was reinforced by interrupted Lembert suture using absorbable 3-0 sutures. (C) Completed view of duodenal stump reinforcement (adapted from reference 16).
4.3. Barbed suture
Kim reported a laparoscopic reinforcement suture (LARS) that involves 3–0 15 cm barbed suture [22]. In this technique, a 2 cm long duodenal stump is left. LARS starts from the upper to the lower part on the staple line of duodenal stump, and the reinforcement is a continuous suture with invagination (Fig. 3(A–D)). However, in the case of short duodenal stump, the reinforcement has interrupted sutures without invagination of the duodenal stump [23,24]. The average time for LARS is 8 min. Both in the first retrospective study with 62 patients and in the prospective, single-arm, phase II study including 100 patients, there was no development of DSF [23]. The application of knotless barbed sutures has the advantage of eliminating knot tying, which could be time-consuming under a laparoscope.
Fig. 3.
Illustration of the Barbed suture technique. (A) Duodenal stump reinforcement starts from the upper end with a triangular suture using a barbed suture. (B–C) Reinforcement with continuous suture forward the lower end, with a triangular suture at the end. (D) Completed view of the reinforced invaginated duodenal stump line (adapted from reference 24).
4.4. Single purse-string suture
He et al. introduced a single purse-string suture technique for laparoscopic reinforcement of the duodenal stump [25], om which approximately 2–3 cm of duodenum stump was freed for reinforcement after cutting the duodenum with a 60 mm endoscopic linear stapler (staple height 1.5–1.8 mm) from the left to the right side. Then, a purse-string suture was made 1.0–1.5 cm distal to the duodenal stump edge using a 3-0 single-strand absorbable suture (Fig. 4(A–D)). The average time of this reinforcement method was 5 min and no DSF occurred post-surgery in any of the 183 patients.
Fig. 4.
Illustration of the Single Purse-String Suture. (A) A seromuscular purse-string suture is placed 1.0–1.5 cm away from the duodenal stump. (B–C) The knots are tightened and reinforced while the duodenal stump is fully pushed into the purse-string suture. (D) The view of completed reinforcement (adapted from reference 25).
In open operation, the purse-string suture was reported to be superior to the stapler in combination with seromuscular layer suture and full-thickness in combination with the seromuscular layer suture in terms of duodenal stump closure time, surgical cost and DSF rate [28]. However, it is relatively difficult to perform the purse-string suture under laparoscopy. The single purse-string suture technique, proposed by He et al., was reported to be easy and effective. This technique is also commonly used in our institution. It should be performed by a single operator, which, on the one hand, demands great experience by the operator; on the other hand, it eliminates the disadvantages associated with the assistant's limitations. However, this technique is not recommended when the length of duodenal stump is less than 1 cm.
4.5. Buried suture
Ri et al. developed a duodenal reinforcement technique with buried suture [12]. In this technique, the operator is on the patient's right side. After transection of the duodenum, the first stich is inserted across the center
of the duodenal stump staple line. Before ligation outside of the port, the edge of the duodenal stump on the lesser curvature side is fully inverted by the assistant using a two-handed forceps. Then, the inverted edges are buried by seromuscular suturing. If necessary, the reinforcement of the staple line can be completed with a few added stitches. In the above study, the specific time for reinforcement was not provided. Compared to the non-reinforcement group, in combination with other factors the operation time was extended by 40 min for LTG and 33 min for LDG in the reinforcement group. In the retrospective study of 965 patients, DSF was significantly decreased by reinforcement, with only six out of 895 patients in reinforcement group compared to four out of 70 patients in the non-reinforcement group developed DSF [12]. More importantly, while all the cases of DSF in the non-reinforcement group required re-operation, 5 out of 6 DSF in the reinforcement group were successfully received conservative management, while one patient required reoperation. Compared to the Lembert suture by Inoue et al., this technique buries the corners of the stapled line. However, it still requires an experienced assistant.
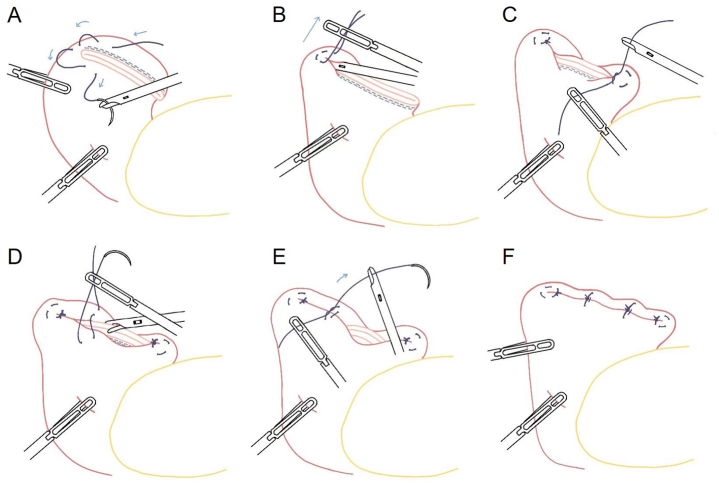
4.6. Handover method
Du et al. described a so called “handover method” for duodenal stump reinforcement [13]. In this method, the duodenal bulb is cut 2 cm away from the pylorus sphincter with a 45 mm (shaft length) × 3.5 mm (open staple height) endoscopic linear stapler. Then, the upper and inferior corners of the duodenal stump are separately wrapped with a hemi-purse-string suture at around 1 cm distance from the stump edge. Lastly, the remaining stump line between the two hemi-purse-string sutures is reinforced invertedly with seromuscular stitches (Fig. 5(A–F)). The average time for duodenal stump reinforcement was 8.5 min. This technique has the advantage of less dependence on the assistant's cooperation. In the retrospective study with 40 patients, none developed DSF [13]. This technique was reported to have 8 advantages and overcame some disadvantages of the buried suture and Lembert sutures.
Fig. 5.
Illustration of the handover method. (A) A hemi-purse-string suture is placed at the upper end with three seromuscular stitches. (B) The knots are tightened with the upper end pushed in the hemi-purse-string suture. (C) The lower end of the staple line is reinforced with another hemi-purse-string suture. (D–E). The staple line between the wrapped U-corner and I-corner is reinforced with interrupted Lembert suture. (F). View of the completed reinforcement (adapted from reference 13).
Although the incidence of DSF is very low and not all surgeons routinely perform reinforcement of the duodenal stump, this measure is still recommended in all patients due to the possible catastrophe after the development of DSF. Thus, it is worthwhile to discusess the published reinforcement methods. More recently, Chung et al. reported favorable result with the usage of falciform ligament patch for the prevention of DSF after gastrectomy [29]. In high-risk patients for DSF, apart from strengthening the duodenal stump, it is recommended to place a drainage tube around the stump to facilitate the early diagnosis and treatment of DSF.
5. Limitations
There are several limitations to this scoping review. First, due to the nature of the included studies, we were unable to make comparisons between the studies. Second, the included studies were either single-arm studies or comparisons between reinforced and unreinforced group and they included no direct comparison between different reinforcement techniques. Therefore, it is challenging to decide which method gives the optimal results. Third, the detailed investigation on risk factors for DSF is beyond the scope of the present study. Except the unreinforced duodenal stump, BMI ≥ 24 kg/m2 and elevated preoperative CRP level were also suggested to be risk factor of DSF [11]. Further large-scale researches are still warranted to decide the necessity of duodenal reinforcement and determine the best possible method.
6. Conclusion
This study gave a concise review on the reinforcement methods of duodenal stump after laparoscopic radical gastrectomy for gastric cancer. Thus far, no direct comparison among these reinforcement methods is available. It should be assumed that the duodenal stump reinforcement method must be fitted to the surgeons’ experience and preferences. Due the low incidence of DSF, further collaborative larger prospective trials are still needed to identify the necessity of duodenal reinforcement and the potential superiority of any specific method.
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Data availability statement
Data included in article/supplementary material/referenced in article.
Source of funding
This work was supported by Hangzhou Health Science and Technology Program (A20210271). The foundation was not involved in study design, data collection, analysis, interpretation or drafting of this report.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors thank MSc Yuan Chen, from Leiden Observatory, for the drawing of illustrations.
References
- 1.Sung H., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Chen Z.D., et al. Recent advances in the diagnosis, staging, treatment, and prognosis of advanced gastric cancer: a literature review. Front. Med. 2021;8 doi: 10.3389/fmed.2021.744839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mocan L. Surgical management of gastric cancer: a systematic review. J. Clin. Med. 2021;10(12) doi: 10.3390/jcm10122557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caruso S., Scatizzi M. Laparoscopic gastrectomy for gastric cancer: has the time come for considered it a standard procedure? Surg. Oncol. 2022;40 doi: 10.1016/j.suronc.2021.101699. [DOI] [PubMed] [Google Scholar]
- 5.Chen X., et al. Laparoscopic versus open distal gastrectomy for advanced gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized comparative studies. Eur. J. Surg. Oncol. 2020;46(11):1998–2010. doi: 10.1016/j.ejso.2020.06.046. [DOI] [PubMed] [Google Scholar]
- 6.Beyer K., et al. Laparoscopic versus open gastrectomy for locally advanced gastric cancer: a systematic review and meta-analysis of randomized controlled studies. World J. Surg. Oncol. 2019;17(1):68. doi: 10.1186/s12957-019-1600-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aiolfi A., et al. Systematic review and updated network meta-analysis of randomized controlled trials comparing open, laparoscopic-assisted, and robotic distal gastrectomy for early and locally advanced gastric cancer. Surgery. 2021;170(3):942–951. doi: 10.1016/j.surg.2021.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Cozzaglio L., et al. Surgical management of duodenal stump fistula after elective gastrectomy for malignancy: an Italian retrospective multicenter study. Gastric Cancer. 2016;19(1):273–279. doi: 10.1007/s10120-014-0445-0. [DOI] [PubMed] [Google Scholar]
- 9.Kim K.M., et al. Major early complications following open, laparoscopic and robotic gastrectomy. Br. J. Surg. 2012;99(12):1681–1687. doi: 10.1002/bjs.8924. [DOI] [PubMed] [Google Scholar]
- 10.Orsenigo E., et al. Laparoscopy-assisted gastrectomy versus open gastrectomy for gastric cancer: a monoinstitutional Western center experience. Surg. Endosc. 2011;25(1):140–145. doi: 10.1007/s00464-010-1147-2. [DOI] [PubMed] [Google Scholar]
- 11.Gu L., et al. Risk factors for duodenal stump leakage after laparoscopic gastrectomy for gastric cancer. J. Gastric Cancer. 2020;20(1):81–94. doi: 10.5230/jgc.2020.20.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ri M., et al. Duodenal stump reinforcement might reduce both incidence and severity of duodenal stump leakage after laparoscopic gastrectomy with Roux-en-Y reconstruction for gastric cancer. Gastric Cancer. 2019;22(5):1053–1059. doi: 10.1007/s10120-019-00946-8. [DOI] [PubMed] [Google Scholar]
- 13.Du J., et al. Handover method: simple, classic and harmonized intracorporeal closure of stapled duodenal stump during laparoscopic gastrectomy. J. Surg. Oncol. 2021;124(1):41–48. doi: 10.1002/jso.26484. [DOI] [PubMed] [Google Scholar]
- 14.Ramos M., et al. Duodenal fistula: the most lethal surgical complication in a case series of radical gastrectomy. Int. J. Surg. 2018;53:366–370. doi: 10.1016/j.ijsu.2018.03.082. [DOI] [PubMed] [Google Scholar]
- 15.Orsenigo E., et al. Duodenal stump fistula after gastric surgery for malignancies: a retrospective analysis of risk factors in a single centre experience. Gastric Cancer. 2014;17(4):733–744. doi: 10.1007/s10120-013-0327-x. [DOI] [PubMed] [Google Scholar]
- 16.Inoue K., et al. Staple-line reinforcement of the duodenal stump with intracorporeal Lembert's sutures in laparoscopic distal gastrectomy with Roux-en-Y reconstruction for gastric cancer. Surg. Laparosc. Endosc. Percutaneous Tech. 2016;26(4):338–342. doi: 10.1097/sle.0000000000000291. [DOI] [PubMed] [Google Scholar]
- 17.Po Chu Patricia Y., et al. Duodenal stump leakage. Lessons to learn from a large-scale 15-year cohort study. Am. J. Surg. 2020;220(4):976–981. doi: 10.1016/j.amjsurg.2020.02.042. [DOI] [PubMed] [Google Scholar]
- 18.Paik H.J., et al. Duodenal stump fistula after gastrectomy for gastric cancer: risk factors, prevention, and management. Ann. Surg. Treat. Res. 2016;90(3):157–163. doi: 10.4174/astr.2016.90.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cai Z.H., et al. Survey on laparoscopic total gastrectomy at the 11th China-Korea-Japan laparoscopic gastrectomy joint seminar. Asian J. Endosc. Surg. 2017;10(3):259–267. doi: 10.1111/ases.12362. [DOI] [PubMed] [Google Scholar]
- 20.Tricco A.C., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 21.Misawa K., et al. Safety and feasibility of linear stapling device with bioabsorbable polyglycolic acid sheet for duodenal closure in gastric cancer surgery: a multi-institutional phase II study. World J. Surg. 2019;43(1):192–198. doi: 10.1007/s00268-018-4748-x. [DOI] [PubMed] [Google Scholar]
- 22.Kim M.-C. Laparoscopic reinforcement suture of duodenal stump using barbed suture during laparoscopic gastrectomy for gastric cancer: preliminary results in consecutive 62 patients. Ann. Laparosc. Endosc. Surg. 2017;2(2) [Google Scholar]
- 23.Kim M.C., Kim S.Y., Kim K.W. Laparoscopic reinforcement suture (LARS) on staple line of duodenal stump using barbed suture in laparoscopic gastrectomy for gastric cancer: a prospective single arm phase II study. J. Gastric Cancer. 2017;17(4):354–362. doi: 10.5230/jgc.2017.17.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim S.Y., et al. Laparoscopic reinforcement suture on staple-line of duodenal stump using barbed suture during laparoscopic gastrectomy for gastric cancer. Ann. Surg. Treat. Res. 2017;93(6):305–309. doi: 10.4174/astr.2017.93.6.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.He H., et al. Single purse-string suture for reinforcement of duodenal stump during laparoscopic radical gastrectomy for gastric cancer. Front. Oncol. 2019;9:1020. doi: 10.3389/fonc.2019.01020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ojima T., et al. Reinforced stapling technique for reconstruction after laparoscopic distal gastrectomy. Surg. Laparosc. Endosc. Percutaneous Tech. 2018;28(5):334–336. doi: 10.1097/SLE.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 27.Oweira H., et al. Using a reinforced stapler decreases the incidence of postoperative pancreatic fistula after distal pancreatectomy: a systematic review and meta-analysis. World J. Surg. 2022;46(8):1969–1979. doi: 10.1007/s00268-022-06572-3. [DOI] [PubMed] [Google Scholar]
- 28.Shao Q.S., et al. Application of purse-string suture for management of duodenal stump in radical gastrectomy. Chin. Med. J. 2011;124(7):1018–1021. [PubMed] [Google Scholar]
- 29.Chung J.H., et al. Application of the falciform ligament patch for the prevention of duodenal stump leakage after gastrectomy: technical report on a case series. J. Laparoendosc. Adv. Surg. Tech. 2022 doi: 10.1089/lap.2022.0454. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.