Abstract
Background:
Health care workers are considered as high-risk population, who deal with many unknown, undiagnosed, and subclinical infectious diseases in their daily life. Currently, the COVID-19 pandemic posed as an add-on burden for these frontline workers in all aspects. Although, many adverse physical and mental effects of pandemic among health care workers (HCWs) were discussed worldwide, a long-term study for delayed complications needed to be explored.
Aim:
The study evaluates and compares three waves of the pandemic in various aspects such as the incidence, prevalence, severity, risk factors, and variations in the pattern of COVID-19 infection, impact of vaccination, and post-infection complications among the HCWs.
Methodology:
A longitudinal observational study was carried out over a period of 2 years and another 6 months for follow-up. The study included all HCWs who tested positive in any one wave of COVID-19 pandemic with any one of the confirmed COVID-19 test. Each COVID-19-affected HCW was followed up through telephone calls and direct interviews conducted at the study site. Admission details and other background details of the study population were collected from the hospital records.
Results:
A total of 968 HCWs were COVID-19 positive in any of the three waves, and highest incidence (53.00%) was caused by the Omicron variant. High severity and hospitalization was observed in the first wave (no vaccination) and fully immunized personnel were found to be out of danger of being hospitalized during all succeeding waves (chi-square value: 87.04, p < 0.05). Predictors such as female gender, occupational exposure, and comorbid status were identified as possible risk factors for infection. A total of 70 HCWs reported with 104 complications, of which chronic diseases such as new onset of diabetes (n = 3), cardiovascular events (n = 8), worsening of preexisting comorbidities (n = 8), etc. were found out.
Conclusions:
This study proves the benefit of being immunized rather than the risk of being infected. This study documents that immunization impacted complication and hospitalization rates of COVID-19 infection. This evidence may help in tackling vaccine hesitancy across the nations.
Keywords: COVID-19 vaccination, health care workers, post-COVID-19 complications, re-infections
Introduction
In early December 2019, the sudden outbreak of a cluster of pneumonia cases with unknown etiology from the city of Wuhan (Hubei province, China) was reported. The identified pathogen had similar characteristics to Severe Acute Respiratory Syndrome (SARS) that appeared in 2002 in China. 1 The World Health Organization (WHO) classified the pathogen as Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-COV-2) and the related disease was named as Coronavirus Disease (COVID-19). 2 On 30 January 2020, WHO declared the outbreak as a Public Health Emergency of International Concern (PHEIC) and later as a pandemic on 11 March 2020. 3 The index case of the pandemic in India was reported on 30 January 2020, from Kerala, a southern state of the country. 4
A developing country such as India suffered drastically from the three consecutive waves of the COVID-19 pandemic in various aspects. On 25 March 2020, the country exceeded 600 diagnosed cases of COVID-19 infection and reached a peak of 98,000 cases by mid-September (the first wave). 5 A steady decline of cases was observed following the next 4 months but reappeared with a more virulent variant of concern (the Delta variant) during the second wave. Over one-half million cases and more than 6000 deaths were reported in June 2021 in the country. 6 On 16 January 2021, the world’s largest vaccination drive was launched in India to vaccinate its large population. 7 However, a third wave also struck the country in the first month of 2022 (the Omicron variant). 5
Among the frontline workers, the health care workers (HCWs) were considered the high-risk population who dealt with this less-understood pathogen initially. There were different hurdles for HCWs such as low neutralizing antibodies generated via previous infection or vaccination, diagnostic detection failure, low treatment or immunization effectiveness, vaccine hesitancy, etc., which remained as add-on burdens to existing challenges. 6 Majority of the countries represent less than 3% of the population with HCWs, while a middle-income country such as India accounts for 5.76 million (0.42% of its total population) HCWs. 8 Globally, 14–35% of COVID-19 cases were reported among HCWs according to WHO. 9
According to the WHO Program for International Drug Monitoring (PIDM) database, till date a total of 335,052 re-infection cases and 6470 vaccine breakthrough cases have been reported 10 while Indian studies alone account for a high rate of re-infection (incidence range of 4.5–34.8%) and breakthrough infections (incidence range of 0.4−13%) among HCWs.11–14 On the 6th of November 2020, the Centers for Disease Control defined ‘prolonged contact’ as the cumulative period of exposure of 15 min or more to an infected person(s) within a period of 24 h. 15 This ensures the safety concerns of HCWs, who daily work in a highly infectious environment (including many subclinical and undiagnosed cases).
Thus the recurrent infections and high-risk environment make HCWs a vulnerable population, who require immediate attention to their health status. Apart from different physical and mental traumas faced during the pandemic, numerous studies reported a high incidence of post-COVID-19 complications among HCWs. 16 While long COVID-19 symptoms, the onset of acute/chronic diseases after infection, and other extra-pulmonary complications were less covered areas, here the study attempted to detail the impact of the pandemic on HCWs on various dimensions such as infection outcomes, severity, risk factors, and pattern in three different COVID-19 waves. The study aim was to evaluate and compare the incidence, prevalence, severity, risk factors, and variations in the pattern of COVID-19 infection among HCWs during the three different waves that hit the country. The study also extends to assess the impact of vaccination and provides a detailed follow-up of post-COVID complications among the study population.
Materials and methodology
This was a longitudinal observational study, carried out retrospectively over a period of 2 years (April 2020–April 2022). The follow-up period of the study population was completed in October 2022. The study was conducted among the HCWs employed in JSS Hospital, Mysuru. This study was reviewed and approved by the Institutional Ethics Committee of study site (Ref. No: JSSMC/IEC/240921/01NCT/2021-22). The study included all HCWs who tested positive in any one wave of COVID-19 pandemic; with any of the confirmed COVID-19 test (approved by the Indian Council of Medical Research).
The study site consists of 1850 HCWs employed in various departments of the hospital, by excluding all the outsourced workers like securities, cleaning staffs, etc. Here the study was limited to the in-house staffs only, due to the limitation of medical records of outsourced staffs (medical check-up and health policies differ according to the outsourcing agency). Out of 1850 HCWs, 968 were tested COVID-19 positive in all three waves and were identified as eligible participants to be included in this study. All 968 positive HCWs were identified from the records maintained by the microbiology and human resources departments of the study site. The study also excluded all HCWs who did not take a laboratory test confirming COVID-19 infection during the study period.
All eligible study participants were enrolled after taking informed consent exclusively designed as per the requirements of Indian Council of Medical Research guideline for biomedical research on human subjects. Demographics, details of COVID-19 infection, and contact details of eligible participants were collected in each wave; later they were followed up for any recurrent infection and post-COVID-19 complications. In the study, the SARS-CoV-2 re-infection is defined by the reappearance of COVID-19 clinical symptoms with viral nucleotide re-positivity in convalescent patients within 90 days exposed to hazardous environments or closing contact with infections. The post-COVID-19 complications is defined as those who suffer from any of the health issues for a long period of time even after recovering from the COVD-19 infection.
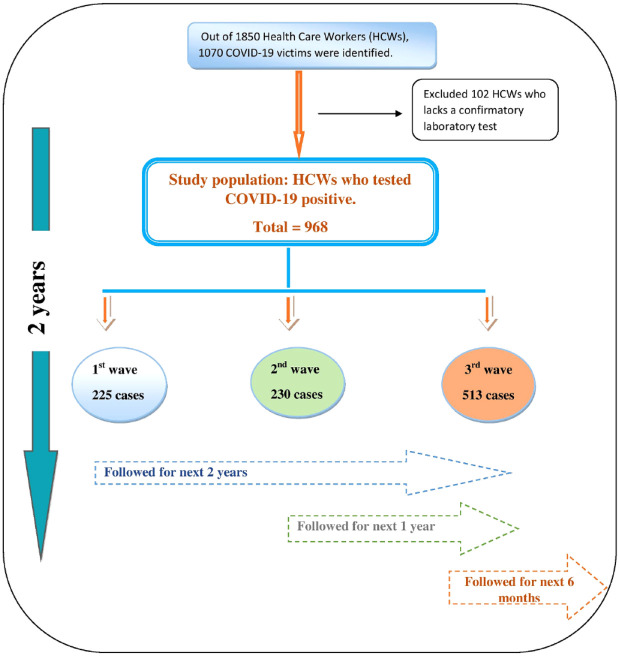
The study population who tested COVID-19 positive in the first wave of the pandemic (i.e., in the year 2020) was actively followed up for the next 2 years for any re-infection and delayed post-COVID complications. Similarly HCWs who tested positive during the second (2020–2021) and third (2022) waves were also followed up for another 1 year and 6 months, respectively. The vaccination status of each study participants was considered at the point of their infection. Each individual in the study population was interviewed either through personal or telephonic contact during the entire follow-up period with a predefined questionnaire to collect the information. In order to reduce the recall bias of the study population, the study team cross-verified with the records of leave application associated with COVID-19 infection documented by the human resources department.
All the HCWs were interviewed, and the relevant information details regarding their COVID-19 infections were documented in the suitably designed data collection form. Apart from the demographic and COVID-19 infection details, additional information details regarding their health status, comorbid status, vaccination status, medical and medication history, preexisting COVID-19 symptoms, and post-COVID complication were interviewed and documented in the data collection form. The study team reviewed medical records and other supporting materials for those who diagnosed with any of the chronic disorders after the infection. The previous medical records of HCWs with a history of re-infection were clubbed together in each wave for the ease of evaluation. This helped the study team to reduce the possible duplication errors during the entire study period.
Statistical analysis
The data obtained were compiled and entered in an Excel spread sheet and analyzed using IBM Statistical Package for the Social Sciences (SPSS) software version 16.0 (licensed to JSS University). Proportions and Chi-square test along with 95% confidence interval were used to express the results. The relative risk of infection of the study population was determined by dividing the incidence of infection among health care professionals (HCPs) by the incidence of infection among non-HCPs.
Result
According to the human resources department records, a total of 1070 (57.84%, n = 1070/1850) HCWs suffered from COVID-19 infection in all three waves. The study excluded 9.53% (n = 102/1070) HCWs with the classical symptoms of COVID-19 infection due to the lack of a confirmed laboratory test (89 HCPs and 13 non-HCPs were excluded). A total of 771 HCPs (out of 1159 HCPs) and 197 non-HCPs (out of 589 non-HCPs) were identified as eligible study population in the study site. Therefore the study was conducted among 968 HCWs who tested COVID-19 positive during the three consecutive waves of the pandemic. Of which 74.48% (n = 721/968) participants confirmed COVID-19 infection through the Real-Time Reverse Transcriptase test and the remaining 25.52% (n = 247/968) underwent the rapid antigen test. Eligible study population was identified in each wave of the pandemic and they were actively followed up for any post-COVID-19 complications. A detailed description of recruitment and follow-up of the study population is demonstrated in the consort diagram (Figure 1)
Figure 1.
Consort diagram of the study.
Among the three waves (that follow the same pandemic timeline that hits the country), the highest cases were reported in the third wave with an incidence rate of 53.00% (n = 513/968) as compared to the other two preceding waves. While the first wave reported high admission rates (increased severity) than the other two waves, the incidence rate and changes in the pattern of each wave of the pandemic are comprehended in Table 1.
Table 1.
Incidence and severity of COVID-19 cases in each wave of the pandemic.
| Wave | Number of cases | Incidence rate (%) | Asymptomatic | Home quarantine | Hospitalized | ICU admission | Death |
|---|---|---|---|---|---|---|---|
| First wave (2020) | 225 | 23.24 | 12 | 146 | 59 | 17 | 1 |
| Second wave (2021) | 230 | 23.76 | – | 173 | 35 | 3 | 1 |
| Third wave (2022) | 513 | 53.00 | 25 | 470 | 9 | 7 | 0 |
Impact of vaccination in each wave
Vaccines against COVID-19 were introduced in the middle of the second wave of the pandemic. The maximum utilized COVID-19 vaccine among the study population was COVISHIELD™. A significant link can be observed among the vaccine beneficiaries and low severity of infection in all waves reported in the study site. A detailed graph of vaccine utilization and variation in the severity pattern of the infection in each wave can be compared in the following figures and table (Figures 2 and 3, and Table 2).
Figure 2.
Risk of infection among non-vaccinated HCWs.
Figure 3.
Right side: Vaccination status of the study population at the point of infection. Left side: COVID-19 vaccine utilization among the study population.
Table 2.
The vaccination status and infection severity among the study population during the three waves of pandemic.
| The vaccination status of the study population | Number of asymptomatic study population | Number of home quarantined study population | Number of hospitalized study population | Number of ICU admission among the study population | Number of death reported in the study population |
|---|---|---|---|---|---|
| Fully vaccinated | 55 | 173 | 5 | 0 | 0 |
| Two doses | 77 | 285 | 15 | 4 | 0 |
| One dose | 0 | 20 | 31 | 9 | 1 |
| Not vaccinated | 0 | 188 | 81 | 23 | 1 |
Fully vaccinated group includes all who immunized including the precautionary dose (total three doses).
During the entire study period, 30.27% (n = 293/968) of the study population remained as non-immunized with any of the COVID-19 vaccine (at the point of infection). The risk of infection and associated morbidity can be observed more among non-vaccinated HCWs. A significant reduction in severity and hospital admission can be accounted for among HCWs who were vaccinated at least with one dose of any of the approved vaccines against COVID-19.
Incidence of re-infection among HCWs
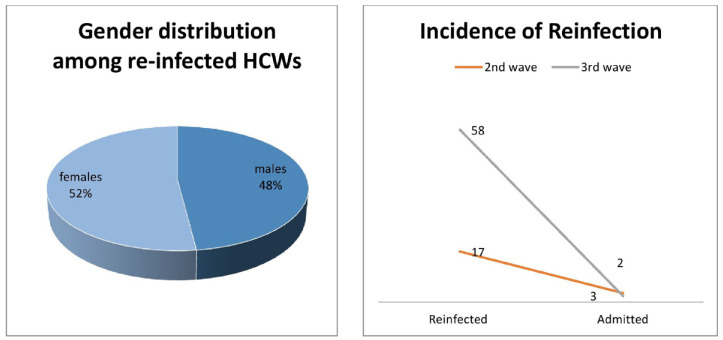
During the entire study period, the incidence rate of re-infection among the HCWS was accounted for as 7.75% (n = 75/968).The demographic details and other possible factors for multiple infections among HCWs were described below in Figure 4.
Figure 4.
Re-infection among HCWs accounted in the succeeding waves.
High incidence of re-infection among the study population was reported in the third wave (77.33%, n = 58/75), and there is no particular gender preference that was observed for re-infection in any of the waves. During the second wave, a total of 17 HCWs were reported with re-infection, of which 64.71% (n = 11/17) and 35.29% (n = 6/17) were received with one and two doses of COVID-19 vaccine, respectively. Similarly the third wave accounted for 58 HCWs with re-infection, of which majority of the re-infection was reported with HCWs who had received two doses of vaccine (72.41%, n = 42/58) as compared to those who had observed all vaccine schedules (including precautionary dose) (27.58%, n = 16/58). Occupational exposure is another risk factor for re-infection, HCPs (91.01%, n = 881/968) were accounted with a high chance of multiple infections and associated health risk as compared to non-HCPs (8.99%, n = 87/968). A comparison between the both groups is depicted in Figure 5.
Figure 5.
Incidence of re-infection and associated severity among health care professionals (HCPs) and non-HCPs.
Post-COVID complications among HCWs
The study population was followed up for a certain period of time after the infection in order to determine the incidence of any post-COVID complications. A very small proportion of male HCWs (22.86%, n = 16/70) reported with post-COVID-19 complications as compared to female HCWs (77.14%, n = 54/70) among the study population. A majority of long haulers belong to the age group of 20–30 years (52.85%, n = 37/70) and 20% of them belong to the 31–40 years age group.
The study identifies a total of 104 post-COVID complications among 70 HCWs. Majority of the complications were categorized under general disorders (29.81%, n = 31/104) followed by respiratory disorders (20.20%, n = 21/104) in the study population. A total of 13.46% (n = 14/104) events were categorized as chronic post-COVID complications. The reported complications were classified and described according to the system organ classification in Table 3.
Table 3.
Various post-COVID complications reported among health care workers (HCWs) during three waves.
| I. Respiratory system | 21 |
| (a) Cough | 8 |
| (b) Breathlessness/dyspnea | 10 |
| (c) Chest tightness | 1 |
| (d) Bronchitis | 1 |
| (e) Tonsillitis | 1 |
| II. Cardiovascular disorders | 8 |
| (a) Pericarditis | 1 |
| (b) Hypertension | 3 |
| (c) LVH | 3 |
| (d) Tachycardia | 1 |
| III. General disorders | 31 |
| (a) Pain (body pain, back pain, leg pain, joint pain, limb pain, orthopedic pain) | 10 |
| (b) Weakness/tiredness/fatigue | 17 |
| (c) Dizziness | 4 |
| IV. Gastrointestinal disorders | 7 |
| (a) Gastritis | 2 |
| (b) Loose stools | 1 |
| (c) Loss of appetite | 2 |
| (d) Loss of smell (anosmia) | 2 |
| V. Skin and appendages | 5 |
| (a) Hair fall | 5 |
| VI. Reproductive disorders | 5 |
| (a) Irregular periods | 2 |
| (b) Cystitis | 1 |
| (c) PCOD | 2 |
| VII. CNS disorders | 7 |
| (a) Headache | 4 |
| (b) Migraine | 3 |
| VIII. Endocrine disorders | 3 |
| (a) New onset of diabetes mellitus | 3 |
| IX. Metabolic and nutritional disorders | 5 |
| (a) Weight loss | 2 |
| (b) Obesity | 2 |
| (c) Vitamin D deficiency | 1 |
| X. Psychiatric disorders | 2 |
| (a) Stress | 1 |
| (b) Sleep disturbance | 1 |
| XI. Infections and immune disorders | 2 |
| (a) Chickenpox | 1 |
| (b) Autoimmune arthritis | 1 |
| XII. Worsening of pre-existing comorbidities | 8 |
| (a) Asthma | 2 |
| (b) Diabetic mellitus | 1 |
| (c) Hypertension | 1 |
| (d) Migraine | 2 |
| (e) Joint pain/orthopedic issues | 2 |
LVH, left ventricular hypertrophy; PCOD, Polycystic Ovarian Disease.
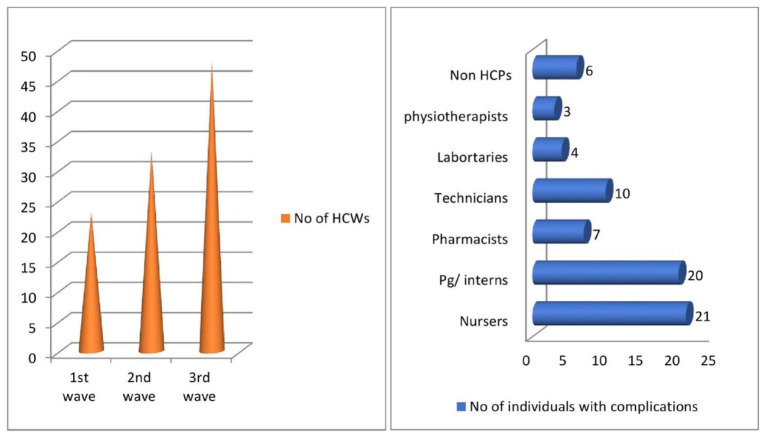
Certain factors which can be potentiated for post-COVID complications were also estimated in this study. An increased incidence of complications was noticed in the third wave (46.15%, n = 48/104) while the second wave accounted for 31.73% (n = 33/104) and the first wave for 22.11% (n = 23/104), respectively. Occupational exposure was considered as one of the major risk factors estimated for post-COVID complications in the study population. Among 7 out of 65 HCWs (10.77%), occupational exposure was considered as one of the major risk factors estimated for post-COVID complications in the study population; another 10.77% (7 out of 65 HCWs with comorbidity) reported severe post-COVID complications during the study period. Estimated potential factors for post-COVID complications have been graphed in Figure 6.
Figure 6.
Right sided: Incidence of post-COVID complications in each wave of pandemic. Left sided: Occupational exposure and incidence of post-COVID complications.
Risk factors and predictors of COVID-19 infection among HCWs
The severity, morbidity, and mortality rate of the study population toward the new virulent infection differ from one person to another one. Here the study tries to understand different risk factors and possible predictors for the infection among the HCWs. The below graph (Figure 7) illustrates the impact of various factors such as age, gender, occupational exposure, and primary contacts as possible predictors for COVID-19 infection. The median age of the study population infected in all three waves of the pandemic was 34.49 ± 10.02.
Figure 7.
Different risk factors of health care workers (HCWs) for COVID-19 infection in each wave: (a) Gender, (b) age category, (c) primary contacts, (d) occupational exposure, and (e) co-morbid status.
The study shows a 59.40% (n = 575/968) of the infected cases were among female gender and highest infected HCWs were between the ages of 20 and 40 years. A total of 69.11% (n = 669/968) of the HCWs had a known history of hospital contact (occupational exposure) and nurses were the mostly infected HCWs in all waves. A hike was observed among the post-graduates and interns only during the third wave (exceeds the nursing staffs). A total of 6.71% (n = 65/968) of the infected HCWs had a history of comorbid condition, of which thyroid-related disorders (n = 22) were reported high among these study populations.
A significant effectiveness was observed between fully vaccinated and not vaccinated HCWs with a Chi-square value of 86.193 (p value <0.05) in the confidence interval of 95%. Similarly remarkable impact was noticed even after partial immunization of COVID-19 as compared to the risk of non-vaccinated HCWs. Detailed statistical difference between the vaccine beneficiaries (at least with one dose of any approved vaccines) and being at the risk of infection is depicted separately in Table 4.
Table 4.
Association of vaccination status and risk of hospitalization.
| S. No. | Variable 1 | Variable 2 | Chi-square value | p-Value | RR of hospitalization | OD of hospitalization |
|---|---|---|---|---|---|---|
| 1 | No. study population fully vaccinated (n = 233) | No. study population not vaccinated (n = 293) | 87.04 | <0.05 | 0.06 | 0.04 |
| 2 | No. study population fully vaccinated (n = 233) | No. study population taken two doses (n = 381) | 2.39 | 0.779 | 0.44 | 0.42 |
| 3 | No. study population fully vaccinated (n = 233) | No. study population taken one dose (n = 61) | 145.17 | <0.001 | 0.03 | 0.01 |
| 4 | No. study population taken two doses (n = 381) | No. study population not vaccinated (n = 293) | 102.94 | <0.001 | 0.14 | 0.09 |
| 5 | No. study population taken two doses (n = 381) | No. study population taken one dose (n = 61) | 161.67 | <0.05 | 0.08 | 0.03 |
| 6 | No. study population taken one dose (n = 61) | No. study population not vaccinated (n = 293) | 18.46 | <0.05 | 1.83 | 3.41 |
Vaccination status of HCWs considered at the point of infection.
HCW, health care worker; OD, odds ratio; RR, relative risk.
A significant difference of being hospitalized among the study population was not able to be determined between fully vaccinated and those who received two doses of vaccine. While all other vaccination status of the HCWs shows significant difference in the reduction of hospitalization associated with the infection severity, low risk of hospitalization was observed among fully vaccinated HCWs and increased risk estimated between not vaccinated and those received one dose of vaccine.
Risk factors for re-infection
During the study period, various risk factors were identified to impact the re-infection frequency in the study population: gender was not identified as a potential factor to develop re-infection among the study population. HCPs were more prone to have re-infection as compared to the non-HCPs (statistically significant), and third wave (omicron variant) accounted more chances of re-infection among HCPs as compared to the second wave. Younger age groups (20–40 years) had less incidence of re-infection as compared to the elder age group. Low re-infection rate was identified among fully vaccinated HCWs as compared to the partially vaccinated (received one or two doses of COVID-19 vaccine) study population. The association between these risk factors and the re-infection rate among the study population is detailed in Table 5.
Table 5.
Association between various risk factors and re-infection among the study population.
| S. no. | Risk factors | Re-infected HCWs | Study population with no incidence of re-infection. | Chi square value | p Value |
|---|---|---|---|---|---|
| 1. | Gender | ||||
| Males | 36 | 357 | 1.846 | 0.174 | |
| Females | 39 | 536 | |||
| 2. | Occupational exposure | ||||
| HCPs | 68 | 703 | 6.088 | <0.001 | |
| Non-HCPs | 7 | 190 | |||
| 3. | Age category | ||||
| 20–30 years | 14 | 395 | 1* | ||
| 31–40 years | 45 | 253 | 30.735 | <0.001 | |
| 41–50 years | 16 | 149 | 9.343 | 0.0022 | |
| 4. | COVID-19 pandemic wave | ||||
| Second wave | 17 | 213 | 5.0217 | 0.025 | |
| Third wave | 68 | 455 | |||
| 5. | Vaccination status | ||||
| Fully vaccinated | 16 | 217 | 1* | ||
| Received two doses | 48 | 333 | 5.086 | 0.0241 | |
| Received one dose | 11 | 50 | 7.2267 | 0.0072 | |
It is used as the reference value. p Values less than 0.01 and 0.05 are considered as statistically significant risk factor.
HCP, health care professional; HCW, health care worker.
Discussion
Worldwide, the COVID-19 pandemic distressed the mental and physical health of HCWs abundantly, because they were the main supporting system against this unprepared medical emergency. The study site alone accounted an incidence rate of 52.32% (968 HCWs tested COVID-19 positive out of 1850) in all the three consecutive waves of the pandemic. The incidence of infected HCPs was calculated as 66.52% (n = 771/1159) and 33.45% (n = 197/589) was the incidence rate of infection among non-HCPs during the study period. This accounted a relative risk of infection among the study population as 1.99, which implies HCPs were more prone for COVID-19 infection as compared to the non-HCPs in this study. Of which maximum number of HCWs tested positive in the third wave with an incidence rate of 53.05% (n = 513/968). While the other two waves have similar graph with an incidence rate of 23.24% and 23.76% in the first and second waves, respectively. A steep hike of positive cases in the third wave can be explained by the high transmissibility of the Omicron variant. 17 Whereas reduced hospitalization and no death associated with the infection in the third wave points out the effectiveness of COVID-19 vaccines. Numerous studies support that the rapidly developed COVID-19 vaccines even though fail to prevent the infection have significant impact to reduce the disease burden and mortality rate among the vaccine beneficiaries.18–21
The impact of vaccination among the study population can be compared between the patients in the first wave (who were not vaccinated) and others who tested positive in the succeeding waves (vaccinated with at least one dose of COVID-19 vaccine). During the entire study period, a total of 30.27% (n = 293/968) were categorized as non-vaccinators (majority belongs to the first wave) at the point of infection. The immunization status of the study population for the entire study period is 24.07% (n = 233/968) as full vaccinators (includes precautionary dose), 39.36% (n = 381/968) with two doses, and 6.30% (n = 61/968) received only one dose of vaccine at the point of infection. The risk of infection in each wave depends on many factors such as the variant causing the infection, virulence of the mutated virus, frequency of exposure, and high occupational contact, etc. 22 Therefore it was proven by the contemporary studies that vaccine alone could not help to prevent the risk of infection among HCWs, but resulted a significant reduction in mortality and associated morbidity. 23
Here the study could track a significant reduction in mortality and hospitalization rate in each subsequent wave after the introduction of vaccine. High hospital admission was reported in the first wave with an incidence of 37.33% (n = 84/225) and encountered one death. Soon after the intervention of vaccines, within a gap of few months, the delta-driven second wave hits the study site and a low admission rate (16.96%, n = 39/230) can be traced out. Of which four HCWs were critical and admitted in the intensive care unit (ICU). A similar reduction of hospitalization (3.12%, n = 16/513) during the third wave was observed, of which seven required ICU admission and no death was observed.
On the other hand, a small percentage of HCWs (5.91%, n = 28) remained as non-vaccinators in the second and third waves, among them 16 (57.14%, n = 16/28) reported severe symptoms of infection and seven (25%, n = 7/28) of the HCWs required the physician’s consultation/hospitalization. The case fatality rate of the study population was 0.21% (n = 2/968), where one death was reported in the first wave (not vaccinated) and second death was during the second wave (received one dose of COVISHIELD vaccine). Both of them had other comorbid complications and were aged above 50 years at the time of death. A study conducted in different phases of the pandemic concluded that high risk of mortality and disease burden were associated with patients having any of the comorbid complications. 24 Therefore the comorbid status of the deceased HCW should be taken into consideration than immunization status (one dose). The case fatality rate among non-vaccinators calculated as 0.34% (n = 1/293) and among partially vaccinated as 1.63% (n = 1/61).
The study tried to determine different factors such as gender, age, occupational exposure, and comorbid status as potential predictors for infection. Here female HCWs were identified with high probability for infection as compared to the male population in all three waves (Chi square value: 13.07, p < 0.05). In contrast, only the first wave marks a small hike in male population as compared to female HCWs. The study conducted by Sobotka et al. 25 provides similar observation of high burden of infection among female population. While here the study could not determine age as a potential predictor (p > 0.05), this can be due to the fact that most of the HCWs were aged between 25 and 40 years and the study site has very less HCWs in the geriatrics age group.
Occupational exposure was another weighty factor identified in the study, where more incidence of infection and associated burden was found among the HCPs (Chi-square value: 3.824, p value <0.05) as compared to non-HCPs. Also the study could overlook the exposure history of the study population, where high infection rate was found among those who had a history of contact inside the hospital settings (chi-square value: 6.355, p < 0.05). A similar study conducted among the HCWs of United Kingdom and United States supports that more risk of occupational exposure among HCWs as compared to the general population. 26 At the same time, a Japanese study states that no difference was found between the general population and HCWs. 27 A multi-centered comparative study among HCWs conducted by Wei et al. 28 identified general medicine, respiratory, and ophthalmology as the three topmost departments with high chances of COVID-19 infections inside hospital settings. While in this study, the study team could understand more number of nursing staffs (irrespective of departments) are equally affected in all three waves, this study could not understand the impact of comorbid status over the infection, because a very small number of HCWs (6.71%, n = 65/968) had comorbid condition.
An average of 80% reduction in re-infection was estimated according to Sarscov2 Immunity & RE-infection Evaluation (SIREN) studies among those with a pre-history of infection.29–31 However the study site could determine an incidence of 7.75% (n = 75/968) re-infections during all the three consecutive waves. Of which five of them were hospitalized and the high severity was reported. This contraindicates the prediction of immunity acquired through previous infection in SIREN studies while other factors such as multiple exposures to the prone areas of infection, 12 prevalence of mutant variants of coronavirus, 18 and range of antibody titers in each individual 30 should be taken into consideration. Among the study population, majority (n = 58) of them were re-infected in the third wave and five of the nursing staffs reported re-infection in all three waves irrespective of their immunization status. This study could find numerous risk factors such as age (old age more prone for infection than young age), occupational exposure (HCPs more prone than non-HCPs), variant of infection (Omicron variant in the third wave was more infectious than the Delta variant in the second wave), and vaccination status (partially vaccinated is more prone to have infection than fully vaccinated) as potential agents for re-infection in the study population. In the study, HCPs were found out to be the most vulnerable population with a high chance of frequent infections, which supports the inefficiency of neutralizing antibodies to prevent or reduce the severity of re-infection. 32 Additionally, several factors such as lower antibody production in prior infections, blood type, virulence of mutated virus, and being a HCW were identified as potential agents for re-infection among Brazilian and European HCWs.33,34
The long-term impact of COVID-19 pandemic can be directly measured through the prevalence of post-COVID-19 health complications. Numerous studies reported during the pandemic stated persistence of long-term post-COVID-19 complications among HCWs with an average incidence rate of 10%.35–37 This study could observe various health complications such as long COVID syndrome (persistence of COVID symptoms beyond weeks and months after recovery), worsening of preexisting comorbidities, and onset of new comorbid conditions, etc. Female predominance (77.14%, n = 54/70) and young infection survivors (74.28%, n = 52/70) irrespective of the severity of their symptoms were identified as victims of post-COVID complications in this study population. The prolongation of respiratory symptoms as well as initiation of other extra-pulmonary complications and the age group (30–40 years) of long haulers identified in this study match with other similar study observations. 38
The study population reported more number of general disorders such as fatigue, weakness, and joint and body pain continued beyond an average of 3 weeks to 4 months. Followed by respiratory system disorders (20.20%, n = 21/104), of which a high rate of breathlessness or dyspnea was preexisted at least for a period of 6 months after the infection. Chronic complications such as cardiovascular manifestations 39 (7.70%, n = 8/104) were diagnosed in this study population makers as a critical observation in the study. One among the HCW who diagnosed with pericarditis after 2 months of COVID-19 infection matches with similar case reports.40,41 Other major chronic manifestations diagnosed after COVID-19 infections such as new onset of diabetic mellitus, 42 hypertension, 43 left ventricular hypertrophy (LVH), 44 autoimmune arthritis, 45 chicken-pox 46 in the study population have shown similarities with identical case reports from the literature search. Significantly, all of these chronic complications were detected among the HCWs who had frequent exposure in high-risk environments in the hospital (such as staffs in ICU, COVID ward, and other intensive medical unit).
This study could also showcase some of the post-COVID complications which affect the reproductive health of women (cystitis, 47 irregular periods, 48 polycystic ovarian disease 49 ). The result of metabolic disturbance due to the cytokine storm induced by COVID-19 infection can be the most possible explanation for these chronic delayed complications. A study conducted by Raveendran 50 addresses different challenges for confirming these delayed complications after the infection and he listed out certain criteria’s for its diagnosis and classification. Accordingly, 78.85% (n = 82/104) of the reported events in this study population can be categorized as confirmed post-COVID complications, while 11.54% (n = 12/104) were possible and 9.62% (n = 10/104) as doubtfully confirmed events.
Another trend that was observed in the study was the worsening of preexisting comorbid conditions among HCWs. An incidence rate of 7.69% (n = 8/104) of the study population reported with worsening of their previous health condition. This indicates the excessive burden tolerated by the frontline workers. A number of long-COVID haulers among the study population were identified in the third wave (68.57%, n = 48/70), and nurses followed by PG and interns were tracked as the most vulnerable population for post-COVID complications in the study. Among the long-COVID haulers, a total of 27.14% (n = 19/70) had a history of re-infections in any of the three waves of the pandemic. Multiple infection resulted in the study population getting exposed to more than one variant of SARS-CoV-2 virus, which indicates a need to enquire the influence of re-infection over post-COVID complications. Here almost all of the victims of post-COVID syndromes were vaccinated at least by two doses of COVID-19 vaccines (only one HCW remained as non-vaccinator) and therefore the effectiveness of immunization to protect them against these delayed complications also should be analyzed further in detail.
Conclusion
The impact of the pandemic, effectiveness of immunization, and the outcomes among the HCWs are specially handled topic. Multiple exposure, continuous working hours in a highly contaminated environment, frequent infections, and repeated immunity interactions with mutated variants, etc. make them a special population to be monitored continuously. This study could bring out many of the long-term struggles faced by HCWs through a small cohort with close monitoring. At the same time, many of the acute and chronic complications after the infection reported from HCWs of a single site highlight the urgent need to address this situation globally. An alarming need is generated through this study to give more attention toward certain areas such as COVID-19-related post-discharge surveillance, asymptomatic infection, re-infections, and dynamic monitoring of genomic mutation of the virus.
Here most of the study population was vaccinated with any of the approved COVID-19 vaccines, and to an extent, the study could portrait the impact of immunization, especially in the prevention of infection-associated morbidity and mortality rate. The continuous re-infections among the study population points out the necessity of variant-specific vaccines for better immunity coverage. Today, vaccine safety is a major concern that leads to unnecessary safety hesitancy among the public. In such a scenario, this study could expose a low risk of vaccine-related health problems as compared to the disease burden of the infection (including the post-COVID complications). Thus this study could once again prove the benefit of being immunized rather than the risk of being infected.
Limitations of the study
The study and its observations were limited to single centered HCW cohorts and the study population was limited to only those with a confirmed COVID-19 laboratory test. The study team had excluded the HCWs with classical symptoms of COVID-19 infections with a negative test or those who did not undergo a laboratory confirmation test. This was an observational study, and no interventions were made in any of the phases of identification and diagnosis of post-COVID complications.
The study population had maximum utilizers with COVISHEILD™ vaccine (adeno-vector vaccine) and utilizers of other vaccines were very less, which made the study team impossible to compare and determine the effectiveness of different types of vaccines. Lastly, the study team was not able to afford a genomic analysis to identify the culprit(s) (mutated variant) that leads to three different waves in the study site. Here the study also follows the same timeline of variant sequences that affected the country. Different parts of the country isolated with new mutated variants that caused an increased disease burden and long-term complications. Therefore, inability to isolate the particular variant in the study site is considered as the major drawback of the study.
Acknowledgments
Authors would like to express sincere thanks to the administration, human resource department, and hospital infection control committee of JSS Hospital for providing necessary resources for the research. The support of the faculty and students of Department of Clinical Pharmacy and Pediatrics of JSS Hospital, Mysuru are also acknowledged.
Footnotes
ORCID iD: Juny Sebastian  https://orcid.org/0000-0002-4626-8729
https://orcid.org/0000-0002-4626-8729
Contributor Information
Merrin Mathew, Department of Pharmacy Practice, JSS College of Pharmacy, JSS Academy of Higher Education and Research, Mysuru, India.
Juny Sebastian, Department of Pharmacy Practice, College of Pharmacy, Gulf Medical University, Ajman, United Arab Emirates.
Narayanappa Doddaiah, Department of Pediatrics, JSS Medical College and Hospital, JSS Academy of Higher Education and Research, Mysuru, Karnataka 570004, India.
Anmaria Thomas, Department of Pharmacy Practice, JSS College of Pharmacy, JSS Academy of Higher Education and Research, Mysuru, India.
Sinchana Narayanappa, Department of Radio Diagnosis, JSS Medical College, JSS Academy of Higher Education and Research, Mysuru, India.
Declarations
Ethics approval and consent to participate: This study was approved by the Institutional Ethics Committee of the study site (Ref No: JSSMC/IEC/240921/01NCT/2021-22).
Consent for publication: Not applicable.
Author Contribution(s): Merrin Mathew: Conceptualization; Investigation; Methodology; Project administration; Supervision; Writing – original draft.
Juny Sebastian: Conceptualization; Formal analysis; Methodology; Supervision; Validation; Writing – review & editing.
Narayanappa Doddaiah: Conceptualization; Methodology; Supervision; Writing – review & editing.
Anmaria Thomas: Data curation; Investigation; Methodology; Resources.
Sinchana Narayanappa: Methodology; Validation; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare that there is no conflict of interest.
Availability of data and materials: The study data and materials are available with the authors and will be provided on request.
References
- 1.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395: 565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (2019, accessed 17 February 2023).
- 3.World Health Organization. COVID-19 situation reports – 130, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (2020, accessed 7 October 2022).
- 4.Andrews MA, Areekal B, Rajesh KR, et al. First confirmed case of COVID-19 infection in India: a case report. Indian J Med Res 2020; 151: 490–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mangal DK, Gupta SD. The third wave of COVID-19 pandemic in India: is it inevitable? J Health Manag 2021; 23: 365–367. [Google Scholar]
- 6.Tareq AM, Emran TB, Dhama K, et al. Impact of SARS-CoV-2 delta variant (B.1.617.2) in surging second wave of COVID-19 and efficacy of vaccines in tackling the ongoing pandemic. Hum Vaccines Immunother 2021; 17: 4126–4127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaghela G, Narain K, Isa MA, et al. World’s largest vaccination drive in India: challenges and recommendations. Health Sci Rep 2021; 4: e355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karan A, Negandhi H, Hussain S, et al. Size, composition and distribution of health workforce in India: why, and where to invest? Hum Resour Health 2021; 19: 39–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Keep health workers safe to keep patients safe: WHO. [Internet], https://www.who.int/news/item/17-09-2020-keep-health-workers-safe-to-keep-patients-safe-who (2020, accessed 7 September 2022).
- 10.World Health Organization. Vigiaccess. [Internet], http://www.vigiaccess.org (2015, accessed 7 September 2022).
- 11.Malhotra S, Mani K, Lodha R, et al. SARS-CoV-2 reinfection rate and estimated effectiveness of the inactivated whole virion vaccine BBV152 against reinfection among health care workers in New Delhi, India. JAMA Netw Open 2022; 5: e2142210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dev N, Meena RC, Gupta DK, et al. Risk factors and frequency of COVID-19 among healthcare workers at a tertiary care centre in India: a case–control study. Trans R Soc Trop Med Hyg 2021; 115: 551–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah JN, Samson P, Pradhan NMS, et al. Breakthrough infection after COVID-19 vaccination: a threat for Nepal due to SARS-CoV-2 variants circulating in 2nd wave ravaging India. J Patan Acad Health Sci 2021; 8: 69–79. [Google Scholar]
- 14.Abhra B, Kheya M, Debojyoti B, et al. Status of health-care workers in relation to COVID-19 infection: a retrospective study in a level 4 COVID hospital in Eastern India. J Assoc Physicians India 2020; 68: 55–57. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for health care personals during the coronavirus disease 2019 (COVID-19) pandemic, https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html (2022, accessed 23 September 2022).
- 16.Silva Andrade B, Siqueira S, de Assis Soares WR, et al. Long-COVID and Post-COVID health complications: an up-to-date review on clinical conditions and their possible molecular mechanisms. Viruses 2021; 13: 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ranjan R. Omicron impact in India: analysis of the ongoing COVID-19 third wave based on global data. BMJ 2022; 13: 1–16. [Google Scholar]
- 18.Haghpanah F, Lin G, Levin SA, et al. Analysis of the potential impact of durability, timing, and transmission blocking of COVID-19 vaccine on morbidity and mortality. EClinicalMedicine 2021; 35: 100863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saban M, Myers V, Wilf-Miron R. Changes in infectivity, severity and vaccine effectiveness against delta COVID-19 variant ten months into the vaccination program: the Israeli case. Prev Med 2022; 154: 106890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roghani A. The influence of COVID-19 vaccination on daily cases, hospitalization, and death rate in Tennessee, United States: case study. JMiRx Med 2021; 2: e29324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agarwala P, Bhargava A, Gahwai DK, et al. Epidemiological characteristics of the COVID-19 pandemic during the first and second waves in Chhattisgarh, Central India: a comparative analysis. Cureus 2022; 14: e24131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hussen H, Alemu ZA. Risk of COVID-19 infection and associated factors among healthcare workers: a cross-sectional study at EkaKotebe Treatment Center in Ethiopia. Int J Gen Med 2021; 14: 1763–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maltezou HC, Panagopoulos P, Sourri F, et al. COVID-19 vaccination significantly reduces morbidity and absenteeism among healthcare personnel: a prospective multicenter study. Vaccine 2021; 39: 7021–7027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stepanova M, Lam B, Younossi E, et al. The impact of variants and vaccination on the mortality and resource utilization of hospitalized patients with COVID-19. BMC Infect Dis 2022; 22: 702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sobotka T, Brzozowska Z, Muttarak R, et al. Age, gender and COVID-19 infections. MedRxiv. 2020. [Google Scholar]
- 26.Nguyen LH, Adrew D, Sgraham M, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Public Health 2020; 5: 475–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chano T, Yamashita T, Fujimura H, et al. Effectiveness of COVID-19 vaccination in healthcare workers in Shiga Prefecture, Japan. Sci Rep 2022; 12: 17621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wei JT, Liu ZD, Fan ZW, et al. Epidemiology of and risk factors for COVID-19 infection among health care workers: a multi-centre comparative study. Int J Environ Res Public Health 2020; 17: 7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall VJ, Foulkes S, Charlett A, et al. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN). Lancet 2021; 397: 1459–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hansen CH, Michlmayr D, Gubbels SM, et al. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet 2021; 397: 1204–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abu-Raddad LJ, Chemaitelly H, Coyle P, et al. SARS-CoV-2 antibody-positivity protects against reinfection for at least seven months with 95% efficacy. EClinicalMedicine 2021; 35: 100861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dimeglio C, Herin F, Da-Silva I, et al. Decreased efficiency of neutralizing antibodies from previously infected or vaccinated individuals against the B.1.617.2 (Delta) SARS-CoV-2 variant. Microbiol Spectr 2022; 10: e0270621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adrielle Dos Santos L, Filho PGG, Silva AMF, et al. Recurrent COVID-19 including evidence of re-infection and enhanced severity in thirty Brazilian healthcare workers. J Infect 2021; 82: 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Porru S, Monaco MG, Spiteri G, et al. SARS-CoV-2 breakthrough infections: incidence and risk factors in a large European multicentric cohort of health workers. Vaccines 2022; 10: 1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pavli A, Theodoridou M, Maltezou HC. Post-COVID syndrome: incidence, clinical spectrum, and challenges for primary healthcare professionals. Arch Med Res 2021; 52: 575–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaber TAZK, Ashish A, Unsworth A. Persistent post-COVID symptoms in healthcare workers. Occup Med 2021; 71: 144–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tawfik HM, Shaaban HM, Tawfik AM. Post-COVID-19 syndrome in Egyptian healthcare staff: highlighting the carers sufferings. Electron J Gen Med 2021; 18: em291. [Google Scholar]
- 38.Vehar S, Boushra M, Ntiamoah P, et al. Post-acute sequelae of SARS-CoV-2 infection: caring for the ‘long-haulers’. Cleve Clin J Med 2021; 88: 267–272. [DOI] [PubMed] [Google Scholar]
- 39.Magadum A, Kishore R. Cardiovascular manifestations of COVID-19 infection. Cells 2020; 9: 2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaminski A, Albus M, Mohseni M, et al. A delayed case of pericarditis following recovery from COVID-19 infection. Cureus 2021; 13: e14397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tung-Chen Y. Acute pericarditis due to COVID-19 infection: an underdiagnosed disease? Med Clin 2020; 155: 44–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burekovic A, Asimi ZV, Divanovic A, et al. Diabetes – a consequence of COVID-19 infection. Mater Sociomed 2022; 34: 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shouman K, Vanichkachorn G, Cheshire WP, et al. Autonomic dysfunction following COVID-19 infection: an early experience. Clin Auton Res 2021; 31: 385–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Unudurthi SD, Luthra P, Bose RJC, et al. Cardiac inflammation in COVID-19: lessons from heart failure. Life Sci 2020; 260: 118482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ferri C, Giuggioli D, Raimondo V, et al. COVID-19 and rheumatic autoimmune systemic diseases: report of a large Italian patients series. Clin Rheumatol 2020; 39: 3195–3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Dam CS, Lede I, Schaar J, et al. Herpes zoster after COVID vaccination. Int J Infect Dis 2021; 111: 169–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lamb LE, Timar R, Wills M, et al. Long COVID and COVID-19-associated cystitis (CAC). Int Urol Nephrol 2022; 54: 17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Al-Najjar MAA, Al-Alwany RR, Al-Rshoud FM, et al. Menstrual changes following COVID-19 infection: a cross-sectional study from Jordan and Iraq. PLoS One 2022; 17: e0270537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Prendergast H, Tyo C, Colbert C, et al. Medical complications of obesity: heightened importance in a COVID era. Int J Emerg Med 2022; 15: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raveendran AV. Long COVID-19: challenges in the diagnosis and proposed diagnostic criteria. Diabetes Metab Syndr 2021; 15: 145. [DOI] [PMC free article] [PubMed] [Google Scholar]