Abstract
For over 30 years, the International Society for Heart and Lung Transplantation (ISHLT) International Thoracic Organ Transplant (TTX) Registry has gathered data regarding transplant procedures, donor and recipient characteristics, and outcomes from a global community of transplant centers. Almost 70,000 adult lung transplant procedures have been reported to the Registry since its inception, each one providing an opportunity for a recipient with end-stage lung disease to regain quality of life and longevity. With each year’s report, we provide more detailed analyses on a particular focus theme important to recipient outcomes. Since 2013, these have been donor and recipient age; retransplantation; early graft failure; indication for transplant; allograft ischemic time; multiorgan transplantation; and donor and recipient size matching.1–7 In response to a changing regulatory environment, the ISHLT TTX Registry is undergoing an update in data acquisition, and the patient cohort examined in this report is therefore derived from the same data source or datasets as that examined in the 2019 annual reports.2,8–10 We refer the reader to the 2019 and prior reports for a detailed description of the baseline characteristics of the cohort, and additional core analyses not directly related to the focus explored in this year’s report. To complement the 2020 report which focussed on donor characteristics, the goal of this year’s report was to focus entirely on changes in recipient factors over the past 3 decades and to identify important recipient characteristics and transplant processes that may influence post-transplant outcomes. Due to small numbers, heart-lung transplant recipient characteristics and transplant outcomes have not been included. This 38th annual adult lung transplant report is hence basedon data submitted to the ISHLT TTX Registry on 67,493 adult recipients of deceased recipient transplants between January 1, 1992 and June 30, 2018.
Keywords: lung transplantation, recipient, characteristics, post-transplant, survival, registry, morbidity
Data collection, conventions and statistical methods
National and multinational transplant collectives and individual transplant centers submitted data to the ISHLT International TTX Registry. Since the Registry’s inception, 481 heart transplant centers, 260 lung transplant centers, and 184 centers that perform combined heart−lung transplants have reported data to the ISHLT TTX Registry.2, 8–10 This report references specific online e-slides when particular data are discussed but not shown due to space limitations; e-slide numbers refer to the online adult lung transplant slides, shortened to ‘L(a)’, and available at https://ishltregistries.org/registries/slides.asp. The ISHLT web site also contains slide sets for previous annual reports.
The ISHLT International TTX website (https://ishlt.org/research-data/registries/ttx-registry) provides detailed spread-sheets of the data elements collected in the Registry. The Registry required submission of core recipient, donor, and transplant procedure variables around the time of transplantation and at annual follow-up and thus, has low rates of missing data. Nevertheless, data quality depends on the accuracy, and completeness of reporting. Rates of missingness may significantly increase for Registry variables that depend on voluntary reporting. The Registry uses various quality control measures to ensure acceptable data quality and completeness before including data for analyses.
Analytical conventions
The current report includes data on adult recipients of deceased donor, lung alone, transplant procedures. Heart-lung and other combinations involving lung transplants are not included in this report. The Registry does not capture the exact occurrence date for most secondary outcomes, such as bronchiolitis obliterans syndrome (BOS), but it does capture a time period for which the event occurred (e.g., the event occurred between the first and the second year annual follow-up visits). For the report’s analyses, we use the mid-point between the annual follow-ups as a surrogate for the event date. Because deceased subjects no longer contribute to the secondary outcomes, to reduce the potential of underestimating event rates or other outcomes, we restrict some analyses to include only surviving recipients. For time-to-event analyses, we censor the follow-up of recipients who have not yet experienced the event at the most recent annual follow-up or the time of retransplantation. We truncate time-to-event graphs (e.g., survival graphs) when the number of individuals at risk becomes <10. Previous Registry report themes provide more details regarding specific donor and recipient characteristics and outcomes.1−7
Focus theme: Recipient characteristics
Lung transplantation has evolved from a rare procedure in the 1980s to a well-accepted option for patients with end-stage lung disease in the modern era. Over 3 decades of clinical experience, bolstered by evidence generated from resources such as the ISHLT TTX Registry, on a background of changing demography (an aging population, declining smoking rates, increasing prevalence of diabetes mellitus), has led to changes and refinements in recipient selection, and medical and surgical approaches. Against this backdrop, we examine recipient characteristics by year of transplantation. This report is complemented by similar analyses in pediatric lung11 and adult12 and pediatric13 heart recipients.
Adult lung transplant recipient characteristics stratified by era (1992–2000, 2001–2009, and 2010–2018) are presented in Table 1. The number of transplants performed has gradually increased over time, from just over 11,000 in the 1990s to almost 22,000 in the 2000s and then to almost 34,000 from 2010 to 2018. In North America the proportion of lung transplantations has fallen over time relative to the rest of the world. Median recipient age has steadily increased from 50 to 57 years (p < 0.0001), and the proportion of transplant recipients who are male has also increased from 52% to 58% in the most recent era (p < 0.0001). The aging of the recipient population over time likely reflects an increased willingness to accept older candidates, along with general population aging, and changes in the indications for transplantation, with a much larger proportion of transplants now being performed for idiopathic pulmonary fibrosis (IPF).2 Median weight, and body mass index (BMI), have both steadily increased from 75.7 kg and 25 kg/m2 respectively in the 1990s to 80 kg and 26.5 kg/m2 in the most recent era (p < 0.0001). Median recipient height has remained unchanged at 174 cm. There have been small but intriguing changes in the proportion of recipient blood type over the 3 eras, with slightly less blood type A, and slightly more blood type O. The proportion of AB and B recipients have also increased slightly. The reasons behind these trends are not known, but could for example reflect a recognition of the relative disadvantage that recipients who are blood type O, the ‘universal donor’, face with respect to organ allocation, and subsequent attempts to redress this disadvantage, or changes in proportion of patients transplanted in different regions.
Table 1.
Recipient Characteristics by Era (Transplants: January 1992 − June 2018)
| Jan 1992-Dec 2000 (n = 11,796) | Jan 2001-Dec 2009 (n = 21,806) | Jan 2010-Jun 2018 (n = 33,891) | p-value | |
|---|---|---|---|---|
| Geographic Location: | ||||
| - Europe | 3,751 (31.8%) | 7,818 (35.9%) | 12,414 (36.6%) | <0.0001 |
| - North America | 7,324 (62.1%) | 12,545 (57.5%) | 18,594 (54.9%) | <0.0001 |
| - Other | 721 (6.1%) | 1,443 (6.6%) | 2,883 (8.5%) | |
| Age (years) | 50 (23 – 63) | 54 (23 – 66) | 57 (24 – 69) | |
| Male | 51.9% | 55.6% | 58.0% | <0.0001 |
| Weight (kg) | 75.7 (53.5 – 101.6) | 78.0 (54.0 – 106.1) | 80.0 (54.4 – 108.9) | <0.0001 |
| Height (cm) | 174.0 (157.0 – 188.0) | 174.0 (157.5 – 188.0) | 174.0 (157.5 – 188.0) | 0.0463 |
| BMI (kg/m2) | 25.0 (19.1 – 32.4) | 25.7 (19.3 – 33.7) | 26.5 (19.6 – 34.6) | <0.0001 |
| BLood type: | ||||
| -A | 45.2% | 43.3% | 42.0% | <0.0001 |
| - AB | 5.2% | 5.3% | 5.8% | |
| -B | 12.2% | 13.1% | 14.1% | |
| -O | 37.4% | 38.2% | 38.1% | |
| PRA > 20% | 3.4% | 6.2% | 14.6% | <0.0001 |
| PRA > 80% | 0.4% | 0.7% | 2.0% | <0.0001 |
| CMV antibody positive | 62.9% | 59.5% | 56.2% | <0.0001 |
| EBV antibody positive | 76.7%a | 86.0% | 90.5% | <0.0001 |
| Hep B antibody positive | 2.4%b | 4.1% | 4.8% | <0.0001 |
| Hep C antibody positive | 1.7%b | 1.8% | 1.8% | 0.8656 |
| Diabetes | 6.1%b | 15.2% | 20.1% | <0.0001 |
| History of malignancy | 2.7%b | 5.2% | 7.9% | <0.0001 |
| History of smoking | - | 62.5%c | 57.9% | <0.0001 |
| Previous lung surgery | 25.7%b | 21.8% | 15.0% | <0.0001 |
| Ventilator use | 2.5% | 4.2% | 6.5% | <0.0001 |
| Hospitalized | 9.2% | 12.0% | 21.7% | <0.0001 |
| Bilirubin (mg/dl) | 0.5 (0.2 – 1.3)b | 0.5 (0.2 – 1.2) | 0.5 (0.2 – 1.2) | <0.0001 |
| Creatinine (mg/dl) | 0.9 (0.5 – 1.4)b | 0.8 (0.5 – 1.3) | 0.8 (0.5 – 1.3) | <0.0001 |
| GFR (ml/min/1.73 m2)d | 90.5 (50.8 – 154.1)b | 93.5 (53.0 – 157.5) | 97.9 (55.5 – 169.9) | <0.0001 |
| PCW mean (mm Hg) | 11.0 (4.0 – 21.0)b | 10.0 (4.0 – 22.0) | 10.0 (3.0 – 21.0) | <0.0001 |
| PA mean (mm Hg) | 25.0 (15.0 – 54.0)b | 25.0 (14.0 – 49.0) | 25.0 (14.0 – 49.0) | 0.0095 |
| PVR (Wood units) | 2.7 (1.0 – 7.6)b | 2.7 (1.0 – 7.3) | 2.8 (1.1 – 7.9) | <0.0001 |
| FEV1% predicted | 23.0 (12.0 – 78.0) | 29.0 (13.0 – 77.0) | 35.0 (14.0 – 78.0) | <0.0001 |
| FVC% predicted | 48.0 (24.0 – 86.0) | 47.0 (25.0 – 82.0) | 46.0 (25.0 – 82.0) | <0.0001 |
BMI, body mass index; CVA, cerebrovascular accident; CMV, cytomegalovirus; EBV, Epstein Barr virus; GFR, glomerular filtration rate. Summary statistics excluded transplants with missing data
Continuous factors are expressed as median (5th − 95th percentiles)
Comparisons for categorical variables were made using the chi-square statistic
Comparisons for continuous variables were made using the Wilcoxon test
Based on October 1999− December 2000 transplants
Based on April 1994 − December 2000 transplants
Based on July 2004 − December 2009 transplants
GFR was estimated using the Cockcroft-Gault formula
The proportion of recipients who are sensitized has steadily increased over time. For instance, candidates with panel of reactive antibodies (PRA) ≥20% increased from 3.4% between January 1992 and December 2000 to 6.2% between January 2001 and December 2009 and then finally to 14.6% in the most recent era (p < 0.0001). These changes may reflect an acceptance for increased immunologic risk amongst transplant centers. The proportion who are cytomegalovirus (CMV) antibody positive has decreased over time from 62.9% to 56.2% in the most recent era (p < 0.0001). This change has occurred despite a steadily aging recipient population, and thus may reflect changes of CMV seroprevalence over time reported in some countries. Importantly, the increasing number of CMV negative recipients will need to be monitored closely going forward, since there is a significant survival disadvantage among CMV mismatched (negative recipient, positive donor) transplants.1–3 In contrast, the proportion of recipients who are Epstein-Barr virus antibody positive has steadily increased from 77% to just over 90%. A small but increasing number of recipients are hepatitis B antibody positive (4.8% in the most recent era), while the proportion of recipients who are hepatitis C antibody seropositive has remained static over time at 1.8%.
The proportion of recipients with a history of diabetes mellitus has almost tripled from 6.1% in the 1990s to 20.1% in the most recent era (p < 0.0001), while the proportion with a history of malignancy has also increased from 2.7% to 7.9% (p < 0.0001). The prevalence of a history of smoking has declined from 62.5% in the 2000s to 57.9% in the most recent era (p < 0.0001). While a history of lung surgery has become less common, the proportion of lung transplant recipients with a history of ventilator use or current hospitalization has increased over the past 3 decades, suggesting that the acuity of lung transplantation is increasing over time.
Changes in recipient diagnosis by geographic region are presented in Figure 1 (eSlide L[a] 8). While the indications for transplantation have remained relatively static in Europe, there have been an increasing number of transplants performed for IPF in North America and elsewhere in the world. These changes likely explain the changes in spirometric parameters seen over the last 3 decades (Table 1), with increasing FEV1% and reducing FVC% predicted amongst lung transplant recipients, as more recipients with restrictive rather than obstructive lung disease are transplanted. The changes in median recipient age, BMI, and glomerular filtration rate (estimated using the Cockcroft-Gault formula, eGFR) by geographic region are presented in Figure 2 (eSlide L[a] 10), and confirm a steady rise in age and BMI over time. There has also been a slight increase in eGFR comparing the earliest to most recent eras, possibly related to increasing weight since this variable is included in the calculation of eGFR. The rates of change in recipient history of malignancy, diabetes, and smoking (>20 pack-years) are shown in Figure 3 (eSlide L [a] 11).
Figure 1.
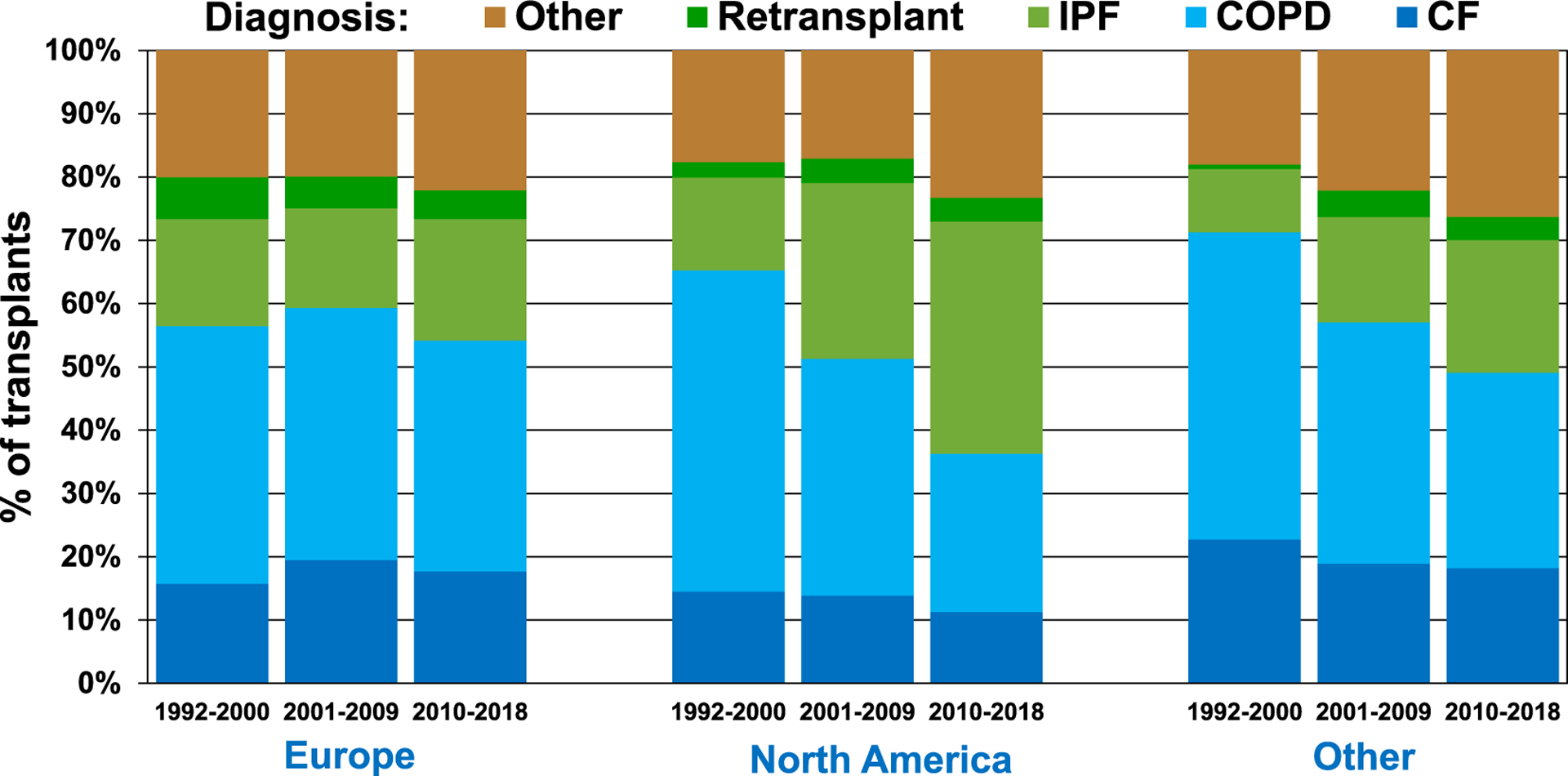
Recipient diagnosis by location and era (transplants: January 1992-June 2018).
Figure 2.
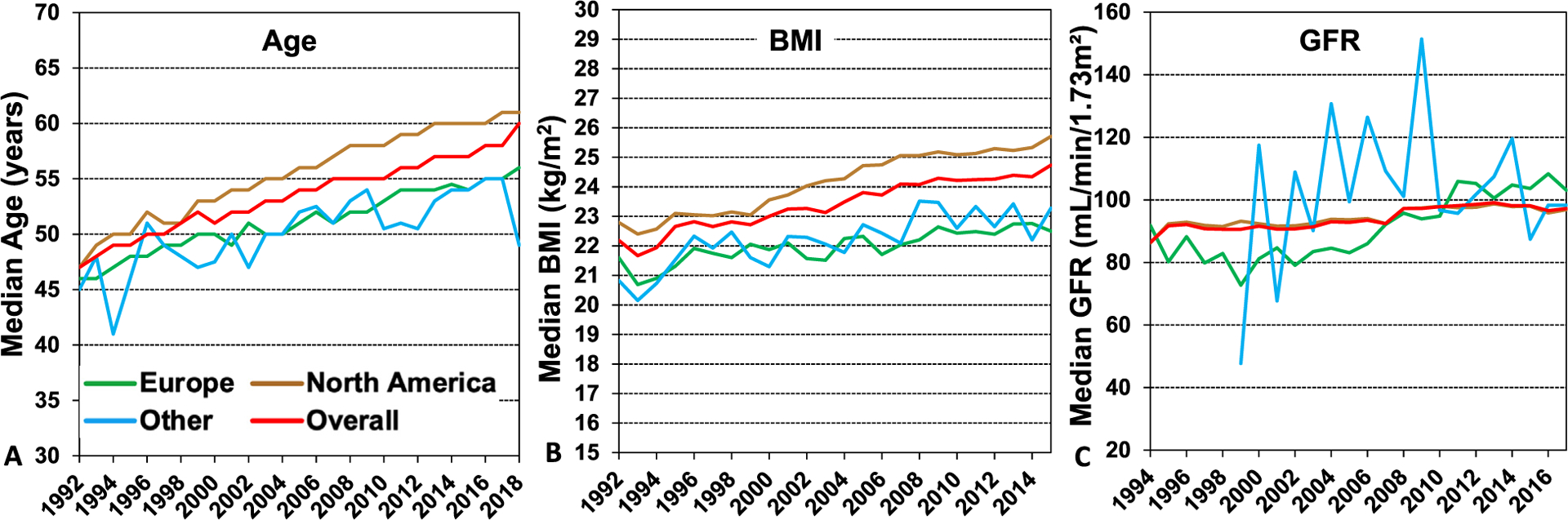
Median recipient (A) age (transplant: January 1992 − June 2018), (B) body mass index (transplant: January 1992-June 2018), and (C) glomerular filtration rate (GFR) (transplants: January 1994-June 2018), by year, and region. GFR was estimated using the Cockcroft-Gault formula.
Figure 3.
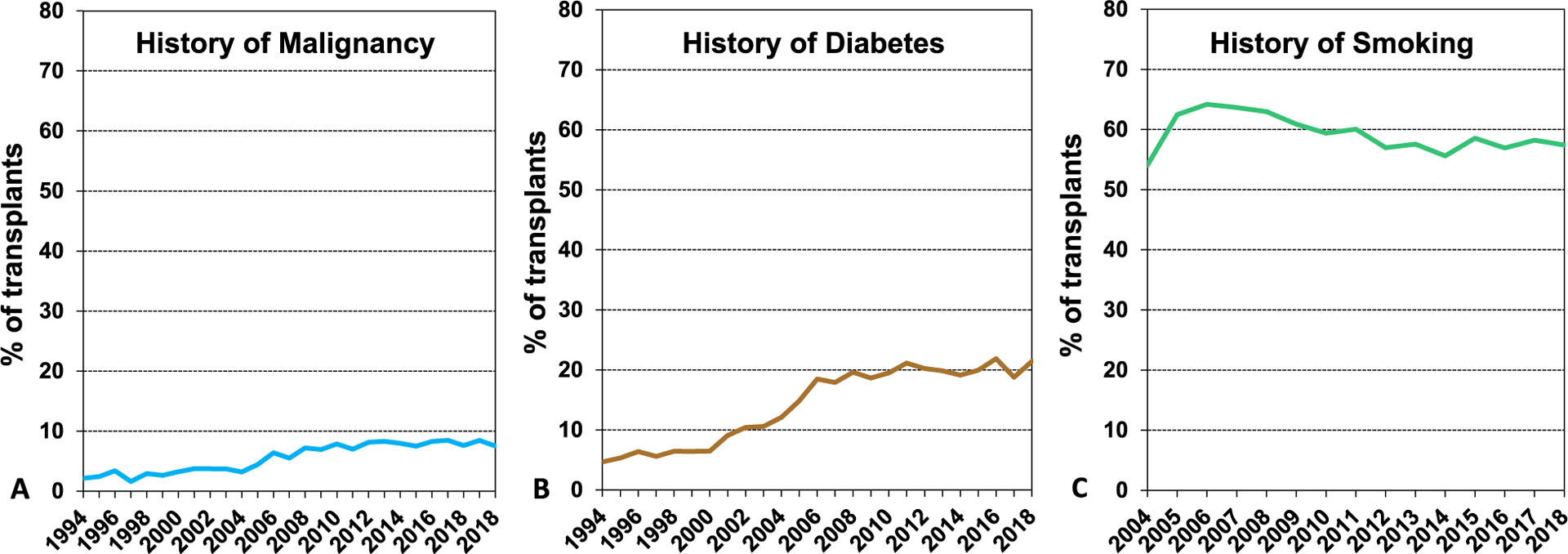
Recipient history of (A) malignancy (transplants: January 1994-June 2018), (B) diabetes (transplants: January 1994-June 2018), (C) smoking* (transplants: January 2004-June 2018). *Cigarette use for more than 20 pack years.
Survival analyses
We next examined associations between recipient risk factors and post-transplant survival. We first present a number of stratified unadjusted analyses. It should be kept in mind that these analyses have not been adjusted for potential confounders that may account for some of the reported differences. It is also important to remember that multivariable analyses, when performed, necessarily only contain variables that are reported to the Registry, so that some potential explanatory variables (e.g., a history of primary graft dysfunction, which is not recorded in the Registry) will not appear in the multivariable models. All 5-year survival analyses are conditional on survival to 1 year. Since the impact of donor related factors was the focus of the 2020 Report14 this has only received limited attention in this report.
One-year survival
We examined associations between recipient risk factors and post-transplant survival. Overall 12-month survival by era is presented in Figure 4A (eSlide L[a] 13). Survival in adults who underwent lung transplantation from January 2000 to June 2017 improved significantly over time, confirming a previously noted trend towards improved survival in recent eras.1–3 Figure 5 (eSlide L[a] 14) displays Kaplan-Meier survival within 12 months for adult lung transplant recipients by location and era. There is significant improvement in survival for the most recent eras in North America and Europe, but not elsewhere in the world. This may reflect the commencement of transplantation as a low volume procedure2 at centers reporting from outside North America and Europe or could be related to low statistical power.
Figure 4.
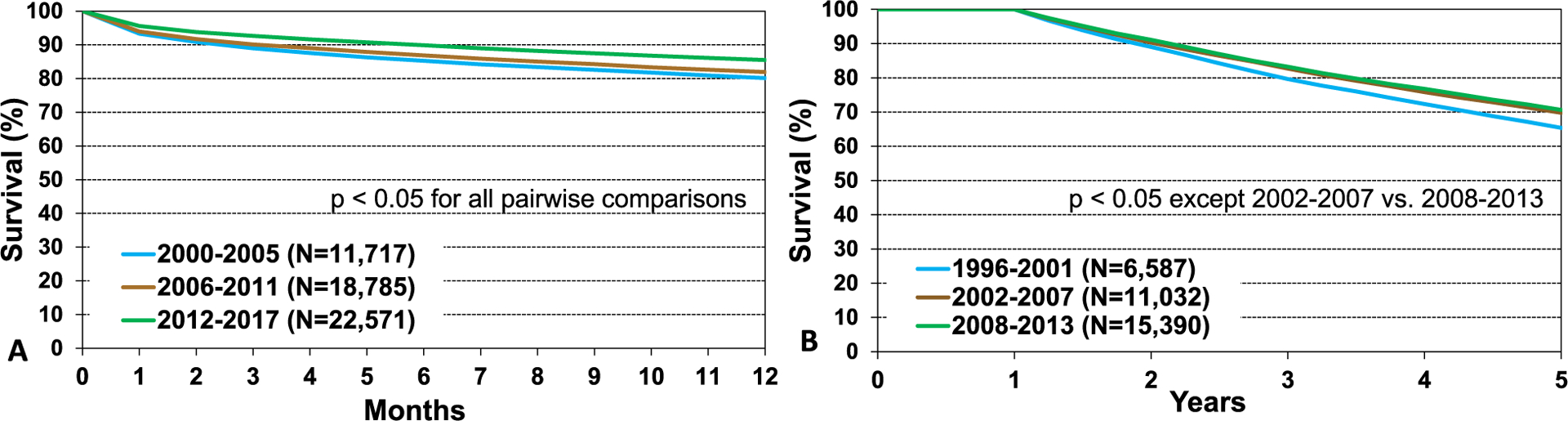
Kaplan-Meier survival within (A) 12 months (transplants: January 2000-June 2017), and (B) 5 years conditional on survival to 1 year (transplants: January 1996-June 2013), by transplant era.
Figure 5.
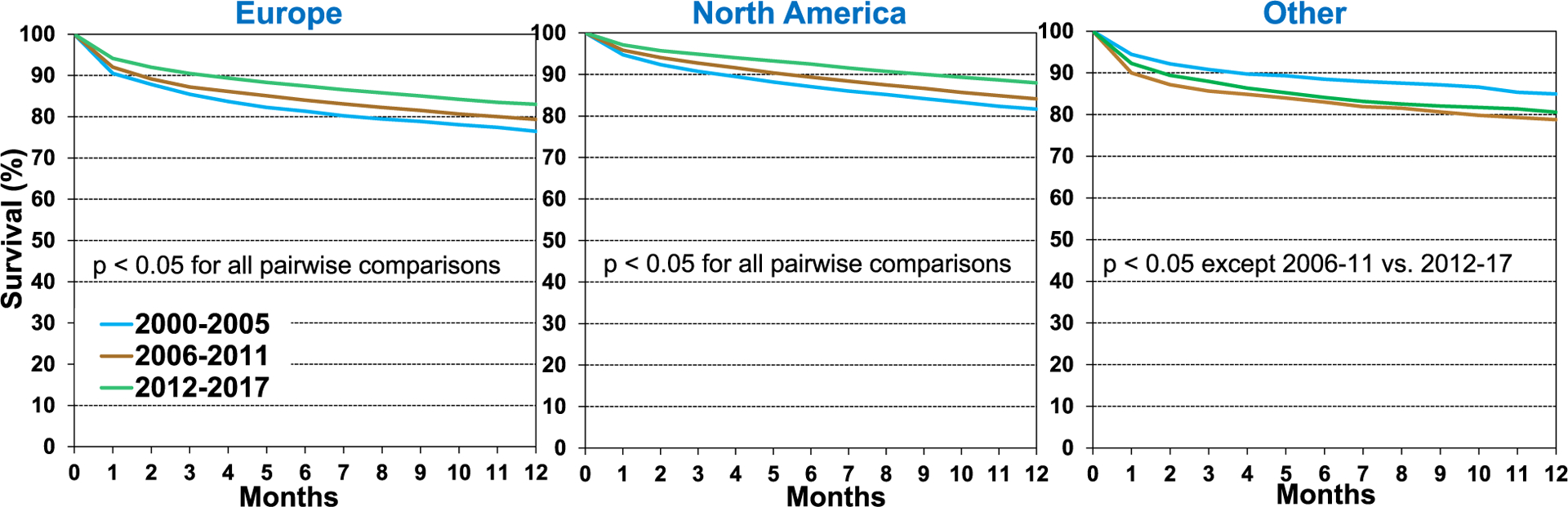
Kaplan-Meier survival within 12 months for adult lung transplant recipients by location and era (transplants: January 2000-June 2017).
Twelve-month survival improved in all recipient age groups over time as seen in unadjusted Kaplan-Meier analyses (Figure 6, eSlide L[a] 16). Previous reports have observed that dialysis-dependent renal failure has a significant impact on 1- and 5-year survival after lung transplantation.1,2 For this year’s analysis, eGFR was quantified using the Cockroft-Gault equation to estimate renal reserve in adult lung transplant candidates. Interestingly we only saw slight differences in overall survival to 12 months when recipients were stratified by eGFR, with survival improving by era for all strata (Figure 7, eSlide L[a] 19). However, there was an independent association between eGFR, and survival when eGFR was included as a continuous variable in the multivariable models (see below).
Figure 6.
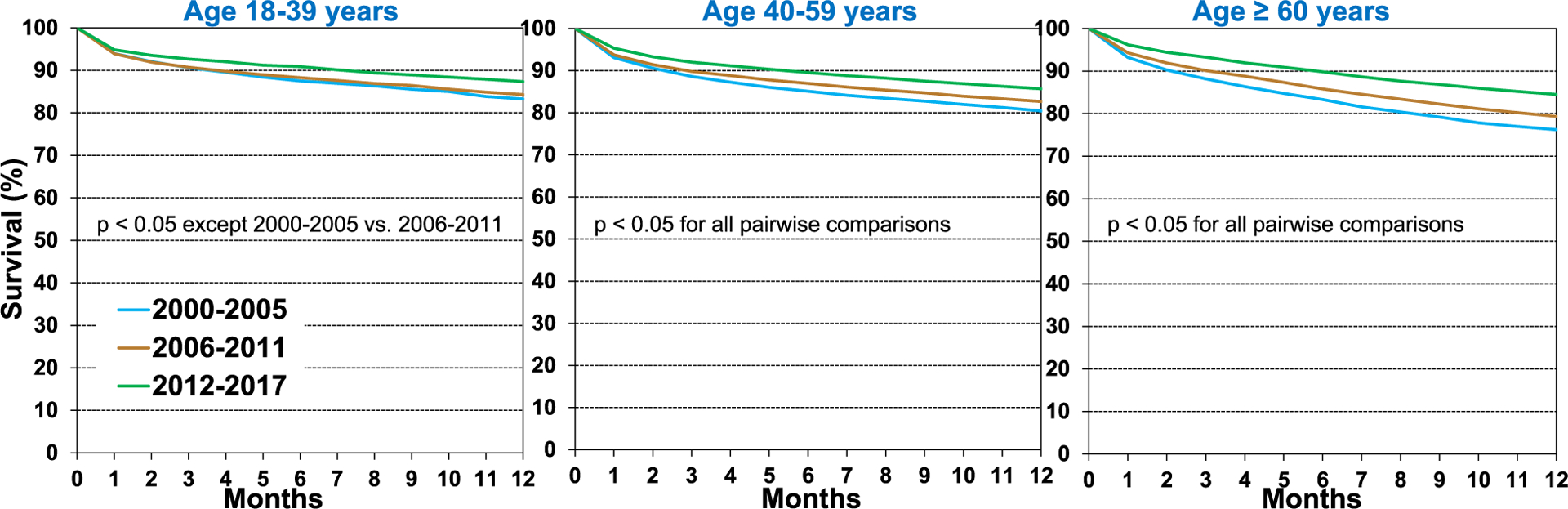
Kaplan-Meier survival within 12 months for adult lung transplant recipients by recipient age and era (transplants: January 2000-June 2017).
Figure 7.
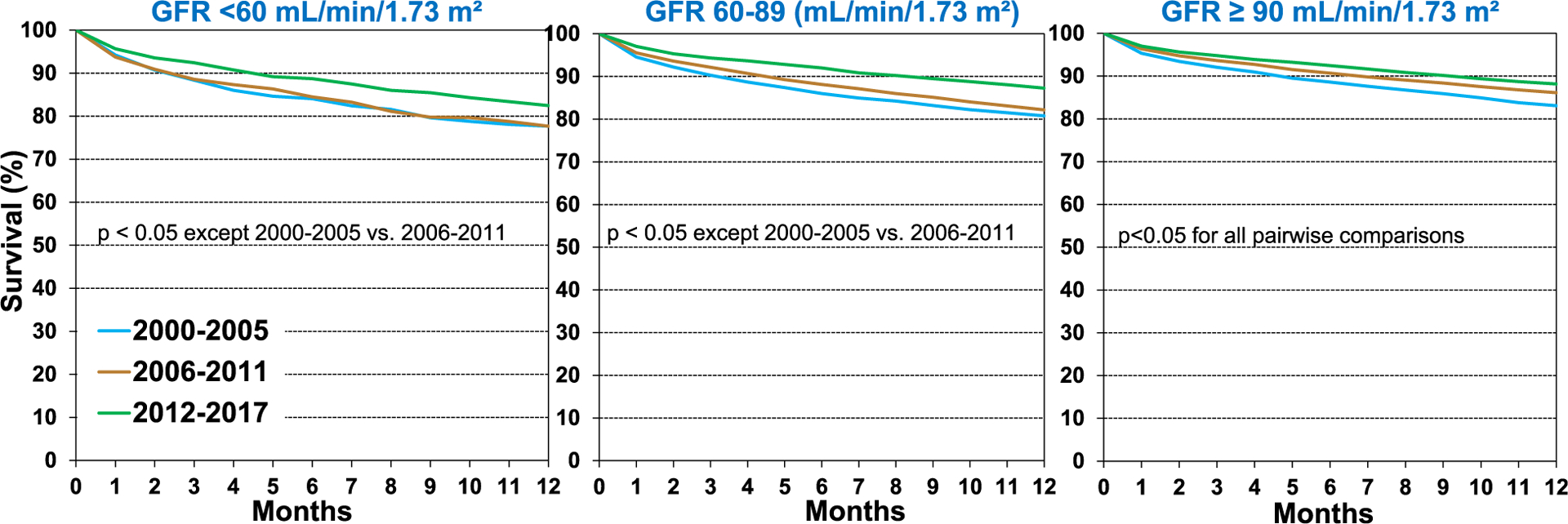
Kaplan-Meier survival within 12 months for adult lung transplant recipients by recipient glomerular filtration rate (GFR) and era (transplants: January 2000-June 2017). GFR was estimated using the Cockcroft-Gault formula.
Five-year survival conditional on surviving to 1 year
We next examined 5-year survival conditional on 1-year survival in adult lung transplant recipients over time from January 1996 to June 2013. Survival improved significantly from the early era of 1996 to 2001 but was unchanged for the latter 2 eras (Figure 4B, eSlide L[a] 24). When stratifying by age, 5-year conditional survival for patients transplanted in the most recent era was lower in recipients above 60 years of age at 62%, compared to 75% in younger recipients. However, there was a significant improvement in survival in all ages from the earliest (1996–2001) to the middle era (2002–2007). Improvements in survival for older adult lung transplant recipients appear to have plateaued in the most recent era, with only the 40 to 59 age group experiencing a further improvement in survival (Figure 8, eSlide L[a] 27).
Figure 8.
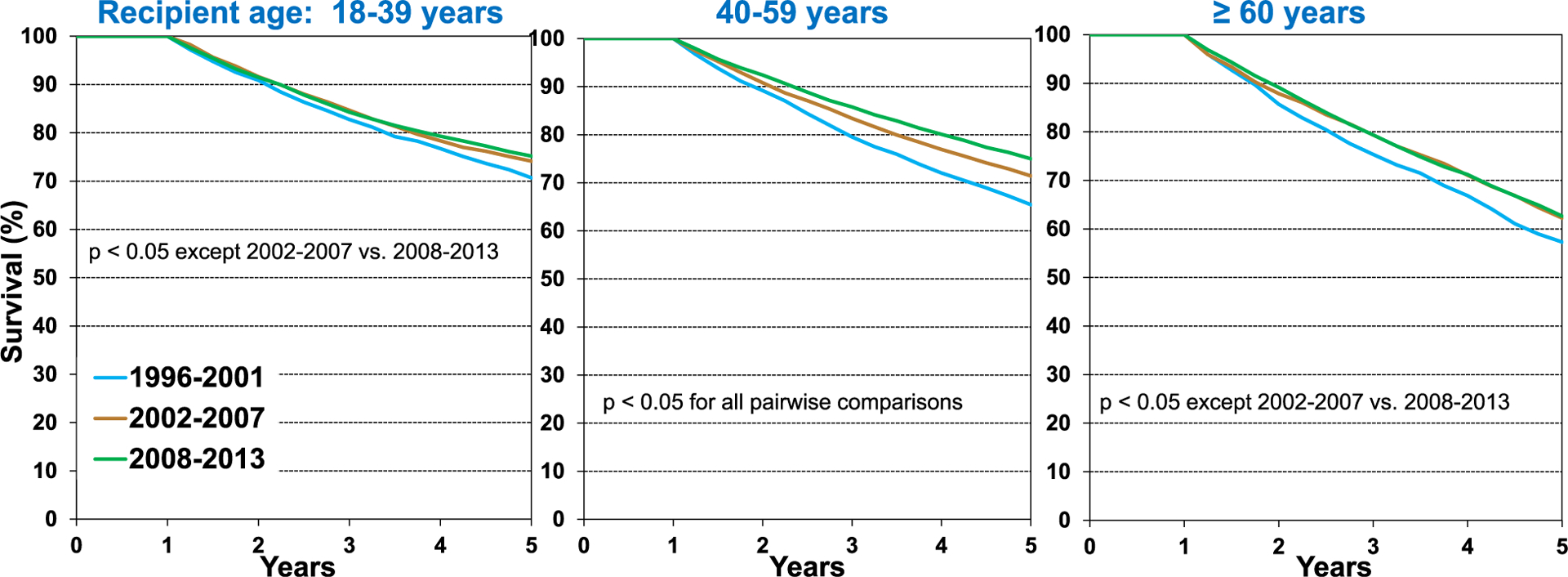
Kaplan-Meier survival within 5 years conditional on survival to 1 year, for adult lung transplant recipients by recipient age, and era (transplants: January 1996-June 2013).
Malignancies are common after lung transplantation and are a common cause of death. It would therefore be reasonable to assume that previous malignant disease in the recipient would also impact survival. However, this was not the case when stratifying recipients by history of malignancy, as there were no significant differences in 5-year conditional survival by history of malignancy (Figure 9, eSlide L[a] 32).
Figure 9.
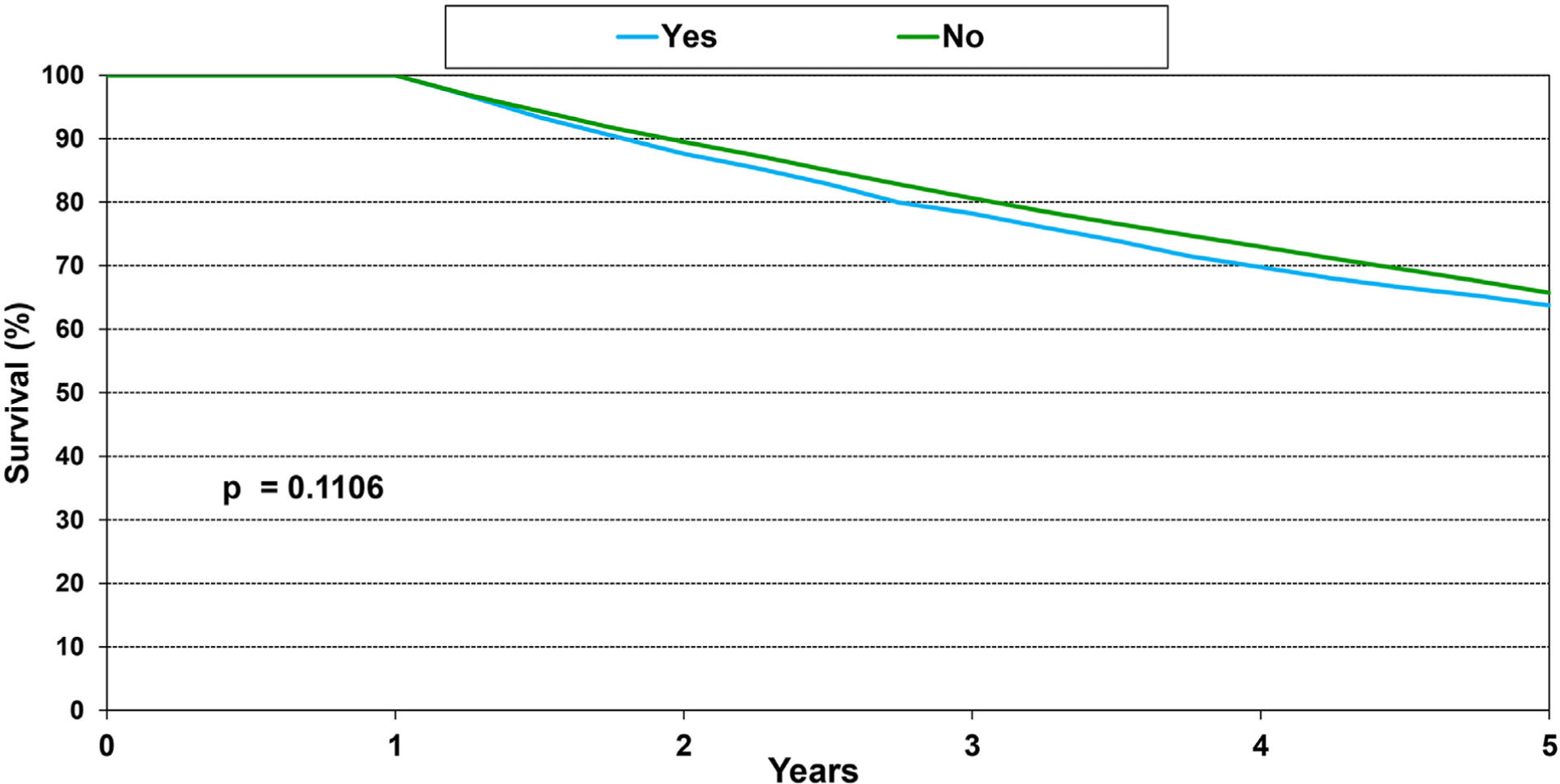
Kaplan-Meier survival within 5 years conditional on survival to 1 year, for adult lung transplant recipients by history of malignancy (transplants: January 1996-June 2013).
Freedom from bronchiolitis obliterans syndrome (BOS) conditional on survival to discharge
Bronchiolitis obliterans syndrome (BOS) continues to be a major cause of morbidity and mortality after lung transplantation. We studied freedom from BOS in adult lung transplant recipients who survived the transplant hospitalization. Overall, there was higher freedom from BOS at 5 years (57%) in the early 1996 to 2001 period compared with the 2 later time periods 2002 to 2007 (49%) and 2008 to 2013 (47%) (Figure 10, eSlide L[a] 35). Although risk factors for BOS have been extensively investigated2,15 the possibility of an era effect has not previously been explored, to our knowledge. This is an interesting finding which is concerning if explanations such as reporting, changes in diagnostic criteria over time and other biases are not responsible. Again, it should be kept in mind that these univariate analyses have not been adjusted for potential confounders that may account for some of the reported differences.
Figure 10.
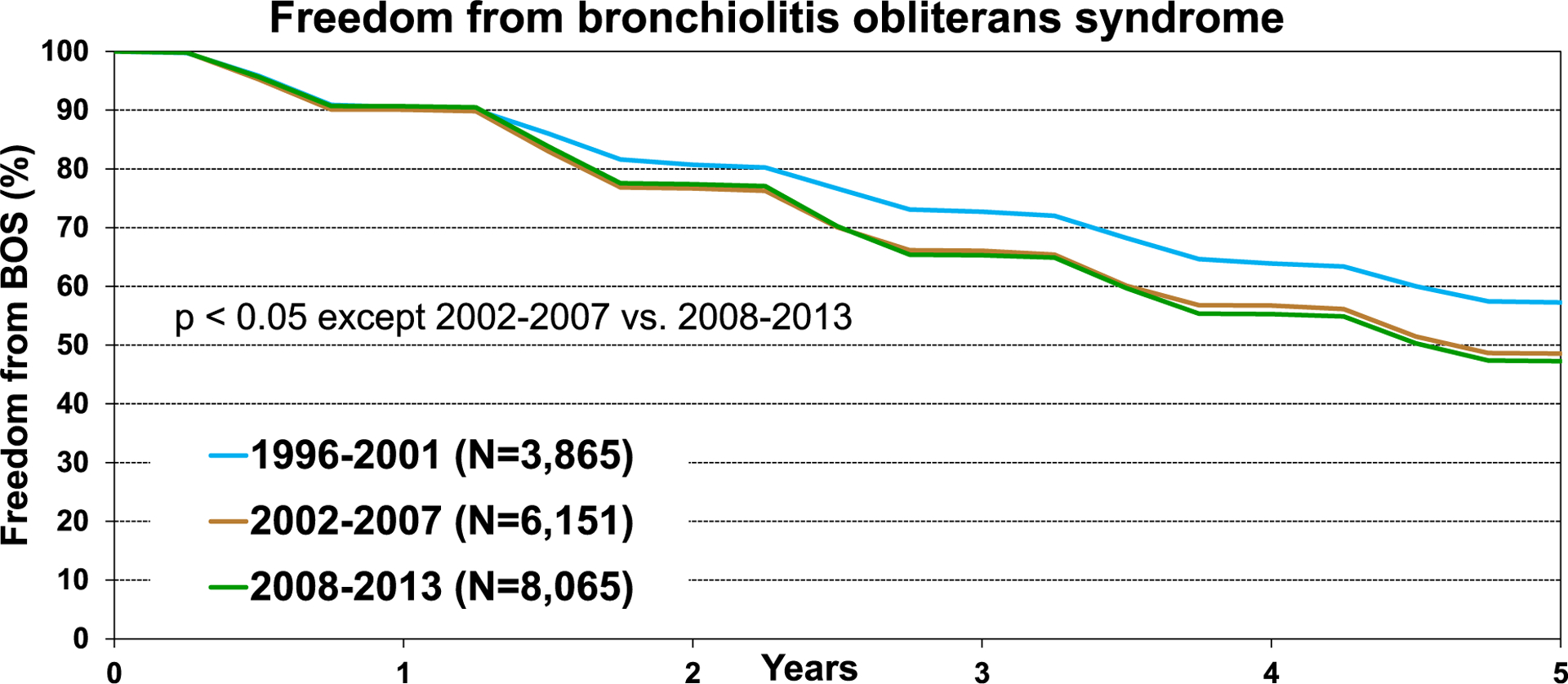
Kaplan-Meier freedom from bronchiolitis obliterans syndrome (BOS) conditional on survival to discharge, for adult lung transplant recipients by era (transplants: January 1996-June 2013).
Multivariable analyses
We next performed multivariable Cox regression analyses to evaluate risk factors for 1-year mortality, 5-year mortality conditional upon surviving the first post-transplant year, and risk of developing BOS conditional upon surviving to hospital discharge. Covariates included in the multivariable models are listed in Supplemental Table 1.
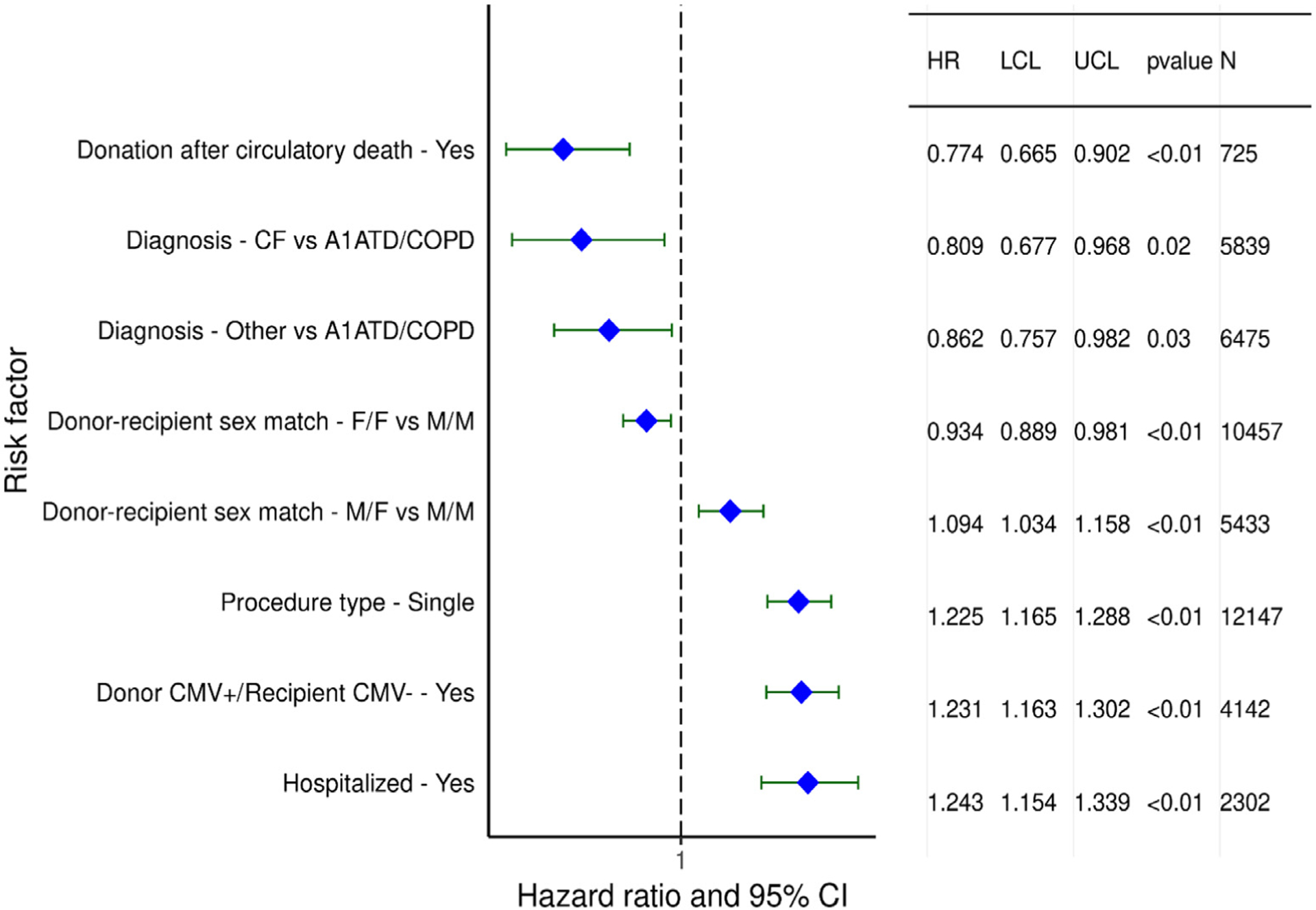
One-year mortality
Categorical variables independently associated with risk of higher 1-year mortality in adult lung transplant recipients between January 2000 and June 2017 include donor/recipient sex mismatch, donor/recipient CMV antibody mismatch, prior lung surgery, being hospitalized, and being on mechanical ventilation at time of transplant. Having a single lung transplant vs a double lung transplant was also associated with higher risk for 1-year mortality. A diagnosis of IPF or ‘Other’ as the indication for transplantation, and especially re-transplantation, was also associated with increased risk compared to a diagnosis of chronic obstructive pulmonary disease (Figure 11, eSlide L[a] 42). To further explore how the risk associated with the diagnosis leading to transplantation may have changed across eras, the transplant era, and diagnosis interaction was investigated. The interaction between these variables was significant for 1-year mortality, suggesting a consistent decrease in the mortality risk across the different indications and transplant eras (Figure 12A, eSlide L[a] 43), with the decline in the hazard of mortality being larger for those with a diagnosis of cystic fibrosis and less in retransplants.
Figure 11.
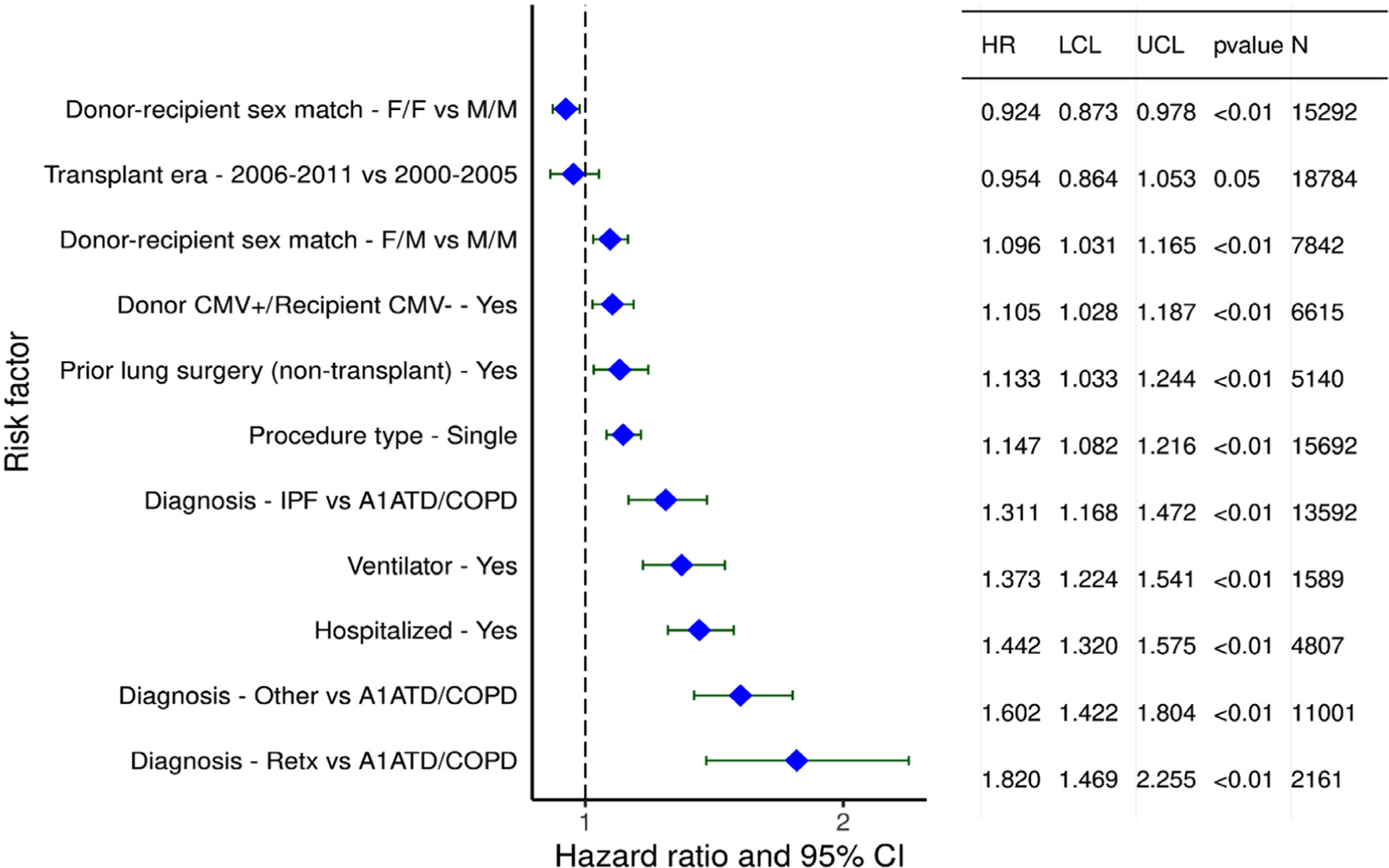
Statistically significant categorical risk factors for 1-year mortality for adult lung transplant recipients with 95% confidence limits (transplants: January 2000-June 2017, n = 53,072).
Figure 12.
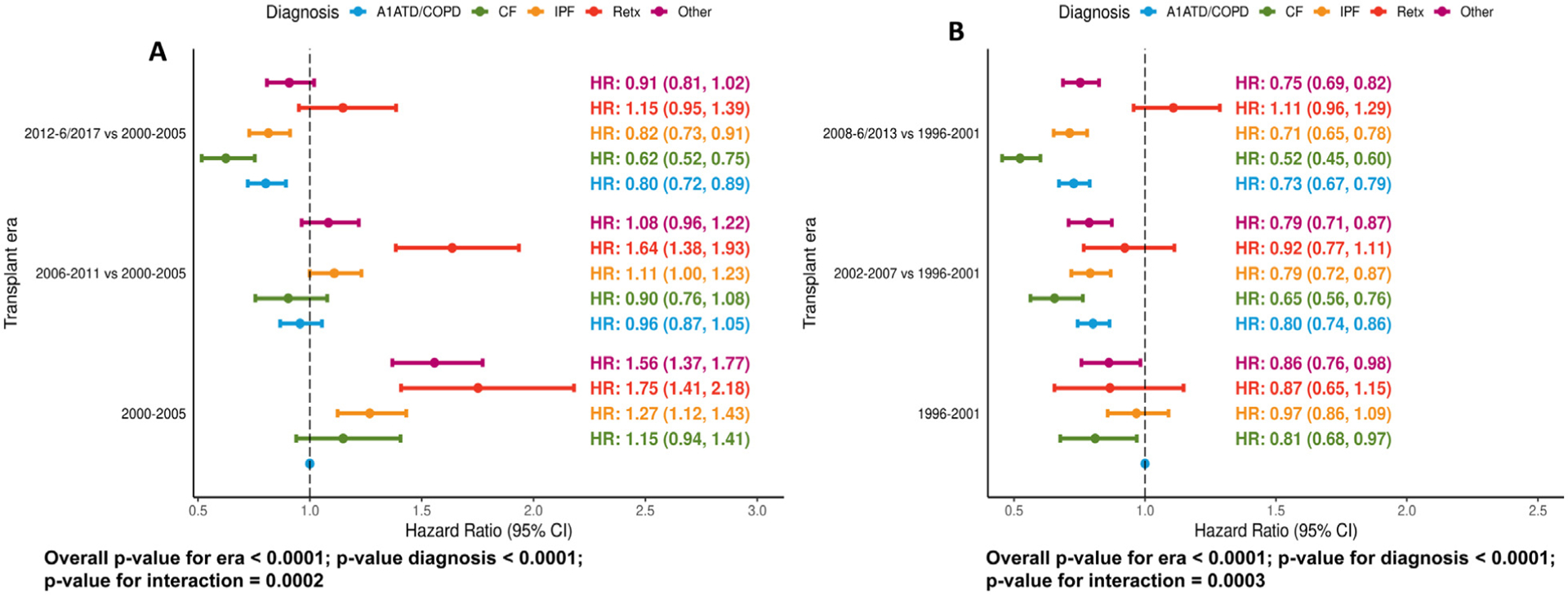
Statistically significant categorical risk factors with 95% confidence limits for (A) 1-year mortality (transplants: January 2000-June 2017, n = 53,072) and (B) 5-year mortality (transplants: January 1996-June 2013, (n = 35,214). Transplant era and diagnosis interaction.
Continuous variables associated with increased risk of 1-year mortality were examined in the same population. The hazard ratio increased significantly for older recipients (Figure 13A, eSlide L[a] 46), and there was a significant interaction between transplant era and recipient age, suggesting that some age groups saw larger improvements in survival than others (Figure 13B, eSlide L[a] 47). Higher recipient BMI (Figure 14A, eSlide L[a] 49), lower recipient eGFR (Figure 14B, eSlide L[a] 50), higher recipient bilirubin (Figure 14C, L[a] eSlide 52), older donor age (Figure 14D, L [a] eSlide 53), and lower center volume (number of transplant procedures performed in the previous 3 years, Figure 15B, L [a] eSlide 55) were all significantly and independently associated with 1-year mortality. Ischemic time was also associated with 1-year mortality, with increased risk of mortality observed with longer ischemic times (Figure 15A, eSlide L[a] 54). The impact of ischemic time on lung transplant outcomes was reviewed in depth in the 2017 report.3
Figure 13.
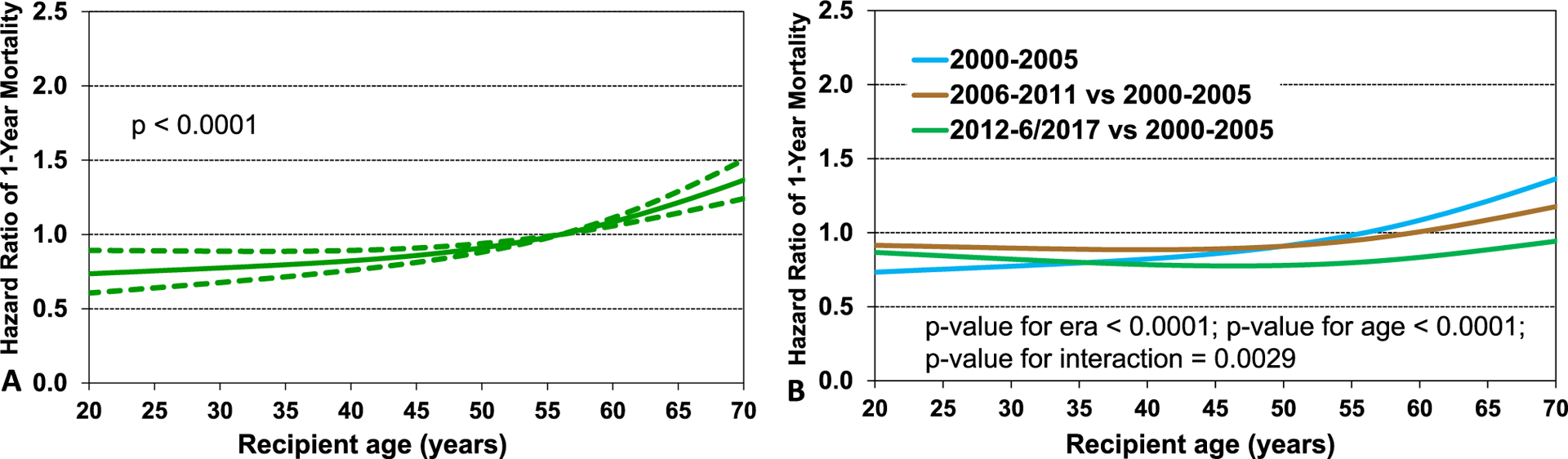
(A) Hazard ratio of 1-year mortality for adult lung transplant recipients by recipient age. The reference value for age is 56 years. (B) Transplant era and recipient age interaction (transplants: January 2000-June 2017, n = 53,072).
Figure 14.
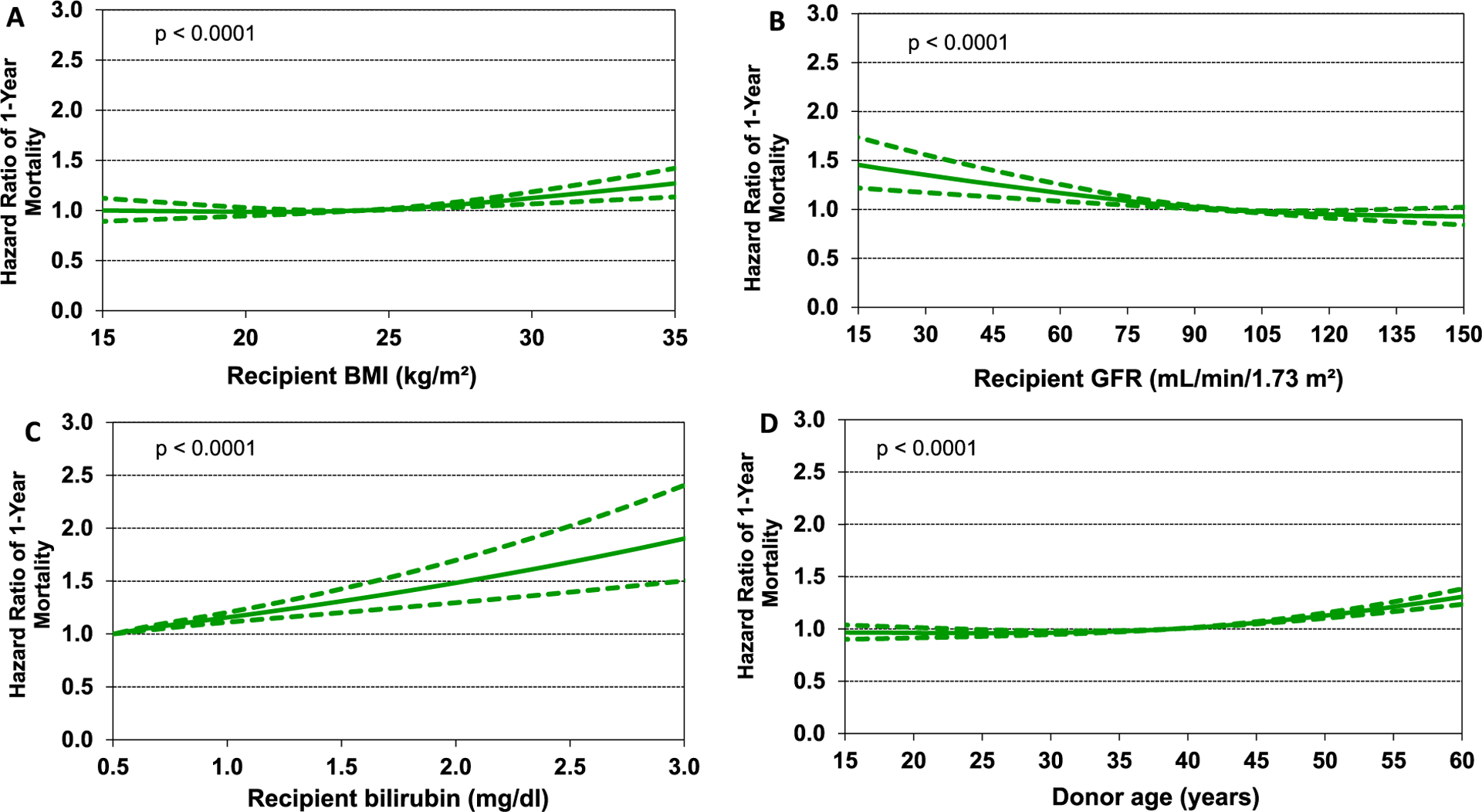
Hazard ratio of 1-year mortality for adult lung transplant recipients by (A) recipient body mass index (BMI), (B) recipient glomerular filtration rate (eGFR), (C) recipient bilirubin, and (D) donor age (transplants: January 2000-June 2017, n = 53,072). GFR was estimated using the Cockcroft-Gault formula. The reference value for BMI was 24, for eGFR was 95, for bilirubin was 0.5, and for donor age was 39.
Figure 15.
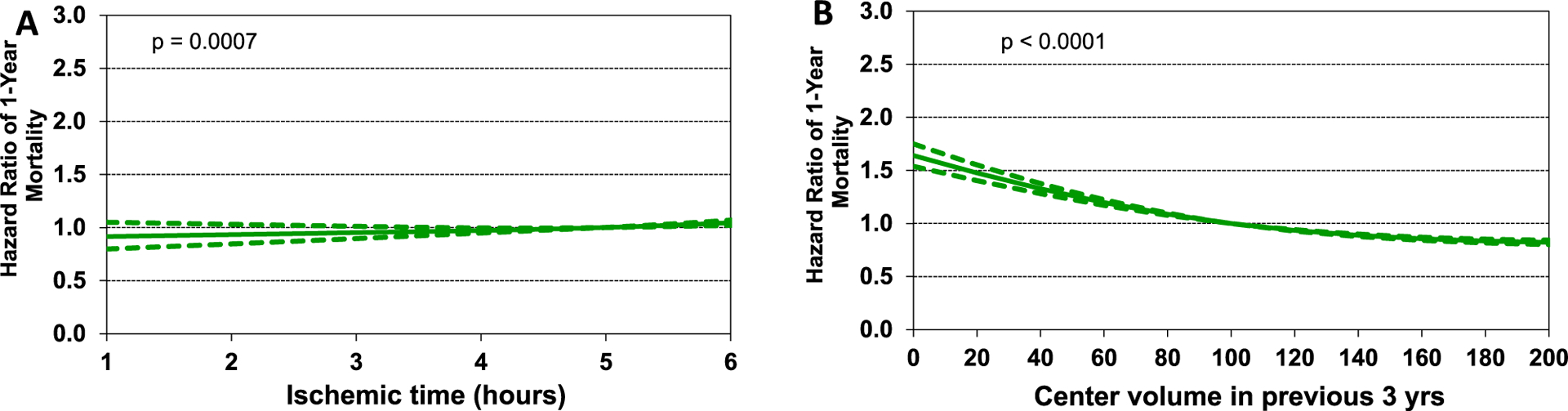
Hazard ratio of 1-year mortality for adult lung transplant recipients by (A) ischemic time and (B) center volume in the previous 3 years (transplants: January 2000-June 2017, n = 53,072). The reference value for ischemic time was 5 and for center volume was 100.
Five-year mortality conditional upon surviving the first post-transplant year
Statistically significant categorical risk factors for 5-year mortality, conditional on survival to 1 year, from the period of January 1996 to June 2013 are shown in Figure 16 (eSlide L[a] 57). The following factors were independently associated with lower risk of 5-year mortality: transplantation with organs acquired from a donor after a circulatory death and diagnosis of cystic fibrosis and ‘other’. In contrast the following variables were independently associated with higher risk of 5-year mortality: male-to-female transplant vs male-to-male transplant, male-to-male transplant vs female-to female transplant, single lung transplant, CMV mismatch and hospitalization at time of transplant.
Figure 16.
Statistically significant categorical risk factors for 5-year mortality conditional on survival to 1 year with 95% confidence limits (transplants: January 1996-June 2013, n = 35,214).
With respect to continuous variables leading to increased risk for 5-year mortality conditional on 1-year survival, recipient age was independently associated with mortality, with the hazard ratio increased for both younger and older recipients (Figure 17A, eSlide L[a] 61). Other continuous variables associated with increased risk of 5-year mortality were similar to those associated with 1-year mortality including increasing BMI (Figure 17B,eSlide L[a] 63), decreasing eGFR (Figure 17C, eSlide L[a] 64) and, perhaps counterintuitively, shorter ischemic time (Figure 18A, eSlide L[a] 66), as previously described.3 Finally, the relationship between center volume, and 5-year mortality was significant, even though the hazard differences were quite small (Figure 18B, eSlide L[a] 67).
Figure 17.
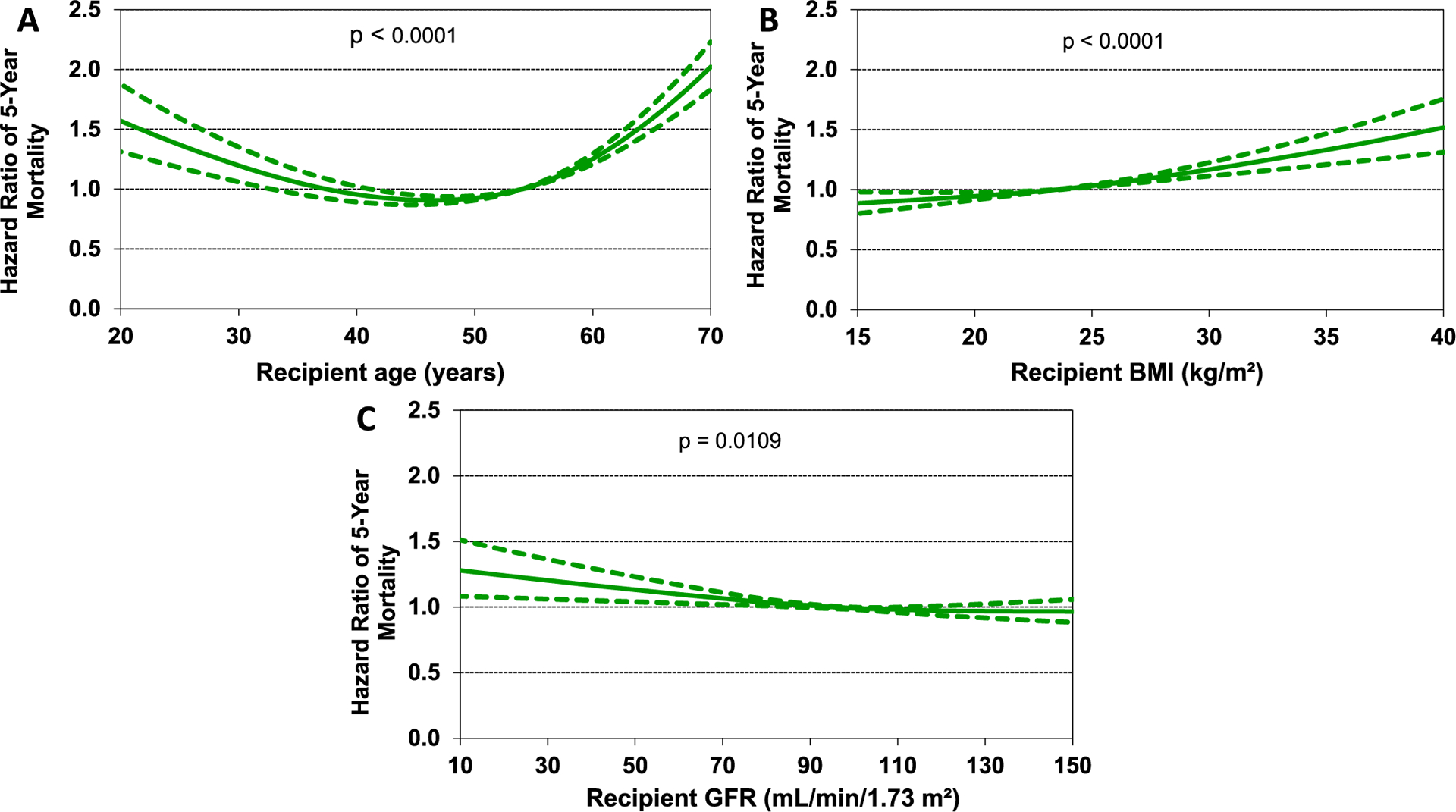
Hazard ratio of 5-year mortality for adult lung transplant recipients by (A) recipient age, (B) recipient body mass index (BMI), and (C) recipient glomerular filtration rate (GFR) (transplants: January 1996-June 2013, n = 35,214). GFR was estimated using the Cockcroft-Gault formula. The reference value for age was 54, for BMI was 23.5, and for GFR was 94.
Figure 18.
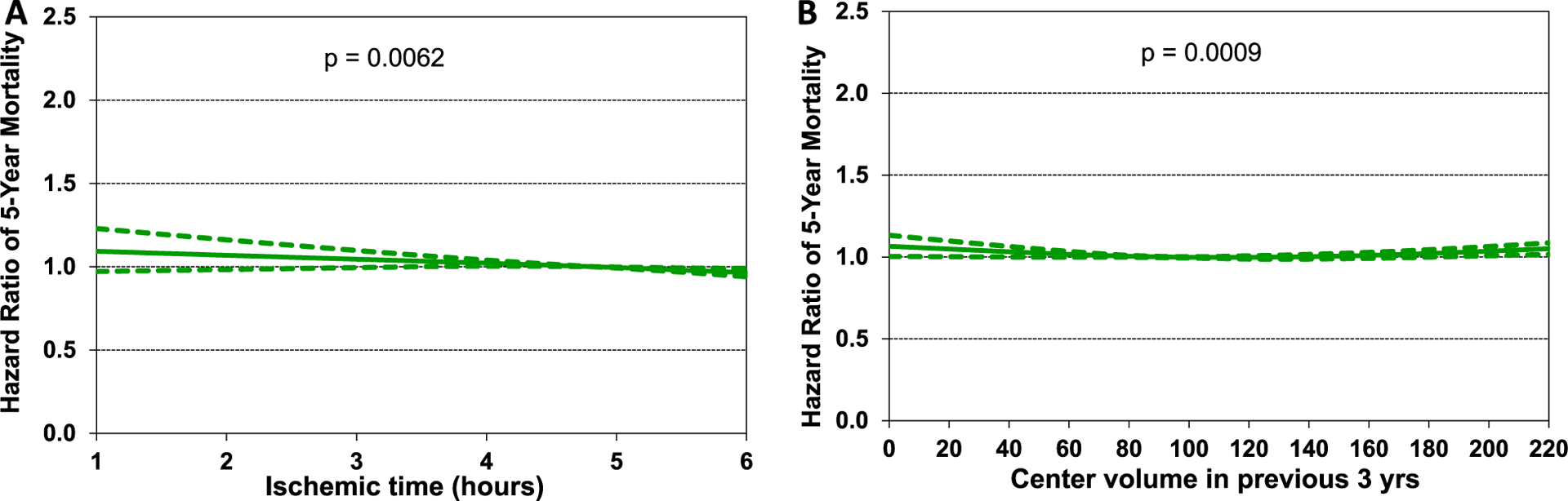
Hazard ratio of 5-year mortality for adult lung transplant recipients by (A) ischemic time and (B) center volume in the previous 3 years (transplants: January 1996-June 2013, n = 35,214). The reference value for ischemic time was 4.8 and for center volume was 91.
Freedom from bronchiolitis obliterans syndrome (BOS) conditional on survival to discharge
We next investigated continuous variables significantly associated with developing BOS during the first 5 years after transplant in recipients who survived to hospital discharge from January 1996 to June 2013. Many of the significant associations were similar to the risk factors for both 1- and 5-year survival, but there were some unique risk factors for BOS identified. Younger recipient age was independently associated with BOS risk (Figure 19A, eSlide L[a] 73), possibly due to a heightened immunologic response, or an increased prevalence of non−adherence observed in adolescents and young adults.16 Interestingly, lower BMI was associated with lower risk of BOS (Figure 19B, eSlide L[a] 76). Similar to 1-year mortality, increasing bilirubin and increasing donor age were both associated with increased risk of developing BOS (Figure 19C and 19D, eSlides L[a] 78,79). In contrast to the impact on 1-year survival, longer ischemic time was associated with slightly reduced risk of BOS, as previously noted (Figure 20A, eSlide L[a] 80).3 The association between center volume and risk of BOS was complex, suggesting lower risk of BOS in both low and high-volume centers. (Figure 20B, eSlide L[a] 81). Multiple reasons for these associations are possible, including reporting bias (not all centers report BOS to the Registry), as well as factors that are difficult to quantitate such as clinician experience, caseload, and protocols for follow-up.
Figure 19.
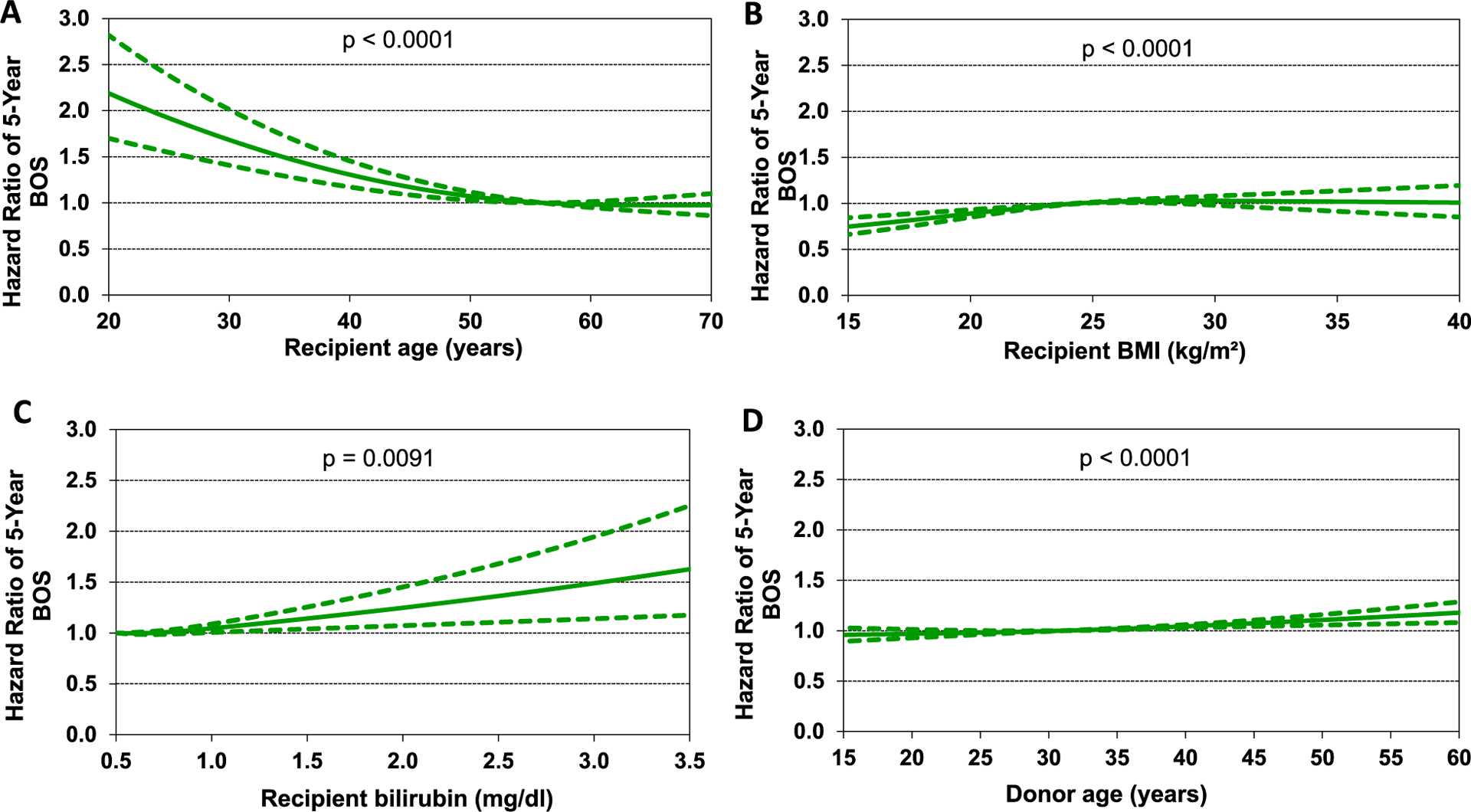
Hazard ratio of bronchiolitis obliterans syndrome (BOS) within 5-years for adult lung transplant recipients by (A) recipient age, (B) recipient body mass index (BMI), (C) recipient bilirubin, and (D) donor age (transplants: January 1996-June 2013, n = 18,830). The reference value for age was 56, for BMI was 24, for bilirubin was 0.5, and for donor age was 31.
Figure 20.
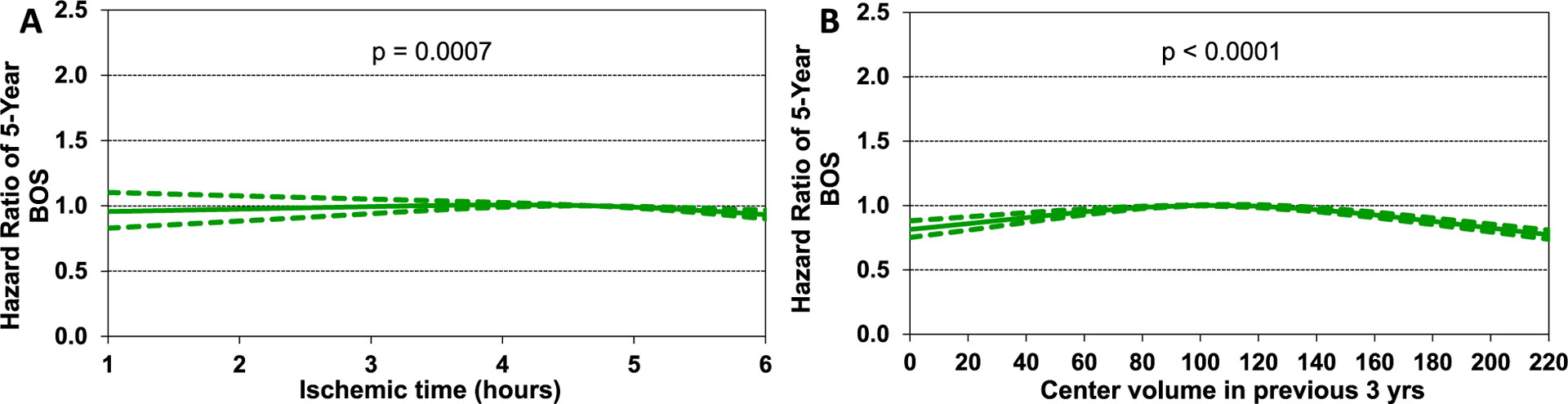
Hazard ratio of bronchiolitis obliterans syndrome (BOS) within 5-years for adult lung transplant recipients by (A) ischemic time and (B) center volume in the previous 3 years (transplants: January 1996-June 2013, n = 18,830). The reference value for ischemic time was 4.7 and for center volume was 94.
Conclusions
In this 2021 ISHLT TTX Registry Report, we focused on recipient trends over time. We observed many important changes over the years, reflecting changing practice, and demographics worldwide. Lung transplant recipients are ageing, are more likely to be transplanted for fibrosing lung disease, have an increasing BMI, are much more likely to have a history of diabetes mellitus, are more likely to be sensitized, less likely to be CMV seropositive, and more likely to have a history of malignancy. For the first time, in this report we present data on the impact of recipient eGFR (rather than serum creatinine), and interactions between important recipient factors such as age, diagnosis, and transplant era on post-transplant mortality. In univariable and multivariable analyses, we identified significant associations between recipient factors and transplant outcomes including mortality and BOS. Some of the more notable findings were the associations between freedom from BOS and transplant era, BMI, center volume, and ischemic time. We hope that providing a historical perspective on the practice of transplantation will highlight important trends and stimulate interest in the development of protocols, procedures, and further studies that may improve transplant outcomes in the years to come.
Disclosure statement
Daniel C. Chambers received travel support from Astellas Pharma, Inc, and served as a consultant and speaker for Roche Ltd; Kiran K. Khush serves as a consultant and speaker for CareDx, Inc; Josef Stehlik serves as a consultant for Medtronic, receives research funding from Natera and receives funding from ISHLT; Michael Perch receives research funding from Roche, travel support from Boer-inger-Ingelheim, and is a speaker for Mallinckrodt, Glaxo Smith Kline, and Astra-Zeneca; Wida S. Cherikh, Aparna Sadavarte, and Kelsi Lindblad received funding from ISHLT; Don Hayes, Jr; Michael O. Harhay; Aparna Sadavarte; Eileen Hsich; Luciano Potena; and Tajinder P. Singh do not have any relevant disclosures.
Supplementary Material
Acknowledgments
The authors wish to thank Ms. Lyna Cherikh, United Network of Organ Sharing Research Summer Intern, for her assistance with preparing the figures/table for the manuscript, and for reviewing the manuscript.
Footnotes
Supplementary materials
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.healun.2021.07.021.
References
- 1.Chambers DC, Cherikh WS, Goldfarb SB, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: thirty-fifth adult lung and heart-lung transplant report-2018; focus theme: multiorgan transplantation. J Heart Lung Transplant 2018;37:1169–83. [DOI] [PubMed] [Google Scholar]
- 2.Chambers DC, Cherikh WS, Harhay MO, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: thirty-sixth adult lung and heart-lung transplantation report-2019; focus theme: donor and recipient size match. J Heart Lung Transplant 2019;38:1042–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chambers DC, Yusen RD, Cherikh WS, et al. The registry of the international society for heart and lung transplantation: thirty-fourth adult lung and heart-lung transplantation report-2017; focus theme: allograft ischemic time. J Heart Lung Transplant 2017;36:1047–59. [DOI] [PubMed] [Google Scholar]
- 4.Yusen RD, Christie JD, Edwards LB, et al. The registry of the international society for heart and lung transplantation: thirtieth adult lung and heart-lung transplant report−2013; focus theme: age. J Heart Lung Transplant 2013;32:965–78. [DOI] [PubMed] [Google Scholar]
- 5.Yusen RD, Edwards LB, Dipchand AI, et al. The registry of the international society for heart and lung transplantation: thirty-third adult lung and heart-lung transplant report-2016; focus theme: primary diagnostic indications for transplant. J Heart Lung Transplant 2016;35:1170–84. [DOI] [PubMed] [Google Scholar]
- 6.Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the international society for heart and lung transplantation: thirty-first adult lung and heart-lung transplant report−2014; focus theme: retransplantation. J Heart Lung Transplant 2014;33:1009–24. [DOI] [PubMed] [Google Scholar]
- 7.Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the international society for heart and lung transplantation: thirty-second official adult lung and heart-lung transplantation report−2015; focus theme: early graft failure. J Heart Lung Transplant 2015;34:1264–77. [DOI] [PubMed] [Google Scholar]
- 8.Khush KK, Cherikh WS, Chambers DC, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: thirty-sixth adult heart transplantation report - 2019; focus theme: donor and recipient size match. J Heart Lung Transplant 2019;38:1056–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rossano JW, Singh TP, Cherikh WS, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: twenty-second pediatric heart transplantation report −2019; focus theme: donor and recipient size match. J Heart Lung Transplant 2019;38:1028–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hayes D Jr, Cherikh WS, Chambers DC, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: twenty-second pediatric lung and heart-lung transplantation report-2019; focus theme: donor and recipient size match. J Heart Lung Transplant 2019;38:1015–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayes D Jr., Harhay MO, Cherikh WS, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: twenty-fourth pediatric lung transplantation report - 2021; focus on recipient characteristics. J Heart Lung Transplant 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khush KK, Hsich E, Potena L, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: 38th adult heart transplantation report-2021; focus on recipient characteristics. J Heart Lung Transplant 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh TP, Cherikh WS, Hsich E, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: 24th pediatric heart transplantation report-2021; focus theme: changing recipient characteristics. J Heart Lung Transplant 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chambers DC, Zuckermann A, Cherikh WS, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: 37th adult lung transplantation report - 2020; focus on deceased donor characteristics. J Heart Lung Transplant 2020;39:1016–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kulkarni HS, Cherikh WS, Chambers DC, et al. Bronchiolitis obliterans syndrome-free survival after lung transplantation: an international society for heart and lung transplantation thoracic transplant registry analysis. J Heart Lung Transplant 2019;38:5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paraskeva MA, Edwards LB, Levvey B, et al. Outcomes of adolescent recipients after lung transplantation: an analysis of the international society for heart and lung transplantation registry. J Heart Lung Transplant 2018;37:323–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


