Abstract
Vaccination is the primary defense against severe acute respiratory syndrome coronavirus 2, especially among older adults and those with chronic conditions. Using a nationally representative sample of 12,900 participants from the fifth wave (2021–2022) of the China Health and Retirement Longitudinal Study (CHARLS), we examined the coronavirus disease 2019 (COVID-19) vaccination status and the determinants of vaccination hesitancy in Chinese adults aged 52 and older. By July/August 2022, 92.3% of the Chinese population aged 60 years and older had received at least one COVID-19 vaccination, 88.6% had completed the primary series and 72.4% had received a booster. Those aged 80 years and older had lower vaccination rates, with 71.9% and 46.7% completing the primary series and booster shots, respectively. These statistics represent the situation before China ended the Zero-COVID policy in November 2022 because vaccination stagnated between July/August and November 2022. Multivariate regression analysis revealed that belonging to the oldest age groups (individuals aged 70 years and older and especially those aged 80 years and older) as well as being female and unmarried, residing in urban areas, being functionally dependent and having chronic conditions meant that these individuals were less likely to receive COVID-19 vaccines. Our regression analysis results were corroborated by self-reported reasons for nonvaccination. Vaccination hesitancy probably contributed to excessive mortality among vulnerable populations after China ceased its Zero-COVID policy. Our study provides important lessons on how to balance containment efforts with vaccination and treatment measures, as well as highlighting the need to clarify the side effects and contraindications of vaccines early on.
The coronavirus disease 2019 (COVID-19) pandemic has resulted in over 6.6 million deaths worldwide to date, most of these recorded among older adults (≥60 years old)1,2. Vaccination is the primary defense against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and studies have demonstrated that vaccines effectively reduce critical conditions and fatalities3. However, even after vaccines became freely available, a substantial proportion of older people from various countries and regions, including mainland China and Hong Kong, were reluctant to be vaccinated4,5. Therefore, it is of critical importance to vaccinate high-risk populations, including older individuals and those with certain comorbidities6,7.
China has the highest number of older individuals globally8. Fearing a catastrophe for the older population under a less developed medical infrastructure, China adhered to a Zero-COVID strategy for nearly 3 years until November 2022, effectively shielding the population against COVID-19. However, the highly infectious Omicron variant severely challenged this strategy by raising the economic and social costs of containment. As infections skyrocketed in November 2022 (ref.9), the public and the government were pushed to the brink of collapse, both psychologically and financially. The Chinese government finally ended the Zero-COVID policy. As of 11 December 2022, most cities stopped requiring SARS-CoV-2 testing in public places and those with SARS-CoV-2 infection are no longer subject to mandatory quarantines, practices that China had adhered to for nearly 3 years10.
Official statistics have consistently shown lower vaccination rates among older Chinese individuals than in their younger counterparts, contrary to the pattern observed in the United States and China’s neighboring countries; this had been the reason behind adopting and adhering to a Zero-COVID policy, despite China being the last country with a large population to relax restrictions8,11. Answers to why China lagged in vaccinating its older population could inform what China can and should do to reverse this situation in preparation for the next COVID-19 wave.
When China-made vaccines (including Vero Cell, CoronaVac and CanSinoBIO) first became available in January 2021 (refs.12,13), the government excluded older populations (those aged 60 or older) from its early vaccination guidance. Older people were encouraged to be vaccinated starting on 31 March 2021. Even then, before the end of the Zero-COVID policy, vaccinators routinely turned away people they suspected might be in danger of experiencing side effects. In particular, anyone older than 60 would first receive a blood pressure test and was disqualified if their diastolic blood pressure was greater than 160 mmHg. Vaccinators also refused those with preexisting conditions such as diabetes, heart disease, stroke, kidney disease and cancer14. The definition of ‘contraindication’ was broad and ambiguous and resulted in public distrust of vaccines. In the third quarter of 2021, as the Delta variant spread rapidly through India, China introduced booster vaccines for younger adults and started to promote vaccination in children15. As Omicron became the dominant variant in late 2021, efforts were made to vaccinate as many people as possible. These measures included financial incentives, material gifts, coercion in some places (some local governments required workers in key industries, such as public security, transportation and mail delivery, to receive a primary vaccine series before returning to work) and vaccination vans driven directly to communities to increase accessibility16. Free insurance against adverse reactions to vaccines was also provided. However, vaccinators continued to exclude people they suspected of having contraindications. Finally, on 29 November 2022, after an abrupt COVID-19 policy change, a new guideline was released. This emphasized the importance of completing primary series and boosters in older populations17. The various stages of vaccination and vaccination rates among older people in China are shown in Fig. 1.
Fig. 1 |. Vaccination campaign and vaccination rates among older adults (60 years and over) in China, from March 2021 to November 2022.
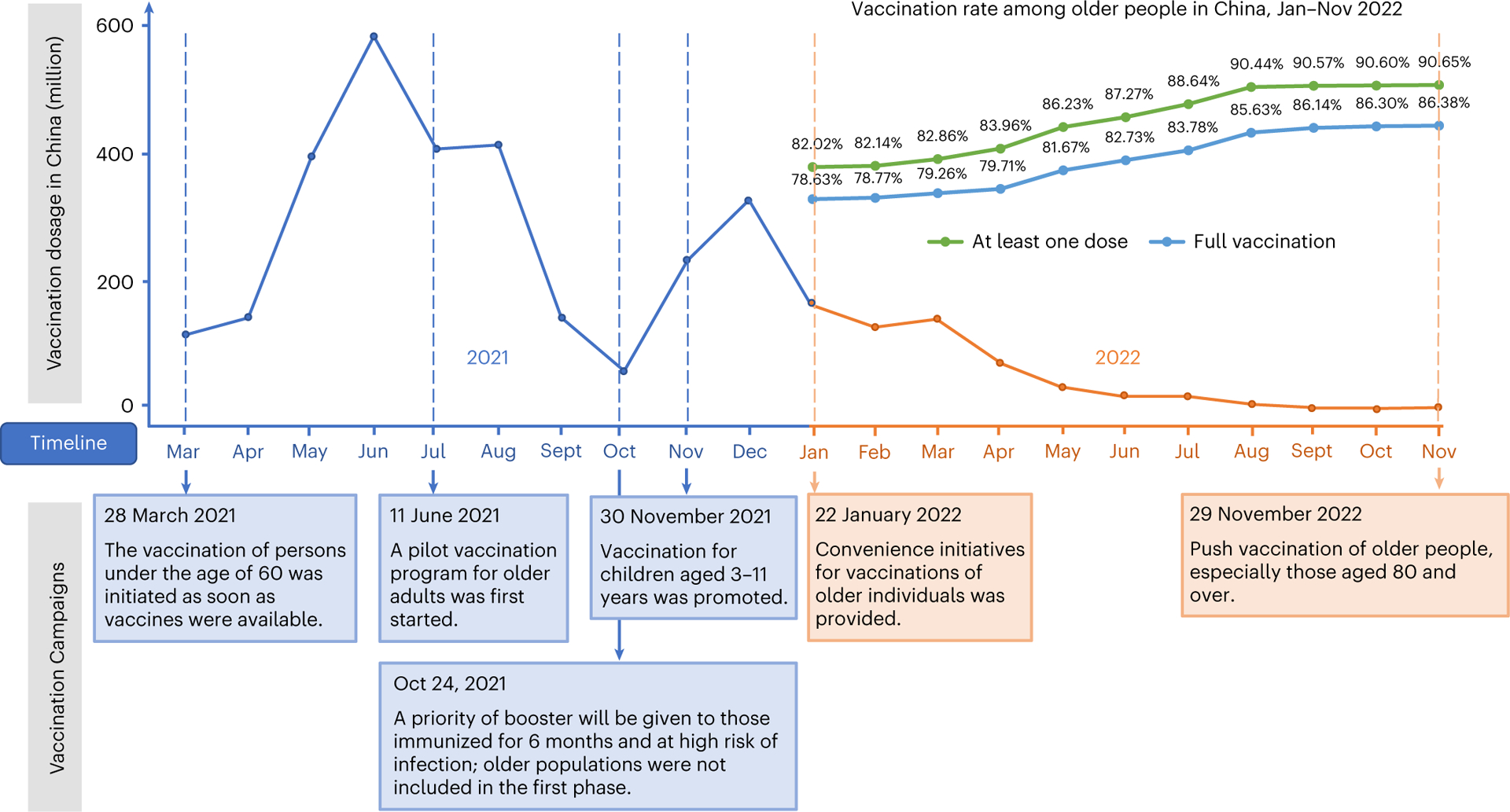
The vaccination dosages per month for whole population in China were presented above the timeline, from March 2021 to November 2022. The major government-led vaccination campaigns were presented below the timeline. The vaccination information in 2021 and 2022 was presented in blue and orange, respectively. The vaccination rate among older Chinese was only available at 2022 and was presented in the upper right.
Developing immediate and efficient vaccination programs requires an understanding of determinants, such as the concerns and motivations that influence the decision-making of older people to be vaccinated or not. The aforementioned vaccination policies suggest that China’s delay in vaccinating older people and those with chronic illnesses was not due to age discrimination; rather, it was influenced by ill-placed paternalism centered around the fear of side effects.
Vaccination hesitancy is common among older people in some countries including China2,18–21. However, actual vaccination rates are higher among older Europeans or Americans (≥65 years old); the opposite is true for China2,22. The difference between China and Western countries suggests that the role of health authorities deserves special attention, especially in how they approach vaccine side effects. Research is lacking in this area. A few studies have reported vaccine uptake in Hong Kong or parts of China, but none has examined the role of health issues and none has focused on a nationwide community-dwelling older population in China23–25.
To address these gaps in knowledge, we included questions about vaccination in the fifth wave of the China Health and Retirement Longitudinal Study (CHARLS) in July/August 2021 and 2022, with vaccine status updated for all respondents in July/August 2022. Given that the vaccination rate in this population did not increase between July/August and November 2022 (Fig. 1), our data reflect the vaccination status of older adults when China ended the Zero-COVID policy. Using regression and textual analysis of narrative reasons, we investigated what drove older people to refuse vaccination or to be hesitant about vaccines.
Results
Study participants
A total of 12,900 participants from the fifth wave of CHARLS (Fig. 2) were included in the analysis of vaccine status as of July/August 2022. The mean age of participants was 65.2 ± 9.5 years (range: 52–101 years); 53% were female. Most participants were married (82.6%), had Han ethnicity (93.0%) and lived in rural households (81.4%). A total of 13.2% had functional dependency, 44.9% had doctor-diagnosed hypertension and 21.9% had doctor-diagnosed diabetes. The unweighted nonvaccination rate of participants was 6.1% and ranged from 3.7% in the 52–59 age range to 17.9% in those aged 80 years and older. A detailed summary of the characteristics of the study participants is presented in Table 1.
Fig. 2 |. Flow chart of the study selection process.

The flow chart exhibits the inclusion and exclusion criteria for the study sample derived from the fifth wave of CHARLS.
Table 1 |.
Characteristics of the study participants in the CHARLS study according to age group
| Characteristic | Total sample n=12,900 | 52–59 n=3,536 | 60–69 n=4,587 | 70–79 n=3,578 | ≥80 n=1,199 |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 6,858 (53.2%) | 1,919 (54.3%) | 2,429 (53.0%) | 1,858 (51.9%) | 652 (54.4%) |
| Male | 6,042 (46.8%) | 1,617 (45.7%) | 2,158 (47.0%) | 1,720 (48.1%) | 547 (45.6%) |
| Marital status | |||||
| Married | 10,635 (82.6%) | 3,290 (93.2%) | 4,047 (88.4%) | 2,701 (75.5%) | 597 (49.9%) |
| Unmarried or widowed | 2,245 (17.4%) | 241 (6.8%) | 529 (11.6%) | 875 (24.5%) | 600 (50.1%) |
| Vaccination status | |||||
| Unvaccinated | 791 (6.1%) | 130 (3.7%) | 199 (4.3%) | 247 (6.9%) | 215 (17.9%) |
| Only one dose | 337 (2.6%) | 43 (1.2%) | 85 (1.9%) | 115 (3.2%) | 94 (7.8%) |
| Primary series completed | 1,805 (14.0%) | 379 (10.7%) | 587 (12.8%) | 560 (15.7%) | 279 (23.3%) |
| Booster | 9,967 (77.3%) | 2,984 (84.4%) | 3,716 (81.0%) | 2,656 (74.2%) | 611 (51.0%) |
| Ethnicity | |||||
| Han | 11,929 (93.0%) | 3,231 (92.1%) | 4,230 (93.0%) | 3,342 (93.7%) | 1,126 (94.1%) |
| Non-Han (minority) | 892 (7.0%) | 276 (7.9%) | 320 (7.0%) | 225 (6.3%) | 71 (5.9%) |
| Education | |||||
| Illiterate | 3,716 (28.8%) | 539 (15.2%) | 1,310 (28.6%) | 1,291 (36.1%) | 576 (48.0%) |
| Primary (includes literate) | 4,899 (38.0%) | 1,392 (39.4%) | 1,456 (31.7%) | 1,621 (45.3%) | 430 (35.9%) |
| Middle and high school or higher | 4,281 (33.2%) | 1,604 (45.4%) | 1,820 (39.7%) | 664 (18.6%) | 193 (16.1%) |
| Residence (Hukou) | |||||
| Rural residence | 10,500 (81.4%) | 2,963 (83.8%) | 3,773 (82.3%) | 2,841 (79.4%) | 923 (77.0%) |
| Urban residence | 2,398 (18.6%) | 572 (16.2%) | 814 (17.7%) | 736 (20.6%) | 276 (23.0%) |
| Region | |||||
| East | 4,448 (34.5%) | 1,215 (34.4%) | 1,705 (37.2%) | 1,116 (31.2%) | 412 (34.4%) |
| Central | 3,836 (29.7%) | 1,034 (29.2%) | 1,301 (28.4%) | 1,134 (31.7%) | 367 (30.6%) |
| West | 3,719 (28.8%) | 1,050 (29.7%) | 1,218 (26.6%) | 1,096 (30.6%) | 355 (29.6%) |
| Northeast | 897 (7.0%) | 237 (6.7%) | 363 (7.9%) | 232 (6.5%) | 65 (5.4%) |
| Functional dependency | 1,699 (13.2%) | 226 (6.4%) | 464 (10.2%) | 601 (16.8%) | 408 (34.2%) |
| Chronic conditions | |||||
| Hypertension | 5,773 (44.9%) | 1,198 (34.0%) | 2,013 (44.0%) | 1,937 (54.2%) | 625 (52.4%) |
| Heart disease | 2,814 (21.9%) | 522 (14.8%) | 979 (21.4%) | 999 (28.0%) | 314 (26.3%) |
| Stroke | 809 (6.3%) | 122 (3.5%) | 248 (5.4%) | 329 (9.2%) | 110 (9.2%) |
| Diabetes | 1,980 (15.4%) | 442 (12.5%) | 757 (16.6%) | 629 (17.6%) | 152 (12.8%) |
| Lung disease | 1,975 (15.4%) | 381 (10.8%) | 684 (15.0%) | 671 (18.8%) | 239 (20.1%) |
| Cancer | 331 (2.6%) | 78 (2.2%) | 127 (2.8%) | 105 (2.9%) | 21 (1.8%) |
| Dyslipidemia | 3,428 (26.7%) | 865 (24.5%) | 1,270 (27.8%) | 1,051 (29.4%) | 242 (20.3%) |
| Liver disease | 862 (6.7%) | 224 (6.4%) | 319 (7.0%) | 260 (7.3%) | 59 (4.9%) |
| Kidney disease | 1,128 (8.8%) | 238 (6.8%) | 409 (8.9%) | 371 (10.4%) | 110 (9.2%) |
| Asthma | 789 (6.1%) | 116 (3.3%) | 276 (6.0%) | 302 (8.5%) | 95 (8.0%) |
| Arthritis/rheumatism | 4,817 (37.5%) | 1,126 (31.9%) | 1,745 (38.2%) | 1,499 (42.0%) | 447 (37.5%) |
| Digestive disease | 3,718 (28.9%) | 1,038 (29.4%) | 1,339 (29.3%) | 1,042 (29.2%) | 299 (25.1%) |
The weighted vaccination rate (that is, individuals having received at least one dose) for older people (aged 60 years and older) was 92.3%; for those who received the first dose, the completion rates of the primary series and booster doses were 88.6% and 72.4%, respectively (Fig. 3). Vaccination rates declined with age. Among the oldest age group (aged 80 years and older), the weighted rates for first-dose, primary series and booster vaccinations were 80.5%, 71.9% and 46.7%, respectively. A negative age gradient of vaccination was found within subgroups according to sex, rural or urban residence, or education (Extended Data Table 1).
Fig. 3 |. Vaccination rates among older Chinese individuals.

Top, subset of the main sample (n = 9,872) who also participated in the 2021 survey and were older than 52 years in 2021. Bottom, main sample of this study (n = 12,900). The 95% confidence intervals (CIs) are shown as capped horizontal spikes. The length of each horizontal bar, that is, the position of each spike’s center, is indicated by the number to the right.
Vaccination rates based on the CHARLS data are roughly similar to official statistics released by China’s National Health Committee; both were calculated around July/August 2022. Both sources reported similar rates for those aged 60–79 years. There was a slight increase in CHARLS vaccination rates in the oldest group, that is, those aged 80 years and older (Extended Data Fig. 1).
Determinants of nonvaccination in the older age groups
The logistic regressions reporting the associations between different determinants of vaccination status are shown in Table 2. In column 1, we focused on comparing those who received at least one vaccine dose with those who were unvaccinated. Being older, female, unmarried and residing in urban areas (defined by household registration status when first enrolled in the study) were associated with lower vaccination rates (P < 0.05). Among the age groups, the oldest group (80 years and older) was least likely to be vaccinated (odds ratio (OR) = 0.37, 95% CI (0.28–0.49), P < 0.001) compared to those aged 52–59 years. Those who were functionally dependent were less likely to be vaccinated than those who were independent in their activities of daily living (ADLs) (OR = 0.29 (0.24–0.35), P < 0.001). A similar pattern was observed in individuals with chronic conditions that are often mistakenly perceived as vaccine contraindications, including hyper-tension (OR = 0.84 (0.72–0.99), P = 0.037), heart disease (OR = 0.61 (0.51–0.74), P < 0.001), stroke (OR = 0.75 (0.58–0.96), P = 0.023), diabetes (OR = 0.79 (0.65–0.98), P = 0.029), lung disease (OR = 0.71 (0.57–0.88), P = 0.002) and cancer (OR = 0.25 (0.18–0.34), P < 0.001). However, kidney disease, liver disease (cancer excluded) and dyslipidemia did not have statistically significant effects on vaccination, presumably because they were not perceived as contraindications. Individuals with arthritis were more likely to be vaccinated.
Table 2 |.
Determinants of vaccination status among older adults
| Binary dependent variable in the logistic regression model (1 versus 0) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (1) Vaccinated (at least one dose) versus unvaccinated | (2) Primary series recipients versus others | (3) Booster recipients versus others | (4) Primary series recipients versus those vaccinated but who had not completed the primary series doses | (5) Booster recipients versus those who had completed the primary series doses but who had yet to receive booster doses | ||||||
| Number of observations; mean of dependent variable |
n=12,900 mean=0.939 |
n=12,900 mean=0.913 |
n=12,900 mean=0.773 |
n=12,069 mean=0.972 |
n=11,772 mean=0.847 |
|||||
| Characteristic | OR (95% Cl) | P | OR (95% Cl) | P | OR (95% Cl) | P | OR (95% Cl) | P | OR (95% Cl) | P |
| Female | 0.83 (0.70–0.98) | 0.026 | 0.82 (0.71–0.94) | 0.005 | 0.93 (0.86–1.01) | 0.094 | 0.81 (0.65–1.03) | 0.081 | 1.00 (0.91–1.11) | 0.958 |
| Married | 1.52 (1.26–1.83) | 0.000 | 1.40 (1.18–1.65) | 0.000 | 1.19 (1.06–1.35) | 0.004 | 1.14 (0.86–1.52) | 0.363 | 1.07 (0.93–1.24) | 0.351 |
| Minority ethnic group | 0.91 (0.64–1.29) | 0.599 | 0.67 (0.52–0.88) | 0.004 | 0.65 (0.54–0.78) | 0.000 | 0.49 (0.34–0.69) | 0.000 | 0.68 (0.55–0.84) | 0.000 |
| Urban residence | 0.63 (0.51–0.77) | 0.000 | 0.73 (0.61–0.88) | 0.001 | 0.98 (0.86–1.11) | 0.727 | 1.08 (0.76–1.52) | 0.668 | 1.15 (0.98–1.34) | 0.091 |
| Age group (reference: 52–59) | ||||||||||
| 60–69 | 1.02 (0.81–1.29) | 0.879 | 0.90 (0.74–1.11) | 0.332 | 0.86 (0.76–0.98) | 0.023 | 0.69 (0.47–1.01) | 0.057 | 0.85 (0.73–0.98) | 0.029 |
| 70–79 | 0.80 (0.63–1.03) | 0.082 | 0.66 (0.53–0.81) | 0.000 | 0.65 (0.56–0.75) | 0.000 | 0.43 (0.29–0.64) | 0.000 | 0.66 (0.56–0.78) | 0.000 |
| 80+ | 0.37 (0.28–0.49) | 0.000 | 0.27 (0.21–0.35) | 0.000 | 0.27 (0.23–0.32) | 0.000 | 0.16 (0.11–0.26) | 0.000 | 0.33 (0.27–0.41) | 0.000 |
| Education (reference: illiterate) | ||||||||||
| Primary school (literate) | 1.05 (0.86–1.28) | 0.623 | 0.92 (0.77–1.08) | 0.309 | 1.02 (0.91–1.14) | 0.780 | 0.71 (0.54–0.94) | 0.018 | 1.08 (0.94–1.23) | 0.267 |
| Middle, high schooland higher | 1.17 (0.91–1.49) | 0.218 | 1.16 (0.94–1.43) | 0.170 | 1.11 (0.97–1.27) | 0.145 | 1.17 (0.81–1.69) | 0.393 | 1.09 (0.93–1.28) | 0.296 |
| Region (reference: East) | ||||||||||
| Central | 1.07 (0.87–1.30) | 0.531 | 1.27 (1.06–1.51) | 0.008 | 1.14 (1.01–1.29) | 0.040 | 1.98 (1.41–2.78) | 0.000 | 1.07 (0.92–1.23) | 0.398 |
| West | 1.50 (1.21–1.85) | 0.000 | 1.37 (1.14–1.64) | 0.001 | 1.27 (1.12–1.45) | 0.000 | 1.14 (0.85–1.51) | 0.381 | 1.20 (1.03–1.39) | 0.019 |
| Northeast | 1.38 (0.99–1.93) | 0.061 | 1.20 (0.90–1.60) | 0.216 | 0.89 (0.73–1.09) | 0.253 | 0.89 (0.56–1.41) | 0.620 | 0.77 (0.61–0.98) | 0.034 |
| Functionally dependent | 0.29 (0.24–0.35) | 0.000 | 0.32 (0.27–0.37) | 0.000 | 0.45 (0.40–0.51) | 0.000 | 0.43 (0.33–0.57) | 0.000 | 0.65 (0.56–0.76) | 0.000 |
| Chronic conditions | ||||||||||
| Hypertension | 0.84 (0.72–0.99) | 0.037 | 0.81 (0.71–0.93) | 0.002 | 0.86 (0.79–0.95) | 0.002 | 0.76 (0.60–0.96) | 0.022 | 0.91 (0.81–1.02) | 0.091 |
| Heart disease | 0.61 (0.51–0.74) | 0.000 | 0.72 (0.61–0.84) | 0.000 | 0.86 (0.77–0.96) | 0.007 | 1.09 (0.81–1.46) | 0.592 | 0.97 (0.85–1.11) | 0.683 |
| Stroke | 0.75 (0.58–0.96) | 0.023 | 0.78 (0.62–0.98) | 0.033 | 0.75 (0.64–0.89) | 0.001 | 0.90 (0.60–1.35) | 0.612 | 0.78 (0.63–0.96) | 0.016 |
| Diabetes | 0.79 (0.65–0.98) | 0.029 | 0.76 (0.64–0.91) | 0.003 | 0.86 (0.76–0.97) | 0.014 | 0.73 (0.55–0.98) | 0.035 | 0.94 (0.81–1.09) | 0.409 |
| Lung disease | 0.71 (0.57–0.88) | 0.002 | 0.85 (0.70–1.02) | 0.087 | 0.94 (0.82–1.08) | 0.374 | 1.34 (0.93–1.92) | 0.115 | 1.00 (0.85–1.17) | 0.957 |
| Cancer | 0.25 (0.18–0.34) | 0.000 | 0.28 (0.21–0.38) | 0.000 | 0.40 (0.32–0.51) | 0.000 | 0.52 (0.29–0.95) | 0.035 | 0.60 (0.44–0.81) | 0.001 |
| Dyslipidemia | 1.25 (1.04–1.51) | 0.020 | 1.21 (1.03–1.43) | 0.023 | 1.13 (1.01–1.27) | 0.028 | 1.10 (0.82–1.47) | 0.529 | 1.08 (0.94–1.23) | 0.281 |
| Liver disease | 1.02 (0.74–1.41) | 0.898 | 0.93 (0.71–1.21) | 0.578 | 1.01 (0.85–1.22) | 0.880 | 0.77 (0.50–1.20) | 0.253 | 1.08 (0.86–1.34) | 0.518 |
| Kidney disease | 0.81 (0.62–1.04) | 0.101 | 0.86 (0.69–1.08) | 0.209 | 1.07 (0.91–1.26) | 0.412 | 1.05 (0.69–1.59) | 0.834 | 1.23 (1.00–1.51) | 0.048 |
| Asthma | 1.02 (0.76–1.38) | 0.872 | 0.95 (0.74–1.23) | 0.718 | 0.88 (0.73–1.06) | 0.185 | 0.82 (0.52–1.29) | 0.396 | 0.86 (0.69–1.08) | 0.191 |
| Arthritis/rheumatism | 1.44 (1.21–1.72) | 0.000 | 1.37 (1.18–1.59) | 0.000 | 1.15 (1.04–1.27) | 0.006 | 1.17 (0.92–1.50) | 0.206 | 1.04 (0.93–1.17) | 0.514 |
| Digestive disease | 1.16 (0.96–1.39) | 0.117 | 1.22 (1.04–1.43) | 0.013 | 1.20 (1.08–1.33) | 0.000 | 1.32 (1.01–1.74) | 0.045 | 1.16 (1.03–1.31) | 0.015 |
| Constant | 22.71 (15.93–32.37) | 0.000 | 17.84 (13.12–24.25) | 0.000 | 4.67 (3.80–5.75) | 0.000 | 81.25 (47.06–140.28) | 0.000 | 6.72 (5.25–8.61) | 0.000 |
Standard errors are clustered at the household level. The CI was calculated based on a Wald test. P values are based on a two-sided Wald test. ‘Others’ in column 2 refers to unvaccinated individuals and vaccinated individuals who had yet to complete the primary series doses. ‘Others’ in column 3 refers to unvaccinated individuals and vaccinated individuals who had yet to receive booster doses.
When primary series and booster vaccinations were used as the outcomes in columns 2 and 3 of Table 2, the directions of the associations, particularly regarding older age, functional dependency and chronic diseases, were the same. Although no difference was found in vaccination odds between the non-Han and Han Chinese groups (P = 0.599), non-Han ethnicity was strongly associated with delayed vaccination in the primary series (OR = 0.67 (0.52–0.88), P = 0.004) and booster doses (OR = 0.65 (0.54–0.78), P < 0.001). There were no significant differences in vaccination status according to educational attainment. Digestive disease was also positively associated with vaccination. Its association was marginally significant in individuals who received the first dose; however, the associations were stronger in individuals who received the primary series doses or boosters.
Next, we conducted a separate analysis by excluding unvaccinated individuals and examined the decision to complete the primary series doses in individuals who had previously received at least one vaccine shot (column 4). Additionally, we excluded those who had not completed the primary series doses and examined the decision to receive a booster shot among those who completed the primary series (column 5). In columns 4 and 5, the ORs were similar to those in columns 2 and 3 for variables such as older age, non-Han ethnicity, functional dependency, stroke and cancer. However, the associations between commonly perceived contraindications, such as heart disease, diabetes and lung disease, and completing the primary series doses or receiving a booster were statistically nonsignificant. This suggests that past experiences of vaccination may have helped build confidence in vaccine safety and changed people’s perception of vaccine contraindications.
Our data have some limitations. For respondents who missed the 2021 interview but were interviewed in 2022, all variables pertained to their vaccination status in 2022. However, in respondents who completed their interviews in 2021, although their vaccination status was updated to 2022, the rest of the questionnaire was not. Therefore, there is a 1-year timing mismatch for a subset of respondents; that is, while vaccination status refers to that recorded in 2022, health-related variables were from 2021. This may not be a major concern because chronic conditions rarely change in 1 year. Nevertheless, we conducted a sensitivity analysis using the health conditions derived from the 2018 wave for all respondents and the results were consistent (Extended Data Table 2).
Another way to address the timing mismatch is to restrict our analysis to the subset of respondents who were interviewed in 2021 and reinterviewed in 2022, so that all included health variables for the regression came from 2021. The results (Extended Data Table 3) were unchanged, suggesting that nonresponse in the 2021 interview was not correlated with a person’s vaccination status in 2022.
Finally, we performed an analysis of comorbidity to substitute the ten main conditions with a measure counting the incidence of these conditions (Extended Data Table 4). Consistent with our baseline analysis, which used the full set of disease indicators, comorbidity as a composite measure was a strong predictor of vaccination hesitancy (OR = 0.82 (0.79–0.86), P < 0.001).
Changes in vaccine status due to government-driven vaccination campaigns
Using a multinomial logit regression (Table 3), we examined the determinants of vaccination timing: individuals vaccinated before July/August 2021 (thereafter referred to as phase 1); individuals vaccinated between the two summers (July/August) of 2021 and 2022 (phase 2); and individuals not vaccinated by July/August 2022. Nonvaccination was used as the baseline outcome in columns 1 and 2. The two phases correspond to the early and late vaccination campaigns. During phase 1, that is, in the 6 months since COVID-19 vaccines became available, being female, older (70 years and older, especially 80 years and older), unmarried or widowed, having non-Han ethnicity, residing in an urban location, or being functionally dependent or chronically ill reduced the odds of receiving vaccinations (P value for relative risk ratio (RRR) < 0.01). Phase 2 showed significantly higher odds of vaccination in high-risk populations, especially for older age groups, individuals with functional dependency and individuals with major chronic diseases typically considered contraindications to vaccination, reflecting the government’s efforts to close the vaccination gap. The results remained when we relaced disease data from 2021 to 2018 (Extended Data Table 5).
Table 3 |.
Determinants of early, late and nonvaccination status among older adults
| Multinomial logit regressiona | (1) Phase 1 vaccination (Jan 2021-Jul/Aug 2021) versus nonvaccination | (2) Phase 2 vaccination (Jul/Aug 2021-Jul/Aug 2022) versus nonvaccination | (3) Phase 2 versus phase 1 vaccination | |||
|---|---|---|---|---|---|---|
| n=9,890 | n=9,890 | n=9,890 | ||||
| RRR (95% CI) | P | RRR (95% CI) | P | RRR (95% CI) | P | |
| Female | 0.80 (0.67–0.95) | 0.010 | 0.82 (0.68–0.99) | 0.035 | 1.03 (0.93–1.13) | 0.605 |
| Married | 1.65 (1.35–2.01) | 0.000 | 1.38 (1.12–1.71) | 0.003 | 0.84 (0.72–0.97) | 0.020 |
| Minority ethnicity | 0.58 (0.40–0.84) | 0.004 | 1.38 (0.97–1.96) | 0.075 | 2.39 (1.92–2.97) | 0.000 |
| Urban residence | 0.59 (0.47–0.73) | 0.000 | 0.41 (0.32–0.52) | 0.000 | 0.70 (0.59–0.84) | 0.000 |
| Age group (reference: 52–59) | ||||||
| 60–69 | 0.93 (0.73–1.18) | 0.530 | 2.03 (1.54–2.69) | 0.000 | 2.20 (1.85–2.61) | 0.000 |
| 70–79 | 0.66 (0.51–0.85) | 0.001 | 2.21 (1.66–2.95) | 0.000 | 3.35 (2.78–4.03) | 0.000 |
| 80+ | 0.19 (0.14–0.26) | 0.000 | 1.63 (1.18–2.25) | 0.003 | 8.44 (6.65–10.72) | 0.000 |
| Education (reference: illiterate) | ||||||
| Primary school (literate) | 1.00 (0.82–1.23) | 0.969 | 0.99 (0.80–1.22) | 0.900 | 0.98 (0.86–1.12) | 0.792 |
| Middle, high school and higher | 1.12 (0.87–1.44) | 0.388 | 0.87 (0.66–1.14) | 0.311 | 0.78 (0.66–0.92) | 0.003 |
| Region (reference: East) | ||||||
| Central | 0.88 (0.71–1.09) | 0.231 | 0.97 (0.77–1.22) | 0.802 | 1.11 (0.95–1.29) | 0.207 |
| West | 1.38 (1.10–1.74) | 0.006 | 1.59 (1.25–2.02) | 0.000 | 1.15 (0.99–1.35) | 0.070 |
| Northeast | 1.06 (0.75–1.49) | 0.742 | 2.03 (1.41–2.92) | 0.000 | 1.91 (1.51–2.43) | 0.000 |
| Functionally dependent | 0.20 (0.17–0.24) | 0.000 | 0.48 (0.40–0.59) | 0.000 | 2.41 (2.08–2.79) | 0.000 |
| Chronic conditions | ||||||
| Hypertension | 0.78 (0.66–0.92) | 0.004 | 1.01 (0.85–1.21) | 0.874 | 1.30 (1.16–1.45) | 0.000 |
| Heart disease | 0.57 (0.47–0.70) | 0.000 | 0.65 (0.53–0.80) | 0.000 | 1.14 (0.99–1.31) | 0.064 |
| Stroke | 0.59 (0.45–0.77) | 0.000 | 0.91 (0.69–1.19) | 0.475 | 1.53 (1.25–1.87) | 0.000 |
| Diabetes | 0.74 (0.59–0.92) | 0.008 | 0.90 (0.71–1.13) | 0.372 | 1.21 (1.04–1.42) | 0.014 |
| Lung disease | 0.73 (0.58–0.92) | 0.007 | 0.73 (0.58–0.93) | 0.012 | 1.00 (0.85–1.18) | 0.982 |
| Cancer | 0.20 (0.14–0.28) | 0.000 | 0.44 (0.31–0.63) | 0.000 | 2.20 (1.60–3.03) | 0.000 |
| Dysli pidemia | 1.25 (1.02–1.52) | 0.029 | 1.12 (0.90–1.38) | 0.316 | 0.89 (0.78–1.03) | 0.111 |
| Liver disease | 0.91 (0.65–1.28) | 0.585 | 0.93 (0.65–1.33) | 0.681 | 1.02 (0.81–1.28) | 0.867 |
| Kidney disease | 0.72 (0.55–0.94) | 0.018 | 0.71 (0.53–0.95) | 0.021 | 0.99 (0.81–1.20) | 0.910 |
| Asthma | 0.90 (0.65–1.24) | 0.513 | 1.00 (0.72–1.39) | 0.997 | 1.11 (0.88–1.42) | 0.381 |
| Arthritis/rheumatism | 1.54 (1.29–1.86) | 0.000 | 1.23 (1.01–1.49) | 0.038 | 0.79 (0.71–0.89) | 0.000 |
| Digestive disease | 1.22 (1.01–1.47) | 0.042 | 1.05 (0.85–1.29) | 0.651 | 0.86 (0.76–0.97) | 0.018 |
The dependent variable has three discrete outcomes, each compared to the one used as the baseline outcome. All results are from one multinomial logit regression and each column shows the results from an outcome pair. In column 3, only the baseline outcome changed, so the RRRs are the quotients between those from columns 2 and 1. Standard errors are clustered at the household level. The phase 1 vaccination campaign ran from January 2021 to July/August 2021 and represents the early period when vaccines had not been available for more than 6 months; the phase 2 vaccination campaign ran from July/August 2021 to July/August 2022 and represents the later period. The 95% CI was calculated based on a Wald test.
Changes in government priorities are evident in column 3, where the RRRs between late and early vaccinations are shown. We found a substantial increase in vaccine uptake among older adults from minority ethnic groups (RRR = 2.39 (1.92–2.97), P < 0.001), aged 60–69 years (RRR = 2.20 (1.85–2.61), P < 0.001), those aged 70–79 years (RRR = 3.35 (2.78–4.03), P < 0.001) and particularly those aged 80 and older (RRR = 8.44 (6.65–10.72), P < 0.001). Similarly, significant increases in vaccine uptake were noted in those with functional dependency (RRR = 2.41 (2.08–2.79), P < 0.001) and major chronic conditions, including hypertension (RRR = 1.30 (1.16–1.45), P < 0.001), stroke (RRR = 1.53 (1.25–1.87), P < 0.001), diabetes (RRR = 1.21 (1.04–1.42), P < 0.001) and cancer (RRR = 2.20 (1.60–3.03), P < 0.001).
Sex differences did not change between the two vaccination campaigns (RRR = 1.03 (0.93–1.13), P = 0.605), suggesting that vaccination for women continued to lag behind. The vaccination rates of married older adults were closer to their counterparts in phase 2 (RRR = 0.84 (0.72–0.97), P = 0.02), but this effect was small. Vaccination for urban older adults fell even further behind during phase 2 (RRR = 0.70 (0.59–0.84), P < 0.001).
Because vaccine uptake for the oldest age group, especially those with severe health conditions, lagged behind in vaccination uptake in phase 1 (RRR = 0.19 (0.14–0.26), P < 0.001), a significant acceleration in vaccinations during phase 2 did not help the government to achieve the same coverage for this population as for the other age groups. By July/August 2022, they were still undervaccinated.
Self-reported reasons for vaccine hesitancy
Extended Data Table 6 shows the reasons for vaccine hesitancy by the end of each of the two vaccination campaign phases. In July/August 2022, the top five reasons were having contraindications (48%), being old, frail or having a chronic disease (21%), poor accessibility to vaccination due to barriers such as travel, mobility and short supply of vaccine (18%), concerns about side effects or efficacy (9%) and having never heard of COVID-19 vaccines (6%). In the oldest age group, lack of knowledge about vaccines was an important factor. On the other hand, concerns regarding contraindications were more pronounced among the youngest older adults (Extended Data Table 7). More concerns on health-related factors were raised in phase 2. We observed an increase in reasons attributed to contraindications, from 30% in July/August 2021 to 48% in July/August 2022. Reasons for lack of vaccine uptake that decreased in frequency included accessibility (from 22% in 2021 to 18% in 2022) and unawareness of COVID-19 vaccines (from 8% in 2021 to 6% in 2022).
Discussion
During China’s Zero-COVID policy era, despite the government’s efforts in vaccinating the population, efforts were insufficient, with vaccination rates among older people remaining lower than those of their younger counterparts. In our study, only 71.9% of the oldest age group (80 years and older) had completed their primary series and 46.7% had received booster doses as of July/August 2022; little progress was made from that time until China dropped the Zero-COVID policy in November 2022. This left those population groups at substantial risk as the COVID-19 pandemic continued to sweep through China in December 2022 and January 2023.
Combined with mask wearing, physical distancing, sanitation and ventilation, vaccines contribute to the control of the COVID-19 pandemic and have saved millions of lives, especially among older people26. However, even after vaccines became freely available, a substantial proportion of older people from several countries and regions, including mainland China and Hong Kong, were reluctant to take them4,5. Using both quantitative and qualitative analyses, we found that women, the oldest age groups (older than 70 but especially those older than 80), unmarried or widowed individuals, urban individuals, and functionally dependent individuals, and those with chronic diseases were less likely to be vaccinated against COVID-19. Many of these results are in agreement with the existing literature on vaccine uptake. For example, studies from China and France observed higher vaccination hesitancy in women5,27,28. Regarding the difference between age groups, early in 2022 Hong Kong experienced an Omicron variant outbreak and reported the highest number of COVID-19-related deaths per capita in the world; 90% of COVID-19-related deaths in older adults were in individuals who had not received the full vaccination course4. By contrast, countries with much lower COVID-19-related mortality, such as Singapore and Japan, adequately vaccinated their older citizens (vaccination rate above 95%)29.
Unmarried or widowed older individuals had lower vaccination rates, possibly because of limited access to information or lacking social support30–32. In many other countries, people with functional disabilities are likely to receive vaccinations; therefore, policies often target this group by providing at-home vaccinations33. A study from Shanghai (China) found that people older than 60 with diabetes had lower booster vaccination rates than those younger than 60 (ref.11). Older urban residents have lower vaccination rates than their rural counterparts. The urban–rural difference among older people can be explained by much higher employment rates in older rural residents due to early labor market exits by urban workers34. Even if we only look at non-agricultural work, older rural residents also work at much higher rates than their urban counterparts. Because non-agricultural jobs (employed or self-employed) often require vaccination, rural people tend to vaccinate more. Additionally, rural residents are more responsive to financial incentives due to lower income levels and rural leaders are more likely to use coercive measures to enforce vaccination16.
China stands out for the negative perceptions about vaccination among older age groups and those with chronic illnesses. Given China’s paternalistic tradition, the way health authorities handled information about vaccine side effects had a role. In particular, vaccine clinics refused to vaccinate older people with potentially life-threatening conditions14. In addition, both the public and local vaccinators often misunderstand COVID-19-related contraindications. Older people have often been denied vaccination because of hypertension or diabetes, which are mistakenly considered as vaccine contraindications14. Although on the decline, this incorrect perception continued until late 2022, when the government ended its Zero-COVID policy35. The lack of clear guidelines and public education with transparent data on vaccine safety has, in turn, undermined public trust in vaccines.
A strength of this study is the relatively precise estimation of vaccination rates among older people right before China ended its Zero-COVID policy by taking advantage of data from a nationally representative cohort of older adults in China. We reported the uptake rates of individuals who had received at least one dose, individuals who had received primary series vaccination and individuals who had received booster doses as of July/August 2022; after this period and up until the end of the Zero-COVID policy, vaccination rates in China remained stagnant. Another strength of this study is the successive surveys of the study sample in July/August 2021 and 2022, which enabled us to track the dynamics of vaccination among diverse subpopulations and identify the roles health authorities had in this process. Furthermore, by combining qualitative and quantitative analyses, we examined the determinants of vaccine hesitancy among older adults; this allowed us to formulate pragmatic recommendations for future vaccination campaigns.
Our study has several limitations. The data presented in this study describe the situation before China’s discontinuation of the Zero-COVID policy. Some of this hesitancy probably reflected a misplaced complacency resulting from low perceived risk of infection due to the Zero-COVID policy that lasted nearly 3 years. Because of data limitations, we did not study the effect of the perceived risk of infection in this study.
The vaccine hesitancy we have documented in this article has domestic policy implications. China experienced a surge in infections within a short period since the end of the Zero-COVID policy. One study reported that infections in Beijing would reach 92.3% by the end of January 2023 (ref.36). High infection rates, especially within a short time, probably caused excessive mortality in China. Because vaccination is effective in reducing disease severity and deaths, those who have been vaccinated are likely to have a higher probability of surviving the pandemic. It is unfortunate that those who need protection the most, that is, older people with chronic conditions, are less vaccinated in China. Looking ahead, COVID-19 is not over and the virus is continuing to evolve. China should learn this lesson and devote more efforts toward vaccinating the whole population before the next wave strikes.
China’s experience also has implications for global responses to future pandemics. In particular, attention should be paid to coordinate and balance efforts in containment, vaccination and treatment. In the early stage of an outbreak, when vaccination is not available, containment probably has the larger returns. After vaccines are available, priority should be shifted to vaccination and building up treatment capacity. During vaccination campaigns, it is important to set a clear timeline for relaxing containment measures and make this known to the public. This information can preempt any unrealistic expectations of the perpetual protection containment policies may or may not offer. Additionally, we demonstrated that misconceptions of contraindications and concerns about vaccine side effects are often the leading determinants of vaccine hesitancy; thus, vaccine development should prioritize research to clarify these side effects and contraindications.
Methods
Sampling strategy of the CHARLS survey
CHARLS, which follows the design of the Health and Retirement Study, the English Longitudinal Study of Ageing, the Survey of Health, Ageing and Retirement in Europe and other aging surveys, collects a nationally representative sample of Chinese residents aged 45 and older to inform scientific research on older individuals and assess their health trends. Its baseline survey included 450 villages and communities across the country, with a sample size of 17,708 individuals in 10,257 households37. CHARLS uses multistage systematic random sampling to select respondents. First, district and county units are stratified by region, rural or urban areas and gross domestic product per capita. Based on probability proportional to population size, 150 counties or districts were randomly chosen and three village or community units (primary sampling units (PSUs)) were further randomly selected within each county or district unit. The team developed a customized mapping software to help draw a sample frame of all households in each PSU. Within each household selected from the mapping frame, one resident aged 45 and older was randomly chosen to be the main respondent; this person’s spouse was automatically included in the sample. To avoid human error and manipulation, each sampling stage was computerized and all interviews were conducted using computer-aided personal interview technology. Thanks to the strict quality control implemented in the sampling and survey process, the CHARLS sample is representative of the population of older adults in the country.
Study design and participants
A total of 17,708 CHARLS respondents were interviewed at baseline in 2011. These respondents have since been reinterviewed in 2013, 2015, 2018, 2020 and 2021–2022. In these follow-up surveys, some individuals were lost due to deaths and new representative samples were added for the following reasons: (1) those who did not respond in the baseline survey were interviewed in a follow-up wave; (2) refresher samples were added; (3) new spouses of incumbent respondents were added. Some baseline respondents were replaced when later waves highlighted previous sample errors. The current intended sample size is 19,010 individuals for the fifth wave of the CHARLS survey, which includes all currently living representative respondents who have appeared in at least one previous wave.
Figure 2 shows the study selection process based on this target sample of 19,010 individuals. The fifth wave of CHARLS, including a module on COVID-19, was originally planned for July and August 2021; however, the fieldwork was disrupted in many locations due to COVID-19 outbreaks. Thus, 11,647 individuals were successfully interviewed in July and August 2021. Once the survey resumed in the summer of 2022 (July and August), CHARLS attempted to update the vaccination status of all individuals in the sample, eventually completing 15,293 interviews; 1,798 individuals did not respond to the COVID-19 module. The size of the COVID-19 respondent sample is thus 13,495 individuals.
To adjust for sample attrition, CHARLS constructed a probit model to account for attrition and multiplied the inverse of the predicted response probability with the original sampling weights inherited to obtain the updated sampling weight. We further obtained weights after stratification to align the sample with the age and sex composition in the national population statistics. Because no refreshment samples were added after the 2015 wave, 595 respondents were younger than 52 in 2021 and 2022; they were too few to be assigned weights after stratification, so the sample size for our main analysis was reduced to 12,900. In this main sample, a total of 3,010 respondents missed the COVID-19 interview in 2021. For our analysis of vaccination timing, that is, whether the first dose was received in phase 1 or 2 of the vaccination campaign, we used a balanced sample size of 9,890.
Ethics statement
All participants or their legal representatives signed written informed consent forms to participate in the baseline and follow-up surveys. Informed consent was obtained from the study participants before completing the study questionnaire. The study was approved by the biomedical ethics committee of Peking University, Beijing, China (no. IRB00001052–11015).
Procedures
Vaccination-related questions in the COVID-19 module asked about the number of doses the respondents had received, the number of required doses to complete the primary series vaccination and reasons why an individual was still unvaccinated. The COVID-19 vaccination rate is defined as the share of those individuals who received at least one dose of COVID-19 vaccine by the time of their interview in July and/or August 2022. Depending on whether the number of doses received was less than, equal to or more than the dose requirement of the primary series vaccination, we further divided vaccinated individuals into three groups: incomplete vaxers; primary series vaxers; and booster vaxers.
The CHARLS data included basic sociodemographics, including age, sex, marital status, ethnic origins, education, Hukou residence in the rural or urban household registry and regional residence. We divided the sample into four age groups: 52–59; 60–69; 70–79; and older than 80. Marital status was classified as married and unmarried (single or widowed). Ethnicity consisted of Han and other minority ethnic groups referred to as non-Han. Educational attainment was divided into three groups: illiterate; literate or primary school graduates; and those educated to middle school level or higher. Urban residents were defined by their non-agricultural resident status when they first entered the study. Regional residence followed the official definition of four mega-regions: northeast; east; central; and west.
Health measures included 12 diagnosed chronic disorders reported by the interviewees. We used self-reported disorders because the decision to be vaccinated would be based on the information known to the respondent. We selected six basic ADLs and five instrumental activities of daily living (IADLs) to define a variable of ‘ADL/IADL dependency’ as needing help to perform at least one of these activities38. This variable of functional dependency indicates a severe health condition and poor accessibility to vaccine clinics. For each of the chronic conditions, we constructed a binary indicator of incidence, that is, 1 for having the disorder and 0 for not having the disorder.
Unvaccinated interviewees offered highly detailed reasons for their decision. Aside from selecting one or more among the ten preset choices, respondents were allowed to provide further explanations or give any reasons not listed in the questionnaire. All open-ended answers were typed into the computer-aided personal interview immediately by the interviewers. A total of 3,436 in 2021 and 856 in 2022 unvaccinated respondents answered the question regarding their reasons for not being vaccinated. We conducted a textual analysis of these open-ended answers by searching for keywords related to each reason. The search order was determined by the reliability of a reason to be identified using its related keyword(s). Overall, we identified ten different reasons not listed as preset choices and further classified a total of 20 reasons into nine categories.
Statistical analysis
We calculated vaccination rates at the national level, and in the different demographic groups; we also provided statistics for primary series vaxers and booster vaxers. We calculated the share of each self-reported reason among those unvaccinated.
To examine the vaccination factors, we fitted a logistic regression to model the vaccination decision:
| (1) |
where yi is a binary indicator of whether an older adult i received at least one dose as of July/August 2022, xij is the j explanatory variable in the regression representing the sociodemographic factors and health measures. We estimated standard errors by clustering the sample at the household level to account for within-household correlations. The same model was applied when studying the outcomes of primary series vaccination and booster shots.
To maintain the same sample between the descriptive and regression analyses, we imputed a few tens of missing sociodemographic factors, chronic disease incidence and ADL dependencies (Extended Data Table 8).
We examined the dynamics of vaccinations by analyzing the vaccination status of individuals interviewed twice (collected in 2021 and 2022). There were two waves of vaccine campaigns initiated by the Chinese government. The first was in the middle of 2021 and was aimed at the entire adult population. The second wave started in October 2021, lasted for another 6 months and focused on older adults. These two waves coincided with the two phases of the fifth wave of CHARLS (2021–2022), so we constructed a multinomial logit regression model to study whether a person’s first-dose vaccination occurred in phase 1, phase 2 or in neither phase. Comparing vaccination outcomes between the two phases can shed light on the effectiveness of the government’s vaccination policy.
The regression framework of the multinomial logit regression model is as follows:
| (2) |
where β(1) = 0. We specified three outcomes: unvaccinated (yi = 1); vaccinated at phase 2 (yi = 2); or vaccinated at phase 1 (yi = 3). The explanatory variables are the same as in the logistic model for binary choice. The value of this multinomial model lies in the comparison of associations with late (phase 2) vaccination relative to early (phase 1) vaccination.
All statistical analyses were performed with Stata v.17.0.
Extended Data
EDI Figure 1.

A comparison of vaccination rates between the sources of CHARLS and China's National Health Committee (NHC)
Table A1.
Vaccination rate by age group, gender, rural/urban residence, and education group.
| Age group | ||||||||
|---|---|---|---|---|---|---|---|---|
| 52–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80+ | Total | |
| % | % | % | % | % | % | % | % | |
| Gender | ||||||||
| Male | 96.8 | 95.1 | 97.0 | 95.9 | 94.9 | 92.1 | 80.7 | 94.5 |
| Female | 97.2 | 95.9 | 95.4 | 93.4 | 92.7 | 88.1 | 78.0 | 93.0 |
| Hukou | ||||||||
| Rural (Agricultural) | 97.4 | 96.1 | 96.0 | 95.5 | 94.2 | 92.8 | 80.4 | 94.6 |
| Urban (Non-Agricultural) | 95.8 | 93.7 | 96.6 | 92.0 | 92.8 | 83.4 | 76.7 | 91.5 |
| Education group | ||||||||
| Illiterate | 96.7 | 95.3 | 96.4 | 95.2 | 94.1 | 90.6 | 76.1 | 91.8 |
| Literate | 99.0 | 95.6 | 96.2 | 96.0 | 92.5 | 90.6 | 81.6 | 94.0 |
| Primary school graduates | 96.1 | 96.3 | 93.8 | 92.8 | 94.4 | 92.8 | 83.8 | 94.0 |
| Middle school graduates | 98.1 | 95.0 | 95.9 | 94.4 | 95.9 | 90.9 | 84.8 | 95.2 |
| High school and above graduates | 95.0 | 95.6 | 97.5 | 94.0 | 90.6 | 77.3 | 74.0 | 93.6 |
| Total | 97.0 | 95.5 | 96.2 | 94.6 | 93.8 | 89.9 | 79.1 | 93.7 |
Note: Rates are calculated with our post-stratification weights that were constructed based on the non-response adjusted weights by CHARLS. Vaccination is defined as having received at least one dose of COVID-19 vaccine.
Table A2.
Determinants of vaccination status among older adults: a separate analysis by using individual health measures in 2018
| Dependent variable in logistic regression | Vaccination (at least one dose) vs. the unvaccinated | Primary series recipients vs. others | Booster recipients vs. others | |||
|---|---|---|---|---|---|---|
| (n/mean of dep. variable) | n=12900 | mean=.939 | n=12900 | mean=.913 | n=12900 | mean=.773 |
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Female | 0.85 (0.72–1.00) | 0.045 | 0.84 (0.73–0.96) | 0.012 | 0.94 (0.87–1.03) | 0.179 |
| Married | 1.52 (1.27–1.83) | 0.000 | 1.39 (1.19–1.64) | 0.000 | 1.20 (1.07–1.35) | 0.003 |
| Ethnic minorities | 0.92 (0.65–1.30) | 0.654 | 0.69 (0.53–0.90) | 0.006 | 0.65 (0.55–0.79) | 0.000 |
| Urban Hukou | 0.60 (0.49–0.73) | 0.000 | 0.70 (0.59–0.84) | 0.000 | 0.96 (0.85–1.09) | 0.551 |
| Age group (ref. 52–59) | ||||||
| Age 60–69 | 0.99 (0.78–1.25) | 0.925 | 0.88 (0.72–1.08) | 0.228 | 0.85 (0.75–0.96) | 0.012 |
| Age 70–79 | 0.73 (0.57–0.93) | 0.012 | 0.61 (0.49–0.76) | 0.000 | 0.62 (0.54–0.71) | 0.000 |
| Age 80+ | 0.30 (0.23–0.40) | 0.000 | 0.23 (0.18–0.29) | 0.000 | 0.24 (0.20–0.29) | 0.000 |
| Education (ref. illiterate) | ||||||
| Primary school (literate) | 1.09 (0.90–1.32) | 0.393 | 0.95 (0.80–1.12) | 0.545 | 1.04 (0.93–1.16) | 0.500 |
| Middle and high school + | 1.20 (0.95–1.53) | 0.129 | 1.19 (0.96–1.46) | 0.106 | 1.14 (0.99–1.30) | 0.065 |
| Region (ref. East) | ||||||
| Central | 1.07 (0.88–1.31) | 0.467 | 1.28 (1.07–1.52) | 0.006 | 1.14 (1.01–1.29) | 0.034 |
| West | 1.47 (1.19–1.81) | 0.000 | 1.35 (1.13–1.62) | 0.001 | 1.26 (1.11–1.43) | 0.000 |
| Northeast | 1.31 (0.95–1.82) | 0.101 | 1.17 (0.88–1.55) | 0.282 | 0.88 (0.72–1.07) | 0.203 |
| Functionally dependent | 0.51 (0.42–0.61) | 0.000 | 0.52 (0.44–0.61) | 0.000 | 0.67 (0.60–0.76) | 0.000 |
| Chronic conditions | ||||||
| Hypertension | 0.75 (0.64–0.88) | 0.001 | 0.73 (0.64–0.84) | 0.000 | 0.83 (0.76–0.92) | 0.000 |
| Heart diseases | 0.79 (0.65–0.95) | 0.014 | 0.84 (0.71–0.99) | 0.041 | 0.94 (0.84–1.06) | 0.326 |
| Stroke | 0.71 (0.55–0.92) | 0.009 | 0.72 (0.57–0.90) | 0.005 | 0.77 (0.65–0.92) | 0.003 |
| Diabetes | 0.84 (0.67–1.05) | 0.135 | 0.76 (0.63–0.92) | 0.006 | 0.84 (0.73–0.96) | 0.013 |
| Lung diseases | 0.76 (0.61–0.94) | 0.013 | 0.83 (0.69–1.01) | 0.058 | 0.98 (0.85–1.12) | 0.750 |
| Cancer | 0.29 (0.20–0.43) | 0.000 | 0.36 (0.25–0.51) | 0.000 | 0.51 (0.38–0.67) | 0.000 |
| Dyslipidaemia | 1.02 (0.84–1.23) | 0.866 | 1.11 (0.94–1.31) | 0.229 | 1.07 (0.95–1.21) | 0.256 |
| Liver diseases | 1.34 (0.95–1.90) | 0.097 | 1.24 (0.93–1.67) | 0.142 | 1.07 (0.89–1.28) | 0.466 |
| Kidney diseases | 0.92 (0.71–1.21) | 0.565 | 1.02 (0.80–1.29) | 0.886 | 1.20 (1.01–1.42) | 0.035 |
| Asthma | 0.82 (0.60–1.12) | 0.220 | 0.84 (0.64–1.10) | 0.201 | 0.78 (0.64–0.96) | 0.017 |
| Arthritis/rheumatism | 1.49 (1.25–1.77) | 0.000 | 1.40 (1.21–1.62) | 0.000 | 1.16 (1.05–1.28) | 0.003 |
| Digestive disease | 1.09 (0.92–1.30) | 0.326 | 1.11 (0.96–1.29) | 0.165 | 1.17 (1.05–1.29) | 0.003 |
| Constant | 19.76 (13.91–28.07) | 0.000 | 16.23 (11.98–21.98) | 0.000 | 4.34 (3.53–5.32) | 0.000 |
Note: Health measures, including functional dependency and chronic disease incidence, were from the 2018 wave. Other specifications are same as in Table 2. Standard errors are clustered at the household level. OR stands for odds ratio.
Table A3.
Determinants of vaccination status among older adults: a separate analysis by using the sample observed in both phases
| Dependent variable in logistic regression | Vaccination (at least one dose) vs. the unvaccinated | Primary series recipients vs. others | Booster recipients vs. others | |||
|---|---|---|---|---|---|---|
| (n/mean of dep. variable) | n=9882 | mean=.920 | n=9882 | mean=.893 | n=9882 | mean=.758 |
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Female | 0.81 (0.69–0.97) | 0.018 | 0.82 (0.71–0.95) | 0.009 | 0.91 (0.83–1.00) | 0.061 |
| Married | 1.54 (1.27–1.87) | 0.000 | 1.40 (1.17–1.67) | 0.000 | 1.18 (1.03–1.35) | 0.018 |
| Ethnic minorities | 0.83 (0.58–1.20) | 0.322 | 0.68 (0.51–0.90) | 0.008 | 0.61 (0.49–0.75) | 0.000 |
| Urban Hukou | 0.52 (0.43–0.64) | 0.000 | 0.61 (0.50–0.73) | 0.000 | 0.89 (0.77–1.03) | 0.113 |
| Age group (ref. 52–59) | ||||||
| Age 60–69 | 1.05 (0.83–1.33) | 0.684 | 0.95 (0.76–1.17) | 0.617 | 0.88 (0.76–1.02) | 0.087 |
| Age 70–79 | 0.85 (0.66–1.09) | 0.202 | 0.70 (0.56–0.87) | 0.001 | 0.65 (0.55–0.76) | 0.000 |
| Age 80+ | 0.39 (0.29–0.52) | 0.000 | 0.29 (0.22–0.38) | 0.000 | 0.26 (0.21–0.32) | 0.000 |
| Education (ref. illiterate) | ||||||
| Primary school (literate) | 0.99 (0.81–1.22) | 0.954 | 0.89 (0.74–1.06) | 0.184 | 1.00 (0.88–1.13) | 0.968 |
| Middle and high school+ | 1.05 (0.82–1.35) | 0.691 | 1.07 (0.85–1.33) | 0.566 | 1.11 (0.95–1.30) | 0.175 |
| Region (ref. East) | ||||||
| Central | 0.91 (0.74–1.11) | 0.350 | 1.08 (0.89–1.30) | 0.429 | 1.01 (0.88–1.16) | 0.890 |
| West | 1.43 (1.15–1.79) | 0.001 | 1.28 (1.06–1.55) | 0.011 | 1.24 (1.07–1.43) | 0.004 |
| Northeast | 1.34 (0.96–1.88) | 0.083 | 1.17 (0.87–1.58) | 0.287 | 0.97 (0.78–1.21) | 0.769 |
| Functionally dependent | 0.28 (0.24–0.34) | 0.000 | 0.30 (0.25–0.35) | 0.000 | 0.44 (0.38–0.50) | 0.000 |
| Chronic conditions | ||||||
| Hypertension | 0.86 (0.73–1.01) | 0.062 | 0.82 (0.71–0.95) | 0.007 | 0.83 (0.75–0.92) | 0.001 |
| Heart diseases | 0.59 (0.49–0.72) | 0.000 | 0.70 (0.59–0.83) | 0.000 | 0.83 (0.73–0.94) | 0.003 |
| Stroke | 0.70 (0.54–0.90) | 0.006 | 0.73 (0.58–0.92) | 0.008 | 0.74 (0.61–0.89) | 0.002 |
| Diabetes | 0.79 (0.64–0.98) | 0.028 | 0.77 (0.64–0.93) | 0.006 | 0.88 (0.77–1.02) | 0.084 |
| Lung diseases | 0.73 (0.58–0.91) | 0.005 | 0.87 (0.71–1.06) | 0.159 | 0.98 (0.84–1.14) | 0.769 |
| Cancer | 0.26 (0.19–0.35) | 0.000 | 0.29 (0.22–0.39) | 0.000 | 0.43 (0.33–0.56) | 0.000 |
| Dyslipidaemia | 1.19 (0.98–1.45) | 0.076 | 1.13 (0.95–1.35) | 0.159 | 1.06 (0.94–1.20) | 0.358 |
| Liver diseases | 0.92 (0.66–1.28) | 0.615 | 0.89 (0.66–1.19) | 0.425 | 0.98 (0.79–1.21) | 0.830 |
| Kidney diseases | 0.71 (0.55–0.93) | 0.013 | 0.75 (0.60–0.96) | 0.020 | 0.99 (0.82–1.19) | 0.882 |
| Asthma | 0.93 (0.69–1.26) | 0.652 | 0.87 (0.66–1.14) | 0.319 | 0.83 (0.67–1.03) | 0.088 |
| Arthritis/rheumatism | 1.43 (1.19–1.71) | 0.000 | 1.35 (1.15–1.58) | 0.000 | 1.13 (1.01–1.26) | 0.029 |
| Digestive disease | 1.17 (0.97–1.40) | 0.107 | 1.26 (1.06–1.48) | 0.007 | 1.23 (1.10–1.38) | 0.000 |
| Constant | 20.25 (14.06–29.15) | 0.000 | 16.57 (11.96–22.94) | 0.000 | 5.02 (3.98–6.34) | 0.000 |
Note: Other specifications are same as in Table 2. Standard errors are clustered at the household level. OR stands for odds ratio. The imputation of some variables fails because very few missing values are present and the dummy indicator of missing values can predict an outcome perfectly. As a result, the sample size is eight short of the size 9,890 in Table 3, that is also based on the sample observed in both phases.
Table A4.
Determinants of vaccination status among older adults: an analysis of using a comorbidity measure counting the number of major conditions
| Dependent variable in logistic regression | Vaccination (at least one dose) vs. the unvaccinated | Primary series recipients vs. others | Booster recipients vs. others | |||
|---|---|---|---|---|---|---|
| (n/mean of dep. variable) | n=12900 | mean=.939 | n=12900 | mean=.913 | n=12900 | mean=.773 |
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Female | 0.82 (0.70–0.97) | 0.019 | 0.81 (0.71–0.93) | 0.002 | 0.93 (0.85–1.01) | 0.068 |
| Married | 1.52 (1.26–1.83) | 0.000 | 1.40 (1.19–1.65) | 0.000 | 1.20 (1.06–1.35) | 0.003 |
| Ethnic minorities | 0.91 (0.64–1.28) | 0.571 | 0.68 (0.52–0.88) | 0.003 | 0.64 (0.54–0.77) | 0.000 |
| Urban Hukou | 0.62 (0.51–0.76) | 0.000 | 0.73 (0.61–0.87) | 0.000 | 0.98 (0.87–1.12) | 0.787 |
| Age group (ref. 52–59) | ||||||
| Age 60–69 | 1.00 (0.79–1.27) | 0.972 | 0.89 (0.73–1.09) | 0.278 | 0.85 (0.75–0.97) | 0.015 |
| Age 70–79 | 0.78 (0.61–1.00) | 0.051 | 0.64 (0.52–0.80) | 0.000 | 0.64 (0.55–0.73) | 0.000 |
| Age 80+ | 0.36 (0.27–0.48) | 0.000 | 0.27 (0.21–0.34) | 0.000 | 0.27 (0.22–0.32) | 0.000 |
| Education (ref. illiterate) | ||||||
| Primary school (literate) | 1.03 (0.85–1.25) | 0.786 | 0.91 (0.77–1.07) | 0.244 | 1.01 (0.91–1.13) | 0.823 |
| Middle and high school + | 1.16 (0.91–1.48) | 0.231 | 1.15 (0.94–1.42) | 0.179 | 1.11 (0.97–1.27) | 0.126 |
| Region (ref. East) | ||||||
| Central | 1.08 (0.89–1.32) | 0.434 | 1.29 (1.08–1.54) | 0.004 | 1.15 (1.02–1.30) | 0.026 |
| West | 1.52 (1.23–1.87) | 0.000 | 1.40 (1.17–1.67) | 0.000 | 1.30 (1.14–1.47) | 0.000 |
| Northeast | 1.38 (0.99–1.91) | 0.057 | 1.22 (0.92–1.62) | 0.170 | 0.91 (0.74–1.10) | 0.327 |
| Functionally dependent | 0.29 (0.24–0.34) | 0.000 | 0.31 (0.26–0.36) | 0.000 | 0.44 (0.39–0.50) | 0.000 |
| Chronic conditions | ||||||
| Comorbidity | 0.82 (0.79–0.86) | 0.000 | 0.85 (0.81–0.89) | 0.000 | 0.92 (0.89–0.94) | 0.000 |
| Arthritis/rheumatism | 1.46 (1.23–1.73) | 0.000 | 1.39 (1.20–1.61) | 0.000 | 1.17 (1.06–1.28) | 0.002 |
| Digestive disease | 1.13 (0.95–1.34) | 0.184 | 1.22 (1.05–1.42) | 0.011 | 1.22 (1.10–1.35) | 0.000 |
| Constant | 22.90 (16.20–32.39) | 0.000 | 17.53 (12.98–23.67) | 0.000 | 4.58 (3.73–5.61) | 0.000 |
Note: Other specifications are same as in Table 2. Standard errors are clustered at the household level. OR stands for odds ratio. The variable “Comorbidity” counts the number of the ten major conditions, including hypertension, heart diseases, stroke, diabetes, lung diseases, cancer, dyslipidaemia, liver diseases, kidney diseases, and asthma.
Table A5.
Determinants of early, late and non-vaccination: a separate analysis by using individual health measures in 2018
| Multinomial logit regression Dep. variable with three outcomes (one used as the base outcome) |
Phase 1 vaccination from Jan 2021 to summer 2021 vs. unvaccinated | Phase 2 vaccination from summer 2021 to summer 2022 vs. unvaccinated | Phase 2 vaccination vs. phase 1 vaccination | |||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | ||||
| n=9890 | n=9890 | n=9890 | ||||
| RRR (95% CI) | p value | RRR (95% CI) | p value | RRR (95% CI) | p value | |
| Female | 195.00 (0.70–1.00) | 66.000 | 0.85 (0.70–1.02) | 0.081 | 1.01 (0.90–1.13) | 0.850 |
| Married | 28.00 (1.38–2.01) | 10.000 | 1.39 (1.13–1.70) | 0.001 | 0.83 (0.73–0.95) | 0.008 |
| Ethnic minorities | 6.00 (0.44–0.84) | 2.000 | 1.42 (1.02–1.98) | 0.037 | 2.35 (1.95–2.84) | 0.000 |
| Urban Hukou | 184.00 (0.46–0.68) | 57.000 | 0.39 (0.31–0.49) | 0.000 | 0.70 (0.60–0.83) | 0.000 |
| Age group (ref. 52–59) | ||||||
| Age 60–69 | 44.00 (0.74–1.18) | 9.000 | 2.07 (1.58–2.72) | 0.000 | 2.22 (1.88–2.61) | 0.000 |
| Age 70–79 | 114.00 (0.49–0.80) | 28.000 | 2.21 (1.67–2.91) | 0.000 | 3.51 (2.96–4.15) | 0.000 |
| Age 80+ | 340.00 (0.13–0.22) | 34.000 | 1.54 (1.14–2.09) | 0.005 | 9.07 (7.34–11.21) | 0.000 |
| Education (ref. illiterate) | ||||||
| Primary school (literate) | 0.06 (0.88–1.30) | 0.077 | 1.03 (0.84–1.27) | 0.767 | 0.97 (0.85–1.10) | 0.611 |
| Middle and high school + | 0.01 (0.92–1.49) | 0.012 | 0.90 (0.69–1.17) | 0.422 | 0.77 (0.65–0.90) | 0.001 |
| Region (ref. East) | ||||||
| Central | 0.05 (0.73–1.07) | 0.067 | 0.98 (0.79–1.20) | 0.823 | 1.10 (0.96–1.26) | 0.159 |
| West | 0.30 (1.11–1.69) | 0.185 | 1.58 (1.26–1.98) | 0.000 | 1.15 (1.01–1.32) | 0.037 |
| Northeast | 0.01 (0.77–1.47) | 0.011 | 2.02 (1.43–2.84) | 0.000 | 1.90 (1.55–2.31) | 0.000 |
| Functionally dependent | 0.03 (0.34–0.50) | 0.033 | 0.64 (0.52–0.78) | 0.000 | 1.55 (1.35–1.78) | 0.000 |
| Chronic conditions | ||||||
| Hypertension | 0.08 (0.60–0.85) | 0.064 | 0.92 (0.76–1.10) | 0.347 | 1.28 (1.14–1.44) | 0.000 |
| Heart diseases | 0.74 (0.61–0.90) | 0.002 | 0.78 (0.63–0.97) | 0.022 | 1.06 (0.92–1.22) | 0.436 |
| Stroke | 0.60 (0.46–0.79) | 0.000 | 0.85 (0.64–1.13) | 0.256 | 1.41 (1.15–1.72) | 0.001 |
| Diabetes | 0.79 (0.63–0.99) | 0.043 | 0.97 (0.76–1.24) | 0.815 | 1.23 (1.05–1.45) | 0.012 |
| Lung diseases | 0.75 (0.60–0.95) | 0.017 | 0.81 (0.63–1.04) | 0.104 | 1.08 (0.92–1.27) | 0.353 |
| Cancer | 0.29 (0.20–0.43) | 0.000 | 0.39 (0.25–0.62) | 0.000 | 1.35 (0.92–1.99) | 0.129 |
| Dyslipidaemia | 1.01 (0.82–1.23) | 0.937 | 0.94 (0.75–1.17) | 0.588 | 0.93 (0.81–1.08) | 0.343 |
| Liver diseases | 1.29 (0.91–1.83) | 0.153 | 1.43 (0.98–2.07) | 0.062 | 1.11 (0.89–1.37) | 0.363 |
| Kidney diseases | 0.96 (0.73–1.26) | 0.747 | 0.81 (0.60–1.10) | 0.174 | 0.85 (0.70–1.03) | 0.105 |
| Asthma | 0.77 (0.55–1.08) | 0.135 | 0.83 (0.58–1.19) | 0.308 | 1.07 (0.84–1.37) | 0.584 |
| Arthritis/rheumatism | 1.59 (1.33–1.90) | 0.000 | 1.27 (1.05–1.53) | 0.014 | 0.80 (0.71–0.90) | 0.000 |
| Digestive disease | 1.12 (0.93–1.35) | 0.215 | 1.00 (0.82–1.21) | 0.965 | 0.89 (0.78–1.00) | 0.052 |
| Constant | 14.57 (10.21–20.80) | 0.000 | 1.67 (1.12–2.48) | 0.011 | 0.11 (0.09–0.15) | 0.000 |
Note: Health measures, including functional dependency and chronic disease incidence, were from the 2018 wave. Standard errors are clustered at the household level. RRR stands for relative risk ratio. Phase 1 is from January 2021 to July 2021, the early period when the vaccination had not been available for more than 6 months; Phase 2, from September 2021 to July 2022, is the later period. Main column (3) only changed the base outcome, so the RRRs were quotients between those from column (2) and column (1). Summer is the survey season of CHARLS, mostly spanning from July to August.
Table A6.
Reasons for non-vaccination among participants having not received COVID-19 vaccine
| Reasons for non-vaccination | Summer 2021 | Summer 2022 |
|---|---|---|
| n=3436 | n=856 | |
| Having contraindications | 30% | 48% |
| Old, frail, or with specific health conditions | 25% | 21% |
| Access problems* | 22% | 18% |
| Concerns about the side effect or efficacy | 6% | 9% |
| Never heard of the COVID-19 vaccine | 8% | 6% |
| Low chance of COVID-19 infection | 3% | 4% |
| Rejected by vaccinators (rather than the above reasons) | 5% | 2% |
| Unwilling to get vaccinated (rather than the above reasons) | 4% | 3% |
| Other# | 6% | 2% |
“Access problems” comprised the following reasons: vaccine sites were far from home (long travel) or couldn’t be located; individual mobility; local communities did not arrange vaccinations; short supply; and vaccination was not free.
“Other” comprised the following reasons: fear of injection, being busy or absent from home, and vaccination had been scheduled at the interview time.
Note: Reason categories were aggregated from 20 more detailed types (Table A8, next page). The sum of shares can be greater than 100% because the interviewees may answer more than one category of reasons. The indicator “comorbid” represents having more than one of the ten major conditions, including hypertension, heart diseases, stroke, diabetes, lung diseases, cancer, dyslipidaemia, liver diseases, kidney diseases, and asthma. Summer is the survey season of CHARLS, mostly spanning from July to August.
Table A7.
More detailed reasons for non-vaccination by respondent age group
| 2022 | 2021 | |||||||
|---|---|---|---|---|---|---|---|---|
| 52–59 | 60–69 | 70–79 | 80+ | 52–59 | 60–69 | 70–79 | 80+ | Self-reported reason for non-vaccination |
| n=147 | n=209 | n=264 | n=236 | n=517 | n=1060 | n=1153 | n=706 | |
| % | % | % | % | % | % | % | % | |
| 5.4% | 9.6% | 6.8% | 8.5% | 9.5% | 5.4% | 5.6% | 3.4% | Side effect |
| 1.4% | 1.0% | 0.4% | 2.1% | 1.7% | 0.8% | 0.7% | 0.3% | Effectiveness concern |
| 0.7% | 0.0% | 0.0% | 0.4% | 0.2% | 0.1% | 0.3% | 0.0% | Vaccination is not free |
| 4.1% | 5.7% | 7.2% | 8.5% | 2.7% | 4.5% | 6.2% | 7.2% | Long travel to the vaccine clinic |
| 19.7% | 23.9% | 19.7% | 11.4% | 42.0% | 34.7% | 28.7% | 17.0% | Contraindications (2021) |
| Self-decision due to contraindications (2022) | ||||||||
| 40.8% | 40.7% | 34.1% | 23.3% | n/a | n/a | n/a | n/a | Rejected due to contraindications (2022) |
| 2.7% | 0.0% | 0.8% | 1.3% | 1.5% | 1.7% | 1.2% | 0.6% | Concern of vaccine injection |
| 2.7% | 1.4% | 3.4% | 5.1% | 2.5% | 3.7% | 3.7% | 2.7% | Unaware of the clinic location to get vaccinated |
| 2.7% | 3.8% | 5.3% | 3.4% | 7.2% | 10.6% | 9.8% | 11.0% | No organized vaccination event in local communities |
| 3.4% | 6.2% | 6.1% | 8.9% | 4.3% | 7.2% | 8.7% | 11.8% | Never heard of the vaccine |
| 4.8% | 4.3% | 5.3% | 7.2% | 2.3% | 2.5% | 3.4% | 5.7% | Low mobility |
| 17.7% | 18.2% | 11.4% | 5.1% | 15.3% | 10.9% | 8.8% | 4.7% | Health conditions |
| 2.0% | 1.0% | 4.2% | 6.8% | 2.9% | 2.2% | 2.7% | 2.7% | Low chance of infection |
| 0.0% | 0.5% | 0.0% | 0.4% | 1.0% | 2.5% | 2.0% | 0.4% | Vaccination already scheduled, but not received yet |
| 1.4% | 0.0% | 1.9% | 0.0% | 7.2% | 4.4% | 1.3% | 0.7% | Being busy or absent |
| 0.7% | 0.0% | 0.0% | 0.0% | 2.5% | 3.1% | 1.4% | 1.4% | Waiting for a smaller queue |
| 7.5% | 3.3% | 3.4% | 3.4% | 3.1% | 2.9% | 3.5% | 3.3% | Frailty (not mentioning a specific condition) |
| 4.1% | 0.5% | 1.9% | 3.4% | 1.2% | 3.8% | 6.9% | 7.6% | Rejected (for any reason not listed above) |
| 0.0% | 0.0% | 2.7% | 14.0% | 0.6% | 7.0% | 14.7% | 23.8% | Being old (not mentioning health conditions or frailty) |
| 1.4% | 1.9% | 4.2% | 4.7% | 4.4% | 3.6% | 3.4% | 5.0% | Unwilling (for any reason not listed above) |
Note: The upper panel shows the ten reasons preset in the questionnaire. The lower panel shows the ten reasons categorized from open-ended answers provided by the respondents. The sum of shares can be greater than 100% because the interviewees may answer more than one category of reasons.
Table A8.
Number of missing values for the explanatory variables in regression
| Number of missing values | |
|---|---|
| Married | 20 |
| Ethnic minorities | 79 |
| Functionally dependent | 45 |
| Chronic conditions | |
| Hypertension | 39 |
| Heart diseases | 39 |
| Stroke | 39 |
| Diabetes | 39 |
| Lung diseases | 39 |
| Cancer | 39 |
| Dyslipidaemia | 39 |
| Liver diseases | 39 |
| Kidney diseases | 39 |
| Asthma | 40 |
| Arthritis/rheumatism | 40 |
| Digestive disease | 40 |
Notes: We imputed missing values by adding a binary dummy indicator for the variable whenever multi-linearity did not occur.
Acknowledgements
We acknowledge grants from the National Institute on Aging (no. R01-AG037031), the Natural Science Foundation of China (nos. 72061137005, 72173008, 81903392, 71603013, 71873010) and the China Medical Board (no. 20-364). The funders had no role in study design, data collection, management, analysis, interpretation of data and writing of the manuscript. We thank L. Ren, S. Li and Y. Hu from the China Center for Health Development Studies at Peking University for assisting with the literature search, policy data extraction and preparation of the figures.
Footnotes
Online content
Any methods, additional references, Nature Portfolio reporting summaries, source data, extended data, supplementary information, acknowledgements, peer review information; details of author contributions and competing interests; and statements of data and code availability are available at https://doi.org/10.1038/s41591-023-02241-7.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Code availability
The code for this study is available on GitHub at https://github.com/econwang/covid19-vax.
Competing interests
The authors declare no competing interests.
Extended data is available for this paper at https://doi.org/10.1038/s41591-023-02241-7.
Supplementary information The online version contains supplementary material available at https://doi.org/10.1038/s41591-023-02241-7.
Data availability
The fifth wave of the CHARLS data is scheduled to be released within 2 years after the fieldwork is completed. The public release files will be available for download from its official website: https://charls.pku.edu.cn/en/.
References
- 1.Johns Hopkins University Coronavirus Resource Center. Global map of COVID-19 deaths (2022); https://coronavirus.jhu.edu/map.html
- 2.Lazarus JV et al. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun 13, 3801 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wan EYF et al. Safety of an inactivated, whole-virion COVID-19 vaccine (CoronaVac) in people aged 60 years or older in Hong Kong: a modified self-controlled case series. Lancet Healthy Longev. 3, e491–e500 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor L Covid-19: Hong Kong reports world’s highest death rate as zero covid strategy fails. BMJ 376, o707 (2022). [DOI] [PubMed] [Google Scholar]
- 5.Hou Z et al. Influenza vaccination hesitancy and its determinants among elderly in China: a national cross-sectional study. Vaccine 40, 4806–4815 (2022). [DOI] [PubMed] [Google Scholar]
- 6.Persad G et al. Public perspectives on COVID-19 vaccine prioritization. JAMA Netw. Open 4, e217943 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Privor-Dumm LA et al. A global agenda for older adult immunization in the COVID-19 era: a roadmap for action. Vaccine 39, 5240–5250 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen X et al. The path to healthy ageing in China: a Peking University-Lancet Commission. Lancet 400, 1967–2006 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Euronews. China expands lockdowns as COVID-19 cases hit daily record (2022); https://www.npr.org/2022/11/24/1139147636/china-expands-lockdowns-as-covid-19-cases-hit-daily-record
- 10.State Department COVID-19 Prevention and Control Mechanism Integrated Group. Notice on further optimization of the implementation of measures for the prevention and control of the COVID-19 outbreak (2022); http://www.gov.cn/xinwen/2022-11/11/content_5726122.htm
- 11.Zhang Y, Wang Y, Ning G, He P & Wang W Protecting older people: a high priority during the COVID-19 pandemic. Lancet 400, 729–730 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Sinovac CoronaVac [Vero Cell]- inactivated, COVID-19 vaccine (2021); https://www.who.int/publications/m/item/sinovac-coronavac-vero-cell---inactivated-covid-19-vaccine
- 13.National Medical Products Administration of China. China NMPA grants approval for CanSinoBIO’s Covid-19 vaccine as booster (2022); https://www.pharmaceutical-technology.com/news/nmpa-cansinobio-covid-vaccine/
- 14.China News Weekly. Why are the country’s ‘vulnerable’ older adults resisting vaccinations? (2022); https://mp.weixin.qq.com/s/pfSYcrtkK7QvyGkdzZqh4A
- 15.National Health Commission of China. Questions and answers about the COVID-19 vaccination for children aged 3–11 years (2021); http://www.nhc.gov.cn/xcs/s7847/202111/79103c66c2de404b8e50583816f5e31e.shtml
- 16.Bureau of Disease Control and Prevention, National Health Commission of China. Guideline for the normalization of prevention and control related to the Covid-19 epidemic in key places, key units and key populations (2021); http://www.nhc.gov.cn/jkj/s5898bm/202108/ead4082ee97b49a38a8512e112f53dbf.shtml
- 17.National Health Commission of China. Vaccination program for the older people against Covid-19 (2022); http://www.nhc.gov.cn/xcs/gzzcwj/202211/9bb71c9c7d664fb0bbcd2b3eaaefcf84.shtml
- 18.Diesel J et al. COVID-19 vaccination coverage among adults—United States, December 14, 2020–May 22, 2021. MMWR Morb. Mortal. Wkly. Rep 70, 922–927 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luk TT et al. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: a population-based survey. Vaccine 39, 3602–3607 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Veronese N et al. Prevalence of unwillingness and uncertainty to vaccinate against COVID-19 in older people: a systematic review and meta-analysis. Ageing Res. Rev 72, 101489 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olivera Mesa D et al. Modelling the impact of vaccine hesitancy in prolonging the need for non-pharmaceutical interventions to control the COVID-19 pandemic. Commun. Med 2, 14 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergmann M, Hannemann T-V, Bethmann A & Schumacher AT Determinants of SARS-CoV-2 Vaccinations in the 50+ Population (Mea-Munich Center for the Economics of Aging, 2021). [Google Scholar]
- 23.Yu Y, Lau MMC, Jiang H & Lau JTF Prevalence and factors of the performed or scheduled COVID-19 vaccination in a Chinese adult general population in Hong Kong. Vaccines 9, 847 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gong F et al. Impact of media use on Chinese public behavior towards vaccination with the COVID-19 vaccine: a latent profile analysis. Vaccines 10, 1737 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagner AL et al. Vaccine hesitancy and concerns about vaccine safety and effectiveness in Shanghai, China. Am. J. Prev. Med 60, S77–S86 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lazarus JV et al. A multinational Delphi consensus to end the COVID-19 public health threat. Nature 611, 332–345 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwarzinger M, Watson V, Arwidson P, Alla F & Luchini S COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health 6, e210–e221 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freeman D et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med 52, 3127–3141 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma A & Parry J When Hong Kong’s ‘dynamic zero’ covid-19 strategy met omicron, low vaccination rates sent deaths soaring. BMJ 377, o980 (2022). [DOI] [PubMed] [Google Scholar]
- 30.Zhang D et al. Vaccine resistance and hesitancy among older adults who live alone or only with an older partner in community in the early stage of the fifth wave of COVID-19 in Hong Kong. Vaccines 10, 1118 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okubo R, Yoshioka T, Ohfuji S, Matsuo T & Tabuchi T COVID-19 vaccine hesitancy and its associated factors in Japan. Vaccines 9, 662 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siu JY, Cao Y & Shum DHK Perceptions of and hesitancy toward COVID-19 vaccination in older Chinese adults in Hong Kong: a qualitative study. BMC Geriatr. 22, 288 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rotenberg S et al. COVID-19 vaccination for people with disabilities. Science Briefs of the Ontario COVID-19 Science Advisory Table (2021); 10.47326/ocsat.2021.02.35.1.0; https://covid19-sciencetable.ca/sciencebrief/covid-19-vaccination-for-people-with-disabilities/ [DOI] [Google Scholar]
- 34.Giles J, Lei X, Wang G & Zhao Y One country, two systems: evidence on retirement patterns in China. J. Pension Econ. Finan 10.1017/S1474747221000391 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Health Commission of China. Authoritative response: can elderly people with chronic diseases get vaccinated? (2022); http://www.gov.cn/fuwu/2022-12/07/content_5730559.htm
- 36.Leung K, Lau EHY, Wong CKH, Leung GM & Wu JT Estimating the transmission dynamics of SARS-CoV-2 Omicron BF.7 in Beijing after the adjustment of zero-COVID policy in November–December 2022. Nat. Med 10.1038/s41591-023-02212-y (2023). [DOI] [PubMed] [Google Scholar]
- 37.Zhao Y, Hu Y, Smith JP, Strauss J & Yang G Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol 43, 61–68 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gong J et al. Nowcasting and forecasting the care needs of the older population in China: analysis of data from the China Health and Retirement Longitudinal Study (CHARLS). Lancet Public Health 7, e1005–e1013 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The fifth wave of the CHARLS data is scheduled to be released within 2 years after the fieldwork is completed. The public release files will be available for download from its official website: https://charls.pku.edu.cn/en/.


