Abstract
Background:
The prevalence of uncontrolled type 2 diabetes has been increasing, and the nurse is a primary healthcare provider to patients when health professionals are scarce in the community setting. A feasible intervention delivered by nurses is necessary to fulfill patients’ needs to help them achieve glycemic control.
Aim:
To investigate whether Thai adults with uncontrolled diabetes in community hospitals lack self-care competency and whether a nurse-led supportive education program can enhance their self-care skills, change behavior, and control HbA1C levels.
Methods:
We employed a multi-community hospital cluster randomized controlled trial design. Participants were randomly selected in the experimental group (2 hospitals) and control group (2 hospitals), with 30 patients from each hospital. One hundred twenty adults with HbA1c 7—10% treated by oral glycemic medication were recruited. Using Orem’s Theory as a framework, nurses implemented self-care deficit assessments and supportive-educative nursing programs into their work. Participants in the control group received usual care, and those in the experimental group underwent a nurse assessment and supportive education measures. Data were collected at baseline, with 4-week and 12-week follow-ups. Data analysis were a repeated measures ANOVA with post hoc analysis, and Independent t-test.
Results:
One hundred three patients completed the trial (51 in the experimental group and 52 in the control group). At 12 weeks, there were statistically significant improvements in HbA1c (P < .001), fasting plasma glucose (P = .03), knowledge (P < .001), diabetes self-care agency (P < .001), diet consumption (P < .001), physical activity (P < .001), and medical adherence (P = .03) in the experimental group significantly greater than those in the control group. Also, the between-group effect sizes were 0.49 or greater.
Conclusion:
The self-care deficit assessment and supportive education program were essential to the nursing intervention that effectively improved knowledge, changed behavior, and HbA1c levels among adults with uncontrolled blood glucose.
Keywords: community, diabetes, HbA1c, nurse, Orem’s self-care theory
Introduction
Type 2 diabetes mellitus (T2DM) is a severe chronic disease globally, particularly in lower-income countries. 1 Diabetes self-management education and support (DSME/S) has been documented as a successful intervention for HbA1c improvement and behavior change through healthy eating, being active, and medication adherence.2-4 It is an accepted intervention used for years for Thai adults with diabetes. However, the adult prevalence of uncontrolled T2DM is still high, estimated at 64% in diabetic patients. 5 Specifically, self-care in adults with diabetes is complicated because they live with a chronic illness with long-term treatment and require specific practice based on their illness conditions and environment.6-8 This suggests there may be a need for self-care assistance, such as knowledge and self-care skills through eating habits, physical activity, and medical adherence to maintain their health and well-being.9,10
Enhancing adults’ competence in their diabetes self-care and maintaining such behavior is the greatest challenge particularly in the community setting. The nurse is an essential health professional to assist patients in ensuring glycemic improvements through developing practical diabetes self-care to secure various clinical outcomes.11-13 Most past studies have focused on providing education, self-care management, and emotional support with nurse training conducted to ensure the quality of healthcare and education delivery. Previous reviews of nurse-led interventions suggested that supporting nurses beyond initial training can build their confidence to enhance intervention delivery.14,15
According to Orem’s Self-Care Deficit Nursing Theory (SCDNT), nurses foster essential care skills based on a person’s self-care deficits. One’s self-care agency is the self-care ability of a person to engage in self-care operations and is developed through a learning process. Information regarding everyday self-care actions and capabilities is assessed for nurses to determine the cause of problems and change activities to improve one’s self-care ability. 16 In the case of adults with uncontrolled diabetes, nurses can identify self-care limitations and reduce self-care deficits. This is consistent with a meta-analysis and systematic review, which indicated that, successfully implementing DSME/S into the community healthcare service requires nurses to train and practice assessing patients’ self-care needs, acknowledge patients’ decision-making skills, and the development of supportive education plans to foster actions and guide patients to competence in diabetes self-care. 17
Community health nurses are crucial in assisting patients to continue daily self-care to maintain health and well-being in community areas of Thailand, where there is a limited healthcare workforce to perform effective healthcare service. 18 Consequently, nurses’ descriptions of practically integrated self-care deficit assessment and supportive education programs into routine care provided by nurses are limited. Therefore, our study aimed to evaluate whether Thai adults with uncontrolled diabetes in community hospitals lack self-care competency and whether a nurse-led supportive education program can enhance their self-care skills, change behavior, and control HbA1C levels.
Methods
This cluster randomized controlled trial was conducted from October 2021 to May 2022 in 4 community hospitals.
Study Population
The sample size was calculated using the G*Power program, and the primary study outcome was the HbA1c level with the power set at 0.8 and the effect size based on a previous study (d = .56). 19 A α value of .05 was used to calculate the sample size, yielding a sample size of 51 persons per group. With an attrition rate of 20%, the total number was 60 persons per group.
The recruitment process was conducted in 2 steps. The first step involved the selection of community hospitals as units to avoid contamination among participants. Two provinces were selected, and 9 community hospitals were in these 2 provinces. Four were selected by cluster randomization and allocated for the experiment (2 hospitals) and control groups (2 hospitals). These hospitals provided similar diabetes clinic services, where a physician provided physical assessment and treatment, whereas teaching, guiding, and consultation was mainly provided by registered nurses.
For the second step, adults with type 2 diabetes who received care at the diabetes clinics in 4 community hospitals were assessed for eligibility. Inclusion criteria included adults with an HbA1c level of 7 to 10% and taking oral glycemic medication. The exclusion criteria were those prescribed insulin injections, were pregnant or had a severe illness or accidental injury, which would be barriers to performing healthy behaviors. After signing the consent form, eligible participants were asked to consent to HbA1c testing. If they met the inclusion criteria, they were invited to complete the baseline questionnaires and enroll in the program. The researcher continued to recruit participants at the clinics until there were 30 participants per hospital.
Before the study began, 4 registered nurses (a nurse per clinic) who have the responsibility to deliver care in diabetes clinics were invited to participate in the study. All nurses were asked to provide usual care to participants and were blinded to their study group. Nurses in the experimental groups were trained and conduct the trial with mentoring by the researcher.
Training for Nurses
Two nurses in the experimental group were asked to attend a 12-hour training on patient self-care deficit assessment and supportive education methods. The first 3-hour were an overview of diabetes self-management and support based on the diabetes clinical practice guidelines and literature reviews20-22 along with 3-hour discussions on the problems they usually faced. A booklet regarding diabetes and its complications, signs and symptoms management, and recommended behavior change for HbA1c improvement developed by the researchers was included for teaching and mentoring patients to ensure the quality of program delivery.
In another 3-hour training, the self-care deficits assessment and supportive education program were discussed and practiced by nurses with mentoring from the researcher. The self-care deficits assessment initially focused on patient health deviation of self-care requisites such as blood glucose testing, diabetes knowledge, decision-making skills, and self-care, including diet consumption, active physical activity, and medication adherence. Then, a supportive education program was practiced, including goal planning, disease information, and expected behavior change skills. Then, nurses were asked to try this assessment and the program with their patients and discuss it with the researchers. This process was approximately 3 hours.
Four semi-structured questions for self-care deficit assessment were developed by the researchers with the purpose of quick screening before teaching and guiding patients. The questions were validated regarding self-care management and healthy behavior by a diabetes physician, nutritionist, and nurse in the diabetes clinic. The content validity index (CVI) was 0.96. Then, adults with diabetes were asked to give feedback on their understanding of the questions. They were as follows; “what is diabetes, and how do you manage symptoms if you have hypoglycemia?” “What kind of food do you like to have?” “What type of activities do you usually perform?” “Have you ever forgotten to take medication?”
Patients in the experimental group received the study intervention delivered by nurses for 4 weeks, while those in the control group received the usual care. Also, exit interviews with approximately 30 minutes were conducted with participants and community health nurses.
Intervention
The nurse-led supportive education program is based on Orem’s Self-Care Deficit Nursing Theory (SCDNT). At week 1, participants were assessed for deficits in self-care based on the study guideline (10 minutes). If they had insufficient knowledge or lacked decision-making skills, they discussed barriers to performing behaviors with nurses. Then, they received education for 60 minutes: general information about diabetes, signs and symptoms management, self-care practice focusing on diet consumption, physical activity, and medication adherence. Next, they received skills training, which was approximately 60 minutes. The food model was used during a skill practice session to indicate the types and portions of diet they should have for 1 meal.
In contrast, exercise with an elastic band was demonstrated to increase physical activity, and in short scenarios, media was used to enhance medication adherence. All participants were asked to maintain consumption suggested by the nutrition flags, exercise at least 3 days a week, and take medications according to the prescription. Details were provided in the patient booklet and validated by a physician, a pharmacist, a diabetes nurse care manager, and a nutritionist. Then, goals for behavior change were established, and activity plans were discussed among nurses and patients (20 minutes). All activities in this session were approximately 2 hours and 30 minutes.
In week 4, patients repeated the assessment of self-care deficits and skills (5–10 minutes). Then, barriers to performing behavioral change goals based on evaluations were discussed. Self-care knowledge, including diet, physical activity, and medication taking, was reviewed (30 minutes). Then, they received diet consumption skills practice using food models to increase their decision-making skills in choosing suitable kinds and amounts of food (30 minutes). Also, a change goal was set, and their activity plan was adjusted based on their needs (20 minutes). This session was about 1 hour and 30 minutes. Additional calls from nurses were offered at week 8 if participants’ assessments showed improper behavior change. However, none of the participants reported problems with behavior change.
Usual Care
Participants in the control group received routine care based on Thai diabetes clinical practice guidelines that involved symptoms and self-care management. After their physician appointments, patients received education individually on diabetes and expected behaviors to reduce blood glucose levels, which lasted 5 to 10 minutes based on available time.
Outcomes
The trial duration was 12 weeks. The experimental and control groups received fasting plasma glucose testing and answered the questionnaires at baseline, 4 weeks, and 12 weeks. Also, HbA1c was assessed at baseline and week 12.
Personal information
This questionnaire was developed by the researcher and composed of body weight, blood pressure, age, gender, marital status, education level, occupation, income, family income, number of family members, position in the family, relationship in the family, duration of DM, and so on.
The researcher developed a knowledge of diabetes self-care questionnaire to assess an understanding of the disease, dietary consumption, physical activity, and medication adherence. It was ten items of true/false questions, where 1 was correct, and 0 was incorrect, with a CVI of .93 and a KR-20 reliability of .64.
The diabetes self-care agency questionnaire was an assessment using the Self-efficacy for Diabetes scale. 23 It examined patients’ confidence in certain self-care activities related to diabetes and included 8 items with responses “not at all confident” to “totally confident” on a 10-point Likert scale. It had a CVI of .92 and Cronbach’s alpha of .76.
Self-care questionnaire
This questionnaire assessed self-care activities related to controlling blood glucose. It consisted of 3 subscales as follows:
A dietary consumption questionnaire developed by Jantraporn et al 24 assessed eating habits during the past week. It is self-administered with 12 items. Responses included “None of the time” to “all of the time” on a 4-point Likert scale. Higher scores indicate more excellent dietary consumption behavior. It had a CVI of .97 and Cronbach’s alpha of .72.
Physical activity was examined using The Stanford Leisure-Time Activity Categorical Item (L-Cat), 25 with permission, and it has previously been used among Thai adults with diabetes. 26 It was a single item comprised of 6 activity categories describing common activity patterns differing in frequency, intensity, duration, and types of activities in the past month, with the score ranging from inactive to very active. It had a CVI of 1.00 and a test-retest reliability with intraclass correlation coefficients of .72 (95% CI: 0.61-0.80, P < .001).
With permission, the medication adherence questionnaire used the Hill-Bone Medication Adherence Scale (HB-MAS). 27 It assessed participants’ adherence to medication regimens through prescription refills. It measured 9 items, with responses including “none of the time” to “more than four times/week” on a 4-point Likert scale. It had a CVI of 1.0 and Cronbach’s alpha of .79.
Statistical Analysis
All analyses used the Statistical Package for Social Science program (SPSS) for Windows (Version 24). Baseline demographic characteristics were descriptive, and chi-square and Fisher’s exact test were used to determine the difference between the groups for the categorical variables. A repeated measures ANOVA with post hoc analysis and Independent t-test was used to test between-group differences. Results were presented as estimated marginal means (95% CI). Cohen d was used to estimate the effect size, with value .2 defined as a small effect size, >.5 as a medium effect size, and >.8 as a large effect size. Statistical significance was reported at the .05 alpha level.
Results
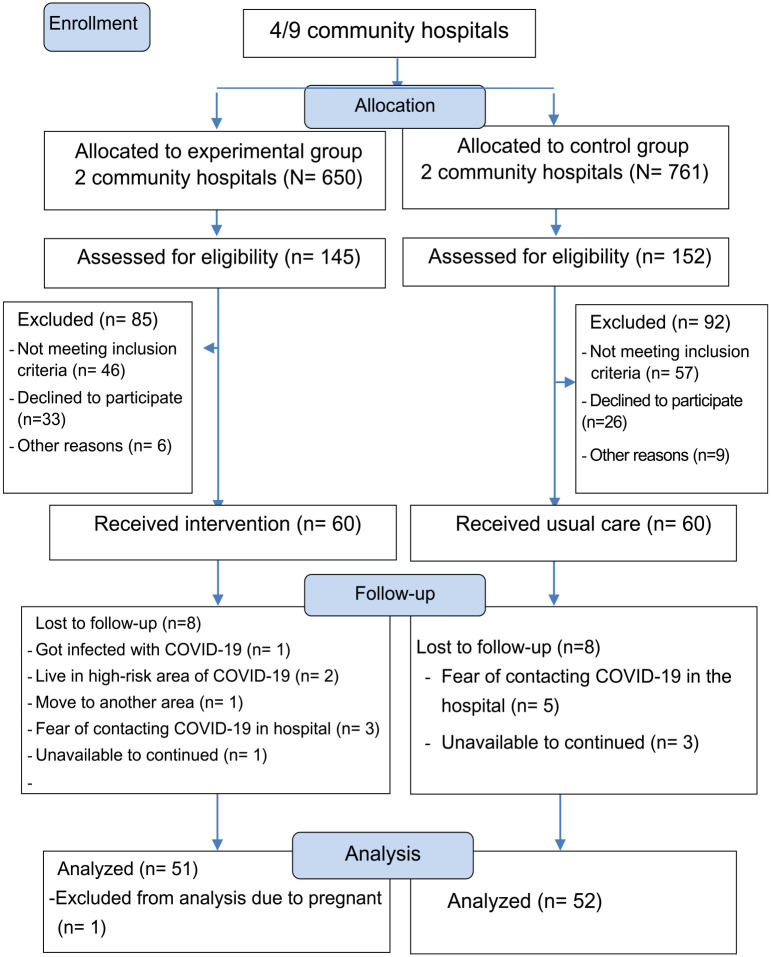
Two hundred ninety-seven participants from 4 community hospitals were initially assessed for eligibility, with 145 participants in the experimental and 152 in the control groups. One hundred twenty participants (60 in each group) were recruited. Eight patients in the experimental group were lost during the follow-up stage and excluded from the analysis. Eight patients in the control group were lost during follow-up. A participant who was pregnant was excluded. For the final analysis, 51 patients from the experimental and 52 from the control groups were considered (Figure 1).
Figure 1.
Consort flow diagram for enrollment and data analysis.
As shown in Table 1, the demographic characteristics of the participants were similar in the 2 groups. The differences between groups were insignificant except for diastolic blood pressure and the number of participants with comorbid hypertension and dyslipidemia. Participants were female (63.1%), finished primary school (49.5%), and employed (83.5%). The mean age of the sample was 50.9 (SD = 7.4) years, and the mean scores for all outcome variables at baseline did not differ between the groups (P > .05). The majority of them were diagnosed with T2DM alongside hypertension and dyslipidemia.
Table 1.
Characteristics of the Participants at Baseline.
| Variables | Total (n = 103) | Experimental group (n = 51) | Control group (n = 52) | P |
|---|---|---|---|---|
| Age (years), mean (SD) | 50.9 (7.4) | 50.3 (7.8) | 51.5 (6.9) | .43 a |
| Gender (female), n (%) | 65 (63.1) | 33 (64.7) | 32 (61.5) | .74 b |
| Status (married), n (%) | 79 (76.7) | 37 (72.5) | 42 (80.8) | .32 b |
| Education, n (%) | .73 b | |||
| Primary school | 51 (49.5) | 25 (49.0) | 26 (50.0) | |
| Secondary school | 20 (19.5) | 12 (23.5) | 8 (15.4) | |
| high school/diploma and higher | 32 (31.0) | 14 (27.5) | 18 (34.6) | |
| Occupation (employed), n (%) | 86 (83.5) | 44 (86.3) | 42 (80.8) | .45 b |
| Duration of DM (years), n (%) | .73 a | |||
| <5 | 61 (59.2) | 30 (58.8) | 31 (59.6) | |
| 5-10 | 30 (29.1) | 16 (31.4) | 14 (26.9) | |
| >10 | 12 (11.7) | 5 (9.8) | 7 (13.5) | |
| Min-max, mean (SD) | 5.2 (4.9) | 6 months-20 years 5.1 (4.8) | 6 months-20 years 5.4 (5.1) | |
| Comorbidity, n (%) | ||||
| None | 8 (7.8) | 1 (1.9) | 7 (13.5) | .06 c |
| DLP | 18 (17.5) | 6 (11.8) | 12 (23.1) | .13 b |
| HT | 16 (15.5) | 6 (11.8) | 10 (19.2) | .30 b |
| DLP and HT | 61 (59.2) | 38 (74.5) | 23 (44.2) | .002* b |
| BW (kg), mean (SD) | 72.1 (15.1) | 72.1 (15.4) | 72.1 (15.0) | 1.00 a |
| SBP (mmHg), mean (SD) | 132.6 (11.8) | 131.9 (11.7) | 133.3 (12.1) | .54 a |
| DBP (mmHg), mean (SD) | 78.9 (8.4) | 81.0 (7.9) | 76.9 (8.5) | .01* a |
| Knowledge, mean (SD) | 8.2 (1.2) | 8.1 (1.3) | 8.2 (1.1) | .68 |
| DSCA, mean (SD) | 46.8 (15.7) | 48.6 (14.7) | 45.1 (16.6) | .26 |
| Diet consumption, mean (SD) | 32.6 (5.21) | 32.8 (4.7) | 32.4 (5.7) | .67 |
| Physical activity, mean (SD) | 2.1 (0.9) | 1.9 (0.8) | 2.1 (1.0) | .38 |
| Med adherence, mean (SD) | 34.3 (1.9) | 34.3 (2.0) | 34.4 (1.9) | .70 |
| FBG, mean (SD) | 181.1 (55.1) | 180.8 (57.6) | 181.4 (53.1) | .96 |
| HbA1c, mean (SD) | 8.31 (0.9) | 8.5 (0.9) | 8.2 (1.0) | .12 |
Abbreviations: BW, body weight; DBP, diastolic blood pressure; DLP, dyslipidemia; DSCA, diabetes self-care agency; FBG, fasting blood glucose; HbA1c, glycated hemoglobin; HT, hypertension; SBP, systolic blood pressure.
Independent t-test.
Chi square test.
Fisher’s exact test.
P < .05.
A significant improvement in knowledge, diabetes self-care agency, dietary consumption behavior, and physical activity was observed in the experimental group compared to the control group at week 4. It was maintained to week 12, with a significant Cohen d effect size of at least 1.0 between groups (all P < .001). Also, the intervention was more effective in diastolic blood pressure and medication adherence only at week 12 (all P = .03), with a small effect size (Cohen d < .5). (Table 2)
Table 2.
Estimated Marginal Mean Changes From Baseline to 4 and 12 weeks.
| Variables | Experimental group (n = 51) EMM (95% CI) | Control group (n = 52) EMM (95% CI) | Between group difference, Mean (95%CI) | P a | Cohen d between groups |
|---|---|---|---|---|---|
| BW | |||||
| 4 week | −0.0 (−0.6, 0.5) | −0.3 (−1.0, 0.3) | 0.3 (−0.4, 1.0) | .38 | 0.37 |
| 12 weeks | 0.3 (−0.5, 1.3) | 0.7 (−0.1, 1.6) | −0.4 (−1.4, 0.6) | .45 | 0.02 |
| SBP | |||||
| 4 week | −0.8 (−5.0, 3.4) | 2.4 (−2.7, 7.6) | −3.2 (−8.6, 2.1) | .23 | 0.30 |
| 12 weeks | −2.1 (−7.1, 2.9) | 0.5 (−4.4, 5.5) | −2.6 (−8.3, 3.0) | .36 | 0.30 |
| DBP | |||||
| 4 week | −0.4 (−4.0, 3.3) | 3.4 (0.0, 6.8) | −3.8 (−7.8, 0.2) | .06 | 0.05 |
| 12 weeks | −1.9 (−6.0, 2.2) | 3.3 (−0.9, 7.4) | −5.2 (−9.8, −0.5) | .03* | 0.12 |
| Knowledge | |||||
| 4 week | 1.4** (0.9, 1.9) | −0.2 (−0.7, 0.4) | 1.6 (1.0, 2.1) | <.001** | 1.34 |
| 12 weeks | 1.9** (1.4, 2.3) | 0.0 (−0.4, 0.5) | 1.9 (1.4, 2.4) | <.001** | 2.53 |
| DSCA | |||||
| 4 weeks | 14.6** (9.4, 19.8) | 1.7 (−3.2, 6.6) | 12.9 (7.2, 18.7) | <.001** | 1.33 |
| 12 weeks | 20.1** (15.2, 24.9) | 2.6 (−3.5,8.8) | 17.5 (11.2, 23.6) | <.001** | 1.77 |
| Diet consumption | |||||
| 4 weeks | 4.4** (2.8, 6.0) | 0.4 (−1.0, 1.8) | 4.0 (2.4, 5.7) | <.001** | 1.08 |
| 12 weeks | 5.9** (3.9, 7.8) | 0.7 (−0.9, 2.7) | 5.2 (3.2, 7.3) | <.001** | 1.12 |
| Physical activity | |||||
| 4 weeks | 1.1** (0.7, 1.4) | −0.2 (−0.6, 0.3) | 1.3 (1.2, 1.9) | <.001** | 1.02 |
| 12 weeks | 1.2** (0.9, 1.5) | −0.5 (−0.8, −0.1) | 1.7 (1.3, 2.1) | <.001** | 1.92 |
| Medical adherence | |||||
| 4 weeks | 0.8* (0.1, 1.5) | 0.1 (−0.6, 0.8) | 0.7 (−0.1, 1.5) | .09 | 0.30 |
| 12 weeks | 1.2* (0.5, 1.8) | 0.1 (−0.8, 1.0) | 1.1 (0.1, 1.9) | .03* | 0.49 |
| FBG | |||||
| 4 weeks | −27.6* (−45.2, −9.9) | −5.2 (−23.8, 13.6) | −22.4 (−43.0, −1.9) | .03* | 0.49 |
| 12 weeks | −27.1* (−45.4, −8.9) | −2.8 (−23.7, 18.1) | −24.3 (−46.6, −2.0) | .03* | 0.56 |
| HbA1c | |||||
| 12 weeks | −0.7 (−0.9, −0.4) | 0.4 (0.1, 0.7) | −1.1 (−1.5, −0.7) | <.001** | 0.68 |
| P b | < .001** | .01* | |||
Abbreviations: BW, body weight; DBP, diastolic blood pressure; DSCA, diabetes self-care agency; EMM, estimated marginal mean.; FBS, fasting blood glucose; HbA1c, glycated hemoglobin; SBP, systolic blood pressure.
Independent t-test.
paired t-test;
P < .05. **P < .001.
Fasting plasma glucose was significantly decreased in the experimental group, with 51 participants (EMM −27.6, CI −45.2, −9.9) compared to those in the control group, with 52 participants in week 4 (EMM −5.2, CI −23.8, 13.6; P = .03) and maintaining more significant reductions in week 12 (P = .03). Comparing the mean HbA1c at baseline and 12 weeks; the HbA1c was reduced by the mean of 0.7% (P < .001). Compared to the control group, experimental group participants reported more significant reductions in HbA1c at week 12 (P < .001), with a medium Cohen d effect size of at least .5 between groups.
Among participants, 52.9% (27/51) in the experimental group reported HbA1c reduction by at least 0.5% compared to 15.3% (8/52) participants in the control group. However, a quarter of participants in the experimental group (13/51, 25.5%) reported worsening HbA1c levels (Table 3). All participants had no change in glucose-lowering medication.
Table 3.
Changes of HbA1c From Baseline to 12 weeks.
| Experimental group | Control group | |
|---|---|---|
| n (%) | n (%) | |
| Improved | ||
| ≥1% | 20 (39.2) | 6 (11.5) |
| 0.9-0.5% | 7 (13.7) | 2 (3.8) |
| 0.1-0.4% | 9 (17.7) | 8 (15.4) |
| No change | 2 (3.9) | 4 (7.7) |
| Exacerbation | 13 (25.5) | 32 (61.6) |
Exit Interview
Exit interviews of 13 participants and 2 nurses from the experimental group were conducted. Participants reported satisfaction with the individual self-care agency (SCA) assessment, followed by nurses’ guidance, support, and teaching according to patient deficit needs. Most participants began to control their food habits, exercise, and diabetic medicines, and they became aware of medication side effects they had not known about. In addition, they learned from others by sharing information and speaking out more quickly. The nurses felt the program was beneficial for adults with diabetes and valuable to them. Also, the program helped them to review their knowledge and increased their confidence in providing diabetes care.
Discussion
In this trial, a nurse-led supportive education program compared with usual care resulted in significant behavior changes such as food habits, active physically, medical adherence, and clinically relevant improvement in fasting blood glucose and HbA1c in patients with uncontrolled type 2 diabetes, which is consistent with previous studies.28,29 Findings were consistent with a recent systematic review of 34 articles from 16 countries, concluding that nurse-led interventions showed a significant lowering of HbA1c in adults with diabetes, ranging from 0.03% to 2.0%. 30 Also, the findings supported the Self-Care Deficit Nursing Theory (SCDNT) that patients with uncontrolled diabetes should be helped to overcome deficits to meet their needs for self-care when they come to the hospital, and that nurses have the primary role of coordinating patient care to help them do so.
Differences in the characteristics of participants’ dyslipidemia and hypertension between groups at baseline might have an impact on the overall results. Previous study has shown that diabetic adults with hypertension and dyslipidemia were more likely to have negative attitudes towards self-care activity, which lead to less behavior change in diet and physical activity. 31 In the study, information of diabetes-related complication (cardiovascular disease: CVD) and CVD risk factors (dyslipidemia and hypertension) that participants received might make them fear a greater risk of mortality if they had greater level of dyslipidemia and hypertension, lacking adherence to healthy self-care practice. Therefore, they actively focused on eating grains, vegetables, and unsweetened fruits, and increased physical activity. This is consistent with findings that adults with diabetes who perceived high risk of complications were more likely to engage in self-care practice. 32 However, the study did not directly identify an effect of the dyslipidemia and hypertension on behavior change. Future research may further investigate the potential impact of different levels of lipid parameters in patients with diabetes on behavior change.
Interestingly, adequate medication adherence was observed only at week 12, with a small effect size. It is consistent with a systematic review of the effects of nurse-led interventions on medication adherence in adults with metabolic syndrome, which reported a small effect size when the interventions were carried out using guidelines/protocol/script. In contrast, education/discussion showed a moderate effect size on medication adherence. 33 This moderate effect size might be explained by the time constraints for guidance and unclear supportive education material about the medication regimen. Findings suggest the need for additional medication support for nurses to supervise patients and user-friendly material for medication regimens for patients.
The findings demonstrated the feasibility of implementing a nurse-led supportive education program in a community hospital. Approximately 85% of participants completed the intervention in both groups (51/60 in the experimental group and 52/60 in the control group), and compliance with the intervention was observed based on self-care deficits assessment and HbA1c reduction, which means the program was acceptable to this population. Also, results from exit interviews supported participant program satisfaction, and nurses reported the possibility of the program integration into routine work. Nurses indicated that with limited time and a scarce healthcare workforce in the community hospitals, this assessment and the program intervention allowed them to discuss with each patient quickly and provide confidence in teaching and behavior guidance.
In the experimental group, 8 participants dropped out in the week 12 follow-up study. Although it is considered an acceptable number based on the sample size calculation, improving participants’ adherence in further research is crucial. The study’s main reason was that it was conducted during the pandemic of COVID-19 and patients feared to get infected during clinical visits, which is consistent with previous studies that vulnerable populations such as elderly and adults with diabetes who feared COVID-19 exposure were less likely to attend healthcare services or delay care.34,35 This suggests a need to develop interventions to remotely deliver face-to-face and scaled-up digital technology, user-friendly for participants with low education.
The study has strength in the randomized controlled trial and was implemented over 12 weeks, which was enough time to yield the results. Also, the study was based on the Self-Care Deficit Nursing Theory (SCDNT), which initially involved nurses in assessing patients’ needs and the work necessary to support patients’ knowledge and skills to perform self-care actions. However, some limitations of the study for generalization should be noted. First, the majority of participants were women with low educational levels. Although supporting education material was prepared for patients who were middle-aged and had only finished primary school for readability and understanding before starting the intervention, there might be some reading barriers. Further studies are needed to develop material with concise content and bigger fonts. Secondly, the study period might be too short to evaluate the long-term effects of medication adherence.
Conclusion
Our nurse-led supportive education program benefitted high-risk adults with diabetes. The trial supports the feasibility of implementing a self-care deficit assessment and a nurse-led supportive education program for behavior changes and clinical relevance in community hospitals. Adults with uncontrolled diabetes reported satisfaction with the nurse-led program, and the intervention was practically integrated into the natural setting.
Footnotes
Author Contributions: PC, PP, SL, PL conceptualized, designed, and management of the study. PC, PP were responsible for delivering the intervention, collecting, and analyzing the data. PC, PP, SL, PL contributed to the interpretation and report on the study. PP, PC drafted and critical reviewed the manuscript. All authors approved the final version for submission.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported for research funding by National Research Council of Thailand (NRCT), partially supported by the Faculty of Graduate Studies and Graduate Studies of Mahidol University Alumni Association, Mahidol University, Bangkok, Thailand. Also, the study was partially supported for publication by Faculty of Public Health, Mahidol University, Bangkok, Thailand.
Ethical Consideration: Ethics approval was obtained from the Human Research Ethics Committee, Faculty of Public Health, Mahidol University (MUPH 2020-164). The study procedures were conducted following the Declaration of Helsinki. They were free to answer the questionnaires or withdraw anytime without compromising their care from the health providers and the hospitals.
Trial Registration: The Thai Clinical Trials (clinical registration number TCTR20220217003; https://www.thaiclinicaltrials.org/show/TCTR20220217003).
ORCID iD: Panan Pichayapinyo  https://orcid.org/0000-0002-5320-5291
https://orcid.org/0000-0002-5320-5291
References
- 1.Kaiser AB, Zhang N, der Pluijm WV.Global prevalence of type 2 diabetes over the next ten years (2018-2028). Diabetes. 2018;67(1):202. [Google Scholar]
- 2.Del Prato S, Felton AM, Munro N, Nesto R, Zimmet P, Zinman B.Improving glucose management: ten steps to get more patients with type 2 diabetes to glycaemic goal: recommendations from the global partnership for effective diabetes management. Int J Clin Pract. 2005;59(11):1345-1355. [DOI] [PubMed] [Google Scholar]
- 3.Ernawati U, Wihastuti TA, Utami YW.Effectiveness of diabetes self-management education (DSME) in type 2 diabetes mellitus (T2DM) patients: systematic literature review. J Public Health Res. 2021;10(2):2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dube L, Van den Broucke S, Housiaux M, Dhoore W, Rendall-Mkosi K.Type 2 diabetes self-management education programs in high and low mortality developing countries: a systematic review. Diabetes Educ. 2015;41(1):69-85. [DOI] [PubMed] [Google Scholar]
- 5.Sakboonyarat B, Pima W, Chokbumrungsuk C, et al. National trends in the prevalence of glycemic control among patients with type 2 diabetes receiving continuous care in Thailand from 2011 to 2018. Sci Rep. 2021;11(1):14260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kolb L.Association of Diabetes Care & Education Specialists. An effective model of diabetes care and education: the ADCES7 self-care behaviors™. Sci Diabetes Self Manag Care. 2021;47(1):30-53. [DOI] [PubMed] [Google Scholar]
- 7.Monfared EL, Tehrani H, Teiho Z, Jafari A.The study of eye care behaviors in patients with type 2 diabetes. J Diabetes Metab Disord. 2020;19:257-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Powers MA, Bardsley JK, Cypress M, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. 2020;43(7):1636-1649. [DOI] [PubMed] [Google Scholar]
- 9.Lambrinou E, Hansen TB, Beulens JW.Lifestyle factors, self-management and patient empowerment in diabetes care. Eur J Prev Cardiol. 2019;26(2_suppl):55-63. [DOI] [PubMed] [Google Scholar]
- 10.Preechasuk L, Sriussadaporn P, Likitmaskul S.The obstacles to diabetes self-management education and support from healthcare professionals’ perspectives: a nationwide survey. Diabetes Metab Syndr Obes. 2019;12:717-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azami G, Soh KL, Sazlina SG, et al. Effect of a nurse-led diabetes self-management education program on glycosylated hemoglobin among adults with type 2 diabetes. J Diabetes Res. 2018;2018:4930157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tshiananga JK, Kocher S, Weber C, Erny-Albrecht K, Berndt K, Neeser K.The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Diabetes Educ. 2012;38(1):108-123. [DOI] [PubMed] [Google Scholar]
- 13.Welch G, Garb J, Zagarins S, Lendel I, Gabbay RA.Nurse diabetes case management interventions and blood glucose control: results of a meta-analysis. Diabetes Res Clin Pract. 2010;88(1):1-6. [DOI] [PubMed] [Google Scholar]
- 14.Nikitara M, Constantinou CS, Andreou E, Diomidous M.The role of nurses and the facilitators and barriers in diabetes care: a mixed methods systematic literature review. Behav Sci. 2019;9(6):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stephen C, McInnes S, Halcomb E.The feasibility and acceptability of nurse-led chronic disease management interventions in primary care: an integrative review. J Adv Nurs. 2018;74(2):279-288. [DOI] [PubMed] [Google Scholar]
- 16.Orem DE.Nursing Concepts of Practice. 6th ed.Mosby; 2001. [Google Scholar]
- 17.Massimi A, De Vito C, Brufola I, et al. Are community-based nurse-led self-management support interventions effective in chronic patients? Results of a systematic review and meta-analysis. PLoS One. 2017;12(3):e0173617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jithitikulchai T.Improving allocative efficiency from network consolidation: a solution for the health workforce shortage. Hum Resour Health. 2022;20:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zareban I, Niknami S, Hidarnia A, Rakhshani F, Shamsi M, Karimy M.Effective intervention of self-care on glycaemia control in patients with type 2 diabetes. Iran Red Crescent Med J. 2014;16(12):e8311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Diabetes Association. Standards of medical care in diabetes—2018. Abridged for primary care providers. Clin Diabetes. 2018;36(1):14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Waddell J.An update on type 2 diabetes management in primary care. Nurse Pract. 2017;42(8):20-29. [DOI] [PubMed] [Google Scholar]
- 22.Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American Association of Clinical Endocrinologists and American College of Endocrinology–clinical practice guidelines for developing a diabetes mellitus comprehensive care plan–2015—executive summary. Endocr Pract. 2015;21(4): 413-437. [PubMed] [Google Scholar]
- 23.Ritter PL, Lorig K, Laurent DD.Characteristics of the Spanish-and English-language self-efficacy to manage diabetes scales. Diabetes Educ. 2016;42(2):167-177. [DOI] [PubMed] [Google Scholar]
- 24.Jantraporn R, Pichayapinyo P, Lagampan S, Mayurasakorn K.Effects of carbohydrate reduction program and telemonitoring on glycosylated hemoglobin in patients with poorly controlled type 2 diabetes: a randomized controlled trial. J Med Assoc Thai. 2019;102(5):523-529. [Google Scholar]
- 25.Kiernan M, Schoffman DE, Lee K, et al. The Stanford Leisure-Time Activity Categorical Item (L-Cat): a single categorical item sensitive to physical activity changes in overweight/obese women. Int J Obes. 2013;37(12):1597-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pichayapinyo P, Saslow LR, Aikens JE, et al. Feasibility study of automated interactive voice response telephone calls with community health nurse follow-up to improve glycaemic control in patients with type 2 diabetes. Int J Nurs Pract. 2019;25(6):e12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim MT, Hill MN, Bone LR, Levine DM.Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs. 2000;15(3):90-96. [DOI] [PubMed] [Google Scholar]
- 28.Artha IM, Bhargah A, Dharmawan NK, et al. High level of individual lipid profile and lipid ratio as a predictive marker of poor glycemic control in type-2 diabetes mellitus. Vasc Health Risk Manag. 2019;15:149-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang S, Ji X, Zhang Z, Xue F.Relationship between lipid profiles and glycemic control among patients with type 2 diabetes in Qingdao, China. Int J Environ Rese Public Health. 2020;17(15):5317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holloway D, James S, Ekinci E, Craft J.Systematic review of the effectiveness of nurse-led care in reducing glycated haemoglobin in adults with Type 1 or 2 diabetes. Int J Nurs Pract. 2023:e13135. [DOI] [PubMed] [Google Scholar]
- 31.Silva ALDA, Santos CMS, Oliveira MVG, et al. Factors related to negative self-care adherence in individuals with diabetes mellitus. Rev Rene. 2021;22:e70902. [Google Scholar]
- 32.Nie R, Han Y, Xu J, Huang Q, Mao J.Illness perception, risk perception and health promotion self-care behaviors among Chinese patient with type 2 diabetes: a cross-sectional survey. Appl Nurs Res. 2018;39:89-96. [DOI] [PubMed] [Google Scholar]
- 33.Kim CJ, Kim M, Lee GY, Park E, Schlenk EA.Effectiveness of nurse-led interventions on medication adherence in adults taking medication for metabolic syndrome: a systematic review and meta-analysis. J Clin Nurs. Published online November 24, 2022. doi: 10.1111/jocn.16589 [DOI] [PubMed] [Google Scholar]
- 34.Sharifi N, Rezaei N, Fathnezhad-Kazemi A, Ghiasi F.Association between fear of COVID- 19 with self-care behaviors in elderly: a cross-sectional study. Soc Work Public Health. 2021;36(5):606-614. [DOI] [PubMed] [Google Scholar]
- 35.Purvis RS, Moore RA, Ayers BL, et al. Diabetes self-care behaviors and barriers to clinical care during COVID-19 pandemic for Marshallese adults. Sci Diabetes Self-Manag Care. 2022;48(1):35-43. [DOI] [PMC free article] [PubMed] [Google Scholar]