Abstract
Purpose
To understand malnutrition recovery at a Guatemalan Nutrition Rehabilitation Center (NRC) before and during the COVID-19 pandemic.
Design and methods
A retrospective chart review was conducted on-site in November 2022. The NRC is located on the outskirts of Antigua, Guatemala. They manage the care of 15–20 children at a time, providing food, medicine, and health assessments. A total of 156 records were included (126 prior to the onset of COVID; 30 after the onset of COVID). Descriptive variables collected were age, gender, severity of malnutrition, height, weight, amoxicillin, multivitamins, nebulizer/bronchodilator, and zinc.
Principal results
There was no significant difference in time-to-recovery between COVID cohorts. Mean time-to-recovery was 5.65 weeks, or 39.57 days (SD = 25.62, 95% CI [35.5, 43.7]) among all recovered cases (n = 149). The cohort admitted after the onset of COVID-19 (March 1, 2020) had a significantly higher weight gain and discharge weight. In the total sample, amoxicillin was the only significant predictor variable for recovery time; with children receiving it being more likely to recover in >6 weeks. The few differences between cohorts was possibly attributed to the sample after the onset of COVID-19. These records had minimal sociocultural data.
Major conclusions
Conducting a family needs assessment on admission could identify sociocultural factors that may facilitate nutritional recovery, such as housing conditions and potable water access. Further research is needed to more fully understand the complexities that the COVID-19 pandemic has had on childhood malnutrition recovery.
Keywords: Malnutrition, Time-to-recovery, Guatemala, Nutrition Rehabilitation Center
Introduction
Nearly half of all deaths of children under age five are linked to malnutrition.1 Severe Acute Malnutrition (SAM) puts children at greater risk of communicable diseases, delayed recovery and increased risk of complications.2 Children in low- and middle-income countries (LMIC) are disproportionately affected by SAM.3 Guatemala, a low-income country, has the highest rate of childhood malnutrition in Latin America, and fifth highest worldwide.4
Malnutrition in Guatemala
In a recent cross-sectional study of nine Latin American and Caribbean countries, Guatemala had the highest prevalence of growth stunting and number of households in rural areas.5 Socioeconomic and ethnic disparities of SAM within Guatemala are constant; children who identified as indigenous Maya, and living in poorer, rural areas are at greatest risk for SAM.6 , 7 The home environment contributes largely to child health; many Guatemalan homes do not have reliable access to potable water and sanitation.8 , 9 A controversial concept, maternal employment has had both positive and negative impacts on child health; there are potential financial benefits, but there is also uncertainty in the management of childcare and food preparation by someone other than the mother.10, 11, 12
Investigators have found community food assistance programs13 , 14 and home gardens,15 offered a solution to childhood malnutrition in Guatemala. However, there are concerns about sustainability of these types of interventions, since they require complementary strategies to achieve sustainability.15 Rohloff16 highlighted the need to reduce persistent health disparities, by recognizing social context and prioritizing families’ needs. Investigators must consider the impact of the sociocultural context on child health outcomes to eliminate malnutrition in Guatemala.
Impact of COVID-19
The World Health Organization (WHO) announced a global pandemic of the novel SARS-CoV2 virus in the Spring of 2020.17 The pandemic disproportionately impacted LMICs, placing an estimated 1.2 million Guatemalans in need of emergency food-aid; many faced loss of jobs and food insecurity from the closure of public transportation systems and open food markets.18 , 19 As the pandemic approaches its third year, young children from LMICs are at greatest risk of food insecurity and subsequent malnutrition.2 Overall, the onset of the pandemic threatens long-term sequela for undernourished children, particularly those who are marginalized, and has the potential to undo previous efforts to improve global nutrition.20
Nutritional standards and management
Nutritional standards for effective management of SAM are (a) a recovery rate of at least 75%, (b) a mortality rate less than 10%, (c) recovery within 6 weeks, and (d) children gaining ≥8 g/kg/day.21 , 22 In managing SAM, supplementation of vitamins and minerals, including zinc is recommended to improve outcomes.3 , 23 Oral amoxicillin is also recommended; yet, research on its use has had inconsistent findings, suggesting benefits21 , 24 and risks.25 , 26 Malnutrition severity is determined by the on-site nutritionist using height-for-weight. It is classified using the WHO child growth standards, defined as the number of standard deviations below the growth curve, with −1 SD as mild, −2 SD as moderate and −3 SD as severe.27 Children are considered ‘recovered’ when they are within the standard range for healthy weight based on weight-for-height.27
Malnutrition treatment interventions include Outpatient Treatment Programs (OTPs) and Nutrition Rehabilitation Centers (NRCs). In OTPs, children are assessed in a community-based setting, provided food and medications, in particular Ready-to-Use Therapeutic Food (RUTF), and managed at home with regular evaluation.28 In previous studies, time-to-recovery in OTPs ranged from 38.5 to 73 days; rates of weight gain were 4.2 −10.5 g/kg/day; and predictors of recovery included antibiotics,29 , 30 vitamins, lack of comorbidities when enroled in outpatient treatment,31 and admission weight greater than 7 kg.32 Community health workers (CHWs) often collaborate with OTPs to identify and refer at-risk children, as well as to independently manage acute cases within the community.33 The OTPs provide a means of local access for early intervention; however, these programs have not consistently achieved nutritional standards for recovery.28
In NRCs, malnourished children recover in a residential care setting that is monitored by healthcare professionals.34 The majority of studies on NRCs have been set in India. Rates of weight gain in these studies ranged from 3.8 to 9.92 g/kg/day.34, 35, 36 Despite the prevalence of NRCs in other countries, few studies have examined predictors of malnutrition recovery and none have been conducted in Guatemala. This is a unique setting in a country that could contribute to malnutrition recovery, making it an ideal setting to advance the science. Thus, the purpose of the study was to understand malnutrition recovery at a Guatemalan NRC before and during the COVID-19 pandemic.
Research questions
The research questions were: What impact has COVID-19 had on malnutrition recovery at an NRC in Guatemala? What relationships exist between individual clinical variables and time-to-recovery?
Material and methods
Design
A retrospective chart review was conducted in November 2021 to examine cases before and during the COVID-19 pandemic in order to evaluate the effects on malnutrition recovery. The research team consisted of a PhD nursing student (Principal Investigator) with primary proficiency in Spanish, biostatistician, and nursing professor with expertise in Latino population health; NRC leadership served as consultants. This study builds on a long-term community-university partnership and was approved by the university institutional review board (IRB # 21-001884).
Setting
The NRC is located on the outskirts of Antigua, Guatemala. Children are referred to the NRC by hospitals, health clinics, social services, or self-referral. The NRC staff are composed of nursing assistants, a nutritionist, and pediatrician. They manage the care of 15–20 children at a time, providing food, medicine, and health assessments. Family-centered care is encouraged, where mothers reside at the center to help care for their child.
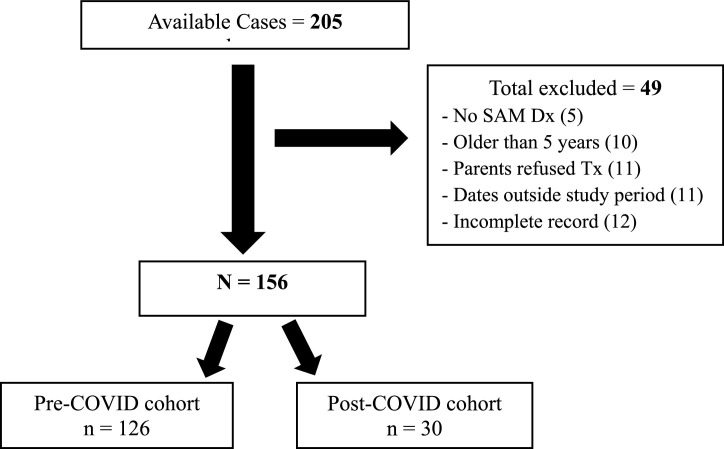
Sample
The sample consisted of the medical records (cases) of eligible children treated at the NRC from January 1, 2019 to December 31, 2020. Inclusion criteria were: ≤ 5 years of age upon admission; a diagnosis of acute, moderate, or severe malnutrition; and a discharge from the NRC within the study period. Cases were excluded if parents refused to complete treatment. Cases were classified by date of admission as either pre-COVID-19 (prior to March 1, 2020) or post-COVID-19 (after March 1, 2020). Data was verified with the NRC leadership as needed. There were 205 cases available; 49 were excluded, leaving a total sample of 156 cases (see Fig. 1 ).
Fig. 1.
NRC cases included and excluded in the study.
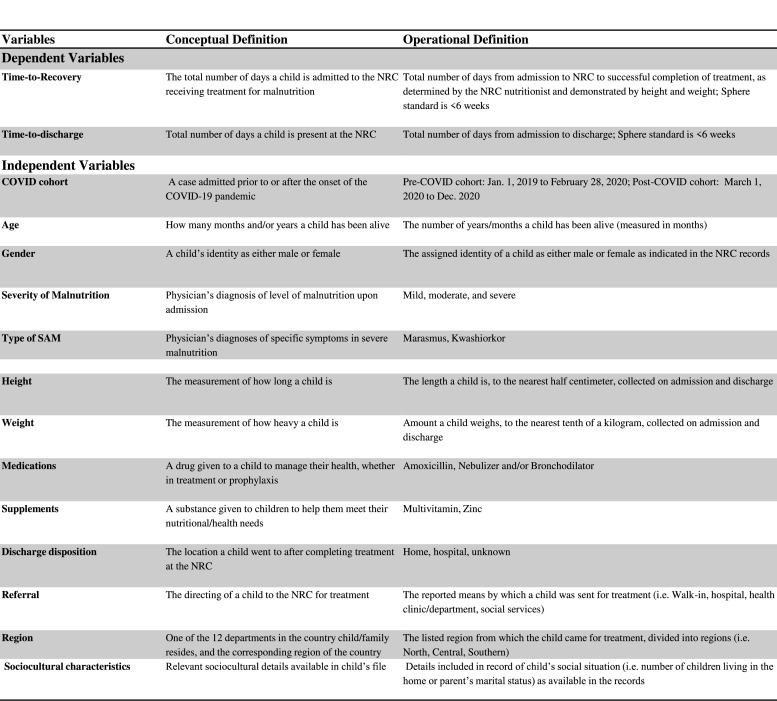
Measures
A structured audit tool, based on a pilot study,37 was developed for data entry. No records were removed or photographed; all data were deidentified. The primary outcome variable was time-to-recovery. Primary predictor variables were pre- and post-COVID cohort, age, gender, severity of malnutrition, and admission weight. Secondary predictor variables were use of amoxicillin, multivitamins, nebulizer/bronchodilator, and zinc (see Fig. 2 ). Secondary diagnoses were not available in the records.
Fig. 2.
Conceptual and operational definitions.
Data management and analytic strategy
Data were collected on-site at the NRC by the PI and records were given an identification number using year (19 or 20) and case (01, 02, 03, etc.) in ascending order; for example, 1901, 1902, or 2001, 2002. Data were uploaded and analyzed using SPSS v. 28 and SAS v. 9.4. Variables were coded, outliers and missing data were identified, discussed by the research team and managed appropriately. Coded variables were validated by two members of the research team to ensure accuracy. Excluding sociocultural factors, there was less than 1% missing data.
Descriptive statistics, Chi-Square tests, Student's t-tests, and multiple logistic regression were performed to answer the research questions (α = 0.05). Chi-square tests were done to analyze relationships between categorical variables. In some cases, Mantel-Haenszel Chi-square test was reported instead of the regular Chi-square when a categorical variable was not dichotomous. In cases where minimum expected counts were not met (≥5 in each cell), Fisher's or Mantel-Haenszel exact test was reported.
Theory
This study was guided by the Social Ecological Model,38 which informed the examination of the multilevel factors influencing childhood malnutrition. The model considers how health outcomes are shaped through the social context. Health outcomes are achieved from the interactions within and between the five levels (individual, interpersonal, organizational, community, and public policy), which continuously interact with one another.38 Data collected in this study were analyzed within the framework of the model to collectively inform the researcher's holistic understanding of the influence of external factors on individual health outcomes.
Results
The major finding of this study was that there was no significant difference in the primary outcome variable, mean time-to-recovery, between pre-COVID (n = 126) and post-COVID (n = 30) cohorts. The mean time-to-recovery for the pre-COVID cases was 40.46 days (SD = 26.65, 95% CI [35.8, 45.1]), or 5.78 weeks, and for the post-COVID cases was 35.90 days (SD = 20.80, 95% CI [28.5, 43.3]), or 5.13 weeks; (t (147) = 0.860, p = .391, two-tailed). Additionally, the post-COVID cohort had significantly greater discharge weight (p = .034) and weight gain (p = .010) (see Table 1 ). Both cohorts’ rates of weight gain were below the national standard (8 g/kg/day) .22 There was no difference in height between cohorts (see Table 1).
Table 1.
Mean Growth among Recovered Cases in Pre- and Post- COVID Cohorts.
| Variables | Pre-COVID (n = 118) |
Post-COVID (n = 29) |
||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | z | p | |||
| Admission Weight |
6.1 |
2.0 |
6.6 |
2.2 |
1.65 |
.099 |
||
| Height | 66.2 | 9.5 | 69.1 |
11.2 | 1.61 | .108 | ||
| Discharge Weight |
7.1 |
2.0 |
7.9 |
2.1 |
2.12 |
.034* |
||
| Height | 67.0 | 9.2 | 70.2 |
10.3 | 1.77 | .077 | ||
| Weight Gained | 1.0 | 0.5 | 1.3 | 0.5 | 2.56 | .011* | ||
| Height Gained | 0.9 | 1.2 | 1.2 | 1.4 | 1.27 | .204 | ||
| Grams/KG/Day | 6.6 | 6.9 | 7.7 |
5.5 | 1.78 | .076 | ||
Note. Weight reported in kilograms, height in centimeters. Reported growth on recovered cases; the six pre-COVID cases and one post-COVID case did not complete recovery were excluded. Missing data points led to the pre-COVID n = 118, and post-COVID n = 29. Mann-Whitney U/Wilcoxon Two-Sample test reported. Asterisks (*) indicate significant results.
Six of the 17 categorical variables examining the relationship between COVID cohorts were significant: type of SAM (p < .001), admission weight <7 kg (p = .036), referral type (p = .025), multivitamins (p < .001), nebulizers/bronchodilators (p = .004), and mother's occupation (p = .013) (see Table 2 ). The majority of cases in both cohorts were admitted from the Southern region of Guatemala. Pre-COVID cases were primarily referred by the hospital, followed by self-referrals, while the majority of post-COVID cases were referred from health clinics, followed by the hospital. Of note, after the onset of COVID-19, the NRC required a 14-day isolation period upon admission, where mothers and children were isolated together and monitored for symptoms of COVID-19 (personal communication, November 8, 2021, NRC Director). Caution should be used in interpreting mother's occupation due to a majority of missing data (n = 92) (See Table 2). There was no statistically significant difference in the gender or age distribution of the two cohorts.
Table 2.
Frequencies and Chi-Square Results Between Pre-COVID (n = 126) and Post-COVID (n = 30).
| Pre-COVID |
Post-COVID |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | n | % | n | % | Total | χ2.‡ | df | p |
| Age | ||||||||
| ≤24 months | 115 | 82.7 | 24 | 17.3 | 139 | – | – | .100 |
| >24 months | 11 | 64.7 | 6 | 35.3 | 17 | |||
| Gender | ||||||||
| Male | 69 | 83.1 | 14 | 16.9 | 83 | .64 | 1 | .425 |
| Female | 57 | 78.1 | 16 | 21.9 | 73 | |||
| Severity of SAM | ||||||||
| Mild | 5 | 100.0 | 0 | 0.0 | 5 | 3.52 | 1 | .061 |
| Moderate | 59 | 85.5 | 10 | 14.5 | 69 | |||
| Severe | 62 | 75.6 | 20 | 24.4 | 82 | |||
| Type of SAM | ||||||||
| Marasmus | 22 | 66.7 | 11 | 33.3 | 33 | 11.83 | 1 | <0.001* |
| Kwashiorkor | 4 | 50.0 | 4 | 50.0 | 8 | |||
| None | 100 | 87.0 | 15 | 13.0 | 115 | |||
| Admit Weight | ||||||||
| <7 kg | 92 | 85.2 | 16 | 14.8 | 108 | 4.41 | 1 | .036* |
| ≥7 kg | 34 | 70.8 | 14 | 29.2 | 48 | |||
| Referral Type | ||||||||
| Walk-in | 31 | 93.9 | 2 | 6.1 | 33 | 6.62 | 1 | .010* |
| Hospital | 61 | 84.7 | 11 | 15.3 | 72 | |||
| Health Clinic/Dept. | 25 | 61.0 | 16 | 39.0 | 41 | |||
| Social Services | 9 | 90.0 | 1 | 10.0 | 10 | |||
| Amoxicillin | ||||||||
| Yes | 49 | 87.5 | 7 | 12.5 | 56 | 2.64 | 1 | .104 |
| No | 76 | 76.8 | 23 | 23.2 | 99 | |||
| Multivitamin | ||||||||
| Yes | 28 | 56.0 | 22 | 44.0 | 50 | 28.72 | 1 | <0.001* |
| No | 97 | 92.4 | 8 | 7.6 | 105 | |||
|
Variable |
n |
% |
n |
% |
Total |
χ2.‡ |
df |
p |
| Nebulizer/ Bronchodilator |
||||||||
| Yes | 70 | 89.7 | 8 | 10.3 | 78 | 8.33 | 1 | .004* |
| No | 55 | 71.4 | 22 | 28.6 | 77 | |||
| Zinc | ||||||||
| Yes | 106 | 80.9 | 25 | 19.1 | 131 | – | – | .785 |
| No | 19 | 79.2 | 5 | 20.8 | 24 |
|||
| Region | ||||||||
| Northern | 3 | 75.0 | 1 | 25.0 | 4 | 1.01 | 1 | .356 |
| Central | 50 | 86.2 | 8 | 13.8 | 58 | |||
| Southern | 73 | 77.7 | 21 | 22.3 | 94 | |||
| Mother's Occupation | ||||||||
| Agriculture | 1 | 50.0 | 1 | 50.0 | 2 | 6.30 | 1 | .013* |
| Homemaker | 39 | 84.8 | 7 | 15.2 | 46 | |||
| Sales | 6 | 85.7 | 1 | 14.3 | 7 | |||
| Service | 0 | 0.0 | 7 | 100.0 | 7 | |||
| No Contribution | 1 | 50.0 | 1 | 50.0 | 2 | |||
| Unknown | 79 | 85.9 | 13 | 14.1 | 92 | |||
| Father's Occupation | ||||||||
| Agriculture | 18 | 78.3 | 5 | 21.7 | 23 | .07 | 1 | .807 |
| Construction | 4 | 66.7 | 2 | 33.3 | 6 | |||
| Food Service | 4 | 80.0 | 1 | 20.0 | 5 | |||
| Homemaker | 0 | 0.0 | 1 | 100.0 | 1 | |||
| Security/Govern. | 2 | 66.7 | 1 | 33.3 | 3 | |||
| Service/Industry | 3 | 60.0 | 2 | 40.0 | 5 | |||
| Technology | 5 | 100.0 | 0 | 0.0 | 5 | |||
| No Contribution | 37 | 77.1 | 11 | 22.9 | 48 | |||
| Unknown | 53 | 88.3 | 7 | 11.7 | 60 | |||
Note. N = 155 for the following variables, Amoxicillin, Nebulizer/bronchodilator, Zinc, and Multivitamin. Asterisks (*) indicate significant results.
Refers to Mantel-Haenszel for all non-binary (nominal or ordinal) variables, and Fisher's Exact (–) when minimum expected counts (≥5) were not met.
Recovery and discharge
Since there was no significant difference in time-to-recovery, the primary outcome variable, cohorts were combined in further analyses. In the total sample (N = 156), 59% (n = 92) of the cases recovered within six weeks, 37% (n = 57) recovered in greater than six weeks, and 4% (n = 7) did not recover within the study timeframe. Overall, mean time-to-recovery, or the mean of the total number of days from admission to recovery (n = 149), was 39.57 days (SD = 25.62, 95% CI [35.5, 43.7]), or 5.65 weeks, which meets the international standard of recovery (<6 weeks). Time-to-discharge, or the total number of days from admission to discharge, for the total sample (N = 156) was an average of 43.97 days (SD = 25.59, 95% CI [40.0, 48.0]), or 6.28 weeks. The discrepancy between time-to-recovery and time-to-discharge existed because 21% (n = 36) recovered nutritionally but had a delay in discharge, ranging from 2 to 50 days, with a mean of 20.1 days (SD = 14.24, 95%CI [15.5, 24.8]), or 2.87 weeks. The majority of all cases were severely malnourished on admission (n = 82, 53%), followed by moderate (n = 69, 44%) and mild (i.e. acute) (n = 5, 3%). There was no significant relationship between malnutrition severity on admission and delayed discharge.
Sociocultural variables
Data regarding sociocultural characteristics was more limited than projected. Occupation was available for 41% of mothers (n = 64) and 62% of fathers (n = 96). Among mothers, 30% (n = 46) were homemakers, 10% (n = 16) were employed in the service sector (i.e. laundry or food sales), and 1% (n = 2) were not financially contributing to their child's care. There were 30% of fathers (n = 47) employed in professional jobs, such as journalism or law enforcement, and 31% (n = 48) fathers not financially contributing (see Table 2). Mothers’ (n = 141) mean age was 26 (SD = 6.59), ranging from 15 to 41 years; fathers’ (n = 99) mean age was 30 (SD = 8.85), ranging from 18 to 66 years.
Additionally, 17 cases had no access to running water and 42 cases indicated grandparents were involved in their living situation or providing for their daily needs. Overall, investigators are cautious when interpreting findings related to sociocultural data, due to the large amount of unknown data (see Table 2). Also, while not formally reported in case records, investigators were informed that few families return for follow-up assessments due to lack of transportation, particularly with increased bus fares after the onset of the pandemic (personal communication, November 12, 2021, NRC Director).
Indicators of recovery
Several predictor variables were analyzed to determine impact on recovery time (see Table 3 ). Univariate analysis indicated a significant association between recovery time and only two predictors, use of amoxicillin (p = .014) and nebulizers/bronchodilators (p = .039). Of note, there was no significant relationship between severity of malnutrition on admission with use of either amoxicillin χ2 (1, N = 155) = 0.210, p = .659, or nebulizers/bronchodilators, χ2 (1, N = 155) = 0.619, p = .476 (Data not shown).
Table 3.
Frequencies and Chi-Square Results Evaluating Categorical Variables and Recovery (N = 156).
| ≥6 weeks or no recovery | <6 weeks | Univariate Analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | n | % | n | % | Total | χ2. | df | OR [95% CI] | p |
| COVID Cohorts | |||||||||
| Post-COVID | 10 | 33.3 | 20 | 66.7 | 30 | .91 | 1 | 0.67 [0.29,1.54] | .341 |
| Pre-COVID | 54 | 42.9 | 72 | 57.1 | 126 | ||||
| Age | |||||||||
| ≤24 months | 56 | 40.3 | 83 | 59.7 | 139 | .29 | 1 | 0.76 [0.28,2.09] | .592 |
| >24 months | 8 | 47.1 | 9 | 52.9 | 17 | ||||
| Gender | |||||||||
| Female | 29 | 39.7 | 44 | 60.3 | 73 | .10 | 1 | 0.90 [0.48,1.71] | .757 |
| Male | 35 | 42.2 | 48 | 57.8 | 83 | ||||
| Severity of Malnutrition |
|||||||||
| Mild | 1 | 20.0 | 4 | 80.0 | 5 | 3.44 | 1 | 0.28 [0.03,2.57] | .064 |
| Moderate | 24 | 34.8 | 45 | 65.2 | 69 | 0.47 [0.05, 4.43] | |||
| Severe | 39 | 47.6 | 43 | 52.4 | 82 | 0.59 [0.30, 1.14] | |||
| Admit Weight | |||||||||
| <7 kg | 49 | 45.4 | 59 | 54.6 | 108 | 2.74 | 1 | 1.83 [0.89,3.75] | .098 |
| ≥7 kg | 15 | 31.3 | 33 | 68.8 | 48 | ||||
| Amoxicillin | |||||||||
| Yes | 30 | 53.6 | 26 | 46.4 | 56 | 6.07 | 1 | 2.31 [1.18,4.52] | .014** |
| No | 33 | 33.3 | 66 | 66.7 | 99 |
||||
| Multivitamin | |||||||||
| Yes | 17 | 34.0 | 33 | 66.0 | 50 | 1.35 | 1 | 0.66 [0.33,1.33] | .245 |
| No | 46 | 43.8 | 59 | 56.2 | 105 | ||||
| Nebulizer/ Bronchodilator |
|||||||||
| Yes | 38 | 48.7 | 40 | 51.3 | 78 | 4.24 | 1 | 1.98 [1.03,3.79] | .039* |
| No | 25 | 32.5 | 52 | 67.5 | 77 | ||||
|
Variables |
n |
% |
n |
% |
Total |
χ2. |
df |
OR [95% CI] |
p |
| Zinc | |||||||||
| Yes | 57 | 43.5 | 74 | 56.5 | 131 | 2.88 | 1 | 2.31 [0.86,6.20] | .090 |
| No | 6 | 25.0 | 18 | 75.0 | 24 | ||||
Note. N = 155 for the following variables, Amoxicillin, Nebulizer/bronchodilator, Zinc, and Multivitamin. Mantel-Haenszel was reported for non-binary variables (Severity of Malnutrition). Asterisks (*) indicate significant results. Double asterisks (**) indicate significance in both univariate and multivariable analyses (Data for multivariate not shown).
Multiple logistic regression was conducted to assess the impact of the nine predictor variables on the outcome variable (recovery in ≤6 weeks). Only one predictor variable of the model, amoxicillin, was significant, Wald χ2 = 4.14, p = .042. The adjusted odds ratio for amoxicillin was aOR = 2.14 [1.03,4.47], indicating children receiving amoxicillin were 2.14 times more likely to recover in >6 weeks, after controlling for other predictor variables (see Table 3).
Discussion
This retrospective chart review provides insight on time-to-recovery among children admitted to an NRC in Guatemala before and during COVID-19. The lack of difference in the primary outcome variable, time-to-recovery, between the pre- and post-COVID cohorts may be due to the considerably small sample size in the post-COVID. The small sample was likely impacted by both fear of the pandemic, and new isolation policies at the NRC. There was also a difference in referral trends between cohorts; with fewer self-referrals in the post-COVID cohort (n = 2) than the pre-COVID cohort (n = 31). This would suggest that families were less inclined to seek out treatment or experienced other challenges post-pandemic, preventing them from seeking treatment.
The significantly higher weight gain and discharge weight post-COVID compared to pre-COVID was unanticipated. This could be explained by the small post-COVID cohort receiving closer attention by NRC staff, due to the lower staff to child ratio. Overall, average time-to-recovery, the rate of weight gain, and lack of fatalities in this sample are evidence that the NRC has effectiveness levels comparable to other NRCs and OTPs.21 , 35 , 36 One concern is the delay many children faced between recovery and discharge. Due to the nature of the medical records (paper charts) used to collect data, there is limited insight as to why children experienced these delays. Often this is due to treatment of secondary illnesses, such as respiratory or gastrointestinal infections, or adverse social conditions that delay a safe discharge plan (personal communication, November 9, 2021, NRC Director). However, this could not be verified in the data.
Although the Social Ecological Model38 informed the study, findings were primarily at the individual level and macro-level data was sparse. Despite limited data, the sociocultural findings in this study provide further environmental concern for child health in this setting. There was some evidence that these families relied on extended family for housing, financial needs, and childcare. Additionally, when evaluating parents’ employment, mothers were most often homemakers, and fathers were not contributors to family financial well-being. Compounding this, working mothers’ occupations were lower-paying jobs (i.e. food sales or laundry) compared to fathers (i.e. law enforcement, banking). Employment opportunities and family obligations are ongoing challenges for Guatemalan women.10 , 11 Additionally, in some cases, families were without access to transportation or potable water. For these reasons, collecting sociocultural data upon admission, it is essential to consider the impact of limited income and transportation barriers.
Amoxicillin was the only significant predictor of time-to-recovery in this study. Previous studies evaluating amoxicillin as treatment for malnutrition have had inconsistent findings; some indicate it contributes to recovery, others found no benefit.24 , 25 Interestingly, in this sample, the relationship between amoxicillin and recovery was the inverse of what was expected; it was found to be associated with slower recovery rates. Further, there was no significant relationship between amoxicillin and severity of malnutrition. A known side effect of amoxicillin is increased risk of diarrhea,39 which could be a possible explanation of the slower recovery rates in these children. Of note, amoxicillin was not widely used in this sample (n = 56, 36%).
Predictor variables in other studies, i.e., gender, age, vitamin supplementation, and admission weight less than 7 kg29 , 30 , 32 had no influence on recovery in this study. This could be related to the homogeneity of the cases; for example, there was a nearly even distribution between males and females, and most children (n = 139, 89%) were ≤2 years. Another unanticipated finding was the widespread use nebulizers/bronchodilators (n = 78, 50%), suggesting respiratory illnesses. An absence of secondary diagnoses in the case records prevents analysis of this in the data. While medications were not the focus of this study, numerous medications were prescribed to children during their recuperation, such as, acyclovir, acetaminophen, folic acid, and reflux prescriptions. Future investigation of medications might provide insight to secondary diagnoses and prescription practices for malnutrition.
Strengths and limitations
This study had several strengths. The findings add to our understanding of malnutrition in a vulnerable population and provides timely data on a population with limited representation in the literature within the context of a pandemic. Also, this study built on a community-university partnership and NRC staff provided the local perspective; such partnerships are critical to advance the science of global health.
Two limitations were in the sample and setting. A smaller sample in the post-COVID cohort could have negatively affected the statistical power of the tests used in the analysis. Also, the post-COVID sample came from only 10 months, as opposed to 14 months pre-COVID. Still, the post-COVID sample suggests the impact of the pandemic on child health. It was anticipated that the effects of the pandemic would have resulted in an intense need for nutrition services like the NRC; however, the services were less utilized than in previous years. Additionally, data was only collected from one NRC in Guatemala (albeit the largest), thus, findings have limited generalizability. Collecting data from case records handwritten in Spanish was a challenge; in cases where notes were not discernible, the PI consulted the NRC director.
Implications for policy, research, and practice
A health policy concern at the time of this study was the need for increased availability of COVID-19 testing in Guatemala. Access to testing would decrease the need for a lengthy isolation period for newly admitted children, improving parent's experience and receptiveness toward receiving needed care, as well as promoting staff safety. Another policy issue is management of acute malnutrition, which is generally not considered a major health concern by the Guatemalan Ministry of Health (personal communication, November 23, 2021, NRC Nutritionist). However, close monitoring of acute cases is critical to mitigate worsened conditions. Five cases (1 pre-COVID, 4 post-COVID) in this study were admitted with acute malnutrition; these cases could have been managed within the community through collaboration with CHWs, supplemental nutrition, and ongoing evaluation.33 Development of CHW outreach with rural and indigenous communities7 in the Southern region may be an area to focus on in future intervention studies. When provided proper training and support from public health nurses, CHWs can monitor and track at-risk children, in line with the USAID4 current work in supporting rural indigenous populations.
Future research could further explore the long-term effects the COVID-19 pandemic on childhood malnutrition. Investigation of secondary diagnoses and detailed medication uses could provide understanding of the additional medical complexities commonly experienced by malnourished children and the impacts of these complexities on recovery. A prospective cohort design might decrease the likelihood of missing data. A multi-site study evaluating the impact of amoxicillin on recovery would solidify understanding of its effectiveness and risks. A number of features in this dataset could benefit from a qualitative descriptive case study for a greater depth of understanding from the perspectives of families and staff. A qualitative study investigating the sociocultural context could provide needed data to increase the effectiveness of SAM recovery interventions.
In clinical practice, understanding the sociocultural characteristics that impact child health is key, as these factors inform all aspects of care, including health education and discharge planning. A strategy to increase access to sociocultural data among malnourished children is to implement an admission family needs assessment, including a home evaluation. This will allow clinicians to quickly identify upstream factors contributing to food insecurity, such as potable water and housing conditions. The home evaluation piece is essential to establish childcare and home safety needs on admission, in order to prevent children staying at the center longer than necessary, increasing risk of contracting communicable diseases. Once needs are identified, families can be connected with appropriate governmental resources, such as the health department, as well as local non-profit resources dedicated to mothers and children, such as Corazon de Los Niños (http://www.corazondelosninos.org/) or other university partnerships.
A family needs assessment could also provide further evidence of population health necessities; this information could serve in procurement of additional resources and funding.
Conclusion
This study informs our understanding of malnutrition recovery at a Guatemalan NRC before and during the COVID-19 pandemic. The discovery of relevant information on clinical variables in a vulnerable population informs potential program development strategies within the NRC. Further research is needed to more fully understand the long-term complexities that the pandemic has had on childhood malnutrition recovery. Findings may be utilized in further investigation and intervention development to reduce malnutrition in LMICs amid the ongoing COVID-19 pandemic.
Financial support
This study was supported by East Carolina University College of Nursing's doctoral student research grant.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to sincerely thank the leadership of Casa Jackson, a program of La Asociación Nuestros Ahijados. In particular, we want to express our appreciation to Vecany Sanchez and Robbie Middleton, for their partnership with the research team.
References
- 1.World Health Organization [WHO]. Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1, 2021(accessed 16 May 2023).
- 2.United Nations International Children's Emergency Fund [UNICEF]. Malnutrition. https://data.unicef.org/topic/nutrition/malnutrition/, 2021 (accessed 16 May 2023).
- 3.United Nations International Children's Emergency Fund [UNICEF]. Children, food and nutrition. https://www.unicef.org/media/106506/file/The%20State%20of%20the%20World%E2%80%99s%20Children%202019.pdf, 2019 (accessed 16 May 2023).
- 4.United States Agency for International Development [USAID]. Nutrition profile: guatemala. https://2017-2020.usaid.gov/sites/default/files/documents/1864/Guatemala-Nutrition-Profile-Mar2018-508.pdf, 2021 (accessed 16 May 2023).
- 5.Flores-Quispe M., Restrepo-Méndez M.C., Maia M., Ferreira L.Z., Wehrmeister F.C. Trends in socioeconomic inequalities in stunting prevalence in Latin America and the Caribbean countries: differences between quintiles and deciles. Int J Equity Health. 2019;18:156. doi: 10.1186/s12939-019-1046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Batis C., Mazariegos M., Martorell R., Gil A., Rivera J.A. Malnutrition in all its forms by wealth, education and ethnicity in Latin America: who are more affected? Public Health Nutr. 2020;23:s1–s12. doi: 10.1017/S136898001900466X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gatica-Domínguez G., Victora C., Barros A. Ethnic inequalities and trends in stunting prevalence among Guatemalan children: an analysis using national health surveys 1995-2014. Int J Equity Health. 2019;18:110. doi: 10.1186/s12939-019-1016-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kragel E.A., Merz A., Flood D., Haven K.E. Risk factors for stunting in children under the age of 5 in rural Guatemalan highlands. Ann Glob Health. 2020;86:8. doi: 10.5334/aogh.2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voth-Gaeddert L.E., Oerther & D.B. Acute to chronic malnutrition: how significant water, sanitation, and hygiene factors change with health outcomes and geographies in the western highlands of Guatemala. J Environ Health. 2019;82:20–28. [Google Scholar]
- 10.Burroway R. Are all jobs created equal? A cross-national analysis of women's employment and child malnutrition in developing countries. Soc Sci Res. 2017;67:1–13. doi: 10.1016/j.ssresearch.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Ekbrand H., Halleröd B. The more gender equity, the less child poverty? A multilevel analysis of malnutrition and health deprivation in 49 low- and middle-income countries. World Dev. 2018;108:221–230. doi: 10.1016/j.worlddev.2018.01.028. [DOI] [Google Scholar]
- 12.Oddo V.M., Surkan P.J., Hurley K.M., Lowery C., Ponce S., Jones-Smith J.C. Pathways of the association between maternal employment and weight status among women and children: qualitative findings from Guatemala. Matern Child Nutr. 2018;14:e12455. doi: 10.1111/mcn.12455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juarez M., Dionicio C., Sacuj N., Lopez W., Miller A.C., Rohloff P. Community-based interventions to reduce child stunting in rural Guatemala: a quality improvement model. Int J Environ Res Public Health. 2021;18:773. doi: 10.3390/ijerph18020773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olney D.K., Leroy J., Bliznashka L., Ruel M.T. PROCOMIDA, a food-assisted maternal and child health and nutrition program, reduces child stunting in Guatemala: a cluster-randomized controlled intervention trial. J Nutr. 2018;148:1493. doi: 10.1093/jn/nxy138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guzmán-Abril A., Alajajian S., Rohloff P., Proaño G.V., Brewer J., Jimenez E.Y. A home garden intervention improves child length-for-age z-score and household-level crop count and nutritional functional diversity in rural Guatemala. J Acad Nutr Diet. 2021;122:640–649. doi: 10.1016/j.jand.2021.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Rohloff P. On the frontlines of chronic paediatric undernutrition in Guatemala. EBioMedicine. 2021;64 doi: 10.1016/j.ebiom.2021.103223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization [WHO]. Archived: WHO timeline- COVID-19. https://www.who.int/news/item/27-04-2020-who-timeline-covid-19, 2020 (accessed 16 May 2023).
- 18.Action Against Hunger. Number of people facing hunger doubled due to COVID-19. https://www.actionagainsthunger.org/story/number-people-facing-hunger-guatemala-doubled-due-covid-19, 2020 (accessed 12 November 2021).
- 19.People for Guatemala. Coronavirus crisis in Guatemala: a timeline. https://www.peopleforguatemala.org/covid-19/coronavirus-crisis-in-guatemala-a-timeline/, 2020 (accessed 12 November 2021).
- 20.Victora C.G., Christian P., Vidaletti L.P., Gatica-Domínguez G., Menon P., Black R.E. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet. 2021;397:1388–1399. doi: 10.1016/S0140-6736(21)00394-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kabalo M.Y., Seifu C.N. Treatment outcomes of severe acute malnutrition in children treated within Outpatient Therapeutic Program (OTP) at Wolaita Zone, Southern Ethiopia: retrospective cross-sectional study. J Health Popul Nutr. 2017;36:7. doi: 10.1186/s41043-017-0083-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sphere Project. The Sphere handbook: humanitarian charter and minimum standards in humanitarian response. http://www.sphereproject.org/handbook, 2011 (accessed 12 November 2021).
- 23.M.Palacios A., Hurley K.M., De-Ponce S., et al. Zinc deficiency associated with anaemia among young children in rural Guatemala. Matern Child Nutr. 2020;16:e12885. doi: 10.1111/mcn.12885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization [WHO]. Severe acute malnutrition update: current WHO guidelines and the WHO essential medicine list for children. https://www.who.int/selection_medicines/committees/expert/21/applications/s6_paed_antibiotics_appendix7_sam.pdf, 2016 (accessed 12 November 2021).
- 25.Isanaka S., Grantz K.H., Berthé F., Schaefer M., Adehossi E., Grais R.F. Extended follow-up from a randomized clinical trial of routine amoxicillin in the treatment of uncomplicated severe acute malnutrition in Niger. JAMA Pediatr. 2020;174:295–297. doi: 10.1001/jamapediatrics.2019.5189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nel E. Severe acute malnutrition. Curr Opin Clin Nutr Metab Care. 2018;21:195–199. doi: 10.1097/MCO.0000000000000465. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization [WHO]. WHO child growth standards and the identification of severe acute malnutrition in infants and children. https://apps.who.int/iris/bitstream/handle/10665/44129/9789241598163_eng.pdf;jsessionid=C0453EB7C82A0AABCDD77015F4F73DAB?sequence=1 (accessed 14 June 2023). [PubMed]
- 28.Liben M.L., Wuneh A.G., Shamie R., G/Her K. Factors associated with child survival in children admitted to outpatient therapeutic program at public health institutions in Afar Regional State, Ethiopia: a prospective cohort study. J Health Popul Nutr. 2019;38:35. doi: 10.1186/s41043-019-0193-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mamo W.N., Derso T., Gelaye K.A., Akalu T.Y. Time to recovery and determinants of severe acute malnutrition among 6–59 months children treated at outpatient therapeutic programme in North Gondar zone, Northwest Ethiopia: a prospective follow up study. Ital J Pediatr. 2019;45:136. doi: 10.1186/s13052-019-0732-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teshome G., Bosha T., Gebremedhin S. Time-to-recovery from severe acute malnutrition in children 6–59 months of age enrolled in the outpatient treatment program in Shebedino, southern Ethiopia: a prospective cohort study. BMC Pediatr. 2019;19 doi: 10.1186/s12887-019-1407-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doocy S., Tappis H., Villeminot N., et al. Point-of-use water treatment improves recovery rates among children with severe acute malnutrition in Pakistan: results from a site-randomized trial. Public Health Nutr. 2018;21:3080–3090. doi: 10.1017/S1368980018001647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gebremedhin K., Ayele G., Boti N., Andarge E., Fikadu T. Predictors of time-to-recovery from severe acute malnutrition treated in an outpatient treatment program in health posts of Arba Minch Zuria Woreda, Gamo zone, Southern Ethiopia: a retrospective cohort study. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0234793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.López-Ejeda N., Charle Cuellar P., Vargas A., Guerrero S. Can community health workers manage uncomplicated severe acute malnutrition? A review of operational experiences in delivering severe acute malnutrition treatment through community health platforms. Matern Child Nutr. 2019;15:e12719. doi: 10.1111/mcn.12719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rastogi S., Maheshwari C., Raghav S.K., Muzammil K. A prospective observational study to evaluate the efficacy of facility-based management in malnourished children at NRC, district Meerut. J Family Med Prim Care. 2018;7:1341–1345. doi: 10.4103/jfmpc.jfmpc_157_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaturvedi A., Patwari A.K., Soni D., et al. Progress of children with severe acute malnutrition in the malnutrition treatment centre rehabilitation program: evidence from a prospective study in Jharkhand, India. Nutr J. 2018;17:69. doi: 10.1186/s12937-018-0378-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Golandaj J.A., Vatavati S.R., Kallihal K.G. Effect of nutritional interventional measures on admitted children in selected nutritional rehabilitation centres of Karnataka, India. Nutr Food Sci. 2017;47:53–66. doi: 10.1108/NFS-06-2015-0078. [DOI] [Google Scholar]
- 37.Authors A feasibility study to examine clinical variables of childhood malnutrition in Guatemala. Hisp Health Care Int. 2023:1–8. doi: 10.1177/15404153221150452. [DOI] [PubMed] [Google Scholar]
- 38.U. Bronfenbrenner, The ecology of Human Development. Harvard University Press, 1979.
- 39.National Library of Medicine. Amoxicillin. https://medlineplus.gov/druginfo/meds/a685001.html (accessed 14 June 2023).