Abstract
Drug-resistant tuberculosis (DRTB) is a growing concern worldwide. The poor rate of service delivery exacerbates the severity, leading to an increase in community transmission, which is further amplified by stigma. Health care workers (HCWs) are at the forefront lines of service delivery; their efforts are suspected of resulting in stigmatization, negatively impacting patient-centered care. However, little is known about DRTB-related stigma among these HCWs, and interventions are limited. Our scoping review is significant because it provides an overview of the DRTB stigma confronting HCWs and informs subsequent stigma-reduction initiatives. Utilizing Arksey and O’Malley framework, we exhaustively searched electronic databases for relevant English-language studies published from 2010 to 2022, identifying the drivers and facilitators of DRTB-related stigma among HCWs from high-TB and -DRTB burden countries, and compiling recommendations that could reduce DRTB stigma. From 443 de-duplicated papers, 11 articles on HCWs’ DRTB-related stigma were reviewed and synthesized. Fear was mentioned across included articles as a stigma driver. Other reported stigma drivers identified included feelings of discrimination, isolation, danger, lack of support, shame, and stress. Poor infection control (IC) was the leading stigma facilitator. Other stigma facilitators identified were differing IC interpretations, workforce culture, and workplace inequality facilitating to stigmatization of HCWs. Three key recommendations identified were addressing infection control issues; increase the competence of healthcare workers; and provide psychosocial assistance, emphasizing HCW safety during DRTB activities. DRTB stigma among HCWs is multifaceted, largely driven by fear and facilitated by varying implementation or interpretations of policies within the workplace. Making HCWs feel safe while conducting DRTB activities is a priority issue that should be addressed by improving IC, training and psychosocial support. More studies investigating country-specific and multilevel DRTB-related stigma among HCWs are required to inform the development of an effective stigma intervention strategy.
Keywords: drug-resistant tuberculosis, DRTB stigma, health workers, stigma, TB stigma, tuberculosis stigma
What do we know so far about this topic?
Health workers are on the front lines of DRTB service delivery; their efforts in all areas of disease control are suspected of resulting in stigmatization, which has a negative impact on patient-centered care.
What contribution does this research make to the field?
This is the first study to provide an overview of the DRTB stigma drivers and facilitators, which could assist program managers and policymakers in identifying the policies that need to be addressed to create a stigma-free healthcare environment.
What are the implications of the research for theory, practise, or policy?
Policymakers must examine TB and DRTB policies, particularly IC and risk-payments, in order to minimize disparities and develop viable, effective solutions that discourage DRTB factors that driver and facilitator stigma among HCWs.
Introduction
Tuberculosis (TB) is a global public health concern. 1 About a fourth of the world’s population had latent TB in 2020, and 10 million had active TB. 1 Alarmingly, TB drug resistance is growing and affecting about 500 000 people annually, and its persisting increase is an urgent and challenging obstacle to TB control and prevention. 2
Combatting DRTB requires therapeutic efficacy, equity, and safety, as well as patient-centered care. 3 Patient-centered care addresses socioeconomic issues that worsen DRTB, like poverty and geographic barriers to health care. Its holistic approach rewards patients, treatment advocates, and healthcare providers, minimizing stigma. 4 Healthcare workers (HCWs) involved in DRTB activities and psychosocial support are integral to patient-centered care. 5
TB is a stigmatized disease. 6 Stigma is the community’s labeling of a trait as undesirable or devalued, which can lead to disgust, fear, guilt, and shame.7,8 In healthcare, TB-related stigma is commonly associated with “dirty work,” and HCWs delivering care for TB are viewed as facing the dirty work stigma. 9
The stigma of TB causes diagnostic delays and treatment refusals. Stigmatized TB patients are reluctant to seek and complete treatment 10 ; whereas stigmatized HCWs exhibit undesirable behaviors toward their patients or co-workers. 11 However, stigma’s impacts extend beyond disease prevention and treatment, affecting the quality of life of patients and those around them, including HCWs12-15; consequently, DRTB spread. 2
DRTB stigma is pronounced, 2 and patients are particularly vulnerable to it. 16 The psychosocial concerns surrounding the disease disrupt the social lives of patients and their families.17-19 Similarly, stigma in DRTB affects HCWs’ well-being and often leads to stigmatizing behaviors in healthcare settings, 11 thus, a major barrier to patient-centered care.20-22
Stigmatization mechanisms frequently share characteristics, but their consequences can differ. 11 For instance, many DRTB patients experience depression, guilt, loss of self-identity or self-esteem 23 ; while others experience isolation, relationship failure, or separation. 24 Despite a lot of study on the consequences of DRTB stigma on patients and their families, no study has systematically examined the stigma confronted by HCWs.
As a growing concern, reducing DRTB workplace stigma is important 11 and calls for a sustainable response that should be addressed at all levels.9,25 At the facility level, targeting the factors comprising the stigmatization process is increasingly recognized. Stigma factors may include illness characteristics (eg, virulence), features from within the facility (eg, policies), and individual HCW (eg, attitude). 25 However, measures addressing workplace health stigma are lacking. 26 Thus, this review on DRTB-associated stigma among HCWs is significant to TB program managers and researchers to build sustainable stigma reduction efforts.
Methods
Part of a larger study on DRTB stigmatizing Filipino HCWs, this review highlights materials that may influence future research and decision-making.27,28 Unlike systematic review, which synthesizes primary studies to address a specific topic to minimize bias, 29 this review combines material and finds gaps in workplace DRTB-related stigma. 28
This review aimed to (1) acquire a better understanding of the stigma surrounding DRTB; and (2) provide insights that could inform the development of interventions to reduce DRTB stigma among HCWs. DRTB-related stigma factors affecting HCWs were identified by identifying stigma drivers and facilitators and HCW stigma experiences. We collected DRTB stigma-reduction recommendations.
This review utilized Arksey and O’Malley framework, 30 Peters et al’s recommendations 31 and the Joanna Briggs Institute System for the Unified Management of the Assessment and Review of Information (JBI SUMARI) utilities. To ensure systematic reporting, the PRISMA Extension for Scoping Reviews (PRISMA-ScR) checklist was used. 32 Prior to conducting this review, this scoping review was registered in Open Science Framework osf.io/43kp9 and a protocol was published. 33
Study Selection
Preliminary search was conducted in February 2022 and updated in September–November 2022. Peters et al’s 34 Population, Concept, and Context (PCC) criteria (Table 1) guided our search strategy, focusing on 2 concepts – DRTB and stigma. The search followed JBI scoping review protocol—pilot search, search protocol preparation, and database search utilizing Medical Subject Heading (MeSH) terms (Supplemental Appendix 1).
Table 1.
Scope of Inquiry for Examining DRTB Stigma Drivers and Facilitators Among HCWs.
| Participants | Health workers—including physicians, nurses, midwives, medical technologist, pharmacists, and other allied professionals in healthcare settings such as hospitals, clinics, community centers, and TB treatment facilities delivering DRTB services such as case-finding, screening, diagnosis, treatment, and prevention. |
| Concept | Stigma of health workers delivering services to DRTB patients - stigma drivers and facilitators, including but not limited to beliefs, fears, lack of awareness about the DRTB and stigma, inability to clinically manage the condition, negative attitudes, and institutionalized procedures or practices. |
| Context | Available data from countries identified in the World Health Organization’s list of high TB- and drug-resistant TB burden countries (Supplemental Appendix 1). |
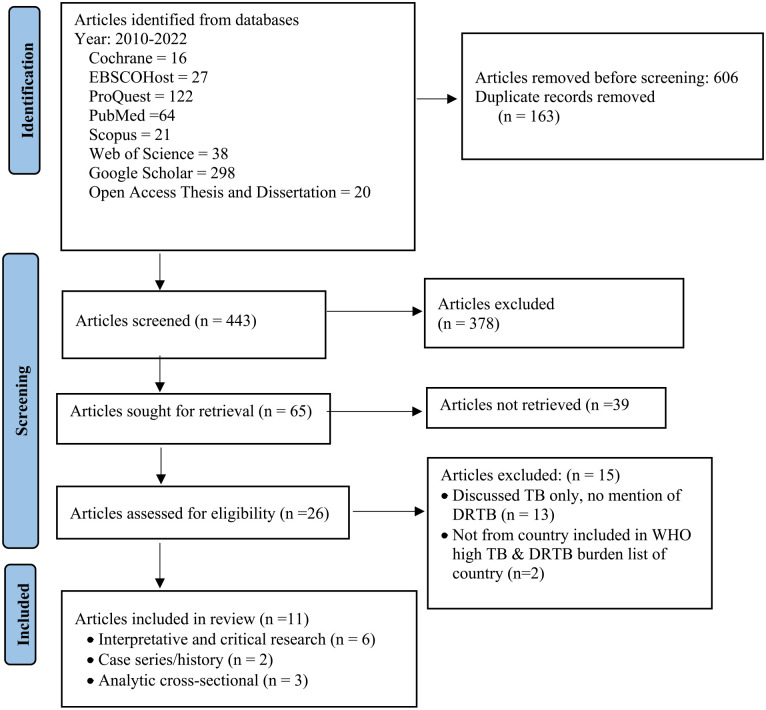
After de-duplication, the searches yielded 443 articles, 65 were selected for title and abstract evaluation, and 39 were excluded due to inclusion criteria ineligibility. After reviewing 26 full-text articles, 11 relevant articles were reviewed and synthesized. Figure 1 shows the PRISMA-ScR article flow from identification through inclusion.
Figure 1.
PRISMA-SCr flow diagram in examining the driver and facilitators of DRTB-related stigma among CHWs and recommendations to help address the stigma.
Inclusion Criteria
Eligibility of included studies were:
focused on DRTB stigma among HCWs, or
presented evidence that are associated to DRTB stigma among health workers, and
participants from WHO high-TB/DRTB burden countries (Supplemental Appendix 2)
Studies pertaining to health professionals’ stigma toward TB, not DRTB, was excluded. DRTB stigma studies on patients and their families, and those from non-WHO high TB and DRTB-burden countries were excluded. Editorials and comments were excluded.
Data Charting
Data charting was iterative to ensure comprehensive literature search. Reviewers independently and thoroughly evaluated the articles and charted the relevant material in a chart developed beforehand (Supplemental Appendix 3). Utilization of data charting was to prevent removing potential results of importance to this review’s synopsis. 35 Endnote’s citations and full texts imported into NVivo were used to improve data charting and textual data source analysis. Citation specifics, study details, the verbatim accounts of stigma experience and the findings associated with stigma reduction were likewise charted.
The articles were examined using JBI’s quality assessment tool. Unlike a systematic review, which formally analyzes methodological quality for risk of bias, our scoping review broadly examined the quality of the studies to provide an overview of research activity on a topic. 36 It was not intended to rank the articles based on the evidence provided, and no articles were excluded from the review based on their quality. Supplemental Appendix 4 contains a quality assessment of each study design included in this review.
Results
Included Studies’ Characteristics
This review comprised case series/case history (n = 2), analytical cross-sectional (n = 3), and interpretative and critical research (n-= 6), with most studies from South Africa (n = 8) and one each from Indonesia, the Philippines, and Tanzania. Nine studies used interviews and surveys, 3 used historical data, and no systematic reviews. Only 2 of 11 studies focused solely on DRTB stigma among HCWs. The other 9 studies focused on HCWs’ perspectives on DRTB care (n = 4), HCWs and DRTB infection control (IC) (n = 2), and DRTB infection among HCWs (n = 3). However, the studies found evidence of DRTB-related stigma among HCWs. Eight studies included a mix of health workers, while 3 studies solely included physicians. No studies solely included nurses, medical laboratory technologists, pharmacists, and other allied health workers. Supplemental Appendix 5 describes the included research by design. Table 2 summarizes the stigma drivers and facilitators, including verbatim quotes from the included studies.
Table 2.
Summary of Included Studies in Examining the Evidence of DRTB Related Stigma Among HCWs in High TB and DRTB Countries.
| Citation | Study design | Data collection | Target population | Study setting or country | Drivers of stigma | Facilitator of stigma | Verbatim quote descriptions of stigma experience | Verbatim quote recommendation for stigma reduction |
|---|---|---|---|---|---|---|---|---|
| Padayatchi et al. 40 | Case Series | Historical data | Physician | South Africa | Fear of contracting the disease; Stress in providing care; Shame; Feeling unsafe | Lack of infection control; Weak psychosocial support |
“Doctors felt the personal and professional stresses of carrying on work after being diagnosed with DRTB”
37
“Several doctors experienced difficulty and awkwardness re-integrating into a teaching environment where their illness have been publicised.” 37 “Doctors expressed feeling ashamed and blamed for acquiring TB as they were professionals who are expected to be fully aware of risk exposure yet ill-equipped to apply this knowledge to protect themselves.” 37 |
“Prioritization of infection control education and practice;
Enhanced infection control education in medical curricula and practice, towards mitigating occupational risks; Adherence to legislation for occupational safety.” 37 “Psychological support and professional counselling should be a routine part of conventional medical care for doctors with TB in high-risk settings.” 37 |
| Kanjee et al. 39 | Cross-sectional Study | Questionnaire | HCWs | South Africa | Fear of contracting the disease; Feeling unsupported; Feeling isolated; Shame |
Lack of infection control |
“As several staff members had died from confirmed TB/MDR-TB/XDR-TB, 82.1% and 42.9% of respondents were less willing to work in high-risk areas of the hospital or to work as an HCW, respectively.”
38
“HCWs do not trust the health services to take care of them if they have TB” 38 “HCWs fear potential rejection and stigma from staff if they have TB; and think it is shameful to admit they might have TB” 38 |
“Facilities must implement multi-faceted TB IC facility and behavioural change interventions”
38
“Facilities should ensure confidentiality of staff health information and reduce the stigma in order to improve HCW uptake of personal diagnosis and other risk-reduction strategies.” 38 |
| Naidoo et al. 46 | Cross-sectional study | Self-administered questionnaire | Physicians (inlcuding 4 respondents with DRTB) | Sub-sahara Africa | Feeling discriminated, unsupported. | Lack of infection control; Lack of psychosocial support |
“It hurts when our own well-being is jeopardized, and our own colleagues and management show an uncaring attitude towards us.”
39
“Physicians regretted choosing clinical medicine as a career option, another stated being treated inappropriate by colleagues and criticised for taking sick leave” 39 |
The study emphasizes the need for improved educational and awareness programs for all healthcare personnel, including hospital administrators, and changes in attitudes on the part of senior medical colleagues and administrators towards medical doctors with TB. |
| Tudor et al. 22 | Cross-sectional Study | Questionnaire | HCWs | South Africa | Fear of contracting the disease; Feeling isolated; Feeling discriminated; Feeling unsupported | Lack of infection control; Inequity in income protection |
“they were concerned about being isolated from their family for long periods of time “to be isolated and away from family and friends”
22
“how will society accept you, how will your colleagues treat you?” 22 “. . . getting infected with MDR- or XDR-TB and no one cares about what happens to me” 22 “HCWs do not receive danger allowance for working in MDR-/XDR-TB wards and the lack of compensation they would receive if they were to acquire MDR-/XDRTB” 22 “HCWs responded that they were concerned about stigma and the perceived lack of psychosocial support if they become ill.” 22 |
“It is imperative that efforts are made to improve IC and ensure safe working conditions for all HCWs.”
22
This study highlights training of HCWs in IC measures, and specifically on protecting self and others from the TB(DRTB) Recommended all HCWs, to have free access occupational health services and income protection. |
| Daftary and Padayatchi 42 | Qualitative Study | Interviews | HCWs | South Africa | Stress in providing care; Fear of contracting the disease |
Lack of infection control | “Junior HCWs expressed concern on nosocomial exposure due to patients no closing their mouths when coughing.” 40 | This study recommended addressing suboptimal infection control practices and complacency in the workplace through leadership and governance |
| Jaramillo et al. 45 | Qualitative Study | Interviews | HCWs | Philippines | Fear of contracting the disease Stress in providing DRTB care |
Lack of infection control | “There is poor infection control practices, fear, and limited capacity in rural health centers” 41 | This study recommended that professional development opportunities, oversight of personnel, and information campaigns should be in place to curb stigma in the community |
| Lyakurwa et al. 41 | Qualitative Study | Interview and focus group discussions | HCWs | Tanzania | Fear of contracting the disease. Feeling unsupported |
Lack of knowledge in DRTB care, Lack of financial support |
“HCWs lacked confidence in the quality of care at their facility and fear DRTB because they have no experience in treating DRTB patients and assume having a higher risk to be infected by them”
42
“. . .no extra-duty pay for staff working on holidays” 42 |
“The teams proposed to train more HCWs, including facility managers in the training and ongoing mentorship” 42 |
| Probandari et al. 37 | Qualitative Study | Questionnaire | Primary Health Care health staff | Indonesia | Fear of contracting the disease; Feeling unsafe; Stress in providing care |
Lack of infection control | “Staff fear of being infected and feeling afraid to talk to MDRTB patients; they are stressed and fearful of conducting MDRTB care” 43 | The study emphasized the need for knowledge and capacity building for infection control The Study identified that training alone is not sufficient; and research is needed to evidence effective strategies that reduce stigma among health staff providing MDRTB care |
| Vanleeuw et al. 43 | Qualitative Study | Interviews | HCWs | South Africa | Fear of contracting the disease; Stress in providing care |
Lack knowledge in DRTB program implementation; Lack of administrative support in addressing changes in DRTB care. |
“These doctors are scared of TB patients and refer them quickly.”
44
“Majority of HCWs at primary healthcare level did not have this experience and expressed concern with the sudden addition of DR-TB patients to their daily routine” 44 |
The study recommended that attention is required as to how the decentralized DR-TB unit can be supported by district management and other healthcare providers. |
| Zelnick et al. 38 | Qualitative Study | Key informant interview and survey questionnaire | HCWs | South Africa | Fear of contracting the disease; Feeling unsafe; Feeling discriminated | Lack of infection control; Inequity in income protection |
“Nurse: TB is all over, so we can’t get a risk allowance. . .the only compensation we can get is being treated free when you are diagnosed with TB.” 25 | This study recommended for evaluation of IC efforts and the decentralized management of DRTB as part of the initiatives to control DRTB and create as safe workplace. |
| Von Delft et al. 44 | Text and opinion | Historical data | Physicians | South Africa | Feeling isolated; Fear of discriminated; Fear of infection |
Lack of infection control |
“The medical student with MDR tuberculosis experienced extreme social isolation, driven by a lack of understanding from family members and peers as well as the medical school administrator.”
45
“HCWs in low-resource settings with possible tuberculosis symptoms are already wary of presenting for testing and treatment, because of stigma and career implications; and fear of infecting family members.” 45 |
This study recommends for an urgent action to improve IC implementation. |
Stigma drivers
All studies identified more than one stigma driver, with an emphasis on fear. HCWs working in DRTB wards are most afraid about catching the disease, which could spread to their families and others.22,37-45 HCWs’ nosocomial infection concerns vary, reflecting workplace behaviors,38,39,42,43 and lack of knowledge on IC guidelines.37,38,41,42
Another stigma driver noted is stress from treating DRTB patients. Four studies found that HCWs were stressed about providing DRTB care, mostly due to a lack of experience,37,40,42,43 and confidence in their facility’s capability to provide DRTB care. 41
Two studies mentioned HCWs’ stigma being perpetuated by their colleagues and peers. Example, HCWs were concerned about potential rejection or compromising work relationships if they became ill, whereas those who became ill faced discrimination and career implications.39,44 In 4 studies, infected HCWs’ psychological experiences were described as extensive, including depression, anxiety, resentment, paranoia, and intense fear of relapse or re-exposure.22,40,44,46 Two studies mentioned the fear of isolation or separation from family and friends.22,46
Stigma facilitators
Stigma facilitators are perceived influences that reduce or enhance stigmatizing behaviors. 47 In healthcare, cultural norms, workplace safety requirements, and health policy are examples of stigma facilitators. 25 Poor occupational safety standards, including a lack of IC, were most frequently regarded as a stigmatizing facilitator in the included studies. Seven South African studies reported HCWs’ worry with workplace poor IC practices and complacency22,37-40,42,44 with some HCWs not following IC advice. 39 Six studies mentioned inadequate IC due to disparities in risk perceptions among co-workers, varying policy interpretations, or lack of knowledge about IC.22,37,38,42,44,45
Weak workplace structure support was also mentioned. Six studies identified HCWs’ low morale as a result of disparities in hazard compensation, job instability, and organizational bureaucracy.22,37,38,40,44,45 Also with “freeze hire policy” in place, HCWs felt helpless to provide support to colleagues, while others felt anxious about not receiving the necessary support to conduct the DRTB care program. 43
Stigma reduction recommendations
Three key recommendations surfaced from the studies: (a) address IC issues; (b) increase the competence of healthcare workers; and (c) provide psychosocial assistance. In tackling IC, the recommendations centered on behavioral modification, skill enhancement, and implementation governance. One recommendation mentioned ensuring adequate IC supply, 39 while others recommended educating HCWs in IC control22,37 and ensuring compliance with IC policy. 40 Two studies recommend assessing the IC program and leadership to address HCWs’ mistrust in IC initiatives, traditional workplace practises, and workplace hierarchies that result in poor IC practices.38,42
Stigma reduction recommendations also included knowledge and capacity training, notably in the new DRTB care paradigm that includes primary health services. The recommendations addressed HCWs’ worry and anxiety around DRTB care changes by engaging and supporting them. One recommendation was for DRTB program managers to be mindful of the assistance required by the decentralized DRTB units. 43 Three studies recommended training41,43,45; however, continued mentoring, 41 and intensified information campaigns to curb DRTB stigma among HCWs and community were emphasized. 45
Most agreed that HCWs’ safety and security during DRTB activities is a priority.22,37,38,40,44,48 For example, one study recommended ensuring the confidentiality of information in DRTB facilities to encourage testing and diagnosis among HCWs, 39 while another recommended providing equitable compensation and free access to appropriate health services. 22 But for Probandari et al, 37 more research is needed to collect evidence about the effective strategies to reduce stigma among CHWs providing MDR-TB care.
Discussions
We found few studies, predominantly from South Africa and one each from Indonesia, the Philippines, and Tanzania. No literature review DRTB stigma among HCWs was found, so far. The stigma associated with communicable diseases 49 is consistent with this review. In this review, DRTB stigma is driven by fear of the disease, comparable to studies where HCWs reported stigma from infectious disease exposure.50-52 The inherent characteristics of DRTB, treatment toxicity, and poor treatment outcomes all contribute to stigmatization.9,53 We found that impacted HCWs engage in stigmatizing behaviors such as avoiding delivery care, transferring patients with DRTB quickly, or performing unnecessary overprotection IC practices.37,43 More concerning is the report that 82.1% of hospital staff and 42.9% of HCWs are less willing to work in DRTB-specific areas or continue to work as health workers. 39
Our analysis found multiple stigma facilitators, with healthcare system social and structural variables having the biggest impact. IC was frequently mentioned as requiring proper execution, not adhering to, or having its policy interpreted differently among stigma facilitators. HCWs worried about inadequate IC practice and complacency in their health facilities.22,38-40,42,44,46 Due to limited IC supply at health institutions, some HCWs were stigmatized for not following IC procedure.39,46 Even more alarming is the reluctance of other HCWs to adhere to the IC’s TB recommendations. 39 We found that the IC reluctance was due to lack of knowledge regarding DRTB risks or conflicting interpretations of IC policy.22,37,39,40,42,46 Unsurprisingly, inadequate IC in the workplace facilitates HCWs’ fear of the disease.
Working with stigmatized individuals or diseases promotes stigmatization54,55; and this is echoed in this review. We identified the stigmatizing experiences of HCWs, such as discrimination, isolation, rejection, and shame. For example, co-workers may reject HCWs if they become ill, but those who contracted DRTB delayed testing and diagnosis out of fear of discrimination and career implications. 39 Some HCWs with DRTB suffered anxiety and depression as a result of isolation from family and friends, or lost contact with colleagues due to extended absences from work.22,40,44,46 Yet concerning is leaving their families, particularly their children, to pursue DRTB treatment. 22
We, likewise, identified discriminating behaviors in the workplace. For instance, senior HCWs do not feel themselves to be in danger from the disease, hence blaming junior colleagues for IC wastage and limiting their access to supplies. 42 Arguably, stigmatizing tendencies are prevalent among HCWs who lack knowledge and training in DRTB.41,45,48 We also identified policies characterized by disparities in financial security among HCWs. Compared to those working in other high-risk settings, like HIV, some HCWs in DRTB wards do not receive a “danger pays,” day off on holidays, or compensation if they acquire DRTB.22,41 In another instance, some HCWs were excluded from training opportunities, thus felt discriminated.43,45
Additionally, we found that decentralization of DRTB care to community health centers also stressed HCWs. Fear and anxiety resulted from the increase in workload, with HCWs expressing concern about the lack of assistance from coordinators to guide them through the adjustments and aid them with patient-related issues, and coordinators experiencing stress due to excessive workloads.41-43 We found that an appointment moratorium prevented DRTB supervisory assistance. 43 Our findings support WHO’s 56 assertion that a lack of appropriate structures and support at work could adversely impact HCWs’ mental health, thereby hindering their capacity to enjoy and perform well at work.
Of note, data on the causes and facilitators of stigma are necessary for determining the most effective stigma reduction intervention in a given environment. 25 In this review, we identified the stigma drivers and facilitators that could assist the DRTB community with identifying the policies that need to be modified to promote a stigma-free healthcare environment. With our findings, we urge DRTB implementers and policymakers to enable policy revisions, notably regarding occupational health and safety, and HCW income protection.
Most studies concluded with stigma reduction interventions, emphasizing DRTB knowledge, current training (including refresher training), and capacity building on IC, and enhancing administrative IC operational standards. However, HCWs were concerned that training could not overcome stigma; implying that IC training could help reduce barriers to implementing IC, but not fear. This finding supports the claim that training alone is insufficient for sustainability if the healthcare system lacks infrastructure. 57 We found that continual mentoring and supportive supervision that improves knowledge and abilities may reduce stigma better because additional attention and on-the-job mentoring were deemed essential for HCWs to acquire confidence in providing DRTB care. 41
Notably, stigmatization in DRTB workforce is viewed as a result of both individual and institutional factors. This review, however, falls short of identifying stigma drivers and facilitators from multiple countries due to a significant lack of literature that explicitly characterizes the domains in DRTB-related stigma. The WHO 58 identifies many countries with significant TB and DRTB burdens combined; yet, only few countries have investigated the stigmatization of HCWs providing DRTB care. Also, workplace DRTB-associated stigma has just recently been recognized. We urge stakeholders, including academics and policymakers, to investigate stigma routes at facility level, focusing on HCWs experiencing stigma and those perpetuating stigma. Similarly, it is important to identify and understand the elements that facilitate and mediate stigmatization in a multi-level context, addressing the ecological and social pathways to DRTB stigma. 25
Strengths and Limitations
This review summarizes stigma among HCWs caring DRTB patients from TB- and DRTB-affected countries. So far, this is the first review to focus solely on DRTB stigma and HCWs. With limited studies found, our review is unable to comprehensively picture DRTB-associated stigma among HCWs; a significant information gap requiring attention. HCWs’ DRTB stigma needs further study at the facility, program, and national levels.
This review has some limitations. Despite attempts to be as exhaustive as possible, this review may not have found every study in the published and gray literature. The literature search’s inclusivity in terms of period, language, and study location may have missed some relevant studies. Our review is focused on studies conducted in countries with the highest TB and DRTB burdens, according to the WHO. While many TB- and DRTB-burden nations have non-English-speaking populations, this review may have omitted non-English studies. The MeSH search included phrases related to DRTB and health professionals, but they may not have been in the title or abstract.
Our review objective is to provide breadth rather than depth of evidence regarding DRTB related stigma confronting HCWs; thus, included studies regardless of research design, or outcome. Studies’ quality gives an overview of research effort on a topic but is not a reason for exclusion. The studies’ variabilities limit the conduct of meta-analysis, which is an inherent limitation of scoping reviews. We ensured a complete and transparent presentation of results by utilizing the recommended conventions of PRISMA-Scr.
Research and Practice Implications
Healthcare professionals and DRTB stigma have not yet been extensively studied. More research is needed to fully reflect DRTB stigma in healthcare and develop the requisite stigma reduction strategy and evaluate its efficacy. To overcome inequities and create effective, viable solutions that discourage stigma facilitators, policymakers must reconsider TB and DRTB policies, notably IC and risk-payments. Researchers need more data to critically identify the factors that contribute to and facilitate stigmatization among HCWs. It is prudent to take note of the WHO’s recommendation to expand country-specific DRTB research and Stangl et al’s 25 recommendation to investigate stigmatization across its socio-ecological range.
Conclusions
Our scoping research aims to identify the drivers and facilitators of stigma around HCWs providing crucial services for DRTB, particularly in countries with a high prevalence of TB and DRTB, as well as recommendations to reduce stigma. Despite the low number of studies reviewed, the findings imply that the stigma associated with DRTB in the healthcare sector is multifaceted and largely driven by the fear of infection. Other collective stigmas experienced by HCWs included discrimination, loneliness, insecurity, embarrassment and stress. Inconsistencies health workplace structure, such as conflicting IC interpretations and culture and values, also significantly contribute to the stigmatization among HCWs. Making HCWs feel safe while conducting DRTB activities is a priority issue that should be addressed. There are gaps in the literature, with no studies were found in most of the WHO’s high-burden TB and DRTB nations. Further research regarding country-specific and multi-level DRTB-related stigma among HCWs is necessary.
Supplemental Material
Supplemental material, sj-docx-1-inq-10.1177_00469580231180754 for Drug-Resistant Tuberculosis Stigma Among HealthCare Workers Toward the Development of a Stigma-Reduction Strategy: A Scoping Review by Lolita Liboon Aranas, Khorshed Alam, Prajwal Gyawali and Rashidul Mahumud Alam in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declarations: This study utilized secondary data and does require ethical committee approval. No editorial assistance was made for this manuscript.
Ethical Considerations: This study does not require ethical approval because of the study type.
ORCID iD: Lolita Liboon Aranas  https://orcid.org/0000-0003-3944-8470
https://orcid.org/0000-0003-3944-8470
Khorshed Alam  https://orcid.org/0000-0003-2232-0745
https://orcid.org/0000-0003-2232-0745
Supplemental Material: Supplemental material for this article is available online.
References
- 1.WHO. Tuberculosis. World Health Organizarion. January15, 2021. Accessed January 15, 2021. https://www.who.int/health-topics/tuberculosis [Google Scholar]
- 2.WHO. Tackling the Drug-Resistant TB Crisis. WHO. Accessed January 10, 2022. https://www.who.int/activities/tackling-the-drug-resistant-tb-crisis [Google Scholar]
- 3.Udwadia Z, Furin J.Quality of drug-resistant tuberculosis care: gaps and solutions. J Clin Tuberc Other Mycobact Dis. 2019;16:100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Isaakidis P, Smith S, Majumdar S, Furin J, Reid T.Calling tuberculosis a social disease—an excuse for complacency? Lancet. 2014;384(9948):1095. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Global TB Progress at Risk. World Health Organization; 2020. Accessed November 16, 2021. https://www.who.int/news/item/14-10-2020-who-global-tb-progress-at-risk [Google Scholar]
- 6.Kane JC, Elafros MA, Murray SM, et al. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med. 2019;17(1):17. doi: 10.1186/s12916-019-1250-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Link BG, Phelan JC.Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363-385. [Google Scholar]
- 8.Goffman E.Stigma: Notes on the Management of Spoiled Identity. Simon & Shuster; 1963:1963. [Google Scholar]
- 9.Craig G, Meershoek A, Zwerling A, et al. TB Stigma–Measurement Guidance. University of Hertfordshire. 2018. 10.18745/PB.20489 [DOI] [Google Scholar]
- 10.Evangelista de Andrade SL, Oliveira Diniz Pinheiro PG, de Cassia Cordeiro de Oliveira R, et al. The adherence for the tuberculosis treatment: the mark of stigma in the discourse of nurses. Int Arch Med. 2016;9. doi:10.3823/1965 [Google Scholar]
- 11.Nyblade L, Stockton MA, Giger K, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17(1):25. doi: 10.1186/s12916-019-1256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macq J, Solis A, Martinez G.Assessing the stigma of tuberculosis. Psychol Health Med. 2006;11(3):346-352. [DOI] [PubMed] [Google Scholar]
- 13.Mbuthia GW, Nyamogoba HDN, Chiang SS, McGarvey ST.Burden of stigma among tuberculosis patients in a pastoralist community in Kenya: A mixed methods study. PLoS One. 2020;15(10):e0240457. doi: 10.1371/journal.pone.0240457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dodor EA, Kelly SJ.Manifestations of tuberculosis stigma within the healthcare system: the case of Sekondi-Takoradi Metropolitan district in Ghana. Health Policy. 2010;98(2-3):195-202. [DOI] [PubMed] [Google Scholar]
- 15.Datiko DG, Habte D, Jerene D, Suarez P.Knowledge, attitudes, and practices related to TB among the general population of Ethiopia: Findings from a national cross-sectional survey. PLoS One. 2019;14(10):e0224196. doi: 10.1371/journal.pone.0224196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baral SC, Karki DK, Newell JN.Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health. 2007;7(1):211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thiruvalluvan E, Thomas B, Suresh C, Sellappan S, Muniyandi M, Watson B.The psychosocial challenges facing multi drug resistance tuberculosis patients: a qualitative study. SAARC J Tuberc Lung Dis HIV/AIDS. 2017;14(1):14-21. [Google Scholar]
- 18.Redwood L, Mitchell EMH, Viney K, et al. Depression, stigma and quality of life in people with drug-susceptible TB and drug-resistant TB in Vietnam. Int Journal Tuberculosis Lung Dis. 2021;25(6):461-467. doi: 10.5588/ijtld.20.0952 [DOI] [PubMed] [Google Scholar]
- 19.Das M, Mathur T, Ravi S, et al. Challenging drug-resistant TB treatment journey for children, adolescents and their care-givers: A qualitative study. PLoS One. 2021;16(3):e0248408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Macq J, Solis A, Martinez G, Martiny P.Tackling tuberculosis patients' internalized social stigma through patient centred care: an intervention study in rural Nicaragua. BMC Public Health. 2008;8(1):154-154. doi: 10.1186/1471-2458-8-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O'Donnell MR, Daftary A, Frick M, et al. Re-inventing adherence: toward a patient-centered model of care for drug-resistant tuberculosis and HIV. Int Journal Tuberculosis Lung Dis. 2016;20(4):430-434. doi: 10.5588/ijtld.15.0360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tudor C, Mphahlele M, Van der Walt M, Farley JE.Health care workers' fears associated with working in multidrug- and or extensively-resistant tuberculosis wards in South Africa. Int J Tuberc Lung Dis. 2013;17(10Suppl 1):22-29. doi: 10.5588/ijtld.13.0109 [DOI] [PubMed] [Google Scholar]
- 23.Thomas BE, Shanmugam P, Malaisamy M, et al. Psycho-socio-economic issues challenging multidrug resistant tuberculosis patients: A systematic review. PLoS One. 2016;11(1):e0147397. doi: 10.1371/journal.pone.0147397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cannon L-AL, Kelechi Elizabeth O, Daniel TG.Socio-Economic Drivers of Drug-Resistant Tuberculosis in Africa: A Scoping Review. Research Square; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stangl AL, Earnshaw VA, Logie CH, et al. The Health Stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sommerland N, Masquillier C, Rau A, et al. Reducing HIV- and TB-Stigma among healthcare co-workers in South Africa: Results of a cluster randomised trial. Soc Sci Med. 2020;266:113450. [DOI] [PubMed] [Google Scholar]
- 27.Canadian Institute for Health Research. Knowledge translation. April2, 2022. https://cihr-irsc.gc.ca/e/29418.html
- 28.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E.Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Uman LS.Systematic reviews and meta-analyses. J Am Acad Child Adolesc Psychiatry. 2011;20(1):57-59. [PMC free article] [PubMed] [Google Scholar]
- 30.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 31.Peters MDJ, Marnie C, Colquhoun H, et al. Scoping reviews: reinforcing and advancing the methodology and application. Syst Rev. 2021;10(1):263. doi: 10.1186/s13643-021-01821-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMAScR): Checklist and explanation. Ann Intern Med. 2018;169:467-473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 33.Aranas LL, Alam K, Gyawali P, Mahumud RA.Examining Drug-resistant tuberculosis stigma among health care workers toward the development of a stigma-reduction intervention: Protocol for a Scoping Review. JMIR Res Protoc. 2023;12:e43084. doi: 10.2196/43084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: Scoping reviews (2020 version). In: Aromataris E, Munn Z. (eds) Manual for Evidence Synthesis. JBI; 2020. Available from https://synthesismanual.jbi.global; 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- 35.Noyes J, Booth A, Cargo M, et al. Chapter 21: Qualitative Evidence. Cochrane. Accessed March 16, 2022. https://training.cochrane.org/handbook/current/chapter-21 [Google Scholar]
- 36.Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA.A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371-385. doi: 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Probandari A, Sanjoto H, Mahanani MR, Azizatunnisa L, Widayati S.Being safe, feeling safe, and stigmatizing attitude among primary health care staff in providing multidrug-resistant tuberculosis care in Bantul District, Yogyakarta Province, Indonesia. Hum Resour Health. 2019;17(1):16. doi: 10.1186/s12960-019-0354-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zelnick JR, Gibbs A, Loveday M, Padayatchi N, O'Donnell MR. Health-care workers' perspectives on workplace safety, infection control, and drug-resistant tuberculosis in a high-burden HIV setting. J Public Health Policy. 2013;34(3):388-402. doi: 10.1057/jphp.2013.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kanjee Z, Catterick K, Moll AP, Amico KR, Friedland GH.Tuberculosis infection control in rural South Africa: Survey of knowledge, attitude and practice in hospital staff. J Hosp Infect. 2011;79(4):333-338. doi: 10.1016/j.jhin.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 40.Padayatchi N, Daftary A, Moodley T, Madansein R, Ramjee A.Case series of the long-term psychosocial impact of drug-resistant tuberculosis in HIV-negative medical doctors. Int J Tuberc Lung Dis. 2010;14(8):960-966. [PubMed] [Google Scholar]
- 41.Lyakurwa D, Lyimo J, Mulder C, Pelzer PT, Koppelaar I, Heus M.Assessment of training and mentoring for DR-TB care decentralization in Tanzania. Hum Resour Health. 2021;19(1):56. doi: 10.1186/s12960-021-00600-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Daftary A, Padayatchi N.Provider perspectives on drug-resistant tuberculosis and human immunodeficiency virus care in South Africa: a qualitative case study. Int J Tuberc Lung Dis. 2016;20(11):1483-1488. doi: 10.5588/ijtld.16.0111 [DOI] [PubMed] [Google Scholar]
- 43.Vanleeuw L, Atkins S, Zembe-Mkabile W, Loveday M.Provider perspectives of the introduction and implementation of care for drug-resistant tuberculosis patients in district-level facilities in South Africa: a qualitative study. BMJ Open. 2020;10(2):e032591. doi: 10.1136/bmjopen-2019-032591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.von Delft A, Dramowski A, Sifumba Z, et al. Exposed, but not protected: More is needed to prevent drug-resistant tuberculosis in healthcare workers and students. Clin Infecti Dis. 2016;62:S275-S280. doi: 10.1093/cid/ciw037 [DOI] [PubMed] [Google Scholar]
- 45.Jaramillo J, Endo Y, Yadav R-P.Clinician perspectives of drug-resistant tuberculosis care services in the Philippines. Indian J Tuberc. 2023;70:107-114. doi: 10.1016/j.ijtb.2022.03.022 [DOI] [PubMed] [Google Scholar]
- 46.Naidoo A, Naidoo SS, Gathiram P, Lalloo UG.Tuberculosis in medical doctors – a study of personal experiences and attitudes. S Afr Med J. 2013;103(3):176-180. doi: 10.7196/samj.6266 [DOI] [PubMed] [Google Scholar]
- 47.Pulerwitz J, Oanh KT, Akinwolemiwa D, Ashburn K, Nyblade L.Improving hospital-based quality of care by reducing HIV-related stigma: evaluation results from Vietnam. AIDS Behav. 2015;19(2):246-256. [DOI] [PubMed] [Google Scholar]
- 48.Naidoo P, Peltzer K, Louw J, Matseke G, McHunu G, Tutshana B.Predictors of tuberculosis (TB) and antiretroviral (ARV) medication non-adherence in public primary care patients in South Africa: A cross sectional study. BMC Public Health. 2013;13(1):396-396. doi: 10.1186/1471-2458-13-396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fischer LS, Mansergh G, Lynch J, Santibanez S.Addressing disease-related stigma during infectious disease outbreaks. Disaster Med Public Health Prep. 2019;13(5-6):989-994. doi: 10.1017/dmp.2018.157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stringer KL, Turan B, McCormick L, et al. HIV-related stigma among healthcare providers in the deep south. AIDS Behav. 2016;20(1):115-125. doi: 10.1007/s10461-015-1256-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Villa S, Jaramillo E, Mangioni D, Bandera A, Gori A, Raviglione MC.Stigma at the time of the COVID-19 pandemic. Clin Microbiol Infect. 2020;26(11):1450-1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Engelbrecht M, Rau A, Kigozi G, et al. Waiting to inhale: factors associated with healthcare workers' fears of occupationally-acquired tuberculosis (TB). BMC Infect Dis. 2019;19(1):475-475. doi: 10.1186/s12879-019-4115-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jang JG, Chung JH.Diagnosis and treatment of multidrug-resistant tuberculosis. Yeungnam Univ J Med. 2020;37(4):277-285. doi: 10.12701/yujm.2020.00626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jesse SR.Secondary Stigma for Professionals Who Work With Marginalized Groups: A Comparative Study. Bowling Green State University; 2015. [Google Scholar]
- 55.Courtwright A, Turner AN. Tuberculosis and stigmatization: Pathways and interventions. Public Health Rep. 2010;125(Suppl 4):34-42. doi: 10.1177/00333549101250s407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.WHO. Mental Health at Work. WHO. January26, 2023. Accessed January 26, 2023. https://www.who.int/news-room/fact-sheets/detail/mental-health-at-work [Google Scholar]
- 57.Ehrlich R, Spiegel JM, Adu P, Yassi A.Current guidelines for protecting health workers from occupational tuberculosis are necessary, but not sufficient: towards a comprehensive occupational health approach. Int J Environ Res Public Health. 2020;17(11):3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.WHO. WHO global lists of high burden countries for tuberculosis (TB), TB/HIV and multidrug/rifampicin-resistant TB (MDR/RR-TB), 2021–2025. CC-BY-NC-SA 3.0 IGO. https://cdn.who.int/media/docs/default-source/hq-tuberculosis/who_globalhbcliststb_2021-2025_backgrounddocument.pdf?sfvrsn=f6b854c2_9
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-inq-10.1177_00469580231180754 for Drug-Resistant Tuberculosis Stigma Among HealthCare Workers Toward the Development of a Stigma-Reduction Strategy: A Scoping Review by Lolita Liboon Aranas, Khorshed Alam, Prajwal Gyawali and Rashidul Mahumud Alam in INQUIRY: The Journal of Health Care Organization, Provision, and Financing