Abstract
Background
Acute respiratory distress syndrome (ARDS) is a severe and life-threatening condition that can occur in critically ill patients. Mechanical ventilation is a commonly used intervention with ARDS patients, but weaning patients off the ventilator can be challenging. An ARDSnet-like ventilator weaning protocol was implemented with the goal of reducing triggers for ventilator-associated events (VAEs).
Methods
The implementation of the new protocol was used to complete a retrospective investigation of patient outcomes for 1,233 ventilator periods. Periods were included between April and December 2022 for any ventilated patient lasting at least four days. National Healthcare Safety Network (NHSN) VAE criteria was used to surveille the patient data. Triggers were based on positive end expiratory pressure (PEEP) increases or fraction of inspired oxygen (FiO₂) increases. The pre-set weaning criteria was a reduction by two cmH2O per 24 hours.
Results
Of the total 1,233 individual ventilator periods, VAE criteria were met in 10%. Of the total 126 periods with VAE, 39.2% met criteria for appropriate protocol implementation. There was a statistically significant relationship between VAE identification and implementation of the protocol.
Conclusions
The implementation of a protocol for ventilator weaning affects the outcome of developing a VAE. The findings emphasize the importance of implementing ARDS weaning protocol as a template to reduce the triggers for VAEs and improve overall patient outcomes.
Keywords: Acute Respiratory Distress Syndrome (ARDS), Mechanical ventilation, Ventilator–associated Events (VAE), Infection related ventilator-associated complications (IVAC), Possible ventilator- associated pneumonia (PVAP), Trauma, Ventilator-Associated Condition (VAC), Burn, Ventilator weaning protocol
BACKGROUND
Acute Respiratory Distress Syndrome (ARDS) is a common critical illness that requires mechanical ventilation to support respiratory function.1 ARDS requires appropriate management of mechanical ventilation to improve patient prognosis and reduce incidence of VAEs.2 Prolonged mechanical ventilation is linked to issues like ventilator-induced lung injury (VILI), muscle weakness, and infections, which can result in higher morbidity and mortality rates.3 Multiple complications, like fluid imbalanced and trauma, associated with ARDS may exacerbate existing respiratory issues. 3 The National Healthcare Safety Network (NHSN) uses the term “ventilator-associated events” (VAEs) to refer to a range of problems that may occur in patients who need mechanical ventilation to maintain their respiratory capability.4 Major influences on VAEs may include pneumonia, lung damage, and other ailments that contribute further to the incidence of impaired respiratory function.
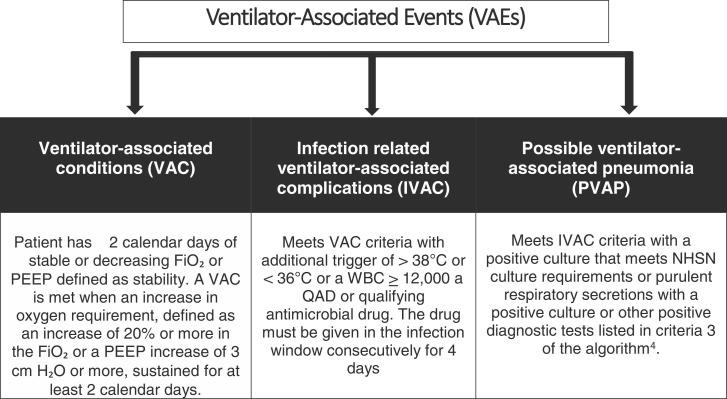
The NHSN criteria establishes clear guidelines to determine when a new VAE is defined and when the current VAE moves up through the higher risk VAE ( Figure 1).4 A patient starting with mechanical ventilation that is maintained following the protocol may never meet criteria for a ventilator-associated condition (VAC). However, once a VAC is determined, the risk for an infection related ventilator-associated complication (IVAC) or possible ventilator-associated pneumonia (PVAP) greatly increases. Due to multiple variables, including extended mechanical ventilation and reduced immunological function, patients with ARDS are more likely to acquire VAEs.5, 6 Increased pneumonia risk is one of the main ways that ARDS affects VAE.3 Pneumonia may exacerbate general health and cause additional lung damage. Patients with traumatic injuries such as rib fractures, pulmonary contusions, pneumothorax, or aspiration are placed at a higher risk for the development of VAE and pneumonia.7, 8
Fig. 1.
VAE categories:.
Ventilator weaning is a complex process that requires an implementation of evidence-based, lung protective strategies.9 Understanding the best practices for ventilator weaning in ARDS patients is critical in reducing morbidity and mortality associated with prolonged mechanical ventilation.9 The outcome of the study was to determine if an association exists between the implementation of an evidence-based protocol for mechanically ventilated patients and subsequent development of VAE.
METHODS
A new protocol was developed through collaboration of a ventilator work group including intensivists, Chief Medical Officer, infection preventionists, and respiratory therapists. The implementation of the new protocol was used to complete a retrospective investigation of patient outcomes for 1,233 ventilator periods which includes a new ventilator period if there is at least one full calendar day break between ventilator removals. All patients that had a ventilator period of at least four days was included. Those with three or fewer ventilator days were excluded as they would not meet criteria for a VAE. The study included periods between April 2022 and December 2022. The specialty ICU units included services from burn, cardiovascular, medical, neurosurgical, and trauma. In these ICUs there were 173 beds and all ventilated patients had the protocol ordered. The ICUs were chosen due to the broad type of potential ventilator management based on the patient medical needs, including traumatic injuries and/or medical conditions. The protocol was implemented to identify ventilator parameters and adjustments to FiO₂ to optimize the management for each individual patient. The protocol provides a sliding scale method for oxygenation-based positive end expiratory pressure (PEEP) increases or fraction of inspired oxygen (FiO₂) adjustment. The protocol was followed for patients with acute lung injury or (ARDS) when ordered by the physician. FiO₂ and PEEP were adjusted using the criteria listed in Table 1.
Table 1.
Oxygenation Goal Table:.
| Oxygenation Goal TABLE | |||||||
|---|---|---|---|---|---|---|---|
| FIO2 | 0.4 | 0.5 | 0.6 | 0.7 | 0.8 | 0.9 | 1.0 |
| PEEP | 8 | 10 | 12 | 14 | 14 | 16 | 18 |
The protocol scale outlines goals for the initiation and escalation of PEEP values when oxygenation needs increase. The scale was not to be used for rapid de-escalation of PEEP when FiO₂ is decreased. PEEP and FiO₂ adjustments were based on the oxygenation goal when responding to the patient’s whole clinical picture. If a PEEP greater than 12 cmH2O is needed for multiple days in a row, then when weaning PEEP, the baseline should not be reduced by more than two cmH2O every 24 hours.10 The application of PEEP improves gas exchange and lung function. The main effect of increasing PEEP is to maintain the recruitment of alveolar units that were previously collapsed. Thus, since the tidal volume is distributed to more alveoli, peak airway pressure is reduced and elasticity is increased., 11 It is not recommended to lower the PEEP faster than 2 cmH₂O per day or below eight cmH₂O for this population. When determining whether extubation is appropriate, a brief time interval of PEEP of five may be used. If FiO₂ requirements are rising in response to provider orders, PEEP may be increased and adjusted more frequently to achieve adequate oxygenation levels. An added benefit of using the oxygenation goals is that inadvertent triggers for VAE are avoided. A chi-square test of independence was performed to examine the relationship between the implementation of an ARDSnet-like evidence-based lung protective protocol for mechanically ventilated patients and development of VAE.
RESULTS
In this period, a total of 56,127 patient days occurred with 16,360 ventilator days which were spread among seven intensive care units (ICU). The highest percentage of the total VAE were in medical, cardiovascular and trauma ICUs ( Table 2). Ventilator utilization per 100 patient days for the top three services were medical, cardiac (step down from cardiovascular), and trauma (Table 2). The rate of VAE per 1,000 ventilator days was the highest in order cardiovascular, burn, cardiac, and trauma (Table 2).
Table 2.
VAE Totals and Ventilator Utilization.
| Total VAE | Ventilator Utilization per 100 patient days | Rate of VAE per 1,000 vent days | |
|---|---|---|---|
| Burn | 5 | 11.11 | 12.76 |
| Cardiac | 8 | 42.1 | 9.22 |
| Medical Step-down | 1 | 17.45 | 0.42 |
| Cardiovascular | 20 | 12.29 | 17.75 |
| Medical | 55 | 53.31 | 8.90 |
| Neuro | 10 | 30.57 | 5.19 |
| Trauma | 27 | 35.32 | 7.71 |
| Total | 126 | 29.15 | 61.95 |
NHSN VAE classifications were used for the study period of April through December 2022.The overall total of ventilator periods was 1,233 ( Table 3). Of the total 1,233 periods, 66% of the periods followed the protocol. Of the 66% (813), 6% were complicated by a VAE. Of the total 49 periods where a VAE developed, 53% developed into a VAC, 37% developed into an IVAC, and 10% developed into a PVAP after following the protocol. VAC developed in 44.6% less periods when the protocol was implemented compared to when the protocol was not implemented. Similarly, IVAC developed 18.2% less and PVAP developed 28.6% less when the protocol was implemented. The association between the implementation of an ARDSnet-like evidence-based lung protective protocol for mechanically ventilated patients and development of VAE was significant, X 2(2, N =1,233) = 44.2728, p =.00001. There is an a statistically significant relationship between the implementation of an ARDSnet-like protocol and development of a VAE. Overall, the VAEs identified when protocol was not implemented outweighed the VAEs where the protocol was implemented by 35.5%.
Table 3.
Crosstabulation of Protocol Followed and Type of VAE Identified Protocol.
| PROTOCOL FOLLOWED |
||||
|---|---|---|---|---|
| NO | YES | TOTAL | ||
| VAC | Count | 47 | 26 | 73 |
| IVAC | Count | 22 | 18 | 40 |
| PVAP | Count | 7 | 5 | 12 |
| No VAE | Count | 344 | 764 | 1108 |
| Total | Count | 420 | 813 | 1233 |
DISCUSSION
Implementation of a ventilator weaning protocol has a statistically significant relationship with the development of a VAE. Based on the results, reduction occurred in all levels of the VAE algorithm when the protocol was implemented. The findings show that a decrease in VAE triggers leads to a decrease in progression of the clinical processes that can lead to further respiratory complications including mortality12. In line with other research comparing NHSN and PVAP outcomes, the periods showed similar distribution with trauma having the second highest VAEs identified while having the fourth highest ventilator utilization rates.12 The protocol outlines a consistent process for implementing standardized ventilator management coordination. The time when the highest patient risk for events existed was post implementation of PEEP levels of 13 to 20 cm H₂O. Implementation of the protocol was a mitigation technique. Lung integrity is maintained by reducing the PEEP by only 2 cm H2O per 24 hours. FiO2 levels can be reduced more aggressively when weaning high PEEP levels because the lung integrity is maintained by functional residual capacity which is already sustained by the PEEP. The level of periods where a VAE did not develop showed that regardless of underlying medical issues, the protocol achieves a successful outcome by gradually lowering the ventilator's level of support while maintaining the patient's respiratory function and while appropriately reacting to the needed clinical changes. A properly implemented ARDS ventilator weaning approach is crucial for enhancing patient outcomes, potentially lowering morbidity and mortality while potentially maximizing hospital resource use.
ETHICAL CONSIDERATIONS
Data access to the secondary data set required permission via a publisher clearing process through the company submitted by the primary author. Confidentiality, honesty, and integrity in all data gathering, storage, and use were consistently maintained. All data were kept secured via password protection for at least 5 years.
CONCLUSIONS
The results showed a statistically significant association between implementation of the protocol and development of a VAE. The findings reiterate the importance of implementing a protocol to reduce the triggers for VAE and improving overall patient outcomes. Protocol implementation as a part of a multidisciplinary process, can assist patients in recovering their ability to breathe on their own while lowering the chance of consequences related to ventilation such as pneumonia, infections, and other respiratory issues.
DISCLAIMER
This research was supported (in whole or in part) by HCA Healthcare and/ or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Conflict of Interest
No conflict of interests to disclose
References
- 1.Saguil, A., & Fargo, M.V. (2012). Acute respiratory distress syndrome: diagnosis and management. American fam. [PubMed]
- 2.Sim J.K., Oh J., Min K., Hur G., Lee S.H., Lee S.Y., Kim J., Shin C., Shim J., Kang K. Clinical significance of ventilator-associated event. Journal of Critical Care. 2016;35:19–23. doi: 10.1016/j.jcrc.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Magill S.S., Rhodes B., Klompas M. Improving ventilator-associated event surveillance in the National Healthcare Safety Network and addressing knowledge gaps: update and review. Current opinion in infectious diseases. 2014;27(4):394–400. doi: 10.1097/QCO.0000000000000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Healthcare Safety Network. (2023), Ventilator-Associated Event (VAE) - CDC. 〈https://www.cdc.gov/nhsn/pdfs/pscmanual/10-vae_final.pdf〉.
- 5.Magill S.S., Klompas M., Balk R., Burns S.M., Deutschman C.S., Dikeman D., Lipsett P. ). Developing a new, national approach to surveillance for ventilator-associated events: executive summary. Clinical infectious diseases. 2013;57(12):1742–1746. doi: 10.1093/cid/cit577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Villar J. The use of positive end-expiratory pressure in the management of the acute respiratory distress syndrome. Minerva Anestesiol 2005;71(6):265-272.Klompas M. Interobserver variability in ventilator-associated pneumonia surveillance. Am J Infect Control 2010;38: 237-9.ily physician, 85(4), 352-358. [PubMed]
- 7.Cook A., Norwood S., Berne J. Ventilator-associated pneumonia is more common and of less consequence in trauma patients compared with other critically ill patients. J Trauma. 2010;69(5):1083–1091. doi: 10.1097/TA.0b013e3181f9fb51. Nov. [DOI] [PubMed] [Google Scholar]
- 8.Rello J., Ollendorf D.A., Oster G., Vera-Llonch M., Bellm L., Redman R., Kollef M.H., VAP Outcomes Scientific Advisory Group Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest. 2002;122(6):2115–2121. doi: 10.1378/chest.122.6.2115. Dec. [DOI] [PubMed] [Google Scholar]
- 9.Wawrzeniak I.C., Regina Rios Vieira S., Almeida Victorino J. Weaning from Mechanical Ventilation in ARDS: Aspects to Think about for Better Understanding, Evaluation, and Management. BioMed research international. 2018;2018 doi: 10.1155/2018/5423639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papazian L., Aubron C., Brochard L., Chiche J.D., Combes A., Dreyfuss D., Faure H. Formal guidelines: management of acute respiratory distress syndrome. Annals of intensive care. 2019;9(1):1–18. doi: 10.1186/s13613-019-0540-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pintado M.C., de Pablo R., Trascasa M., Milicua J.M., Rogero S., Daguerre M., Sánchez-García M. Individualized PEEP setting in subjects with ARDS: a randomized controlled pilot study. Respiratory care. 2013;58(9):1416–1423. doi: 10.4187/respcare.02068. [DOI] [PubMed] [Google Scholar]
- 12.Michetti C.P., Fakhry S.M., Ferguson P.L., Cook A., Moore F.O., Gross R. AAST Ventilator-Associated Pneumonia Investigators. Ventilator-associated pneumonia rates at major trauma centers compared with a national benchmark: a multi-institutional study of the AAST. J Trauma Acute Care Surg. 2012;72(5):1165–1173. doi: 10.1097/TA.0b013e31824d10fa. May. [DOI] [PubMed] [Google Scholar]