Abstract
Oral Medicine is a young dental specialty born almost a century ago and deals with orofacial conditions not directly attributable to the most prevalent tooth pathologies such as dental caries or periodontal diseases. Presentations may reflect local disease or orofacial manifestations of more widespread pathology affecting other parts of the body. Due to its recency as a distinct discipline and to heterogeneous global settings, Oral Medicine has not yet achieved a shared scope and definition, as well as a recognized status across the globe. The current report presents survey data gathered from Oral Medicine practitioners in Europe and Australia and aimed to identify practitioner characteristics including demographics, training, clinical and research activity. As expected, Oral Medicine clinical practice commonly deals with conditions such as immune‐mediated disorders, potentially malignant disorders, oral mucosal infections and chronic pain disorders, but geographical heterogeneities are observed. The present data, representative of current clinical practice, are valuable in order to understand the evolution of Oral Medicine as a distinct discipline and should be taken into consideration in order to create or update postgraduate training curricula able to meet the needs of future practitioners and the communities they serve.
Keywords: clinical practice, oral disorders, oral medicine, research activity, training pathways
1. BACKGROUND
Oral Medicine (OM) is a young dental specialty born almost a century ago in the United States treating patients with complex oral mucosal manifestations. Such demanding clinical conditions lead to the combination of knowledge in general medicine, dermatology and pathology to provide care to such patients (Shklar & McCarthy, 2008).
Briefly, it could be stated that OM practice includes diagnosis and management of orofacial conditions not directly attributable to the most prevalent tooth‐related pathologies such as dental caries or periodontal diseases. Presentations may reflect specific mouth disease or orofacial manifestations of systemic multifocal conditions. Nevertheless, the scope, definition and academic education vary significantly across the world (Bez et al., 2017; Scully et al., 2016). The field of Oral Medicine independently developed across the globe and the young age of this discipline, jointly with diversity of cultures and heterogeneity of global settings and healthcare systems, has led to differences in its practice (Bez et al., 2017; Scully et al., 2016).
Few studies have investigated OM practice in the last decade. They provide descriptive information from single or multiple geographical settings (Farah et al., 2008; Pinto et al., 2015; Stoopler et al., 2011) without an attempt to analyse variations potentially related to distinct geographical locations or to differences in training pathways and national regulatory requirements. This study aimed to provide information about the practice of OM among Oral Medicine expert practitioners (OMPs) across European countries and Australia. The understanding of potential geographical variations may lead to knowledge of the spectrum of OM practice as it further develops across these jurisdictions and beyond.
2. METHODS
Data used for the current report derived from a 93‐item survey designed by the European Association of Oral Medicine (EAOM) Position Paper on Diagnosis and Management of Oral Leukoplakia Team aiming to analyse clinical practice variability in the diagnosis and management of oral potentially malignant disorders (OPMD) and early oral squamous cell carcinoma (OSCC). By means of consensus, a questionnaire including previously validated items, as well as items specifically designed for the survey, was developed in English and pretested on a group of potential respondents to ensure practicability, validity and interpretation of answers. The whole survey took approximately 10–25 min to complete. The wide range of questions and potential answers relies on the use of skip logic branching creating a custom path through the survey based on a respondent's answers. All responses were completely anonymous. The sections of the survey which were used for the present study can be accessed in the File S1.
To obtain a representative sample of OMPs from Europe and Australia, members of the European Association of Oral Medicine (EAOM) and the Oral Medicine Academy of Australasia (OMAA) were invited to participate in the survey. An email was sent to members of both organizations in June 2018 with a cover letter describing the study's aim and a link to participate. In order to avoid potential duplicate responses, duplicated email addresses were removed from the OMAA mailing list. The survey was administered through SurveyMonkey®. Mailing was repeated 15 and 45 days after the first post.
The first section of the questionnaire (17 questions) collected respondents’ demographic/background information and assessed respondents’ sociodemographic characteristics, type of under‐ and postgraduate training received, country where under‐ and postgraduate degrees were obtained, workplace country, workplace setting (public hospital, university hospital, private practice), rate of working time devoted to research activity, nature of current clinical practice (rate of clinical practice devoted to oral medicine or oral pathology or oral surgery or special needs dentistry or general dentistry) and research activities (rate of research activities devoted to laboratory, translational, clinical or epidemiological).
Respondents were asked to specify (in percentage) their extent of engagement in diagnosis and treatment of diseases and disorders as outlined in Figure 1. Similarly, respondents were asked to rank their research activity related to the same disease categories.
FIGURE 1.

Oral medicine clinical practice based on type of disease/disorder diagnosed
In addition to the first 17‐item section, two additional questions were included in order to investigate the habit of self‐performing of biopsy or surgical treatment for oral leukoplakia or early OSCC (stage 1 tumour not requiring nodal dissection (Brierley et al., 2017)).
2.1. Data evaluation and statistical analysis
Responses were collated electronically and held securely at the Oral Medicine and Oral Oncology Section of the Department of Oncology, University of Torino, Italy. Data were entered into an SPSS database, and analyses were performed using SPSS release 26.0 (SPSS Inc.). The “EAOM Regions” as reported in Table 1 and the OMAA membership (henceforth jointly referred as Regions) served to assess geographical variations associated with sociodemographic characteristics, academic training or clinical practice. Due to strong heterogeneity, EAOM respondents from Region 6 were included in the present study only if practising in Australia. Analyses were carried out in two stages. Firstly, descriptive statistics (frequency/per cent distribution) were generated to describe the sample and each response from the survey. The chi‐square test was employed to detect possible associations in the presence of dichotomous or qualitative data. Depending on the normal or non‐normal distribution of quantitative data, one‐way analysis of variance (ANOVA) or non‐parametric tests (independent‐samples Kruskal–Wallis or Mann–Whitney U test) were used to determine the presence of any statistically significant differences between groups identified by nominal variables (i.e. gender, EAOM Regions/OMAA, OMPs mainly practising OM, OMPs with low/high involvement in research). The Spearman's rho correlation coefficient was used to assess the relationship between OMPs’ engagement in diagnosis and treatment of different groups of disorders and to assess the relationship between OMPs’ engagement in different groups of disorders.
TABLE 1.
EAOM Regions
| EAOM Region | Country |
|---|---|
| Region 1 | Ireland, UK |
| Region 2 | Denmark, Estonia, Finland, Iceland, Latvia, Lithuania, Norway, Sweden |
| Region 3 | Austria, Belgium, Czech Republic, Germany, Hungary, Luxemburg, Netherlands, Poland, Slovakia, Switzerland |
| Region 4 | France, Italy, Portugal, Spain, Malta |
| Region 5 | Albania, Bosnia Herzegovina, Bulgaria, Croatia, Cyprus, Greece, Israel, Romania, Russia, Serbia, Slovenia, Ukraine, Turkey |
| Region 6 | Rest of the world |
EAOM Regions are geographical grouping representing institutional entities within the EAOM. Countries in bold are represented by at least 5 respondents.
3. RESULTS
3.1. Respondents
Excluding EAOM Region 6 members as described above, invitations were sent to 276 subjects: 242 EAOM members and 34 OMAA members.
One hundred forty subjects participated corresponding to a response rate of 50.7%. No significant differences between EAOM and OMAA members were observed in the response rate (p = .201), and the EAOM respondents were representative of the 5 EAOM Regions (Table 2). Among respondents, 52.1% were male with small variations among regions. The mean age was 47.6 years, with females significantly younger than males (43.3 SE 1.2 versus 51.6 SE 1.5; p < .001). Examining each Region, differences in age were observed in Region 1 and in Australia, where 52.6% of OMPs were under 40 years of age, while the highest mean age was found in Region 2 (Figure 2).
TABLE 2.
Geographical distribution, gender and age of respondents
| Response rate | Gender | Age | ||
|---|---|---|---|---|
| (F/M) | Median ± ½ IQR years | |||
| EAOM Region 1 | 28/67 | 41.8% | 14/14 | 44 ± 9 |
| EAOM Region 2 | 14/23 | 60.9% | 6/8 | 57 ± 8.5 |
| EAOM Region 3 | 11/27 | 40.7% | 6/5 | 60 ± 11 |
| EAOM Region 4 | 41/68 | 60.3% | 16/25 | 42 ± 10.5 |
| EAOM Region 5 | 27/57 | 47.4% | 14/13 | 48 ± 18 |
| OMAA | 19/34 | 55.9% | 11/8 | 39 ± 9 |
| Total | 140/276 | 50.7% | 67/73 | 45.5 ± 10.5 |
FIGURE 2.

Mean age profile of respondents in different geographical regions
3.2. Training
Most respondents had an undergraduate dental degree (78%); the double qualification (medical and dental degree) characterizing 12% of respondents, while the remaining 10% held only a medical degree. From a geographical standpoint, several distinctions were observed. The Netherlands had the lowest rate of practitioners qualifying with a dental undergraduate education: dentally qualified OMPs only represented 17%, while double‐qualified OMPs represented 50%, and medically qualified represented 33%. Excluding this observation, dual‐qualified practitioners were more frequently located in Region 1 (30%).
Dentally qualified OMPs were significantly younger than medically qualified (p = .007) or dual‐qualified counterparts (p = .044) (Figure 3). This is particularly evident in specific geographical settings. In Spain, all medically qualified OMPs were over the age of 58, while all dentally qualified OMPs were under 49 years of age. Similarly, in Italy, all medically qualified OMPs were over the age of 56, and all dentally qualified OMPs under the age of 52.
FIGURE 3.
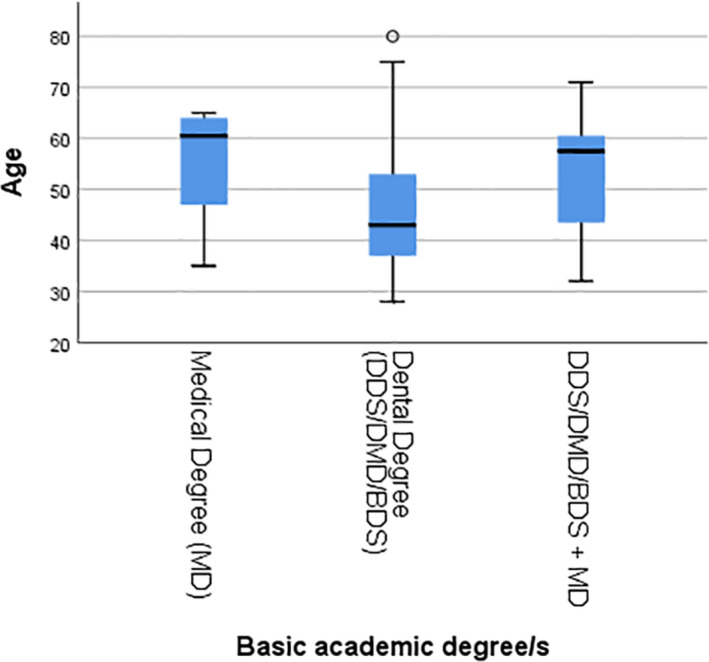
Age of respondents with different undergraduate degrees
Analyses focused on postgraduate training were performed on respondents over 35 years of age (114 out of 140 respondents). Most attended an OM postgraduate training programme (83%). This ranged from 70% in Regions 2 and 4 to 100% in Australia without significant geographical variations. An increasing trend negatively related to age was observed overall (p = .002) (Figure S1). Age‐related differences were observed only in Region 4 particularly due to data from Italy (p = .001). Postgraduate training was frequently attained abroad (22.5%), with the UK representing the most frequent destination (48%) followed by Spain (16%) and United States (12%). Respondents who chose to study abroad had obtained their undergraduate degree in Portugal (24%), Italy (14%) or Greece (12%). Conversely, all OMPs who graduated in Region 1 continued their postgraduate training there. The lack of OM as a recognized specialty was not significantly associated with the choice of undertaking postgraduate OM training abroad. Of note, a large proportion of practitioners who attended postgraduate training programmes abroad remained there to practice (36.8%).
A large proportion of respondents held a postgraduate degree in disciplines other than OM (65.1%). A postgraduate degree in orofacial pain was most frequently attained by medically qualified OMPs (p = .004); no other association between under‐ and postgraduate training was observed. Both Regions 1 and 5 had low proportions of concurrent postgraduate degrees compared to other Regions, approximately 43% and 48%, respectively (p = .013). Oral/Maxillofacial Surgery (25.7%) and Oral Pathology (20.2%) were the most frequently held disciplines, while a low number of respondents held a postgraduate degree in Orofacial Pain (6.4%) or Special Needs Dentistry (3.7%). Of note, when considering Oral/Maxillofacial Surgery and Oral Pathology, the interest in these specialties significantly varied between Regions (chi‐square test; p = .002 and p = .009, respectively). In Region 3, 78% of respondents had surgical postgraduate training; this proportion decreased to 31% for Region 4, 20% for Regions 1, 2 and 5, with no OMPs with postgraduate surgical training in Australia. Conversely, Australia had the highest proportion of respondents with a postgraduate degree in Oral Pathology (58%), compared to European countries. In Regions 2, 3 and 5, this was approximately 22%, while the lowest was observed in Region 1 (4.8%).
3.3. Workplace and OM practice setting
Almost all respondents (97.5%) practice OM in hospitals, either Public or University, and most do not practice OM in private practice (58.5%). When private practice opportunities were available, respondents stated that this accounted for 50% of their clinical time. In any European Region, 65%–85% of respondents spent more than 40% of their working time in University Hospitals. Conversely in Australia, a high proportion of respondents (46.6%) spent most of their time in a private practice setting.
3.4. Clinical practice
In the present analyses, OM was considered the main field of clinical practice of respondents when this exceeded 40% of their time. Most respondents (75.9%) mainly practised OM, but significant differences were observed between Regions (p = .007). In Regions 1 and 2 and Australia, this ranged from 83% to 96%, in Region 5 (71%), and in Regions 3 and 4 (57%–58%). Specifically, a high proportion of respondents with non‐predominant OM practice (<40%) were observed in Portugal (75%), Spain (44.4%), Greece (40%) and Italy (36.4%). Such practitioners mainly dealt with oral surgery or general dentistry.
Approximately 40% of OMPs practise oral surgery with significant geographical variations (p = .004); Regions 1 and Australia had very low rates ranging from 13.3% to 16%, Regions 3, 4 and 5 had high rates (50%–61.9%), while Region 2 had an intermediate rate (33.3%). This was consistent with the above‐reported data in relation to postgraduate training. Conversely, oral pathology represented a substantial field of practice (>20% of practice) for a low proportion of respondents (8.6%) without significant geographical variations (p = .843). This could be driven by the fact that in most European countries, oral pathology is not practised distinct from general pathology, thus preventing OMPs’ autonomous practice.
Regardless of the OMPs’ dental background, more than half of respondents (52.9%) did not practise general dentistry at all, although significant differences among Regions were observed (p = .001). In Region 1 and Australia, only a very low proportion of practitioners (6.7%–12%) practised general dentistry. This is in contrast to that of Regions 2 and 3 (33.3%–42.9%) and Regions 4 and 5 (52.8%–57.1%). Special Needs Dentistry rarely represented a significant domain of practice as it accounted for more than 20% of clinical practice for only 12.1% of respondents.
3.5. Oral medicine practice
Oral medicine clinical practice of respondents was quite varied. Only 17% of respondents spent more than half of their practice time dealing with one single group of disorders with no correlation with the OM practice setting. A correlation was found between the involvement in diagnosis and management for all the disorder groups: the more OMPs were involved in the diagnosis of a disorder group the more they were involved in its management (Table 3). Otherwise, when comparing the percentage of cases diagnosed with the percentage of time dedicated to treating a disorder, it was found that for patients with OSCC, OMPs spent more time undertaking diagnosis than managing the disease (p < .001), while the contrary was true for immune‐mediated inflammatory diseases (IMIDs) (p = .024). This could well be related to the chronic course of IMID. Diagnosis and management of IMID were by far the main area of practice for most of OMPs (Figure 1 and Figure S2) representing more than 20% of clinical practice in all countries with at least 5 respondents except for Greece (10.2%), which was considered an outlier. Leukoplakia represented the second most commonly managed disease, but geographical variations were observed (p = .015). This was true only in Regions 1 and 4 and Australia. Patients with chronic pain disorders or benign conditions, lumps and bumps or salivary gland disorders each represented about 10% of patients referred to OMPs without significant geographical variations. Conversely, all groups of disorders accounting for a proportion of practice lower than 10% displayed significant geographical variations.
TABLE 3.
Oral medicine clinical practice
|
% (based on cases diagnosed) |
% (based on time spent treating) |
Spearman's rho correlation coefficient |
|
|---|---|---|---|
| Immune‐mediated disorders (including OLP, bullous disorders, aphthous stomatitis, orofacial granulomatosis) | 24.8 | 26.4 | rs = .836, p < .001 |
| Leukoplakia | 12.5 | 11.6 | rs = .791, p < .001 |
| Chronic pain disorders (including BMS, dysgeusia/dysosmia, facial pain) | 10.7 | 11.3 | rs = .822, p < .001 |
| Benign conditions, lumps and bumps (fibroma, mucocele, papilloma, etc.) | 10.0 | 10.5 | rs = .820, p < .001 |
| Salivary gland disorders (including dry mouth) | 9.7 | 9.8 | rs = .765, p < .001 |
| Oral infection (candidosis, viral infections, etc.) | 9.1 | 9.3 | rs = .802, p < .001 |
| Disorders due to toxicity of cancer treatments or other systemic conditions (including MRONJ, mucositis) | 6.0 | 6.1 | rs = .820, p < .001 |
| Oral Squamous Cell Carcinoma | 5.6 | 3.5 | rs = .431, p < .001 |
| Special Needs Dentistry (e.g. immunocompromised patients and patients undergoing transplantation) | 5.5 | 5.8 | rs = .911, p < .001 |
| Temporomandibular joint/myofascial disorders | 5.2 | 4.8 | rs = .930, p < .001 |
| Dental Sleep Medicine (sleep disordered breathing appliance therapy) | 0.9 | 0.9 | rs = .999, p < .001 |
Practitioners from Regions 1 and 3 were less frequently involved in the diagnosis of OSCC (2.9%–3.5%), which conversely represented a substantial field of practice among practitioners from Region 4 (8.2%) (p = .010).
Patients suffering from disorders due to toxicity of cancer treatment were infrequently managed by OMPs in Regions 1, 3, 5 and Australia (3.2%–5.4%), while they represented 8%–10% of patients managed in Regions 2 and 4 (particularly in Sweden and Italy) (p = .002). Special Needs Dentistry represented a negligible field of practice for OMPs from Region 1 and Australia, about 8.5% of practice in Regions 2, 3 and 5 and approximately 5% in Region 4 (p = .016). Of interest, particularly high rates were observed in Sweden (13%) and Israel (25%).
Temporomandibular joint (TMJ) disorders represented a large field of practice in Australia (16% of patients) and a sizeable one in Regions 1 and 3 (7%–8%). Conversely, this represented only 1%–2% in Regions 2, 4 and 5 (p < .001). Patients with sleep apnoea syndrome presenting to OMPs constituted less than 1% of patients in most regions except for Australia where this accounted for 4% of patients (p = .006).
A Spearman's rank‐order correlation was undertaken to determine the relationship between respondents' involvement in different disorder groups. It was noted that OMPs who had greater involvement in dealing with IMID were less likely to deal with disorders due to toxicity of cancer treatment, Special Needs care, oral infections, benign conditions, lumps and bumps. Conversely, there was a positive correlation between involvement in disorders due to toxicity of cancer treatment and Special Needs care. Moreover, OMPs devoted to these latter areas were more often involved in the management of benign conditions, lumps and bumps. As may be expected, dealing with leukoplakia had a positive correlation to dealing with OSCC, but negative correlations to dealing with salivary gland disorders and TMJ disorders. Finally, a positive correlation was found between dealing with TMJ disorders and practising dental sleep medicine.
Less than half (46%) of OMPs practising in Region 1 refer patients to other colleagues to perform biopsies, while in the rest of Europe and Australia, 97% of OMPs perform biopsies themselves (p < .001). Consistently, 91% of OMPs from Region 1 always refer patients for surgical treatment of oral leukoplakia or early OSCC not requiring neck dissection, while in other countries, OMPs more frequently undertake surgical treatment themselves. In Australia, 57% of OMPs refer their patients for management of oral leukoplakia or early OSCC, while this figure drops to 43% for Regions 3 and 5 and 33% for Regions 2 and 4 (p = .001).
3.6. Research activity
Oral medicine practitioners’ involvement in research showed significant geographical variation (p = .025). The proportion of respondents spending no more than 20% of their time on research ranged from 80% to 88% in Regions 1 and 3 and Australia, 61.5% and 73.9% in Regions 2 and 5, respectively, and only 50% in Region 4. No other significant association with respondent‐associated features was observed.
As such, reliable data about OMPs’ research activity were derived from a subset of about 30% of respondents spending more than 20% of their time on research. This subset of OMPs did not display any particular demographic or academic background but had a higher rate of respondents who spent more than 40% of their working time in University Hospitals (91.7% versus 62.2%; p = .001).
Most OMPs were mainly interested in clinical research compared to laboratory, translational or epidemiological research. No geographical variations were observed when assessing different kinds of research activity. Clinical research accounted for more than 40% of the collective research activity for 72.3% of respondents. Both epidemiological and laboratory research were not practised at all by 33.3% of respondents, while 41.7% of respondents were not interested in translational research.
When considering the object of research activity, leukoplakia research represented the main topic for 10 of 36 respondents, followed by oral lichen planus (5 respondents) and OSCC (4 respondents). Bullous diseases, chronic pain, salivary gland diseases and adverse effects of oncological treatments were the main field of interest for 3 respondents each. Other topics were selected as the main field of research by single respondents.
Irrespective of research, examining the clinical practice of this subset of OMPs, IMID remained the main field of practice, but they were significantly more involved in managing OSCC patients (p = .001) and patients suffering from disorders due to toxicity of cancer treatment (p = .010), while they were less involved in managing TMJ/myofascial disorders (p = .010).
4. DISCUSSION
Medical specialties develop aiming to respond to clinical need. Oral Medicine was created to manage patients with complex oral mucosal manifestations of systemic conditions. Because of its young age, it is conceivable that its scope could still be developing while displaying global variations. The present survey investigates OM clinical practice across Europe and Australia reporting interesting data about its development in different geographical settings.
Expert OMPs can be found worldwide; nevertheless, scope, definition and academic education are not identical globally probably directly related to the young age of OM as a clinical discipline, jointly with diversity of cultures and heterogeneity of settings and healthcare systems. This also implies that many clinicians and patients are often unaware of the existence of OMPs. It has recently been estimated that 4 in 5 patients who could benefit from OMPs’ care present to other physicians (e.g. oral and maxillofacial surgeons, otolaryngologists, dermatologists) (Miller & Peterson, 2018).
The UK General Dental Council (GDC) published the OM specialty training curriculum in 2010 (Felix et al., 2010) which defines the specialty of OM as “oral health care of patients with chronic recurrent and medically related disorders of the mouth and with their diagnosis and non‐surgical management.” Conversely, the Scandinavian Fellowship for Oral Pathology and Oral Medicine refers to OM as being concerned with “aetiology, pathogenesis, epidemiology, diagnosis, prevention and management of oral disorders and symptoms, which may be either primary oral diseases or manifestations of systemic diseases and which may be related to medically complex states including side effects of medical treatments” thus not excluding surgical management of oral disorders (Kragelund et al., 2012). In Australia, the speciality of OM is defined by OMAA as “that specialist branch of dentistry concerned with the diagnosis, prevention and predominantly non‐surgical management of medically related disorders and conditions affecting the oral and maxillofacial region, in particular oral mucosal disease and orofacial pain, as well as the oral health care of medically complex patients” (Oral Medicine Academy of Australasia, 2021).
A consistent view of OM training and practice throughout Europe is still lacking (Bez et al., 2017), compared to Australia where academic programmes conform to the curriculum set out by the OMAA as part of its fellowship programme, and which relies heavily on the UK GDC model. The 2017 framework for European undergraduate dental education does not report a collectively agreed undergraduate curriculum for OM, but a brief comment on this area of practice (Field et al., 2017). In most European countries, OM is not a recognized speciality but a distinct field of study (Bez et al., 2017), thus implying potential geographical variations in postgraduate training and OM fields of practice. The presence of OM as a recognized specialty could influence the choice of undertaking postgraduate OM training abroad; most OMPs moved from countries where OM is not a recognized specialty (i.e. Portugal, Italy and Greece) to UK. At least in Spain and Italy, the lack of a recognized specialty in OM implies that OMPs do not find appropriate job opportunities in the public health system and most often hold part‐time employment in academic settings, not able to provide an adequate income. Only a minority gain a position where they can afford to devote themselves fully to OM. Difficulties in finding appropriate job opportunities could also be related to the high proportion of OMPs who attain postgraduate training in disciplines other than OM. The lowest proportion, although not negligible (43%), was found in Region 1 where OM is a recognized specialty.
Nevertheless, lacking any supranational coordination, even in the presence of specialty training programmes, the development of OM is pursuing dissimilar paths.
The high proportion of OMPs who received their predoctoral training in dental schools reveals that OM is a dental specialty. This is evident when considering the evolution of national curricula necessitating the practice of dentistry and OM and could be related to different undergraduate curricula depending on the respondents’ age. In both Italy and Spain, a dental degree (separate from a medical degree) was created in the 1980s and 1990s (Bez et al., 2017). Previously, dental practitioners (and therefore all OMPs) were required to graduate in Medicine first and then specialize in a medical speciality known as Stomatology. In the UK, OM is one of the 13 specialties of dentistry and since 2010 the medical degree is no longer required to enter an OM specialty training programme. The fact that more than half of respondents do not practice general dentistry at all, outlines OMPs as dentists who strongly moved their interests and practice from dental to oral care. Data from the present study reveal that this remains true even when considering respondents who practice Special Needs Dentistry. This is interesting given that in a previous survey the vast majority of OMPs from Israel, Spain, Italy, Croatia and Sweden considered provision of dental treatment for medically complex patients within the scope of OM practice (Stoopler et al., 2011). Global geographical variations reported here may be related to differences in postgraduate training. Special Needs Dentistry is an independent distinct specialty officially recognized in UK and Australia, conversely in Sweden “Orofacial Medicine” is a broad specialty (created in 2018) combining OM and hospital dentistry/special needs dentistry for adults, and this almost certainly will modify the clinical practice of Swedish OMPs in the future. Data from the United States are somewhat conflicting. The National Provider Identifier Database depicts OM providers’ activity as focused on non‐dental pathologies/conditions, but OM specialists are significantly involved in dental care as general/hospital dentistry accounts for 21% of their clinical practice activity (Villa et al., 2018), and lacking a recognized specialty of Special Needs Dentistry, dental care of medically complex/compromised patients has recently been suggested as a potential expansion field of OM (Miller & Peterson, 2018). Importantly, OM has for a long time not been recognized as a speciality in the United States until this was adopted by the American Dental Association in September 2020. There OM is defined as “the specialty of dentistry responsible for the oral health care of medically complex patients and for the diagnosis and management of medically related diseases, disorders and conditions affecting the oral and maxillofacial region” (American Dental Association, 2021). Importantly, this is a stand‐alone speciality separate from Orofacial Pain which was also adopted at the same time and is different to other jurisdictions such as Australia (Tiwari & Balasubramaniam, 2020).
The strikingly high rate of OMPs who attended OM postgraduate training programmes highlights that younger graduates moving into OM practice feel the need for additional specific training. The need for training in both medicine and science in order to enrich scholarship with essential links between medical and dental education have been espoused (Baum & Scully, 2015). The popularity of the UK as a destination for postgraduate studies could be related to the high presence of OMPs under 40 years of age observed in Region 1.
Noteworthy, OMPs also show frequent interest for additional training in oral surgery. OM is frequently defined as aiming to provide diagnosis and mostly non‐surgical care, and in Region 1 where OM is a well‐recognized non‐invasive clinical specialty, a particularly high rate of referrals by OMPs to perform biopsy was observed. Nevertheless, in regions other than Region 1 and Australia, almost 30% of OMPs attended postgraduate courses in Oral/Maxillofacial Surgery. Such academic training is also reflected in OMPs’ clinical practice. A high proportion of OMPs clearly declared their habit of performing not only biopsies but also surgical treatment for oral leukoplakia or early OSCC not requiring neck dissection. Such surgical practice performed in European countries could be a result of “heritage” of a past European model of stomatology when dentistry was a medical specialty which also included oral surgery, or as an intent to provide comprehensive management of patients. Alternatively, it could be a consequence of oral surgeons being more interested in other surgical fields such as periodontal surgery, regenerative procedures, implant surgery or tooth extraction, rather than in treatment of oral mucosal disorders, allowing OMPs to occupy this domain. Finally, financial reasons could be considered even if unlikely due to the fact that private practice is quite marginal in OM. Nonetheless, when examining OMPs’ clinical practice related to OSCC, they are significantly more involved in diagnosis rather than treatment as most often maxillofacial or head and neck surgeons are needed to perform more extensive surgical treatment.
The literature has mainly reported reasons for referral or diagnosis of patients managed by OMPs and not specifically surgical treatment by them. A retrospective cross‐sectional study from Australia reported data consistent with present findings (Farah et al., 2008). The authors clearly state that in OM clinics, surgical procedures were almost exclusively diagnostic biopsies, and that OMPs most commonly referred patients to oral surgeons for extraction, excision and surgical exploration (21.7% of patients). This suggests that patients requiring surgical treatment for oral leukoplakia are usually referred to maxillofacial/head and neck surgeons, although based on the current study, this may be shifting. Conversely, excisional biopsies with histopathological results consistent with benign conditions, lumps and bumps (e.g. fibro‐epithelial hyperplasia, mucocele, benign squamous papilloma) were routinely performed by OMPs themselves (Farah et al., 2008).
Oral medicine practitioners deal with a variety of conditions affecting the orofacial region, with the management of oral mucosal diseases representing their main activity. IMID are by far the main field of practice followed by oral leukoplakia. A couple of surveys from the United States report a slightly lower rate of oral mucosal lesions (24%–29%) but this difference could be due to reported involvement of OMPs in the treatment of dental pathologies/conditions (Pinto et al., 2015; Villa et al., 2018). The low involvement in IMID management observed in OMPs from Greece could be attributed to lack of facilitates. Direct or indirect immunofluorescence is available in only a few hospitals forcing patients to be referred to other professionals, for example dermatologists.
In the present survey, the management of patients with chronic pain disorders represented the third most frequent field of practice of OMPs without geographical variations. Similar involvement has recently been reported for OMPs in Australia (Tiwari & Balasubramaniam, 2020) and from the United States where about 15% of practice is reported to deal with TMD and orofacial pain (Villa et al., 2018). Given that OM and Orofacial Pain have been recognized in the United States as distinct dental specialties, there may be potential future deviations in the clinical practice of OMPs in that country.
The present survey depicts OM as primarily practised in public or university hospitals in European countries. This mirrors data from previous surveys investigating OM practice in non‐European countries such as United States (Pinto et al., 2015; Stoopler et al., 2011). Of note, a different trend is observed in Australia, and this is consistent with the previous report by Farah and colleagues where the hospital/private rate of patients was 1:2.2 (Farah et al., 2008). When considering many European countries, it must be said that the high ratio of OMPs practising in public or university hospitals does not mean that they have been able to find a full‐time position to practise OM. This just means that their OM practice, often related to partial engagement, is performed within a hospital/university.
About 30% of OMPs are significantly involved in research activity and as may be expected this subset of practitioners spent more than 40% of their working time in University Hospitals. In 2011, the global survey by the World Workshop in Oral Medicine presented similar data, where 16% of OMPs spent more than 25% of their time on research (Stoopler et al., 2011), and recent data from the United States show that OMPs devote about 5 hr/week to research activity (Villa et al., 2018). Geographical variations show that most OMPs not engaged in concerted research activities in UK and Australia, along with data from the United States, suggest that where OM is a recognized specialty, OMPs have more job opportunities outside of academic settings. When considering the subset of OMPs with significant interest in research activity, leukoplakia is the main research topic. Notwithstanding such interest even for this subset of OMPs, the management of IMID patients still represents the main field of clinical practice.
5. CONCLUSION
Oral Medicine practice is characterized by several common features which can be found in all European Regions and Australia, in relation to the management of mucosal disorders, but uniformity is still far from being achieved. Important differences observed in the present study relate to dentistry for medically complex/compromised patients and to surgical treatment of mucosal disorders. Despite accounting for reported geographical variations, the present study depicts OM as moving away from dental care and displaying an interest for surgical treatment of oral disorders never previously reported. In the light of this evidence, retaining OM and Special Needs Dentistry as distinct specialties should be supported and several reflections may arise from the reported interest of OMPs towards surgical intervention. Should be better moving oral surgeons (or at least part of them) to oral mucosal disorders or widening the surgical competence of OMPs? Such insight may be useful in order to better define postgraduate training curricula for practitioners of OM, but irrespective of their content, scientific societies and academics should cooperate in order to develop OM a homogeneous discipline across the globe.
CONFLICT OF INTEREST
None to declare.
AUTHOR CONTRIBUTIONS
Monica Pentenero: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Supervision; Validation; Writing‐original draft. Samuele Sutrera: Data curation; Writing‐review & editing. Giovanni Lodi: Conceptualization; Methodology; Writing‐review & editing. Jose Bagan: Conceptualization; Methodology; Writing‐review & editing. Camile Farah: Conceptualization; Methodology; Project administration; Writing‐review & editing.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/odi.13881.
Supporting information
Fig S1
Fig S2
File S1
ACKNOWLEDGEMENTS
The authors wish to acknowledge and thank the EAOM and OMAA for supporting the present study and all members who responded to the consultation making this study possible. The authors would like to thank the EAOM Position Paper on Oral Leukoplakia Team: Josè V Bagan, Camile S. Farah, Giovanni Lodi, Monica Pentenero, Catherine F. Poh (Oral Oncology, BC Cancer; Oral Biological and Medical Sciences, Faculty of Dentistry, University of British Columbia, Vancouver, Canada), Sook‐Bin Woo (Department of Oral Medicine, Infection and Immunity, Harvard School of Dental Medicine, Boston, MA, USA) for their support in the development of the survey and Grazia Vicario (Department of Mathematical Sciences, Politecnico di Torino, Turin, Italy), for useful discussions and suggestions about data analysis and statistical approaches.
Data from the present study were subject to statistical analyses performed by Giorgio Bussiglieri, Camilla Calzoni and Giulio Cerruto as part of their graduation thesis (Politecnico di Torino, Turin, Italy), and Octavian Fiore discussed part of the reported results during his final examination of the specialty programme in Oral Surgery (University of Torino, Turin, Italy).
Pentenero M, Sutera S, Lodi G, Bagan JV, Farah CS. Oral medicine practice in Europe and Australia: Identifying practitioner characteristics and their clinical activity. Oral Dis. 2022;28:2043–2051. 10.1111/odi.13881
Funding information
The present study was supported by MURST ex‐60% “Università di Torino”
REFERENCES
- American Dental Association (2021). National commission on recognition of dental specialties and certifying boards ‐ specialty definitions. Retrieved from https://www.ada.org/en/ncrdscb/dental‐specialties/specialty‐definitions [Google Scholar]
- Baum, B. J. , & Scully, C. (2015). Training specialists in oral medicine. Oral Diseases, 21, 681–684. [DOI] [PubMed] [Google Scholar]
- Bez, C. , Sklavounou, A. , & Carrozzo, M. (2017). Oral medicine in Europe: Past, present and future. British Dental Journal, 223, 726–728. [DOI] [PubMed] [Google Scholar]
- Brierley, J. D. , Gospodarowicz, M. K. , & Wittekind, C. (2017). TNM classification of malignant tumours. Wiley. [Google Scholar]
- Farah, C. S. , Simanovic, B. , & Savage, N. W. (2008). Scope of practice, referral patterns and lesion occurrence of an oral medicine service in Australia. Oral Diseases, 14, 367–375. [DOI] [PubMed] [Google Scholar]
- Felix, D. H. , Atkin, P. A. , Nolan, A. , Smith, G. L. F. , Hegarty, A. , Hodgson, T. , Lewis, M. A. O. , Mighell, A. J. , Pemberton, M. N. , & Richards, A. (2010). Specialty training curriculum for oral medicine. Retrieved from https://www.gdc‐uk.org/docs/default‐source/specialist‐lists/oralmedicinecurriculum.pdf?sfvrsn=8a9b42fa_2. [Google Scholar]
- Field, J. C. , Cowpe, J. G. , & Walmsley, A. D. (2017). The graduating European dentist: A new undergraduate curriculum framework. European Journal of Dental Education, 21(Suppl 1), 2–10. [DOI] [PubMed] [Google Scholar]
- Kragelund, C. , Reibel, J. , Hietanen, J. , Hadler‐Olsen, E. , Johannessen, A. C. , Kenrad, B. , Nylander, K. , Puranen, M. , Salo, T. , Syrjanen, S. , Soland, T. M. , van der Waal, I. , van der Wal, J. E. , Warfvinge, G. , Fellowship, S. , & Scandinavian Fellowship for Oral P and Oral M (2012). Scandinavian fellowship for oral pathology and oral medicine: Guidelines for oral pathology and oral medicine in the dental curriculum. European Journal of Dental Education, 16, 246–253. [DOI] [PubMed] [Google Scholar]
- Miller, C. S. , & Peterson, D. E. (2018). Oral medicine: Today's future can become tomorrow's reality. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 126, 409–414. [DOI] [PubMed] [Google Scholar]
- Oral Medicine Academy of Australasia (2021). OMAA website. Retrieved from http://www.omaa.com.au/ [Google Scholar]
- Pinto, A. , Khalaf, M. , & Miller, C. S. (2015). The practice of oral medicine in the United States in the twenty‐first century: An update. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 119, 408–415. [DOI] [PubMed] [Google Scholar]
- Scully, C. , Miller, C. S. , Aguirre Urizar, J. M. , Alajbeg, I. , Almeida, O. P. , Bagan, J. V. , Birek, C. , Chen, Q. , Farah, C. S. , Figueirido, J. P. , Hasseus, B. , Jontell, M. , Kerr, A. R. , Laskaris, G. , Lo Muzio, L. , Mosqueda‐Taylor, A. , Nagesh, K. S. , Nikitakis, N. G. , Peterson, D. , … Zadik, Y. (2016). Oral medicine (stomatology) across the globe: Birth, growth, and future. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 121, 149–157.e5. [DOI] [PubMed] [Google Scholar]
- Shklar, G. , & McCarthy, P. L. (2008). Francis P. McCarthy, pioneer in oral medicine. Journal of the History of Dentistry, 56, 145–147. [PubMed] [Google Scholar]
- Stoopler, E. T. , Shirlaw, P. , Arvind, M. , Lo Russo, L. , Bez, C. , De Rossi, S. , Garfunkel, A. A. , Gibson, J. , Liu, H. , Liu, Q. , Thongprasom, K. , Wang, Q. , Greenberg, M. S. , & Brennan, M. T. (2011). An international survey of oral medicine practice: Proceedings from the 5th world workshop in oral medicine. Oral Diseases, 17(Suppl 1), 99–104. [DOI] [PubMed] [Google Scholar]
- Tiwari, L. , & Balasubramaniam, R. (2020). Patterns of orofacial pain practice amongst oral medicine specialists in Australia. Journal of Oral Pathology and Medicine, 49, 590–594. [DOI] [PubMed] [Google Scholar]
- Villa, A. , Stoopler, E. T. , & Napenas, J. (2018). Employment type and career satisfaction among oral medicine specialists. Journal of Dental Education, 82, 630–635. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Fig S2
File S1


