Abstract
Objectives:
This study examines the relationships between self-reported exposure to smokeless tobacco marketing and initiation/onset of smokeless tobacco use/susceptibility at 6-month follow-up, among a cohort of young adults in urban Texas.
Methods:
Participants were 3597 18–25 year old never smokeless tobacco users, attending 24 Texas two-year colleges and four-year universities. A multi-level, multivariate logistic regression model, accounting for school clustering, examined the impact of self-reported recall of smokeless tobacco marketing exposure at baseline and subsequent initiation of smokeless tobacco use. A subsample analysis of non-susceptible never users (n = 3097) examined the impact of self-reported exposure to smokeless tobacco marketing at baseline and onset of susceptibility to use smokeless tobacco. Both outcomes were assessed at 6-month follow-up. Baseline covariates included age, race/ethnicity, sex, two–/four-year institution, and other tobacco use. For the full analysis, susceptibility to use smokeless tobacco at baseline was included as a covariate.
Results:
From baseline to 6-month follow-up, 6.1% of never users initiated smokeless tobacco use (n = 219) and 7.0% of non-susceptible never users became susceptible to smokeless tobacco use (n = 221). Self-reported recall of smokeless tobacco marketing exposure at baseline was associated with initiation of smokeless tobacco (Adj OR: 1.17; 95% CI: 1.08–1.27) and onset of susceptibility to use smokeless tobacco (Adj OR: 1.11; 95% CI: 1.02–1.21) at 6-month follow-up, controlling for all covariates.
Conclusions:
Findings build on previous research by demonstrating an association between recall of smokeless tobacco marketing and subsequent use. Findings are concerning given the 300% increase in smokeless tobacco marketing expenditures from 2006 to 2016.
Keywords: Marketing, Smokeless tobacco, Young adults, Initiation, Susceptibility
1. Introduction
Smokeless tobacco use has steadily increased since 2000, particularly among young adults (Agaku, King, Husten, et al., 2014; Cheng, Rostron, Day, et al., 2017; Lipari & Van Horn, 2017; Loukas, Batanova, Fernandez, & Agarwal, 2015; U.S. Department of Health and Human Services, 2014). Increased use of smokeless tobacco is concerning since smokeless tobacco use is linked to oral cancer and gastro-intestinal disorders (Piano et al., 2010; U.S. Department of Health and Human Services, 2014; World Health Organization, 2007), and smokeless tobacco is frequently used concurrently with other tobacco products (i.e., dual/poly use), particularly conventional cigarettes (Cheng et al., 2017; Mantey, Creamer, Pasch, & Perry, 2018; Osibogun, Taleb, Bahelah, Salloum, & Maziak, 2018). Furthermore, smokeless tobacco use may undermine cigarette smoking cessation attempts (Kalkhoran, Grana, Neilands, & Ling, 2015; Parascandola, Augustson, & Rose, 2009) or act as a “gateway” to other tobacco use (Haddock, Weg, DeBon, et al., 2001; Soneji, Sargent, Tanski, & Primack, 2015; Tam, Day, Rostron, & Apelberg, 2015; Tomar, 2003). These direct and indirect consequences of smokeless tobacco use may ultimately increase the incidence of tobacco-related morbidity and mortality.
One possible cause for the increased prevalence in smokeless tobacco use is increased marketing of these products. Specifically, smokeless tobacco marketing expenditures increased by > 300% from 2006 ($250.8 million) to 2016 ($759.3 million) (Federal Trade Commission, 2018). This substantive growth in smokeless tobacco marketing expenditures began as large American cigarette companies (i.e., Reynold American, Altria) consolidated much of the smokeless tobacco market and subsequently launched products and marketed them under established brand names (e.g., Camel, Marlboro) (Federal Trade Commission, 2013; National Cancer Institute and Centers for Disease Control and Prevention, 2014). The prolific marketing of branded smokeless tobacco products is a possible driving force of persistent smokeless tobacco use (Delnevo et al., 2014).
Along with increased marketing expenditures, smokeless marketing campaigns have used messaging that may be considered misleading. For example, large tobacco companies have promoted smokeless tobacco as “harm reduction” products (Altria Client Services Inc. Philip Morris USA Inc. and U.S. Smokeless Tobacco Company, 2012; Calantzopoulos, 2012; Reynolds American, 2012) while simultaneously advertising concurrent use of conventional cigarettes and smokeless tobacco (Richardson, Ganz, Stalgaitis, Abrams, & Vallone, 2013; Carpenter, Connolly, Ayo-Yusuf, & Wayne, 2009; Romito, Saxton, Coan, & Christen, 2011; Timberlake, Pechmann, Tran, & Au, 2011; University of Medicine and Dentistry of New Jersey, School of Public Health, 2010). Though exclusive smokeless tobacco use likely has fewer direct health consequences relative to exclusive cigarette smoking, messaging aimed at increasing multiple tobacco use under the pretense of harm reduction may create reduced harm perceptions. While messages used to market smokeless tobacco have been studied extensively (Richardson et al., 2013; Altria Client Services Inc. Philip Morris USA Inc. and U.S. Smokeless Tobacco Company, 2012; Calantzopoulos, 2012; Carpenter et al., 2009; Reynolds American, 2012; Romito et al., 2011; Timberlake et al., 2011; University of Medicine and Dentistry of New Jersey, School of Public Health, 2010), limited research has examined the impact of marketing exposure on perceptions and use of these products.
The combination of increased marketing expenditures (Federal Trade Commission, 2018) and utilization of misleading marketing tactics (Richardson et al., 2013; Altria Client Services Inc. Philip Morris USA Inc. and U.S. Smokeless Tobacco Company, 2012; Calantzopoulos, 2012; Carpenter et al., 2009; Reynolds American, 2012; Romito et al., 2011; Timberlake et al., 2011; University of Medicine and Dentistry of New Jersey, School of Public Health, 2010) to promote smokeless tobacco use is concerning for several reasons. Specifically, research has consistently demonstrated an association between tobacco marketing exposure and tobacco use behaviors (U.S. Department of Health and Human Services, 2014; U.S. Department of Health and Human Services, 2016), across product types. Further, the use of mitigated health claims in marketing campaigns for other tobacco products (e.g., conventional cigarettes, electronic cigarettes) (Grana & Ling, 2014; Klein et al., 2016; Kong et al., 2017; U.S. Department of Health and Human Services, 2014) has been shown to impact the psycho-social precursors of tobacco use (e.g., intentions, harm perceptions) (Pokhrel, Fagan, Herzog, et al., 2018; Pokhrel, Fagan, Kehl, & Herzog, 2015; U.S. Department of Health and Human Services, 2014) and has been linked to increased tobacco initiation and sustained use (Pokhrel, Fagan, Herzog, et al., 2016; Robertson, McGee, Marsh, & Hoek, 2015; U.S. Department of Health and Human Services, 2014). As such, increased smokeless tobacco marketing exposure may induce comparable changes in smokeless tobacco use behaviors.
Tobacco industry marketing messages have long been tailored to target young adults (Curry, Pederson, & Stryker, 2011; Gilpin, White, & Pierce, 2005; Mejia & Ling, 2010; Sepe, Ling, & Glantz, 2002; Timberlake et al., 2011). Targeted marketing is likely a primary factor in the disproportionate increase in smokeless tobacco use (Agaku et al., 2014; Cheng et al., 2017; Loukas et al., 2015) and susceptibility to use smokeless tobacco (Choi, Fabian, Mottey, Corbett, & Forster, 2012), observed in young adults, relative to other age groups. Specifically, while smokeless tobacco use was considered rare among young adults through the 1990s (Rigotti, Lee, & Wechsler, 2000), more recent cross-sectional data (Enofe, Berg, & Nehl, 2014) from 2010, and longitudinal data (Richardson, Williams, Rath, Villanti, & Vallone, 2014) from 2011 to 2012, show a substantial increase in smokeless tobacco use behaviors (Enofe et al., 2014), particularly experimentation (Richardson et al., 2014), among young adults. While research has revealed a change in smokeless tobacco use behaviors among young adults (Agaku et al., 2014; Cheng et al., 2017; Enofe et al., 2014; Loukas et al., 2015; Richardson et al., 2014), the relationship between tobacco marketing exposure and these behaviors has not been thoroughly studied.
Research on smokeless tobacco marketing content has revealed a clear targeting of younger individuals, as well as a new focus on female and urban populations (Richardson et al., 2013; Curry et al., 2011; Mejia & Ling, 2010; Timberlake et al., 2011). While research has examined receptivity to smokeless marketing, conceptualized as recognition of a smokeless brand or willingness to wear smokeless branded merchandise (Thrul, Lisha, & Ling, 2016; Timberlake, 2016), there have been no studies which examine the association between recall of smokeless tobacco marketing exposure and subsequent smokeless tobacco use or susceptibility to use smokeless tobacco among young adults, an important psycho-social precursor to future use (Pierce, Choi, Gilpin, et al., 1996). It is vital to understand the relationship between exposure to smokeless tobacco marketing and subsequent smokeless tobacco use behaviors given the proliferation of marketing and use of smokeless tobacco (Delnevo et al., 2014; Federal Trade Commission, 2018).
An additional limitation of existing research on smokeless tobacco use behaviors among young adults is a lack of racial/ethnic diversity in the study samples (Enofe et al., 2014; Richardson et al., 2014; Rigotti et al., 2000). This limitation has several consequences that reduce the overall understanding of smokeless tobacco use. First, a lack of racial/ethnic diversity reduces the ability to apply study findings to the contemporary young adult population, which is more diverse than previous generations (Vespa, Armstrong, & Medina, 2018). Second, a lack of adequate sample size across race/ethnic groups increases the probability of failing to reject the null hypothesis (i.e., Type II error) (Woodward, 1999). Specifically, from a statistical perspective, the likelihood of detecting significant differences between two groups is reduced when comparing a disproportionately large referent group to a small comparison group (Woodward, 1999). The present research is one of the first studies to examine a diverse sample (described in the methods section) with the statistical power to detect demographic differences in smokeless tobacco use behaviors.
1.1. Study aims & hypotheses
The purpose of this study was to examine the prospective associations between self-reported recall of exposure to smokeless tobacco marketing at baseline and smokeless tobacco use behaviors at 6-month follow-up, among a cohort of young adult college students. Specifically, this study examined the initiation of smokeless tobacco use among a cohort of young adult never smokeless tobacco users. Moreover, this study examined the onset of susceptibility to use smokeless tobacco among a subsample of non-susceptible young adult never smokeless tobacco users.
We hypothesized that self-reported recall of exposure to smokeless tobacco marketing at baseline would be positively associated with the initiation of smokeless tobacco use among young adult never smokeless tobacco users at 6-month follow-up. We also hypothesized that self-reported recall of exposure to smokeless tobacco marketing at baseline would be positively associated with the onset of susceptibility to use smokeless tobacco among young adult non-susceptible never smokeless tobacco users at 6-month follow-up. To our knowledge, this is the first prospective study to examine self-reported recall of exposure to smokeless tobacco marketing and subsequent smokeless tobacco use behaviors among young adults.
2. Methodology
2.1. Study design
This study is a prospective analysis of data collected at baseline and the first 6 month follow-up, of the larger four-year, multi-wave, Marketing and Promotions across Colleges in Texas study (Project M-PACT); a rapid response surveillance study. Baseline data were collected between November 2014 and February 2015 with follow-up data collected 6 months later, between May and June 2015.
2.2. Procedure and participants
Participants were college students attending 24 two- and four-year institutions in five counties containing the four largest cities in Texas: Austin, Dallas/Fort Worth, Houston, and San Antonio. Eligibility criteria for the M-PACT study included being a full- or part-time, degree or certificate seeking undergraduate student attending a two-year vocational/technical program, or a four-year college/university. The full M-PACT study included participants between the ages of 18–29 at baseline. However, the present study included only M-PACT participants who were 18 to 25 years old at baseline, as this age range is generally considered to be young adulthood (U.S. Department of Health and Human Services, 2012).
Participants were recruited via email to participate in an online survey. Informed consent was obtained prior to survey completion. Upon completion of both the baseline and follow-up survey, students received a $10 electronic gift card and were entered into a drawing to win one of 20 $50 electronic gift cards. A total of 13,714 students were eligible to participate in the study and 5482 of these (40%) provided consent and completed the baseline survey; 4326 participants completed the 6 month follow-up survey (a 79% response rate). The study design and procedures for Project M-PACT are further detailed elsewhere (Loukas, Chow, Pasch, et al., 2016).
For this study, only eligible participants that reported never use of smokeless tobacco and had complete data at baseline and follow-up were included (n = 3597). A subsample of non-susceptible never users (n = 3097) was selected from these 3597 participants. Specifically, individuals eligible for this study that did not report susceptibility to smokeless tobacco use at baseline (defined in the measures section) were included for subsample analyses; this then excluded never users that were susceptible to smokeless tobacco use. Sample selection is further detailed in Fig. 1. Approval to conduct this research was provided by the University of Texas at Austin IRB [Protocol Number: 2013-06-0034].
Fig. 1.
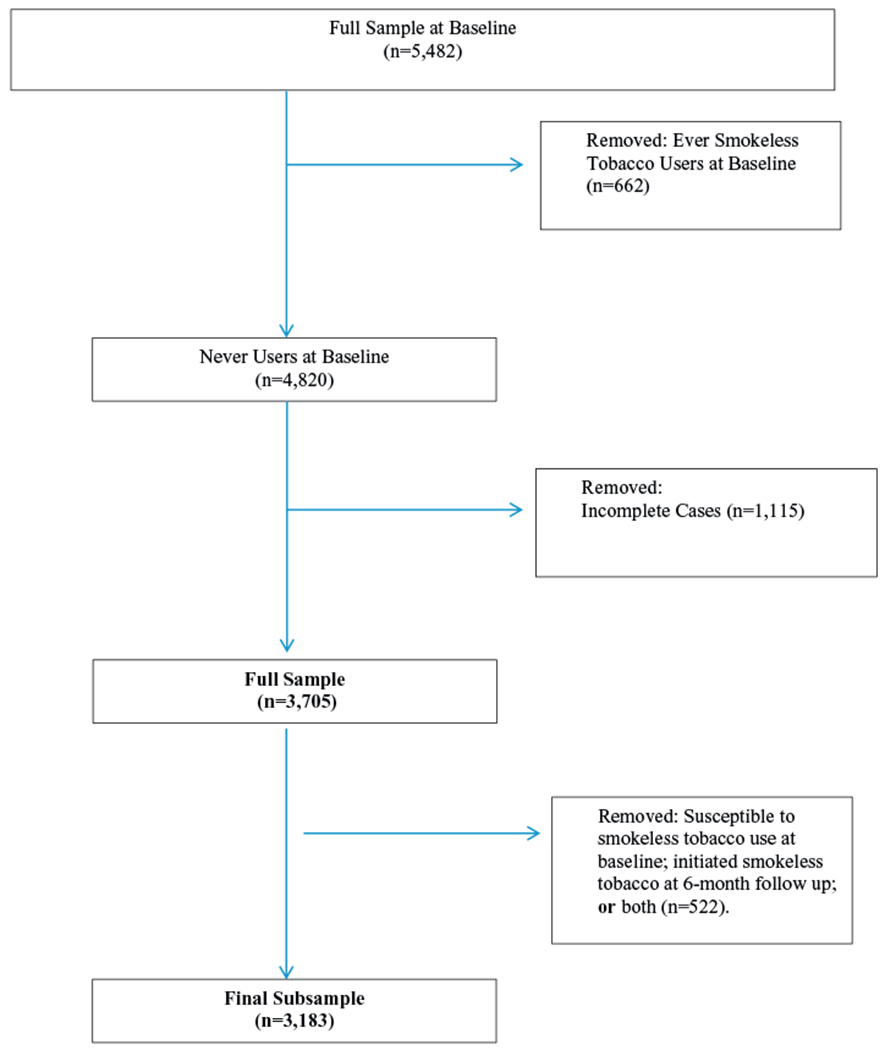
Sample selection.
2.3. Measures
Study participants were provided the following text prior to receiving questions pertaining to smokeless tobacco: “The next questions are about smokeless tobacco, which you put in your mouth and chew, suck, or spit. There are many kinds of smokeless tobacco, such as snus, moist snuff, dip, spit, pouches, and chewing tobacco. Common brands include Skoal, Copenhagen, Grizzly, Camel or Marlboro Snus, Redman, Levi Garrett, and Beechnut. We mean any of these products when we refer to smokeless tobacco.” Accompanying this explanation was an image that contained several types of smokeless tobacco such as snus, loose leaf chewing tobacco, and moist snuff. This image is available in Fig. 2. Cognitive interviews were used to refine all assessments in the M-PACT study (Hinds, Josephine, Loukas, Chow, et al., 2016).
Fig. 2.

Assessment of smokeless tobacco use behaviors.
“The next questions are about smokeless tobacco, which you put in your mouth and chew, suck, or spit. There are many kinds of smokeless tobacco, such as snus, moist snuff, dip, spit, pouches, and chewing tobacco. Common brands include Skoal, Copenhagen, Grizzly, Camel or Marlboro Snus, Redman, Levi Garrett, and Beechnut. We mean any of these products when we refer to smokeless tobacco.”
2.3.1. Outcome variables
There were two outcomes of interest for this study. First, we examined initiation of smokeless tobacco use at 6-month follow-up. Participants were asked, “Have you ever used smokeless tobacco such as moist snuff, dip, snus, or chewing tobacco?” Those that reported “yes” were considered smokeless tobacco initiators.
Second, we examined the onset of susceptibility to use smokeless tobacco among a subsample of non-susceptible (at baseline) participants that did not initiate at 6-month follow-up (n = 3166). Susceptibility was assessed through two questions: “Do you think you will use smokeless tobacco in the next 12 months?” and “If one of your friends offered you smokeless tobacco, would you use it?” Possible responses for each of these questions were “definitely yes,” “probably yes,” “probably not,” and “definitely not.” Consistent with previous research (Timberlake, 2016), susceptibility was treated as a binary outcome (no = 0/yes = 1). If a participant responded to either question with anything other than “definitely not” (coded as 0), they were considered susceptible to use smokeless tobacco and coded as 1.
2.3.2. Self-reported recall of exposure to smokeless tobacco marketing
Self-reported recall of exposure to smokeless tobacco marketing served as the independent variable. Self-reported recall of exposure to smokeless tobacco marketing via eight channels was assessed through the following question at baseline: “Where do you remember seeing or hearing advertisements for smokeless tobacco?” Participants were allowed to select all that applied. The following channels were assessed: (1) Gas stations, convenience stores, drug stores (such as CVS or Walgreens), or grocery stores; (2) Liquor Stores; (3) Bars/Clubs; (4) Music Events/Festivals; (5) Radio/Internet Radio; (6) Internet/Online; (7) Magazines/Newspapers; (8) Billboards. Possible responses for each question were “yes” (coded as 1) and “no” (coded as 0). Total self-reported recall of exposure to smokeless tobacco marketing was computed for each participant with possible total self-reported recall of exposure to smokeless tobacco marketing ranging from 0 to 8.
2.3.3. Covariates
Socio-demographic variables: Baseline covariates included age (ranging 18–25 years), sex (male = 0 and female = 1), race/ethnicity (non-Hispanic white = 0; Hispanic/Latino = 1; African American or Black = 2; Asian = 3; and American Indian/Alaska Native, Native Hawaiian/Pacific Islander, or any other race/ethnicity = 4), and college type (two-year = 0 and four-year = 1).
Other tobacco use: Baseline use of tobacco products, other than smokeless tobacco, was included as a covariate. Participants were considered other tobacco users if they reported use of any of the following tobacco products in the past 30 days: conventional cigarettes, electronic cigarettes, hookah, large cigars, little filtered cigars, or cigarillos.
2.4. Attrition analyses
To account for possible selection bias through participant attrition, t-test and chi-square analyses were conducted to determine whether participants with complete data, who were included in the present study (n = 3597), differed significantly from those who were removed due to incomplete data (n = 1062), on all baseline variables. No substantive threat to selection bias was found. As shown in Table 1, t-test and chi-square test analyses indicated statistically significant differences across all baseline variables (other than sex) for eligible participants with complete data (n = 3597) and those with incomplete data (n = 1062). However, post-tests (Cohen’s D, phi coefficient, Cramer’s V) revealed these differences (i.e., strength of association) were small (Cohen, 1988; Olivier & Bell, 2013), suggesting that significant findings are likely due to the large sample size, rather than substantive differences between those included in the present study and those that were dropped due to incomplete data. Furthermore, cohort studies frequently experience a greater rate of attrition among tobacco users (McDonald, Haardoerfer, Windle, Goodman, & Berg, 2017).
Table 1.
Descriptive statistics and attrition analysis.
| Complete cases (n = 3597)a | Incomplete cases (n = 1062)b | Statistical analysisc | |
|---|---|---|---|
| Marketing exposure (mean; SD) | 1.54 (1.53) | 1.73 (1.61) | t(4657) = 3.56; p = .004 |
| Age (mean; SD) | 20.0 (1.79) | 20.2 (1.87) | t(4657) = 3.24; p = .056 |
| Sex | χ2 (1,N = 4656) = 0.02; p = .875 | ||
| Male | 31.9% | 32.2% | |
| Female | 68.1% | 67.8% | |
| Race/Ethnicity | χ2 (4, N = 4, 656) = 47.59; p < .001 Cramer’s V = 0.10 |
||
| Non-Hispanic White | 34.4% | 33.5% | |
| Hispanic/Latino | 29.9% | 35.7% | |
| African American | 8.0% | 10.8% | |
| Asian American | 20.4% | 12.1% | |
| Otherd | 7.4% | 7.9% | |
| Other tobacco usee | χ2 (1,N = 4, 659) = 24.51; p < .001 Phi coefficient = 0.07 |
||
| No | 76.9% | 69.5% | |
| Yes | 23.1% | 30.5% |
Full sample of eligible participants.
Subsample of non-susceptible, never smokeless tobacco users.
T-test and chi-square analyses.
Participants that reported race/ethnicity of American Indian/Alaska Native, Native Hawaiian/Pacific Islander, or any other race/ethnicity were categorized as “Other”.
Any use of conventional cigarettes, electronic cigarettes, hookah, large cigars, little filtered cigars, or cigarillos in the past 30-days.
2.5. Statistical analyses
Study hypotheses were tested using multilevel, multivariate logistic regression models. First, a multilevel, multivariate logistic regression model was conducted to examine the association between self-reported recall of exposure to smokeless tobacco marketing at baseline and initiation of smokeless tobacco use at 6-month follow-up, controlling for baseline age, race/ethnicity, sex, college type, other tobacco use, and susceptibility to use smokeless tobacco. Next, a subsample analysis was performed among non-susceptible participants (n = 3166; see Fig. 1) to examine the association between self-reported recall of exposure to smokeless tobacco marketing at baseline and onset of susceptibility to use smokeless tobacco at 6-month follow-up, controlling for baseline age, race/ethnicity, sex, two–/four-year college type, and other tobacco use. Multilevel analyses were conducted for all models to account for the nesting of participants within their baseline college or university (i.e., school was included as a random effect in multilevel models). All analyses were conducted using Stata 14.0 (College Station, TX).
3. Results
3.1. Sample characteristics
Participants were 3597 baseline never smokeless tobacco users (68.1% female) aged 18–25 years old (mean age: 20.0; SD: 1.79). The sample was 34.4% non-Hispanic white, 29.9% Hispanic/Latino, 20.4% Asian American, 8.0% African American, and 7.4% multi-racial/ethnic or another race/ethnicity. At baseline, 23.1% of the sample reported past 30-day use of other tobacco products (Table 1).
Among the full sample, 219 never users (6.1%) initiated smokeless tobacco use from baseline to 6-month follow-up. Among non-susceptible never users at baseline, 221 (7.1%) became susceptible to using smokeless tobacco at 6-month follow-up (Table 2).
Table 2.
Prevalence of marketing exposure and smokeless tobacco use behaviors.
| Never users at baseline (n = 3597)a | Non-susceptible at baseline (n = 3097)b | |
|---|---|---|
| Marketing exposure at Baselinec (mean; sd) | 1.54 (1.53) | 1.49 (1.50) |
| Retail environment | 55.7% | 56.0% |
| Liquor store | 11.2% | 10.1% |
| Bars/Clubs | 6.3% | 5.8% |
| Music Events/Festivals | 6.3% | 5.5% |
| Radio/Internet Radio | 9.7% | 8.9% |
| Internet/Online | 26.0% | 24.7% |
| Print Media | 25.0% | 24.4% |
| Billboards | 13.8% | 13.4% |
| Behavioral changes at 6-month follow-up | ||
| Initiate smokeless tobaccod | 6.1% | N/A |
| Onset of susceptibilitye | 9.5% | 7.1% |
Full sample of eligible participants.
Subsample of non-susceptible, never smokeless tobacco users.
Cumulative number of channels of self-reported exposure to smokeless tobacco marketing from the following categories: (1) Gas stations, convenience stores, drug stores (such as CVS or Walgreens), or grocery stores; (2) Liquor Stores; (3) Bars/Clubs; (4) Music Events/Festivals; (5) Radio/Internet Radio; (6) Internet/Online; (7) Magazines/Newspapers; (8) Billboards. Possible scores ranged from 0 to 8.
Participants reported “ever” use of smokeless tobacco at 6-month follow-up.
Participants reported “susceptibility to use smokeless tobacco” at 6-month follow-up.
3.2. Self-reported recall of exposure to smokeless tobacco marketing
As shown in Table 2, 69.9% of participants were exposed to smokeless tobacco marketing through at least one of the eight channels (e.g., gas stations, internet/online, billboards, etc.) at baseline. The mean number of channels by which participants were exposed to smokeless tobacco marketing was 1.54 [95% Confidence Interval (CI): 1.49–1.59], indicating participants were exposed via one or two channels, on average. Retail advertising and promotion (55.7%) was the most prevalent source of self-reported recall of exposure to smokeless tobacco marketing followed by internet/online (26.0%), print media (25.0%), billboards (13.8%), liquor stores (11.2%), radio/internet radio (9.7%), bars/clubs (6.4%), and event sponsorships (6.3%).
3.3. Testing study hypotheses: 6-month follow-up
Among never smokeless tobacco users, self-reported recall of exposure to smokeless tobacco marketing via more channels at baseline was positively and significantly associated with initiating smokeless tobacco use at 6-month follow-up. With each additional channel of smokeless tobacco marketing exposure reported at baseline, the odds of smokeless tobacco initiation at 6-month follow-up increased by 1.17 (95% CI: 1.08–1.27), accounting for baseline covariates, including strong predictors of smokeless tobacco initiation such as past 30-day use of other tobacco products (Adj OR: 2.33) and susceptibility to smokeless tobacco use (Adj OR: 2.89).
Among never smokeless tobacco users who were not susceptible to using smokeless tobacco at baseline, self-reported recall of exposure to smokeless tobacco marketing via more channels at baseline was positively and significantly associated with the onset of susceptibility to use smokeless tobacco at 6-month follow-up. With each additional channel of smokeless tobacco marketing exposure, odds of onset of susceptibility to use smokeless tobacco increased by 1.11 (95% CI: 1.02–1.22), accounting for baseline covariates, including strong predictors of susceptible smokeless tobacco use such as past 30-day use of other tobacco products (Adj OR: 2.13) (Table 3).
Table 3.
Smokeless tobacco marketing exposure and smokeless tobacco use/susceptibility.
| Ever smokeless tobacco use (n = 3597)a | Susceptibility to smokeless tobacco use (n = 3097)b | |
|---|---|---|
|
|
||
| Adj OR (95% CI) | Adj OR (95% CI) | |
| Advertising exposurec | ||
| Smokeless tobacco marketing exposure | 1.17*** (1.08–1.27) | 1.11* (1.02–1.21) |
| Susceptibility to smokeless tobacco use | ||
| No | 1.00 (Ref) | N/A |
| Yes | 2.89*** (2.05–4.09) | N/A |
| Age | 1.16*** (1.08–1.25) | 0.91* (0.84–0.99) |
| Race | ||
| Non-Hispanic, Whites | 1.00 (Ref) | 1.00 (Ref) |
| Hispanic/Latino | 1.26 (0.87–1.82) | 1.54* (1.08–2.20) |
| African American | 1.13 (0.61–2.09) | 0.94 (0.50–1.75) |
| Asian ancestry | 2.19*** (1.49–3.22) | 1.43 (0.95–2.15) |
| Otherd | 1.29 (0.74–2.27) | 1.56 (0.91–2.68) |
| Sex | ||
| Male | 1.00 (Ref) | 1.00 (Ref) |
| Female | 0.77 (0.58–1.03) | 0.90 (0.67–1.21) |
| Institution type | ||
| 2-year | 1.00 (Ref) | 1.00 (Ref) |
| 4-year | 1.34 (0.69–2.60) | 0.99 (0.56–1.79) |
| Other tobacco usee | ||
| No | 1.00 (Ref) | 1.00 (Ref) |
| Yes | 2.33*** (1.74–3.13) | 2.13*** (1.58–2.87) |
| School-level effect | < 0.01 | 0.01 |
Full sample of eligible participants.
Subsample of non-susceptible, never smokeless tobacco users.
Cumulative number of channels of self-reported exposure to smokeless tobacco marketing from the following categories: (1) Gas stations, convenience stores, drug stores (such as CVS or Walgreens), or grocery stores; (2) Liquor Stores; (3) Bars/Clubs; (4) Music Events/Festivals; (5) Radio/Internet Radio; (6) Internet/Online; (7) Magazines/Newspapers; (8) Billboards. Possible scores ranged from 0 to 8.
Participants that reported race/ethnicity of American Indian/Alaska Native, Native Hawaiian/Pacific Islander, or any other race/ethnicity were categorized as “Other”.
Any use of conventional cigarettes, electronic cigarettes, hookah, large cigars, little filtered cigars, or cigarillos in the past 30-days.
4. Discussion
To our knowledge, this is the first study to prospectively investigate the associations between self-reported recall of exposure to smokeless tobacco marketing and use/susceptibility of smokeless tobacco among young adults. Findings revealed a positive and statistically significant association between self-reported recall of exposure to smokeless tobacco marketing at baseline and initiation of smokeless tobacco use among young adults at 6-month follow-up. Further, this study found a statistically significant relationship between self-reported recall of exposure to smokeless tobacco marketing and onset of susceptibility to use smokeless tobacco, among non-susceptible never users, at 6-month follow-up. These findings are consistent with cross-sectional and longitudinal studies of other tobacco products (e.g., conventional cigarettes, electronic cigarettes), which demonstrate an association between tobacco marketing exposure and subsequent tobacco initiation and sustained use among young adults (Mantey, Pasch, Loukas, & Perry, 2019; Pokhrel et al., 2016; U.S. Department of Health and Human Services, 2014). Furthermore, this research builds on previous research by demonstrating an association between receptivity to smokeless tobacco marketing and subsequent use (Thrul et al., 2016).
This research has several implications. The results of this prospective analysis of young adult smokeless tobacco use behaviors are concerning given the increases in smokeless tobacco marketing expenditures (Federal Trade Commission, 2018). The tobacco industry spent $759.3 million on marketing smokeless tobacco products in 2016 (Federal Trade Commission, 2018), an increase of 11% from 2015 and 26% from 2014 (Federal Trade Commission, 2018). These increases in marketing expenditures suggest the trend of increased market presence is likely to continue. As such, continued environmental influences (i.e., marketing exposure) on smokeless tobacco use may increase the overall prevalence of smokeless tobacco use as well as dual- or poly-tobacco use with other products (Cheng et al., 2017; Mantey et al., 2018; Osibogun et al., 2018).
Further, this study indicates the tobacco industry initiative to market smokeless tobacco to younger people, urban areas, and other demographics may be working (Curry et al., 2011; Gilpin et al., 2005; Mejia & Ling, 2010; Sepe et al., 2002; Timberlake et al., 2011). Smokeless tobacco use, traditionally, has been concentrated in non-urban areas (Cheng et al., 2017; Lipari & Van Horn, 2017; Roberts, Doogan, Kurti, et al., 2016). However, more recent data from a nationally representative sample found rates of smokeless tobacco use did not differ between urban and non-urban individuals (Jones et al., 2017). As the sample presented in this study is exclusively urban young adults, the findings presented here add context to the geographical shift in smokeless tobacco use recently observed (Jones et al., 2017).
A notable descriptive finding of this study is that 6.1% of never smokeless tobacco users initiated from baseline to 6-month follow-up. During the 1990s, smokeless tobacco use among young adults was relatively rare and disproportionately concentrated in males, relative to females (Rigotti et al., 2000). More recent research has found rates of smokeless tobacco initiation among young adults similar to those in our study. Specifically, data from 2011 to 2012 indicate that initiation of smokeless tobacco among young adult never users over a 12-month span was: 4.6% for chewing tobacco, dip, or snuff; 2.3% for snus; and 0.5% for dissolvable tobacco (Richardson et al., 2014), with younger individuals (i.e., 18–24 year olds) having the greatest odds of initiating non-combustible tobacco use (Richardson et al., 2014). The presented findings add to existing literature that suggests there has been a substantial shift in smokeless tobacco use behaviors among young adults (Enofe et al., 2014; Richardson et al., 2014).
A secondary finding of this study was that individuals of Asian Ancestry had greater odds of smokeless tobacco initiation (Adj OR: 2.19), relative to non-Hispanic whites. To our knowledge, this is the first study to observe this relationship between race and smokeless tobacco initiation. This is a particularly unique finding given that Asian Americans, relative to other racial/ethnic groups, traditionally report lower levels of tobacco use (Wang, Asman, Gentzke, et al., 2018). However, there is much variation within this population as unique cultural attitudes influence use within subgroups. For example Korean American women and Vietnamese men have tobacco use prevalence rates > 20%; substantially greater than the 7% prevalence among all Asian Americans (Martell, Garrett, & Caraballo, 2016; Wang et al., 2018). Similarly, individuals from the south Asia region (i.e., India) have a high rate of smokeless tobacco use (Messina, Freeman, Rees, et al., 2013; Mukherjea, Modayil, & Tong, 2018), largely due to cultural smokeless tobacco products such as paan, paan masala, and gutka (Messina et al., 2013; Mukherjea et al., 2018). Research has found that Asian Indians have greater rates of cultural smokeless tobacco use than conventional cigarette smoking (Messina et al., 2013) and that cultural smokeless tobacco use is frequent even among younger Asian Indians born in English speaking countries (Mukherjea et al., 2018). Further study is needed to provide a comprehensive examination of tobacco use behaviors, including initiation, among Asian Americans.
Strengths in sample recruitment and study design may also explain the secondary finding pertaining to smokeless tobacco initiation among individuals of Asian ancestry. Specifically, previous studies of smokeless tobacco use have relied on study samples that are largely homogenous in race/ethnicity, often with 60–80% non-Hispanic white and < 10% of other race/ethnicity groups (Enofe et al., 2014; Richardson et al., 2014; Rigotti et al., 2000) and typically re-classify participants of Asian ancestry with other racial/ethnic minorities (e.g., Native Americas; Pacific Islanders) (Enofe et al., 2014; Richardson et al., 2014; Rigotti et al., 2000). Conversely, the sample for the current study was majority-minority, with a similar number of non-Hispanic whites (34.4%) as Hispanic/Latinos (29.9%) as well as sizable percentage of individuals with Asian ancestry (20.4%). From an analytic perspective, the racial/ethnic diversity of our study sample reduces the probability of failing to reject the null hypothesis (i.e., Type II error), thus decreasing the bias of our findings (Woodward, 1999). Further, study participants of Asian ancestry were not re-classified with other racial/ethnic groups, thus maintaining the construct validity of our comparisons across race/ethnicity (Burlew, Weekes, Montgomery, et al., 2011; Grimes & Schulz, 2002).
Recent data indicate that young adults are initiating tobacco use at alarming rates, with greater incidence of initiation than adolescents (Cheng et al., 2017; Perry, Pérez, Bluestein, et al., 2018; Thompson, Mowery, Tebes, & McKee, 2018). Given the concurrent increase in smokeless tobacco use among young adults (Agaku et al., 2014; Cheng et al., 2017; Lipari & Van Horn, 2017; Loukas et al., 2015; U.S. Department of Health and Human Services, 2014) and simultaneous decrease in use among youth (Jamal, Gentzke, Hu, et al., 2017), it is possible that trends in smokeless tobacco use may contribute to the growing divide in tobacco use initiation among youth and young adults. Our findings suggest that smokeless tobacco marketing exposure is a factor influencing this change in young adult tobacco use behaviors, specifically the initiation and increased susceptibility to smokeless tobacco use.
This study has some limitations. First, this study is specific to young adult college students in urban Texas and thus may not be representative of other demographics. However, the sample was racially/ethnically diverse and included two-year college students. This is an important strength of our study since minority populations and two-year college students typically use tobacco at higher rates compared other young adult groups (Biener, McCausland, Curry, & Cullen, 2011; Loukas, Murphy, & Gottlieb, 2008). Second, there is the possibility of recall bias as marketing exposure was assessed through self-reported measures. As such, future research might utilize additional methodologies, including ecological momentary assessment (Hébert et al., 2018; Shiffman, Stone, & Hufford, 2008; Soong, Chen, & Borzekowski, 2015), experimental studies of marketing exposure (Durkin, Bayly, & Wakefield, 2016; Maloney & Cappella, 2016), and direct observations of the tobacco marketing environment (i.e., point-of-sale). Finally, as each channel of marketing exposure was assessed utilizing a single-item measure and responses were dichotomous (i.e., “yes” or “no”) prior to generating a cumulative marketing exposure variable, the primary exposure variable of this study may be less robust than multiple-item measures with greater variability across responses.
Despite these limitations, study findings add to our understanding of the relationships between smokeless tobacco marketing exposure and smokeless tobacco use behaviors. Our findings indicate recall of exposure to smokeless tobacco marketing is associated with subsequent smokeless tobacco use/susceptibility among young adult college students in urban Texas, after controlling for other important factors related to smokeless tobacco use. Traditionally, tobacco prevention efforts have focused on youth while marketing directed at young adults remains largely unopposed (Ling & Glantz, 2002). Prevention efforts including counter-marketing campaigns should be developed for, and implemented among, young adults to ensure smokeless tobacco use among this demographic does not continue to increase.
Acknowledgements
Research reported in this publication was supported by grant number [1 P50 CA180906] from the National Cancer Institute and the Food and Drug Administration (FDA) Center for Tobacco Products. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
References
- Agaku IT, King BA, Husten CG, et al. (2014). Tobacco product use among adults—United States, 2012–2013. MMWR, 63(25), 542–547. [PMC free article] [PubMed] [Google Scholar]
- Altria Client Services Inc. Philip Morris USA Inc. and U.S. Smokeless Tobacco Company (2012). LLC comments FDA’s draft guidance for industry: Modified risk tobacco product applications. Retrieved from http://www.altria.com/About-Altria/Federal-Regulation-of-Tobacco/Regulatory-Filing/FDAFilings/Comments-to-FDA-on-IOM-MRTP-Report.pdf, Accessed date: 28 May 2018.
- Biener L, McCausland K, Curry L, & Cullen J (2011). Prevalence of trial of snus products among adult smokers. American Journal of Public Health, 101, 1874–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burlew AK, Weekes JC, Montgomery L, et al. (2011). Conducting research with racial/ethnic minorities: Methodological lessons from the NIDA clinical trials network. The American Journal of Drug and Alcohol Abuse, 37, 324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calantzopoulos A Remarks by Andre Calantzopoulos, chief operating officer, Philip Morris International Inc. Investor Day—June 21, 2012. 2012. Retrieved from https://edge.media-server.com/m/s/a27vta8g/p/ny3a2u57/l/1. Accessed May 28, 2018.
- Carpenter CM, Connolly GN, Ayo-Yusuf OA, & Wayne GF (2009). Developing smokeless tobacco products for smokers: An examination of tobacco industry documents. Tobacco Control, 18(1), 54–59. [DOI] [PubMed] [Google Scholar]
- Cheng Y, Rostron BL, Day HR, et al. (2017). Patterns of use of smokeless tobacco in US adults, 2013–2014. American Journal of Public Health, 107, 1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K, Fabian L, Mottey N, Corbett A, & Forster J (2012). Young adults’ favorable perceptions of snus, dissolvable tobacco products, and electronic cigarettes: Findings from a focus group study. American Journal of Public Health, 102(11), 2088–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power and analysis for the behavioral sciences (2nd ed.). Hillsdale, N.J: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Curry LE, Pederson LL, & Stryker JE (2011). The changing marketing of smokeless tobacco in magazine advertisements. Nicotine & Tobacco Research, 13, 540–547. [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Wackowski OA, Giovenco DP, Michelle T, Manderski B, Hrywna M, & Ling PM (2014). Examining market trends in the United States smokeless tobacco use: 2005–2011. Tobacco Control 23, 107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin SJ, Bayly M, & Wakefield MA (2016). Can e-cigarette ads undermine former smokers? An experimental study. Tobacco Regulatory Science, 2(3), 263–277. [Google Scholar]
- Enofe N, Berg CJ, & Nehl EJ (2014). Alternative tobacco use among college students: Who is at highest risk? American Journal of Health Behavior, 38, 180–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Trade Commission (2013). Smokeless tobacco report for 2011. Washington, DC: Federal Trade Commission. [Google Scholar]
- Federal Trade Commission (2018). Smokeless tobacco report for 2016. Washington, DC: Federal Trade Commission. [Google Scholar]
- Gilpin EA, White VM, & Pierce JP (2005). How effective are tobacco industry bar and club marketing efforts in reaching young adults? Tobacco Control 14, 186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grana RA, & Ling PM (2014). “Smoking revolution”: A content analysis of electronic cigarette retail websites. American Journal of Preventive Medicine, 46(4), 395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimes DA, & Schulz KF (2002). Bias and causal associations in observational research. Lancet, 359, 248–252. [DOI] [PubMed] [Google Scholar]
- Haddock CK, Weg MV, DeBon M, et al. (2001). Evidence that smokeless tobacco use is a gateway for smoking initiation in young adult males. Preventive Medicine, 32, 262–267. [DOI] [PubMed] [Google Scholar]
- Hébert ET, Vandewater EA, Businelle MS, Harrell MB, Kelder SH, & Perry CL (2018). Real time assessment of young Adults’ attitudes toward tobacco messages. Tobacco Regulatory Science, 4, 644–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds III, Josephine T, Loukas A, Chow S, et al. (2016). Using cognitive interviewing to better assess young adult E-cigarette use. Nicotine & Tobacco Research, 18, 1998–2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, Gentzke A, Hu SS, et al. (2017). Tobacco use among middle and high school students – United States, 2011–2016. MMWR, 66, 597–603. 10.15585/mmwr.mm6623al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DM, Majeed BA, Weaver SR, Sterling K, Pechacek TF, & Eriksen MP (2017). Prevalence and factors associated with smokeless tobacco use, 2014–2016. American Journal of Health Behavior, 41, 608–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkhoran S, Grana RA, Neilands TB, & Ling PM (2015). Dual use of smokeless tobacco or e-cigarettes with cigarettes and cessation. American Journal of Health Behavior, 39, 277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein EG, Berman M, Hemmerich N, Carlson C, Htut S, & Slater M (2016). Online E-cigarette marketing claims: A systematic content and legal analysis. Tobacco Regulatory Science, 2(3), 252–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong AY, Eaddy JL, Morrison SL, Asbury D, Lindell KM, & Ribisl KM (2017). Using the vape shop standardized tobacco assessment for retail settings (V-STARS) to assess product availability, Price promotions, and messaging in New Hampshire vape shop retailers. Tobacco Regulatory Science, 3, 174–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling PM, & Glantz SA (2002). Why and how the tobacco industry sells cigarettes to young adults: Evidence from industry documents. American Journal of Public Health, 92, 908–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipari RN, & Van Horn SL (May 31, 2017). Trends in smokeless tobacco use and initiation: 2002 to 2014. The CBHSQ report Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. [PubMed] [Google Scholar]
- Loukas A, Batanova M, Fernandez A, & Agarwal D (2015). Changes in use of cigarettes and non-cigarette alternative products among college students. Addictive Behaviors, 49, 46–51. [DOI] [PubMed] [Google Scholar]
- Loukas A, Chow S, Pasch KE, et al. (2016). College students’ polytobacco use, cigarette cessation, and dependence. American Journal of Health Behavior, 40, 514–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loukas A, Murphy JL, & Gottlieb NH (2008). Cigarette smoking and cessation among trade or technical school students in Texas. Journal of American College Health, 56, 401–407. [DOI] [PubMed] [Google Scholar]
- Maloney EK, & Cappella JN (2016). Does vaping in e-cigarette advertisements affect tobacco smoking urge, intentions, and perceptions in daily, intermittent, and former smokers? Health Communication, 2015(31), 129–138. 10.1080/10410236.2014.993496. [DOI] [PubMed] [Google Scholar]
- Mantey DS, Creamer MR, Pasch KE, & Perry CL (2018). Marketing exposure recall is associated with past 30-day single, dual, polytobacco use among US adolescents. Nicotine & Tobacco Research, 20, S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantey DS, Pasch KE, Loukas A, & Perry CL (2019). Exposure to point-of-sale marketing of cigarettes and E-cigarettes as predictors of smoking cessation behaviors. Nicotine & Tobacco Research, 21, 212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martell BN, Garrett BE, & Caraballo RS (2016). Disparities in adult cigarette smoking - United States, 2002-2005 and 2010-2013. MMWR, 65, 753–758. [DOI] [PubMed] [Google Scholar]
- McDonald B, Haardoerfer R, Windle M, Goodman M, & Berg C (2017). Implications of attrition in a longitudinal web-based survey: An examination of college students participating in a tobacco use study. JMIR Research Protocols, 3, e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejia AB, & Ling PM (2010). Tobacco industry consumer research on smokeless tobacco users and product development. American Journal of Public Health, 100, 78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina J, Freeman C, Rees A, et al. (2013). A systematic review of contextual factors relating to smokeless tobacco use among south Asian users in England. Nicotine & Tobacco Research, 15, 875–882. [DOI] [PubMed] [Google Scholar]
- Mukherjea A, Modayil MV, & Tong EK (2018). Moving toward a true depiction of tobacco behavior among Asian Indians in California: Prevalence and factors associated with cultural smokeless tobacco product use: Asian Indian tobacco use. Cancer, 124, 1607–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute and Centers for Disease Control and Prevention (2014). Report on smokeless tobacco and public health: A global perspective. Washington, DC: National Cancer Institute and Centers for Disease Control and Prevention. [Google Scholar]
- Olivier J, & Bell ML (2013). Effect sizes for 2×2 contingency tables. PLoS One, 8, e58777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osibogun O, Taleb ZB, Bahelah R, Salloum RG, & Maziak W (2018). Correlates of poly-tobacco use among youth and young adults: Findings from the population assessment of tobacco and health study, 2013–2014. Drug and Alcohol Dependence, 187, 160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parascandola M, Augustson E, & Rose A (2009). Characteristics of current and recent former smokers associated with the use of new potential reduced-exposure tobacco products. Nicotine & Tobacco Research, 11(12), 1431–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Pérez A, Bluestein M, et al. (2018). Youth or young adults: Which group is at highest risk for tobacco use onset? Journal of Adolescent Health, 63, 413–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piano MR, Benowitz NL, Fitzgerald GA, Corbridge S, Heath J, Hahn E, et al. (2010). Impact of smokeless tobacco products on cardiovascular disease: Implications for policy, prevention, and treatment: A policy statement from the American Heart Association. Circulation, 122(15), 1520–1544 (cited 2014 Oct 31). [DOI] [PubMed] [Google Scholar]
- Pierce JP, Choi WS, Gilpin EA, et al. (1996). Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychology, 15, 355e61. [DOI] [PubMed] [Google Scholar]
- Pokhrel P, Fagan P, Herzog TA, et al. (2016). E-cigarette advertising exposure and implicit attitudes among young adult non-smokers. Drug and Alcohol Dependence, 163, 134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P, Fagan P, Herzog TA, et al. (2018). Social media e-cigarette exposure and e-cigarette expectancies and use among young adults. Addictive Behaviors, 78, 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P, Fagan P, Kehl L, & Herzog TA (2015). Receptivity to e-cigarette marketing, harm perceptions, and e-cigarette use. American Journal of Health Behavior, 39, 121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds American. Tobacco harm reduction: market leadership through transformation. 2012. Available at: http://www.reynoldsamerican.com/harmreduction.cfm?plank=harmReduction2. Accessed May 28, 2018.
- Richardson A, Ganz O, Stalgaitis C, Abrams D, &Vallone D (2013). Noncombustible tobacco product advertising: How companies are selling the new face of tobacco. Nicotine & Tobacco Research, 16, 606–614. [DOI] [PubMed] [Google Scholar]
- Richardson A, Williams V, Rath J, Villanti AC, & Vallone D (2014). The next generation of users: Prevalence and longitudinal patterns of tobacco use among US young adults. American Journal of Public Health, 104, 1429–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti NA, Lee JE, & Wechsler H (2000). US college students’ use of tobacco products: Results of a National Survey. JAMA, 284(6), 699–705. 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- Roberts ME, Doogan NJ, Kurti AN, et al. (2016). Rural tobacco use across the United States: How rural and urban areas differ, broken down by census regions and divisions. Health & Place, 39, 153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson L, McGee R, Marsh L, & Hoek J (2015). A systematic review on the impact of point-of-sale tobacco promotion on smoking. Nicotine & Tobacco Research, 17(1), 2–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romito LM, Saxton MK, Coan LL, & Christen AG (2011). Retail promotions and perceptions of R.J. Reynolds’ novel dissolvable tobacco in a US test market. Harm Reduction Journal, 8, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sepe E, Ling PM, & Glantz SA (2002). Smooth moves: Bar and nightclub tobacco promotions that target young adults. American Journal of Public Health, 92, 414e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. [DOI] [PubMed] [Google Scholar]
- Soneji S, Sargent JD, Tanski SE, & Primack BA (2015). Associations between initial water pipe tobacco smoking and snus use and subsequent cigarette smoking: Results from a longitudinal study of US adolescents and young adults. JAMA Pediatrics, 169, 129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soong A, Chen JC, & Borzekowski DL (2015). Using ecological momentary assessment to study tobacco behavior in urban India: there’s an app for that. JMIR Research Protocols, 4, e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam J, Day HR, Rostron BL, & Apelberg BJ (2015). A systematic review of transitions between cigarette and smokeless tobacco product use in the United States. BMC Public Health, 15, 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson AB, Mowery PD, Tebes JK, & McKee SA (2018). Time trends in smoking onset by sex and race/ethnicity among adolescents and young adults: Findings from the 2006-2013 National Survey on drug use and health. Nicotine & Tobacco Research, 20, 312–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrul J, Lisha NE, & Ling PM (2016). Tobacco marketing receptivity and other tobacco product use among young adult bar patrons. Journal of Adolescent Health, 59, 642–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timberlake D (2016). Advertising receptivity and youth initiation of smokeless tobacco. Substance Use & Misuse, 51(9), 1077–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timberlake DS, Pechmann C, Tran SY, & Au V (2011). A content analysis of Camel Snus advertisements in print media. Nicotine & Tobacco Research, 13, 431–439. [DOI] [PubMed] [Google Scholar]
- Tomar S (2003). Is use of smokeless tobacco a risk factor for cigarette smoking? The U.S. experience. Nicotine & Tobacco Research, 5, 561–569. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2012). Preventing tobacco use among youth and young adults: A report of the surgeon general Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- U.S. Department of Health and Human Services (2014). The health consequences of smoking—50 years of progress: A report of the surgeon general Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- U.S. Department of Health and Human Services (2016). E-Cigarette use among youth and young adults. A report of the surgeon general Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- University of Medicine and Dentistry of New Jersey, School of Public Health (2010). Marketing smokeless tobacco: Moist snuff, snus, dissolvables. Trinkets and Trash: Artifacts of the Tobacco Epidemic. Available at http://trinketsandtrash.org/tt-feature. [Google Scholar]
- Vespa J, Armstrong DM, & Medina L (2018). Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports, P25-1144 Washington, DC: U.S. Census Bureau. [Google Scholar]
- Wang TW, Asman K, Gentzke AS, et al. (2018). Tobacco product use among adults - United States, 2017. MMWR, 67, 1225–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward M (1999). Epidemiology: Study design and data analysis. Boca Raton, FL: Chapman & Hall/CRC Press. [Google Scholar]
- World Health Organization (2007). IARC monographs on the evaluation of carcinogenic risks to humans. Smokeless Tobacco and Some Tobacco-Specific N-Nitrosamines. [PDF–3.18 MB], Vol 89. Lyon (France): World Health Organization, International Agency for Research on Cancer. [PMC free article] [PubMed] [Google Scholar]


