To the Editor,
Small-sized (<10mm) basal cell carcinoma (BCC) lacking specific dermoscopic features are challenging to diagnose. Even with reflectance confocal microscopy (RCM) the specificity remains low (37.5%−75.5%)1 due to limited imaging depth (200 μm), en face visualization, and a lack of melanin contrast for non/lightly pigmented lesions.2 A novel, combined, hand-held RCM and optical coherence tomography (OCT) device (RCM-OCT) has been developed to overcome these limitations. RCM-OCT provides real-time en-face RCM and vertical OCT3 images simultaneously and has been shown to confirm the diagnosis of BCC4; however, it has not been evaluated for equivocal lesions in clinical settings. In a Tertiary Cancer Center, we performed an IRB-approved prospective study to assess the performance of RCM-OCT over RCM-alone for the diagnosis of lesions equivocal for BCC. We enrolled consecutive patients referred by dermoscopy experts for routine RCM imaging over one year.
Two RCM-OCT readers, an expert (M.J.) and a novice (J.M.) first evaluated the routine RCM images for features of BCC2 and made a diagnosis of ‘BCC’ or ‘non-BCC’. Next, the same lesions were re-imaged with RCM-OCT; OCT features of BCC5 were evaluated and a final RCM-OCT diagnosis (‘BCC’ or ‘non-BCC’) was rendered. Diagnostic confidence was recorded for each device. Image acquisition time was ≤10 minutes per lesion with the RCM-OCT device. All lesions were biopsied for histopathology confirmation.
To validate our results and confirm the utility of RCM-OCT over RCM-alone and OCT-alone, another expert (N.D.) examined two separate, randomized datasets retrospectively: one with RCM images and another with OCT images. The expert noted the presence or absence of BCC features on RCM2 and OCT5 images separately before rendering a final diagnosis of ‘BCC’ or ‘non-BCC’ with confidence levels.
For data analysis, the final diagnoses were given a binary score of ‘1’ or ‘0’ for BCC or non-BCC, respectively. Diagnostic confidence was stratified as −2 for non-BCC and −1, 0, 1, and 2 for BCC, ranging from ‘indeterminant’ to ‘high confidence’. Finally, the diagnoses and diagnostic confidence scores were added to generate ROC curves, area under the curve (AUC), sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for each evaluation.
Eighteen equivocal lesions were imaged from 18 patients (Table 1; supplementary material). On histopathology, 56% lesions were BCCs and 44% benign. Prospective analysis using RCM-alone for the diagnosis of BCC yielded an AUC of 0.85 with 90% sensitivity, 62.5% specificity, 75% PPV, and 83% NPV. With RCM-OCT, the results improved to an AUC of 1 with 100% sensitivity, specificity, PPV, and NPV. Prospective and retrospective analysis of RCM-alone yielded similar results; however, OCT-alone showed inferior results (AUC of 0.81; 90% sensitivity; 50% specificity; 69% PPV; 80% NPV).
RCM-OCT improved the diagnosis of featureless dermoscopic lesions equivocal for BCC, especially specificity, for non/lightly pigmented lesions on the face. We anticipate that when RCM-OCT device becomes commercially available, the cost and readers’ learning curve would be comparable to existing RCM and OCT devices.2,5 The main limitation was a relatively small patient cohort which might explain more female participants in this study. Large-scale studies are needed to validate our promising results.
Supplementary Material
Figure 1 (A) and Figure 2 (B):
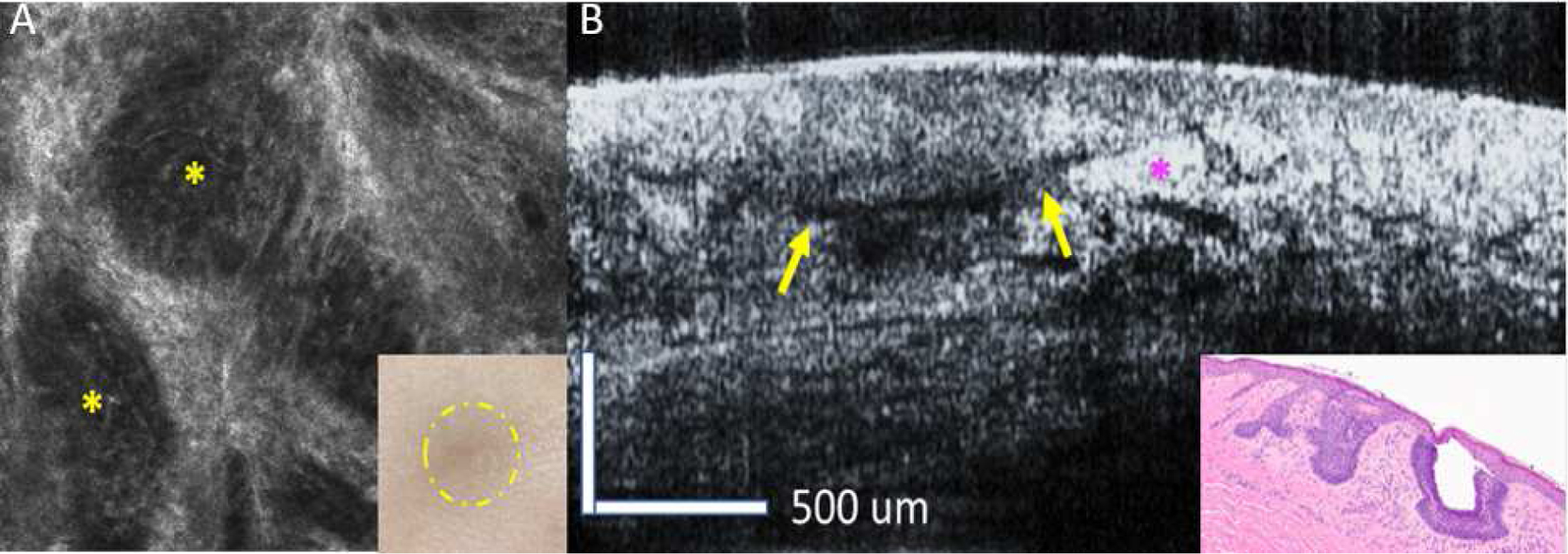
Images of a small 2 mm non-pigmented equivocal papule, featureless on dermoscopy (inset A, circled area), acquired with an RCM hand-held device (A) and an RCM-OCT device (B). (A) RCM image shows a dark silhouette at the level of epidermis/ dermo-epidermal junction (yellow asterisks). In the absence of a definitive BCC tumor nodule with palisading and clefting a diagnosis of BCC with moderate confidence was made with RCM- alone. (B) OCT image acquired with the RCM-OCT device shows a grey nodule connected to the epidermis with clefting (yellow arrow) and compressed collagen compressed bundle (purple asterisks). The BCC tumor nodule measured 220 μm in depth on OCT. Combined RCM-OCT increased the diagnostic confidence for BCC over RCM-alone which led to the direct excision of the lesion. The lesion showed a superficial BCC on histopathology (inset B). FOV: RCM image= 0.75mm x 0.75mm; OCT image= 2 mmx 1mm; H&E image: 10x magnification.
Funding sources:
This project was supported by the National Institutes of Health Grant No.2R44CA162561, National Cancer Institute Cancer Center Support Grant No. P30 CA008748.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest:
Manu Jain received one time travel re-imbursement in past by Caliber ID for a scientific congress. Nicusor Iftimia works at Physical Sciences, Inc. However, the company does not have any financial interest, as this is research instrument, and its development was funded by NIH.
The other authors have no disclosures or conflicts of interest to report.
IRB approval status: Reviewed and approved by Western IRB; approval #99–099, retrospective # 17–078
Supplementary figure: Table with patient and lesion demographics Attachments: CONSORT checklist, research protocol
Supplemental material available at https://data.mendeley.com/datasets/f95b7wh83x/1
References
- 1.Kadouch DJ, Leeflang MM, Elshot YS, Longo C, Ulrich M, van der Wal AC, et al. Diagnostic accuracy of confocal microscopy imaging vs. punch biopsy for diagnosing and subtyping basal cell carcinoma. J Eur Acad Dermatol Venereol oct 2017;31(10):1641–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain M, Pulijal SV, Rajadhyaksha M, Halpern AC, Gonzalez S. Evaluation of Bedside Diagnostic Accuracy, Learning Curve, and Challenges for a Novice Reflectance Confocal Microscopy Reader for Skin Cancer Detection In Vivo. JAMA Dermatol January 2018;154(8):962–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iftimia N, Yélamos O, Chen C-SJ, Maguluri G, Cordova MA, Sahu A, et al. Handheld optical coherence tomography–reflectance confocal microscopy probe for detection of basal cell carcinoma and delineation of margins. JBO. juill 2017;22(7):076006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sahu A, Yélamos O, Iftimia N, Cordova M, Alessi-Fox C, Gill M, et al. Evaluation of a Combined Reflectance Confocal Microscopy-Optical Coherence Tomography Device for Detection and Depth Assessment of Basal Cell Carcinoma. JAMA Dermatol January 2018;154(10):1175–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmes J, Braunmühl T von, Berking C, Sattler E, Ulrich M, Reinhold U, et al. Optical coherence tomography of basal cell carcinoma: influence of location, subtype, observer variability and image quality on diagnostic performance. British Journal of Dermatology 2018;178(5):1102–10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


