Abstract
Background
Scholarly activity is a requirement for most graduate medical education training programs. However, barriers exist for residents to accomplish projects.
Objective
To evaluate the correlation between a resident research mentoring team (RRMT) program and meeting presentations and publications of resident research projects. We further plan to report feasibility of the RRMT.
Methods
We performed a before-and-after study of meeting presentations and/or publication of resident research projects before institution of the RRMT (2004-2011) and post-RRMT implementation (2016-2019). The RRMT is a diverse group of faculty, statisticians, and research staff who meet regularly with residents to provide guidance for their research studies. It is part of overall research support from the department, which also includes biostatistics, database and regulatory help, travel funds, and project budget funds. Data on meeting presentations and publications were collected from Google Scholar, PubMed, Scopus, and the IUPUI ScholarWorks institutional repository, using resident and faculty names and titles of projects. Comparisons of pre- and post-RRMT groups were made.
Results
Seventy-four residents were in the pre-RRMT group and 40 were in the post-RRMT group. Post-RRMT residents published, presented, and combined published or presented their projects more frequently than those in pre-RRMT group (57.5% vs 28.4%, P=.002; 50% vs 16.2%, P=.001; 67.5% vs 37.8%, P=.002). Controlling for winning a Research Day award and pursuing a fellowship, being in the post-RRMT group was independently associated with presentation or publication of the resident research project (OR 3.62, 95% CI 1.57-8.83).
Conclusions
Support of resident scholarly activity, such as thorough implementation of a program like the RRMT, is associated with increased presentations and publications of research projects.
Introduction
Scholarly engagement in medicine is an important topic that has been frequently addressed by medical educators.1-6 Residency training offers a critical opportunity window with regard to fostering scholarly engagement among future physicians. While clinical training remains the main purpose of residency, resident scholarly activity, often functionally defined as performing a research project, is required during that training.7 Resident research productivity, measured in publications, scholarly presentations, and program involvement, has been shown to positively correlate with clinical performance, satisfaction during residency, and future employment.8-10 Publication output during residency was also found to be predictive of academic achievements such as fellowship training, which can be a notable external motivating factor for residents' involvement in research.9,11 In addition, the incorporation of research curricula in residency programs has led to more physicians pursuing primary careers in research.10
While the Accreditation Council for Graduate Medical Education (ACGME) has mandated that all accredited programs promote resident engagement in research to address 3 ACGME Core Competencies (Medical Knowledge, Practice-Based Learning and Improvement, and Professionalism),7 there is lack of uniformity in how programs satisfy this requirement. Support provided to residents for research activities also varies widely. Some programs focus on enhancing a culture supportive of science, peer-to-peer mentorship, establishment of groups focused on helping with study design and project lists, structured curricula, and support for services such as biostatistics.12-15 Some implemented programs, however, address only a few of the barriers to or costs of enhancing research productivity for trainees. Several challenges face accredited residency programs with regard to attaining the scholarly activity requirement. These challenges include structural and funding limitations, limited faculty and resident time, lack of a research curriculum and mentors, inadequate resident research skills and interest, and the perception that engaging in scholarly activities is time taken away from clinical training.15-17 In fact, surveys reveal that more than half of residency programs lack research curricula or statistics-centered didactics.8,18
After recognizing struggles our residents encountered in their research activity, in 2012 the obstetrics and gynecology department developed a resident research mentoring team (RRMT). The primary objective of this study was to describe and evaluate the impact of RRMT implementation on resident research productivity. A secondary objective was to determine if productivity was higher for residents winning research presentation awards or in pursuit of fellowship training. A third objective was to report on feasibility of the program.
Methods
Setting and Program Participants
The RRMT is an interdisciplinary team created by the Vice Chair for Research and Residency Program leadership that was constructed based on feedback by residents when asked what resources would be most helpful to them and their primary faculty advisor to better engage during the research/scholarly activity process. Our RRMT is part of an overall program of support for resident research (as well as student, fellow, and faculty research) provided by the department. The department's support is meant to address and overcome all the barriers commonly identified by our residents and faculty members. Our department is part of a large academic medical center in the Midwest with 10 residents per year. As noted in the Box, at implementation of the RRMT, resources were added to previous areas of support.
The interdisciplinary team meets with the residents at least 4 times during their research endeavors. The team is made of several faculty members with interest in research who have expertise in cohort studies, qualitative research, clinical trials, lab-based translational research, survey studies, and other areas. The data manager, regulatory specialist, data/informatics scientist, biostatisticians, and if applicable, research coordinators with expertise in participant recruitment, are all invited to the meetings. Residents, with their primary faculty advisor, present their project ideas, in whatever phase they are in, and solicit advice to develop a plan for their projects with the experts in the room.
Resident Research Timeline
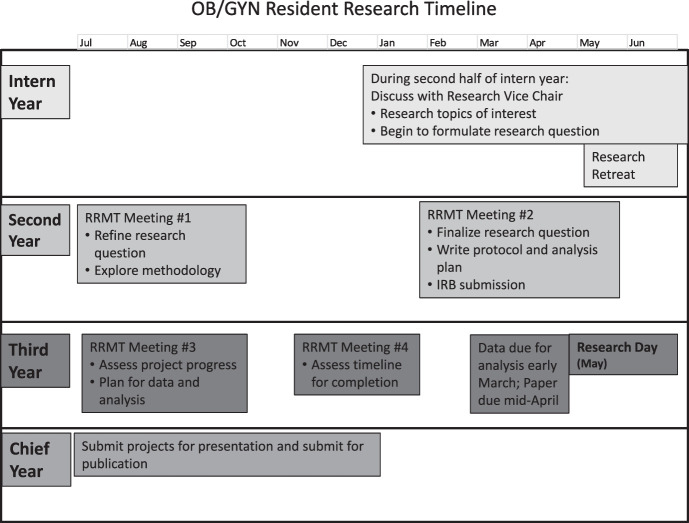
The research journey for the residents in our program, which used to begin and end in the third year, has been transformed through an iterative process with feedback from the residents and faculty. The journey now begins in the first year and encompasses the following (Figure):
Figure.
Schematic Representation of Resident Research Experience Over 4 Years of Obstetrics and Gynecology Residency
Abbreviations: OB/GYN, obstetrics or gynecology rotation; RRMT, resident research mentoring teams; IRB, institutional review board.
Note: Meeting #1 is focused on developing a project idea and research question and understanding the background, motivation, and hypotheses for the study topics. Meeting #2 is focused on refining the research study question and methodology. This includes working with the statisticians on sample size calculation, regulatory specialists on IRB submissions if not already accomplished, and planning for data collection. Meeting #3 is focused on performance of the study and troubleshooting issues that have arisen. If it is clear the project will not be able to succeed, a pivot alternative project is discussed. Meeting #4 is focused on how to bring the study to completion or alternatively determining if the project is on track to succeed and complete on time and if a pivot alternate project is needed.
-
▪
First year: In the spring, interns meet one-on-one with the vice chair for research to discuss potential research questions and are given directed readings or ideas for advisors. An intern research retreat is held in June where there is an informal half day of instruction about study designs along with tales of research journeys from various faculty members.
-
▪
Second year: The RRMT meets with the residents early and midway through the year to give more formal guidance on project activities. A checklist with all pertinent contacts, instructions, and timelines is provided.
-
▪
Third year: The RRMT meets 2 more times with the residents to document project progress. Guidance is given to help successful completion of the project. In the spring of third year is Research Day where residents are expected to present their research.
-
▪
Fourth year: All residents are encouraged, but not required, to submit and present their research at a national meeting and to submit for publication.
Analysis
We hypothesized that the establishment of a formal resident research program that relied heavily on mentorship and guided support would lead to higher research productivity during residency training. We explored this hypothesis through a retrospective before-and-after study of 2 cohorts of graduates of our obstetrics and gynecology residency program. The first cohort encompassed classes of 2004-2011 (pre-RRMT implementation), while the second encompassed classes of 2016-2019 (post-RRMT implementation). Classes of 2012-2015 were excluded as a washout cohort during RRMT implementation and revision. We analyzed 3 outcomes: publication of the project, presentation of the project at a regional or national meeting, or a combined outcome of the project being either presented or published. This combined outcome represents any type of dissemination of the project by the resident beyond the Research Day presentation. Research productivity was assessed through the percentage of graduates whose projects achieved these outcomes. We performed the search in December 2021 to allow for at least 2 years after resident graduation (3 years after Research Day presentation) for the national meeting or publication to occur. With the guidance and assistance of our departmental librarian, research projects were checked against publication and presentation statuses using Google Scholar, PubMed, Scopus, and the IUPUI ScholarWorks institutional repository. The results of this search were then confirmed with the corresponding research project mentors and the residents themselves whenever possible.
We compared the 2 cohorts with regard to research productivity and examined the relationship between this productivity and the pursuit of fellowship training. Finally, we explored the relationship between Research Day award-winning resident projects and likelihood of these projects being published and/or presented at regional or national conferences. Our program has a maximum of 10 residents per year, and there are awards for the top 3 presented abstracts, determined by a panel of 3 Research Day judges. Given our fixed sample size, we did not perform an a priori sample size calculation. However, with 40 in the RRMT group and about twice as many in the pre-RRMT group, we would have 99% power to detect a doubling of the rate of presentation or publication. A chi square test was utilized in comparing the categorical variables with statistical significance defined as P<.05. Confidence intervals around the main point estimates were calculated using the Clopper-Pearson (exact) method. To determine the impact of the RRMT on productivity, we performed a logistic regression including pursuit of fellowship training and winning an award on Research Day in the model. All statistical analyses were performed using IBM SPSS Statistics version 28. This study was deemed exempt from institutional review board approval. No funding was provided for this study.
Results
The pre-RRMT cohort consisted of 74 residents, while the post-RRMT cohort consisted of 40 residents. Residents in the post-RRMT cohort were more likely to publish their research projects compared to pre-RRMT residents (57.5% vs 28.4%; P= .002), present them at regional and national conferences (50% vs 16.2%; P<.001), and be in the combined outcome of either publishing or presenting them (67.5% vs 37.8%; P= .002; Table 1). The projects were both presented and published more frequently in the post-RRMT group as well (40% vs 6.8%; P<.001). As these were their projects, the residents were almost universally the main presenters or lead authors.
Table 1.
Rates of Publication, Presentation, or Either Across Pre- and Post-RRMT Cohorts
| Publication/Presentation | Pre-RRMT (n=74) | Post-RRMT (n=40) | P value | |
| Published, n (%; 95% CI) | Yes | 21 (28.4; 18.5-40.1) | 23 (57.5; 40.9-73.0) | .002 |
| No | 53 (71.6; 59.9-81.5) | 17 (42.5; 27.0-59.1) | ||
| Presented, n (%; 95% CI) | Yes | 12 (16.2; 7.7-25.0) | 20 (50.0; 33.8-66.2) | .001 |
| No | 62 (83.8; 75.0-92.3) | 20 (50.0; 33.8-66.2) | ||
| Published or presented, n (%; 95% CI) | Yes | 28 (37.8; 25.6-48.5) | 27 (67.5; 50.9-81.4) | .002 |
| No | 46 (62.2; 51.5-74.4) | 13 (32.5; 18.6-49.1) | ||
| Published and presented, n (%; 95% CI) | Yes | 5 (6.8; 2.2-15.1) | 16 (40; 24.9-56.7) | <.001 |
| No | 69 (93.2; 84.9-97.8) | 24 (60.0; 43.3-75.1) | ||
Abbreviation: RRMT, resident research mentoring team.
Note: Data presented as n (% for point estimate; 95% CI around the point estimate).
Both cohorts had similar rates of fellowship pursuit (14 of 74 [18.9%] pre-RRMT cohort vs 8 of 40 [20%] post-RRMT cohort). Overall, while those who went for fellowship training had higher rates of being likely to publish (54.4% vs 34.8%; P= .09), present (31.8% vs 27.2%; P= .66), and publish or present (63.6% vs 44.6%; P= .11) their projects across both cohorts when compared to residents who did not go on to fellowship training, these differences were not statistically significant. Prior to RRMT implementation, those residents going to fellowship were 23.8% more likely to publish or present their research projects when compared to their non-fellowship-bound residents (P = .10), while the difference between post-RRMT fellowship aspiring trainees and non-fellowship-bound residents was less than 10% (75% vs 65.6%; P= .61; Table 2).
Table 2.
Fellowship-Bound and Research Day Award-Winning Status and Rates of Publication, Presentation, or Either of Research Projects in Pre- and Post-RRMT Cohorts
| Publication/ Presentation | Fellowship, n (%) | Award-Winning, n (%) | ||||||
| Yes (n=14 Pre-RRMT, 8 Post-RRMT) | No (n=60 Pre-RRMT, 32 Post-RRMT) | P value | Yes (n=25 Pre-RRMT, 12 Post-RRMT) | No (n=49 Pre-RRMT, 28 Post-RRMT) | P value | |||
| Pre-RRMT | Published | Yes | 6 (42.9) | 15 (25) | .18 | 11 (44) | 10 (20.4) | .033 |
| No | 8 (57.1) | 45 (75) | 14 (56) | 39 (79.6) | ||||
| Presented | Yes | 4 (28.6) | 8 (13.3) | .16 | 5 (20) | 7 (14.3) | .53 | |
| No | 10 (71.4) | 52 (86.7) | 20 (80) | 42 (85.7) | ||||
| Published or presented | Yes | 8 (57.1) | 20 (33.3) | .10 | 12 (48) | 16 (32.7) | .20 | |
| No | 6 (42.9) | 40 (66.7) | 13 (52) | 33 (67.3) | ||||
| Post-RRMT | Published | Yes | 6 (75) | 17 (53.1) | .26 | 7 (58.3) | 16 (57.1) | .94 |
| No | 2 (25) | 15 (46.9) | 5 (41.7) | 12 (42.9) | ||||
| Presented | Yes | 3 (37.5) | 17 (53.1) | .43 | 8 (66.7) | 12 (42.9) | .17 | |
| No | 5 (62.5) | 15 (46.9) | 4 (33.3) | 16 (57.1) | ||||
| Published or presented | Yes | 6 (75) | 21 (65.6) | .61 | 9 (75) | 18 (64.3) | .21 | |
| No | 2 (25) | 11 (34.4) | 3 (25) | 10 (35.7) | ||||
Abbreviation: RRMT, resident research mentoring team.
Award-winning resident projects were more often published, presented, and published or presented when compared to projects that did not win awards both in the pre- and post-RRMT cohorts (Table 2). This difference was statistically significant for publication rate in the pre-RRMT cohort (44% vs 20.4%; P= .033) but not in the post-RRMT cohort (58.3% vs 57.1%; P= .94). Seventy-five percent of first-place award-winning residents published their research projects both prior to and after RRMT implementation compared to 22.7% in the pre-RRMT cohort and 55.6% in the post-RRMT cohort (P= .006).
To better assess the impact of implementing RRMT we ran logistic regression on both cohorts accounting for award-winning and fellowship pursuit statuses, which revealed that RRMT independently increased odds to publish or present resident research projects (OR=3.62; 95% CI 1.57-8.31; Table 3).
Table 3.
Logistic Regression for Factors Associated With Presenting or Publishing Resident Research Projects
| Characteristic | OR (95% CI) |
| Group (post-RRMT vs pre-RRMT) | 3.62 (1.57-8.83) |
| Won award on research day (yes vs no) | 1.62 (0.69-3.82) |
| Pursued fellowship training (yes vs no) | 2.03 (0.73-5.68) |
Abbreviation: RRMT, resident research mentoring team.
Note: Logistic regression adjusted for each factor input in the model.
Regarding feasibility, the RRMT itself is an “in-kind” activity of interested faculty and was typically conducted during protected didactic time for residents and faculty. No financial departmental faculty compensation was provided (Box). The additional support provided for travel for residents to present their work, and the additional personnel costs for a regulatory coordinator and database manager to aid with project support, total an additional $46,000 to the department support budget annually (∼$4,600 per resident).
Objectives
We sought to evaluate the correlation between a resident research mentoring team (RRMT) program and meeting presentations and publications of resident research projects.
Findings
Controlling for winning a Research Day award and pursuing a fellowship, being in the post-RRMT group was independently associated with presentation or publication of the resident research project (OR 3.62, 95% CI 1.57-8.83).
Limitations
Our study was limited in that the RRMT was part of an overall support for resident scholarly activity, we may have missed some publications or presentations, and we did not control for the number of publications a resident had before entering the program.
Bottom Line
Support of resident scholarly activity, such as thorough implementation of a program like the RRMT, is associated with increased presentations and publications of research projects.
Discussion
In this study, we found that implementation of an RRMT, along with other support resources, increased the number of resident research projects that went on to be presented and/or published. This was true even controlling for residents pursuing fellowship training or winning research awards. Interestingly, winning an award at Research Day was associated with a higher rate of project publication in the pre-RRMT group. We found that there were higher rates of projects being presented or published for pre-RRMT residents pursuing fellowships compared to non-fellowship-bound residents (57.1% vs 33.3%), but the difference was not statistically significant. Most other analyses on this topic have not considered these resident and project characteristics.12-14
Supporting high-quality research to meet the requirement for scholarly activity has many benefits.15,19,20 Research involvement expectations were key in deciding whether to pursue a career in academic medicine or fellowship training, with the relationship between the 2 likely being bidirectional.15,20 While research requirements have become universal across ACGME-accredited residency programs, studies suggest several barriers continue to impede attaining that goal.8,19 A gap appears to exist between goals and expectations of residency programs and directors, and the research experience of residents during their training. Many residents report dissatisfaction with the research environment and training at their program and note that they are uncomfortable discussing basic study designs and interpreting basic statistics.8,19 Other barriers likely in play include limited resources, as well as a lack of time, mentorship, interest, and effective outcome assessment.21-24 Our RRMT program, embedded within a variety of support resources aimed at overcoming commonly cited barriers to resident engagement in research (Box), has helped overcome some of these barriers to improve productivity.
In response to challenges of supporting research, programs across specialties have explored initiatives and evaluated their effectiveness toward attaining and sometimes exceeding ACGME requirements.13,15,25 A recent systematic review revealed that mentorship, curriculum, and protected time were the most reported initiatives utilized by residency programs.26 Of note, variation exists in how these initiatives are implemented by various programs. For example, mentorship can take the form of a dedicated resident research director, a paired mentor, or regular meetings, among others.9,15 Dedicated time can take the form of a dedicated research rotation, as well as continuous or longitudinal dedicated time.9,13,15 Surgical specialty training programs often have difficulty instituting protected research block time given the number of surgical cases required for graduation.7,12
Other reported program-specific initiatives have been implemented and evaluated within residency programs of many different specialties, often taking the form of bundled interventions such as ours. Successful initiatives comprised various forms of mentorship, including the recruitment of assistant program directors and simultaneous implementation of research curriculums, formal mentorship with or without programmatic deadlines, and the addition of research study teams.14,27-29 Other successful interventions included financial support, the recruitment of a medical editor, biweekly research workshops, and providing protected research time.15,29,30 Focused efforts to develop a sustainable research curriculum have been developed for various specialties, including general surgery.14
To overcome the potential limitation in capturing all possible research presentations or publications, we engaged multiple resources to accurately discover all presentations and publications. Conversely, more recent projects may be in a publication pipeline and not published yet. This was why we used the combined outcome of presentation or publication as evidence of the resident project going forward beyond Research Day. The shorter possible publication time for post-RRMT studies would potentially bias against the post-RRMT group. This makes our finding of increased productivity in the post-RRMT group potentially more notable. We did not control for the number of publications a resident may have had during medical school. Additionally, several residents perform multiple projects during their residencies. We considered only the one project that was presented at Research Day. In addition, our sample size limited the power to detect differences in some of our subgroup analyses. While we did not categorize every resident project (eg, clinical project, quality improvement, survey, etc), most of our resident projects are clinical research studies and use an array of study designs. We would be underpowered to perform any meaningful comparisons based on study design. A feasibility limitation for the program may be that some residencies may lack the faculty expertise, time, or access to other resources to support the project, thus possibly limiting generalizability.
Conclusions
In conclusion, our RRMT intervention and existing support was correlated with an increase in resident presentations and publications with a feasible use of resources.
Box Departmental Program of Support for Faculty and Trainee Research
The following lists the overall departmental support for resident research at the time of the resident research mentoring team (RRMT). These resources are now also available for fellows and faculty but originally were funded for residents. Over the first 3 years of the program (2012-2015), the overall support evolved to encompass all the components below. By 2015, the RRMT and program of support were codified as the following measures.
-
▪
Salary support for several members of the biostatistics department to aid residents with analytic plans, data analysis, presentation, and manuscript writing help. This includes ∼0.2 full-time equivalent (FTE) for a PhD statistician and 0.5 FTE for a Master's level statistician (total support cost is ∼$100,000 per year, with some offset by research grants)a
-
▪
Salary support for a database manager to help ensure security of research data through guiding residents through REDCap database creation for their projects (∼$25,000 per year, mostly offset through research grants)
-
▪
Salary support for a regulatory specialist to help advise residents and provide guidance throughout the institutional review board submission process (total salary ∼$68,000 per year, about 25% of effort dedicated for residents, some offset by research grants)
-
▪
Additional funding for research budgets for projects ($5,000 per year, typically)a
-
▪
Additional travel funding provided for residents to present their work at national conferences and meetings (budgeted $4,000 per year)
-
▪
Salary support for a data core scientist to aid residents in large retrospective clinical database searches (budgeted ∼$10,000 per year)a
a Resources also available during the pre-RRMT implementation.
Funding Statement
Funding: The authors report no external funding source for this study.
Footnotes
Conflict of interest: The authors declare they have no competing interests.
This work was previously presented as a poster at the 2022 Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists, May 7, 2022, San Diego, CA.
References
- 1.Fincher RM, Simpson DE, Mennin SP, et al. Scholarship in teaching: an imperative for the 21st century. Acad Med . 2000;75(9):887–894. doi: 10.1097/00001888-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Simpson D, Fincher RM, Hafler JP, et al. Advancing educators and education by defining the components and evidence associated with educational scholarship. Med Educ . 2007;41(10):1002–1009. doi: 10.1111/j.1365-2923.2007.02844.x. [DOI] [PubMed] [Google Scholar]
- 3.Glassick CE. Boyer's expanded definitions of scholarship, the standards for assessing scholarship, and the elusiveness of the scholarship of teaching. Acad Med . 2000;75(9):877–880. doi: 10.1097/00001888-200009000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Glassick CE. Reconsidering scholarship. J Public Health Manag Pract . 2000;6(1):4–9. doi: 10.1097/00124784-200006010-00003. [DOI] [PubMed] [Google Scholar]
- 5.Irby DM, Cooke M, Lowenstein D, Richards B. The academy movement: a structural approach to reinvigorating the educational mission. Acad Med . 2004;79(8):729–736. doi: 10.1097/00001888-200408000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Simpson DE, Fincher RM. Making a case for the teaching scholar. Acad Med . 1999;74(12):1296–1299. doi: 10.1097/00001888-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education. Common Program Requirements (Residency) 2021. Accessed March 29, 2023. https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/CPRResidency_2022v2.pdf.
- 8.Kenton K, Brubaker L. Research education in obstetrics and gynecology: how are we doing. Am J Obstet Gynecol . 2007;197(5):532.e1–4. doi: 10.1016/j.ajog.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 9.Seaburg LA, Wang AT, West CP, et al. Associations between resident physicians' publications and clinical performance during residency training. BMC Med Educ . 2016;16(1):22. doi: 10.1186/s12909-019-1858-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tamim H, Zeineldine S, Tabbara F, et al. Structure and evaluation of a residency research program in a university hospital. BMC Med Educ . 2019;19(1):406. doi: 10.1186/s12909-019-1858-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang G, Zaid UB, Erickson BA, Blaschko SD, Carroll PR, Breyer BN. Urology resident publication output and its relationship to future academic achievement. J Urol . 2011;185(2):642–646. doi: 10.1016/j.juro.2010.09.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benesch MGK, Mathieson A, Pace DE. Research and surgical residency: moving beyond one-and-done projects and motivating for scholarly excellence. Can J Surg . 2022;65(4):e485–e486. doi: 10.1503/cjs.013821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doman ER, Abdo MS, Boyce DSK, Desmond DH, Roswarski JL, Hostler DC. Improvement of resident scholarship in an internal medicine training program. J Gen Intern Med . 2022;37(1):274–276. doi: 10.1007/s11606-021-06887-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harrison LM, Woods RJ, McCarthy MC, Parikh PP. Development and implementation of a sustainable research curriculum for general surgery residents: a foundation for developing a research culture. Am J Surg . 2020;220(1):105–108. doi: 10.1016/j.amjsurg.2019.09.028. [DOI] [PubMed] [Google Scholar]
- 15.Rothberg MB, Kleppel R, Friderici JL, Hinchey K. Implementing a resident research program to overcome barriers to resident research. Acad Med . 2014;89(8):1133–1139. doi: 10.1097/ACM.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 16.Robbins L, Bostrom M, Marx R, Roberts T, Sculco TP. Restructuring the orthopedic resident research curriculum to increase scholarly activity. J Grad Med Educ . 2013;5(4):646–651. doi: 10.4300/JGME-D-12-00303.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rothberg MB. Overcoming the obstacles to research during residency: what does it take. JAMA . 2012;308(21):2191–2192. doi: 10.1001/jama.2012.14587. [DOI] [PubMed] [Google Scholar]
- 18.Worly B. OB/GYN resident research curriciulum: a critical review. Curr Women Health Rev . 2017;13(2):82–88. doi: 10.2174/1573404813666170427151725. [DOI] [Google Scholar]
- 19.Oakley SH, Crisp CC, Estanol MV, Fellner AN, Kleeman SD, Pauls RN. Attitudes and compliance with research requirements in OB/GYN residencies: a national survey. Gynecol Obstet Invest . 2013;75(4):275–280. doi: 10.1159/000348562. [DOI] [PubMed] [Google Scholar]
- 20.Cain JM, Schulkin J, Parisi V, Power ML, Holzman GB, Williams S. Effects of perceptions and mentorship on pursuing a career in academic medicine in obstetrics and gynecology. Acad Med . 2001;76(6):628–634. doi: 10.1097/00001888-200106000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Stevenson MD, Smigielski EM, Naifeh MM, Abramson EL, Todd C, Li ST. Increasing scholarly activity productivity during residency: a systematic review. Acad Med . 2017;92(2):250–266. doi: 10.1097/ACM.0000000000001169. [DOI] [PubMed] [Google Scholar]
- 22.Abramson EL, Naifeh MM, Stevenson MD, et al. Research training among pediatric residency programs: a national assessment. Acad Med . 2014;89(12):1674–1680. doi: 10.1097/ACM.0000000000000404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ledford CJW, Seehusen DA, Villagran MM, Cafferty LA, Childress MA. Resident scholarship expectations and experiences: sources of uncertainty as barriers to success. J Grad Med Educ . 2013;5(4):564–569. doi: 10.4300/JGME-D-12-00280.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brubaker L, Kenton K. Clinical research education study teams: a research curriculum for obstetric and gynecology residents. Obstet Gynecol . 2011;117(6):1403–1407. doi: 10.1097/AOG.0b013e3182179705. [DOI] [PubMed] [Google Scholar]
- 25.Monn MF, Wang MH, Gilson MM, Chen B, Kern D, Gearhart SL. ACGME core competency training, mentorship, and research in surgical subspecialty fellowship programs. J Surg Educ . 2013;70(2):180–188. doi: 10.1016/j.jsurg.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Wood W, McCollum J, Kukreja P, et al. Graduate medical education scholarly activities initiatives: a systematic review and meta-analysis. BMC Med Educ . 2018;18(1):318. doi: 10.1186/s12909-018-1407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogunyemi D, Solnik MJ, Alexander C, Fong A, Azziz R. Promoting residents' professional development and academic productivity using a structured faculty mentoring program. Teach Learn Med . 2010;22(2):93–96. doi: 10.1080/10401331003656413. [DOI] [PubMed] [Google Scholar]
- 28.Guiahi M, Alston M, Metz T, Mazzoni S. Spicing up scholarly productivity: impact of a structured resident research program. Obstet Gynecol . 2019;134(suppl):40. doi: 10.1097/01.AOG.0000585436.40474.ef. [DOI] [PubMed] [Google Scholar]
- 29.Brackmann M, Reynolds RK, Uppal S, McLean K. Association of a biweekly research workgroup with enhanced resident research productivity. Obstet Gynecol . 2016;128(3):617–620. doi: 10.1097/AOG.0000000000001574. [DOI] [PubMed] [Google Scholar]
- 30.Manring MM, Panzo JA, Mayerson JL. A framework for improving resident research participation and scholarly output. J Surg Educ . 2014;71(1):8–13. doi: 10.1016/j.jsurg.2013.07.011. [DOI] [PubMed] [Google Scholar]