Abstract
Purpose:
Adolescents have limited access to sexual healthcare services, and the Emergency Department (ED) may be the only place some will seek care. We implemented an ED-based contraception counseling intervention to assess intervention feasibility, and adolescent intention to initiate contraception, contraception initiation, and follow-up visit completion.
Methods:
This prospective cohort study trained advanced practice providers in the EDs of two pediatric urban academic medical centers to deliver brief contraception counseling. A convenience sample of patients enrolled from 2019 to 2021 included females aged 15–18 not pregnant/desiring pregnancy and or using hormonal contraception/an intrauterine device. Participants completed surveys to assess demographics and intention to initiate contraception (yes/no). Sessions were audiotaped and reviewed for fidelity. We ascertained contraception initiation and follow-up visit completion via medical record review and participant survey at 8 weeks.
Results:
27 APPs were trained, and 96 adolescents were counseled/responded to surveys (mean age 16.7 years; 19% non-Hispanic White, 56% non-Hispanic Black; 18% Hispanic). Mean counseling duration was 12 minutes and >90% of reviewed sessions maintained fidelity to content/style. Most partcipants (61%) reported intention to initiate contraception, and these participants were older and more likely to report prior contraceptive use, compared to those without intention. One-third (33%) initiated contraception in the ED or after the follow-up visit.
Discussion:
Contraceptive counseling was feasible to integrate in the ED visit. Intention to initiate contraception was common and many adolescents initiated contraception. Future work should increase the pool of trained providers and supports for same-day contraception initiation for those desiring in this novel setting.
Keywords: Emergency Department, Contraception, Counseling
Unintended adolescent pregnancy is a major public health problem in the United States (US) [1, 2]. Although adolescent pregnancy rates in the US are at record lows, they remain among the highest among industrialized countries [3]. While the decline has largely been due to increased contraceptive use [4–6], the majority of adolescent pregnancies are due to lack of, inconsistent or incorrect contraceptive use [7, 8]. One approach to increase contraceptive access among adolescents is to utilize non-traditional settings, such as the Emergency Department (ED) to reach those with limited access to care [9–11]. Adolescents in the ED frequently report recent unprotected sexual intercourse as well as intention to avoid pregnancy, increasing their risk for unintended pregnancy [11–13]. Furthermore, there is growing support for providing sexual and reproductive healthcare (SRH) services in the ED [14–18]. As threats to SRH access increase, providing appropriate care in a variety of settings becomes even more crucial as we seek to protect the health and well-being of our adolescent patients [19, 20].
Therefore, the ED provides a vital potential window of opportunity to improve contraception access for adolescents who may not be reached through other clinical settings. While several studies have investigated the feasibility [21] and acceptability of providing ED-based SRH services, these have been primarily single-center studies investigating adolescent preferences for theoretical services [22–25]. Additionally, most of these studies focused on SRH services other than pregnancy prevention [26–29], thus an important gap remains regarding the optimal delivery of ED-based contraceptive counseling services to maximize patient-centered SRH.
However, providing preventive health care in the ED setting is complex due to the fast-paced nature of the environment as well as the potential for significant time constraints. Therefore, identifying an appropriate person or group of people to provide these services can be challenging. In many EDs, advanced practice providers (APPs – Nurse Practitioners and Physician Assistants) are a consistent and motivated part of the workforce, caring for patients primarily and/or under the supervision of an attending physician. These providers commonly staff the ED for 16 hours per day, and at times 24 hours per day, depending on the setting. Given their educational background and the fact that APPs generally face fewer time constraints or competing demands than their emergency medicine physician colleagues, we felt this group held great potential to train for a contraception counseling program.
The primary objective of this study was to assess intention to initiate contraception among adolescents who received contraceptive counseling from a trained ED APP. Additional objectives included assessing feasibility and acceptability of the counseling intervention, completion of a contraception-related referral visit and initiation of contraception within 8 weeks of the ED visit.
Methods
We conducted a prospective cohort study of female (biologically) patients ages 15–18 years old (inclusive) presenting to the ED of two urban, free-standing pediatric hospitals in geographically distinct regions of the US, with up to 170,000 visits annually (combined; 100K at site 1, 70K at site 2). At least one APP is typically working in each ED between 7am and midnight, with up to six APPs working in various teams at a given time, depending on scheduling algorithms and patient volume. At both sites, APPs provide care independently to less acutely ill patients and provide care under the supervision of attending physicians for more complex or seriously ill or injured patients. The study protocol was approved by the lead site’s Institutional Review Board, with a cooperative agreement with the second site. A Data Safety Monitoring Board (DSMB) was convened, comprised of experts in adolescent SRH not affiliated with this project or the involved institutions. The DSMB met on an ad hoc basis to monitor participant safety and study progress.
Participants
Advanced Practice Providers were eligible to train to deliver contraceptive counseling if they worked in the ED for at least 6 months, with no exclusion criteria. APPs were recruited through email and word of mouth and provided informed consent for participation during counseling training. We used an “opt-in” strategy for recruiting APPs at both sites.
Adolescent participants were eligible for inclusion if they were females (biologically) between the ages of 15 and 18 years (inclusive); if they were noted to be at risk of unintended pregnancy (defined as reporting heterosexual sex within the last 6 months or likely future sexual activity, did not desire pregnancy (as determined through routine care by either the ED clinician or the study APP), were not currently using hormonal contraception/copper intrauterine device); and were proficient in reading and speaking English. Participants were excluded if they were pregnant; presented after a sexual assault; had a developmental delay limiting participation; or were deemed too ill to participate by the treating team.
Adolescent recruitment occurred through two approaches. First, APPs identified potentially eligible adolescents through regular ED patient care and contacted the research team for further eligibility assessment and consent procedures. Second, trained research assistants (RAs) identified potentially eligible adolescents using computerized ED tracking boards, which log patient visit information in real time, and the electronic medical record (EMR), when trained APPs were working in the ED; in these cases, the RA approached the provider caring for the adolescent to confirm that a confidential history had been obtained that included a sexual history. Once a potential subject was identified, an RA confirmed whether the patient met inclusion criteria; if the adolescent was interested in participating and an APP was available to counsel, the RA obtained written consent or assent and HIPAA authorization. Subjects who were 18 years old provided consent and HIPAA authorization for their own participation. For minors, a waiver of parental permission and waiver of HIPAA authorization were granted, and the minor provided assent for her own participation. Participants were given the option of having their parent or legal guardian involved in the consent process, if desired. If a participating minor’s caregiver was present in the ED, we followed our established practice to share a general overview of the study with the adolescent while the parent was in the room. Then we asked to speak alone with the adolescent so they could decide if they wanted to participate and if they wanted their caregiver involved. If we were unable to speak privately with the adolescent, they were not enrolled in the study. In addition, caregivers could choose to opt the adolescent out of the study prior to assent procedures. All counseling sessions took place in private unless the participant explicitly requested that a parent be present. Participants received $20 for the initial ED visit and $20 for completing the 8-week follow-up survey.
Counseling Intervention
We created a counseling intervention to incorporate evidence-based contraceptive care into the pediatric ED setting [30, 31] (Expanding Contraception Access for Teens, eCAT) by convening a group of pediatric emergency medicine physicians and adolescent SRH experts from the two study sites and one additional site. This group developed training learning objectives, based on contraceptive counseling interventions successfully utilized in other settings [32, 33]. Details about the training are published separately [34]. In summary, the counseling focused on a tiered-effectiveness approach to patient-centered contraceptive services and aimed to assess participants’ knowledge and preferences about methods, personal motivations, and environmental factors affecting contraceptive choice. The counseling included an overview of contraception options and counseling best practices [35–40], and utilized Jaccard’s framework for understanding contraceptive choices [18].
Counseling Training and Implementation
As mentioned above, a detailed description of the training is published elsewhere [34]. In brief, experts in adolescent SRH at each site trained APPs to employ a patient-centered approach that included a semi-structured clinical interview to determine factors influencing contraceptive choice, and review contraceptive options, and their risks and benefits. Interviews used open-ended questions and reflective listening to enhance focus on patient preferences and autonomy.
The training consisted of two 4-hour units: a self-paced webinar and an in-person interactive session. The webinar covered understanding adolescent pregnancy and the ED as the intervention site; the psychology of contraceptive choices; contraceptive options, including indications, contraindications, and side effects; and patient-centered counseling techniques, including teach-back methods. The in-person session reviewed study objectives and logistics, components of high-quality counseling, and included mock counseling scenarios with APPs as patients and adolescent medicine expert physicians providing feedback. APPs were paid their hourly rate for the training time. Weekly study-team emails were sent including a “Tip of the Week” enabling ongoing education and reinforcing key training components, and several optional drop-in question and answer sessions occurred throughout the study. Finally, a resource manual including information about contraceptive options, a counseling roadmap, and other pertinent information was available for APP use in real time. These materials allowed the APPs to use visual aids in addition to verbally sharing information about contraception and were publicly available [35, 36].
As part of counseling, all interested adolescents were referred to an appropriate site (based on patient preference) for additional counseling, contraception initiation, or follow-up on contraceptive initiation, as applicable. APPs were trained in prescribing contraceptive medications and were able to incorporate prescribing when aligned with patient preference and within the individual APP’s comfort in prescribing. In these cases, those interested in starting contraception during the visit (oral pills, patch, vaginal ring [both sites], or hormonal injection [one site only]) received the medication or a prescription before their ED visit was completed.
Data Collection
Prior to counseling, participants completed a brief questionnaire to ascertain demographic information, sexual and contraception history (Appendices A–B). Reporting race and ethnicity in this study was mandated by the US National Institutes of Health, consistent with the Inclusion of Women, Minorities, and Children policy. Race and ethnicity were based on the participants’ report. Trained APPs then provided the confidential counseling session. Intention to initiate contraception was assessed through a post-counseling survey question, “are you interested in starting a type of birth control; yes/no” (Appendix C). Those answering “yes” were categorized as having “high intention” to initiate contraception. To assess acceptability, after counseling participants responded to a 4-question survey about their learning about side effects, satisfaction with counseling, and understanding of information using 5-point Likert-scale (Appendix D). Each response was dichotomized by grouping strongly disagree/disagree/neutral vs. agree/strongly agree, and we dichotomized each participant into “agree with 0–3 items” v. “agree with all 4 items.” The APP providing counseling also completed a brief questionnaire including questions about counseling ease and timing (Appendix E).
To assess completion of a contraception-related referral visit and the proportion who ultimately initiated contraception within 8 weeks, all participants were contacted by text message 8 weeks after the ED visit to complete a follow-up survey. If the participant did not respond, up to three follow-up texts/phone calls were attempted. In addition, we reviewed the EMR to determine contraception prescription or administration at the index visit and/or for participants seen for follow-up at hospital-affiliated clinics. Data obtained from survey or EMR review were included in outcome measurement. All consent forms, data collection and text messaging were managed through the Research Electronic Data Capture (REDCap, ©Vanderbilt University).
All counseling sessions were audiotaped to allow for monitoring for fidelity to intervention content, as one measure of feasibility. After each APP’s first counseling session, a study team member with expertise in adolescent health reviewed the audiotape using a 17-item standardized assessment form, based on methods utilized in the CHOICE project [32, 33]. The assessment included items such as using open-ended questions, explaining the limits of confidentiality, using a tiered-effectiveness approach to contraception choice, providing medically accurate information, and utilizing teach-back (Appendix F). The APP received constructive feedback and needed to demonstrate fidelity to the counseling prior to performing additional counseling. A second counseling session by an APP was reviewed if the feedback from the first session indicated this was necessary. During the study period, a convenience sample of additional recorded sessions was reviewed to assess ongoing fidelity to counseling procedures, with the goal of reviewing one half of the sessions. As part of the sampling strategy, we aimed to review additional sessions from the full cohort of participating APPs.
Data Analysis
The primary outcome was the reported intention to initiate contraception. Additionally, feasibility was assessed by measuring counseling session duration and assessing fidelity to the counseling principles; acceptability was assessed through analysis of both the adolescent acceptability and APP feasibility surveys (questions about ease of delivery and time to deliver). Additional outcomes included the completing a contraception related referral visit and contraception initiation as assessed through EMR review and/or follow-up survey data.
Baseline and demographic characteristics were summarized by standard descriptive summaries. Participant demographics and behaviors were compared between those intending and not intending to initiate contraception using chi-square test and t-test. We used univariate logistic regression models first to identify associated behaviors with the intention to initiate contraception. Due to multicollinearity and clinical relevance, we then conducted bivariate logistic regression analyses after adjusting for participant race and age. We conducted all statistical analyses using Stata version 16 (StataCorp, College Station, TX).
Results
Participant Demographics
A total of 159 eligible adolescents were approached for enrollment from November 2019 until February 2021, with a brief pause in enrollment due to the onset of the COVID 19 pandemic; of these, 108 consented to participate (Figure 1). None refused to participate specifically because of the audiotaping of the session. Nine were withdrawn from the study due to ineligibility or inability to provide counseling, leaving 99 total participants (54 at site 1, 45 at site 2). Of these, 29 included their parent or caregiver in the counseling session. A total of 96/99 participants responded to the primary outcome question and comprised our final sample. Demographic data and sexual history information are noted in Table 1. Across the two sites, 44 APPs were eligible for inclusion at the start of the study (24 at site 1, 20 at site 2); of these, we trained 27 (16 at site 1, 11 at site 2).
Figure 1.
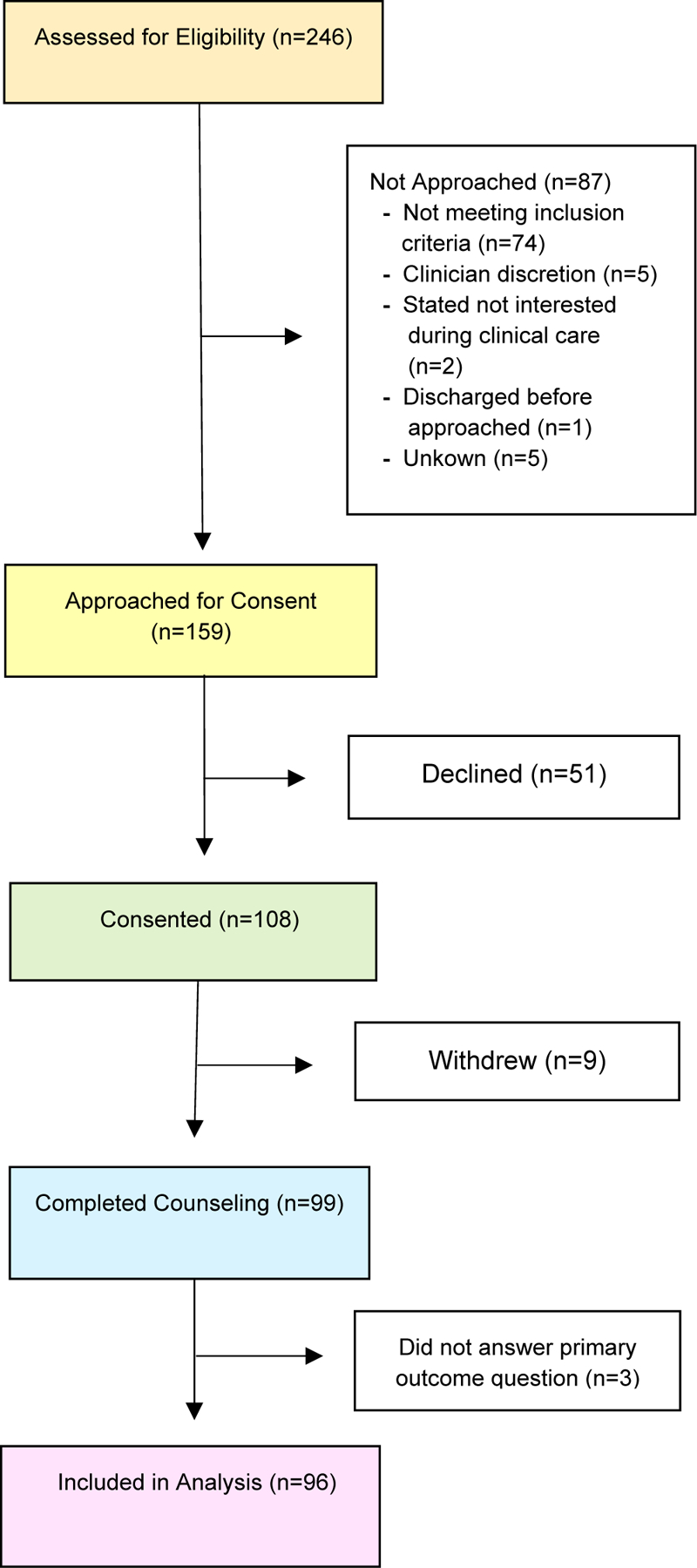
Screening Consort Flow Diagram
Table 1.
Participant Demographics (n=96)
| Characteristic | N (%) |
|---|---|
| Age in years, Mean (SD) | 16.7 (1.0) |
| Race/ethnicity, % | |
| Non-Hispanic white | 18 (19) |
| Non-Hispanic black | 54 (56) |
| Hispanic | 17 (18) |
| Non-Hispanic other/mixed | 6 (6) |
| No response | 1 (1) |
| Education, % | |
| Completed high school | 22 (23) |
| Not completed high school | 73 (76) |
| No response | 1 (1) |
| History of pregnancy, % | |
| No | 83 (87) |
| Yes | 3 (3) |
| No response | 10 (10) |
| Number of sex partners, % | |
| 0 | 17 (18) |
| 1 | 22 (23) |
| 2+ | 50 (52) |
| No response | 7 (7) |
| Previous emergency contraception use, % | |
| No | 78 (81) |
| Yes | 18 (19) |
| Previous birth control usea, % | |
| Never | 26 (27) |
| Ever | 70 (73) |
Included birth control pills, condom, injection, contraceptive patch and contraceptive ring.
Counseling Feasibility
Of the providers who were trained, 14 providers at site 1 and nine providers at site 2 conducted one or more sessions during the study period. The mean number of counseling sessions per individual provider was four at site 1 (range 0–6) and five at site 2 (range 0–10), and counseling lasted a mean of 12 minutes (range 5 to 29 minutes).
The audiotapes of 50 sessions (52%) were reviewed for fidelity to counseling content and style. Nearly all reviewed sessions included an overview of the risks, benefits and side effects profiles of the various contraceptive methods (98%, n=49). Further, most sessions were noted to include a tiered-effectiveness approach to prioritize the most effective methods (92%, n=46); nearly all APPs asked open-ended questions (96%, n=48); and most used teach-back methods (76%, n=38) in their counseling. APPs discussed confidentiality (96%, n=48) and personal goals of the adolescent (96%, n=48), and also used shared decision-making to establish a contraceptive plan (92%, n=46).
Intention, follow-up and contraception initiation
Most of the participants (59/96, 61%) reported intention to initiate contraception (“high intention”). Compared with those not reporting intention to initiate contraception (“low intention”), those with high intention were slightly older (16.9 years v. 16.4 years), reported 2 or more sex partners, and were more likely to report prior birth control use. A total of 32 participants (33%) initiated contraception either during the ED or follow-up visit, including two who reported no prior sexual activity. Five received an injectable hormonal contraceptive and 11 were provided prescriptions for oral contraceptives during their ED visit. Thirty-five participants (36%) completed a contraception-related referral visit within 8 weeks of their ED visit. Forty-five additional participants completed the follow-up survey or were reached by phone for follow-up; sixteen were not reached and were grouped in the “no follow-up visit” category. Participants who indicated high intention to start contraception were significantly more likely to initiate contraception and complete a contraception-related referral visit (Table 2).
Table 2.
Association of Intention to Initiate Contraception with Participant Demographics, Referral Completion, and Contraceptive Initiation Characteristic
| Low Intention (N=37) N (%) | High Intention(N=59) N (%) | P-value | |
|---|---|---|---|
| Age in years, Mean (SD) | 16.4 (1.0) | 16.9 (1.0) | 0.03 |
| Race/ethnicity | 0.10 | ||
| Hispanic | 11 (65) | 6 (35) | |
| Non-Hispanic black | 16 (30) | 38 (70) | |
| Non-Hispanic other/mixed | 3 (50) | 3 (50) | |
| Non-Hispanic white | 7 (39) | 11 (61) | |
| No response | 0 (0) | 1 (100) | |
| Education | 0.14 | ||
| Completed high school | 5 (23) | 17 (77) | |
| Not completed high school | 32 (44) | 41 (56) | |
| No response | 0 (0) | 1 (100) | |
| History of pregnancy | 0.09 | ||
| No | 29 (35) | 54 (65) | |
| Yes | 1 (33) | 2 (67) | |
| No response | 7 (70) | 3 (30) | |
| Number of sex partners | 0.002 | ||
| 0 | 10 (59) | 7 (41) | |
| 1 | 13 (59) | 9 (41) | |
| 2+ | 10 (20) | 40 (80) | |
| No response | 4 (51) | 3 (43) | |
| Previous emergency contraception use | 0.11 | ||
| No | 33 (42) | 45 (58) | |
| Yes | 4 (22) | 14 (78) | |
| Previous birth control usea, | 0.004 | ||
| None | 16 (62) | 10 (38) | |
| Yes, any type | 21 (30) | 49 (70) | |
| Contraception initiated or prescribed at ED or referral visit, | 0.004 | ||
| No | 31 (48) | 33 (52) | |
| Yes | 6 (19) | 26 (81) | |
| Completed a contraceptive referral visit by 8 weeks after counseling | 0.004 | ||
| Not completed | 30 (49) | 31 (51) | |
| Completed | 7 (20) | 28 (80) |
T-test and chi-square tests. Row percent was presented.
Included birth control pills, condom, injection, contraceptive patch and contraceptive ring.
After adjusting for race and age, adolescents had a higher odds of high intention to initiate contraception if they reported two or more sex partners (OR 4.3, 95% CI 1.1, 16.5); had previously used birth control (OR 3.9, 95% CI 1.3–11.3); and agreed to all four items on the counseling acceptability survey (OR 4.2, 95% CI 1.2–14.4). The odds of completing a contraception-referral visit were increased only in the group reporting intention to initiate contraception (OR 3.9, 95% CI 1.4–11.3). Finally, the odds of intention were not impacted by report of prior emergency contraception use. Reporting high intention was the only factor associated with increased odds of initiating contraception (OR 4.5, 95% CI 1.5–3.7) (Table 3).
Table 3.
Associated Factors in the Odds of Initial Intention, Completion of a Contraception Related Visit and Contraception Initiation (n=96)
| OR (95% CI) | |||
|---|---|---|---|
| Characteristic | High intention to initiate contraception | Contraception-referral visit | Contraception initiation |
| Number of sex partners | |||
| 0 (reference) | |||
| 1 | 0.7 (0.2–3.0) | 0.8 (0.2–3.3) | 0.7 (0.2–3.1) |
| 2+ | 4.3 (1.1–16.5) | 2.5 (0.7–9.4) | 1.9 (0.5–7.4) |
| Previous emergency contraception use | |||
| No (reference) | |||
| Yes | 3.5 (0.7–18.2) | 0.7 (0.2–2.4) | 0.6 (0.2–2.3) |
| Previous birth control usea | |||
| Never (reference) | |||
| Ever | 3.9 (1.3–11.3) | 2.6 (0.8–7.8) | 2.0 (0.7–6.0) |
| Patient acceptability | |||
| Agree to 0–3 items (reference) | |||
| Agree to 4 items | 4.2 (1.2–14.4) | 2.7 (0.7–10.6) | 2.5 (0.6–9.6) |
| Intention to initiate contraceptive | |||
| Low (reference) | |||
| High | - | 3.9 (1.4–11.3) | 4.5 (1.5–13.7) |
Bivariate logistic regression model after adjusting for race and age and excluding no responses.
Included birth control pills, condom, injection, contraceptive patch and contraceptive ring.
Counseling Acceptability
APPs reported that counseling was easy to deliver (n=24; 90%) and they had sufficient time (n=23; 85%) to provide the counseling. Most adolescents (n=89; 90%) reported satisfaction with the counseling session. While responses to the individual acceptability questions did not differ between high and low intention groups, adolescents in the high intention group were significantly more likely to respond positively to all four items on the acceptability survey (Table 4).
Table 4.
Comparing the Level of Counseling Acceptance by Intention to Initiate Contraception (n=96)
| Total N | Low intention (N=37) | High intention (N =59) | P-value | |
|---|---|---|---|---|
| Learned about side effects, % | 0.16 | |||
| Neutral/disagree | 7 | 71 | 29 | |
| Agree | 87 | 36 | 64 | |
| No response | 2 | 50 | 50 | |
| Would recommend birth control, % | 0.06 | |||
| Neutral/disagree | 6 | 83 | 17 | |
| Agree | 88 | 35 | 65 | |
| No response | 2 | 50 | 50 | |
| Was satisfied with the counseling, % | 0.13 | |||
| Neutral/disagree | 5 | 80 | 20 | |
| Agree | 89 | 36 | 64 | |
| No response | 2 | 50 | 50 | |
| Found the information easy to understand, % | 0.50 | |||
| Neutral/disagree | 9 | 55.6 | 44 | |
| Agree | 85 | 37 | 64 | |
| No response | 2 | 50 | 50 | |
| Overall acceptability, % | 0.04 | |||
| Agree to 0–3 items of above | 15 | 67 | 33 | |
| Agree to 4 items of above | 79 | 33 | 67 | |
| No response | 2 | 50 | 50 |
Chi-square tests
Discussion
Our ED-based study assessed the intention to initiate contraception among adolescents who received contraceptive counseling from a trained ED provider. A majority of counseled adolescents expressed intention to initiate contraception after the session. In addition, we demonstrated the feasibility of training APPs in contraceptive counseling, with a focus on patient-centered care, confidentiality, and a tiered-effectiveness approach to contraceptive counseling based on recommended best practices at the time of the study [37–41]. Once trained, the APPs were able to implement the counseling during the ED visit for interested adolescents in a succinct manner, typically requiring only 10–15 minutes of time. APPs were trained to identify appropriate patients during their shifts, without constraints limited to specific chief complaints, allowing for a broad reach of the intervention.
Of note, while the participants with the highest risk of pregnancy (those who were sexually active with more than one partner and those with a prior use of hormonal contraception) were the most likely to express interest in initiating contraception, almost one-fifth of study adolescents reported they were not yet sexually active. This finding is critical when designing interventions to improve reproductive health outcomes among adolescents. Future studies should include adolescents before they report being sexually active to maximize the intervention’s impact, which aligns with the American College of Obstetrics and Gynecology recommendation [31] that “contraceptive counseling conversations should take place before [adolescents] are sexually active.”
Perhaps unsurprisingly, most participants did not complete a follow-up visit even though the majority of adolescents expressed intention to initiate contraception after the counseling. Similar results were reported from a recent intervention to improve access to long-acting reversible contraceptives for adolescents in the ED [42]. Side effects and safety concerns, uncertainty about the future / pregnancy desire, ambivalence, peer and family influences, contraception experience, and method knowledge, myths and misinformation have been identified as barriers to contraception use among adolescents and young women [43–47]. While our counseling intervention was designed to mitigate many of these concerns, there is opportunity to further refine the content to improve follow-up visit rates. Additionally, our findings suggest that incorporating a same-day start for contraception or contraceptive referral options for patients may improve contraception initiation rates; however a “one size fits all” approach is not likely to be successful in the ED setting. More work is needed to continue to understand the barriers to contraceptive initiation to allow for intervention tailoring.
The strengths of our project include designing and implementing a counseling strategy that was grounded by theory and based on already-studied interventions adapted to the ED setting [22–25]. In addition, our study builds on prior work by including more than one site, which provided important geographic diversity, and including the intervention as part of routine clinical care, allowing for the potential to scale up the intervention at our own sites as well as in other EDs. Another strength of our study was the robust plan to ensure fidelity to the counseling principles and content. Finally, while many of our trained APPs had no prior experience with contraceptive counseling, we found high acceptability of the intervention as well as fidelity to the counseling among the trained group.
There are several limitations to this study. First, both study sites are academic centers in urban settings, potentially limiting generalizability. Future studies should implement a similar intervention in other settings, such as rural or suburban areas, to see if this approach produces a similar result. Future studies could employ our intervention with different types of providers, such as registered nurses, or physicians in training. Additionally, the training was time-intensive, and because counseling encounters were rare for an individual provider, we provided ongoing support; the time needed to ensure comfort and competency with the counseling could inhibit implementation in other settings. Despite this concern, we believe this training can be reproduced elsewhere given that much of the training was online and the remainder could be completed during regularly scheduled educational sessions. The APPs reported feeling comfortable with the counseling [34] and frequently used point-of-care materials such as the resource binder and counseling roadmap. While the mean time of counseling was only 12 minutes, this time could impact patient flow through the ED and there is the potential that the number of patients seen by an APP on a given shift could decrease. Given that counseling can occur while patients are waiting for test results or other reassessments, and that only one or two patients per shift would be appropriate for counseling, we believe the impact on these metrics is likely minimal or negligible. Furthermore, the number of patients presenting for care during the study period varied considerably, from very many to very few, due to the COVID-19 pandemic. It is possible that our enrollment and counseling implementation was affected by this variation, although we did not match counseling data to daily ED census data.
Next, there were some participants that were not reached for follow-up data collection who may have sought care outside of our health systems. However, we expect that this would be a rare occurrence for adolescents in our communities, as comprehensive reproductive care opportunities for adolescents are limited. Additionally, contraception counseling best practice has recently moved away from using a tiered-effectiveness approach in favor of approaches that focus on individual values, experience, and needs [48–50]. Counseling approaches that consider individual perspective and adolescent needs during counseling may help reduce barriers to contraception use [48–52]. The counseling should be revised to reflect this shift. Lastly, this study took place during the COVID-19 pandemic which presented challenges in recruitment and data collection. However, pandemic-related changes in care could address some of these challenges, such as leveraging telehealth platforms to provide counseling services in the ED setting. Future studies may explore how best to use technology/media to improve our existing counseling intervention [42,53]
Conclusion
This is one of the first studies to assess contraception counseling and initiation among adolescents in the ED. We found that training providers is feasible, increases access to care and can facilitate contraception initiation for interested adolescents. Our training was developed using evidence-based, theory-driven principles specifically tailored to adolescents in the ED. Adolescents found counseling to be a useful adjunct to the ED visit, and many reported intention to initiate contraception after counseling. Future work should focus on increasing the pool of trained counseling providers, as well as on considering same-day initiation of contraception, when appropriate.
Supplementary Material
Implications and contributions:
Increased access to contraceptive services for adolescents is needed to improve adolescent health. This study shows that it is feasible to train Advanced Practice Providers to deliver brief contraception counseling to adolescents during the Emergency Department visit. Intention to initiate contraception was common and one third of adolescents initiated contraception.
Acknowledgements:
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (NIH) under award number R21HD095096. The NIH had no role in the study design/implementation.
Conflicts of interest/financial disclosures:
Dr. Melissa K. Miller received funds from Organon to support some of her research. No other authors have any other conflicts of interest or financial disclosures to report.
We would like to thank the participating APPs for their time and hard work dedicated to this study. Additionally, we would like to thank Dr. Laurel Gabler for her significant contribution to developing the training curriculum for providers. Dr. Cynthia Mollen attests that all persons that have contributed substantively to this manuscript have been acknowledged.
Abbreviations:
- US
United States
- ED
Emergency Department
- SRH
Sexual and Reproductive Healthcare
- DSMB
Data Safety Monitoring Board
- APP
Advanced Practice Provider
- RA
Research Assistant
- EMR
Electronic Medical Record
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This work was presented at the 2021 Pediatric Academic Society annual conference and the 2022 American Academy of Pediatrics annual conference.
Clinical trial registration: An Emergency Department-Based Study to Reduce Adolescent Pregnancy, NCT04120376
Contributor Information
Cynthia Mollen, Division of Emergency Medicine, Children’s Hospital of Philadelphia (CHOP); Perelman School of Medicine at the University of Pennsylvania; Department of Pediatrics Department of Emergency Medicine, 3501 Civic Center Boulevard, Philadelphia, PA 19104, United States of America (USA).
Tara Ketterer, PolicyLab, CHOP Roberts Center for Pediatric Research, 2716 South Street, 10th Floor, Philadelphia, PA 19146, USA;.
Jungwon Min, Department of Biomedical and Health Informatics, CHOP Roberts Center for Pediatric Research, 2716 South Street, 15th Floor, Philadelphia, PA 19146, USA.
Romina L. Barral, Division of Adolescent Medicine, Children’s Mercy Hospital (CMH); University of Missouri-Kansas City School of Medicine; University of Kansas School of Medicine Division of Adolescent Medicine, Children’s Mercy at the University of Kansas Hospital, 2000 Olathe Boulevard, Kansas City, KS 66103, USA.
Aletha Akers, Division of Adolescent Medicine, CHOPI Division of Adolescent Medicine, Specialty Care Center, 3550 Market Street, Philadelphia, PA 19104, USA.
Amber Adams, Department of Emergency Medicine, CMH Department of Emergency Medicine, Children’s Mercy Adele Hall Campus, 2401 Gillham Road, Kansas City, MO 64108, USA.
Elizabeth Miller, Division of Adolescent and Young Adult Medicine, University of Pittsburgh Medical Center Children’s Hospital of Pittsburgh; Public Health and Clinical and Translational Science, University of Pittsburgh School of Medicine University Center, Suite 302.2, 120 Lytton Avenue, Pittsburgh, PA 15213, USA.
Melissa K. Miller, Department of Emergency Medicine, CMH; University of Missouri-Kansas City School of Medicine; University of Kansas School of Medicine Department of Emergency Medicine, Children’s Mercy Adele Hall Campus, 2401 Gillham Road Kansas City, MO 64108, USA.
References
- [1].Hoffman SD, Maynard RA. Kids having kids: Economic costs & social consequences of teen pregnancy. The Urban Insitute; 2008. [Google Scholar]
- [2].Guttmacher Institute. Unintended pregnancy in the United States. Fact sheet; August 2019. Available at: https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states. Accessed January 18, 2022.
- [3].Sedgh G, Finer LB, Bankole A et al. Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. J Adolesc Health. 2015;56(2):223–230. doi: 10.1016/j.jadohealth.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lindberg LD, Firestein L, Beavin C. Trends in U.S. adolescent sexual behavior and contraceptive use, 2006–2019. Contracept X. 2021;3:100064. doi: 10.1016/j.conx.2021.100064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Congressional Research Service. Teen birth trends. In brief. R45184. Updated May 13, 2020. 1–10 https://crsreports.congress.gov [Google Scholar]
- [6].Sonfield A, Hasstedt K, Gold RB. Moving Forward: Family Planning in the Era of Health Reform, New York: Guttmacher Institute, 2014. Available at: https://www.guttmacher.org/report/moving-forward-family-planning-era-health-reform. Accessed March 1, 2022. [Google Scholar]
- [7].Frost JJ, Darroch JE, Remez L. Improving contraceptive use in the United States. In brief. Vol 1. New York: Guttmacher Institute; 2008. [PubMed] [Google Scholar]
- [8].Santelli JS, Morrow B, Anderson JE, Lindberg LD. Contraceptive use and pregnancy risk among U.S. high school students, 1991–2003. Perspect Sex Reprod Health. 2006;38(2):106–111. doi: 10.1363/psrh.38.106.06 [DOI] [PubMed] [Google Scholar]
- [9].Solomon M, Badolato GM, Chernick LS et al. Examining the role of the pediatric emergency department in reducing unintended adolescent pregnancy. J Pediatr. 2017;189:196–200. doi: 10.1016/j.jpeds.2017.06.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Fine LC, Mollen CJ. A pilot study to assess candidacy for emergency contraception and interest in sexual health education in a pediatric emergency department population. Pediatr Emerg Care. 2010;26(6):413–416. doi: 10.1097/PEC.0b013e3181e0578f [DOI] [PubMed] [Google Scholar]
- [11].Zuckerman B, Nathan S, Mate K. Preventing unintended pregnancy: a pediatric opportunity. Pediatrics. 2014;133(2):181–183. doi: 10.1542/peds.2013-1147 [DOI] [PubMed] [Google Scholar]
- [12].Miller MK, Pickett M, Leisner K et al. Sexual health behaviors, preferences for care, and use of health services among adolescents in pediatric emergency departments. Pediatr Emerg Care. 2013;29(8):907–911. doi: 10.1097/PEC.0b013e31829ec244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chernick L, Kharbanda EO, Santelli J, Dayan P. Identifying adolescent females at high risk of pregnancy in a pediatric emergency department. J Adolesc Health. 2012;51(2):171–178. doi: 10.1016/j.jadohealth.2011.11.023 [DOI] [PubMed] [Google Scholar]
- [14].Walton MA, Resko S, Whiteside L et al. Sexual risk behaviors among teens at an urban emergency department: relationship with violent behaviors and substance use. J Adolesc Health. 2011;48(3):303–305. doi: 10.1016/j.jadohealth.2010.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hoehn EF, Hoefgen H, Chernick LS et al. A pediatric emergency department intervention to increase contraception initiation among adolescents. Acad Emerg Med. 2019;26(7):761–769. doi: 10.1111/acem.13565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bernstein SL, D’Onofrio G. Public health in the emergency department: Academic emergency medicine consensus conference executive summary. Acad Emerg Med. 2009;16(11):1037–1039. doi: 10.1111/j.1553-2712.2009.00548.x [DOI] [PubMed] [Google Scholar]
- [17].Gordon JA, Billings J, Asplin BR, Rhodes KV. Safety net research in emergency medicine: proceedings of the academic emergency medicine consensus conference on “The Unraveling Safety Net”. Acad Emerg Med. 2001;8(11):1024–1029. doi: 10.1111/j.1553-2712.2001.tb01110.x [DOI] [PubMed] [Google Scholar]
- [18].Jaccard J, Levitz N. Counseling adolescents about contraception: towards the development of an evidence-based protocol for contraceptive counselors. J Adolesc Health. 2013;52(4 Suppl):S6–S13. doi: 10.1016/j.jadohealth.2013.01.018 [DOI] [PubMed] [Google Scholar]
- [19].Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV and STD racial disparities: the need for new directions. Am J Public Health. 2007;97(1):125–132. doi: 10.2105/AJPH.2005.075747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Krass P, Tam V, Min J, et al. Adolescent access to federally funded clinics providing confidential family planning following changes to Title X funding regulations. JAMA Netw Open. 2022;5(6):e2217488. Published 2022 Jun 1. doi: 10.1001/jamanetworkopen.2022.17488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Miller MK, Champassak S, Goggin K, et al. A brief intervention to reduce adolescent sexual risk behaviors: feasibility and impact. J Adolesc Health. 2014;54(2S):S11. [Google Scholar]
- [22].Mollen CJ, Miller MK, Hayes KL, et al. Developing emergency department-based education about emergency contraception: adolescent preferences. Acad Emerg Med. 2013;20(11):1164–1170. doi: 10.1111/acem.12243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Miller MK, Hornberger L, Sherman AK, Dowd MD. Acceptability of sexual health discussion and testing in the pediatric acute care setting. Pediatr Emerg Care. 2013;29(5):592–597. doi: 10.1097/PEC.0b013e31828e646f [DOI] [PubMed] [Google Scholar]
- [24].Suffoletto B, Akers A, McGinnis KA, et al. A sex risk reduction text-message program for young adult females discharged from the emergency department. J Adolesc Health. 2013;53(3):387–393. doi: 10.1016/j.jadohealth.2013.04.006 [DOI] [PubMed] [Google Scholar]
- [25].Mollen CJ, Miller MK, Hayes KL, Barg FK. Knowledge, attitudes, and beliefs about emergency contraception: a survey of female adolescents seeking care in the emergency department. Pediatr Emerg Care. 2013;29(4):469–474. doi: 10.1097/PEC.0b013e31828a3249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Mehta SD, Hall J, Lyss SB, et al. Adult and pediatric emergency department sexually transmitted disease and HIV screening: programmatic overview and outcomes. Acad Emerg Med. 2007;14(3):250–258. doi: 10.1197/j.aem.2006.10.106 [DOI] [PubMed] [Google Scholar]
- [27].Silva A, Glick NR, Lyss SB, et al. Implementing an HIV and sexually transmitted disease screening program in an emergency department. Ann Emerg Med. 2007;49(5):564–572. doi: 10.1016/j.annemergmed.2006.09.028 [DOI] [PubMed] [Google Scholar]
- [28].Trent M, Chung SE, Burke M, et al. Results of a randomized controlled trial of a brief behavioral intervention for pelvic inflammatory disease in adolescents. J Pediatr Adolesc Gynecol. 2010;23(2):96–101. doi: 10.1016/j.jpag.2009.06.005 [DOI] [PubMed] [Google Scholar]
- [29].Goyal MK, Teach SJ, Badolato GM, et al. Universal screening for sexually transmitted infections among asymptomatic adolescents in an urban emergency department: high acceptance but low prevalence of infection. J Pediatr. 2016;171:128–132. doi: 10.1016/j.jpeds.2016.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gutman CK, Dorfman D, Meese H, et al. Identifying a golden opportunity: adolescent interest in contraceptive initiation in a pediatric emergency department. J Womens Health (Larchmt). 2020;29(5):622–626. doi: 10.1089/jwh.2019.7821 [DOI] [PubMed] [Google Scholar]
- [31].Committee opinion no. 710: Counseling adolescents about contraception. Obstet Gynecol. 2017;130(2):486–487. doi: 10.1097/AOG.0000000000002228 [DOI] [PubMed] [Google Scholar]
- [32].Madden T, Mullersman JL, Omvig KJ, et al. Structured contraceptive counseling provided by the contraceptive CHOICE project. Contraception. 2013;88(2):243–249. doi: 10.1016/j.contraception.2012.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Birgisson NE, Zhao Q, Secura GM et al. Preventing unintended pregnancy: the contraceptive CHOICE project in review. J Womens Health (Larchmt). 2015;24(5):349–353. doi: 10.1089/jwh.2015.5191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Gabler LS, Shankar M, Ketterer T, et al. Contraceptive counseling for adolescents in the emergency department: A novel curriculum for nurse practitioners and physician assistants. J Am Assoc Nurse Pract. 2023. Feb 2. doi: 10.1097/JXX.0000000000000824. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Reproductive Health Access Project. Your birth control choices fact sheet. Updated October 7th 2022. Available at: https://www.reproductiveaccess.org/resource/bc-fact-sheet/https://www.reproductiveaccess.org/resource/bc-fact-sheet/ Accessed February 7, 2023.
- [36].Bedsider.org and Bixby Center for Global Reproductive Health. How well does birth control work. Available at: https://beyondthepill.ucsf.edu/sites/beyondthepill.ucsf.edu/files/Tiers%20of%20Effectiveness_English-043019.pdf.https://beyondthepill.ucsf.edu/sites/beyondthepill.ucsf.edu/files/Tiers%20of%20Effectiveness_English-043019.pdf. Accessed February 7, 2023.
- [37].World Health Organization (WHO) Department of Reproductive Health and Research; Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs (CCP) Knowledge for health project. Family planning: a global handbook for providers (2011 update). Baltimore, Md., and Geneva, Switzerland; 2011. [Google Scholar]
- [38].Reproductive Health Access Project. Contraception. Available at: www.reproductiveaccess.org/contraception/. Accessed June 9, 2019.
- [39].Principles for providing quality counseling. Family Planning National Training Center. Presented at: National Family Planning and Reproductive Health Association national conference; April 27, 2015. Accessed June 26, 2019. [Google Scholar]
- [40].Reproductive Health National Training Center. Training packages. Available at: rhntc.org/training-packages. Accessed June 27, 2019.
- [41].Jaccard J Unlocking the contraception conundrum: reducing unplanned pregnancies in emerging adulthood. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy, 2009. Accessed June 2, 2019. [Google Scholar]
- [42].Vayngortin T, Bachrach L, Patel S, Tebb K. Adolescents’ acceptance of long-acting reversible contraception after an educational intervention in the emergency department: a randomized controlled trial. West J Emerg Med. 2020;21(3):640–646. doi: 10.5811/westjem.2020.2.45433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Claringbold L, Sanci L, Temple-Smith M. Factors influencing young women’s contraceptive choices. Aust J Gen Pract. 2019;48(6):389–394. doi: 10.31128/AJGP-09-18-4710 [DOI] [PubMed] [Google Scholar]
- [44].Chernick LS, Schnall R, Higgins T, et al. Barriers to and enablers of contraception use among adolescent females in an emergency department-based intervention. Contraception. 2015;91(3):217–225. doi: 10.1016/j.contraception.2014.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Cohen R, Sheeder J, Kane M, Teal SB. Factors associated with contraceptive method choice and initiation in adolescents and young women. J Adolesc Health. 2017;61,454–460. doi: 10.1016/j.jadohealth.2017.04.008 [DOI] [PubMed] [Google Scholar]
- [46].Gilliam ML, Warden M, Goldstein C, Tapia B. Concerns about contraceptive side effects among young Latinas: a focus-group approach. Contraception. 2004;70,299–305. doi: 10.1016/j.contraception.2004.04.013. [DOI] [PubMed] [Google Scholar]
- [47].Kaye K, Suellentrop K, Sloup C. The fog zone: how misperceptions, magical thinking, and ambivalence put young adults at risk for unplanned pregnancy. Power to decide. 2009. Accessed November 21, 2022. Available at: https://powertodecide.org/what-we-do/information/resource-library/fog-zone [Google Scholar]
- [48].College of Obstetricians and Gynecologists. Committee statement no. 1: Patientcentered contraception counseling. Am J Obstet Gynecol. 2022;139(2):349–353. doi: 10.1097/AOG.0000000000004659 [DOI] [Google Scholar]
- [49].https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-statement/articles/2022/02/patient-centered-contraceptive-counseling.pdfRaidoo S, Kaneshiro B. Contraception counseling in adolescents. Curr Opin Obstet Gynecol. 2017;29(5):310–315. doi: 10.1097/GCO.0000000000000390 [DOI] [PubMed] [Google Scholar]
- [50].Hoopes AJ, Timko AC, Akers AY. What’s known and what’s next: contraceptive counseling and support for adolescents and young adult women. J Pediatr Adolesc Gynecol. 2021;34(4):484–490. doi: 10.1016/j.jpag.2020.12.008 10.1016/j.jpag.2020.12.008 [DOI] [PubMed] [Google Scholar]
- [51].Walker AW, Stern L, Cipres D, Rodriquez A, Alvarez J, Sediman D. Do adolescent women’s contraceptive preferences predict method use and satisfaction? A survey of northern California family planning clients. J Adolesc Health. 2019;64(5):640–647. doi: 10.1016/j.jadohealth.2018.10.291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Gomez AM, Mann ES, Torres V. ‘It would have control over me instead of me having control’: intrauterine devices and the meaning of reproductive freedom. Crit Public Health. 2018;28(2):190–200. doi: 10.1080/09581596.2017.1343935 [DOI] [Google Scholar]
- [53].Chernick LS, Santelli J, Stockwell MS, et al. A multi-media digital intervention to improve the sexual and reproductive health of female adolescent emergency department patients. Acad Emerg Med. 2022;29(3):308–316. doi: 10.1111/acem.14411 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


