Summary:
The transconjunctival incision is a common and effective approach for establishing surgical exposure to the orbital floor. When access to the lateral orbit is also required, this incision may be extended by an accompanying lateral canthotomy, which releases the tarsal plates from the conjunctiva. Although this approach broadens surgical access through a simple extension, it is often remarked for unpredictable healing patterns and negative aesthetic sequelae, such as rounding of the lateral canthal angle. Traditionally, lateral canthotomy is performed by a transverse incision through a natural skin crease of the lateral palpebral fissure. Herein, we discuss our experience with a less common approach to lateral canthotomy, in which only the inferior crus of the lateral canthal tendon is divided. This approach limits manipulation of delicate orbital anatomy and aims to minimize unsightly scarring while still affording excellent visualization of the lateral orbit and orbital floor.
Takeaways
Question: Traditional lateral canthotomy involves a transverse incision through the lateral palpebral fissure. However, this technique is remarked for unpredictable healing patterns and negative aesthetic sequelae. We aim to evaluate a modified approach to lateral canthotomy which may reduce these complications.
Findings: In a retrospective study of 47 patients undergoing lateral canthotomy using the modified approach, no patients demonstrated ectropion, entropion, rounding of the lateral canthal angle, or other aesthetic concerns.
Meaning: This modified approach to lateral canthotomy provides excellent access to the orbit while optimizing aesthetic outcomes.
CONCISE PRESENTATION OF UNIQUE IDEA, INNOVATION, OR TECHNIQUE
Refinement for Lateral Canthotomy
The transconjunctival incision is a common approach for surgical access to the orbital floor. This approach, which can be made in either a pre-septal or a retro-septal fashion, has become popular due to the absence of an external incision, while still affording adequate exposure to the inferior orbit.1,2 To broaden exposure, lateral canthotomy can be performed. Traditionally, canthotomy involves horizontal transection of the lateral palpebral fissure, orbicularis oculi, and lateral canthal tendons. Despite the benefits of this maneuver, lateral canthotomy has also been reported to lead to unpredictable healing and possible negative sequelae, such as rounding of the lateral canthal angle, lower lid malposition, and entropion.1,3,4 Herein, we discuss our experience with a less common modification that aims to minimize aesthetic and functional complications while improving access to the orbital floor.
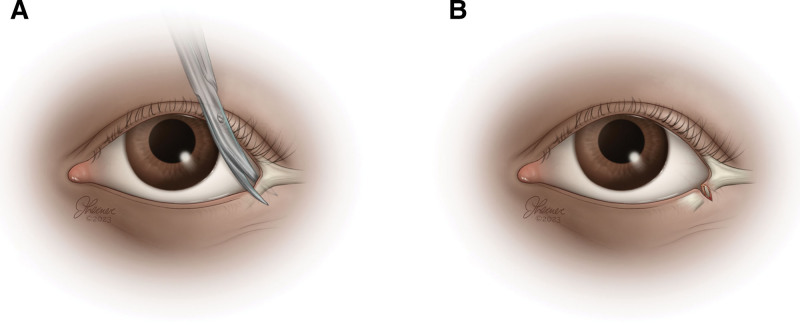
In our preferred approach, a vertically-oriented incision is made 2–3 mm medial to the lateral canthal angle along the lower lid, as illustrated in Figure 1. Silk retraction sutures are anchored into the tarsal plate, and a malleable retractor is placed overlying the orbit to expose the conjunctiva. Needle tip cautery is used to divide the conjunctiva in either the pre-septal or retro-septal plane, depending on surgeon preference.3 Blunt dissection with cotton tip applicators can then expose the orbital rim. The periosteum is incised with cautery, and periosteal elevators are used to elevate the entire orbital rim and provide exposure to the bony orbit. If necessary, exposure to the zygomaticofrontal suture may also be achieved through dissection of the lateral orbit.
Fig. 1.
Surgical illustrations of a modified lateral canthotomy. A, Division along the inferior canthal tendon, B, Inferior canthal release following transection.
A retrospective chart review was performed of all patients with orbital floor fractures evaluated at a tertiary academic medical center who underwent operative intervention using a transconjunctival incision with lateral canthotomy by the senior author (A.S.W.). Patients undergoing surgery by other incisional approaches or without lateral canthotomy were excluded. Patient demographic data, including sex and age at presentation, were documented. Clinical characteristics such as concomitant compound facial fractures were also recorded. Postoperative clinical documentation from serial outpatient follow-up visits was evaluated for a range of complications, such as rounding of the lateral canthal angle, entropion, and scleral show.
The senior author (A.S.W.) performed 47 orbital floor repairs using a transconjunctival approach with lateral canthotomy. The average patient was 35.2 years of age (range, 4 – 75), and 12 (25.5%) were women (Table 1). Panfacial fracture was the most common pattern of injury (25.5%), followed by isolated orbital floor fracture (17.0%). Patients were followed up for an average of 20.7 weeks (range, 0.4–132.1). The overall complication rate was 10.6%, consisting of residual enophthalmos, three (6.4%); blurry vision, one (2.1%); and infection, one (2.1%) (Table 2). No patients demonstrated ectropion, entropion, rounding of the lateral canthal angle, or other aesthetic concerns.
Table 1.
Demographic and Clinical Data for Patients Meeting Inclusion Criteria
| Patient Demographics | ||
|---|---|---|
| No. patients | 47 | |
| Age (y) | 35.2 (range, 4–75) | |
| Female status | 12 (25.5%) | |
| Follow-up (wk) | 145 (range, 0.4–132.1) | |
| Fracture Type | ||
| Isolated orbital floor | 8 (17.0%) | |
| Nasal bone | 2 (4.3%) | |
| Lateral orbital wall | 0 | |
| Medial orbital wall | 4 (8.5%) | |
| Fronto-zygomatic | 2 (4.3%) | |
| Naso-orbito-ethmoid | 8 (17.0%) | |
| Zygomaticomaxillary | 9 (19.1%) | |
| Le Fort I | 1 (2.1%) | |
| Le Fort II | 1 (2.1%) | |
| Le Fort III | 0 | |
| Panfacial | 12 (25.5%) | |
Table 2.
Postoperative Incidence of Aesthetic or Functional Complications after the Described Transconjunctival Incision with Accompanied Lateral Canthotomy
| Complications | Total | Rate of Complication | |
|---|---|---|---|
| Rounding of lateral canthal angle | Present | 0 | 0.0% |
| Absent | 47 | ||
| Total | 47 | ||
| Scleral show | Present | 0 | 0.0% |
| Absent | 47 | ||
| Total | 47 | ||
| Enophthalmos | Present | 3 | 6.4% |
| Absent | 44 | ||
| Total | 47 | ||
| Blurry vision | Present | 1 | 2.1% |
| Absent | 46 | ||
| Total | 47 | ||
| Infection | Present | 1 | 2.1% |
| Absent | 46 | ||
| Total | 47 | ||
| Entropion | Present | 0 | 0.0% |
| Absent | 47 | ||
| Total | 47 | ||
| Ectropion | Present | 0 | 0.0% |
| Absent | 47 | ||
| Total | 47 | ||
| Pruritis | Present | 0 | 0.0% |
| Absent | 47 | ||
| Total | 47 | ||
| Chemosis | Present | 0 | 0.0% |
| Absent | 47 | ||
| Total | 47 | ||
| All complications | 5 | 10.6% |
Each complication was managed conservatively. All patients presenting with residual enophthalmos (<2 mm) reported no significant difference compared with preoperative appearance, and revision procedures were not performed. The patient with blurry vision presented with visual disturbance on postoperative day 3, and normal vision was progressively restored over 1 month. The patient with infection was prescribed a short course of oral antibiotics; after 2 days of therapy, significant improvement was noted. Supplemental Digital Content 1 shows clinical images immediately after lateral canthal tendon approximation and subsequent healing on clinical follow-up. (See figure, Supplemental Digital Content 1, which shows a repair of canthal tendon and a postoperative evaluation in clinic several weeks after surgery demonstrating absence of a significantly visible scar or aesthetic concerns. http://links.lww.com/PRSGO/C575.)
DISCUSSION: SAFE AND EFFICACIOUS ACCESS TO THE LATERAL ORBIT
Although lateral canthotomy is often performed to increase surgical exposure to the orbit, unpredictable healing and consequent cosmetic and functional concerns related to cantholysis have remained challenges. We highlight an uncommon approach to lateral canthotomy that minimizes risks traditionally associated with this surgical maneuver while still affording the same degree of surgical exposure. Contrary to complications described in the literature, we observed no instances of rounding of the lateral canthal angle, lower lid malposition, entropion, or aesthetic issues using this technique. Residual enophthalmos (<2 mm) was the most common complication noted, arising in three of 47 patients (6.4%). Notably, enophthalmos was minimal and documented only for quantitative purposes using a Hertel exophthalmometer. It was not clinically appreciable by any of these patients, and each declined revision surgery due to lack of concern for the unappreciable deformity. Additionally, this complication would not be associated with the canthotomy procedure itself.
Transconjunctival incision with lateral canthotomy was first described in a unified approach around the 1980s for access to zygomatic fractures.5,6 In these initial procedures, a 3–5 mm incision was made through a natural crease along the lateral canthus, and the inferior and superior rami of the lateral canthal tendons were severed. At the time, this technique innovatively offered new access to both the floor and lateral orbit through a single incision, obviating the need for a separate surgical access through the upper brow or eyelid. Long-term experience, however, demonstrated that this approach exhibited less than desirable rates of complication. In a retrospective study, Salgarelli et al discovered a significant aesthetic complication rate of 34.8% for combined transconjunctival incision with canthotomy, compared with 0.3% for patients undergoing transconjunctival access alone.3 Of these complications, the most common was categorized broadly as lower eyelid malposition, consisting of rounding of the lateral canthal angle, scleral show, and ectropion. Other surgeons with similar experiences advised against the technique due to significant risk of adverse cosmetic outcomes.7,8 Still, many surgeons in contemporary practice continue to opt for a traditional lateral canthotomy despite the high rates of complication reported in the literature.
We believe that traditional cantholysis, though effective for establishing surgical access, damages delicate structures at their insertion, complicating reapproximation and closure. By a modified approach, releasing the inferior crus alone still provides excellent access to the orbital floor and lateral orbit, while optimizing outcomes by eliminating the need for reinsertion of the lateral canthus. Moreover, the more medially-based incision facilitates straightforward reapproximation of the tarsal plate by preserving a segment of the tarsus on either side. The present work builds on previous “lateral para-canthal” incisions in which only the inferior limb is divided.9,10 These investigations report results in modest cohorts of approximately 20 patients; in each study, at least one patient was noted to have a notch deformity of the lower lid. Additionally, the technique described in one of these articles is distinct, in which the canthotomy is performed extending from a conjunctival incision.9 In our experience, this frequently offers a less optimal line for closure at the conclusion of the procedure, compared with an initial canthotomy followed by a conjunctival incision made with pinpoint electrocautery. As the authors note in their article, they encountered complications requiring reoperation related to inadequate closure. The other article discusses a technique more similar to ours, however, in a cohort that is smaller and limited only to an East Asian population.10 Although the approach presented here is similar, we contend that this study bolsters the reliability of the combined transconjunctival and para-canthal incision for lateral orbital access in a larger cohort of patients, and that the specific technique described here offers superior aesthetic results.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 22 May 2023.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Kesselring AG, Promes P, Strabbing EM, et al. Lower eyelid malposition following orbital fracture surgery: a retrospective analysis based on 198 surgeries. Craniomaxillofac Trauma Reconstr. 2016;9:109–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oztel M, Goh R, Hsu E. Subtarsal versus transconjunctival approach: a long-term follow-up of esthetic outcomes and complications. J Oral Maxillofac Surg. 2021;79:1327.e1–1327.e6. [DOI] [PubMed] [Google Scholar]
- 3.Salgarelli AC, Bellini P, Landini B, et al. A comparative study of different approaches in the treatment of orbital trauma: an experience based on 274 cases. Oral Maxillofac Surg. 2010;14:23–27. [DOI] [PubMed] [Google Scholar]
- 4.Baumann A, Ewers R. Use of the preseptal transconjunctival approach in orbit reconstruction surgery. J Oral Maxillofac Surg. 2001;59:287–91; discussion 291–292. [DOI] [PubMed] [Google Scholar]
- 5.McCord CD, Moses JL. Exposure of the inferior orbit with fornix incision and lateral canthotomy. Ophthalmic Surg. 1979;10:53–63. [PubMed] [Google Scholar]
- 6.Nunery WR. Lateral canthal approach to repair of trimalar fractures of the zygoma. Ophthalmic Plast Reconstr Surg. 1985;1:175–183. [DOI] [PubMed] [Google Scholar]
- 7.Zingg M, Chowdhury K, Lädrach K, et al. Treatment of 813 zygoma-lateral orbital complex fractures. New aspects. Arch Otolaryngol Head Neck Surg. 1991;117:611–20; discussion 621–622. [DOI] [PubMed] [Google Scholar]
- 8.Turk JB, Ladrach K, Raveh J. Repair of zygomaticomalar complex fractures. The Swiss method. Arch Facial Plast Surg. 1999;1:123–126. [DOI] [PubMed] [Google Scholar]
- 9.de Chalain TM, Cohen SR, Burstein FD. Modification of the transconjunctival lower lid approach to the orbital floor: lateral paracanthal incision. Plast Reconstr Surg. 1994;94:877–880. [DOI] [PubMed] [Google Scholar]
- 10.Song J, Lee GK, Kwon ST, et al. modified transconjunctival lower lid approach for orbital fractures in east asian patients: the lateral paracanthal incision revisited. Plast Reconstr Surg. 2014;134:1023–1030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.