Background:
The risk of women developing breast cancer after augmentation mammaplasty may be lower than the general population, with minimal current literature on breast reconstruction in this population. We sought to evaluate the impact of previous augmentation on postmastectomy breast reconstruction.
Methods:
Retrospective review of patients who underwent mastectomies from 2017 to 2021 at our institution was performed. Analysis included frequencies and percentages, descriptive statistics, chi-square analysis, and Fisher exact test.
Results:
Four hundred seventy patients were included, with average body mass index of 29.1 kg/m2, 96% identifying as White, and an average age at diagnosis of 59.3 years. Twenty (4.2%) patients had a prior breast augmentation. Reconstruction was performed in 80% of the previously augmented patients compared to 49.9% of nonaugmented patients (P = 0.01). Reconstruction was alloplastic in 100% of augmented and 88.7% of nonaugmented patients (P = 0.15). All reconstructed augmented patients underwent immediate reconstruction compared with 90.5% of nonaugmented patients (P = 0.37), and two-stage reconstruction was most common (75.0% versus 63.5%; P = 0.42). Of the previously augmented patients, 87.5% increased implant volume, 75% underwent same implant plane reconstruction, and 68.75% underwent same implant-type reconstruction as their augmentation.
Conclusions:
Previously augmented patients were more likely to undergo reconstruction after mastectomy at our institution. All reconstructed augmented patients underwent alloplastic reconstruction, with most performed immediately in staged fashion. Most patients favored silicone implants and maintained the same implant type and plane of reconstruction, with increased implant volume. Larger studies are required to further investigate these trends.
Takeaways
Question: What impact does previous augmentation mammaplasty have on breast reconstruction after mastectomy for breast cancer?
Findings: After retrospective review at a single institution, previously augmented patients more often underwent postmastectomy reconstruction that was implant-based with immediate reconstruction in a staged fashion, compared with nonaugmented patients. Most patients favored silicone implants, had increased implant volumes, and maintained the same implant type and plane during reconstruction as their previous augmentation.
Meaning: Previously augmented patients may be more likely to undergo breast reconstruction after mastectomy than nonaugmented patients, and in a similar fashion to their previous augmentation.
INTRODUCTION
Augmentation mammaplasty (breast augmentation) is one of the most commonly performed cosmetic surgery procedures in the United States and worldwide.1–3 As more breast augmentations are performed, the rate of patients who present with new breast cancer diagnoses in this population is expected to increase. This is despite the fact that the incidence of breast cancer in patients who had previously undergone breast augmentation has been historically lower than expected, and may actually decrease the risk of developing breast cancer.4–6 Previous studies have focused on cancer detection in patients with breast implants, as there was concern that implants could delay detection and impact survivorship, which has now been demonstrated to be inaccurate.4,5,7–13 This highlights the safety of this procedure and may explain why its rate of performance continues to increase.
Breast reconstruction after mastectomy has been demonstrated to have numerous benefits, including increased self-esteem, quality of life, patient satisfaction, and psychosocial well-being.14,15 The rate of overall breast reconstruction has increased, along with immediate breast reconstruction, and use of breast implants in general.16–20 Despite the increasing rates of augmentation mammaplasties and overall breast reconstruction after mastectomy being performed, there is limited literature on the trends and outcomes of reconstruction in patients with previous augmentations. Previous studies examining the impact that breast augmentation has on breast cancer management and reconstruction have focused on the types of surgical resection, timing of reconstruction, and complication rates.9,21
Although these findings are important, no studies to our knowledge compared postmastectomy reconstruction (PMR) in patients with and without prior breast augmentation while specifically examining the impact of breast implant characteristics, such as implant type, volume, and plane of placement. The purpose of this study was to evaluate the impact that breast augmentation has on PMR in patients with breast cancer at a single institution.
METHODS
A retrospective review of patients who underwent mastectomy for breast cancer from 2017 to 2021 at a single tertiary-care institution was performed. This study was institutional review board approved with waiver of informed consent requirement (University of Tennessee Graduate School of Medicine, Knoxville, Tenn., IRB reference 4810). Each patient underwent review of all available information in our electronic medical records for possible inclusion. Male patients, those with incomplete records, and those who did not undergo mastectomies at our institution were excluded. Prior breast augmentation information was collected from operative reports, imaging findings, pathology reports, and physician- or patient-reported data. To remain consistent throughout comparisons, the term “prepectoral” (PP) is used to represent both the “subglandular” augmentation plane and the “prepectoral” reconstruction plane, and the term “submuscular” (SM) is used to represent the “dual-plane submuscular” and “totally submuscular” augmentation and reconstruction planes.
Statistical Analysis
The demographic and clinical characteristics of the sample were calculated using frequencies and percentages for discrete variables, and descriptive statistics (mean and standard deviation) were used to describe continuous variables. Chi-square analyses and Fisher exact tests were performed to compare independent groups on categorical outcomes, and independent samples t tests were performed to test for differences between groups on continuous variables. Descriptive statistics were reported to give context to the group comparisons. Statistical significance was assumed at an alpha value of 0.05, and all analyses were performed using SPSS version 28 (Armonk, N.Y.; IBM Corp.).
RESULTS
A total of 470 patients were included for final analysis. Within this sample, the average body mass index (BMI) was 29.1 kg/m2, 96% of patients identified as White, and average age of breast cancer diagnosis was 59.3 years. The average length of follow-up was 23.9 months. Of these patients, 20 (4.2%) had undergone prior breast augmentation, of which all were bilateral augmentation mammaplasty (BAM).
Comparison between all patients with a history of breast augmentation (group A), patients with no history of augmentation who underwent PMR (group B), and patients with no prior augmentation who did not undergo PMR (group C) was performed. The age at diagnosis between groups was significantly different (59.25 versus 53.38 versus 65.10; P < 0.001), but there was no significant difference in BMI or race/ethnicity. There were significant differences in insurance status (P < 0.001), rates of diabetes mellitus (P < 0.001), and rates of tobacco use (P = 0.011) among groups (Table 1).
Table 1.
Demographics and Comorbidities
| Variable | Previously Augmented (Group A) (n = 20) | Reconstructed Nonaugmented (Group B) (n = 222) | Nonreconstructed and Nonaugmented (Group C) (n = 228) | P |
|---|---|---|---|---|
| Age at diagnosis (y)* | 59.25 (12.7) | 53.4 (11.4) | 65.1 (11.9) | <0.001 |
| Body mass index (kg/m2)* | 24.0 (4.4) | 28.8 (6.3) | 29.9 (15.0) | 0.07 |
| Race/ethnicity† | ||||
| White | 20 (100.0) | 214 (96.4) | 217 (95.2) | |
| Black | 0 (0.0) | 6 (2.7) | 9 (3.9) | |
| Asian | 0 (0.0) | 2 (0.9) | 1 (0.4) | |
| Hispanic | 0 (0.0) | 0 (0.0) | 1 (0.4) | 0.83 |
| Insurance status† | ||||
| Uninsured | 0 (0.0) | 4 (1.8) | 2 (0.9) | |
| Medicaid | 2 (10.0) | 15 (6.8) | 17 (7.5) | |
| Medicare | 9 (45.0) | 54 (24.3) | 127 (55.7) | |
| Private insurance | 0 (0.0) | 7 (3.2) | 1 (0.4) | |
| Other public insurance | 9 (45.0) | 142 (64.0) | 81 (35.5) | <0.001 |
| Diabetes mellitus† | ||||
| Yes | 2 (10.0) | 17 (7.7) | 48 (21.1) | <0.001 |
| Tobacco status† | ||||
| No history of use | 10 (50.0) | 160 (72.1) | 131 (57.5) | |
| Current smoker | 4 (20.0) | 20 (9.0) | 38 (16.7) | |
| Former smoker | 6 (30.0) | 42 (18.9) | 59 (25.9) | 0.01 |
Denotes outcomes reported as average (standard deviation).
Denotes outcomes reported as total number (percentage).
Bold indicates P < 0.05, statistically significant.
Bilateral total mastectomy was performed in 50% of group A patients, compared with 63.1% of group B and 39.0% of group C patients (P < 0.001). There was no significant difference between groups in rates of neoadjuvant therapy, postoperative chemotherapy, postoperative radiation therapy, or hormonal therapy. (See table, Supplemental Digital Content 1, which shows oncologic treatment, http://links.lww.com/PRSGO/C579.) Of the five previously augmented patients who underwent adjuvant radiation therapy (ART), three (60.0%) did not undergo PMR. Two of these patients had strong suspicion of need for ART during counseling preoperatively. Only one augmented patient who had strong preoperative suspicion of need for ART underwent reconstruction. Disease status at last follow-up was significantly different between groups, with 100% of group A patients having no evidence of disease compared to other groups (98.6% group B versus 93.0% group C; P = 0.03).
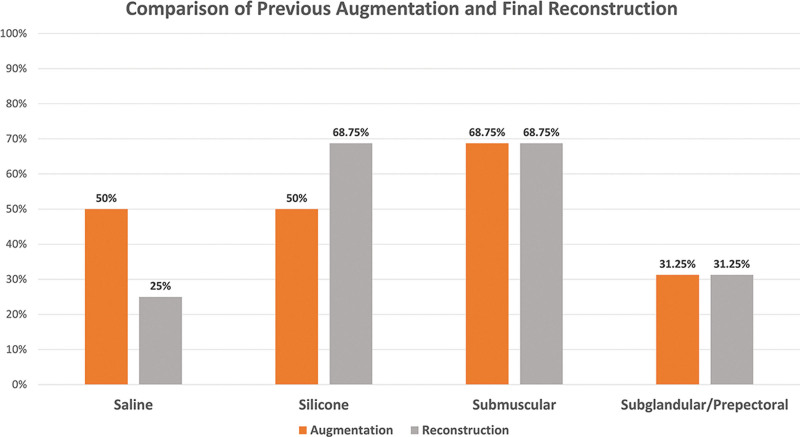
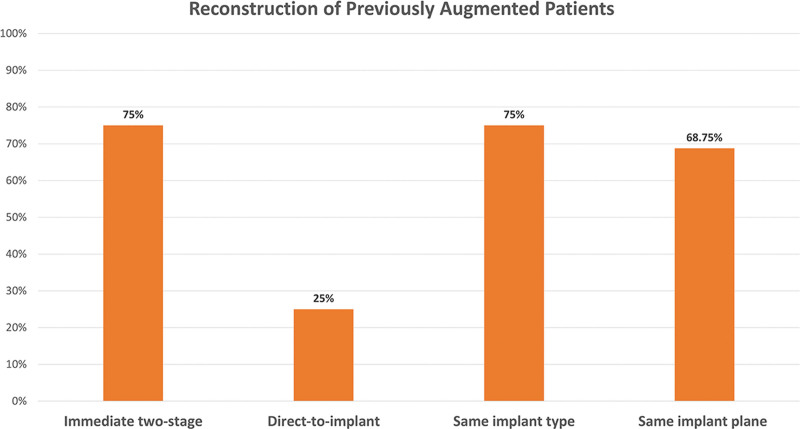
The descriptions of all previously augmented patients are included in Table 2. Of patients who had prior breast augmentation, nine underwent prepectoral (subglandular) augmentation and 11 submuscular, with 50% having silicone implants. PMR was performed in 80% of the previously augmented patients compared with 49.9% of nonaugmented patients (P = 0.01). Within these groups, 100% of patients with prior augmentation underwent alloplastic reconstruction compared with 88.7% in the previously nonaugmented group (P = 0.15). Submuscular reconstruction was performed in 11 patients, while prepectoral was performed in five patients (Table 2). Of reconstructed previously augmented patients, 100% underwent immediate reconstruction compared with 90.5% of nonaugmented patients (P = 0.37). Of augmented patients, 25.0% underwent direct-to-implant (DTI) reconstruction compared with 26% of nonaugmented patients (P = 1.00). During reconstruction, 11 patients chose silicone (68.8%) in the previously augmented group compared with 53.0% in the nonaugmented group (P = 0.43) (Fig. 1). Of reconstructed patients with prior augmentation, 75% underwent the same implant plane reconstruction, and 68.75% underwent the same implant-type reconstruction as their previous augmentation (Fig. 2). Four of the eight patients who had saline implants and underwent reconstruction transitioned to silicone, while no patients with prior silicone implants transitioned to saline (Table 2). Two patients transitioned from prepectoral to submuscular planes during reconstruction, and two patients, from submuscular to prepectoral. All patients who changed planes during reconstruction had previous saline augmentation implants.
Table 2.
Previously Augmented Patients
| No. | Prior Augmentation Type | Prior Augmentation Implant Type | Prior Augmentation Implant Plane | Reconstruction Timing | Reconstruction Implant Type | Reconstruction Implant Plane | Change in Implant Volume (cc) |
|---|---|---|---|---|---|---|---|
| 1 | BAM | Saline | SM | ITS | Silicone | SM | +400 |
| 2 | BAM | Saline | SM | ITS | Saline | PP | −200 |
| 3 | BAM | Saline | SM | DTI | Silicone | SM | +350 |
| 4 | BAM | Saline | SM | DTI | Silicone | PP | +280 |
| 5 | BAM | Saline | PP | ITS | Saline | SM | +190 |
| 6 | BAM | Saline | SM | ITS | Silicone | SM | +280 |
| 7 | BAM | Saline | PP | ITS | Saline | PP | +100 |
| 8 | BAM | Saline | PP | ITS | Saline | SM | +150 |
| 9 | BAM | Saline | PP | None | None | N/A | N/A |
| 10 | BAM | Saline | PP | None | None | N/A | N/A |
| 11 | BAM | Silicone | PP | None | None | N/A | N/A |
| 12 | BAM | Silicone | PP | None | None | N/A | N/A |
| 13 | BAM | Silicone | SM | ITS | Silicone | SM | +155 |
| 14 | BAM | Silicone | PP | ITS | Tissue expanders only | PP | −160 |
| 15 | BAM | Silicone | SM | DTI | Silicone | SM | +200 |
| 16 | BAM | Silicone | SM | ITS | Silicone | SM | +50 |
| 17 | BAM | Silicone | SM | ITS | Silicone | SM | +85 |
| 18 | BAM | Silicone | PP | ITS | Silicone | PP | +325 |
| 19 | BAM | Silicone | SM | DTI | Silicone | SM | +150 |
| 20 | BAM | Silicone | SM | ITS | Silicone | SM | +165 |
BAM, bilateral augmentation mammaplasty; DTI, direct to implant; ITS, immediate two-stage; N/A, not applicable; PP, prepectoral/subglandular; SM, submuscular.
Change in volume expressed as difference of final reconstructed implant volume from augmentation volume.
Fig. 1.
Comparison of augmentation and reconstructive implant characteristics among the previously augmented patients who underwent reconstruction.
Fig. 2.
Comparison of the timing and type of reconstruction performed in the previously augmented patients who underwent reconstruction.
Of the augmented patients who underwent reconstruction, 87.5% increased implant volume from their prior augmentation. The average volume change in those who underwent an increase was 205.7 cubic centimeters (cc) (SD = 105.4), while the average volume change of those who underwent a decrease was 180 cc (SD = 28.3). The average augmentation implant volume of reconstructed patients was 405.3 cc (SD = 108.8), with 10 (62.5%) patients having volumes greater than or equal to 400 cc. Of these 10 patients, 70% underwent two-stage reconstruction, and 80% increased implant volume during reconstruction. Reconstructed patients with augmentation implant volumes greater than or equal to 400 cc and less than 400 cc were compared, with no significant differences in rates of two-stage reconstruction (70% versus 83.3%; P = 0.55) or rates of implant plane change during reconstruction (20% versus 33.3%; P = 0.55) between groups. Most patients who underwent two-stage reconstruction had an increase in implant volume (83.3%), with an average change of 128.3 cc (Table 3). All patients who underwent DTI reconstruction had an increase in implant volume, with an average change of 245.0 cc. There was no significant difference between rates of increased volume (P = 1.00) or change in volume amount between groups (P = 0.12). Most patients who changed implant planes during reconstruction had an increase in implant volume (75.0%), with an average change of 105.0 cc. This was also true for patients who did not change planes during reconstruction, with 91.7% undergoing an increase in volume, with an average change of 175.0 cc (Table 3). There was no significant difference between these groups in rates of implant volume increase (P = 0.38) or in change in volume amount (P = 0.24).
Table 3.
Breast Implant Volume Changes in Reconstructed Previously Augmented Patients
| Variable | Two-stage Reconstruction (n = 12) | DTI Reconstruction (n = 4) | P | Implant Plane Change (n= 4) | No Implant Plane Change (n = 12) | P |
|---|---|---|---|---|---|---|
| Increased implant volume* | 10 (83.3) | 4 (100.0) | 3 (75.0) | 11 (91.7) | ||
| Decreased implant volume* | 2 (16.7) | 0 (0.0) | 1.00 | 1 (25.0) | 1 (8.3) | 0.38 |
| Change in implant volume (cc)† | 128.3 (176.2) | 245.0 (88.1) | 0.12 | 105.0 (210.5) | 175.0 (153.2) | 0.24 |
Expressed as increase or decrease in volume from previous augmentation implant to final reconstruction implant.
Denotes outcomes reported as total number (percentage).
Denotes outcomes reported as average (standard deviation).
Reconstructed augmented patients were further compared with reconstructed nonaugmented patients, with no significant differences between rates of bilateral reconstruction, final alloplastic implant type, revision after reconstruction, implant removal, or use of acellular dermal matrix between the two groups (Table 4). Complication rates in previously augmented and nonaugmented patients are presented in Table 5. Rates of overall complications did not differ significantly between these groups (35.0% versus 44.1%; P = 0.43). There was no significant difference in rates of wound infection, wound dehiscence, deep vein thrombosis, hematoma, reoperation, or lymphedema between groups.
Table 4.
Reconstructed Patients
| Variable | Reconstructed with Prior Augmentation (n = 16) | Reconstructed Non-augmented (n = 222) | P |
|---|---|---|---|
| Bilateral reconstruction* | |||
| Yes | 12 (75.0) | 177 (79.7) | 0.60 |
| Alloplastic reconstruction* | |||
| Yes | 16 (100.0) | 197 (88.7) | 0.15 |
| Timing of reconstruction* | |||
| Immediate | 16 (100.0) | 201 (90.5) | |
| Delayed | 0 (0.0) | 21 (9.5) | 0.37 |
| Type of implant reconstruction* | |||
| Two-stage reconstruction | 12 (75.0) | 141 (63.5) | |
| Direct to implant, saline | 0 (0.0) | 14 (6.3) | |
| Direct to implant, silicone | 4 (25.0) | 44 (19.8) | 0.42 |
| Final implant type* | |||
| Saline | 4 (25.0) | 58 (32.0) | |
| Silicone | 11 (68.8) | 96 (53.0 | |
| Tissue expanders | 1 (6.3) | 27 (14.9) | 0.43 |
| ADM use* | |||
| Yes | 9 (56.3) | 116 (55.8) | 1.00 |
| Implant removal* | |||
| Yes | 2 (12.5) | 38 (20.0) | 0.74 |
| Revision* | |||
| Yes | 7 (43.8) | 100 (45.0) | 0.80 |
Denotes outcomes reported as total number (percentage).
ADM, acellular dermal matrix.
Table 5.
Complications between Previously Augmented Patients and Reconstructed Nonaugmented Patients
| Variable | Previously Augmented (n = 20) | Reconstructed Nonaugmented (n = 222) | P |
|---|---|---|---|
| Complications* | |||
| Yes | 7 (35.0) | 98 (44.1) | 0.43 |
| Wound infection* | |||
| Yes | 0 (0.0) | 28 (12.6) | 0.14 |
| Wound dehiscence* | |||
| Yes | 4 (20.0) | 37 (16.7) | 0.76 |
| Deep vein thrombosis* | |||
| Yes | 0 (0.0) | 2 (0.9) | 1.00 |
| Hematoma* | |||
| Yes | 0 (0.0) | 6 (2.7) | 1.00 |
| Lymphedema* | |||
| Yes | 1 (5.0) | 12 (5.4) | 1.00 |
| Reoperation* | |||
| Yes | 6 (30.0) | 75 (33.8) | 0.81 |
Denotes outcomes reported as total number (percentage).
DISCUSSION
Although studies have focused on breast cancer detection and development in patients with cosmetic breast implants,7,13 there is limited literature regarding outcomes and trends of PMR in this population.9,21 This may be partly due to the low prevalence of breast cancer in previously augmented patients, making the study of this population difficult.4–6 We hypothesized that patients with previous breast augmentations would be more likely to undergo PMR, more often undergo implant-based reconstruction, and would have a similar implant type and implant plane of placement in their reconstructed breast as they did during augmentation.
In our study population, 20 (4.2%) patients had undergone previous augmentation mammaplasty. Augmented patients were compared with nonaugmented patients who underwent reconstruction after mastectomy, as well as those who were nonaugmented and nonreconstructed after mastectomy. Nonaugmented patients who did not undergo PMR were significantly older, while there was no significant difference in BMI or race/ethnicity between groups. Our patient population is less diverse than national averages, with 96% of our patients identifying as White, but is similar in other demographics and comorbidities. There was a significant difference in rates of diabetes mellitus between groups, with similar rates in the augmented and reconstructed nonaugmented groups. There was also a significant difference in the rates of tobacco use among groups, with the highest rate found in the previously augmented patients. These findings may be due to the small population of the augmented group and may not be significant on a larger scale. The insurance status of the patients within each group was significantly different, with no patients who had undergone augmentation being uninsured, and with the most common insurance types of Medicare and other non-Medicare/Medicaid insurance. This finding is not surprising, as these patients had previously undergone an elective cosmetic procedure.
Bilateral mastectomy was more common than unilateral mastectomy in all groups. This finding is consistent with national trends that demonstrate increased rates of bilateral mastectomy, specifically in patients with unilateral breast cancer. One study demonstrated that patients with prior breast augmentation were more likely to undergo mastectomy rather than lumpectomy, when compared with patients without prior augmentations and comparable disease.9 A 2013 study discovered that unilateral mastectomies decreased by about 2% per year between 1998 and 2008, while bilateral mastectomies increased by 17% per year during the same time.16 Other studies have corroborated these findings, with approximately 40% of patients undergoing mastectomy, the rate of risk-reducing bilateral mastectomies increasing, and increased rates of PMR.17–20
Among the augmented patients, 80% underwent PMR. This was significantly higher than 49.9% of the nonaugmented group and demonstrates that patients who have undergone previous augmentation mammaplasty may be more likely to be interested in, or be able to undergo, postmastectomy breast reconstruction. There was no significant difference in rates of bilateral reconstruction between augmented and nonaugmented patients. Of the reconstructed augmented patients, 100% underwent alloplastic reconstruction compared with 88.7% of the nonaugmented group. The overall rate of postmastectomy autologous reconstruction at our institution is similar to the recently published national average of 19%.22 Of the reconstructed augmented patients, 100% underwent immediate reconstruction compared with 90.5% of nonaugmented patients, with the majority of the augmented patients undergoing immediate two-stage reconstruction. Albornoz et al16 demonstrated that immediate breast reconstruction rates increased from 20.8% to 37.8% during a 10-year period, with an average increase of 5% per year, whereas autologous reconstruction rates remained the same. Breast implant use, in general, also increased by an average of 11% per year during this time.16 A study investigating plastic surgeon practice patterns and perspectives on PMR demonstrated that immediate reconstruction was most common, with most surgeons performing staged implant-based reconstruction.23 The higher rate of implant-based reconstruction among augmented patients may be in part due to the familiarity and comfort these patients have with breast implants, and therefore the related process of this reconstruction type.
Among augmented patents, four did not undergo PMR, with all these patients having prior prepectoral (subglandular) mammaplasties (50% saline implants). During both augmentation and reconstruction, submuscular implant placement was more common. Four patients had DTI reconstruction, while the remaining 11 (75%) underwent two-stage reconstruction, with no significant difference seen from the reconstructed nonaugmented patients. Silicone implants were more common during reconstruction (Fig. 1), which was not significantly different from the nonaugmented group. Overall, of the reconstructed augmented patients, 75% underwent the same implant plane reconstruction, and 68.75% underwent the same implant-type reconstruction as their augmentation mammaplasty (Fig. 2). This may indicate that augmented patients who undergo PMR would prefer to have a similar reconstruction to their previous augmentation. This could be related to patient satisfaction with their augmentation, or in those patients who had previous submuscular implants, may be partly due to the already developed submuscular plane. None of the patients with previous silicone implants transitioned to saline. The patients who changed from saline to silicone implants reported desire for more “natural” feel, which becomes more important in reconstruction compared with augmentation due to the absence of breast tissue to provide additional coverage over the implant.
Among reconstructed augmented patients, 87.5% underwent an increase in implant volume during reconstruction, with an average increase of 205.7cc. The overall trend of larger reconstructive implants compared with the prior augmentation implants may be explained by the absence of glandular tissue after mastectomy. This is especially true when trying to match the size of a patient’s augmented contralateral breast after unilateral mastectomy and reconstruction. We did not find a statistically significant difference in implant volume changes from augmentation to reconstruction when comparing two-stage and DTI reconstruction, or a significant difference when reconstruction was performed with or without an implant plane change. This may indicate that DTI reconstruction and lack of plane change did not significantly impact the patient’s ability to undergo changes in implant volume during reconstruction. Reconstructed patients with augmentation implants greater than or equal to 400 cc were not significantly more likely to undergo two-stage reconstruction or undergo a plane change during reconstruction when compared with patients with augmentation implants less than 400 cc. Based on our limited series, these findings indicate that larger augmentation implant volumes did not preclude these patients from maintaining the same plane during reconstruction or from undergoing DTI reconstruction to achieve a desired postmastectomy breast size.
The need for ART may play a role in the decision to undergo PMR among augmented patients. Of the five augmented patients who underwent ART, three did not undergo PMR, with two of these patients having strong suspicion of need for ART during counseling preoperatively. Of the two patients who did undergo reconstruction, one underwent DTI reconstruction with silicone implants, and the other underwent two-stage reconstruction with silicone implants. Only the patient who underwent DTI reconstruction had strong suspicion of the need for ART preoperatively. This preoperative consideration likely plays a role in the reconstructive decision process, but a larger sample size is needed to make definitive conclusions.
There was no significant difference between the rates of revision or implant removal after reconstruction among the augmented and nonaugmented reconstructed patients, or a significant difference in rates of overall or individual complications between groups. This is similar to a 2021 study that also demonstrated no significant difference in complications when comparing postmastectomy outcomes in patients with and without prior augmentation mammaplasty.21 That study did find a significantly increased risk of augmented patients undergoing one or more unplanned reoperations after reconstruction,21 which was not consistent with our findings.
There are limitations within this study including its retrospective nature. Although this study included all patients who underwent mastectomies over a 5-year period at a single institution, a low percentage of patients had previously undergone breast augmentation. This may be largely due to the relatively low incidence of breast cancer development in this population and makes study within the population challenging. Our study population is smaller than the discussed publications that have examined different aspects of the reconstructive process in previously augmented patients but is the one to date that has examined these specific characteristics. Furthermore, our study period does not adequately capture the trends of breast reconstruction after the release of the updated US Food and Drug Administration recommendations on breast implants and the boxed warning issued at the end of 2021. Further research is required to capture how recent findings related to the safety of breast implants, such as the risk of breast implant-associated neoplasms and breast implant illness, impact PMR and choice of implant in alloplastic reconstruction.24–28 Finally, future studies incorporating patient reported outcomes would allow for better assessment of patient satisfaction with breast reconstruction in this subset of patients.
CONCLUSIONS
Patients with prior augmentation mammaplasty were significantly more likely to undergo PMR when compared with nonaugmented patients. All previously augmented reconstructed patients underwent alloplastic reconstruction, the majority of which were performed immediately and in staged fashion. Most augmented patients maintained their same implant type and plane of augmentation during reconstruction, with submuscular reconstruction and silicone implants more common. Most previously augmented patients also underwent an increase in implant volume during reconstruction compared with their prior augmentation volume. There was no significant difference in complications after reconstruction between augmented and nonaugmented patients. These findings are important to understand the role of prior breast augmentation in postmastectomy breast reconstruction. This is especially true with increasing rates of breast augmentations being performed, as this will likely increase the incidence of patients diagnosed with breast cancer in this population. As the current prevalence of breast cancer in previously augmented patients remains relatively low, larger multicenter studies should be performed to further investigate these trends.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 22 May 2023.
Presented at Plastic Surgery, The Meeting on October 27, 2022 in Boston, Mass.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Zimmerman AL, Tugertimur B, Smith PD, et al. In the age of breast augmentation, breast reconstruction provides an opportunity to augment the breast. Cancer Control.. 2017;24:1073274817729064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Society of Plastic Surgeons. Cosmetic procedure trends, plastic surgery statistics report 2020. 2020. Accessed March 13, 2023. Available at https://www.plasticsurgery.org/documents/News/Statistics/2020/cosmetic-procedure-trends-2020.pdf.
- 3.The Aesthetic Society. Aesthetic plastic surgery national databank statistics 2020–2021. Published online 2021. Accessed March 13, 2023. Available at https://cdn.surgery.org/media/statistics/2021-TheAestheticSocietyStatistics.pdf.
- 4.Fracol M, Shah N, Dolivo D, et al. Can breast implants induce breast cancer immunosurveillance? An analysis of antibody response to breast cancer antigen following implant placement. Plast Reconstr Surg. 2021;148:287–298. [DOI] [PubMed] [Google Scholar]
- 5.Deapen D. Breast implants and breast cancer: a review of incidence, detection, mortality, and survival. Plast Reconstr Surg. 2007;120(supplement 1):70S–80S. [DOI] [PubMed] [Google Scholar]
- 6.Noels EC, Lapid O, Lindeman JHN, et al. breast implants and the risk of breast cancer: a meta-analysis of cohort studies. Aesthet Surg J. 2015;35:55–62. [DOI] [PubMed] [Google Scholar]
- 7.Spear SL, Clemens MW, Dayan JH. Considerations of previous augmentation in subsequent breast reconstruction. Aesthet Surg J. 2008;28:285–293. [DOI] [PubMed] [Google Scholar]
- 8.Cho EH, Shammas RL, Phillips BT, et al. Breast cancer after augmentation: oncologic and reconstructive considerations among women undergoing mastectomy. Plast Reconstr Surg. 2017;139:1240e–1249e. [DOI] [PubMed] [Google Scholar]
- 9.Sosin M, Devulapalli C, Fehring C, et al. Breast cancer following augmentation mammaplasty: a case-control study. Plast Reconstr Surg. 2018;141:833–840. [DOI] [PubMed] [Google Scholar]
- 10.Miglioretti DL. Effect of breast augmentation on the accuracy of mammography and cancer characteristics. JAMA. 2004;291:442442. [DOI] [PubMed] [Google Scholar]
- 11.Hölmich LR, Mellemkjær L, Gunnarsdóttir KA, et al. Stage of breast cancer at diagnosis among women with cosmetic breast implants. Br J Cancer. 2003;88:832–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azzi AJ, Gornitsky J, Viezel-Mathieu A, et al. The impact of implant location on breast cancer characteristics in previously augmented patients: a systematic literature analysis. J Cancer Prev. 2018;23:93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lavigne E, Holowaty EJ, Pan SY, et al. Breast cancer detection and survival among women with cosmetic breast implants: systematic review and meta-analysis of observational studies. BMJ. 2013;346:f2399. [DOI] [PubMed] [Google Scholar]
- 14.Atisha D, Alderman AK, Lowery JC, et al. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan breast reconstruction outcomes study. Ann Surg. 2008;247:1019–1028. [DOI] [PubMed] [Google Scholar]
- 15.Guyomard V, Leinster S, Wilkinson M. Systematic review of studies of patients’ satisfaction with breast reconstruction after mastectomy. Breast. 2007;16:547–567. [DOI] [PubMed] [Google Scholar]
- 16.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. [DOI] [PubMed] [Google Scholar]
- 17.Sawyer JD, Franke J, Scaife S, et al. Autologous breast reconstruction is associated with lower 90-day readmission rates. Plast Reconstr Surg Glob Open. 2022;10:e4112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kummerow KL, Du L, Penson DF, et al. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150:99. [DOI] [PubMed] [Google Scholar]
- 19.Jones C, Lancaster R. Evolution of operative technique for mastectomy. Surg Clin North Am. 2018;98:835–844. [DOI] [PubMed] [Google Scholar]
- 20.Liede A, Cai M, Crouter TF, et al. Risk-reducing mastectomy rates in the US: a closer examination of the Angelina Jolie effect. Breast Cancer Res Treat. 2018;171:435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammond JB, Foley BM, James S, et al. Does prior breast augmentation affect outcomes after mastectomy with reconstruction? An analysis of postoperative complications and reoperations. Ann Plast Surg. 2021;86:508–511. [DOI] [PubMed] [Google Scholar]
- 22.Broyles JM, Balk EM, Adam GP, et al. Implant-based versus autologous reconstruction after mastectomy for breast cancer: a systematic review and meta-analysis. Plast Reconstr Surg Glob Open. 2022;10:e4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Momoh AO, Griffith KA, Hawley ST, et al. Post-mastectomy breast reconstruction: exploring plastic surgeon practice patterns and perspectives. Plast Reconstr Surg. 2020;145:865–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen Tervaert JW, Mohazab N, Redmond D, et al. Breast implant illness: scientific evidence of its existence. Expert Rev Clin Immunol. 2022;18:15–29. [DOI] [PubMed] [Google Scholar]
- 25.Magnusson MR, Cooter RD, Rakhorst H, et al. Breast implant illness: a way forward. Plast Reconstr Surg. 2019;143:74S–81S. [DOI] [PubMed] [Google Scholar]
- 26.Nelson JA, McCarthy C, Dabic S, et al. BIA-ALCL and textured breast implants: a systematic review of evidence supporting surgical risk management strategies. Plast Reconstr Surg. 2021;147:7S–13S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marra A, Viale G, Pileri SA, et al. Breast implant-associated anaplastic large cell lymphoma: a comprehensive review. Cancer Treat Rev. 2020;84:101963. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg MT, Llaneras J, Willson TD, et al. Squamous cell carcinoma arising in breast implant capsules. Ann Plast Surg. 2021;86:268–272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.