Abstract
Background
The prevalence of perinatal depression increased during the COVID-19 pandemic, which may be due to changes in the profile of specific depressive symptoms.
Aims
To analyze the impact of the COVID-19 pandemic on the (1) prevalence and severity of specific depressive symptoms; and on the (2) prevalence of clinically significant symptoms of depression during pregnancy and postpartum.
Methods
Pregnant and postpartum women recruited before (n = 2395) and during the COVID-19 pandemic (n = 1396) completed a sociodemographic and obstetric questionnaire and the Edinburgh Postnatal Depression Scale (EPDS). For each item, scores ≥1 and ≥ 2 were used to calculate the prevalence and severity of depressive symptoms, respectively.
Results
The prevalence and severity of symptoms of depression were significantly higher during the COVID-19 pandemic. The prevalence of specific symptoms increased by >30%, namely “being able to laugh and see the funny side of things” (pregnancy 32.6%, postpartum 40.6%), “looking forward with enjoyment to things” (pregnancy 37.2%, postpartum 47.2%); and “feelings of sadness/miserable” or “unhappiness leading to crying” during postpartum (34.2% and 30.2%, respectively). A substantial increase was observed in the severity of specific symptoms related to feelings that “things have been getting on top of me” during pregnancy and the postpartum period (19.4% and 31.6%, respectively); “feeling sad or miserable” during pregnancy (10.8%); and “feeling scared/panicky” during postpartum (21.4%).
Conclusion
Special attention should be paid to anhedonia-related symptoms of perinatal depression to ensure that they are adequately managed in present and future situations of crisis.
Keywords: COVID-19 pandemic, Symptoms of depression, Prevalence, Severity, Pregnancy, Postpartum
1. Introduction
Mental health problems emerged as a major public health concern during the COVID-19 pandemic [1] and were considered an integral component of COVID-19 response plans by the World Health Organization (WHO) [2]. Nonetheless, out of 130 WHO member states, <1 in 5 countries allocated additional funding for mental health and psychosocial support, and >60% of antenatal or postnatal mental health services were disrupted [2]. At the same time, perinatal mental health problems increased, including clinically significant symptoms of depression [3].
1.1. COVID-19 pandemic and perinatal symptoms of depression
Systematic reviews published two to three years before the COVID-19 outbreak consistently estimated the prevalence of depressive symptoms to be 9.2% for the prenatal and 9.5% for the postpartum period in high-income countries [4], regardless of the tools used (symptom severity scales or diagnostic tools). In Portuguese cohorts, about 20.0% of pregnant women [5,6] and 15.0%–22.4% of postpartum women had clinically significant symptoms of depression [7,8].
The prevalence of perinatal symptoms of depression increased during the COVID-19 pandemic [3,9,10]. About 30% of women living in European and South American countries scored ≥13 on the Edinburgh Postnatal Depression Scale (EPDS), which indicates the presence of clinically significant symptoms of depression [10]. Specifically in Europe, a study conducted in five countries with pregnant and postpartum women reported lower prevalence of EPDS ≥13 in Switzerland (10.5%/10.4%); the Netherlands (11.5%/9.1%); and Norway (12.0%/14.6%), as compared to the UK (42.1%/42.3%) or Ireland (26.3%/24.3) [11]. The authors hypothesized that differences in prevalence rates could be explained at least partly by differences in social isolation; at the time of the study, social distancing restrictions were still in place in the UK and had recently been reduced in Ireland.
1.2. COVID-19 pandemic and specific symptoms of perinatal depression
The prevalence of clinically significant symptoms of depression during the COVID-19 pandemic is alarming. It is essential to gain knowledge on the increase in the prevalence and severity of specific symptoms of depression as a result of the COVID-19 pandemic. This would enhance the understanding of the presentation of symptoms which will ensure that adequate interventions are developed to meet the women's specific needs. Exploring the presentation of perinatal depression symptoms during the COVID-19 pandemic is especially relevant, as differences have been reported in the literature in relation to depressive symptoms in the perinatal period, as compared to other life periods [12,13,14]. The Edinburgh Postnatal Depression Scale [15] is a validated instrument for screening clinically significant symptoms of depression, both in pregnant and postpartum women [16]. The EPDS provides information on symptoms of depression, categorized as symptoms of anhedonia (items 1 and 2: able to laugh/looking forward); anxiety (items 3 to 5: self-blame, anxious/worried, scared panicky); and depression (items 6 to 10: overwhelmed, difficulty sleeping, sad or miserable, unhappy/crying, self-harm) [17,18]. This scale provides detailed information on the symptoms of perinatal depression, which prevalence and severity may have increased during the COVID-19 pandemic. The results obtained may help improve the readiness of health systems to meet the mental health needs of these women, according to their individual circumstances.
The aim of this study was to analyze the impact of the COVID-19 pandemic on the (1) prevalence and severity of specific symptoms of depression and on the (2) prevalence of clinically significant symptoms of depression during pregnancy and the postpartum period.
This study will contribute to the literature by providing comparative data on the prevalence and severity of specific symptoms of depression before and during the COVID-19 pandemic in a large sample of women in the perinatal period.
2. Method
2.1. Procedure
Data for the pre-pandemic period was collected from longitudinal cohorts of pregnant women recruited at public health centers in Northern Portugal (between 2004 and 2019). The aims and procedures of the study were explained to the participants. Written consent was obtained from pregnant women willing to participate. Data on expectant/postpartum women during the COVID-19 pandemic was collected through an online survey conducted between June 2020 and October 2020. All pregnant women (regardless of the stage of pregnancy) and mothers to infants younger than six months living in Portugal were eligible for inclusion. The aims and procedures of the study were explained to participants. Written consent was obtained prior to access being granted to the questionnaire (detailed procedures are described elsewhere; [19] reference omitted for blinded peer review). All the studies were conducted according to the Declaration of Helsinki. The study was approved by the local Ethics Committees of the participating sites. The final sample included 3791 women from the cohorts described (prior to the COVID-19 pandemic, n = 2395; during the COVID-19 pandemic, n = 1396). Participants filled in a socio-demographic and obstetric questionnaire and completed the EPDS [15] either during pregnancy or postpartum.
2.2. Measures
2.2.1. Socio-demographic and obstetric characteristics
Information regarding age; country of birth (foreign vs. native); education (≤ 9 years of education vs. 10–12 years of education vs. higher education [bachelor, master's degree or postgraduate diploma]); marital status (married/cohabiting vs. single/separated/divorced/widow); employment status (employed vs. unemployed/student/housewife); history of mental health problems (yes vs. no); parity (nulliparous/primiparous vs. multiparous); and risk pregnancy (Yes vs. No; with yes including maternal age over 40 or gestational diabetes or hypertension or short cervix or other clinical condition) was collected via a self-reported questionnaire.
2.2.2. Symptoms of depression
Symptoms of depression were assessed using the EPDS [15]. EPDS is a 10-item self-report scale rated on a four-point Likert-type scale (0 to 3) aimed at assessing the severity of symptoms of depression within the previous seven days. Total scores range from 0 to 30, with higher scores indicating a higher severity of symptoms of depression. The items and scoring system are as follows: “Item 1. I have been able to laugh and see the funny side of things; 0. As much as I always could, 1. Not quite so much now, 2. Definitely not so much now, 3. Not at all”; “Item 2. I have looked forward with enjoyment to things; 0. As much as I ever did, 1. Rather less than I used to, 2. Definitely less than I used to, 3. Hardly at all”; “Item 3. I have blamed myself unnecessarily when things went wrong; 0. No, never, 1. Not very often, 2. Yes, some of the time, 3. Yes, most of the time”; “Item 4. I have been anxious or worried for no good reason; 0. No, not at all, 1. Hardly ever, 2. Yes, sometimes, 3. Yes, very often”; “Item 5. I have felt scared or panicky for no very good reason; 0. No, not at all, 1. No, not much, 2. Yes, sometimes, 3. Yes, quite a lot”; “Item 6. Things have been getting on top of me; 0. No, I have been coping as well as ever, 1. No, most of the time I have coped quite well, 2. Yes, sometimes I haven't been coping as well as usual, 3. Yes, most of the time I haven't been able to cope”; “Item 7. I have been so unhappy that I have had difficulty sleeping; 0. No, not at all, 1. Not very often, 2. Yes, sometimes, 3. Yes, most of the time”; “Item 8. I have felt sad or miserable; 0 No, not at all, 1. Not very often, 2. Yes, quite often, 3. Yes, most of the time”; “Item 9. I have been so unhappy that I have been crying; 0. No, never, 1. Only occasionally, 2. Yes, quite often, 3. Yes, most of the time”; “Item 10. The thought of harming myself has occurred to me; 0. Never, 1. Hardly ever, 2. Sometimes, 3. Yes, quite often”. Two categorization processes were conducted to calculate the prevalence (absent vs. present; score = 0 vs. scores ≥1) and severity (non-severe vs. severe; scores ≤1 vs. scores ≥2) of each item. The Portuguese version of EPDS has good internal consistency [20,21]. In the cohorts assessed prior to the COVID-19 pandemic, Cronbach's α coefficient was 0.83 during pregnancy and 0.85 during the postpartum period. In the cohort assessed during the COVID-19 pandemic, Cronbach's α coefficient was 0.90 during pregnancy and 0.91 during the postpartum period. As recommended, a cut-off of 13 was used to identify women with clinically significant symptoms of depression [16].
2.3. Statistical analyses
Descriptive statistics were calculated to analyze the socio-demographic and clinical characteristics of participants. The estimated prevalence (scores ≥1) and severity (scores ≥2) of each depressive symptom were compared in the cohorts before and during the COVID-19 pandemic. Chi-square tests were performed to compare the prevalence of EPDS ≥13 in the cohorts before and during the COVID-19 pandemic. Two Multivariate Analyses of Covariance (MANCOVAs) and two Univariate Analyses of Covariance (UNIANCOVAs) were conducted to analyze the impact of the COVID-19 pandemic (before vs. during) on specific symptoms of depression during pregnancy and the postpartum period. As independent variables, the models included the period (before vs. during the COVID-19 pandemic) and the stage of pregnancy (early pregnancy –first and second trimester – vs. late pregnancy –third trimester) or stage of postpartum (early postpartum –until 12 weeks after childbirth– vs. late postpartum –>12 weeks after childbirth). The MANCOVA models included the 10 EPDS items as dependent variables, whereas the UNIANCOVA models included EPDS total score as the dependent variable. The models included potential sociodemographic, obstetric and health confounders (age, country of birth, education, marital status, employment status, history of mental health problems, parity, and risk pregnancy) as covariates.
Two-step logistic regressions were performed to analyze the impact of the COVID-19 pandemic on the prevalence of clinically significant symptoms of depression (EPDS ≥13) during pregnancy and the postpartum period. The first step (enter method) was performed to control potential sociodemographic, obstetric and health confounders. As independent variables, the second step included the variables of the first step, along with the period (before vs. during the COVID-19 pandemic), and stage of pregnancy (early pregnancy –first and second trimester – vs. late pregnancy –third trimester) or stage of postpartum (early postpartum –until 12 weeks after childbirth– vs. late postpartum –>12 weeks after childbirth) and clinically significant symptoms of depression (EPDS ≥13) as dependent variable.
Statistical significance was considered at p values < .05. Data were analysed with IBM SPSS 26.0 version (SPSS Inc., Chicago).
3. Results
3.1. Characteristics of participants
Table 1 shows the characteristics of participants by perinatal period: pregnancy vs. postpartum. Most pregnant women were 25 to 35 years old (63.0%); primiparous (78.3%); lived with their partner (85.3%); and about half had higher education (53.6%). Near one in four had experienced a mental health problem ever in life; 20.4% had a risk pregnancy; 28.5% were unemployed; and 8.7% were foreign-born. Most postpartum women were 25 to 35 years old (63.9%), primiparous (66.6%), and lived with their partner (88.0%), and about half had a higher education (57.6%). Near one in four had had a mental health problem ever in life, 21.2% had a risk pregnancy, 18.7% were unemployed, and 8.8% were foreign-born.
Table 1.
Participants' characteristics according to perinatal period, before and during the COVID-19 pandemic.
| Pregnancy |
Postpartum |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| COVID-19 pandemic |
COVID-19 pandemic |
||||||||
| Before |
During |
Total |
Before |
During |
Total |
||||
|
n = 1402 n (%) |
n = 748 n (%) |
N = 2150 N (%) |
p |
n = 993 n (%) |
n = 648 n (%) |
N = 1641 N (%) |
p | ||
| Age | ≤24 | 254 (18.5) | 36 (5.1) | 290 (14.0) | < 0.001 | 156 (15.9) | 24 (3.9) | 180 (11.2) | < 0.001 |
| 25–35 | 870 (63.5) | 438 (62.2) | 1308 (63.0) | 642 (65.2) | 382 (61.8) | 1024 (63.9) | |||
| ≥36 | 247 (18.0) | 230 (32.7) | 477 (23.0) | 186 (18.9) | 212 (34.3) | 398 (24.8) | |||
| Missing | 1371 | 704 | 2075 | 984 | 618 | 1602 | |||
| Country of birth | Native | 1252 (91.1) | 590 (91.6) | 1842 (91.3) | 0.714 | 893 (90.8) | 534 (92.1) | 1427 (91.2) | 0.374 |
| Foreign | 122 (8.9) | 54 (8.4) | 176 (8.7) | 91 (9.2) | 46 (7.9) | 137 (8.8) | |||
| Missing | 28 | 104 | 132 | 984 | 580 | 1564 | |||
| Education | ≤ 9 years of education | 356(26.0) | 7 (1.0) | 363(17.3) | < 0.001 | 235(23.9) | 8(1.3) | 243(15.0) | |
| 10–12 years of education | 443 (32.4) | 167 (22.8) | 610 (29.1) | 300 (30.5) | 145 (22.7) | 445 (27.5) | < 0.001 | ||
| Higher education1 | 569 (41.6) | 557 (76.2) | 1126 (53.6) | 447 (45.5) | 486 (76.1) | 933 (57.6) | |||
| Missing | 1368 | 731 | 2099 | 982 | 639 | 1621 | |||
| Employment status | Unemployed or other2 | 371 (27.1) | 232 (31.1) | 603 (28.5) | 0.051 | 231 (23.5) | 74 (11.5) | 305 (18.7) | < 0.001 |
| Employed | 997 (72.9) | 513 (68,9) | 1510 (71.5) | 752 (76.5) | 572 (88.5) | 1324 (81.3) | |||
| Missing | 1368 | 745 | 2113 | 983 | 646 | 1629 | |||
| Marital status | Married/cohabiting | 1100 (80.4) | 690 (94.4) | 1790 (85.3) | < 0.001 | 813 (82.9) | 613 (95.9) | 1426 (88.0) | < 0.001 |
| Other situation3 | 268 (19.6) | 41 (5.6) | 309 (14.7) | 168 (17.1) | 26 (4.1) | 194 (12.0) | |||
| Missing | 1368 | 731 | 2099 | 981 | 639 | 1620 | |||
| History of mental health problems | Yes4 | 326 (23.9) | 207 (28.0) | 533 (25.3) | 0.039 | 233 (23.7) | 180 (27.9) | 413 (25.4) | 0.059 |
| No | 1039 (76.1) | 533 (72.0) | 1572 (74.7) | 750 (78.3) | 466 (72.1) | 1216 (74.6) | |||
| Missing | 1365 | 740 | 2105 | 983 | 646 | 1629 | |||
| Parity | Nulliparous/Primiparous | 979 (70.3) | 628 (88.1) | 1607 (78.3) | < 0.001 | 723 (73.2) | 360 (56.3) | 1083 (66.6) | < 0.001 |
| Multiparous | 413 (29.7) | 85 (11.9) | 498 (23.7) | 265 (26.8) | 279 (43.7) | 544 (33.4) | |||
| Missing | 1392 | 713 | 2105 | 988 | 639 | 1627 | |||
| Risk pregnancy5 | Yes | 202(16.5) | 199(27.0) | 401(20.4) | < 0.001 | 156(15.9) | 178(29.9) | 334(21.2) | < 0.001 |
| No | 1025(83.5) | 538(73.0) | 1563(79.6) | 824(84.1) | 417(70.1) | 1241(78.8) | |||
| Missing | 175 | 11 | 186 | 13 | 53 | 66 | |||
Notes. 1bachelor, master's degree or postgraduate diploma2Other includes student/housewife3;Other situation includes single/separated/divorced/widow4;Any mental health problem ever in life5;Risk pregnancy includes age over 40 or gestational diabetes or hypertension or short cervix or other clinical condition; COVID-19 = coronavirus disease.
Both, pregnant and postpartum women assessed during the COVID-19 pandemic were more likely (ps < 0.001) to have clinically significant symptoms of depression (EPDS≥13; 24.3% and 28.2%, respectively), as compared to women assessed prior to the COVID-19 pandemic (9.0% and 6.9%, respectively).
Pregnant women assessed during the COVID-19 pandemic were more likely to be older, live with their partner, have a high education, be primiparous, have a history of mental health problem, and have a risk pregnancy, as compared to pregnant women assessed prior to the COVID-19 pandemic. Postpartum women assessed during the COVID-19 pandemic were more likely to be older, live with their partner, have a higher education, be multiparous, and have a risk pregnancy. In addition, they were less likely to be unemployed, as compared to postpartum women assessed prior to the COVID-19 pandemic.
3.2. Impact of the COVID-19 pandemic on specific symptoms of depression (EPDS items and total) during pregnancy and the postpartum period
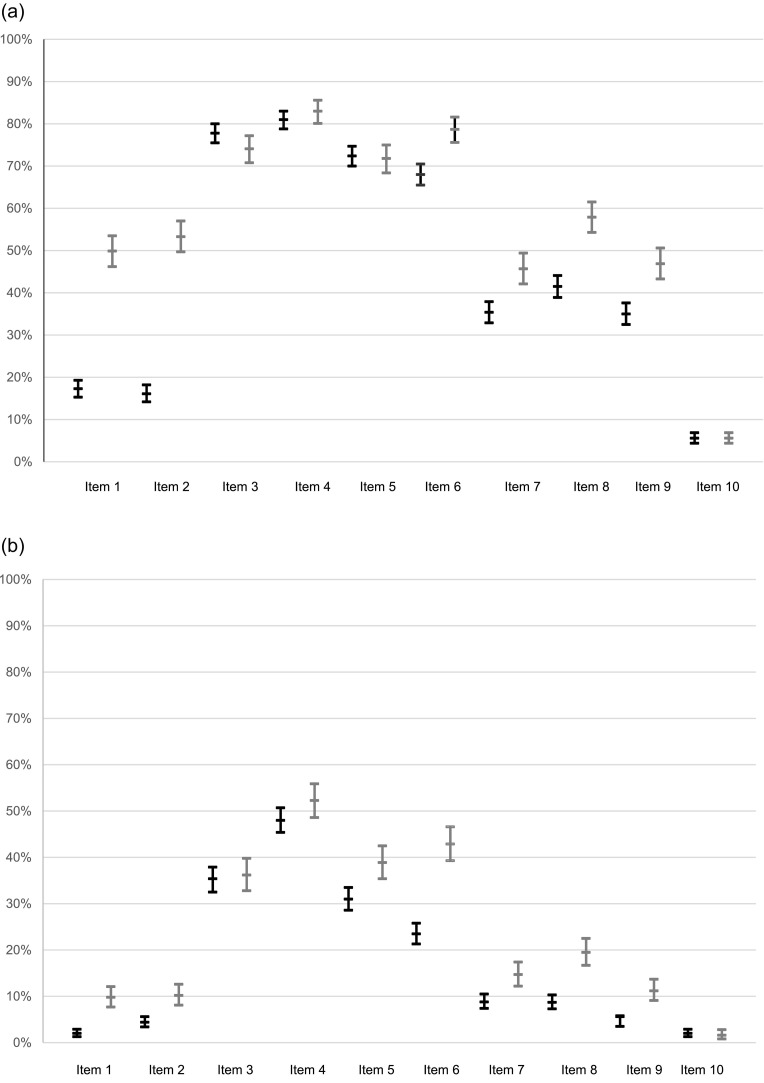
Supplementary Fig. 1 displays the proportion of answer options selected per EPDS item by pregnant women assessed before vs. during the COVID-19 pandemic. The estimated prevalence of symptoms of depression in pregnant women (scores ≥1; see Fig. 1a) was higher during the COVID-19 pandemic for all items, except for items 3, 5, and 10, as compared to the pre-pandemic period. The items which prevalence increased the most (>30%) were item 1 (32.6%) and item 2 (37.2%) during the COVID-19 pandemic (49.9% and 53.3%, respectively), as compared to the pre-pandemic period (17.3% and 16.1%, respectively). The severity of symptoms of depression (scores ≥2; see Fig. 1b) was higher in all items except for item 10. The highest increases in severity were observed in items 6 (19.4%) and 8 (10.8%) during the COVID-19 pandemic (42.9% and 19.5%, respectively), as compared to the pre-pandemic period (23.5% and 8.7%, respectively).
Fig. 1.
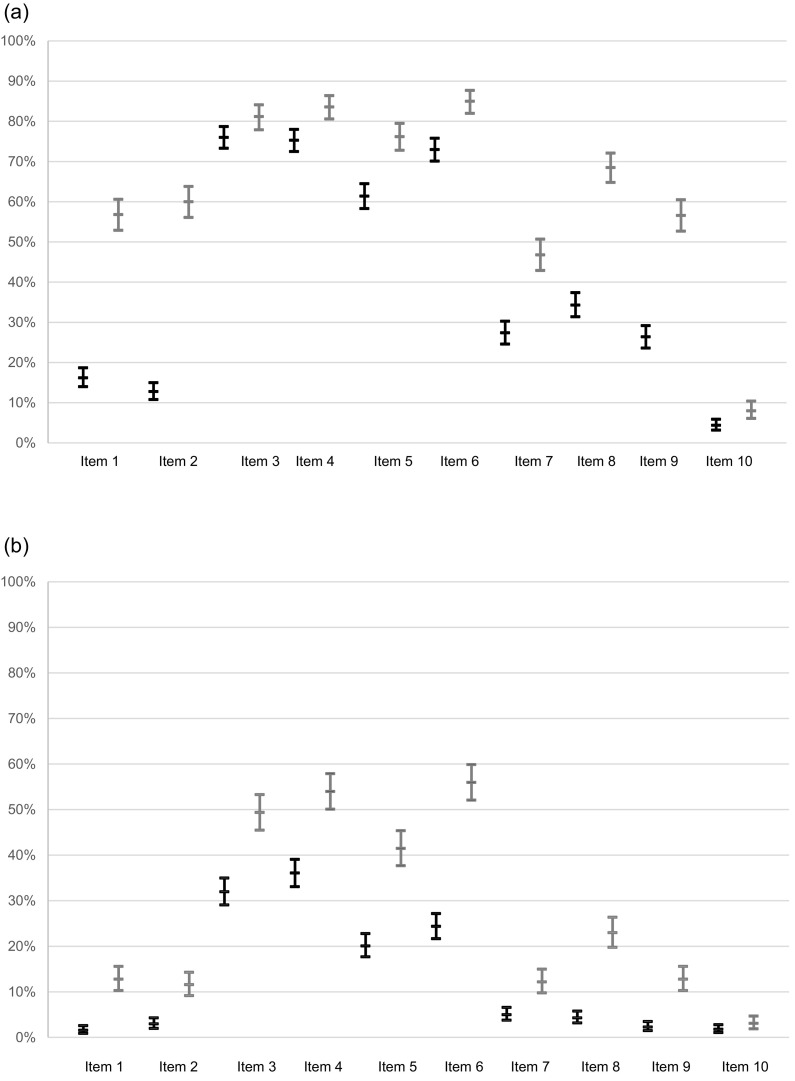
Estimates and 95% CI around the probability of having a depressive symptom (score ≥ 1) before (black) and after (grey) or a severe depressive symptom (score ≥ 2) before (black) and after (grey) the COVID-19 pandemic - Pregnancy.
Supplementary Fig. 2 displays the proportion of answer options selected per EPDS item by postpartum women before vs. during the COVID-19 pandemic. The estimated prevalence of symptoms of depression in postpartum women (scores ≥1; see Fig. 2a) was higher during the COVID-19 pandemic for all EPDS items, as compared to the pre-pandemic period. A > 40% increase was observed in the estimated prevalence of items 1 (40.6%) and 2 (47.2%), followed by a > 30% increase in items 8 (34.2%) and 9 (30.2%) during the pandemic (56.8%, 60.0%, 68.5%, and 56.6%, respectively), as compared to the pre-pandemic period (16.2%; 12.8%, 34.3%, and 26.4% respectively). The severity of symptoms of depression (scores ≥2; see Fig. 2b) was higher in all items during the COVID-19 pandemic. The highest increases in severity were observed in items 5 (21.4%) and 6 (31.6%) during the COVID-19 pandemic (41.5% and 56.0%, respectively), as compared to the pre-pandemic (20.1% and 24.4%, respectively).
Fig. 2.
Estimates and 95% CI around the probability of having a depressive symptom (score ≥ 1) before (black) and after (grey) or a severe depressive symptom (score ≥ 2) before (black) and after (grey) the COVID-19 pandemic - Postpartum.
Significant multivariate effects of the COVID-19 pandemic were found on symptoms of depression (EPDS items) during pregnancy, Wilk's Lambda = 0.86, F(10, 1789) = 28.89, p < .001, ɳp 2 = 0.14. Significant univariate effects of the COVID-19 pandemic were found on EPDS total score and all items, except for items 3 and 10. Pregnant women assessed during the COVID-19 pandemic reported more symptoms of depression, as compared to pregnant women assessed prior to the COVID-19 pandemic (see Table 2 ). Significant multivariate effects of the COVID-19 pandemic were found on symptoms of depression (EPDS items) during postpartum, Wilk's Lambda = 0.77, F(10, 1455) = 44.66, p < .001, ɳp 2 = 0.24. Results revealed significant univariate effects of the COVID-19 pandemic on all EPDS items and the total score. Postpartum women assessed during the COVID-19 pandemic reported more symptoms of depression compared to postpartum women assessed prior to the COVID-19 pandemic (see Table 2).
Table 2.
The impact of COVID-19 pandemic on specific symptoms of depression (EPDS items and total) during pregnancy and the postpartum period, adjusting for sociodemographic and health confounders.
| Pregnancy |
Postpartum |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 pandemic |
COVID-19 pandemic |
|||||||||
| Before n = 1402 |
During n = 748 |
Before n = 962 |
During n = 513 |
|||||||
| EPDS | M | SD | M | SD | F | M | SD | M | SD | F |
| Item 1. I have been able to laugh and see the funny side of things | 0.19 | 0.44 | 0.54 | 0.66 | 187.72*** | 0.17 | 0.42 | 0.71 | 0.71 | 211.28*** |
| Item 2. I have looked forward with enjoyment to things | 0.20 | 0.52 | 0.63 | 0.69 | 185.08*** | 0.15 | 0.44 | 0.74 | 0.70 | 337.06*** |
| Item 3. I have blamed myself unnecessarily when things go wrong | 1.15 | 0.82 | 1.15 | 0.88 | 1.47 | 1.10 | 0.80 | 1.40 | 0.92 | 32.55*** |
| Item 4. I have been anxious or worried for no good reason | 1.35 | 0.88 | 1.42 | 0.86 | 11.55** | 1.14 | 0.83 | 1.48 | 0.88 | 40.01*** |
| Item 5. I have felt scared or panicky for no very good reason | 1.06 | 0.85 | 1.13 | 0.91 | 7.21** | 0.83 | 0.78 | 1.26 | 0.91 | 63.40*** |
| Item 6. Things have been getting on top of me | 0.92 | 0.79 | 1.26 | 0.90 | 54.25*** | 0.99 | 0.76 | 1.51 | 0.87 | 77.98*** |
| Item 7. I have been so unhappy that I have had difficulty sleeping | 0.45 | 0.69 | 0.60 | 0.77 | 27.18*** | 0.32 | 0.58 | 0.59 | 0.74 | 50.95*** |
| Item 8. I have felt sad or miserable | 0.51 | 0.69 | 0.77 | 0.81 | 54.32*** | 0.39 | 0.58 | 0.94 | 0.80 | 175.05*** |
| Item 9. I have been so unhappy that I have been crying | 0.40 | 0.61 | 0.59 | 0.74 | 38.88*** | 0.29 | 0.52 | 0.71 | 0.73 | 128.17*** |
| Item 10. The thought of harming myself has occurred to me | 0.08 | 0.35 | 0.07 | 0.34 | 2.81 | 0.06 | 0.32 | 0.11 | 0.44 | 6.49* |
| Total | 6.30 | 4.28 | 8.20 | 5.74 | 75.62*** | 5.72 | 4.18 | 9.44 | 5.61 | 159.38*** |
Notes. Response options, Item 1. 0. As much as I always could, 1. Not quite so much now, 2. Definitely not so much now, 3. Not at all; Item 2. 0. As much as I ever did, 1. Rather less than I used to, 2. Definitely less than I used to, 3. Hardly at all; Item 3. 0. No, never, 1. Not very often, 2. Yes, some of the time, 3. Yes, most of the time; Item 4. 0. No, not at all, 1. Hardly ever, 2. Yes, sometimes, 3. Yes, very often; Item 5. 0. No, not at all, 1. No, not much, 2. Yes, sometimes, 3. Yes, quite a lot; Item 6. 0. No, I have been coping as well as ever, 1. No, most of the time I have coped quite well, 2. Yes, sometimes I haven't been coping as well as usual, 3. Yes, most of the time I haven't been able to cope; Item 7. 0. No, not at all, 1. Not very often, 2. Yes, sometimes, 3. Yes, most of the time; Item 8. 0 No, not at all, 1. Not very often, 2. Yes, quite often, 3. Yes, most of the time; Item 9. 0. No, never, 1. Only occasionally, 2. Yes, quite often, 3. Yes, most of the time; Item 10. 0. Never, 1. Hardly ever, 2. Sometimes, 3. Yes, quite often.
Models adjusted for age, country of birth, education, marital status, employment status, history of mental health problems, parity, and risk pregnancy.
3.3. Impact of the COVID-19 pandemic on the prevalence of clinically significant symptoms of depression (EPDS ≥ 13) during pregnancy and the postpartum period
The first step of the regression model for the prevalence of clinically significant symptoms of depression (EPDS ≥13) during pregnancy included potential sociodemographic, obstetric and health confounders. The model was statistically significant (χ2(9) = 61.79, p < .001), explained 3% to 6% of the variance in the prevalence of clinically significant symptoms of depression during pregnancy (Cox & Snell R 2= 0.03, Nagelkerke R 2 = 0.06), and correctly classified 86.2% of cases. The period (before vs. during the COVID-19 pandemic) and stage of pregnancy (early vs. late) were added in the second step of the model. The second step of the regression model was statistically significant (χ2(11) = 154.33, p < .001), explained 8% to 15% of the variance in the prevalence of clinically significant symptoms of depression during pregnancy (Cox & Snell R 2 = 0.08, Nagelkerke R 2 = 0.15), and correctly classified 86.6% of cases. Pregnant women assessed during the COVID-19 pandemic had higher odds of reporting clinically significant symptoms of depression, as compared to pregnant women assessed prior to the COVID-19 pandemic. Being foreign or having a low education level or a history of mental health problems increased the odds of reporting clinically significant symptoms of depression during pregnancy (see Table 3 ).
Table 3.
The impact of timing (before vs during COVID-19 pandemic) on the prevalence of clinically significant symptoms of depression (EPDS ≥13) during pregnancy and the postpartum period, adjusting for sociodemographic, obstetric, and health confounders.
| Pregnancy | β | Wald | p | OR | 95% CI |
|---|---|---|---|---|---|
| Step 1 | |||||
| Not married/cohabiting1 (ref. married/cohabiting) | 0.01 | 0.01 | 0.948 | 0.99 | 0.67–1.46 |
| Risk pregnancy2 (ref. normal pregnancy) | 0.25 | 2.10 | 0.147 | 0.78 | 0.56–1.09 |
| Foreign (ref. native) | 0.66 | 9.70 | 0.002 | 1.93 | 1.28–2.92 |
| Unemployed or other3 (ref. employed) | 0.48 | 10.12 | 0.001 | 1.62 | 1.20–2.18 |
| ≤ 9 years of education (ref. higher education4) | 0.21 | 0.94 | 0.332 | 0.81 | 0.53–1.24 |
| 10–12 years of education (ref. higher education4) | 0.22 | 1.69 | 0.193 | 1.24 | 0.90–1.72 |
| Any mental health problem ever in life (ref. no) | 0.81 | 30.38 | < 0.001 | 0.45 | 0.34–0.60 |
| ≤ 24 years old (ref. >33 years old) | 0.16 | 0.37 | 0.541 | 1.17 | 0.71–1.93 |
| 25–33 years old (ref. >33 years old) | −0.18 | 1.10 | 0.294 | 0.84 | 0.60–1.17 |
| Step 2 | |||||
| Not married/cohabiting1 (ref. married/cohabiting) | 0.29 | 1.76 | 0.185 | 1.33 | 0.87–2.03 |
| Risk pregnancy2 (ref. normal pregnancy) | 0.04 | 0.06 | 0.814 | 0.96 | 0.68–1.36 |
| Foreign (ref. native) | 0.81 | 13.06 | < 0.001 | 2.25 | 1.45–3.48 |
| Unemployed or other3 (ref. employed) | 0.28 | 3.22 | 0.073 | 1.33 | 0.97–1.81 |
| ≤ 9 years of education (ref. higher education4) | 0.82 | 10.30 | < 0.001 | 2.27 | 1.38–3.75 |
| 10–12 years of education (ref. higher education4) | 0.55 | 9.77 | 0.002 | 1.74 | 1.23–2.46 |
| Any mental health problem ever in life (ref. no) | 0.73 | 22.82 | < 0.001 | 0.48 | 0.36–0.65 |
| ≤ 24 years old (ref. >33 years old) | 0.32 | 1.45 | 0.228 | 1.38 | 0.82–2.34 |
| 25–33 years old (ref. >33 years old) | −0.06 | 0.12 | 0.725 | 0.94 | 0.67–1.33 |
| During COVID-19 pandemic (ref. before) | 1.60 | 81.35 | < 0.001 | 0.20 | 0.14–0.29 |
| Early pregnancy5 (ref. late pregnancy6) | 0.36 | 4.91 | 0.027 | 0.70 | 0.51–0.96 |
| Postpartum | β | Wald | p | OR | 95% CI |
| Step 1 | |||||
| Not married/cohabiting1 (ref. married/cohabiting) | 0.06 | 0.06 | 0.807 | 0.94 | 0.57–1.56 |
| Risk pregnancy2 (ref. normal pregnancy) | 0.42 | 5.54 | 0.019 | 1.52 | 1.07–2.16 |
| Foreign (ref. native) | 0.54 | 4.84 | 0.028 | 1.71 | 1.06–2.77 |
| Unemployed or other3 (ref. employed) | 0.26 | 1.38 | 0.240 | 0.77 | 0.50–1.19 |
| ≤ 9 years of education (ref. higher education4) | 0.95 | 12.13 | < 0.001 | 0.39 | 0.23–0.66 |
| 10–12 years of education (ref. higher education4) | 0.43 | 4.99 | 0.026 | 0.65 | 0.44–0.95 |
| Any mental health problem ever in life (ref. no) | 0.95 | 33.28 | < 0.001 | 0.39 | 0.28–0.53 |
| ≤ 24 years old (ref. >33 years old) | 0.54 | 2.70 | 0.100 | 1.72 | 0.90–3.27 |
| 25–33 years old (ref. >33 years old) | 0.19 | 1.00 | 0.317 | 1.21 | 0.84–1.74 |
| Step 2 | |||||
| Not married/cohabiting1 (ref. married/cohabiting) | 0.35 | 1.56 | 0.212 | 1.42 | 0.82–2.44 |
| Risk pregnancy2 (ref. normal pregnancy) | 0.18 | 0.94 | 0.332 | 1.20 | 0.83–1.74 |
| Foreign (ref. native) | 0.70 | 7.03 | 0.008 | 2.01 | 1.20–3.36 |
| Unemployed or other3 (ref. employed) | 0.14 | 0.36 | 0.547 | 0.87 | 0.55–1.38 |
| ≤ 9 years of education (ref. higher education4) | 0.11 | 0.12 | 0.734 | 1.12 | 0.60–2.09 |
| 10–12 years of education (ref. higher education4) | 0.13 | 0.43 | 0.513 | 0.87 | 0.59–1.31 |
| Any mental health problem (ref. no) | 0.85 | 24.04 | < 0.001 | 0.43 | 0.30–0.60 |
| ≤ 24 years old (ref. >33 years old) | 0.84 | 5.71 | 0.017 | 2.32 | 1.16–4.61 |
| 25–33 years old (ref. >33 years old) | 0.41 | 4.34 | 0.037 | 1.50 | 1.03–2.21 |
| During COVID-19 pandemic (ref. before) | 1.97 | 89.76 | < 0.001 | 7.14 | 4.75–10.72 |
| Early postpartum7 (ref. late postpartum8) | 0.09 | 0.25 | 0.616 | 0.92 | 0.65–1.29 |
Notes. COVID-19, coronavirus disease; EPDS, Edinburgh Postnatal Depression Scale; OR, odds ratio; CI, Confidence interval1;Includes single/separated/divorced/widow2;Risk pregnancy includes age over 40 or gestational diabetes or hypertension or short cervix or other clinical condition3;Other includes student/housewife; 4bachelor, master's degree or postgraduate diploma; 5first and second pregnancy trimester; 6third pregnancy trimester; 7until 12 weeks after childbirth8; >12 weeks after childbirth.
Models adjusted for age, country of birth, education, marital status, employment status, history of mental health problems, parity, and risk pregnancy.
The first step of the regression model for the prevalence of clinically significant symptoms of depression (EPDS ≥13) during the postpartum period included potential sociodemographic, obstetric and health confounders. The model was statistically significant (χ2(9) = 54.02, p < .001), explained 4% to 7% of the variance in the prevalence of clinically significant symptoms of depression during the postpartum period (Cox & Snell R 2= 0.04, Nagelkerke R 2 = 0.07) and correctly classified 86.2% of cases. The period (before vs. during the COVID-19 pandemic) and stage of postpartum (early vs. late) were added in the second step. The second step was statistically significant (χ2(11) = 165.58, p < .001), explained 11% to 19% of the variance in the prevalence of clinically significant symptoms of depression during the postpartum period (Cox & Snell R 2 = 0.11, Nagelkerke R 2 = 0.19), and correctly classified 86.1% of cases. Postpartum women assessed during the COVID-19 pandemic had higher odds of reporting clinically significant symptoms of depression, as compared to postpartum women assessed prior to the COVID-19 pandemic. A foreign nationality, a history of mental health problems, and a young age increased the odds of reporting clinically significant symptoms of depression during the postpartum period (see Table 3).
4. Discussion
4.1. Main findings
This study provides evidence that pregnant/postpartum women during the COVID-19 pandemic had higher odds of reporting clinically significant symptoms of depression, as compared to pregnant/postpartum women assessed prior to the COVID-19 pandemic. The increased prevalence of clinically significant symptoms of depression during the COVID-19 pandemic can be due to a significantly higher prevalence and severity of specific core depressive and anhedonia-related symptoms, as assessed on the EPDS.
Additionally, being foreign or having a history of mental health problems increased the odds of having clinically significant symptoms of depression during pregnancy/postpartum. A low education only increased the odds of having clinically significant depressive symptoms during pregnancy, whereas a young age only increased the odds during the postpartum period.
During the COVID-19 pandemic, the number and severity of symptoms of depression during pregnancy and the postpartum period was considerably higher, as compared to the pre-pandemic period.
4.2. Prevalence of clinically significant symptoms of depression
Our data show that about one in four pregnant women obtained a score ≥ 13 on the EPDS and this prevalence was even higher in the postpartum period. Lower prevalence rates have been reported in Switzerland and the Netherlands, whereas higher prevalence rates have been reported in the UK, and similar in Ireland [11]. Importantly, the increase observed in the prevalence and severity of depressive symptoms during the pandemic was more remarkable during postpartum, as compared to the pregnancy period (21.3% vs. 15.3%, respectively). This finding suggests a higher burden of the COVID-19 pandemic on the mental health of women during the postpartum period.
4.3. Prevalence of symptoms of depression
Important increases were observed in the prevalence of difficulties in being able to laugh and see the funny side of things (item 1, pregnancy 32.6%, postpartum 40.6%); looking forward with enjoyment to things (item 2, pregnancy 37.2%, postpartum 47.2%); feeling sad/miserable in the postpartum period (item 8, 34.2%); and unhappiness leading to crying in the postpartum period (item 9, 30.2%). The last two symptoms are core symptoms of depression, whereas the first two symptoms have been previously classified as anhedonia-related symptoms [17,18,22] and refer to the inability to feel pleasure in normally pleasurable activities. The increases in the prevalence of core symptoms of depression and anhedonia-related symptoms may be related to non-pharmaceutical interventions (including containment and closure policies) implemented by governments to contain the COVID-19 outbreak [23,24]. These measures had a huge impact on daily routines and prevented engagement in pleasurable activities, particularly those that involved social contact, which resulted in social isolation. In Portugal, within the study period, the Portuguese “lockdown style” was quite strict, with a high median stringency index (index varies from 0 to 100; 100 = strictest [23]) (71.30; P25-P75: 71.30–72.69; Min-Max: 63.43–74.54). This high stringency index indicates that social contact was substantially restricted in the population. Preventive measures included containment and closure policies such as school and workplace closure, cancellation of public events, restrictions on gatherings, closure of public transport, stay-at-home measures, restrictions on internal movements, or border restriction [23], which led to increased social isolation.
The prevalence of anxiety-related symptoms (items 3 to 5: self-blame, anxious/worried, scared panicky) remained steadily. Those symptoms were the most prevalent in the pre-pandemic. During the COVID-19 pandemic, these symptoms remained the most prevalent along with the core depression symptom of overwhelmed (item 6), both during pregnancy and the postpartum period. This finding suggests that the symptoms that were already the most prevalent in women assessed prior to the COVID-19 pandemic may be less prone to variability resulting from contextual changes.
4.4. Severity of symptoms of depression
The severity of symptoms of depression also increased significantly during the COVID-19 pandemic, especially concerning core-symptoms of depression of feeling overwhelmed –“things have been getting on top of me”– during pregnancy and the postpartum period (item 6, pregnancy 19.4%, postpartum 31.6%), and sadness during pregnancy –“I have felt sad or miserable” (item 8, 10.8%)–, as well as the anxiety-related symptom of feeling scared/panicky in the postpartum period (item 5, 21.4%). During pregnancy, severity increased most significantly in two core symptoms of depression (items 6 and 8), whereas in the postpartum period, the highest increases were observed in a core-depressive symptom and an anxiety-related symptom (items 5 and 6).
The feeling of overwhelm during pregnancy and the postpartum might be associated with the significant proportion of Portuguese women reporting difficulties in accessing routine antenatal care (49.2%) and the reduced overall quality of maternal and neonatal care during the COVID-19 pandemic (47.3%) [25]. These concerns added to worries about the lack of social support (e.g., restrictions on visits) [26] resulting from non-pharmaceutical interventions (movement restrictions and stay-at-home requirements). These restrictions may have resulted in isolation and deprivation from the social support that is usually provided to women by relatives and friends around the postpartum period. A previous study showed that support from healthcare providers is associated with lower symptoms of depression [27]. Feeling scared in the postpartum period might be driven by increased worries about the infant and medical care, including the possibility that the infant will be infected with SARS-CoV-2.
The proportion of pregnant women that had feelings of scariness or panic without a reason and of pregnant or postpartum women that had feelings of unnecessary blame or self-harm did not increase in the COVID-19 pandemic compared to before. The first two symptoms are anxiety-related components of depression [17,18,22]. These results suggest that the COVID-19 pandemic had a higher impact on symptoms of depression, as compared to anxiety-related symptoms in the perinatal period.
Finally, the severity of anxiety-related symptoms did not increase during the COVID-19 pandemic. Those symptoms (e.g., self-blame, anxious/worried, scared panicky) were the most severe both before and during the COVID-19 pandemic, along with the core depressive symptom of feeling overwhelmed, both in pregnant and postpartum women.
4.5. Factors associated with the prevalence of clinically significant symptoms of perinatal depression during the COVID-19 pandemic
Overall, pregnant/postpartum women assessed during the COVID-19 pandemic had higher odds of reporting clinically significant symptoms of depression, as compared to those assessed prior to the COVID-19 pandemic, which is consistent with previous evidence [3,9]. This is a major and serious public health concern, in the light that 60% of antenatal or postnatal mental health services were disrupted during the COVID-19 pandemic [2]. Untreated perinatal mental health problems have adverse consequences for children [28]. The finding that a young age, being foreign, a low education level or a history of mental health problems increase the risk for reporting clinically significant symptoms of depression during pregnancy and/or the postpartum period during the COVID-19 pandemic is consistent with previous reports [29]. Awareness should be raised about the mental health needs of the most vulnerable groups of women during the perinatal period. This would greatly contribute to the implementation of priority policies and promote the readiness of mental health services during the perinatal period in a context of crisis.
4.6. Strengths and limitations
The EPDS was used to assess symptoms of depression during pregnancy and the postpartum period. Since it is one of the most widely used self-reported measures to assess perinatal symptoms of depression [16], it allows comparison with other studies. Considering the normative sociodemographic characteristics of the sample, generalization of findings to other populations should be dealt with caution.
Significant differences were found between the cohort of women assessed during the COVID-19 pandemic and the cohort women assessed prior to the COVID-19 pandemic. However, these differences were controlled in the statistical analysis to examine the impact of the COVID-19 pandemic on perinatal symptoms of depression.
4.7. Implications for clinical practice and research
A variety of reliable short versions of the EPDS have been developed [e.g. [30,31]] in order to increase the cost-effectiveness of mental health screening plans. The significant increase in the prevalence and severity of specific depressive symptoms during the COVID-19 pandemic raises concerns on the adequacy of using shortened EPDS versions during future contexts of crisis. For instance, items 5 and 6 were removed in some validated shortened versions of the EPDS [e.g. [31,32]]. However, these items represent symptoms which severity increases in situations of crisis, especially in the postpartum period. Clinicians should be aware that the use of shortened versions of the EPDS may lead to the underestimation of perinatal mental health problems. This may occur as short versions of the EPDS do not assess the symptoms which prevalence and severity increase the most during situations of crisis or when social isolation is required for any reason. Additionally, the administration of shortened versions prevents perinatal mental healthcare services from becoming aware of the occurrence of symptoms of depression in contexts of crisis or social isolation. This limitation results in health services failing to provide adequate screening, monitoring, and health care services, including strategies for reducing social isolation and improving social support, according to the specific needs of women during pregnancy or the postpartum period. We identified vulnerable groups that need the clinicians' special attention in terms of perinatal mental health. Maternal and neonatal health care services should be aware that women who are young, foreign or have a history of mental health problems or a low education level, have higher odds of developing mental health problems. Therefore, screening for mental health problems is of foremost importance to overcome inequities in health care. Funding for mental health and psychosocial support is scarce and antenatal or postnatal mental health services were disrupted during the COVID-19 pandemic [2]. At the same time our study showed that perinatal mental health worsened. If used wisely, the evidence provided in this study may contribute to improving the quality of mental healthcare by targeting and monitoring vulnerable groups using cost-effective tools.
5. Conclusion
The COVID-19 pandemic had an impact on the prevalence and severity of specific symptoms of depression, as well as on the prevalence of clinically significant symptoms of depression during the perinatal period. These deleterious effects were mainly due to the significantly higher prevalence and severity of core depressive and anhedonia-related symptoms. Our results suggest that clinical attention should be focused on the specific symptoms of depression that these women experience, in order to improve screening and treatment in this and future pandemics. The use of appropriate tools that assess a broad range of symptoms and address vulnerable groups is key to improving mental health care during current and future situations of crisis.
Financial disclosure statement
The authors have no financial relationships relevant to this article to disclose.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Funding sources
This study was and supported by the Psychology Research Centre (UID/PSI/01662/2013), University of Minho, by the Portuguese Foundation for Science and Technology and the Portuguese Ministry of Education and Science through national funds and co-financed by FEDER through COMPETE2020 under the PT2020 Partnership Agreement, under the Grant No. POCI-01-0145-FEDER- 007653. This research was supported by the FEDER Funds through the Programa Operacional Factores de Competitividade (COMPETE) and by National Funds through FCT (Fundação para a Ciência e a Tecnologia) under the Grant No. PTDC/SAU/SAP/116738/2010.
Fundação Bial, under the project with the reference 157/12 and by the FCT– Fundação para a Ciência e a Tecnologia, I.P., under the projects PTDC/PSI-PCL/119152/2010, HEI-Lab R&D Unit UIDB/05380/2020, UIDB/04750/2020, and LA/P/0064/2020. It was supported by FEDER through COMPETE2020 under the PT2020 Partnership Agreement (POCI-01-0145-FEDER-007653). Raquel Costa was supported by the FSE and FCT under the Post-Doctoral Grant SFRH/BPD/117597/2016 [RC]. Tiago Miguel Pinto [TMP] was supported by the FSE and FCT under the individual grant SFRH/BD/115048/2016. Ana Conde was supported a doctoral grant for Science in Measure IV.3 and co-funded under the 2010 Science and Innovation Operational Program (POCI 2010) from Science and Technology Foundation, Government of the Portuguese Republic (Ref. SFRH/BD/13768/2003) [AC].
Ana Mesquita is supported from the Portuguese Foundation for Science and Technology (FCT) and from EU through the European Social Fund and from the Human Potential Operational Program - IF/00750/2015.
This article is based upon work from COST Action CA18138 “Research Innovation and Sustainable Pan-European Network in Peripartum Depression Disorder” (Riseup-PPD), supported by COST (European Cooperation in Science and Technology; https://www.cost.eu/).
The funders had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author statement
I declare that I participated in the design, execution, and analysis of the paper by Costa and colleagues entitled “Women's perinatal depression: Anhedonia-related symptoms have increased in the COVID-19 pandemic“, that I have seen and approved the final version and that it has neither been published nor submitted elsewhere. I also declare that I have no conflict of interest, other than any noted in the covering letter to the editor.
Role of the funding source
The funders had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author contributions
Costa and Pinto had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: RC TP AC BF; Acquisition, analysis, or interpretation of data: RC TP AC BF AM EM; Drafting of the manuscript: RC TP AC; Critical revision of the manuscript for important intellectual content: RC TP AC BF AM EM; Statistical analysis: RC TP; Obtained funding: RC AC BF AM.
Declaration of Competing Interest
None.
Acknowledgements
We acknowledge the assistance of the psychologists and other professionals who were involved in the data collection.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.genhosppsych.2023.06.007.
Appendix A. Supplementary data
Supplementary material
Data availability
Data will be made available on request.
References
- 1.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Geneva World Health Organization Licence: CC BY-NC-SA 3.0. 2020. The impact of COVID-19 on mental, neurological and substance use services: results of a rapid assessment. [Google Scholar]
- 3.Chmielewska B., Barratt I., Townsend R., Kalafat E., van der Meulen J., Gurol-Urganci I., et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9(6):e759–e772. doi: 10.1016/S2214-109X(21)00079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woody C.A., Ferrari A.J., Siskind D.J., Whiteford H.A., Harris M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86–92. doi: 10.1016/j.jad.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Alves S., Fonseca A., Canavarro M.C., Pereira M. Dyadic coping and dyadic adjustment in couples with women with high symptoms of depression during pregnancy. Journal of Reproductive & Infant Psychology. 2018;36(5):504–518. doi: 10.1080/02646838.2018.1490496. [DOI] [PubMed] [Google Scholar]
- 6.Teixeira C., Figueiredo B., Conde A., Pacheco A., Costa R. Anxiety and depression during pregnancy in women and men. J Affect Disord. 2009;119(1–3):142–148. doi: 10.1016/j.jad.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Figueiredo B., Conde A. Anxiety and depression in women and men from early pregnancy to 3-months postpartum. Arch Womens Ment Health. 2011;14(3):247–255. doi: 10.1007/s00737-011-0217-3. [DOI] [PubMed] [Google Scholar]
- 8.Marques R., Monteiro F., Canavarro M.C., Fonseca A. The role of emotion regulation difficulties in the relationship between attachment representations and depressive and anxiety symptoms in the postpartum period. J Affect Disord. 2018;238:39–46. doi: 10.1016/j.jad.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Chrzan-Dętkoś M., Walczak-Kozłowska T., Lipowska M. The need for additional mental health support for women in the postpartum period in the times of epidemic crisis. BMC Pregnancy Childbirth. 2021;21(1):114. doi: 10.1186/s12884-021-03544-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mateus V., Cruz S., Costa R., Mesquita A., Christoforou A., Wilson C.A., et al. Rates of depressive and anxiety symptoms in the perinatal period during the COVID-19 pandemic: comparisons between countries and with pre-pandemic data. J Affect Disord. 2022;316:245–253. doi: 10.1016/j.jad.2022.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ceulemans M., Foulon V., Ngo E., Panchaud A., Winterfeld U., Pomar L., et al. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic-A multinational cross-sectional study. Acta Obstet Gynecol Scand. 2021;100(7):1219–1229. doi: 10.1111/aogs.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hendrick V., Altshuler L., Strouse T., Grosser S. Postpartum and nonpostpartum depression: differences in presentation and response to pharmacologic treatment. Depress Anxiety. 2000;11(2):66–72. doi: 10.1002/(SICI)1520-6394(2000)11:2<66::AID-DA3>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 13.Kumar R., Robson K.M. A prospective study of emotional disorders in childbearing women. Br J Psychiatry. 1984;144(1):35–47. doi: 10.1192/bjp.144.1.35. [DOI] [PubMed] [Google Scholar]
- 14.Pitt B. “Atypical” depression following childbirth. Br J Psychiatry. 1968;114(516):1325–1335. doi: 10.1192/bjp.114.516.1325. [DOI] [PubMed] [Google Scholar]
- 15.Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 16.Levis B., Negeri Z., Sun Y., Benedetti A., Thombs B.D., DEPRESsion Screening Data (DEPRESSD) EPDS Group Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ (Clinical Research ed) 2020;371 doi: 10.1136/bmj.m4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lautarescu A., Victor S., Lau-Zhu A., Counsell S.J., Edwards A.D., Craig M.C. The factor structure of the Edinburgh Postnatal Depression Scale among perinatal high-risk and community samples in London. Arch Womens Ment Health. 2021 doi: 10.1007/s00737-021-01153-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tuohy A., McVey C. Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. Br J Clin Psychol. 2008;47(Pt 2):153–169. doi: 10.1111/j.2044-8260.2008.tb00463.x. [DOI] [PubMed] [Google Scholar]
- 19.Omitted reference for blinded review.
- 20.Figueiredo B., Canário C., Tendais I., Pinto T.M., Kenny D.A., Field T. Couples' relationship affects mothers' and fathers' anxiety and depression trajectories over the transition to parenthood. J Affect Disord. 2018;238(10):204–212. doi: 10.1016/j.jad.2018.05.064. [DOI] [PubMed] [Google Scholar]
- 21.Figueiredo B., Conde A. Anxiety and depression symptoms in women and men from early pregnancy to 3-months postpartum: parity differences and effects. J Affect Disord. 2011;132(1–2):146–157. doi: 10.1016/j.jad.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 22.Petrozzi A., Gagliardi L. Anxious and depressive components of Edinburgh Postnatal Depression Scale in maternal postpartum psychological problems. J Perinat Med. 2013;41(4):343–348. doi: 10.1515/jpm-2012-0258. [DOI] [PubMed] [Google Scholar]
- 23.Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., et al. A global panel database of pandemic policies (Oxford COVID-19 government response tracker) Nat Hum Behav. 2021;5(4):529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 24.Kucharski A.J., Klepac P., Conlan A., Kissler S.M., Tang M.L., Fry H., et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis. 2020;20(10):1151–1160. doi: 10.1016/S1473-3099(20)30457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lazzerini M., Covi B., Mariani I., Drglin Z., Arendt M., Hersoug Nedberg I., et al. Quality of facility-based maternal and newborn care during the COVID-19 pandemic: a multicountry cross-sectional study in the WHO European region investigating service users' perspectives. Lancet Regional Health – Europe. 2021;3 doi: 10.1016/j.lanepe.2021.100268. [DOI] [Google Scholar]
- 26.Basu A., Kim H.H., Basaldua R., Choi K.W., Charron L., Kelsall N., et al. A cross-national study of factors associated with women's perinatal mental health and wellbeing during the COVID-19 pandemic. PloS One. 2021;16(4) doi: 10.1371/journal.pone.0249780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ostacoli L., Cosma S., Bevilacqua F., Berchialla P., Bovetti M., Carosso A.R., et al. Psychosocial factors associated with postpartum psychological distress during the Covid-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703. doi: 10.1186/s12884-020-03399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gentile S. Untreated depression during pregnancy: short- and long-term effects in offspring. A systematic review. Neuroscience. 2017;342:154–166. doi: 10.1016/j.neuroscience.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 29.Liu C.H., Erdei C., Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 pandemic. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi S.K., Kim J.J., Park Y.G., Ko H.S., Park I.Y., Shin J.C. The simplified Edinburgh Postnatal Depression Scale (EPDS) for antenatal depression: is it a valid measure for pre-screening? Int J Med Sci. 2012;9(1):40–46. doi: 10.7150/ijms.9.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harel D., Levis B., Ishihara M., Levis A.W., Vigod S.N., Howard L.M., et al. Shortening the Edinburgh postnatal depression scale using optimal test assembly methods: development of the EPDS-Dep-5. Acta Psychiatr Scand. 2021;143(4):348–362. doi: 10.1111/acps.13272. [DOI] [PubMed] [Google Scholar]
- 32.Eberhard-Gran M., Eskild A., Samuelsen S.O., Tambs K. A short matrix-version of the Edinburgh Depression Scale. Acta Psychiatr Scand. 2007;116(3):195–200. doi: 10.1111/j.1600-0447.2006.00934.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
Data will be made available on request.