ABSTRACT
Purposes
To compare the effectiveness of instrument-assisted soft tissue mobilization (IASTM) and pressure algometry with sham ultrasound (control group) on the clinical measures of headache, pressure pain threshold (PPT) of upper trapezius and suboccipital muscles and cervical alignment in patients with tension type headache (TTH).
Methods
Seventy-two patients with TTH of both genders were randomly allocated to 3 experimental groups: a) the IASTM group (n=24), b) pressure algometry group (n=24), and c) sham ultrasound control group (n=24). Headache frequency and disability, pressure pain threshold of upper trapezius and suboccipital muscles, cervical lordosis angle (CA) and anterior head translation (AHT) were measured four weeks before and after intervention. Moreover, headache frequency was followed up for two more weeks after intervention.
Results
Statistically significant improvements (P <0.05; effect size ranges 1.1-1.9) were observed in all outcome measures following IASTM compared to the other two intervention methods. In the IASTM group, the headache frequency decreased from 15 to 2 days/month. Also, headache disability decreased from 19 to 10. Further, CA increased from 17.5° to 31.4° and AHT decreased from 24.1 to 15.5 mm. The pressure algometry group showed significantly lower headache frequency at the follow-up (P < 0.01) than the sham ultrasound control group. However, Similar findings in the other evaluated outcomes were found between the pressure algometry and sham ultrasound control groups (P ˃ 0.05).
Conclusion
The results of the present study indicate the effectiveness of IASTM in improving headache symptoms and cervical alignment in patients with TTH.
KEYWORDS: Cervical alignment, instrument-assisted soft tissue mobilization, manual therapy, myofascial trigger points, Tension-type headache
Introduction
Tension-type headache (TTH) is the most globally prevalent primary headache disorder [1]. TTH leads to reduced work productivity [2], social participation [3], and quality of life [4]. This disorder is usually described as a particular type of musculoskeletal disorder [5] presented with chronic and diffuse pain, which originates from a hyperactive neck and pericranial muscles [6].
It has previously been observed that in TTH, active MTrPs were found in upper trapezius, sternocleidomastoid, temporalis, and suboccipital muscles [7,8]. Additionally, forward head posture (FHP) has been related to chronic TTH [9,8]. Further, a vast majority of patients with TTH were found to have straightened cervical spine as revealed by x-ray studies [10]. Thus, the suggested linkage between abnormal cervical posture and headache has been reported in TTH.
Manual therapy is commonly used in clinical settings to ameliorate TTH-related symptoms. Recently, a systematic review showed that manual therapy achieved positive outcomes in pain intensity and frequency, disability, impact of headache, quality of life, and craniocervical range of motion in adults with TTH [11].
In physiotherapy, a large variety of manual therapy treatments are used [12]. Instrument-assisted soft tissue mobilization (IASTM) is a type of manual deep soft tissue mobilization [13]. IASTM uses ergonomically designed instruments to effectively locate and treat myofascial restrictions in addition to delivering a mobilizing effect to the soft tissue for reducing pain and enhancing the range of motion [14]. Lately, IASTM has been used as an accepted alternative to traditional manual therapy [15]; as the strokes applied during IASTM differ in direction, force, and pattern and helps in dispersing pressure to the underlying tissues [16].
Previous studies examined the impact of IASTM on individuals with musculoskeletal pathology [17,18], [19,20], but not in TTH. A recent systematic review provided moderate supportive evidence regarding the use of IASTM in improving pain and function in an injured population [15]. However, more methodologically robust studies on different patient populations and IASTM products are warranted to validate and generalize these findings.
The pressure algometer is an objective and clinically feasible device that has been used as a treatment for myofascial trigger points (MTrPs) [21–23]. The mechanical stimulus delivered by this application provides controlled pressure on MTrPs [21] and may reduce the hazards of work-related musculoskeletal injuries associated with manual techniques [24]. To date, there are only a few studies that investigated the use of pressure algometer on MTrPs of the upper trapezius compared to sham ultrasound (control group) [21,23]. However, the use of pressure algometer application in TTH patients has not been examined before.
Thus, the purpose of this study was to compare the effectiveness of IASTM and pressure algometry intervention with sham ultrasound (control group) on the clinical measures of headache, MTrPs pressure threshold, and cervical alignment in patients with TTH.
Methods
This study was carried out at the Outpatient Physical Therapy Department, El Gomhorya Hospital from April to December 2019 and approved by the local ethics committee of the Faculty of Physical Therapy, Cairo University (P.T.REC/012/002178) and was registered in Pan African Clinical Trial Registry
(PACTR201901674453376).
Design of the study
A three-armed parallel-group randomized controlled trial.
Participants
A convenient sample of 72 patients with clinically diagnosed TTH participated in this study. Participants of both genders with an age range of 28–52 years were recruited by word of mouth. The diagnosis was conducted according to the International Classification of Headache Disorders (ICHD), 3rd edition [25]. Participants had to describe typical pain features of TTH: bilateral location, pressing or tightening pain, moderate-intensity (≤6.5 on a 10-point numerical pain rate scale, NPRS), and no aggravation of pain during physical activity. According to the ICHD-III criteria, patients also had to report no more than one symptom including photophobia, phonophobia, nausea, or vomiting. Also, patients diagnosed with chronic TTH lasting longer than 3 months were included [25].
The excluded patients from the study were: those who were taking antipsychotic or antidepressant medications, patients with other primary headaches as migraine or secondary headaches as medication overuse headache, those with a history of head or neck trauma [i.e. whiplash), cervical herniated disk or cervical osteoarthritis, and any systemic degenerative disease such as rheumatoid arthritis and lupus erythematosus were also excluded.
All included participants were informed about the research purpose and agreed to participate, and then they signed a written informed consent.
Procedures
For MTrPs identification, participants were screened by a licensed, experienced clinical physiotherapist with 15 years of clinical experience in manual physical therapy. MTrPs detection was done as per the work of [26]. A minimum of one active MTrP in the addressed bilateral muscles (upper trapezius and suboccipital muscles) had to be identified.
Interventions
All patients received hot packs over the target muscles for 10 minutes at the beginning. Then, stretching exercises followed by multi-directional strengthening exercises were done for upper trapezius and suboccipital muscles.
(Group A): IASTM technique
For the application of IASTM, the participant was comfortably seated and rested the forehead on the forearms. A lubricant was applied to the skin on the pericranial and neck area prior to treatment, and the EDGE mobility tool was cleaned with an alcohol pad. Initially, the EDGE mobility tool was used to locate soft tissue restrictions in the bilateral upper trapezius and suboccipital muscles. Then, the therapist applied IASTM strokes for 20 seconds parallel to muscle fibers, followed by strokes for 20 seconds perpendicular to muscle fibers with the EDGE mobility tool held at a 45° to the skin [27]. The EDGE mobility tool was used with the beveled side contacting the skin (Figures 1 and 2). Pressure was applied lightly at first, with a gradual increase due to the participant’s initial sensitivity to treatment, and then it was increased according to the participant’s tolerance to maximal force as it has been shown that heavy pressure evokes more fibroblast proliferation compared to light or moderate pressure. The treatment time with the tool was 5 minutes [28]. Cryotherapy was applied for 10 minutes after the session to control bruising and soreness. A certified physical therapist performed IASTM techniques.
Figure 1.
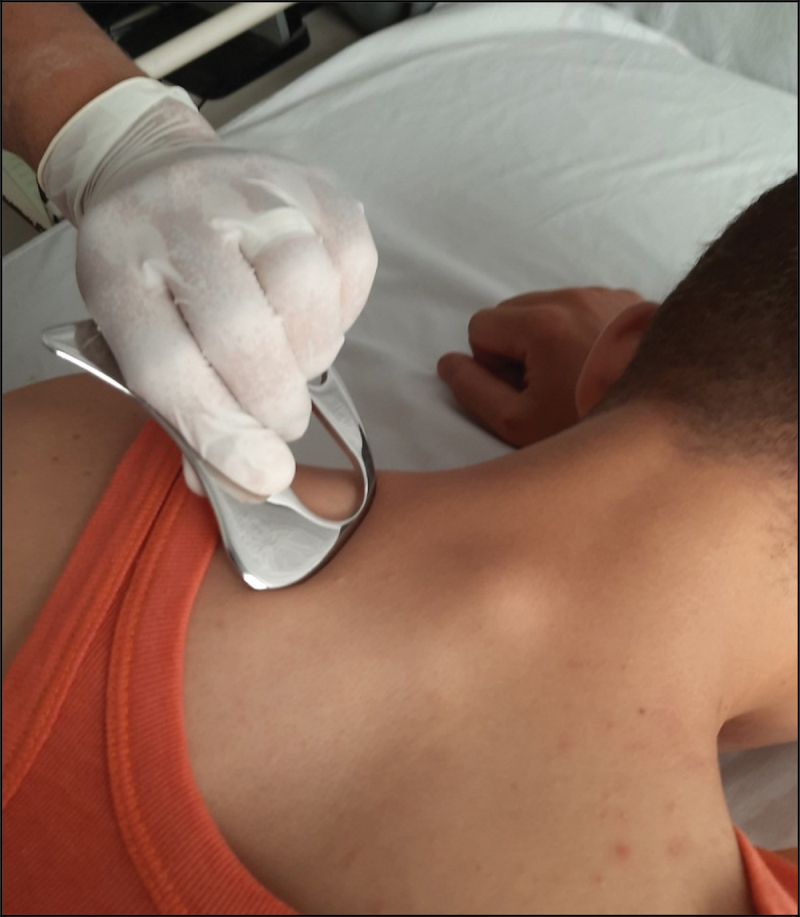
Application of IASTM on the left upper trapezius using Edge Tool.
Figure 2.

Application of IASTM on the left suboccipital muscle using Edge Tool.
(Group B): algometry pressure release
Algometry Pressure Release was performed according to work described by [29,and 21]. A slow pressure was applied perpendicularly at the marked MTrPs over the bilateral upper trapezius and sub-occipital muscles by the algometer until the patient reported a ‘moderate but easily tolerable’ pain which approached 7 out of 10 on NPRS. The amount of pressure was adjusted so that if the patient reported a decrease in the perceived pain (for example, a value of 3 or 4 on NPRS compared with the perceived pain at baseline), the pressure was increased gradually to restore the perceived pain value of 7. Pressure was maintained for 1 min, and this procedure was repeated 3 times with a 30-s rest in between.
(Group C): sham ultrasound control group
Sham ultrasound was administered using the therapeutic ultrasound stimulation unit (ENRAF NONIUS Sonopuls 434 Ultrasound Therapy Unit, Holland) adjusted to an intensity of 0.5 W/cm2 which is lower than that of physiologic effects. The sham ultrasound control group used in this study works as a placebo group, to eliminate the potential skin pressure-related relieving effect [30,31]. The sound head was applied in small overlapping circles deeply and slowly over the bilateral upper trapezius and sub-occipital muscles in the region of MTrPs for 2 min [21].
All participants received two treatment sessions per week separated by at least 48 hours for four weeks. Each session lasted for approximately 45 minutes. During the study, participants were instructed not to render any other treatment to the upper back or neck. To verify their compliance to this instruction, we asked them about it in each session.
Outcome measures
All participants were assessed in the same conditions at baseline and at the end of four weeks’ treatment program. Headache frequency was further assessed after two weeks of follow-up.
1) Headache Frequency: Each patient was asked to record the number of headache attacks with a register daily. Headache frequency was expressed as the number of headache days per month.
2) Headache Under-Response to Treatment (HURT) questionnaire: An 8-item, self-administered questionnaire addressing headache frequency and disability, medication use, and effect, perception of headache ‘control’, and knowledge of diagnosis was used. The range of possible responses to questions 1–8 is 0 to 24, with lower scores indicating better clinical outcome [32]. The Arabic version of HURT questionnaire is reliable and responsive, where it can detect the change in illness over time [33].
3) Pressure pain threshold (PPT): FPK (Wagner Pain TestTM Instruments-Model FPK/FPN-Greenwich-USA) model algometer was used to measure PPT in MTrPs of the bilateral upper trapezius and suboccipital muscles. This task was performed by a licensed clinical physiotherapist with almost 15 years of clinical experience and who was blinded to group allocation. A blind assessor took algometric measurements with excellent intra-rater reliability (two-way mixed effect model ICC, (absolute agreement, multiple measurements) was used. Intra-class correlation coefficient (ICC) = .96-.99, standard error of measurement (SEM) = .0.12–0.19 Kg/cm2, and minimal detectable change (MDC) = .33-.52 Kg/cm2. This reliability study was done on 20 participants with TTH who were part of the clinical trial. The measurements were taken in two separate occasions with one week apart, during which the participants did not receive their assigned treatment.
4) Cervical lordosis angle (CA): was measured on the lateral view of cervical spine X-ray from the two tangent lines drawn on the posterior vertebral body margins of (C2-C7) (posterior tangent method) where the normal range is 34–42° [34], as shown in Figure 3.
Figure 3.
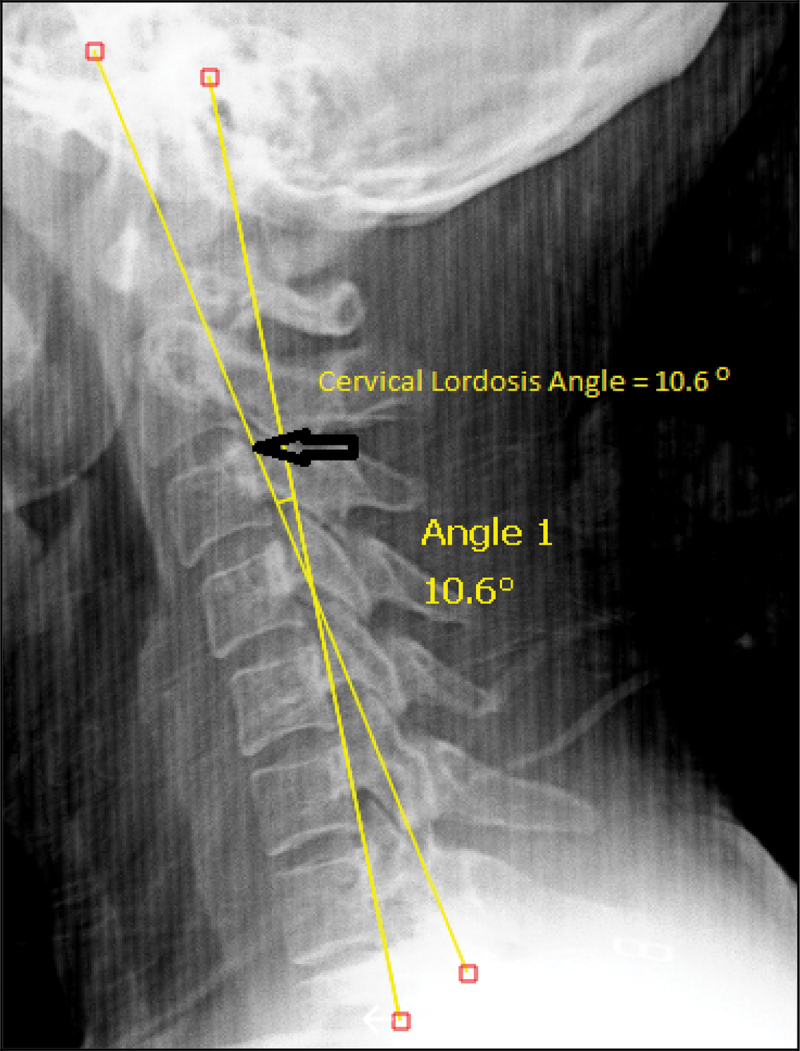
Measurement of Cervical Lordosis Angle (CA) using Surgimap software.
5) Anterior head translation (AHT): AHT is the horizontal distance between the posterior superior body of the second cervical (C2) vertebra and a vertical line drawn superiorly from the posterior inferior body of the (C7) vertebra (Figure 4). The amount of AHT was measured using a standard radiograph in a lateral view [35]. The normal value for this measurement is 10 mm [34].
Figure 4.
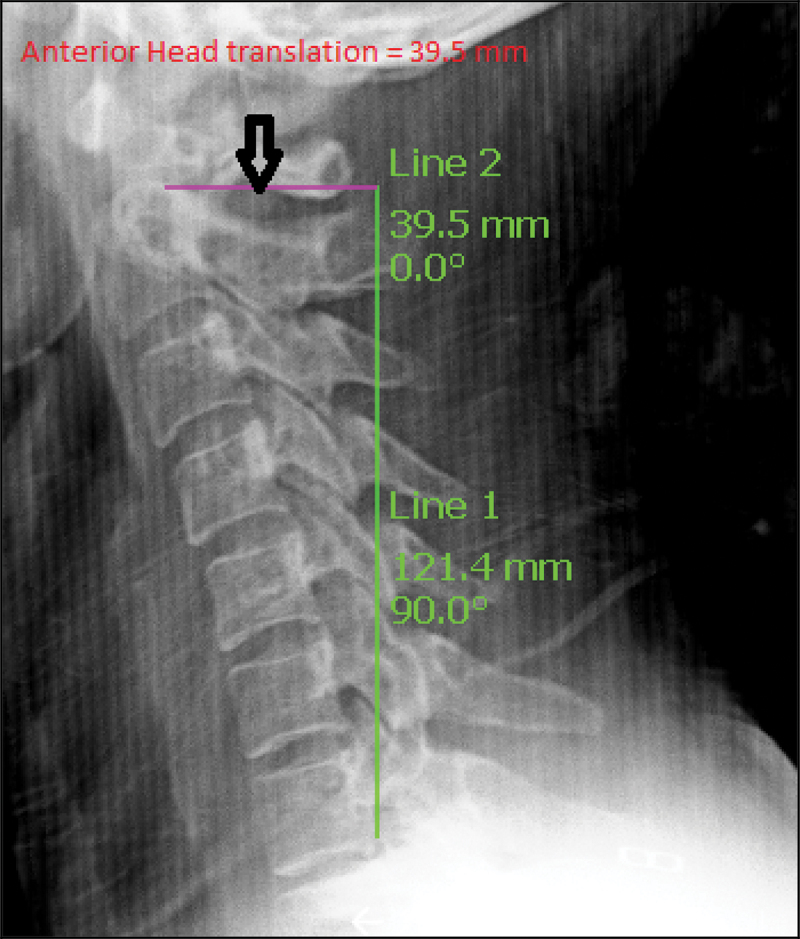
Measurement of Anterior head translation (AHT) using Surgimap software.
CA and AHT were measured using Surgimap Spine software by a blinded examiner with excellent intra-rater reliability (two-way mixed effect model ICC (absolute agreement, multiple measurements) was used. For CA, ICC = .99, SEM = .44°, and MDC = 1.22°. For AHT: ICC = .99, SEM = .6 mm, MDC = 1.68 mm). This reliability study was done on 20 participants and the measurements were taken in two separate occasions with one week apart.
Randomization
A randomization list (1:1:1 allocation ratio) was generated using randomly permuted block sizes of 3 and 6 created with a random number generator, and the treatment allocation was concealed. It was performed by an independent researcher who was not involved in patients’ recruitment and who was blinded to groups assignment. Participants were randomly allocated to three experimental groups: a) IASTM group, b) pressure algometer group, and c) sham ultrasound control group.
Sample size calculation
The sample size was determined as per the study of [36] who stated that 20 patients were needed in each group based on an effect size (Cohen’s d) of approximately 0.84 with alpha of 0.05 and power of 80%, considering the headache frequency as the primary outcome. It was intended to include 24 patients in each group, considering the estimation of sample sizes, the possibility of having dropouts (20%), and the available resources for conducting the study.
Statistical analysis
SPSS version 20.0 statistical software was done using all statistical analyses. For ordinal data (headache frequency and HURT questionnaire), Kruskal Wallis tests were performed to examine the differences among study groups. If the differences between effects were found significant, post hoc comparisons between treatment groups were made using Dunn-Bonferroni tests. Two by two mixed design MANOVA was conducted to compare the study groups’ ‘between-subject effect’ at the pretest and posttest conditions for continuous data (PPT for bilateral upper trapezius and suboccipital muscles, CA and AHT). Moreover, testing for the interaction effects between both independent variables was performed. To estimate clinical significance, Cohen’s d was calculated to determine the effect size for the continuous variables after pairwise comparisons using the following formula: d = Mean(group1) − Mean(group2)/SD(pooled). The d values indicating a ‘small,’ ‘medium,’ and ‘large’ effect size are 20, 50, and 80 respectively [37].
Complete case analysis was performed as the proportion of missing data (11%) was small. The statistically significant level was set at p < 0.05.
Results
A total of 80 patients were evaluated for inclusion; 72 patients of them met the inclusion criteria and were enrolled then equally randomized to the study groups (Figure 5): IASTM (n = 24), pressure algometry (n = 24), and sham ultrasound (n = 24) groups. Table 1 depicts demographic information for the 64 participants analyzed in the present study by treatment group. On average, 40 participants had episodic TTH, and 32 participants had chronic TTH. Thirty-four participants were males. The mean age of participants was 33.5 years old, who experienced TTH for an average of 8.9 years (SD = 6.9).
Figure 5.
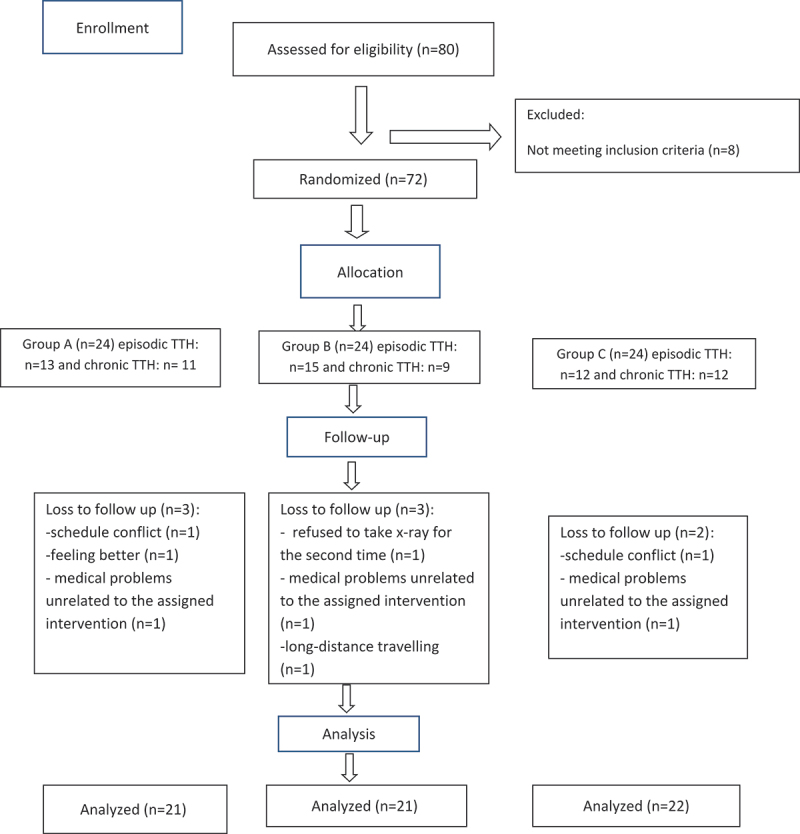
Participants, flow chart.
Table 1.
Descriptive statistics of age, weight, height, BMI and baseline outcome measures of the three study groups.
| Variable | Group A (n = 21) Mean ± SD | Group B (n = 21) Mean ± SD | Group C (n = 22) Mean ±SD |
|---|---|---|---|
| Age (Years) | 41.3 ± 7.7 | 43 ± 5.8 | 39 ± 6.6 |
| Weight (Kg) | 74.1 ± 7.2 | 73.2 ± 6.7 | 72.1 ± 6.5 |
| Height (cm) | 176.6 ± 6.3 | 175.4 ± 7.9 | 174.2 ± 5.5 |
| BMI (Kg/m2) | 23.6 ± 1.4 | 23.7 ± 1.2 | 23.7 ± 1.3 |
| PPT UTrt (Kg/cm2) | 2.7 ± .65 | 2.5 ± .49 | 2.4 ± .94 |
| PPT UTlt (Kg/cm2) | 2.5 ± .53 | 2.27 ± .57 | 2.19 ± .76 |
| PPT Subrt (Kg/cm2) | 2. ± .49 | 1.98 ± .40 | 2. ± .46 |
| PPT Sublt (Kg/cm2) | 1.7 ± .4 | 1.8 ± .42 | 1.9 ± .59 |
| AHT (mm) | 24.17 ± 5.17 | 23.77 ± 4.19 | 21.9 ± 4.35 |
| CA(°) | 17.57 ± 5.25 | 19.16 ± 3.34 | 23.06 ± 6 |
| Headache Frequency Median (IQR) |
15 (11) | 20 (10.5) | 18 (11.25) |
| HURT Median (IQR) |
19 (3.5) | 19 (4) | 20 (5) |
SD: Standard Deviation; BMI: Body Mass Index; Group A: Instrument-assisted soft tissue mobilization; Group B: Pressure Algometry; Group C: Sham Ultrasound Control; CA: Cervical Lordosis Angle; AHT: Anterior Head Translation; PPT: Pain Pressure Threshold; UTrt: right upper trapezius; UTlt: left upper trapezius; Subrt: right suboccipital; Sublt: left suboccipital; IQR: Interquartile Range; HURT: Headache Under-Response to Treatment.
Table 2 illustrates the results of the analyses, which examined the impact of provided treatments on the alteration in headache outcomes over time. Median (IQR) is presented for each time point by treatment group. The Kruskal–Wallis H test revealed a statistically significant differences in headache frequency among the study groups post treatment and at follow-up (P < 0.001). Further, headache disability (HURT) differed significantly among the study groups post treatment (P < 0.001). Dunn’s pairwise tests were performed for the three groups. A statistically significant difference (P < 0.05 adjusted using the Bonferroni correction) was observed between the IASTM group and both pressure algometry and sham ultrasound control groups.
Table 2.
Comparison of median (IQR) of head frequency and HURT questionnaire of the three groups across treatment times.
| Variable | Time | Group A (n = 21) | Group B (n = 21) | Group C (n = 22) |
|---|---|---|---|---|
| Headache Frequency | Post treatment | 8 (3.5)* † | 11 (4) | 14 (8.25) |
| Follow-up | 2 (1.5) * † | 3 (1) * | 5 (2) | |
| HURT | Post treatment | 10 (3.5)* † | 14 (3) | 16 (3.25) |
*P < 0.05 from Control; †p < 0.05 from Algometry Group; HURT: Headache Under Response to Treatment; Group A: Instrument-assisted soft tissue mobilization; Group B: Pressure Algometry; Group C: Sham Ultrasound Control
Headache frequency at end of treatment and at 2-week follow-up was lower in the IASTM group compared to the pressure algometry and sham US control groups. Although there was no difference in headache frequency between the pressure algometry and sham US control groups at the end of treatment, headache frequency in the pressure algometry was lower than in the sham US control group at 2-week follow-up. For the HURT questionnaire, median scores were significantly lower (P < 0.05) in the IASTM group compared to the other two groups. Although, there was no significant difference between the pressure algometry and sham US groups immediately after treatment (P > 0.05), Table 2.
Regarding PPT, 2-way ANOVAs showed significant interaction effects for PPT of the right and left upper trapezius (P < .001) and the right and left suboccipital muscles (P < .001). The improvements in PPT of the bilateral upper trapezius muscles increased in the IASTM group with large effect sizes compared to pressure algometry and sham ultrasound control groups after treatment.
Further, PPT of the bilateral suboccipital muscles increased in the IASTM group with large effect sizes compared to pressure algometry and sham ultrasound control groups after treatment. However, no statistical differences (P > 0.05) were detected between the pressure algometry and sham ultrasound groups (Table 3).
Table 3.
Comparison of mean difference of pain pressure thresholds and cervical alignment of the three groups post treatment.
| Variable | Groups | Mean Difference | 95% CI | Cohens’ d |
|---|---|---|---|---|
| PPT UTrt (Kg/cm2) |
Group A-Group B | .84* | .34-1.35 | 1.7 |
| Group A-Group C | 1.18* | .68-1.68 | 1.6 | |
| Group B-Group C | .34 | −.16-.84 | .5 | |
| PPT UTlt (Kg/cm2) |
Group A-Group B | .80* | .35-1.25 | 1.6 |
| Group A-Group C | 1.09* | .65-1.54 | 1.7 | |
| Group B-Group C | .29 | −.15-.74 | .46 | |
| PPT Subrt (Kg/cm2) |
Group A-Group B | .76* | .39-1.12 | 1.9 |
| Group A-Group C | .94* | .57-1.29 | 1.8 | |
| Group B-Group C | .18 | −.18-.54 | .14 | |
| PPT Sublt (Kg/cm2) |
Group A-Group B | .70* | .30-1.09 | 1.6 |
| Group A-Group C | .74* | .35-1.32 | 1.3 | |
| Group B-Group C | .04 | −.35-.43 | 0 | |
| CA(°) | Group A-Group B | 4.89* | 1.72-8.06 | 1.6 |
| Group A-Group C | 5.68* | 2.54-8.82 | 1.3 | |
| Group B-Group C | .79 | −2.35-3.92 | 0 | |
| AHT (mm) | Group A-Group B | −3.81* | −6.31- −1.31 | 1.3 |
| Group A-Group C | −3.84* | −6.32- −1.36 | 1.1 | |
| Group B-Group C | −.034 | −2.51-2.44 | 0 |
*P < 0.05; Group A: Instrument-assisted soft tissue mobilization; Group B: Pressure Algometry; Group C: Sham Ultrasound Control; CA: Cervical Lordosis Angle; AHT: Anterior Head Translation; PPT: Pain Pressure Threshold; UTrt: right upper trapezius; UTlt: left upper trapezius; Subrt: right suboccipital; Sublt: left suboccipital; CI: Confidence Interval.Cohens’ d values indicating a ‘small,’ ‘medium,’ and ‘large’ effect size are .20, .50, and .80 respectively
Concerning the measures of cervical alignment, 2-way ANOVAs showed significant interaction effects for CA (P < .001) and AHT (P < .001). The IASTM group showed significant improvements in CA and AHT with large effect sizes compared to the other two groups after treatment. However, CA and AHT showed non-significant difference after treatment (P > 0.05) between pressure algometry and sham ultrasound control groups (Table 3).
Discussion
The current study revealed that IASTM was more effective in improving all the measured outcomes compared to pressure algometry and sham ultrasound. The most important clinically relevant finding was the concomitant reduction in headache frequency with decreased headache disability as evaluated by the HURT questionnaire. The findings of this study revealed greater clinically important improvements in the headache measures in the IASTM group in comparison to the other two groups following intervention. Regarding headache frequency at the 2 weeks’ follow-up stage, the IASTM group showed lower episodes compared to the other two groups. It seems that the application of IASTM with wider and deeper penetrating strokes led to better cumulative delayed effect compared to the other two interventions.
These results seem to be supported by recent systematic reviews which revealed that more positive outcomes are observed in TTH patients who receive manual therapy compared to those who receive standard treatment or a placebo [38,39].
The interpretation of the differences between groups for headache frequency should be taken cautiously because the median number of headache days per month at baseline in the IASTM group was 5 days lower than in the pressure algometry and 3 days lower than in the sham US group. This difference in median number of headache days per month at baseline is enough to be concerned that the groups were not really similar on this outcome at baseline.
Interpreting the clinical importance of differences between groups for the HURT questionnaire is difficult due to lack of adequate information on the psychometrics of this outcome measure.
On the other hand, the pressure algometry group exhibited lower episodes than sham ultrasound group only at 2 weeks after completion of intervention. This could be explained by the fact that both devices applied pressure with different amounts (intensities) to the target tissues.
The current study’s findings showed a significant increase in the PPT at upper trapezius and suboccipital muscles after the application of IASTM compared to the other two groups. The findings of this research are consistent with previous studies in which IASTM increased PPT of upper trapezius in asymptomatic volunteers [40] and patients with neck pain [41,42].
Another important finding in our study is that IASTM has a better effect in improving cervical alignment compared to other interventions. 43,found that clinical improvement” [minimal detectable change (MDC)]” needs to exceed 6.2° for cervical lordosis. In the current study, the application of IASTM increased cervical lordosis by 6.5° and 11.15° compared to pressure algometry and sham US respectively. Up to our knowledge, no studies measured the MDC of the AHT. However, reviewing previous studies revealed an improvement greater than 4 mm in fibromyalgia [44] and posture-related pain [45]. In the present experiment, the application of IASTM decreased AHT by 4.2 mm and 6.1 mm compared to pressure algometry and sham US, respectively. This difference between our finding and other studies maybe attributed to the variation in the treatment duration and applied interventions.
Possibly, the improvements in cervical alignment are attributed to the similarity between the effect of IASTM and manual therapy on soft tissue restrictions. The pressure provided by IASTM stretched the fascia of the posterior neck and suboccipital muscles. Previous research revealed that manual therapy improves posture alignment [46,47]. The improvement of FHP following IASTM is in agreement with 48,who showed that Graston technique had a positive effect on the normalization of cervical posture in symptomatic students with FHP.
Interestingly, the comparison between pressure algometry and sham ultrasound revealed no statistically significant differences in headache frequency, HURT, and PPT (upper trapezius and suboccipital) post-intervention. These findings are contrary to 21, who found that pressure application to upper trapezius trigger points using algometer is more effective than sham US. Further, pressure algometry showed similar effect to sham US on CA and AHT.
The use of placebo is recommended in clinical trials on headache in order to avoid overestimation of the findings, as placebo medications may be as effective as an active medication. The placebo effect could be attributed to the neurobiological and psychological mechanisms of patients, expectations [49]. Because US therapy is a ‘hands-on’ treatment, it requires the presence of a therapist, a therapeutic equipment and rituals (contextual effects) that may underpin the analgesic efficacy of US [50,51].
The current study has some potential limitations. First, due to the nature of the interventions, neither the participants nor the treatment providers were blinded to group allocation. In addition, the amount of pressure applied during IASTM could not be controlled or measured, thus, equality of pressure applied in each session is not guaranteed. Lastly, the duration of follow-up was very short.
Conclusion
IASTM is superior to pressure algometry in improving patients, symptoms in TTH. Further, it shows a better corrective effect on cervical mal-alignment than pressure algometry. The use of mechanical interventions in manual therapy techniques may provide avenue to help clinicians in treating musculoskeletal disorders.
Acknowledgments
The authors would like to thank Dr Asmaa Sayed Ali, Dr Sheriff Ahmed Sayed and Dr Sami Mohamed Salaman, El Gomhorya Hospital for their assistance in data collection. Further, the authors are grateful to Prof. Dr Abeer Abd el-rahman, Cairo University for her advices and support.
Biographies
Sherif Moustafa Ramadan is a PhD candidate at the Faculty of Physical Therapy, Cairo University. He earned a Bachelor degree (2005) and a MSc in Physical Therapy (2013) from Cairo University, Egypt. His Master thesis examined the Efficacy of Cranial Base Release in Chronic Tension-type Headache.
Dr. Hussein Awad El gharieb received a Bachelor degree (excellent with honors) in Medicine (1999) and a MSc in Neuropsychiatry (2004) from Al Azhar University, Egypt. Then he received his MD in Neurology (2010) from Al Azhar University. He is an assistant professor of Neurology at the Faculty of Medicine, Al Azhar University.
Prof. Dr. Awatef Mohamed Labib is a Professor of Physical Therapy at the Department of Basic Science, Cairo University. She was appointed a Chairman of the Department of Basic Science (1983-1994). Also, she was appointed a Chairman of the Promotions Committee (2006-2012). She taught courses and published research on manual therapy, pain management and exercise physiology.
Dr. Eman Ahmed Embaby PhD, PT is an associate professor of Physical Therapy at Cairo University since 2016. She is experienced in Biostatistics. In addition, she earned a certificate in Medical Education. She is a managing editor of the “Bulletin of Faculty of Physical Therapy Cairo University”. Her research interest includes posture correction, electromyography, lumbo-pelvic motor control and psychometric properties of measurements.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].GBD 2015 Neurological Disorders Collaborator Group . (2017). Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet Neurol;16(11):877–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Waldie KE, Buckley J, Bull PN, et al. (2015). Tension-type headache: a life-course review. J Headache & Pain Manage. 1(1), 1–9. Retrieved fromhttp://headache.imedpub.com/https://researchspace.auckland.ac.nz/docs/uoa-docs/rights.htm [Google Scholar]
- [3].Allena M, Steiner TJ, Sances G, et al.(2015). Impact of headache disorders in Italy and the public-health and policy implications: a population-based study within the eurolight project. J Headache Pain. 16:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Buse DC, Loder EW, Gorman JA, et al. (2013). Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American migraine prevalence and prevention (AMPP) study. Headache. 53(8):1278–1299. [DOI] [PubMed] [Google Scholar]
- [5].Lardon A, Girard MP, Zaïm C, et al. (2017). Effectiveness of preventive and treatment interventions for primary headaches in the workplace: a systematic review of the literature. Cephalalgia. 37(1):64–73. [DOI] [PubMed] [Google Scholar]
- [6].Monzani L, Zurriaga R, Espí López GV (2018). Anxiety and the severity of tension-type headache mediate the relation between headache presenteeism and workers’ productivity. PLoS One. 9; 13(8): e0202313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Fernández-de-Las-Peñas C, Alonso-Blanco C, Cuadrado ML, et al. (2006b). Myofascial trigger points and their relationship to headache clinical parameters in chronic tension-type headache. Headache. 46(8):1264–1272. [DOI] [PubMed] [Google Scholar]
- [8].Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, et al. (2006c). Trigger points in the suboccipital muscles and forward head posture in tension-type headache. Headache. 46(3):454–460. [DOI] [PubMed] [Google Scholar]
- [9].Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, et al. (2006a). Forward head posture and neck mobility in chronic tension-type headache: a blinded, controlled study. Cephalalgia.;26(3):314–319. [DOI] [PubMed] [Google Scholar]
- [10].Nagasawa A, Sakakibara T, Takahashi A (1993). Roentgenographic findings of the cervical spine in tension-type headache. Headache. 33(2):90–95. [DOI] [PubMed] [Google Scholar]
- [11].Cumplido-Trasmonte C, Fernández-González P, Alguacil-Diego IM, et al. (2018). Manual therapy in adults with tension-type headache: a systematic review. Neurologia. 7: S0213-4853(18)30013–6. [DOI] [PubMed] [Google Scholar]
- [12].Espí GV, Gómez A (2010). Efi cacia del tratamiento en la cefalea tensional. Revisión sistemática Fisioterapia. 32(1): 33–40. [Google Scholar]
- [13].Starkey C (2013). Therapeutic modalities 4th edition. Company FAD. Philadelphia: F.A.Davis Company, pp:349. [Google Scholar]
- [14].MacDonald N, Baker R, Cheatham SW (2016). The effects of instrument assisted soft tissue mobilization on lower extremity muscle performance: a randomized controlled trial. Int J Sports Phys Ther. 11(7):1040–1047. [PMC free article] [PubMed] [Google Scholar]
- [15].Seffrin CB, Cattano NM, Reed MA, et al. (2019). Instrument-assisted soft tissue mobilization: a systematic review and effect-size analysis. J Athl Train. 54(7):808–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Davidson CJ, Ganion LR, Gehlsen GM, et al. (1997). Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc. 29(3):313–319. [DOI] [PubMed] [Google Scholar]
- [17].Blanchette MA, Normand MC (2011). Augmented soft tissue mobilization vs natural history in the treatment of lateral epicondylitis: a pilot study. J Manipulative Physiol Ther. 34(2):123–130. [DOI] [PubMed] [Google Scholar]
- [18].Burke J, Buchberger DJ, Carey-Loghmani MT, et al. (2007). A pilot study comparing two manual therapy interventions for carpal tunnel syndrome.J Manipulative Physiol Ther. 30(1):50–61. [DOI] [PubMed] [Google Scholar]
- [19].Schaefer JL, Sandrey MA (2012). Effects of a 4-week dynamic balance- training program supplemented with Graston instrument-assisted soft-tissue mobilization for chronic ankle instability. J Sport Rehabil. 21(4):313–326. [DOI] [PubMed] [Google Scholar]
- [20].Brantingham JW, Globe GA, Jensen ML, et al. (2009). A feasibility study comparing two chiropractic protocols in the treatment of patellofemoral pain syndrome. J Manipulative Physiol Ther.32(7):536–548. [DOI] [PubMed] [Google Scholar]
- [21].Abu Taleb W, Rehan Youssef A, Saleh A (2016). The effectiveness of manual versus algometer pressure release techniques for treating active myofascial trigger points of the upper trapezius. J Bodyw Mov Ther. 20(4):863–869. [DOI] [PubMed] [Google Scholar]
- [22].Sarrafzadeh J, Ahmadi A, Yassin M (2012). The effects of pressure release, phonophoresis of hydrocortisone, and ultrasound on upper trapezius latent myofascial trigger point. Arch Phys Med Rehabil. 93(1):72–77. [DOI] [PubMed] [Google Scholar]
- [23].Zamani S, Okhovatian F, Naimi S, et al. (2017). The immediate effect of a combination of pressure release and cervical mobilization techniques on the active range of motion in the latent trigger points of upper trapezius muscle in young adult females. Austin Phys Med. 1(1) :1002. [Google Scholar]
- [24].Snodgrass SJ, Rivett DA (2013). Thumb pain in physiotherapists: potential risk factors and proposed prevention strategies. J Manual Manipulative Ther. Jul;10(4):206–217. [Google Scholar]
- [25].ICHD-III (2013). International classification of headache disorder: headache classification subcommittee of the international headache society, 3rd edition beta. Cephalalgia 33: 629–808. [DOI] [PubMed] [Google Scholar]
- [26].Myburgh C, Larsen AH, Hartvigsen J (2008). A systematic, critical review of manual palpation for identifying myofascial trigger points: evidence and clinical significance. Arch Phys Med Rehabil. 89(6):1169–1176. [DOI] [PubMed] [Google Scholar]
- [27].Laudner K, Compton BD, McLoda TA, et al. (2014). Acute effects of instrument assisted soft tissue mobilization for improving posterior shoulder range of motion in collegiate baseball players. Int J Sports Phys Ther. 9(1):1–7. PMID: 24567849,PMCID: PMC3924602. [PMC free article] [PubMed] [Google Scholar]
- [28].Papa JA (2012). Two cases of work-related lateral epicondylopathy treated with Graston technique (R) and conservative rehabilitation. J Can Chiropr Assoc. 56(3):192–200. [PMC free article] [PubMed] [Google Scholar]
- [29].Fryer G, Hodgson L (2005). The effect of manual pressure release on myofascial trigger points in the upper trapezius muscle. J Bodyw Mov Ther; 9 (4), 248e255. [Google Scholar]
- [30].Kienle GS, Kiene H (1997). The powerful placebo effect: fact or fiction? J Clin Epidemiol. 50 (12), 1311e1318. [DOI] [PubMed] [Google Scholar]
- [31].Montan˜ez-Aguilera FJ, Valtuen˜a-Gimeno N, Pecos-Martı´n D, et al. (2010). Changes in a patient with neck pain after application of ischemic compression as a trigger point therapy. J Back Musculoskelet Rehabil. 23 (2), 101e104. [DOI] [PubMed] [Google Scholar]
- [32].Westergaard ML, Steiner TJ, MacGregor EA, et al. (2013) Mar. The headache under-response to treatment (HURT) questionnaire: assessment of utility in headache specialist care. Cephalalgia.33(4):245–255. [DOI] [PubMed] [Google Scholar]
- [33].Al Jumah M, Al Khathaami A, Tamim H, et al. (2013). HURT (headache under-response to treatment) questionnaire in the management of primary headache disorders: reliability, validity and clinical utility of the Arabic version. J Headache Pain. 21; 14(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Harrison DD, Janik TJ, Troyanovich SJ, et al. (1997). Evaluation of the assumptions used to derive an ideal normal cervical spine model. J Manipulative Physiol Ther. 20(4):246–256. PMID: 9168409 [PubMed] [Google Scholar]
- [35].McAviney J, Schulz D, Bock R, et al. (2005). Determining the relationship between cervical lordosis and neck complaint. J Manipulative Physiol Ther. 28(3): 187–193. [DOI] [PubMed] [Google Scholar]
- [36].Moraska AF, Stenerson L, Butryn N, et al. (2015). Myofascial trigger point-focused head and neck massage for recurrent tension-type headache: a randomized, placebo-controlled clinical trial. Clin J Pain. 31(2):159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Cohen J (1988). Statistical power analysis for the behavioral sciences, 2nd ed. Hillsdale- NJ: Erlbaum. [Google Scholar]
- [38].Lozano López C, Mesa Jiménez J, de la Hoz Aizpurúa JL, et al. (2016). Efficacy of manual therapy in the treatment of tension-type headache. A systematic review from 2000-2013. Neurologia. 31(6):357–369. [DOI] [PubMed] [Google Scholar]
- [39].Maistrello LF, Geri T, Gianola S, et al. (2018). Effectiveness of trigger point manual treatment on the frequency, intensity, and duration of attacks in primary headaches: a systematic review and meta-analysis of randomized controlled trials. Front Neurol. 24; 9:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Gulick DT (2018). Instrument-assisted soft tissue mobilization increases myofascial trigger point pain threshold. J Bodyw Mov Ther. 22(2):341–345. [DOI] [PubMed] [Google Scholar]
- [41].El-Hafez HM, Hamdy HA, Takla MK, et al. (2020). Instrument-assisted soft tissue mobilisation versus stripping massage for upper trapezius myofascial trigger points. J Taibah Univ Med Sci; 6; 15(2):87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Emshi ZA, Okhovatian F, Kojidi MM, et al. (2018). The effects of instrument-assisted soft tissue mobilization on active myofascial trigger points of upper trapezius muscle. J Clin Physiother; 3(3):107–114. [Google Scholar]
- [43].Marques C, Granström E, MacDowall A, et al. (2020). Accuracy and reliability of X-ray measurements in the cervical spine. Asian Spine J, 14(2), 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Moustafa IM (2013). Does improvement towards a normal cervical sagittal configuration Aid in the management of fibromyalgia: a randomized controlled trial. Bull Fac Ph Th Cairo Univ. 18 (2): 29–41. [Google Scholar]
- [45].Fortner MO, Oakley PA, Harrison DE (2018). Alleviation of chronic spine pain and headaches by reducing forward head posture and thoracic hyperkyphosis: a CBP® case report. J Phys Ther Sci. 30: 1117–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Dudek E, Hughes L (2019). Manual therapy techniques and their effectiveness on improving posture in adults: a narrative review of the literature. Integr J Orthop Traumatol 2 (1): 1–5. [Google Scholar]
- [47].Kim BB, Lee JH, Jeong HJ, et al. (2016). Effects of suboccipital release with craniocervical flexion exercise on craniocervical alignment and extrinsic cervical muscle activity in subjects with forward head posture. J Electromyogr Kinesiol. 30:31–37. [DOI] [PubMed] [Google Scholar]
- [48].Song B, Choi Y, Cha Y (2019). Comparison of effects of different myofascial meridians methods on pain and postural control of college students with forward head posture. J Korean Soc Phys Med; 14(1): 15–23. [Google Scholar]
- [49].Evers AWM, Colloca L, Blease C, et al. (2018). Implications of placebo and nocebo effects for clinical practice: expert consensus. Psychother Psychosom;87(4):204–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Hafliðadóttir SH, Juhl CB, Nielsen SM, et al. (2021). Placebo response and effect in randomized clinical trials: meta-research with focus on contextual effects. Trials. 26;22(1):493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Parker R, Madden VR (2014). Ultrasound v. sham ultrasound for experimentally induced delayed onset muscle soreness: a double-blind, randomized controlled trial. SAJSM 26(4):99–103. [Google Scholar]


