Abstract
Aims
This is a multicentre, prospective assessment of a proportion of the overall orthopaedic trauma caseload of the UK. It investigates theatre capacity, cancellations, and time to surgery in a group of hospitals that is representative of the wider population. It identifies barriers to effective practice and will inform system improvements.
Methods
Data capture was by collaborative approach. Patients undergoing procedures from 22 August 2022 and operated on before 31 October 2022 were included. Arm one captured weekly caseload and theatre capacity. Arm two concerned patient and injury demographics, and time to surgery for specific injury groups.
Results
Data was available from 90 hospitals across 86 data access groups (70 in England, two in Wales, ten in Scotland, and four in Northern Ireland). After exclusions, 709 weeks' of data on theatre capacity and 23,138 operations were analyzed. The average number of cases per operating session was 1.73. Only 5.8% of all theatre sessions were dedicated day surgery sessions, despite 29% of general trauma patients being eligible for such pathways. In addition, 12.3% of patients experienced at least one cancellation. Delays to surgery were longest in Northern Ireland and shortest in England and Scotland. There was marked variance across all fracture types. Open fractures and fragility hip fractures, influenced by guidelines and performance renumeration, had short waits, and varied least. In all, nine hospitals had 40 or more patients waiting for surgery every week, while seven had less than five.
Conclusion
There is great variability in operative demand and list provision seen in this study of 90 UK hospitals. There is marked variation in nearly all injuries apart from those associated with performance monitoring. There is no evidence of local network level coordination of care for orthopaedic trauma patients. Day case operating and pathways of care are underused and are an important area for service improvement.
Cite this article: Bone Jt Open 2023;4(6):463–471.
Keywords: Trauma, cancellations, delays, time to surgery, waiting times, Orthopaedic Trauma, Open fractures, hip fractures, variance, fracture related infections, orthopaedic trauma surgery, British Orthopaedic Association, Proximal femur fractures, soft-tissue injuries, periprosthetic joint infections
Introduction
Care of the injured patient is a core component of the workload of most orthopaedic surgeons. Trauma management has significant impact on hospital bed occupancy and consumes an important proportion of operating theatre capacity. During periods of high demand, there may be competition for resources with planned care when both groups are co-located in the same hospital. While there is information that considers planned surgery,1 there is a paucity of data to guide pathway development and quality improvement in trauma surgery.
There are perennially high levels of bed occupancy in the NHS, particularly in the winter months (> 95%).2 This pressure, coupled with insufficient capacity and organisational inefficiency,3 is frequently implicated as cause of delay and cancellation of surgical procedures.4
Fragility femur fractures are recorded on the National Hip Fracture Database (NHFD), with time to surgery incentivised as part of the Best Practice Tariff (BPT).5 High energy-transfer open lower limb fractures are recorded as part of the Trauma Audit Research Network (TARN),6 a key performance indicator for major trauma centre status. Other guidelines, including British Orthopaedic Association Standards for Trauma (BOAST) for ankle and distal radius,7,8 make recommendations about the timing of surgery, but are not monitored and are not associated with any financial incentive.
Many other injuries are neither monitored nor incentivised with anecdotal concerns growing that patient experience and outcome suffer because of delays and cancellations.
In recognition of these concerns, the British Orthopaedic Association (BOA) commissioned this prospective, multicentre service evaluation from a representative sample of cases undergoing surgery on orthopaedic trauma lists across the UK between two time points. The BOA provided funding for this study to cover database construction and data analysis. It was appreciated that not all hospitals would be able to enrol, and the original expectation was that between 30 to 50 hospitals would be recruited to generate information to guide policy.
There were four key objectives:
Identify the number of trauma and ambulatory operative sessions at unit level and define the proportion of patients managed as a day case.
Define and quantify the orthopaedic trauma caseload in the UK.
Describe the average time to surgery for individual fracture groups and assess if there is variance both between and within units.
Investigate performance against metrics for management of indicator injuries which have nationalised guidelines (National Institute for Health and Care Excellence (NICE) and British Orthopaedic Association Trauma Association (BOAST) guidelines).
Methods
The study protocol was designed by an expert working group of the British Orthopaedic Association Trauma Committee to run as a multicentre, prospective service evaluation.
All patients listed for an operation on a trauma list, or trauma cases conducted on elective lists between 22 August 2022 and 16 October 2022 and operated on before 31 October 2022 were included.
Cases eligible for inclusion included: all bony and/or soft-tissue injuries, including hands and spine and any infection case (such as fracture related infections, periprosthetic joint infections, and septic arthritis). Nonunion cases and cases where patients were undergoing soft-tissue coverage, even if the orthopaedic part of procedure had been previously completed (such as in open fractures requiring definitive soft-tissue coverage by plastic surgery), were eligible for inclusion if performed on an orthopaedic trauma list.
For data collection, the study was organized into two separate components or ‘arms’. ‘Arm 1’ was designed to record orthopaedic theatre capacity and forecasted caseload each week, with ‘arm 2’ designed to record daily caseload, injuries, and management demographics.
Arm 1: Theatre capacity
This was recorded prospectively at 08:00 of each Monday during the study period, and identified the number of inpatient lists available for general trauma, spine, and hand trauma in addition to dedicated day case/ambulatory trauma lists. Theatre sessions were defined as: morning (0:800 to 13:00), afternoon (14:00 to 17:00), all day (08:00 to 17:00), and three session (08:00 to > 19:00). Day case/ambulatory lists were defined as those specifically for injured patients waiting at home and discharged on the day of surgery. The complete data fields for arm one (eCRF arm one) are available as Supplementary Material i.
Arm 2: Patient, injury, and management demographics
This was recorded each day. The time of diagnosis for fractures was defined as the time of the first diagnostic radiograph. Time of diagnosis for soft-tissue injury without fracture was defined as the time of clinical assessment by a specialist, leading to diagnosis. Time of operation was defined as the time the patient entered the anaesthetic room. Time of decision to operate was also recorded to enable the calculation of time to surgery from decision to operate. The complete data fields for arm two (eCRF arm two) are available as Supplementary Material ii.
Pilot study
The Research Electronic Data Capture (REDCAP) data fields were developed and tested with a pilot study conducted between 18/07/2022 and 18/08/2022, across three sites (James Cook University Hospital, Middlesbrough; Aintree University Hospital, Liverpool; and St George's Hospital, London). The pilot study demonstrated that mirroring previous studies by collecting NHS numbers was impractical due to recent changes in information governance and the national data opt out.9,10 It was decided that this data field should be removed and responsibility for identifying and preventing data duplication at each site was transferred to the local principal investigator.
Site recruitment
Hospitals were contacted and invited to participate in the main study by the BOA. Promotion and encouragement to recruit was conducted by the Orthopaedic Trauma Society (OTS) and British Orthopaedic Trainee Association (BOTA) using social media platforms.
Study registration
The Health Research Authority decision tool confirmed that research and ethics approval was not required for this study. All collaborators secured local approval, registering the study as a service evaluation and returned an information sharing agreement and REDCAP registration form. Information governance (IG) approval was obtained at the lead site. Hospitals were categorized into ‘data access groups’ (DAGs), with unique identification numbers corresponding to their respective information sharing agreements. In some rare cases, where two hospitals from the same trust registered under a shared information sharing agreement, these hospitals were allocated one DAG identification number. It was not possible to divide the shared DAGs into individual hospitals for analysis due to the way that the data was coded. This system is required because the hospital trusts may have different points of access to care; e.g. patient seen in one hospital as part of a trust but operated in another within the same trust is one data access group. This reflects actual care and allows for analysis of a system rather than duplicating hospitals.
Quality assurance
Quality assurance checks were performed at the midpoint (14 October 2022 to 18 October 2022) and end of the study (5 November 2022 to 8 November 2022) to identify potential anomalies and/or missing data. All data was reviewed by the primary study team (TEB) and individualized spreadsheets by the site leads at each hospital.
Data management and analysis
Data was recorded on Research Electronic Data Capture (REDCap; Vanderbilt University, USA), a secure, web-based software platform designed to support data capture for research studies.11,12 Data was stored on servers at the lead site (South Tees NHS Trust) and presented as absolute numbers and proportions, with continuous data are expressed as medians with interquartile ranges (IQRs). Proof of difference or quality of care was not carried out as this was outside the scope of the project.
Results
The study enrolled 91 hospitals (Figure 1). One hospital (hospital #87) enrolled but did not submit data and was withdrawn from all analysis. This meant 90 hospitals across 86 DAGs participated; 70 in England, ten in Scotland, four in Northern Ireland, and two in Wales (Figure 1). This included 24 major trauma centres (MTCs), three of which were designated children’s MTCs. The term ‘hospital’ will now be used synonymously with DAG for the purpose of simplifying the discussion.
Fig. 1.

Distribution of enrolled sites.
Hospital #41 enrolled but subsequently withdrew as they were unable to complete a minimum of four weeks' data collection. Their data was included for analysis but removed for hospital comparison (master sheet; Supplementary material).
Hospitals #14 and #86 submitted recorded operative episodes but did not submit weekly data and were included in analysis of operative episodes (arm 1) but excluded from weekly data analysis (arm 2).
The remaining 84 hospitals recorded 738 weekly episodes on theatre capacity and waiting times (arm 1). Exclusion criteria included patients that were treated outside the study period,13 incomplete/unverified records,14 with 709 weekly data episodes available for comprehensive analysis.
Data from 86 hospitals recorded 25,564 operative cases (Figure 2) with a median collection period of 59 days (IQR 55 to 66). Hand and spinal cases accounted for 2,119 patients. These were not included in the analysis of time to surgery due to the lack of generalisability across all participating hospitals.
Fig. 2.
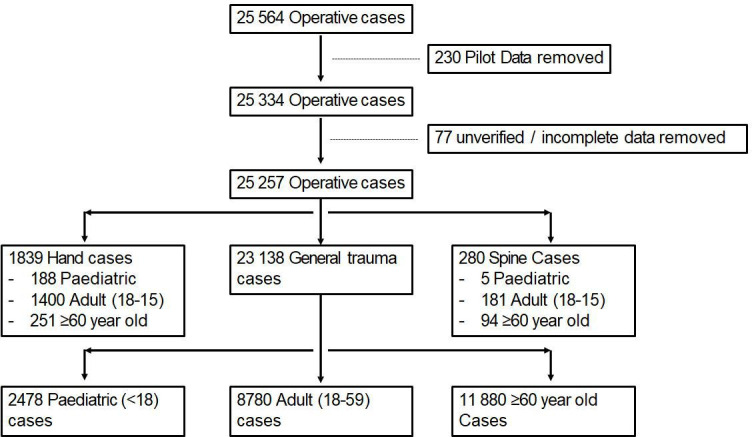
Breakdown of cases.
After deletion of pilot, unverified and incomplete data, 23,138 general trauma cases were available for comprehensive analysis.
General trauma capacity
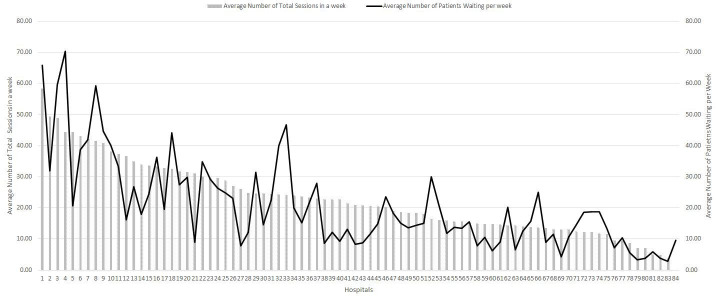
The number of dedicated general trauma sessions per hospital per week varied at hospital and country level with a median of 15.88 (Table I, Figure 3).
Table I.
Comparison of weekly general trauma capacity and outcomes per country.
| Country | Hospitals contributing weekly data, n | Median no. of general trauma sessions per week (IQR) | Median no. waiting per week (IQR) | Median no. waiting per session | Median no. of general trauma cases performed per session (IQR) | Median no. of ambulatory sessions (IQR) | Hospitals with ambulatory lists, n (%) | Number of general trauma cancelled cases, n (%) |
|---|---|---|---|---|---|---|---|---|
| England | 68 | 15.26 (12.43 to 25.06) | 16.00 (10.00 to 28.50) | 0.88 (0.57 to 1.17) | 1.69 (1.36 to 2.11) | 0 (0 to1) | 33/68 (48.5) | 18,152/2,315 (12.75) |
| Northern Ireland | 4 | 14.00 (9.75 to 19.69) | 12.25 (9.75 to 24.38) | 1.03 (0.93 to 1.13) | 1.65 (1.64 to 1.80) | 0 (0 to 2.25) | 1/4 (25) | 1,023/97 (9.48) |
| Scotland | 10 | 24.43 (14.24 to 33.85 | 17.50 (10.63 to 26.38) | 0.78 (0.61 to 0.88) | 1.62 (1.30 to 1.97) | 0 (0 to 0) | 1/10 (10) | 3,241/348 (10.74) |
| Wales | 2 | 27.07 (22.97 to 31.16) | 14.50 (11.75 to 17.25) | 0.48 (0.47 to 0.49) | 1.90 (1.54 to 2.27) | 2 (0 to 8) | 1/2 (50) | 722/81 (11.21) |
| Overall | 84 | 15.88 (12.50 to 26.23) | 16.00 (10.00 to 27.50) | 0.86 (0.56 to 1.10) | 1.69 (1.35 to 2.08) | 0 (0 to 1) | 36/84 (42.8) | 23138/2841 (12.28) |
For England’s cancellation data, 70 hospitals were used as this was recorded as part of operative episodes (arm 2).
IQR, interquartile range.
Fig. 3.
Capacity and demand variance across UK orthopaedic trauma lists.
A total of 36% of hospitals had access to less than a full day of trauma theatre seven days a week and some hospitals ran < five with others > 40 sessions per week. The median number of cases performed per session was comparable across all four nations (Table I; 1.65 to 1.90), but varied between 0.00 and 3.21 cases on an individual hospital basis.
The median number of patients waiting each Monday was also very variable with the lowest being 2.88 and the highest 70.29 (Figure 3). Nine hospitals had 40 or more patients waiting for surgery every week while seven had less than five.
The number of patients waiting compared to number of sessions available allowed comparison at hospital level and varied between 0.29 to 1.93 patients/session.
The study demonstrated that of all available theatre sessions, 842 (5.8%) were allocated to day case surgery and 36 hospitals (42.8%) had a dedicated day case trauma theatre (Table I).
Demographic of trauma
Table II shows the demographic of UK orthopaedic trauma caseload.
Table II.
Comparison of patient demographic per country.
| Country | Adults (aged 18 to < 60 yrs), n (%) | Paediatrics (aged < 18 yrs), n (%) | Adults (aged ≥ 60 yrs), n (%) | Fracture, n (%) | Infection, n (%) | Significant soft-issue, n (%) | Polytrauma, n (%) | Ambulatory, n (%) |
|---|---|---|---|---|---|---|---|---|
| England | 6,822/18,152 (37.58) | 2,073/18,152 (11.42) | 9,257/18,152 (51.00) | 13,528/18,152 (74.53) | 1,661/18,152 (9.15) | 794/18,152 (4.13) | 758/18,152 (4.18) | 5,308/18,152 (29.24) |
| Northern Ireland | 402/1,023 (39.30) | 122/1,023 (11.93) | 499/1,023 (48.78) | 868/1,023 (84.85) | 35/1,023 (3.42) | 33/1,023 (3.23) | 22/1,023 (2.15 | 345/1,023 (33.72) |
| Scotland | 1,227/3,241 (37.86) | 238/3,241 (7.34) | 1776/3,241 (54.80) | 2368/3,241 (73.06) | 304/3,241 (9.38) | 125/3,241 (3.86) | 107/3,241 (3.30) | 896/3,241 (27.65) |
| Wales | 329/722 (45.57) | 45/722 (6.23) | 348/722 (48.20) | 486/722 (67.31) | 74/722 (10.25) | 38/722 (5.26) | 63/722 (8.73) | 186/722 (25.76) |
| Overall | 8,780/23,138 (37.95) | 2,478/23,138 (10.71) | 118,80/23,138 (51.34) | 1,7250/23,138 (74.55) | 2,074/23,138 (8.96) | 945/23,138 (4.08) | 950/23,138 (4.11) | 6,735/23,138 (29.11) |
The largest proportion of operative episodes were recorded in the older patient (aged > 60 years) population (51.3%) and 3.8% sustained multiple injuries. The majority (74.6%) of trauma list cases were for fractures and a large proportion (29.1%) were ambulatory (i.e. waiting at home for surgery).
Waiting for surgery
Table III shows the waiting time to surgery by injury type.
Table III.
Time from decision (days) to operate to surgery categorized by fracture location.
| Fracture location | England, median (IQR) | Scotland, median (IQR) | Wales, median (IQR) | Northern Ireland, median (IQR) | Overall, median (IQR) |
|---|---|---|---|---|---|
| Clavicle | 4.50 (2.00 to 6.50) | 3.00 (2.00 to 4.50) | 8.00 (8.00 to 8.00) | 6.00 (5.50 to 6.00) | 5.25 (2.00 to 6.00) |
| Proximal humerus | 5.00 (4.00 to 7.00) | 5.00 (4.00 to 6.00) | 3.75 (3.63 to 3.88) | 6.00 (3.50 to 8.13) | 5.00 (4.00 - 6.50) |
| Humeral diaphysis | 5.00 (2.50 to 8.00) | 4.25(1.13 to 12.25) | 2.00 (1.25 to 2.75) | 8.00 (5.25 to 12.25) | 4.75 (2.50 - 9.50) |
| Distal humerus | 2.00 (1.00 to 5.00) | 2.00 (1.00 to 3.00) | 4.75 (3.13 to 6.38) | 3.00 (1.88 to 7.25) | 2.00 (1.00 to 6.25) |
| Elbow fracture (radial head, capitellum etc) | 2.75 (1.00 to 5.00) | 2.50 (1.63 to 6.00) | 1.00 (1.00 to 1.00) | 3.50 (1.88 to 7.50) | 2.25 (1.00 to 6.00) |
| Olecranon | 3.00 (1.25 to 5.00) | 3.50 (1.50 to 5.00) | 5.50 (4.75 to 6.25) | 2.00 (2.00 to 3.00) | 3.00 (1.50 to 5.00) |
| Forearm | 1.00 (1.00 to 1.50) | 1.00 (1.00 to 1.00) | 1.75 (1.28 to 2.13) | 1.25 (1.00 to 2.00) | 1.00 (1.00 to 1.50) |
| Distal radius | 2.50 (1.00 to 4.00) | 1.75 (1.00 to 2.00) | 2.00 (1.50 to 2.50) | 3.00 (1.75 to 4.25) | 2.00 (1.00 to 4.00) |
| Pelvic ring | 2.00 (1.00 to 3.00) | 2.50 (1.75 to 4.50) | 3.00 (3.00 to 3.00) | 2.00 (2.00 to 2.00) | 2.00 (1.00 to 3.00) |
| Acetabulum | 2.25 (1.88 to 5.25) | 2.75 (2.38 to 3.13) | 7.50 (7.50 to 7.50) | 2.00 (2.00 to 2.00) | 2.25 (2.00 to 5.00) |
| Proximal femur > 60 | 1.00 (1.00 to 1.00) | 1.00 (1.00 to 1.00) | 1.00 (0.50 to 1.50) | 2.00 (2.00 to 3.00) | 1.00 (1.00 to 1.00) |
| Proximal femur < 60 | 1.00 (1.00 to 1.00) | 1.00 (0.88 to 1.13) | 0.50 (0.25 to 0.75) | 2.50 (1.75 to 4.25) | 1.00 (1.00 to 1.25) |
| Femur shaft > 60 | 1.00 (1.00 to 2.00) | 2.00 (1.00 to 2.00) | 3.00 (3.00 to 3.00) | 1.00 (1.00 to 2.00) | 1.00 (1.00 to 2.00) |
| Femur shaft < 60 | 1.00 (1.00 to 2.00) | 1.00 (1.00 to 1.75) | 1.50 (1.25 to 1.75) | 7.00(3.50 to 16.00) | 1.00 (1.00 to 2.00) |
| Distal femur > 60 | 1.50 (1.00 to 3.00) | 1.75 (1.00 to 3.38) | 1.00 (0.50 to 1.50) | 3.00 (2.75 to 3.25) | 2.00 (1.00 to 3.00) |
| Distal femur < 60 | 1.00 (1.00 to 3.00) | 1.75 (1.00 to 3.00) | 2.50 (2.25 to 2.75) | 0.50 (0.50 to 1.00) | 1.00 (1.00 to 3.00) |
| Periprosthetic fracture > 60 | 3.00 (2.00 to 4.00) | 2.00 (1.25 to 2.00) | 1.75 (1.63 to 1.88) | 4.00 (3.50 to 4.00) | 2.50 (2.00 to 4.00) |
| Patella | 2.00 (1.00 to 3.50) | 1.00 (1.00 to 2.00) | 7.25 (7.13 to 7.38) | 1.50 (1.00 to 2.50) | 2.00 (1.00 to 1.88) |
| Tibial plateau | 2.50 (1.00 to 4.00) | 3.00 (1.25 to 3.75) | 5.00 (3.50 to 6.50) | 7.00 (6.00 to 9.75) | 2.50 (1.00 to 3.50) |
| Tibial diaphysis | 1.00 (1.00 to 1.50) | 1.00 (1.00 to 1.38) | 1.50 (1.25 to 1.75) | 2.50 (1.00 to 6.50) | 1.00 (1.00 to 1.50) |
| Tibial pilon | 2.25 (1.50 to 4.00) | 2.25 (1.75 to 3.50) | 2.75 (2.00 to 3.25) | 3.25 (3.00 to 3.50) | 2.50 (1.38 to 4.00) |
| Ankle | 2.00 (1.00 to 3.00) | 1.00 (1.00 to 2.00) | 5.00 (4.00 to 7.00) | 2.25 (2.00 to 2.63) | 2.00 (1.00 to 3.00) |
| Hindfoot and midfoot | 4.00 (2.00 to 6.00) | 3.00 (1.00 to 6.00) | 2.50 (1.75 to 3.25) | 6.50 (6.00 to 8.00) | 4.00 (2.00 to 6.25) |
| Forefoot | 1.25 (1.00 to 3.50) | 2.50 (1.00 to 4.25) | 1.00 (1.00 to 1.00) | 5.25 (4.38 to 6.13) | 1.50 (1.00 to 4.00) |
| Hand | 3.00 (2.00 to 5.50) | 2.00 (1.50 to 3.00) | 3.00 (3.00 to 3.00) | 4.00 (2.75 to 5.38) | 3.00 (2.00 to 5.00) |
| Spine | 1.00 (0.88 to 3.00) | 1.00 (1.00 to 1.00) | 0.00 (0.00 to 0.00) | 2.00 (2.00 to 2.00) | 1.00 (1.00 to 3.00) |
| Supracondylar distal humeral fracture (paediatric) | 1.00 (1.00 to 2.00) | 0.00 (0.00 to 0.25) | 1.00 (1.00 to 1.00) | 1.00 (0.50 to 1.25) | 1.00 (0.001.00) |
| Open fractures | 1.00 (1.00 to 1.00) | 1.00 (0.50 to 1.00) | 1.00 (0.00 to 1.00) | 0.50 (0.25 to 0.75) | 1.00 (1.00 to 1.00) |
| General trauma | 1.00 (1.00 to 2.00) | 1.00 (1.00 to 1.00) | 1.50 (1.50 to 2.00) | 2.50 (1.50 to 3.00) | 1.00 (1.00 to 2.00) |
| Overall | 2.00 (1.00 to 2.00) | 1.00 (1.00 to 1.75) | 2.50(2.00 to 3.50) | 2.50 (2.00 to 3.50) | 2.00 (1.00 to 3.00) |
Not all injuries are displayed in this table; those with less common injuries are in the Supplementary Material.
IQR, interquartile range.
After the decision to operate, patients had the longest wait in Northern Ireland (median time to surgery; Northern Ireland 2.5 days, Wales 1.5 days, Scotland one day, England one day). Patients with long bone fractures (humerus, femur, or tibia fractures) also waited the longest for fixation in Northern Ireland (Table III).
Open fractures had a median waiting time of one day with minimal variance in performance. Proximal femur fractures in patients aged > 60 years in general had a median waiting time of one day but waited a day longer in Northern Ireland.
Procedures usually performed by upper limb sub-specialists included clavicle, proximal humerus, other shoulder girdle, humeral diaphyseal and had some of the longest waiting times (four days). Periprosthetic fractures of the femur in those aged < 60 years and tibial plateau fractures in all age groups also had long waiting times. Physeal fractures were routinely treated promptly, with the median time to surgery < two days in nearly all fractures (not displayed).
Discussion
Geopolitical events, including the long tail of the COVID-19 pandemic, global recession, and European conflict, have had a detrimental effect on all aspects of contemporary living. This has changed the healthcare landscape and longstanding pressures on provision in the NHS do not appear to be improving. Lack of timely access to medical care is a reality, as patients in the UK experience some of the worst delays to treatment in Europe.
The orthopaedic literature is replete with studies describing and assessing surgical techniques and reporting patient outcomes. However, there remains a paucity of information regarding the effective and efficient delivery of orthopaedic trauma care within a nationalized healthcare system.
The 'Getting It Right First Time' (GIRFT) national programme is designed to improve treatment and care through in-depth review of services, benchmarking, and presenting a data-driven evidence base to support change. This initially focused on planned care,1 and has recently incorporated trauma care, but does not include metrics that enable UK-wide comparison and assessment.
The Trauma Audit Research Network and the National Hip Fracture Database are national enterprises that receive clinical data from all hospitals in the UK. These initiatives offer selective assessment of these injuries and consequently some information on performance, but is limited to two specific categories.
The ORthopaedic Trauma Hospital Outcomes - Patient Operative Delays (ORTHOPOD) study was commissioned and funded by the BOA to assess the challenges faced by providers of orthopaedic trauma care at a national level.
The aim of this study was to analyze national level data to provide the orthopaedic trauma community with an understanding, through a representative sample of hospitals, current performance and facilitate development of workstreams that improve patient flow.
The study is unique in that it provides combined assessment of trauma case load, performance, and resource availability across all nations of the UK and identifies variance in time to surgery in general and for predetermined indicator injuries.
This study presents previously unavailable, prospectively collected information on the demographics of trauma surgery, collected from 90 hospitals (86 DAGs) across four countries and includes > 23,000 general trauma cases. Any patient with an incomplete record was excluded and a full dataset was available for 99.7% for operative episodes and enables robust conclusions about contemporary orthopaedic trauma care in the UK.
The caseload identified in this study is like previous epidemiological studies and established registry data,6,15 suggesting that the data is representative.
The demographics are to be expected for an ageing population,15 with patients aged > 60 years forming the largest group that require surgery following injury. Operative intervention for patients with multiple injuries following major trauma are comparatively rare and many older patients sustain low-energy fractures. The study also demonstrated that a large proportion of patients undergoing surgery are ambulatory, suitable for day case pathways.
The study also determined the absolute caseload and numbers of patients awaiting treatment (Figure 3), providing a method of comparison between hospitals operating on greater numbers with more operating lists and those with a lower caseload and fewer lists. This provided a surrogate metric of strain on the system and identified any mismatch in the resource available to manage the trauma load.
There is a six-fold difference between the hospital with most numbers waiting per sessions available and that with the least. The average number of cases performed per session is a simple marker of productivity and this also varied between hospitals. The reasons for both these observations are multifactorial and is beyond the scope of this study. The explanation is likely to include the complexity of cases however, it will require a methodology like GIRFT ‘deep dives’ to assess current activity and determine pathways and best practice, which can be used to rationalize resource allocation.
Previous reports have highlighted waiting times for elective surgery in general,14 arthroplasty,13 and diagnostic specific delays including hip fracture.5 This is the first study to enable a geographical breakdown of delays for all routine cases performed in orthopaedic trauma theatres.
This study confirms that prompt surgery occurs for older patients with proximal femur fractures and for patients with open fractures. These injuries are subject to audit through national databases and not only are waiting times for these injuries short, but they also demonstrate least variance and demonstrates the impact of performance monitoring.
The variance for other injuries is large with five-fold to seven-fold differences in waiting times for some groups. There is also significant disparity in delays for surgery across the UK with patients in Northern Ireland experiencing the longest waiting times for surgery, including inpatient long bone injury.
These novel observations are fundamentally important and could be used to provide policy makers with objective evidence to inform resource allocation and highlight areas for improvements in care. This could include introduction of day case pathways and increased access to day case operating, simultaneously reducing delays to theatre in addition to unnecessary occupation of the orthopaedic bed base. This is one of the key recommendations of the GIRFT assessment of orthopaedic trauma.16
There is absence of a coordinated approach to case distribution for general trauma management that contrasts to the national major trauma network, which is fully funded to administer to ensure care improvement in a small percentage of cases. There is a need for a similar approach to general orthopaedic trauma, to provide a mechanism to identify hospitals that are overloaded during busy periods and facilitate the allocation of patients to alternative local facilities with capacity. The information highlighted by this study can be used to support an initiative of this type.
A total of 2,841 (12.28%) general trauma patients were cancelled at least once. Short-notice cancellation is distressing for the patient and has considerable resource implications for a hospital and the wider health service. The cancellation rate is a clear metric, which can be used to evaluate management of general trauma and quantify the effect of system modification and reallocation of resources.
Large collaborative studies are well established,9,10,17 but rely on individual investigators taking responsibility for data curation. A consultant surgeon was appointed as a lead investigator in each centre and was responsible for the accuracy of the data.
There are obvious limitations in the methodology used in this study, and there is no mechanism that allows clinical correlation with any of the outcome metrics. Similarly, data was recorded across three months of the calendar year and therefore may not be reflective on the seasonal variation seen in trauma management. Additional limitations include incomplete recording or duplication of some operative episodes and was impacted by removal of centrally recording patient identifiers. To mitigate this, individualized spreadsheets were circulated at the mid-point and end of the study to allow cross-checking of results and identification of potential anomalies.
The ORTHOPOD study has prospectively and comprehensively identified the key metrics that are relevant to hospitals providing orthopaedic trauma surgery. This provides an opportunity to focus on areas where considerable improvement can be made in patient care. Variation is identified between hospital activity and resource, and again in waiting time between units for similar injuries. Across the UK, many hospitals routinely have 40 or more patients waiting, while local units may have capacity with significantly less demand on their resource. This situation is not coordinated, and movement of patients, network models, and day case trauma pathways are underused. This carries increased relevance when around a third of cases are ambulatory, waiting at home, and are in essence mobile in terms of patient flow. ORTHOPOD provides the basis for considerable alteration of UK orthopaedic trauma pathways.
Take home message
- There is great variability in operative demand and list provision seen in this study of 90 UK hospitals. There is marked variation in nearly all injuries apart from those associated with performance monitoring.
- Day case operating and pathways of care are underused and are an important area for service improvement
Author contributions
T. E. Baldock: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
T. Walshaw: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
R. Walker: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
N. Wei: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
S. Scott: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
A. J. Trompeter: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
W. G. Eardley: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding statement
The author(s) disclose receipt of the following financial or material support for the research, authorship, and/or publication of this article: The British Orthopaedic Association provided funding for this study to cover database construction and data analysis.
ICMJE COI statement
A. J. Trompeter reports royalties or licenses from JP Medical and Oxford University Press, consulting fees from Stryker Trauma, payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Stryker Trauma, Smith & Nephew, Orthofix, and J&J DePuy Synthes, payment for expert testimony from AK Medicons, being on the NHSE advisory board on DSF/Osseointegration, and being on the leadership or fiduciary role in other board, society, committee or advocacy group for BOA Trauma committee, OTS Research committee, and BLRS Research committee, all of which is unrelated to this article.
Data sharing
The datasets generated and analyzed in the current study are not publicly available due to data protection regulations. Access to data is limited to the researchers who have obtained permission for data processing. Further inquiries can be made to the corresponding author.
Acknowledgements
We would like to acknowledge Lucksy Kottam, Orthopaedic Research Manager, and Professor Rangan, both of Academic Centre for Surgery, Middlesbrough, UK, for their support during the initial set-up of the ORTHOPOD service evaluation.
Ethical review statement
The Health Research Authority decision tool confirmed that research and ethics approval was not required for this study.
Open access funding
The authors report that they received open access funding for this manuscript from the British Orthopaedic Association.
Supplementary material
Complete data fields for arms one and two, ORTHOPOD collaborators, and breakdown by individual hospitals.
© 2023 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Thomas E. Baldock, Email: mr.thomas.baldock@gmail.com.
Tom Walshaw, Email: tom.walshaw@nhs.net.
Reece Walker, Email: reece.walker@nhs.net.
Nicholas Wei, Email: nicholas.wei@nhs.net.
Sharon Scott, Email: sharon.scott2@liverpoolft.nhs.uk.
Alex J. Trompeter, Email: alex_trompeter@hotmail.com.
William G. P. Eardley, Email: william.eardley@nhs.net.
References
- 1.Briggs T.A national review of adult elective orthopaedic services in England getting it right first time. 2015. [2 May 2023]. https://gettingitrightfirsttime.co.uk/wp-content/uploads/2018/07/GIRFT-National-Report-Mar15-Web.pdf date last. accessed.
- 2.No authors listed NHS hospital bed numbers. The King’s Fund. 2021. [ April 2023]. https://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers date last. accessed.
- 3. Caesar U, Karlsson J, Hansson E. Incidence and root causes of delays in emergency orthopaedic procedures: a single-centre experience of 36,017 consecutive cases over seven years. Patient Saf Surg. 2018;12:2. doi: 10.1186/s13037-018-0149-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wong DJN, Harris SK, Moonesinghe SR, et al. Cancelled operations: a seven-day cohort study of planned adult inpatient surgery in 245 UK National Health Service hospitals. Br J Anaesth. 2018;121(4):730–738. doi: 10.1016/j.bja.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 5.No authors listed . Royal College of Physicians; 2020. [2 May 2023]. Facing new challenges-the National hip fracture database report on 2020.https://www.nhfd.co.uk/FFFAP/Reports.nsf/0/460A8E42CE019C55802588ED0080126F/$file/NHFD%202021%20report%20v2a.pdf date last. accessed. [Google Scholar]
- 6. Shah A, Judge A, Griffin XL. Variation in timely surgery for severe open tibial fractures by time and place of presentation in England from 2012 to 2019 : a cohort study using data collected nationally by the Trauma Audit and Research Network. Bone Jt Open. 2022;3(12):941–952. doi: 10.1302/2633-1462.312.BJO-2022-0130.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.No authors listed . BOAST; [27 April 2023]. The management of distal radial fractures.https://www.boa.ac.uk/static/eca9b368-6c1d-4a44-b98de7cfc9247273/5c46835b-7d0f-40c4-89112dd5beddcda7/boast%20-%20the%20management%20of%20distal%20radial%20fractures.pdf date last. accessed. [Google Scholar]
- 8.No authors listed . BOAST; [27 April 2023]. The management of ankle fractures.https://www.boa.ac.uk/static/f8b1c499-c38a-4805-8cb8d8eb3087bca7/8be763eb-5921-4cb2-b6802f3e65ce8e7f/the%20management%20of%20ankle%20fractures.pdf date last. accessed. [Google Scholar]
- 9. Hadfield JN, Omogbehin TS, Brookes C, et al. The OPEN-Fracture Patient Evaluation Nationwide (OPEN) study : epidemiology of OPEN fracture care in the UK. Bone Jt Open. 2022;3(10):746–752. doi: 10.1302/2633-1462.310.BJO-2022-0079.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Winstanley RJH, Hadfield JN, Walker R, et al. The OPEN-Fracture Patient Evaluation Nationwide (OPEN) study: the management of OPEN fracture care in the UK. Bone Joint J. 2022;104-B(9):1073–1080. doi: 10.1302/0301-620X.104B9.BJJ-2022-0202.R1. [DOI] [PubMed] [Google Scholar]
- 11. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Clement ND, Scott CEH, Murray JRD, Howie CR, Deehan DJ, IMPACT-Restart Collaboration The number of patients “worse than death” while waiting for a hip or knee arthroplasty has nearly doubled during the COVID-19 pandemic. Bone Joint J. 2021;103-B(4):672–680. doi: 10.1302/0301-620X.103B.BJJ-2021-0104.R1. [DOI] [PubMed] [Google Scholar]
- 14.No authors listed . British Orthopeadic Association; 2023. [27 April 2023]. T&O waiting list the largest for over a decade.https://www.boa.ac.uk/resource/t-o-waiting-list-the-largest-for-over-a-decade.html date last. accessed. [Google Scholar]
- 15. Dixon JR, Lecky F, Bouamra O, et al. Age and the distribution of major injury across a national trauma system. Age Ageing. 2020;49(2):218–226. doi: 10.1093/ageing/afz151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.No authors listed Orthopaedic trauma surgery: Getting It Right First Time (GIRFT) [27 April 2023]. https://gettingitrightfirsttime.co.uk/surgical_specialties/orthopaedic-trauma-surgery/ date last. accessed.
- 17. COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]