Abstract
COPD is a heterogeneous condition, the onset and trajectory of which is influenced not only by tobacco exposure but also an individual’s genetics and the exposures they accumulate over their life course. In such a complex chronic disease, phenotyping individuals based on similar clinical or molecular characteristics can aid in guiding appropriate therapeutic management. Treatable traits, characteristics for which evidence exists for a specific favorable treatment response, are increasingly incorporated into COPD clinical guidelines. But the COPD phenotyping literature is evolving. Innovations in lung imaging and physiologic metrics, as well as omics technologies and biomarker science, are contributing to a better understanding of COPD heterogeneity. This review summarizes the evolution of COPD phenotyping, the current use of phenotyping to direct clinical care, and how innovations in clinical and molecular approaches to unraveling disease heterogeneity are refining our understanding of COPD phenotypes.
Keywords: COPD, phenotype, asthma-COPD
Introduction
Heterogeneity in COPD clinical characteristics and pathobiology plays a major role in determining COPD therapeutic responses and outcomes. Phenotyping individuals based on their clinical or biological similarities can thus aid in identifying those most likely to benefit from specific therapeutic strategies. Indeed, COPD treatment guidelines by Global Initiative for Chronic Obstructive Lung Disease (GOLD) and others are progressively focused on using treatable traits, a phenotyping-based approach, to guide COPD treatment.1-3 An increasingly nuanced understanding of COPD heterogeneity will allow for further refinement of these treatment strategies and aid in identifying novel therapeutic options for patient subgroups. This review discusses how our understanding of COPD heterogeneity and phenotyping has evolved, how phenotyping is being considered to direct clinical care, and how recent innovations are refining our understanding of COPD phenotypes.
Tobacco exposure is clearly a major risk factor for COPD development. However, recent consideration has focused on a more comprehensive assessment of exposures incurred over an individual’s life course in relation to COPD development and disease manifestations. How these accumulated exposures interact with an individual’s genetics is known as their exposome.4,5 As COPD symptoms are not typically seen until later in life, an individual has many years to accumulate exposures, increasing the complexity of their exposome. Noxious exposures such as tobacco smoke and air pollutants are obviously key exposures but so are early life and maternal risk factors (eg, premature birth, childhood asthma, and maternal and childhood exposures), individual and social factors (eg, infections, socioeconomic disadvantage, health care access, and racial disparities), as well as external environmental exposures (eg, climate). Sex appears to be a major factor influencing an individual’s manifestation of COPD. Women may experience greater symptoms than men and are more likely to develop COPD in the setting of exposures other than tobacco smoke.6-8 This difference in COPD etiology is in part due to the increased exposure of women to biomass fuels and poor indoor ventilation while cooking in low- and middle-income countries.8 Whereas many exposures and risk factors have been identified as critical to COPD development, there are likely others yet to be fully appreciated.
Clinical Phenotyping and Treatable Traits
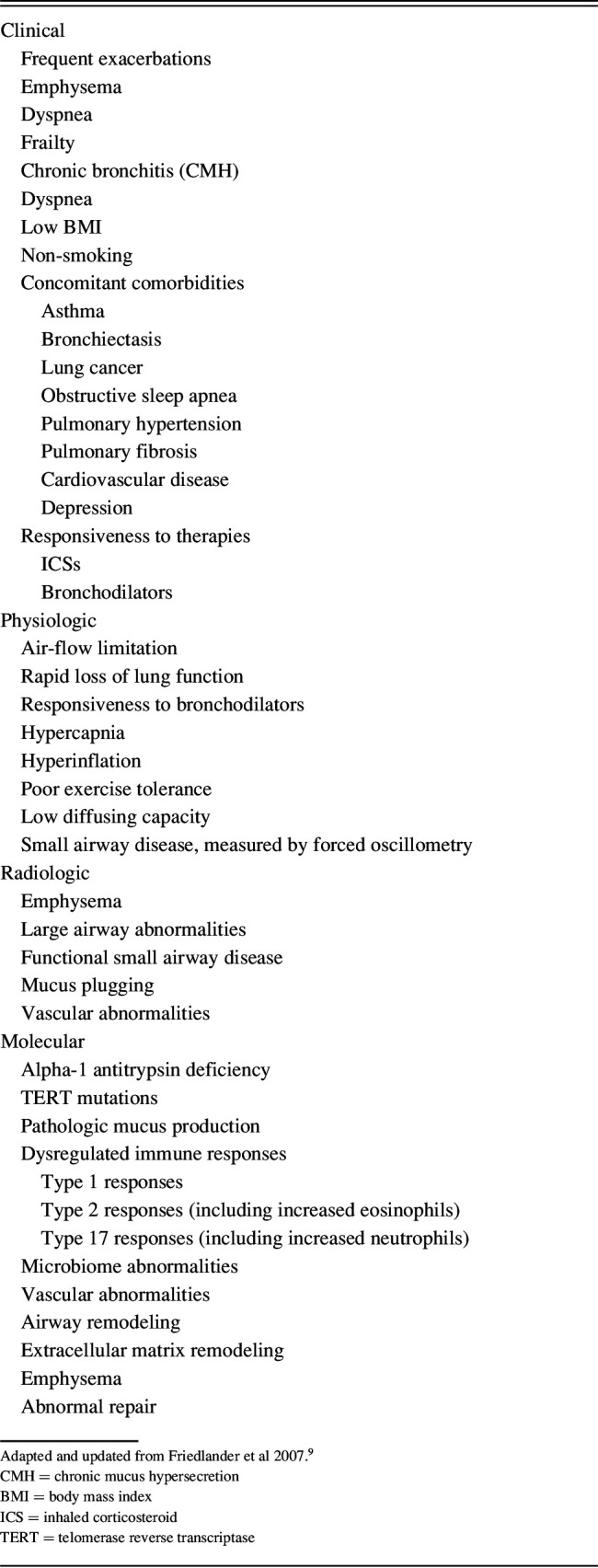
Given the complexity of an individual’s exposome, it is not surprising that COPD is heterogeneous. Indeed, disease heterogeneity in COPD is not a new concept. Classically, COPD is described as comprised of subgroups in which emphysema, chronic bronchitis, or asthma-like features predominate. This description is oversimplified as there are many clinical, radiographic, and physiologic phenotypic features that heterogeneously manifest in COPD as delineated in Table 1.5,9 An individual may display a diverse combination of these disease manifestations that may categorize them into one or multiple clinical phenotypes to varied extents.
Table 1.
Features Contributing to Disease Heterogeneity and Phenotyping in COPD
It is impractical to consider all these disease features in clinical practice. A more pragmatic way to think about clinical phenotyping is based on treatable traits, those features for which there is evidence of a particular treatment response.1,4,10 This approach is now used in guidelines,1 with the greatest evidence for dyspnea and exacerbations as treatable traits. However, other traits are considered in this nuanced approach. Hyperinflation in patients with dyspnea may be a reason to consider lung volume reduction procedures. Exacerbations and elevated eosinophils guide a greater consideration of inhaled corticosteroid (ICS) use. In those with exacerbations not fully responsive to inhaled therapies, former smoking is a reason to consider azithromycin, whereas chronic bronchitis (also referred to as chronic mucus hypersecretion [CMH]) with severe obstruction is a reason to consider roflumilast. Overlap conditions in which diseases such as asthma, sleep apnea, depression, lung cancer, or pulmonary fibrosis are identified will guide alternate treatments or referrals. Overall, phenotyping is increasingly used to guide better treatment in individuals with COPD.
Exacerbation history characterizes a particularly important treatable trait. The GOLD report defines the exacerbation phenotype based on 2 or more exacerbations requiring treatment or one requiring an emergency department visit or hospitalization.1 However, the frequent exacerbation phenotype, defined as ≥ 2 exacerbations per year based on the Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-points (ECLIPSE) study,11 is not very stable. Most individuals experience variable numbers of exacerbations year to year.12 Additional risk factors guiding whether to increase preventive treatments for exacerbations include elevated eosinophils, gastroesophageal reflux disease, and poor baseline health status.11,13,14 Although the exacerbation-prone phenotype is relatively unstable, it is important to identify. Exacerbations greatly increase the risk of many poor outcomes, including cardiovascular events, subsequent hospitalizations, and death.11,15,16
Asthma-COPD overlap (ACO) is also a clinically important phenotype. Defining this entity is difficult because these individuals have been traditionally understudied. The subgroup has largely been excluded from studies targeting asthma or COPD exclusively. Therapy guidelines for these individuals have thus primarily been extrapolated from studies from which they were excluded. Whereas a standard definition is lacking, a description endorsed by Global Initiative for Asthma (GINA)/GOLD considers ACO when several features of both are identified.17 They suggest using a checklist of asthma and COPD features to determine if the ACO categorization applies; however, this approach has not been validated. Regardless of the definition used, studies have found that ACO is a common condition.18,19 Importantly, individuals with ACO have worse outcomes than asthma or COPD alone and higher health care costs.18,19 Thus, recognizing ACO and ensuring proper treatment is warranted. The GINA/GOLD guidelines from 2017 suggested that ICS be considered in this ACO population.17 The most recent GOLD guidelines from 2022, however, recommend that ICS only be considered in combination with a long-acting muscarinic antagonist (LAMA) and long-acting β agonist (LABA) in individuals with COPD.1 Taken together, the guidelines support triple therapy (ICS/LABA/LAMA) over ICS alone, LABA/LAMA, or ICS/LABA combination therapies in this population.
Radiographic and Physiologic Features
The significance of structural and physiologic heterogeneity in COPD is increasingly recognized and better characterized with advances in lung function testing and imaging. Diffusing capacity of the lungs for carbon monoxide (DLCO), a measure of the ability of the lungs to transfer gas from the air to the vascular space, has long been used to characterize the degree of emphysema in ever smokers with airway obstruction. Hypercapnia, as determined by PaCO2, is observed in many individuals with COPD, particularly with increasing disease severity. Two of the most common reasons for this hypercapnia are increased dead-space ventilation and decreased respiratory drive.20 Dead-space ventilation increases in the setting of parenchymal tissue destruction, along with airway and vascular abnormalities. The respiratory drive decreases in the setting of hyperinflation, with the inability of the respiratory muscles to increase respiratory capacity when needed for exertion, compounded by a depressed central respiratory drive, potentially a mechanism to conserve energy in a system that is chronically stressed.
Whereas DLCO and PaCO2 have long provided additional context on COPD heterogeneity and severity, the clinical implications of other common abnormalities are being newly reevaluated, particularly in smokers without spirometrically confirmed post-bronchodilator airway obstruction. A substantial proportion of smokers with preserved spirometry have respiratory symptoms, exacerbation-like events, and evidence of airway disease by imaging.21 Determining which patients may be at greatest risk for progression to COPD may be important for early COPD diagnosis. It appears that individuals with preserved ratio-impaired spirometry (PRISm), defined by a proportionate decrease in FVC and FEV1 with a normal FEV1/FVC, may be one such at risk group.22,23 Individuals with PRISm are more likely to be symptomatic and to progress to COPD than smokers with preserved lung function without PRISm.23-26 Whereas there are no specific therapies recommended for individuals with PRISm, they should be monitored for lung function decline given their propensity to progress.
Newer methods may be used to identify abnormalities in the small airways, a main site of COPD pathology, that are difficult to detect using traditional physiologic measurements. This may be particularly useful early in disease when abnormalities accumulating in the small airways may not yet translate into changes in FEV1. A physiologic metric that can more accurately assess small airway disease, forced oscillometry, is growing in research.27,28 This technique applies an oscillating signal during tidal breathing to measure changes in pressure and flow and compute impedance. Higher oscillation frequencies reflect large airways, and lower oscillation frequencies reflect properties of the entire respiratory system, including the small airways. A contemporary imaging technique, parametric response mapping (PRM), also characterizes small airway disease better than conventional imaging techniques. PRM employs a voxel-based computed tomography (CT) imaging technique that co-registers inspiratory and expiratory scans to distinguishes normal lung from emphysema and functional small airways disease (fSAD).29 These newer techniques are thus useful in discerning structural abnormalities that may contribute heterogeneously to COPD phenotypes.
In addition to small airway disease, imaging techniques can detect other structural abnormalities including emphysema and abnormalities in the larger airways. Imaging-based phenotyping incorporating these various abnormalities is now being executed using clustering analyses. In a study of the SubPopulations and InteRmediate Outcome Measures In COPD Study (SPIROMICS) cohort, investigators identified 4 imaging clusters.30 Cluster 1 included younger individuals with greater body mass index and milder disease, who had the greatest progression in small airway disease. Cluster 2 had less emphysema and fSAD but greater large airway narrowing. Cluster 3 had changes in emphysema but not fSAD metrics over time, and Cluster 4 had the most severe emphysema and fSAD alterations at baseline and increases in fSAD over time. In another analysis using data from Genetic Epidemiology of COPD (COPDGene) and Detection of Early lung Cancer Among Military Personnel (DECAMP), 3 imaging-based clusters were identified.31 The preserved cluster had the lowest scores for interstitial and airway abnormalities. The interstitial predominant cluster had more airway and interstitial abnormalities; the emphysema cluster had greater emphysema but fewer airway and interstitial abnormalities. Only the emphysema group showed decline in lung function over time; however, both the interstitial and emphysema groups had greater declines in exercise capacity and more exacerbations than the preserved group in COPDGene. In DECAMP, genes involved in pro-inflammatory pathways distinguished these 3 groups, with the greatest differences between the preserved and emphysema-predominant groups. Whereas further studies are needed, contemporary imaging-based phenotyping studies suggest that these techniques may eventually assist in determining individuals at risk for progressive disease.
Another imaging biomarker that has recently been used in phenotyping detects mucus plugging. Chronic mucus hypersecretion is an important pathologic finding in COPD, and symptoms of CMH are an associated outcome. Another is mucus plugging of the small airways that could lead to air-flow limitations and if completely occluded poorly ventilated and thus oxygenated lung units distal to the plugging. A study in SPIROMICS found that over half of smokers had mucus plugs on their CT scans.32 Despite only a third of individuals with high mucus plugging scores having symptoms of CMH, plugging was associated with worse lung function and oxygen saturation, particularly in individuals with minimal emphysema. High mucus plug scores were also associated with greater number of exacerbations and worse functional status. Thus imaging-based mucus characterization adds to our understanding of the contributions of mucus to COPD pathology and phenotyping, linking mucus to outcomes beyond symptoms.
Molecular Phenotyping in COPD
Molecular phenotyping or endotyping, where biologic rather than clinical similarities is used to subgroup disease, may best allow for a precision medicine approach to treatment. A therapy with a specific biologic target can be administered to an individual in which that biology is dysregulated and is thus most likely to impact clinical care. This becomes important when the biology underlying a specific clinical phenotype is not apparent. For example, the pathobiology underlying the physiologic or imaging-based characterization of small airway disease could include extracellular matrix remodeling, mucus plugging, and epithelial reprogramming. Thus, we cannot always determine the pathobiology that needs to be treated based on an individual’s clinical or imaging-based characteristics.
Disordered mucus pathology, with the downstream features of mucus plugging or CMH, appears to be enhanced in a subgroup of individuals with COPD. Whereas clinical and radiographic features could be suggestive of mucus pathology, mucus abnormalities can be studied directly by measuring airway mucus concentrations as well. For instance, Kesimer et al33 found that total mucins measured in the sputum were associated with worse outcomes including greater chronic bronchitis, phlegm production, airway obstruction, and exacerbations in COPD. They also found that Mucin 5AC (MUC5AC), generally considered a pathologic respiratory mucin, more reliably associated with COPD manifestations than MUC5B, the typical secreted respiratory mucin.33,34 They found associations not only between MUC5AC and chronic bronchitis symptoms, as might be expected, but also with exacerbations, lung function, and measurements of small airway disease. Measuring mucin concentrations may thus provide additional information on mucin pathology beyond identifying mucus-associated clinical or radiographic features.
Molecular phenotyping has best been studied in terms of immune responses. These include the Type 2 (T2) response, classically associated with an allergic response, elevated eosinophils, and steroid responsiveness; the T1 response, classically considered antiviral and associated with elevated interferons, Interleukin 2 (IL-2), and lymphotaxin alpha; and the T17 response, classically considered a response to extracellular bacteria and associated with elevation in neutrophils and the IL-17 family of cytokines, as well as steroid unresponsiveness. However, immune-based molecular phenotypes are more complex than this, involving intricate communication between immune and structural cells both systemically and at the airway mucosal surface.
Blood eosinophils, as a marker of T2 inflammation, are the best studied molecular phenotyping biomarker in COPD. Several post hoc analyses of clinical trials found that blood eosinophils identify individuals in whom ICS will best aid in exacerbation prevention.35-39 These data resulted in blood eosinophils being added to the GOLD guidelines to guide ICS use in exacerbation-prone COPD. However, eosinophils do not correlate well with airway eosinophil levels in COPD as measured by sputum eosinophils.40 Furthermore, trials of the anti-IL5 biologics that target eosinophilic inflammation and reduce exacerbations in eosinophilic asthma have not reached their primary end points when targeting subjects with high blood eosinophils in COPD.41-43 Recent data also show that triple therapies (ICS/LABA/LAMA) reduce exacerbations to a greater extent than LABA/LAMA regardless of eosinophil count.44 Although, as a caveat, triple therapy exacerbation reduction increases with increasing blood eosinophil levels.36 Overall, blood eosinophils may be useful in guiding ICS use in COPD but has limitations as a biomarker.
Eosinophils are also not the only downstream effector cells of the T2 response. There are now several places along the T2 pathway that can be targeted therapeutically, and subgrouping COPD in ways to best utilize these treatments is warranted. Thymic stromal lymphopoietin and IL-33, the upstream alarmins that initiate the T2 inflammatory cascade in response to a stimulus, can be targeted by biologics. Airway remodeling, goblet cell metaplasia, and elevated immunoglobulin E are all downstream effects of the T2 response and may be other areas to target. Our group has developed a gene expression marker of the T2 response in the bronchial airways.45 This T2 signature is associated with other markers of a T2 response, such as increased sputum eosinophils and spirometric bronchodilator reversibility. In a secondary analysis of a randomized controlled trial of ICS versus placebo, the T2 signature was also associated with a better response to ICS for measures of hyperinflation (residual volume/total lung capacity and inspiratory capacity) even after adjustments for eosinophil count. Thus, measures of T2 inflammation beyond blood eosinophils may have utility in COPD; however, further studies are needed.
IL-17-driven and neutrophilic inflammation are considered more classical COPD pathologic responses, associated with corticosteroid unresponsiveness and emphysema,46-49 but not studied as well in relation to molecular phenotyping as the T2 response. Our group, however, generated a T17 gene expression signature based on airway epithelial cell culture stimulation with IL-17.50 The signature was tested in psoriatic lesions treated with anti–IL-17 biologics in which the signature was associated with an improved response to these biologics. In COPD, we found that, as expected, the T17 signature was associated with airway neutrophil and macrophage accumulation. The signature was also associated with a lack of improvement in lung function, as measured by change in FEV1, to ICS over 30 months. This association was evident even after adjusting for eosinophils or the T2 gene signature, suggesting that the T17 signature marked steroid unresponsiveness. Thus, markers of immune responses unrelated to T2 inflammation may be relevant in COPD.
Finally, molecular phenotypes can be considered in the context of exacerbations and the associated altered biology. Understanding exacerbation molecular phenotypes is even more complex than those identified at disease stability. Heterogeneous precipitants, including viruses, bacteria, and allergens, should be considered as driving exacerbations in concert with heterogeneous underlying chronic biology. Bacteria are cultured out in ∼50% of exacerbations.51,52 However, these bacteria can be present even during disease stability, so it is difficult to know whether they are associated with true infections or colonization. Viruses may be more important precipitants of exacerbations in COPD than once thought, as COPD exacerbation burden decreased substantially during the COVID-19 pandemic when greater social isolation and masking were utilized.53-57 The host response to both microbial and non-microbial precipitants, however, plays a critical role in exacerbation biology, driving a clinical response that does not occur in individuals without airway disease. The host inflammatory response at exacerbation seems to be similar to what is seen during disease stability with T1, T2, and T17/pro-inflammatory responses predominating in subgroups.58,59 These molecular phenotypes are associated with increased viruses, eosinophils, and bacteria, respectively. If molecular phenotyping during exacerbations is implemented in the future, it could provide critical information to direct therapies and predict outcomes. For instance, molecular phenotyping could guide more judicious use of antibiotics and oral steroids. Although they are the mainstays of COPD exacerbation therapy, both antibiotics and steroids are associated with major adverse consequences. Thus, a more discriminating approach to their use could be beneficial.
Summary
There is a growing importance placed on differentiating individuals based on their clinical and molecular characteristics. Treatable traits are now emphasized in guideline-based approaches to COPD treatment. Clinical phenotyping is becoming increasingly refined, informed by technological advances such as innovations in physiologic and imaging-based metrics. Molecular phenotyping of stable disease and exacerbations may allow for more accurate approaches to target therapeutics to an individual’s underlying biology.
Discussion
MacIntyre: Take somebody who smokes a lot of cigarettes and has a lot of tobacco material being delivered into the lungs. Why is one person going to get a particular inflammatory response and develop a more bronchitic phenotype, and why does somebody else smoking the same cigarettes end up with emphysema? I know there’s not a simple answer to that, but I’m interested in your thoughts. To date myself a bit, I remember a joke from back when Clinton was president; because he didn’t inhale, he was going to get bronchitis; and if he had inhaled, he would have gotten emphysema.
Christenson: I think it’s the million-dollar question, why do people get what they get? There are probably many answers, and I have a fellow studying resilience. Why do some people never get COPD despite smoking like chimneys, right? And they’re totally fine. It’s a very interesting phenomenon. Some of the ideas that have come forth, that I didn’t really address in the talk, is dysanapsis or how the airways are formed might mean that certain people have smaller airways where more particulate matter can get lodged over time. I know Ben Smith had a JAMA article where dysanapsis seemed to be linked with worse outcomes.1 That may be one of the reasons, but certain people’s airways are formed in certain ways, and it means that some particles can be trapped more easily. And potentially that could even determine if you have a more chronic bronchitis phenotype versus a more emphysema phenotype. Perhaps it is that you’re getting particles trapped in different places? However, I think that when I was talking about that exposome model that we’re beginning to really understand a lot more that, “Hey COPD is a lot more than just smoking.” Granted, smoking is awful and we want to ensure that we help our patients stop smoking, but there are so many exposures that are potentially contributing to what happens to a patient later in life. We know that patients with asthma are more likely to get COPD later. Do they have a different type of inflammation than others? You can tell that I’ve been thinking about this a lot, and I don’t have a great answer, but I can certainly wax philosophical about it.
MacIntyre: It’s a fascinating question, and I appreciate you sharing your thoughts on it.
Haynes: I have a question about FENO. Does exhaled NO help you phenotype or decide who might respond to corticosteroids?
Christenson: Yes, I think that’s being asked now. I think there’s always been the thought that smoking can change your FENO, and so was it ever really as good as asthma? There are some data coming out. Certainly the pharma companies as they’re thinking about biologics or inhaled steroids for certain patients are very interested in figuring out who’s a responder and knowing that eosinophils are not the end all, be all, in COPD. So people are certainly starting to look at FENO as a potential biomarker of type 2 high disease. I think there’s a lot more that people are trying to study and understand about that biomarker, but it’s certainly attractive, and it might be useful.
Criner: Very good talk. I have two questions for you. The first is, how much of a drawback do you think it is that we’re describing phenotypic characteristics of patients with COPD because these are mainly large observational studies that are conducted in subjects that have characteristics that predispose them to COPD with control subjects that are very small in number. So my question to you is how much of this is population variability as opposed to characteristics of a disease?
Christenson: I will say that this is one of the reasons I don’t use the word endotype when talking about molecular phenotypes, and certainly maybe we must have that for clinical phenotypes as well. Molecular phenotype means there’s a subgroup with a certain type of underlying biology, and when you use the word endotype, it means someone that has underlying biology that we know responds to a particular treatment. That’s at least how it was originally formulated. We know there’s eosinophil-high COPD, well, do we actually? A lot of these are post hoc analyses of randomized controlled trials. But we could say that so far it does look like eosinophil-high COPD seems to respond better to inhaled corticosteroids, and it is probably an endotype. But responding better to therapy is not super useful, at least practically.
Criner: Right. The second question stems from that. How much of this phenotypic variation do you see associated with biological pathways outside of the lungs that are related to systemic differences in cardiac or other forms of non-pulmonary disease that we can really believe that this is a systemic permutation that predisposes the lungs to a systemic factor that’s distinct from a different type of phenotype in COPD?
Christenson: I think that’s a very good question. People are starting to think about that more closely, and maybe people have been trying to think about it to some extent for a long time in that people are measuring biomarkers in the blood, and a lot of those studies aren’t well done to look at an actual phenotype. But I will say there are certain characteristics that seem to be more associated with a systemic biomarker response. Certainly when I look at gene expression, which is what I do, biologically we see people who have exacerbations seem to have more systemic markers, whereas some of these other clinical phenotypes aren’t really associated with as much change. It does seem that there are certain phenotypes that have more systemic inflammation, and I think the more biomarker data we have in larger groups of subjects the better we will be at teasing some of those things out. So stay tuned as we gather more data on these patients.
MacIntyre: I would like to ask you about one of the phenotypes that I’m going to talk about with respiratory failure: hypercapnia. I noticed that didn’t make your list of characteristics. Why are some people prone to hypercapnia? In these individuals, the brain tells the respiratory muscles to cool it in an effort to preserve muscle function. In contrast, others appear to preserve PaCO2 with a dyspnea-driven whip to breathe. Any thoughts as to how the lungs and the brain are talking to each other in this disease?
Christenson: That’s a good question that I think is very understudied. As far as how is that phenotype working and who are those people and how are they different? I’m not sure that I have a wonderful answer for you, maybe somebody else does, as far as why are there certain people who do this. But getting back to Jerry’s question as well, we know that cardiovascular comorbidities are very much linked to certain COPD phenotypes, and it seems to be more than just the fact that they share certain risk factors, although that’s certainly an issue. It seems to be the same thing here. It’s not just that they share these risk factors and they’ll be more likely to get sleep apnea because they share these risk factors, it seems to be a particular phenotype. I do think there are certain people who seem to have more systemic disease, whereas some people are keeping it in the lungs, so to speak, or the rest of their body seems to be able to deal with the particulate matter better than others. To me, it’s a very interesting question that I’m not sure I have a good answer for.
MacIntyre: Let’s go back in time. You showed the image of Frank Netter’s original blue bloater and pink puffer. Is it still reasonable to think that the blue bloater has more heart disease and bronchitic symptoms, and the pink puffer is more of the emphysematous type? Or is that image way too simplified?
Christenson: I feel that those are extremes of the phenotypes. Maybe it’s not oversimplified, but those are the extremes of the examples. But what we can see is that there are a lot of people who fall in between. Some of that data that I brushed over a little bit but is very interesting, the data on mucus plugging and CT scans where they’re seeing that some of the people who have all this mucus in there are not chronic bronchitics. It’s associated with symptoms, but having the symptoms does not mean you’re going to have the mucus plugs. They’re not completely 1:1, but they may share similar underlying biology, and it’s just how they’re manifesting. Maybe it’s because their airways are more inflamed lower down in those small airways, but it’s interesting again that we’re seeing these different manifestations. The imaging, new physiology, and molecular phenotypes add all this complexity. So does it help us more or does it make it more complex? Two sides of the same coin.
Garvey: That was a great talk. I have a question about your thoughts on modifiable risk factors. You mentioned a lot of important comorbidities, and I’m thinking of depression specifically. As you know, in rehab we’re required to measure mood, typically with the PHQ-9, and it’s stunning how many people have findings consistent with depression, which is often undiagnosed and untreated. I think we’re missing an opportunity of managing modifiable risk factors and smoking. You have a lot of experience in this area of understanding and addressing this. Any thoughts on how we could possibly look at doing a better job?
Christenson: Yes, I only touched on it briefly here; but when I give more general COPD talks, I really try to hammer home that there are comorbidities that are very prevalent in COPD, and I think we need to do a better job of screening for them. A lot of people see asthma/COPD overlap because people complain about it; it bothers them. Whereas I think particularly in this population they’re living with depression. If you’re not screening for it, you’re not going to find it, like sleep apnea, fibrosis, cardiovascular comorbidities. We really need to be educating people that COPD is more than just inhalers, and we need to work on identifying depression and cardiovascular disease. Also identifying exacerbations because patients don’t always know what they are and so really talking to them about what does this look like. And one of the reasons, as we talked about with exacerbation phenotype, they’re so strikingly horrible for outcomes including quality of life. So really trying to control their symptoms and prevent exacerbations may help improve their quality of life and potentially their mental health. Maybe that would go a long way of trying to get some of that better controlled. But treating depression and screening for depression is important in these patients.
Orr: Thanks, I really enjoyed that. I’m still trying to formulate this in my mind, but I’m thinking about the variability in some of these phenotypes over time. For example, if you look at eosinophils over time, it can fluctuate wildly. Is that really a phenotype? Should we be focused on things that are variable or that are more stable over time when you’re approaching these patients? It’s hard to call it a phenotype if it’s sort of fleeting.
Christenson: It turns out that type 2 inflammation we basically say you look for eosinophils in asthma patients too, if you’ve ever had high eosinophils ever because they are so fleeting that you can still treat with biologics, and it does seem to help. How much of that holds true for COPD? We’ll see. But it does look like, despite the fluctuations, that some of the biomarkers in longitudinal studies the data show that they seem to be this group of type 2 high and neutrophil high seem to be somewhat stable over time, whereas the patients who get these viral exacerbations are type 1 interferon-high inflammation. That seems to be spontaneous, and it seems to fluctuate a lot. I agree with you that we need to do more as phenotyping grows in COPD, and I think it is, hopefully, we can really understand longitudinally what’s important in some of these groups. And a lot of that is influenced by are they smoking or not, are they taking medications like steroids or not, have they had exacerbations recently or not. I think some of it is that we’re still trying to separate it out. In asthma, it’s much better separated out; type 2 high responds to these therapies very well, whereas in COPD there’s a lot more complexity. Some of that might be that patients are aging, their immune systems are aging, some people are smoking, and so we don’t see the same responses in different people, but some of that needs to be sorted out because it is complex.
Mike Hess: Do you see a big role in studying the microbiome of the lung and how it interacts with other microbiomes in the body in determining phenotypes or watching them progress?
Christenson: Absolutely. It’s somewhat understudied in COPD as well, but I think it’s so important. One of the big issues that’s happening is getting dysbiosis in the airways, again not with everybody but in certain people where potentially they get more mucus built up and that causes the microbes to have a lovely new environment to hang out in those airways and that brings more inflammation and then the spiral downward. So figuring out who are those patients, are there some of these patients who need to be treated with antimicrobials because they get this colonization, which isn’t really colonization that’s causing the problem just not necessarily an acute infection? Or do we need to be treating some of those patients with mucolytics or a better mucolytic than what we have now, which don’t do a great job? Or do we treat the underlying inflammation? There are certain folks who are doing some great work to look at that, but as we start to build these big data sets like SPIROMICS, we start to have microbial data, we have inflammatory data, where we can start teasing apart some of the overlap between the biological entities we’re seeing. And clinical features will also help, so absolutely I think there’s a role for looking at the microbiome. And in the gut as well, there are certainly gut-lung inflammatory axes there that are potentially disruptive.
Footnotes
Dr Christenson discloses relationships with AstraZeneca, Sanofi/Regeneron, and GlaxoSmithKline.
Dr Christenson presented this paper at the 59th Respiratory Care Journal Conference, COPD: Current Evidence and Implications for Practice, held June 21–22, 2022, in St Petersburg, Florida.
REFERENCES
- 1.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Updated 2023. Available at: https://goldcopd.org/2023-gold-report-2.
- 2.Nici L, Mammen MJ, Charbek E, Alexander PE, Au DH, Boyd CM, et al. Pharmacologic management of chronic obstructive pulmonary disease. An official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med 2020;201(9):e56-e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yawn BB, Thomashaw B, Mannino DM, Han MK, Kalhan R, Rennard S, et al. The 2017 update to the COPD Foundation COPD pocket consultant guide. Chronic Obstr Pulm Dis 2017;4(3):177-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet 2022;399(10342):2227-2242. [DOI] [PubMed] [Google Scholar]
- 5.Stolz D, Mkorombindo T, Schumann DM, Agusti A, Ash SY, Bafadhel M, et al. Toward the elimination of chronic obstructive pulmonary disease: a Lancet Commission. Lancet 2022;400(10356):921-972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnes PJ. Sex differences in chronic obstructive pulmonary disease mechanisms. Am J Respir Crit Care Med 2016;193(8):813-814. [DOI] [PubMed] [Google Scholar]
- 7.Foreman MG, Zhang L, Murphy J, Hansel NN, Make B, Hokanson JE, et al. ; COPDGene Investigators. Early-onset chronic obstructive pulmonary disease is associated with female sex, maternal factors, and African American race in the COPDGene Study. Am J Respir Crit Care Med 2011;184(4):414-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sana A, Somda SMA, Meda N, Bouland C. Chronic obstructive pulmonary disease associated with biomass fuel use in women: a systematic review and meta-analysis. BMJ Open Respir Res 2018;5(1):e000246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedlander AL, Lynch D, Dyar LA, Bowler RP. Phenotypes of chronic obstructive pulmonary disease. Chronic Obstr Pulm Dis 2007;4(4):355-384. [DOI] [PubMed] [Google Scholar]
- 10.McDonald VM, Fingleton J, Agusti A, Hiles SA, Clark VL, Holland AE, et al. Treatable traits: a new paradigm for 21st century management of chronic airway diseases: Treatable Traits Down Under International Workshop report. Eur Respir J 2019;53(5):1802058. [DOI] [PubMed] [Google Scholar]
- 11.Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, Tal-Singer R, et al. ; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010;363(12):1128-1138. [DOI] [PubMed] [Google Scholar]
- 12.Han MK, Quibrera PM, Carretta EE, Barr RG, Bleecker ER, Bowler RP, et al. ; SPIROMICS investigators. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med 2017;5(8):619-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, et al. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med 2020;73:1-6. [DOI] [PubMed] [Google Scholar]
- 14.Bowler RP, Kim V, Regan E, Williams AAA, Santorico SA, Make BJ, et al. Prediction of acute respiratory disease in current and former smokers with and without COPD. Chest 2014;146(4):941-950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wedzicha JA, Seemungal TAR. COPD exacerbations: defining their cause and prevention. Lancet 2007;370(9589):786-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kunisaki KM, Dransfield MT, Anderson JA, Brook RD, Calverley PMA, Celli BR, et al. ; SUMMIT Investigators. Exacerbations of chronic obstructive pulmonary disease and cardiac events. A post hoc cohort analysis from the SUMMIT randomized clinical trial. Am J Respir Crit Care Med 2018;198(1):51-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Initiative for Chronic Obstructive Lung Disease. Asthma, COPD, and asthma-COPD overlap syndrome . Available at: https://goldcopd.org/asthma-copd-asthma-copd-overlap-syndrome. Accessed December 5, 2022.
- 18.Wurst KE, Kelly-Reif K, Bushnell GA, Pascoe S, Barnes N. Understanding asthma-chronic obstructive pulmonary disease overlap syndrome. Respir Med 2016;110:1-11. [DOI] [PubMed] [Google Scholar]
- 19.Alshabanat A, Zafari Z, Albanyan O, Dairi M, FitzGerald JM. Asthma and COPD overlap Syndrome (ACOS): a systematic review and meta-analysis. PloS One 2015;10(9):e0136065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Csoma B, Vulpi MR, Dragonieri S, Bentley A, Felton T, Lázár Z, et al. Hypercapnia in COPD: causes, consequences, and therapy. J Clin Med 2022;11(11):3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woodruff PG, Barr RG, Bleecker E, Christenson SA, Couper D, Curtis JL, et al. ; SPIROMICS Research Group. Clinical significance of symptoms in smokers with preserved pulmonary function. N Engl J Med 2016;374(19):1811-1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Regan EA, Lynch DA, Curran-Everett D, Curtis JL, Austin JHM, Grenier PA, et al. ; Genetic Epidemiology of COPD (COPDGene) Investigators. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern Med 2015;175(9):1539-1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wan ES, Hokanson JE, Regan EA, Young KA, Make BJ, DeMeo DL, et al. Significant spirometric transitions and preserved ratio impaired spirometry among ever smokers. Chest 2022;161(3):651-661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higbee DH, Granell R, Davey Smith G, Dodd JW. Prevalence, risk factors, and clinical implications of preserved ratio-impaired spirometry: a UK Biobank cohort analysis. Lancet Respir Med 2022;10(2):149-157. [DOI] [PubMed] [Google Scholar]
- 25.Wijnant SRA, De Roos E, Kavousi M, Stricker BH, Terzikhan N, Lahousse L, et al. Trajectory and mortality of preserved ratio-impaired spirometry: the Rotterdam Study. Eur Respir J 2020;55(1):1901217. [DOI] [PubMed] [Google Scholar]
- 26.Han MK, Agusti A, Celli BR, Criner GJ, Halpin DMG, Roche N, et al. From GOLD 0 to Pre-COPD. Am J Respir Crit Care Med 2021;203(4):414-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berger KI, Turetz M, Liu M, Shao Y, Kazeros A, Parsia S, et al. Oscillometry complements spirometry in evaluation of subjects following toxic inhalation. ERJ Open Res 2015;1(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Segal LN, Martinez FJ. Chronic obstructive pulmonary disease subpopulations and phenotyping. J Allergy Clin Immunol 2018;141(6):1961-1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boes JL, Hoff BA, Bule M, Johnson TD, Rehemtulla A, Chamberlain R, et al. Parametric response mapping monitors temporal changes on lung CT scans in the subpopulations and intermediate outcome measures in COPD Study (SPIROMICS). Acad Radiol 2015;22(2):186-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zou C, Li F, Choi J, Haghighi B, Choi S, Rajaraman PK, et al. Longitudinal imaging–based clusters in former smokers of the COPD cohort associate with clinical characteristics: the subpopulations and intermediate outcome measures in COPD study (SPIROMICS). Int J Chron Obstruct Pulmon Dis 2021;16:1477-1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Billatos E, Ash SY, Duan F, Xu K, Romanoff J, Marques H, et al. ; DECAMP and COPDGene Investigators. Distinguishing smoking-related lung disease phenotypes via imaging and molecular features. Chest 2021;159(2):549-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dunican EM, Elicker BM, Henry T, Gierada DS, Schiebler ML, Anderson W, et al. Mucus plugs and emphysema in the pathophysiology of air-flow obstruction and hypoxemia in smokers. Am J Respir Crit Care Med 2021;203(8):957-968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kesimer M, Ford AA, Ceppe A, Radicioni G, Cao R, Davis CW, et al. Airway mucin concentration as a marker of chronic bronchitis. N Engl J Med 2017;377(10):911-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Radicioni G, Ceppe A, Ford AA, Alexis NE, Barr RG, Bleecker ER, et al. Airway mucin MUC5AC and MUC5B concentrations and the initiation and progression of chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med 2021;9(11):1241-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bafadhel M. Eosinophils in COPD: are we nearly there yet? Lancet Respir Med 2017;5(12):913-914. [DOI] [PubMed] [Google Scholar]
- 36.Pascoe S, Barnes N, Brusselle G, Compton C, Criner GJ, Dransfield MT, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med 2019;7(9):745-756. [DOI] [PubMed] [Google Scholar]
- 37.Watz H, Tetzlaff K, Wouters EFM, Kirsten A, Magnussen H, Rodriguez-Roisin R, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post hoc analysis of the WISDOM trial. Lancet Respir Med 2016;4(5):390-398. [DOI] [PubMed] [Google Scholar]
- 38.Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomized controlled trials. Lancet Respir Med 2015;3(6):435-442. [DOI] [PubMed] [Google Scholar]
- 39.Siddiqui SH, Guasconi A, Vestbo J, Jones P, Agusti A, Paggiaro P, et al. Blood eosinophils: a biomarker of response to extrafine beclomethasone/formoterol in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2015;192(4):523-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hastie AT, Martinez FJ, Curtis JL, Doerschuk CM, Hansel NN, Christenson S, et al. ; SPIROMICS investigators. Association of sputum and blood eosinophil concentrations with clinical measures of COPD severity: an analysis of the SPIROMICS cohort. Lancet Respir Med 2017;5(12):956-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Criner GJ, Celli BR, Brightling CE, Agusti A, Papi A, Singh D, et al. ; TERRANOVA Study Investigators. Benralizumab for the prevention of COPD exacerbations. N Engl J Med 2019;381(11):1023-1034. [DOI] [PubMed] [Google Scholar]
- 42.Pavord ID, Chapman KR, Bafadhel M, Sciurba FC, Bradford ES, Schweiker Harris S, et al. Mepolizumab for eosinophil-associated COPD: analysis of METREX and METREO. Int J Chron Obstruct Pulmon Dis 2021;16:1755-1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pavord ID, Chanez P, Criner GJ, Kerstjens HAM, Korn S, Lugogo N, et al. Mepolizumab for eosinophilic chronic obstructive pulmonary disease. N Engl J Med 2017;377(17):1613-1629. [DOI] [PubMed] [Google Scholar]
- 44.Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, et al. ; IMPACT Investigators. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med 2018;378(18):1671-1680. [DOI] [PubMed] [Google Scholar]
- 45.Christenson SA, Steiling K, van den Berge M, Hijazi K, Hiemstra PS, Postma DS, et al. Asthma-COPD overlap. Clinical relevance of genomic signatures of type 2 inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2015;191(7):758-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roos AB, Sandén C, Mori M, Bjermer L, Stampfli MR, Erjefält JS. IL-17A is elevated in end-stage chronic obstructive pulmonary disease and contributes to cigarette smoke–induced lymphoid neogenesis. Am J Respir Crit Care Med 2015;191(11):1232-1241. [DOI] [PubMed] [Google Scholar]
- 47.Roos A, Sethi S, Bjermer L, Stevenson C, Erjefalt J, Stampfli M. IL-17A is specifically elevated in NTHi-associated AECOPD and end-stage COPD. Eur Respir J 2015;46(Suppl 59):3605. [Google Scholar]
- 48.Al Heialy S, Gaudet M, Ramakrishnan RK, Mogas A, Salameh L, Mahboub B, et al. Contribution of IL-17 in steroid hyporesponsiveness in obese asthmatics through dysregulation of glucocorticoid receptors α and β. Front Immunol 2020;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McKinley L, Alcorn JF, Peterson A, DuPont RB, Kapadia S, Logar A, et al. TH17 cells mediate steroid-resistant airway inflammation and airway hyperresponsiveness in mice. J Immunol 2008;181(6):4089-4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Christenson SA, van den Berge M, Faiz A, Inkamp K, Bhakta N, Bonser LR, et al. An airway epithelial IL-17A response signature identifies a steroid-unresponsive COPD patient subgroup. J Clin Invest 2019;129(1):169-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sethi S. Bacteria in exacerbations of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2004;1(2):109-114. [DOI] [PubMed] [Google Scholar]
- 52.Shimizu K, Yoshii Y, Morozumi M, Chiba N, Ubukata K, Uruga H, et al. Pathogens in COPD exacerbations identified by comprehensive real-time PCR plus older methods. Int J Chron Obstruct Pulmon Dis 2015;10:2009-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alqahtani JS, Oyelade T, Aldhahir AM, Mendes RG, Alghamdi SM, Miravitlles M, et al. Reduction in hospitalized COPD exacerbations during COVID-19: a systematic review and meta-analysis. Plos ONE 2021;16(8):e0255659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blecker S, Jones SA, Petrilli CM, Admon AJ, Weerahandi H, Francois F, et al. Hospitalizations for chronic disease and acute conditions in the time of COVID-19. JAMA Intern Med 2021;181(2):269-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huh K, Kim Y-E, Ji W, Kim DW, Lee E-J, Kim J-H, et al. Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: a nationwide claims study. Thorax 2021;76(9):939-941. [DOI] [PubMed] [Google Scholar]
- 56.Chan KPF, Ma TF, Kwok WC, Leung JKC, Chiang KY, Ho JCM, et al. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir Med 2020;171:106085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saeed MI, Sivapalan P, Eklöf J, Ulrik CS, Browatzki A, Weinreich UM, et al. Social distancing in relation to severe exacerbations of chronic obstructive pulmonary disease: a nationwide semi-experimental study during the COVID-19 pandemic. Am J Epidemiol 2022;191(5):874-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bafadhel M, McKenna S, Terry S, Mistry V, Reid C, Haldar P, et al. Acute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkers. Am J Respir Crit Care Med 2011;184(6):662-671. [DOI] [PubMed] [Google Scholar]
- 59.Ghebre MA, Pang PH, Diver S, Desai D, Bafadhel M, Haldar K, et al. Biological exacerbation clusters demonstrate asthma and chronic obstructive pulmonary disease overlap with distinct mediator and microbiome profiles. J Allergy Clin Immunol 2018;141(6):2027-2036.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
REFERENCE
- 1.Smith BM, Kirby M, Hoffman EA, Kronmal RA, Aaron SD, Allen NB, et al. ; MESA Lung, CanCOLD, and SPIROMICS Investigators. Association of dysanapsis with chronic obstructive pulmonary disease among older adults. JAMA 2020;323(22):2268-2280. [DOI] [PMC free article] [PubMed] [Google Scholar]


