Background:
The deep inferior epigastric perforator (DIEP) flap is the gold standard for autologous breast reconstruction. One or two pedicles may be used. Our study is the first to compare unipedicled and bipedicled DIEP flaps on donor and recipient site outcomes in the same patient cohort.
Methods:
This is a retrospective cohort study comparing DIEP flap outcomes between 2019 and 2022.
Results:
There were 98 patients, categorized differently for recipient or donor site. The recipient groups were unilateral unipedicled (N = 52), bilateral unipedicled (N = 15), and unilateral bipedicled (N = 31), and donor site groups were unipedicled (N = 52) and bipedicled (N = 46, including bilateral unipedicled and unilateral bipedicled). Bipedicled DIEP flaps had 1.15 times greater odds of donor site complication (95% CI, 0.52–2.55). Adjusting for operative time that was longer in bipedicled DIEP flaps (P < 0.001), odds ratio decreased, and there was a lower probability of donor site complication for bipedicled flaps (OR, 0.84; 95% CI, 0.31–2.29). Odds of recipient area complication was not significantly different between groups. Unilateral unipedicled DIEP flaps had significantly higher rates of revisional elective surgery than unilateral bipedicled DIEP flaps (40.4% versus 12.9%; P = 0.029).
Conclusions:
We demonstrate no significant difference in donor site morbidity between unipedicled and bipedicled DIEP flaps. Bipedicled DIEP flaps do have slightly higher rates of donor site morbidity, which can be partly explained by longer operative times. There is no significant difference in recipient site complications, and bipedicled DIEP flaps can reduce rates of further elective surgery.
Takeaways
Question: Is there a difference in donor and recipient site outcomes between unipedicled and bipedicled DIEP flaps?
Findings: We found no significant difference in recipient or donor site morbidity (donor OR, 1.15; 95% CI, 0.52–2.55; bipedicled versus unipedicled). Significantly longer operative time in bipedicled flaps explained increased OR (adjusted OR, 0.84; 95% CI, 0.31–2.29). Bipedicled DIEP flaps can reduce further elective surgery rates (P = 0.029).
Meaning: Bipedicled DIEP flaps do not have significantly different donor site morbidities and can reduce rates of further elective surgery; thus, they should be considered more, not just where an unipedicled flap is unsuitable.
INTRODUCTION
Breast cancer is the most commonly occurring cancer in women,1 and following mastectomy, many women choose autologous reconstruction with the deep inferior epigastric perforator (DIEP) flap.2 Women may also undergo autologous reconstruction as revisional surgery, for example, after capsular contracture with an implant. Unlike the transverse rectus abdominis flap, DIEP flaps preserve muscle. This decreases donor site morbidity3 but can be more technically challenging with longer operation times on average.4
When planning a DIEP flap, computerized tomography angiography5,6 is usually used to provide a roadmap for the pedicle course. This allows surgeons to anticipate a long intramuscular course, and it is particularly important in cases where the vessel has been divided or injured due to previous abdominal surgery. Computerized tomography angiography can also help determine the vascular layout of the flap (Moon Taylor type I, II, or III).
For unilateral DIEP flaps, one (unipedicled) or two vascular pedicles (bipedicled) may be used. Bipedicled DIEP flaps may be used for cases with uncertainty regarding flap perfusion from one pedicle7 and in low body mass index (BMI) patients with limited hemiabdomen available for reconstruction.8 Patients with large flap weights (>800 g) are also often selected to have bipedicled DIEP flaps to decrease the risk of fat necrosis.9
Although studies have found bipedicled DIEP flaps to have lower rates of flap failure or fat necrosis at the recipient site,10,11 there is discrepancy regarding donor site morbidity. Bipedicled DIEPs require increased dissection to find two pedicle origins, thus disturbing more muscle and rectus fascia and also increasing operative time.
Using 98 cases of retrospectively collected data from a single center, the objective of this study was to compare outcomes of unipedicled and bipedicled DIEP flaps on both donor and recipient sites.
METHODS
Patients
Before gathering patient data, we registered our paper as an audit at our trust.
We retrospectively collected data from electronic records of patients who underwent DIEP flap breast reconstruction at our hospital by seven consultants between September 2019 and 2022. By using a single-center study, there are standardized regulations followed during the procedure (although there is an element of personal operative technique with different consultants) and standardized postoperative care. Our trust follows the DIEP flap Enhanced Recovery After Surgery program to shorten inpatient stay, reduce postoperative pain, and improve outcomes.12–14
There were 67 unipedicled and 31 bipedicled DIEP flaps (bilateral unipedicled + unilateral bipedicled). Procedure type varied slightly with some reconstructions being immediately after mastectomy (N = 63) and others delayed (N = 35). Some of the delayed reconstructions included patients who had removal of implants and reconstructions with DIEP flaps (N = 8). There were unilateral (N = 73) and bilateral (N = 15) DIEP flaps. Additional procedures performed at the same time as DIEP flap reconstructions included axillary clearance (N = 10), sentinel lymph node biopsy (N = 18) and simultaneous breast symmetrization (N = 5).
We grouped patients differently to compare recipient and donor site complications. Recipient site groups were unilateral unipedicled DIEP flaps (N = 52), unilateral bipedicled DIEP flaps (N = 31) and bilateral unipedicled DIEP flaps (N = 15), and donor site groups were unipedicled (N = 52) and bipedicled (N = 46) DIEP flaps. The donor site bipedicled group included unilateral bipedicled and bilateral DIEP flaps. We performed this analysis because both procedures require dissection to find the origin of both pedicles; thus, theoretically, they should have the same donor site impact.
Patient baseline characteristics recorded were age and BMI at time of procedure, smoking status (defined as smoker if a current smoker or smoker in the last 8 weeks15,16), if the patient had received neoadjuvant radiotherapy or chemotherapy, whether the patient had undergone previous abdominal surgery, and presence of preoperative hernias.
Surgical Technique
Before DIEP flap elevation, perforators were marked out with a handheld Doppler (Figs. 1, 2).17 Incisions were made in the abdomen, and perforators traced back to origin of deep inferior epigastric artery and venae comitantes. At the chest, part of the third rib costal cartilage was removed, and internal mammary vessels were used as recipient vessels. The flap was disconnected from the donor site, and an end-end anastomosis with the venous coupler (synovis TM) and end-end anastomosis deep inferior epigastric artery to internal mammary artery was performed. On bipedicled flaps, the second anastomosis was retrograde to IMA/IMV. Anastomosis and flow were confirmed using the Acland swipe test or fluorescence imaging with indocyanine green. Abdominal rectus fascia was closed using PDS 2.0 Stratafix; some surgeons placed a Prolene sublay mesh, and some placed drains, according to surgeon preference. One surgeon also harvested and used a superficial inferior epigastric artery, in addition to two deep artery pedicles (N = 3; Figs. 3, 4).
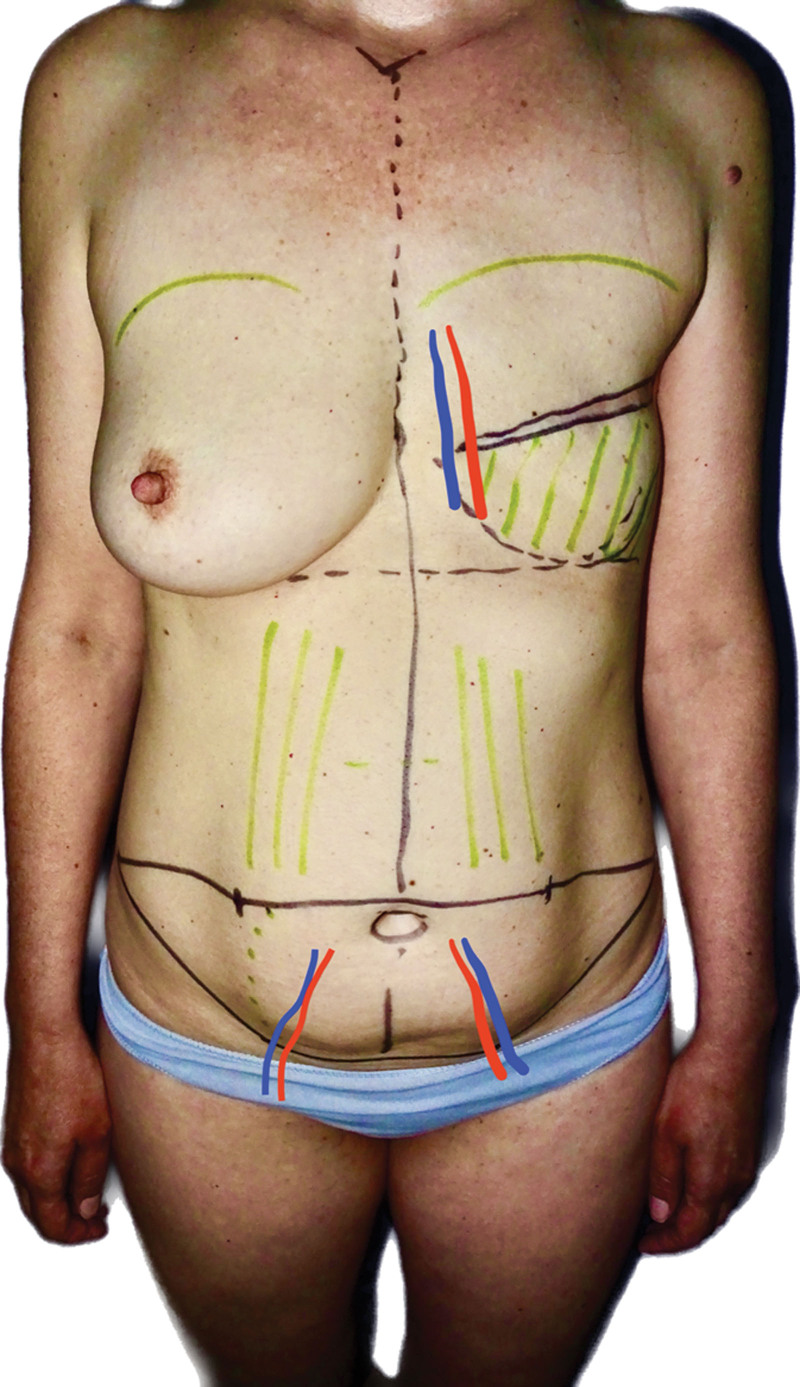
Fig. 1.
A photograph showing the map of vasculature for a bipedicled DIEP flap.
Fig. 2.
A photograph showing where anastomoses have been made for the bipedicled DIEP flap.
Fig. 3.
A photograph showing a patient postmastectomy and before reconstruction.
Fig. 4.
A photograph showing the same patient following bipedicled DIEP flap reconstruction.
From operative notes, we recorded flap weight (if bilateral we did the mean of the two flap weights), mastectomy weight (only immediate reconstructions), and whether a Prolene mesh was used upon closing the abdomen. From the World Health Organization intraoperative record, we recorded operative time.
Variables
Using operative notes, we identified the study exposure: the use of unipedicled or bipedicled DIEP flap. Patient follow-up is summarized in Figure 5 and included plastic surgeon and nurse assessment, dressing clinic notes, and hospital records. We recorded donor and recipient site complications, as summarized in Table 1. Fat necrosis can be difficult to quantify but was examined clinically using the grading system developed by Wagner et al.18 We recorded whether any emergency surgery was performed following DIEP flap reconstruction, including debridement, VAC dressing change, or relook at anastomoses.
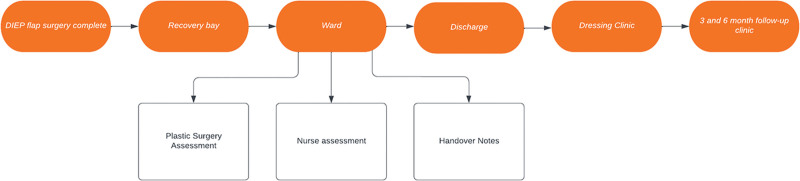
Fig. 5.
A flowchart showing a patient’s postoperative journey following completion of a DIEP flap. Plastic surgery assessment included monitoring general patient health, health of recipient and donor site, looking for signs of infection, notes on wound healing, and using Doppler to assess flap perfusion.
Table 1.
Postoperative Complication Variables Recorded, Categorized Based on Donor or Recipient Site
| Variable | Description |
|---|---|
| Donor site and breast variables | |
| Mild skin necrosis | Surgeon defined as superficial skin necrosis/sloughing |
| Fat necrosis | |
| Hematoma | |
| Infection | Cellulitis, UTI, skin infection, and pseudomonas |
| Wound dehiscence | |
| Other wound healing problems | Hypertrophic scarring, excessive bruising, overgranulation, blistering, and delayed wound healing |
| Donor site specific variables | |
| Abdominal bulge | Palpable abdominal mass |
| Breast specific variables | |
| Flap congestion | Venous or arterial, diagnosed with Doppler or during postoperative surgical exploration |
| Flap failure | Necessary removal of DIEP flap |
Finally, we recorded postoperative characteristics: inpatient stay (from date of surgery) and using clinic letters recorded whether any further elective surgery was planned or performed. This included procedures such as mastopexy symmetrization, nipple reconstruction, and removal of abdominal dog ears.
Statistical Analysis
Our study uses a retrospective cohort study design. Patient characteristics, perioperative data, and postoperative follow-up, including donor site morbidity and recipient complications, were analyzed using χ2 for categorical data and Kruskal-Wallis for nonnormally distributed continuous variables with statistical significance defined as a P value less than 0.05. Binary logistic regression was used to compare the odds of developing each complication and overall incidence of complications, all presented with a 95% confidence interval. We used univariate and mutual multivariate logistic regression to analyze whether any baseline characteristics or perioperative factors altered the odds of complication, and using this data, adjusted donor site morbidity for smoking status and operative time and adjusted recipient site complications for BMI.
RESULTS
Baseline Characteristics
Our study included 98 of 107 patients who underwent DIEP flap reconstruction at our hospital between September 2019 and 2022 and met study inclusion criteria. Exclusion criteria removed patients with incomplete follow-up (less than 4 weeks). Excluded patients did not have significantly different baseline characteristics.
The median age and BMI of all patients included was 50.7 years and 28.2 kg/m2 (classified as overweight19); neither differed significantly between groups (Table 2). Smoking status (defined as not having smoked within the last 8 weeks), whether the patient had neoadjuvant treatment, and presence of preoperative hernia did not differ significantly between groups. Of the unilateral, bipedicled DIEP flap patients, 16.1% had undergone previous abdominal surgery (including cesarean section, appendicectomy, and oophorectomy), but this did not differ significantly between groups (P = 0.233). The number of perforators harvested ranged from one to three perforators; however, over 70% of unilateral cases used only one perforator.
Table 2.
Patient Baseline Characteristics for Unipedicled and Bipedicled DIEP Flaps
| Characteristics | Unipedicled (n = 52), N (%) or Median (IQR) | Bipedicled (n = 46), N (%) or Median (IQR) | P |
|---|---|---|---|
| Age, y | 50.7 (45.8–59.1) | 51.3 (43.3–59.8) | 0.776 |
| BMI, kg/m2 | 26.4 (23.9–30.4) | 28.8 (26.5–31.9) | 0.077 |
| Smoker in last 8 wks, n (%) | |||
| No | 48 (92.3) | 40 (90) | 0.382 |
| Yes | 4 (8.23) | 6 (10) | |
| Previous radiotherapy, n (%) | |||
| No | 42 (80.8) | 36 (78.3) | 0.758 |
| Yes | 10 (19.2) | 10 (21.7) | |
| Previous chemotherapy, n (%) | |||
| No | 43 (82.7) | 36 (78.3) | 0.580 |
| Yes | 9 (17.3) | 10 (21.7) | |
| Previous abdominal surgery, n (%) | |||
| No | 47 (90.4) | 41 (89.1) | 0.838 |
| Yes | 5 (9.6) | 5 (10.9) | |
| Preoperative hernia, n (%) | |||
| No | 49 (94.2) | 43 (93.5) | 0.877 |
| Yes | 3 (5.8) | 3 (6.52) | |
P values are from the χ2 and Kruskal-Wallis tests as appropriate.
IQR, interquartile range.
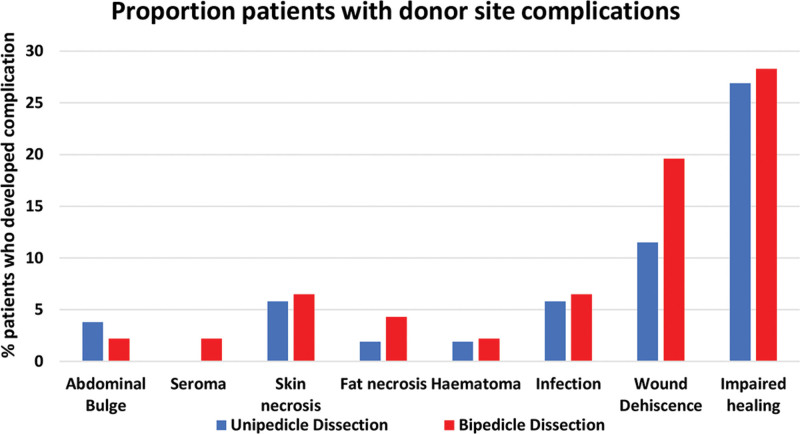
Donor Site Complications
In our study, only two patients required further emergency surgery for abdominal complications, and this was due to one abdominal hematoma and one case of fat necrosis. All other donor site complications were minor and classified as Clavien Dindo grade 1, managed nonoperatively.20 There were 63 donor site complications in 43 patients (44% patients; Table 3), almost all of which were minor. The most common donor site complication was impaired healing (27.6% patients; Fig. 6). This included overgranulation, erythema, hypertrophic scarring, blistering, and delayed healing. Overall, there was no significant difference between the total number of donor site complications between unipedicled and bipedicled DIEPs (P = 0.739).
Table 3.
The Number of Donor Site Complications. Proportion Column Is Percentage of Patients Who Had the Complication
| Complication | Unipedicle Dissection (N = 52) | Bipedicle Dissection (N = 46) | P |
|---|---|---|---|
| N (% | N (% | ||
| Abdominal bulge | 2 (3.8) | 1 (2.2) | 0.632 |
| Seroma | 0 (0) | 1 (2.2) | 0.285 |
| Skin necrosis | 3 (5.8) | 3 (6.5) | 0.877 |
| Fat necrosis | 1 (1.9) | 2 (4.3) | 0.487 |
| Hematoma | 1 (1.9) | 1 (2.2) | 0.930 |
| Infection | 3 (5.8) | 3 (6.5) | 0.877 |
| Wound dehiscence | 6 (11.5) | 9 (19.6) | 0.271 |
| Impaired healing | 14 (26.9) | 13 (28.3) | 0.882 |
| Overall | 30 (57.6) | 33 (71.7) | 0.739 |
Overall percentage = total number of donor site complications/number of patients in the group. P values are from the χ2 test. Impaired healing includes hypertrophic scarring, excessive bruising, overgranulation, blistering, and delayed wound healing.
Fig. 6.
A bar chart showing donor site complications for unipedicled and bipedicled DIEP flaps.
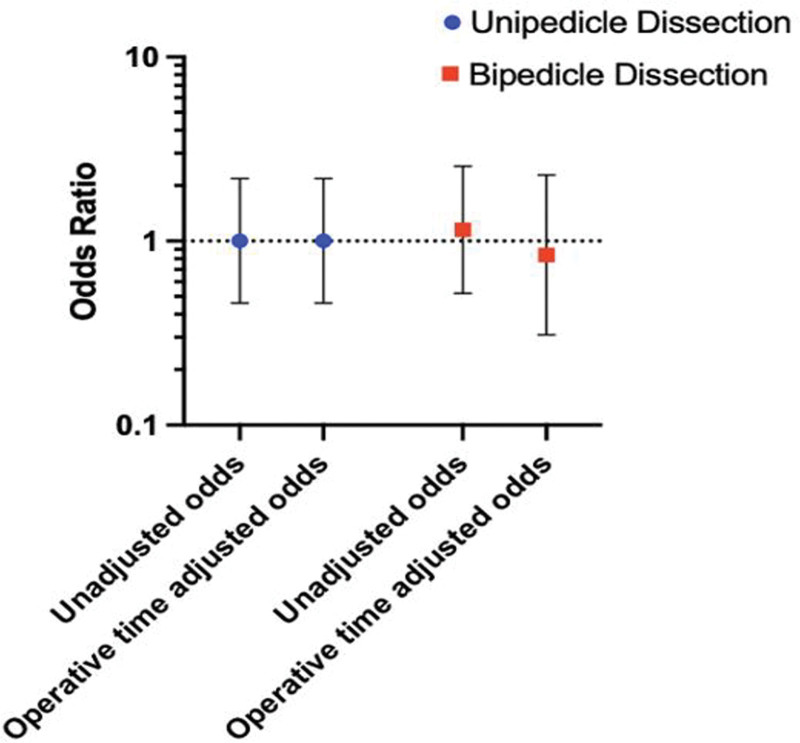
Before operative time and smoking status adjustment, the odds of a donor site complication after a bipedicled DIEP flap were 1.15 times higher than for unipedicled DIEP flaps [95% confidence interval (CI), 0.52–2.55; Table 4]. However, after adjusting odds of donor site complication for operative time, which was significantly longer in bipedicled DIEP flaps (P < 0.001), there was an adjusted odds ratio of 0.84 (95% CI, 0.31–2.29; Table 4; Fig. 7) for bipedicled versus unipedicled DIEP flaps. This suggests that the significantly longer operative time in bipedicled DIEPs partially explained the increased donor site morbidity. Smoking status appeared to increase the odds of donor site morbidity in univariate analysis (OR, 6.07; 95% CI, 1.21–30.22), so we adjusted donor site complications for smoking status. However, this had minimal effect on odds of donor site morbidity (OR, 1.05; 95% CI, 0.46–2.41).
Table 4.
The Odds Ratio of Having a Donor Site Complication Using Logistic Regression and Adjusted for Smoking Status (Smoker versus Nonsmoker in Past 8 Weeks) and Operative Time, Respectively
| Procedure Type | Univariate | Smoking Status Adjusted | Operative Time Adjusted |
|---|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| Unipedicled | 1.00 (0.46–2.18) | 1.00 (0.46–2.18) | 1.00 (0.46–2.18) |
| Bipedicled | 1.15 (0.52–2.55) | 1.05 (0.46–2.41) | 0.84 (0.31–2.29) |
Fig. 7.
A forest plot showing odds of donor site morbidity in bipedicled vs unipedicled DIEP flaps, before and after adjusting for operative time.
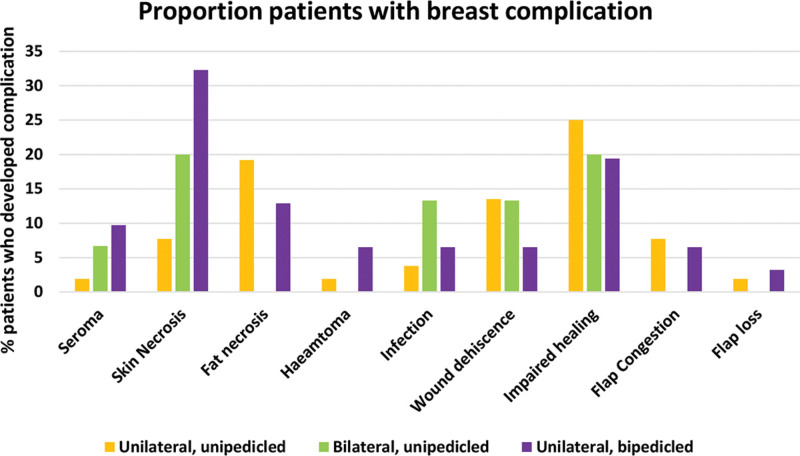
Recipient Site Complications
Unilateral, unipedicled DIEPs had the most recipient site complications (80.8%; Table 5); however, the difference between groups was not statistically significant (P = 0.636). The most common recipient area complication was impaired wound healing (Fig. 8), classified as Clavien Dindo grade 1, a minor complication. For unilateral DIEP flaps, fat necrosis was higher in unipedicled versus bipedicled DIEP flaps (19.2% versus 12.9%). Flap congestion was also higher, and overall, there were 74 recipient area complications in 46 patients (47% patients), most of which were minor.
Table 5.
The Number of Donor Site Complications; Proportion Column is Percentage of Patients Who Had the Complication
| Breast Complications | Unilateral, Unipedicled (n = 52) | Bilateral, Unipedicled (n = 15) | Unilateral, Bipedicled (n = 31) | P |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Seroma | 1 (1.9) | 1 (6.7) | 3 (9.7) | 0.286 |
| Skin necrosis | 4 (7.7) | 3 (20.0) | 10 (32.3) | 0.016 |
| Fat necrosis | 10 (19.2) | 0 (0) | 4 (12.9) | 0.166 |
| Hematoma | 1 (1.9) | 0 (0) | 2 (6.5) | 0.386 |
| Infection | 2 (3.8) | 2 (13.3) | 2 (6.5) | 0.400 |
| Wound dehiscence | 7 (13.5) | 2 (13.3) | 2 (6.5) | 0.595 |
| Impaired healing | 13 (25.0) | 3 (20.0) | 6 (19.4) | 0.596 |
| Flap congestion | 4 (7.7) | 0 (0) | 2 (6.5) | 0.568 |
| Flap loss | 1 (1.9) | 0 (0) | 1 (3.2) | 0.776 |
| Overall | 43 (82.7) | 11 (73.3) | 32 (103.2) | 0.379 |
Overall percentage = total number of donor site complications/number of patients in the group. P values are from χ2 test. Impaired healing includes hypertrophic scarring, excessive bruising, overgranulation, blistering, and delayed wound healing.
Fig. 8.
A bar chart showing recipient complications for unipedicled and bipedicled DIEP flaps.
The odds of recipient site complication did not differ significantly between groups (Table 6). Before BMI adjustment, the odds of a recipient site complication were higher in unilateral, bipedicled DIEP flaps; however, after adjustment, odds decreased drastically. This shows that the 10% higher BMI in unipedicled DIEP flaps (median BMI 29.0 bipedicled versus 26.4 unipedicled) may explain the increased odds of recipient site complications rather than the use of two pedicles. Importantly, the difference in odds of recipient site complication was from minor not major complications.
Table 6.
The Odds Ratio of Having a Donor Site Complication Using Logistic Regression and Adjusted for BMI
| Procedure Type | Univariate | BMI Adjusted |
|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| Unilateral, unipedicled | 1.00 (0.46–2.18) | 1.00 (0.46–2.18) |
| Bilateral, unipedicled | 0.63 (0.19–2.10 | 0.44 (0.12–1.56) |
| Unilateral, bipedicled | 1.75 (0.71–4.29) | 1.19 (0.46–3.12) |
Perioperative and Postoperative Data
There were quite a few differences between groups regarding perioperative data. Unsurprisingly, median operative time was significantly the longest in bilateral, unipedicled DIEP flaps (9 h 8 min) followed by unilateral bipedicled DIEP flaps (8 h 29min) and unilateral unipedicled DIEP flaps (7 h 40 mins; P < 0.001; Table 7). There was a significant difference in proportion of patients undergoing immediate versus delayed DIEP flap reconstruction (P = 0.025). Unilateral unipedicled DIEP flaps comprised almost equal proportions (27 immediate and 25 delayed) and bilateral unipedicled DIEP flaps included more immediate reconstructions (12 immediate and 3 delayed). We adjusted operative time for the proportions of immediate versus delayed reconstructions, as mastectomy before reconstruction may have accounted for the increased operative time. However, the P value operative time difference was still less than 0.001. Flap weight was the highest in unilateral, bipedicled DIEP flaps (673 g), but did not differ significantly between groups (P = 0.279).
Table 7.
Perioperative Data Based on the Surgical Type of DIEP
| Perioperative | Unilateral, Unipedicled (n = 52), N (%) or Median (IQR) | Bilateral, Unipedicled (n = 15), N (%) or Median (IQR) | Unilateral, Bipedicled (n = 31), N (%) or Median (IQR) | P |
|---|---|---|---|---|
| Use of mesh | ||||
| No | 45 | 13 | 30 | 0.300 |
| Yes | 7 | 2 | 1 | |
| Flap weight, g | 514 (351–850) | 517 (402–708) | 673 (491–943) | 0.279 |
| Operative time, h:mm | 7:40 (6:41–8:28) | 9:08 (8:40–10:08) | 8:29 (7:42–9:25) | <0.001 |
| DIEP timing | ||||
| Immediate | 27 | 12 | 24 | 0.025 |
| Delayed | 25 | 3 | 7 | |
| Mastectomy weight, g (if immediate DIEP) | 690 (419–900) | 550 (367–792) | 500 (330–700) | 0.011 |
P values are from the χ2 and Kruskal-Wallis tests as appropriate.
IQR, interquartile range.
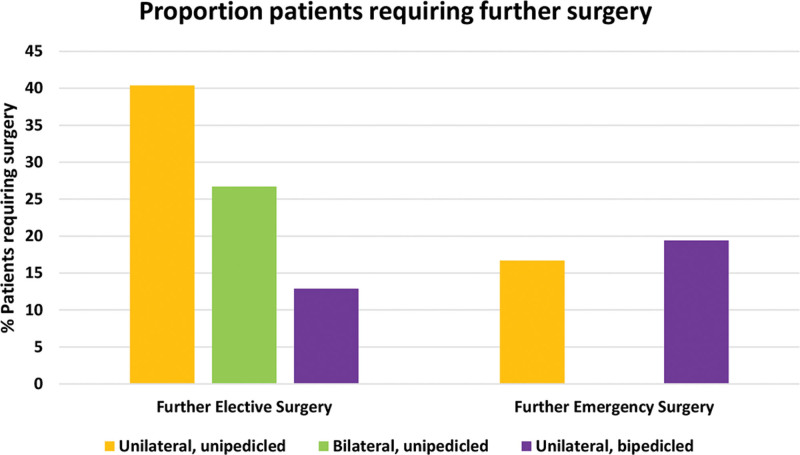
Postoperatively, all groups had a median inpatient stay of 5 days (range, 3–22 days). Unilateral unipedicled DIEP flaps had significantly higher rates of further elective surgery than bipedicled DIEP flaps (40.4% unipedicled versus 12.9% bipedicled; P = 0.029; Table 8; Fig. 9). There was no significant difference between rates of further emergency surgery (P = 0.196).
Table 8.
Postoperative Data Based on the Surgical Type of DIEP
| Postoperative | Unilateral, Unipedicled (n = 52), N (%) or Median (IQR) | Bilateral, Unipedicled (n = 15), N (%) or Median (IQR) | Unilateral, Bipedicled (n = 31), N (%) or Median (IQR) | P |
|---|---|---|---|---|
| Inpatient stay, days | 5 (4–5) | 5 (4–6) | 5 (4–5) | 0.547 |
| Further elective surgery | ||||
| No | 31 (59.6) | 11 (73.3) | 27 (87.1) | 0.029 |
| Yes | 21 (40.4) | 4 (26.7) | 4 (12.9) | |
| Further emergency surgery | ||||
| No | 45 (83.3) | 15 (100) | 25 (80.6) | 0.196 |
| Yes | 9 (16.7) | 0 (0) | 6 (19.4) | |
P values are from the χ2 and Kruskal-Wallis tests as appropriate.
IQR, interquartile range.
Fig. 9.
A bar chart showing patients who required further elective or emergency surgery for unipedicled and bipedicled DIEP flaps.
DISCUSSION
Our results demonstrate several points, but to summarize, there was no statistical difference in the total number of donor site complications (P = 0.193). There is a correlation between the significantly longer operative time in bipedicled DIEP flaps (P < 0.001) and an increased odds of donor site morbidity. This is demonstrated through the odds of a donor site complication in bipedicled DIEP flaps decreasing after adjusting odds ratio for operative time, but this was not significant (OR, 1.15; 95% CI, 0.52–2.55 before adjustment; OR, 0.84; 95% CI, 0.31–2.29 after adjusting for operative time).
In unilateral DIEP flaps, fat necrosis and flap congestion were lower in bipedicled versus unipedicled DIEP flaps. Before BMI adjustment, odds of a recipient site complication was 1.75 times higher in unilateral, bipedicled versus unipedicled DIEP flaps. However, after adjustment for the 10% higher BMI in bipedicled DIEP flaps, odds ratio dramatically decreased to 1.17. The increased odds of recipient site complications in bipedicled DIEPs was composed of minor complications classified as Clavien Dindo grade 1, managed conservatively, and thus, is not a true representation of any serious difference in recipient area outcomes. The greater odds of recipient complications in bipedicled DIEP flaps was confounded by the higher BMI of this group.
Our study has the advantage of being conducted in a single center with standardized Enhanced Recovery After Surgery protocols. It is a large cohort of 98 patients, one of the larger cohorts of patients comparing outcomes of solely DIEP flaps. Our study is the first to compare donor and recipient site complications in the same set of patients undergoing surgery with different types of DIEP flap. There has been literature comparing this in different types of autologous reconstruction21 but not only DIEP flaps.
We hypothesized that increased dissection of the abdomen during a bipedicled DIEP flap would increase donor site morbidity. A systematic review of 2398 patients found a greater risk of donor site morbidity in bilateral DIEP flaps.22 Currently, there is only one published study comparing donor site morbidity in different types of DIEP flap.23 They found no significant difference in odds of donor site morbidity (P = 0.09). However, they did not look at the recipient site and did not record many of the variables that we did, including operative time, further emphasizing the necessity for our study.
Our study shows that bipedicled DIEP flaps had higher rates of donor site morbidity postoperatively, but this was explained by the longer operative time. Variability in operative time was due to surgeon variability and time taken for mastectomy plus minus clearance. Furthermore, our center is a public teaching hospital, with one consultant and surgical trainees. A unilateral DIEP within 8 hours is an acceptable time limit as found by Shammas et al.24 However, with dual consultant operations, operative time can be reduced by nearly an hour and confer increased patient safety.25 With operative time increasing postoperative complications,26 surgeons should consider performing more dual consultant operations. Including bilateral cases in our study could be seen to be a counfounding factor for assessing the effect of operative time on odds of donor site morbidity; however, we felt it necessary to include these cases in our analyses to increase the study power.
Our study includes the peak COVID-19 years of 2020 and 2021, when there were fewer delayed and risk-reducing procedures performed,27 and hence, significantly less DIEP reconstructions performed. Many women had mastectomies without reconstruction, and many DIEP flap cases performed at our center in the COVID-19 aftermath were delayed as opposed to immediately after mastectomy. Immediate DIEP flaps and additional procedures performed at the same time as DIEP flaps increase operative time.
One limitation of our study is the less than optimal follow-up time for assessing long-term outcomes, including hernia or bulge. However, hernia or bulge is rare, as supported by a systematic review assessing incisional hernia incidence, of which no study included had a greater than 5-year follow-up. (See table, Supplemental Digital Content 1, which displays the incidences of hernia and bulging after DIEP flap, http://links.lww.com/PRSGO/C625.) To combat bulge, some surgeons routinely use sublay mesh even when raising a DIEP flap in our institution, particularly if nerves have been divided in cases where lateral row perforators have been taken.
Bipedicled DIEP flaps use two veins plumbed in retrograde and anterograde. Through data analysis, the senior authors have found fewer incidences of flap congestion and need to anastomose the superficial system via vein graft or cephalic turndown. Bipedicled DIEP flaps have the following advantages: the second pedicle can be used as a backup if the first is damaged (especially important in perforators <1 mm); they provide training opportunities for residents to raise the contralateral side; they reduced the risk of fat necrosis and venous congestion; and they reduced the need for contralateral procedures, including breast reduction (due to recruiting the entire abdomen). For unilateral reconstruction, we would consider a bipedicled DIEP flap for patients with a flap weight greater than 500 g to provide a more robust blood supply, and from personal experience, this also yields a softer breast. We would also consider a bipedicled DIEP flap for patients with limited hemiabdomen to reconstruct the breast and for patients due to undergo postoperative radiotherapy, as from observation, bipedicled DIEP flaps are more radioresistant; however, this needs further investigation. In unilateral cases, the lead surgeon has found zonal issues as choke vessels opened, and this has not been the case with bipedicled flaps. They are, in our opinion, safer as there are two vascular pedicles for both artery and vein. Of patients undergoing bipedicled DIEP flap reconstruction, 16.1% had undergone previous abdominal surgery, which may also have been a reason why the primary surgeon chose a bipedicled DIEP flap to increase blood supply. Our findings support that the increased vascularity from two pedicles may decrease major recipient site complications, as a lower proportion of patients with unilateral bipedicled DIEP flaps developed fat necrosis and flap congestion; however, these results were not significant (P = 0.166 and 0.568, respectively). In conjunction with our findings that bipedicled DIEP flaps do not increase donor site morbidity after adjusting for operative time, it can be concluded that bipedicled DIEP flaps are a safe option for women.
An interesting finding is that a significantly higher proportion of patients undergoing unilateral, unipedicled DIEP flaps required further elective surgery (40.4% versus only 12.9% in unilateral, bipedicled DIEP flaps, P = 0.029). This is important because following the pandemic, healthcare services worldwide are tackling a backlog of elective procedures with sources suggesting that waiting lists have increased by one-third.28 In the UK as of 2022, there was the largest NHS backlog for consultant-led treatment since 2007.29 If bipedicled DIEP flaps decrease rates of further elective surgery without increased morbidity, they can save healthcare systems worldwide money and time and prevent adding to waiting lists.
Flap weight is not always accurately recorded, and often only the final, not the initial, harvest weight is recorded. The next steps following our study should be to prospectively gather more data from multiple centers, with accurate documentation of flap weight to see its impact on the donor and recipient sites.
CONCLUSIONS
Our study shows no significant difference in donor site morbidity between unipedicled and bipedicled DIEP flaps. Although bipedicled DIEP flaps do have slightly higher rates of donor site morbidity, this can be explained by longer operative times. We report no significant difference in recipient site complications and show that bipedicled DIEP flaps can reduce rates of further elective surgery. In conclusion, bipedicled DIEP flaps should be considered more by surgeons, not just for patients for whom unipedicled DIEP flaps would be unsuitable.
DISCLOSURES
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 23 June 2023.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Cancer Research UK. Cancer incidence for common cancers. Available at https://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence/common-cancers-compared#ref-3. Accessed January 12, 2022.
- 2.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32–38. [DOI] [PubMed] [Google Scholar]
- 3.He WY, el Eter L, Yesantharao P, et al. Complications and patient-reported outcomes after TRAM and DIEP flaps. Plast Reconstr Surg Glob Open. 2020;8:e3120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knox ADC, Ho AL, Leung L, et al. Comparison of outcomes following autologous breast reconstruction using the DIEP and pedicled TRAM flaps. Plast Reconstr Surg. 2016;138:16–28. [DOI] [PubMed] [Google Scholar]
- 5.Fitzgerald O’Connor E, Rozen WM, Chowdhry M, et al. Preoperative computed tomography angiography for planning DIEP flap breast reconstruction reduces operative time and overall complications. Gland Surg. 2016;5:93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pacifico MD, See MS, Cavale N, et al. Preoperative planning for DIEP breast reconstruction: early experience of the use of computerised tomography angiography with VoNavix 3D software for perforator navigation. J Plast Reconstr Aesthet Surg. 2009;62:1464–1469. [DOI] [PubMed] [Google Scholar]
- 7.Malata CM, Rabey NG. Decision making in double-pedicled DIEP and SIEA abdominal free flap breast reconstructions: an algorithmic approach and comprehensive classification. Front Surg. 2015;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koolen PGL, Lee BT, Lin SJ, et al. Bipedicle-conjoined perforator flaps in breast reconstruction. J Surg Res. 2015;197:256–264. [DOI] [PubMed] [Google Scholar]
- 9.Mulvey CL, Cooney CM, Daily FF, et al. Increased flap weight and decreased perforator number predict fat necrosis in DIEP breast reconstruction. Plast Reconstr Surg Glob Open. 2013;1:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christopoulos G, Sergentanis TN, Vlachogiorgos A, et al. The use of the bipedicled deep inferior epigastric perforator flap for unilateral breast reconstruction. Ann Plast Surg. 2020;85:e66–e75. [DOI] [PubMed] [Google Scholar]
- 11.Khattab NR. Complications of free bipedicled DIEP flaps in breast reconstruction: a systematic review and meta-analysis. Eur J Plast Surg. 2022;45:39–53. [Google Scholar]
- 12.Linder S, Walle L, Loucas M, et al. Enhanced Recovery after Surgery (ERAS) in DIEP-flap breast reconstructions—a comparison of two reconstructive centers with and without ERAS-protocol. J Pers Med. 2022;12:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gort N, van Gaal BGI, Tielemans HJP, et al. Positive effects of the enhanced recovery after surgery (ERAS) protocol in DIEP flap breast reconstruction. Breast. 2021;60:53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haddock NT, Garza R, Boyle CE, et al. Observations from implementation of the ERAS protocol after DIEP flap breast reconstruction. J Reconstr Microsurg. 2022;38:506–510. [DOI] [PubMed] [Google Scholar]
- 15.NHS, SmokeFree, Interventions in secondary care. The clinical case for smoking cessation before surgery. October2022. Available at https://www.ncsct.co.uk/usr/pub/interventions-in-secondary-care-june-10-surgical-patients-factsheet.pdf. Accessed January 12, 2022.
- 16.Lindström D, Sadr Azodi O, Bellocco R, et al. The effect of tobacco consumption and body mass index on complications and hospital stay after inguinal hernia surgery. Hernia. 2007;11:117–123. [DOI] [PubMed] [Google Scholar]
- 17.Jensen JA. Should improved mastectomy and reconstruction alter the primary management of breast cancer? Plast Reconstr Surg. 1999;103:1308–1310. [DOI] [PubMed] [Google Scholar]
- 18.Wagner IJ, Tong WM, Halvorson EG. A classification system for fat necrosis in autologous breast reconstruction. Ann Plast Surg. 2013;70:553–556. [DOI] [PubMed] [Google Scholar]
- 19.NHS England. What is the body mass index (BMI)? Available at https://www.nhs.uk/common-health-questions/lifestyle/what-is-the-body-mass-index-bmi/#:~:text=Back%20to%20Lifestyle-,What%20is%20the%20body%20mass%20index%20(BMI)%3F,of%2025%20means%2025kg%2Fm2. Accessed August 11, 2022.
- 20.The British Association of Urological Surgeons. Grading of surgical complications. Available at https://www.baus.org.uk/patients/surgical_outcomes/grading_of_surgical_complications.aspx. Accessed January 12, 2022.
- 21.Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg. 2006;117:1711–1719. [DOI] [PubMed] [Google Scholar]
- 22.Wormald JCR, Wade RG, Figus A. The increased risk of adverse outcomes in bilateral deep inferior epigastric artery perforator flap breast reconstruction compared to unilateral reconstruction: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2014;67:143–156. [DOI] [PubMed] [Google Scholar]
- 23.Tomouk T, Mohan AT, Azizi A, et al. Donor site morbidity in DIEP free flap breast reconstructions: a comparison of unilateral, bilateral, and bipedicled surgical procedure types. J Plast Reconstr Aesthet Surg. 2017;70:1505–1513. [DOI] [PubMed] [Google Scholar]
- 24.Shammas RL, Sisk GC, Coroneos CJ, et al. Textbook outcomes in DIEP flap breast reconstruction: a Delphi study to establish consensus. Breast Cancer Res Treat. 2023;197:559–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canizares O, Mayo J, Soto E, et al. Optimizing efficiency in deep inferior epigastric perforator flap breast reconstruction. Ann Plast Surg. 2015;75:186–192. [DOI] [PubMed] [Google Scholar]
- 26.Haddock NT, Wen YE, Steppe C, et al. Operative time predicts postoperative outcomes in bilateral DIEP flap reconstruction: multivariate 1000 flap analysis. Plast Reconstr Surg Glob Open. 2022;10:e4713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NHS England and NHS Improvement. Important and urgent—next important and urgent—next steps on NHS Response to COVID-19. 2020. Available at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf. [Google Scholar]
- 28.Uimonen M, Kuitunen I, Paloneva J, et al. The impact of the COVID-19 pandemic on waiting times for elective surgery patients: a multicenter study. PLoS One. 2021;16:e0253875e0253875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carl B. NHS Key Statistics: England, November 2022. London: The House of Commons Library; 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.