Abstract
Heart failure (HF) remains a condition associated with high morbidity, mortality, and associated costs. Although the number of medical and device-based therapies available to treat HF are expanding at a remarkable rate, disparities in the risk for incident HF and treatments delivered to patients are also of growing concern. These disparities span across racial and ethnic groups, socioeconomic status, and apply across the spectrum of HF from stage A to stage D. The complexity of HF risk and treatment is further impacted by the number of patients who experience the downstream impact of social determinants of health. The purpose of this document is to highlight the known health care disparities that exist in the care of patients with HF and to provide a context for how clinicians and researchers should assess both biological and social determinants of HF risk in vulnerable populations. Furthermore, this document provides a framework for future steps that can be used to help diminish inequalities in access and clinical outcomes over time, and offer solutions to help decrease disparities within HF care.
Keywords: Heart failure, health care disparities, race–ethnicity, outcomes
Approximately 6.2 million American adults have heart failure (HF), and the prevalence is projected to increase 46% by 2030 affecting more than 8 million adults.1 Recent clinical trials have shown advances in the treatment of chronic HF, including novel medical and device therapies, as well as innovative tools for remote monitoring. Despite these developments, HF remains the most common cause of hospitalization in patients aged more than 65 years, with the 5-year mortality as high as 75% in patients with a prior hospitalization.2 Therefore, progress for the treatment of HF on a population level requires addressing the impact of health care disparities on patients with HF. HF disproportionately affects Black, Hispanic, and other vulnerable individuals wherein social determinants of health (SDOH) are barriers to receipt of guideline-directed medical therapy (GDMT), as well as advanced HF therapies such as heart transplantation (HT) and left ventricular assist device implantation. This position statement from the Heart Failure Society of America (HFSA) specifically focuses on racial and ethnic disparities within HF and the role of health care societies and systems to help mitigate health care disparities. The authors acknowledge many other disparities in HF care exist (ie, disparities in the care of women with HF), but these issues are not addressed in this article because they are beyond the scope of this statement.
Higher Risk for HF in Patients Who Are Members of Racial or Ethnic Minority Groups
There are noteworthy racial and ethnic differences in the prevalence and incidence of HF. Black individuals have the highest risk of developing HF, followed by Hispanic, White, and Asian individuals.3 The higher risk among racial–ethnic minority individuals is related to the higher prevalence of traditional cardiovascular (CV) risk factors, including hypertension, diabetes, and obesity. More recently, appropriate emphasis has been placed on structural factors that influence socioeconomic status (SES) and other SDOH, including underinsurance and access to care, community environment, and health care quality, that adversely impact health outcomes for racial[C0]ethnic minority individuals (Fig. 1).3–8 Black and Hispanic patients develop HF at younger age, are more likely to be underinsured compared with non-Hispanic White patients, and have higher rates of hospitalization and short-term readmissions.9–11 The rate of HF hospitalization for Black men and women is nearly 2.5 higher than the rate for White patients (Fig. 2).10 Moreover, costs for acute HF hospitalizations are higher among Black and Hispanic patients compared with White patients.12 Racial and ethnic differences also exist in mortality owing to HF, with Black men and women having higher age-adjusted mortality (age adjusted HF death rate per 100,000: Black males 120.9, females 87.3; White males 113.5, females 81.9; American Indian or Alaska native males 98.1, females 72.8; Hispanic males 71.5, females 49.5; Asian or Pacific Islander males 49.6, females 35.8).13 Racial disparities in mortality are more pronounced among younger adults (35–64 years of age) compared with older adults (65–84 years of age).14 This disparity is particularly alarming; younger patients should theoretically be evaluated more often for advanced HF therapies, including HT and left ventricular assist devices, given the greater likelihood of extending duration of life. Although CV disease (CVD) is the leading cause of death among Native Americans, HF continues to be understudied in this population.15 Additionally, for reasons that are not fully understood but are undoubtedly complex, Black patients have the worst survival after HT.16,17 Recent analyses very clearly document that adjusting for racial differences in SES does not fully account for the inferior survival among Black HT recipients.18,19 Lower survival among Black patients after HT likely represents a complex interplay of immunologic susceptibility, as well as clinical and socioeconomic factors that deserve further attention to improve post-transplant outcomes.
Fig. 1.
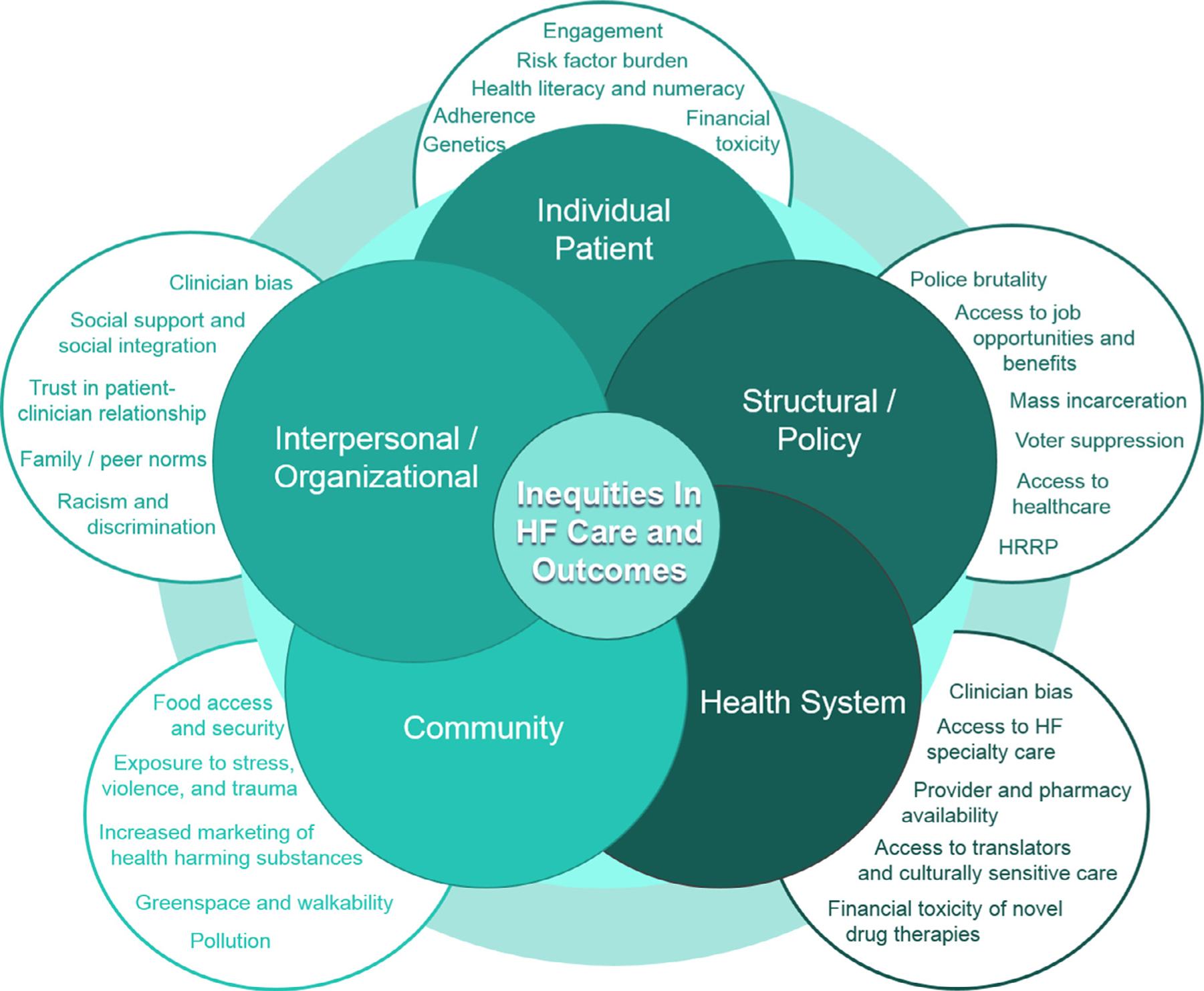
Elements contributing to inequities in heart failure (HF) care and outcomes among racial and ethnic minority groups. The higher risk for HF, and inequities in HF care for racial–ethnic minority individuals, is related to the higher prevalence of traditional risk factors, structural factors that influence socioeconomic status and other social determinants of health, as well as community and health system factors that adversely impact health care quality.
Fig. 2.
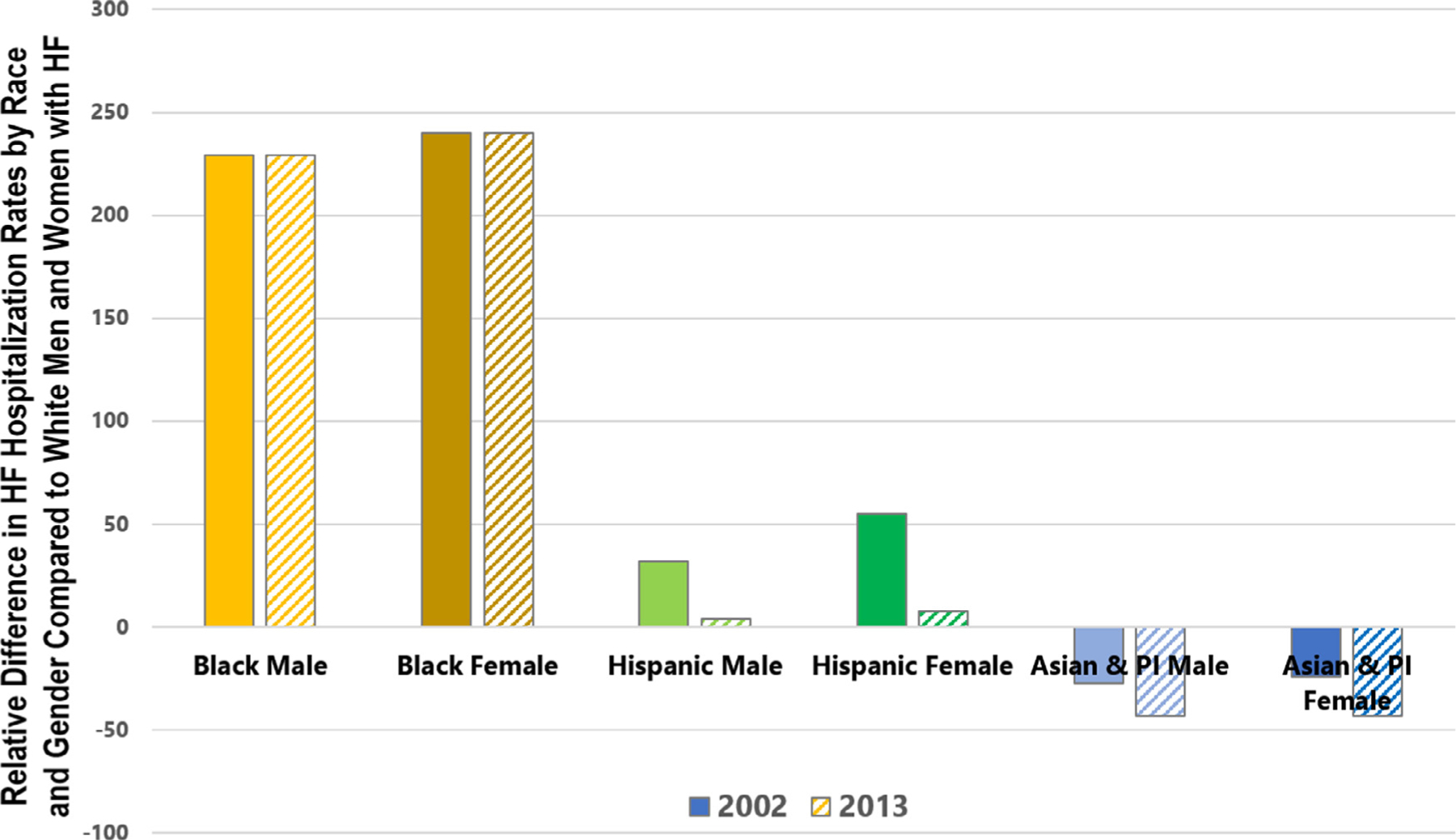
Disparities in heart failure (HF) hospitalization rates for racial and ethnic minority patients compared with White patients. Compared with White men and women, national age-standardized HF hospitalization rates are higher for Black men and women, with no change from 2002 to 2013. Solid bars indicate HF hospitalization rates in 2002, dashed bars indicate HF hospitalization in 2013. Although Hispanic men and women had higher HF hospitalization rates than White men and women in 2002, the relative difference narrowed greatly by 2013. Asian and Pacific Islander (API) men and women had lower HF hospitalization rates than White men and women in 2002, with even greater reductions demonstrated in 2013. Adapted from Ziaeian et al.10API, Asian and Pacific Islander.
The inferior clinical HF outcomes in racial–ethnic minority populations can be attributed to a combination of individual-, community-, organization-, health care system-, and policy-level elements that must be tackled individually to achieve change.7 As advances are made in the diagnosis and treatment of HF that significantly decrease morbidity and mortality, systems that have historically permitted disadvantaged populations to exist with inferior access to health care must be critically evaluated, dismantled, and restructured to improve care models.
The Multiple Facets of Race and Ethnicity
Race and Ethnicity as Social Constructs
Race and ethnicity have an association with genetic ancestry, but ultimately are social constructs.20 Race is based primarily on mutually common cultural, physical, and socioeconomic features. Ethnicity often refers to grouping of individuals with shared characteristics, including geographic origin, culture, and spoken language. Both race and ethnicity are intimately related and are often used to categorize individuals. The categories of race and ethnicity used are often assigned by investigators, but should ideally be derived from participant selfidentification, as in studies like the African American HF Trial (A-HeFT).21
There are multiple important reasons to collect information on individuals’ race and ethnicity, including to (1) describe study populations and assess generalizability of results, (2) facilitate analyses of patterns of care/outcomes, and (3) evaluate treatment effects. However, the challenge in current standards include broad groupings with significant heterogeneity within populations. For example, among Asians, South Asian individuals (from Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan, and Sri Lanka) and Filipinos have a greater proportionate mortality from ischemic heart disease (the most common cause of HF in the United States) than East Asian individuals (from China, Japan, Korea, and Vietnam).22,23 Similarly, among persons with Hispanic ethnicity, the prevalence of left ventricular diastolic dysfunction is approximately 2-fold higher among individuals of Central American and Cuban descent compared with those of Mexican background.24 Furthermore, many individuals are from mixed racial backgrounds, which is often not accounted for in data collection or organization.
There exists a clear relationship between racial–ethnic categorization and systemic as well as structural racism.25 Structural racism refers to racial discrimination that is fostered by laws and practices, sanctioned and implemented by various levels of government, and embedded in the economic system as well as in cultural and societal norms.26 The impact of structural racism spans many domains, including access to care and SES, which are integrally associated with HF risk factors, treatment, and outcomes. Furthermore, it is difficult to discuss structural racism without acknowledging the role of implicit, or unconscious, bias in the process of associating attitudes or stereotypes toward certain groups without conscious awareness. Implicit biases can impact perceptions of patients, attitudes toward individuals, and clinical decision-making. For example, despite an awareness of the higher risk of hospitalization among racial–ethnic minority patients with HF, Black and Hispanic patients are less likely to receive primary care from a cardiologist when admitted to acute care settings for acute HF.11,27,28 Primary care by a cardiologist in this setting is associated with higher survival and a lower risk of readmission, representing a missed opportunity to improve outcomes in Black and Hispanic patients with HF. Implicit bias and medical mistrust among Black and Hispanic patients may also negatively impact enrollment into research studies and clinical trials.
The Role of Biologic Ancestry as a Determinant of HF Risk
The social constructs of race and ethnicity have had an undeniable impact on health outcomes, largely through the creation of inequalities for individuals from underrepresented racial and ethnic minority groups that permeate almost every sector of American life. However, even with the acknowledgment of the immense impact of structural racism and SDOH, is there currently a role for exploring continental genetic ancestry as a determinant of the specific risk for HF? Race is also associated directly with genetic ancestry, and therefore potentially related to the frequency of genetic variants in populations that may affect disease risk and health outcomes.29 In the United States, certain population subgroups, particularly Black and Hispanic Americans, may self-report as being of a singular “race,” despite a complex genetic admixture that reflects African, European, Native American, and other ancestries. Racial differences in nitric oxide physiology have long been acknowledged, with substantial data demonstrating a lower bioavailability of nitric oxide among self-reported Black persons as a cause of higher risk of abnormal vascular reactivity, hypertension, and ultimately, HF.30,31 Similarly, racial differences in signaling of the renin–angiotensin–aldosterone system have also long been recognized, with self-reported Black persons in the United States and Africa being more likely to display a physiology characterized by low levels of renin during normotensive, hypertensive, and HF states.32–34 More recently, African ancestry has been shown to be associated with a relative deficiency of natriuretic peptides that may predispose to a physiology characterized by impaired diuresis and natriuresis, hypertension, left ventricular hypertrophy, and diastolic dysfunction, in addition to hypertension, insulin resistance, and obesity.35,36 The prevalence of the valine-to-isoleucine substitution at position 122 (V142I) on chromosome 18 is carried by 3.5% of Black Americans, and is associated with higher risk for development of hereditary transthyretin cardiac amyloidosis.37,38
Future study design to examine racial–ethnic disparities in health care must be rigorous, and integrate the multiple pathways that simultaneously influence the disparate rates of disease in racial–ethnic minority subgroups. As our ability to quantify genetic ancestry improves with programs such as the International HapMap (National Human Genome Research Institute) Project, our understanding of both genetic risk for HF as well as therapeutic considerations based on ancestry will continue to mature. However, it is clear that a much greater emphasis needs to be placed on the role of implicit bias, SDOH, and structural racism in disease risk and outcomes. Biologic mechanisms link the SDOH with the pathogenesis of CVD, including excess stress hormones, inflammation, and cellular aging.39 Frameworks such as the social ecological model acknowledge the relevance of biological and genetic risk for disease, while placing those risks into the context of interpersonal, community, and societal factors that also influence an individual’s risk and outcomes.7,40
How Can Health Care Societies and Systems Help to Dismantle Health Care Disparities for Patients With HF?
Prioritizing the elimination of health care disparities and the achievement of health equity might be considered the most efficient way to significantly decrease the burden of HF across all populations. For instance, because Black patients have the highest prevalence of HF, and rates of HF hospitalization and 30-day readmission that are higher than their White counterparts, achieving meaningful improvements in clinical outcomes for Black patients with HF would result in substantial decreases in overall HF morbidity and mortality. Moreover, a sustained commitment to advocacy that improves access to health care as well as medical and device therapies will ultimately benefit all patients with HF. To dismantle health care disparities, health care societies and systems must expand their current efforts and prioritize the achievement of health equity through key strategic initiatives. We offer key areas of improvement that can be targeted toward a goal of decreasing health care disparities in HF, with examples of success being implemented from within the HFSA (Fig. 3).
Fig. 3.
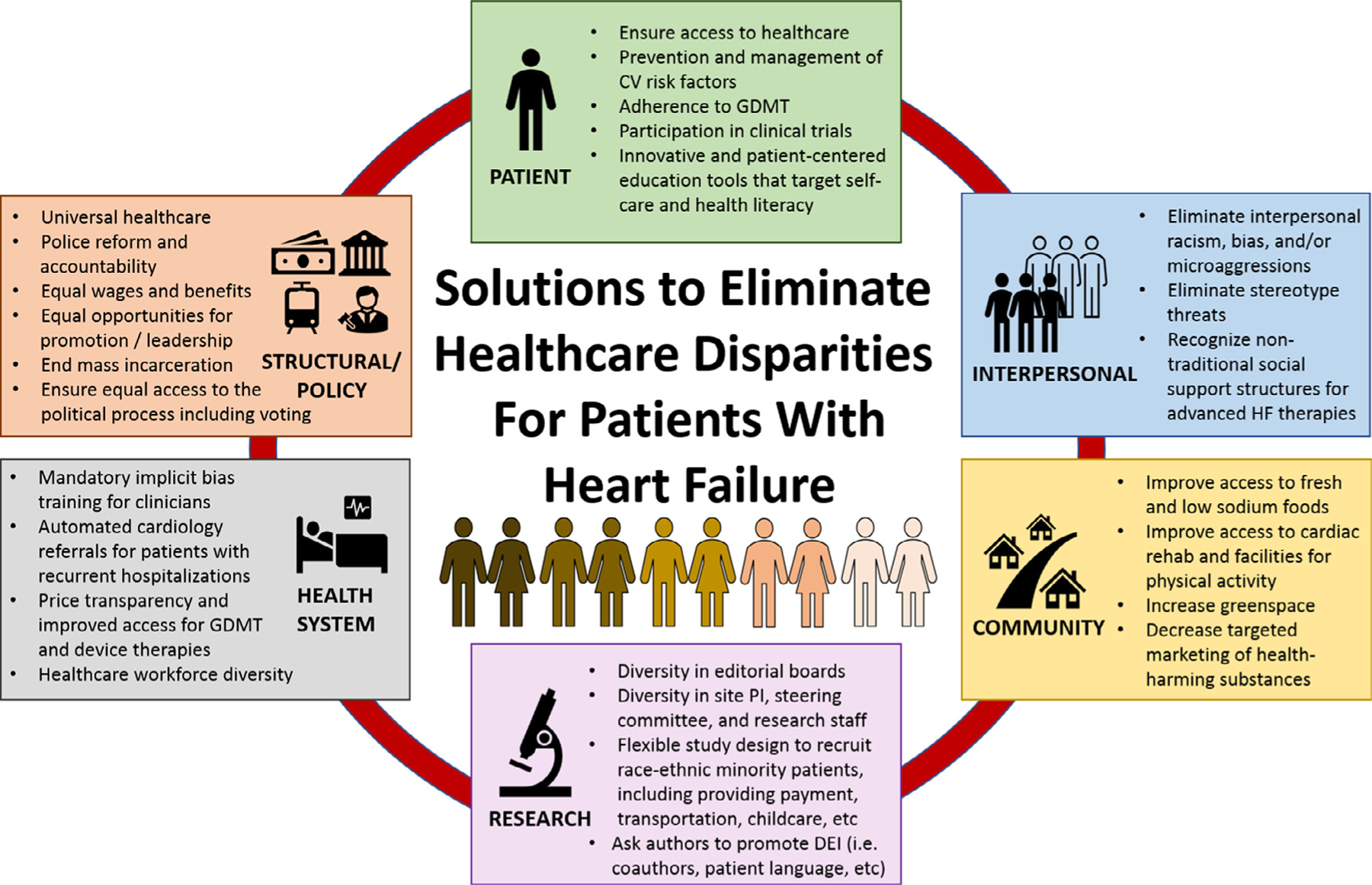
Solutions to eliminate health care disparities for patients with heart failure. CV, cardiovascular; DEI, diversity, equity, and inclusion; GDMT, guideline-directed medical therapy; PI, principal investigator.
Patients
Scope of the Problem.
Patients from marginalized or historically disadvantaged backgrounds may encounter multiple challenges while seeking medical care. Clinicians with stronger preexisting implicit biases consistently demonstrate poorer communication with patients.41 Efforts toward decreasing inequities for patients should focus on the importance of cultural humility for all health care team members, with a downstream goal of improving disparities and achieving equitable health care across patient populations.42
Solutions.
Health care organizations and societies must focus on the patient experience and develop processes that will empower patients with chronic conditions, including HF. Innovative methods can be used to improve health literacy for patients, including mobile applications and behavioral tools that may help to facilitate improved use of GDMT as well as overall HF self-management. Furthermore, the use of innovative tools can provide the opportunity to further learn from patients regarding barriers to care or adherence to medical regimens. For example, the HFSA Patient Committee specifically provides oversight of patient programs within the society, including how to improve patient education with the use of educational modules for patients including podcasts, webinars and other methods. Novel trials, including Care Optimization Through Patient and Hospital Engagement Clinical Trial for Heart Failure (CONNECT-HF),43 Electronically Delivered, Patient-Activation Tool for Intensification of Medications for Chronic Heart Failure with Reduced Ejection Fraction (EPIC-HF),44 and others have generated innovative tools that can be used to enhance patient education and actively engage patients from all socioeconomic strata in their HF care. Learning from patients through the society with regard to major issues in HF care, including health care access, cost, and implicit bias, and documenting the patient experience (eg, patient perspectives at the Annual Scientific Meeting and in the Journal of Cardiac Failure) will help professional members to create actionable steps to decrease disparities over time. In addition, ongoing education with regard to these issues can help to improve training for the next generation of HF clinicians.
Interpersonal
Scope of the Problem.
Racism, not race or ethnicity per se, is a quintessential contributor to the SDOH.45 To this end, many racial–ethnic disparities in health outcomes are in fact owing to the effects of racism.46 Before confronting the issue of racism at any level, a framework is needed to raise new hypotheses about the basis of racial–ethnic disparities in health outcomes, as well as for designing effective interventions to eliminate those differences. Three levels of racism have been proposed in the literature (Table 1).46,47 As a system, racism has been institutionalized in a manner that permits the establishment of patterns, procedures, practices, and policies within organizations (institutionalized/structural), which in turn affects the attitudes, beliefs, and behaviors of individuals toward each other (personally mediated), in addition to how individuals perceive themselves (internalized).46 Racism has been embedded in and is evident across each level of the health care delivery system (eg, patient, clinician, institution, and national organization), and thus impacts the management of patients with HF.48 For example, in addition to the lower rates of admission to inpatient cardiology services for racial[C0]ethnic minority patients with HF,11,27,28 emergency department clinicians are less likely to hospitalize Black as compared with White patients with HF and more often report having spoken with the patient’s outpatient cardiologist for White than for Black or Hispanic patients.49,50
Table 1.
Framework for understanding Racism on Three Levels
| Level | Definition |
|---|---|
| Institutional ized/structural | Manifests both in material conditions (eg, differential access to quality education, sound housing, gainful employment, appropriate medical facilities, and a clean environment) and in access to power (eg, differential access to information, and voice). |
| Origins lie in discrete historical events but persists because of contemporary structural factors that perpetuate those historical injustices. | |
| Embodied in polices, practice, cultural representation, and norms. | |
| Personally mediated | Defined as prejudice and discrimination, where prejudice means differential assumptions about the abilities, motives, and intentions of others according to their race, color, ethnicity and culture. |
| Can be intentional as well as unintentional. Includes acts of commission as well as acts of omission manifesting as lack of respect, suspicion, and scapegoating. Includes microaggressions | |
| Maintains structural barriers and condoned by societal norms | |
| Internalized | Defined as acceptance by members of the stigmatized races of negative messages about their own abilities and intrinsic worth. |
| Characterized by their not believing in others who look like them, and not believing in themselves thus reflecting a system of privilege. | |
| Erodes individual sense of value and undermines collective action. |
This theoretical framework for understanding racism on three levels can be used to raise new hypotheses about the basis of race-associated differences in health outcomes, but also design effective interventions. From Jones.47
Solutions.
Because health care providers have taken an oath to “do no harm,” it could be considered every clinician’s professional and ethical obligation to dismantle structural and interpersonal systems that may perpetuate racism and continue to harm patients.47 Clinicians can actively work to be antiracist by incorporating specific curricula and training models, documenting actions, and tracking behaviors.46 Using the Four Pillars, Table 2 summarizes a potential approach health care societies and systems could use to develop initiatives dedicated to identifying racial injustices, as well as to advance racial justice both within the organization, as well as society at large. All individuals involved in the care of patients with HF should plan and prepare to elevate the issue of racism, practice allyship, and engage stakeholders to empower marginalized individuals. To be successful toward an end-goal of achieving racial justice and advancing health equity, such an approach requires the ongoing dedication of leadership, committees, and the day-to-day work of all clinicians within health care systems.
Table 2.
The Four Pillars Approach in Advancing Racial Justice and Health Equity, and the Role of Medical Organizations
| Pillar* | Description |
|---|---|
| Elevate the issue | Highlight racial inequity and racism in HF at local, state, and federal levels through lobbying efforts, national media outlets, digital communications and social media. |
| Advocate for adequate and affordable insurance and prescription coverage, flexible, community-based HF screening and intervention programs, early HF risk factor modification, and improved referral, access, and utilization of HF care, including advanced HF therapies at local, state, and federal levels. | |
| Have dedicated racial inequity and racism themes at annual Scientific Meetings. | |
| Develop a policy dedicated to embedding racial justice and advancing health equity within the strategic plan of health care societies and systems | |
| Engage stakeholders | Survey membership to evaluate potential racism within the organization as well as potential solutions. |
| Survey patient membership regarding opinions and experiences of racial injustice in the health care setting | |
| Partner and collaborate with external stakeholders such as medical organizations, community advocacy groups, insurers, and industry leaders regarding racial inequities as it effects patient care, health policy, and health care delivery and potential solutions. Identify methods to increase representation of racial and ethnic minorities and women within the profession. | |
| Equip members and communities | Develop durable education programs for providers on types and examples of racism and racial injustice |
| Develop educational materials for patients in recognizing racial injustice in the health care setting and dealing with these issues. | |
| Empower those marginalized | Include representation of racial and ethnic minorities and women within all levels of the organization such as leadership positions and committees. |
HF, heart failure.
Community
Scope of the Problem.
Recent HF classification and staging systems have appropriately intended to place greater emphasis on the prevention of HF by prioritizing the identification of asymptomatic patients with clinical risk factors for HF.51 The emphasis on prevention is particularly relevant with the incorporation of biomarkers in guidelines to guide earlier diagnosis in those at risk for HF, and the increasing availability of medical therapies that have proven efficacy to prevent the onset of HF (ie, Sodium-glucose co-transporter 2 inhibitors).51 The prevention of HF, however, is best achieved when all Americans have equitable access to opportunities for healthy lifestyle as well as high-quality, affordable health care and preventive health services.52 Largely owing to the SDOH, racial–ethnic minority patients are less likely to have access to environments that allow the promotion of ideal CV health, including neighborhoods where high-quality diet and exercise facilities are within reach, jobs that ensure access to high-quality health care, and educational opportunities that promote optimal health literacy. Similarly, SDOH often limit access to the growing armamentarium of medical and device therapies available to decrease morbidity and mortality for patients in whom HF is already manifest.
Neighborhood Health and HF Prevention.
Patients living in neighborhoods with a lower SES have more severe HF symptoms and an increased risk of adverse clinical outcomes, including incident HF and hospital readmissions.11,53–55 The association between neighborhood deprivation and HF risk may be mediated through environmental resources (eg, medical care, grocery stores), psychosocial stressors (lack of safety and social cohesion), and built environment attributes (eg, availability of transportation, greenspace, housing stability) that collectively impact lifestyle behaviors. For instance, socioeconomically deprived neighborhoods have a lower density of grocery stores and availability of fresh, healthy foods, contributing to a lower diet quality for persons living in low SES neighborhoods.56,57 A lack of access to fresh foods may have particularly deleterious consequences for patients with HF, who are almost universally counselled to eat low-sodium diets and require fairly meticulous self-care and frequent medication changes to maintain euvolemia.58 Even after accounting for differences in traditional CV risk factors, living in a food desert is associated with an increased risk of recurrent all-cause and HF hospitalizations.54 As neighborhood deprivation increases, supermarket availability decreases, regardless of race or ethnicity.59 However, as a result of contributions from structural racism, patients who self-identify as members of racial and ethnic minority subgroups are more likely to live in low SES neighborhoods and food deserts. Even at equal levels of poverty, census tracts with the most Black residents have the fewest supermarkets, whereas census tracts with the most White residents have the most supermarkets.59 Across the spectrum of low and high SES neighborhoods, the risk for HF hospitalization and readmissions may still be higher for Black compared with White patients (Fig. 4).11 Lower neighborhood SES is also associated with decreased participation in cardiac rehabilitation, particularly for younger patients.60
Fig. 4.
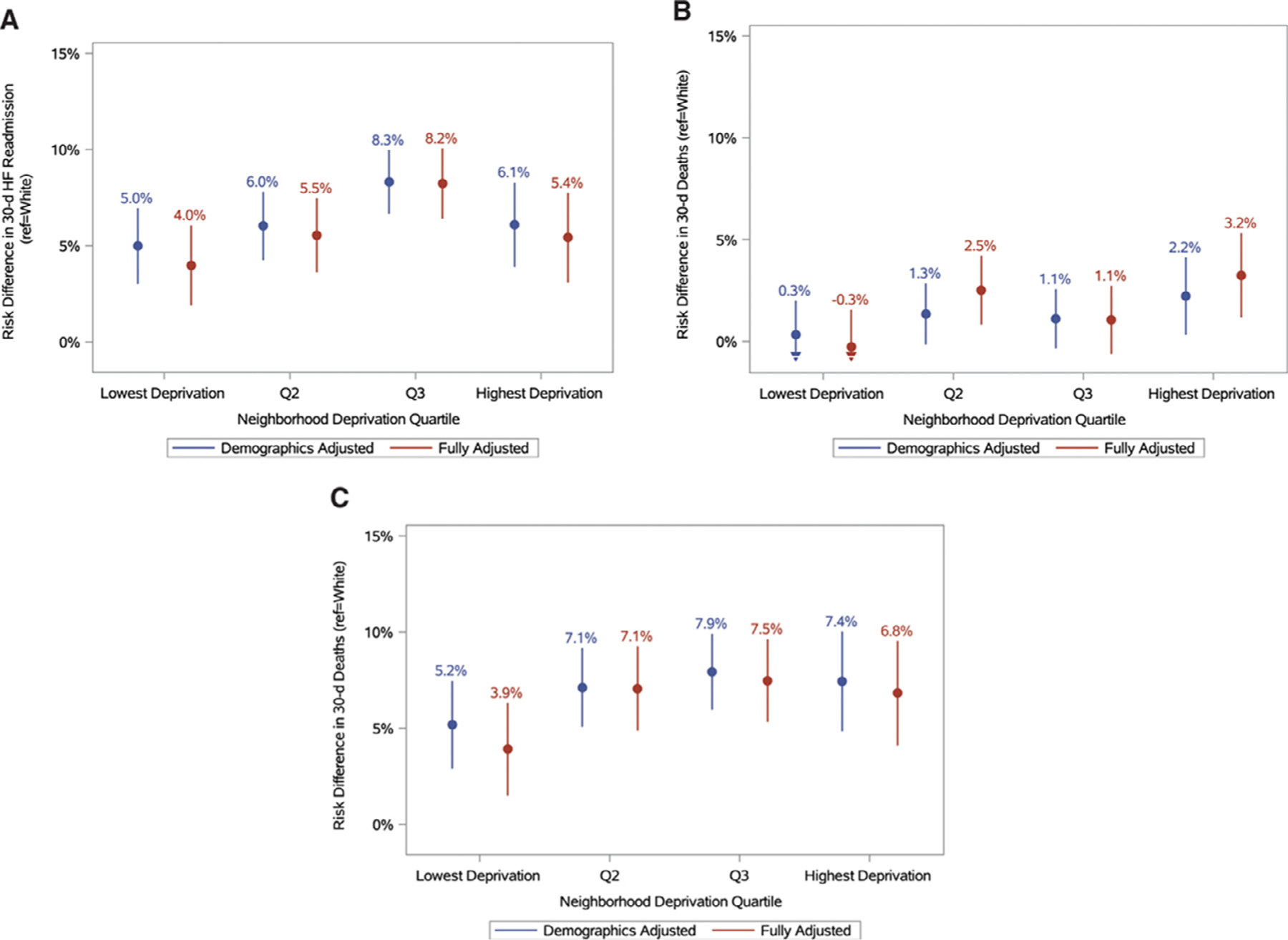
Excess risk of 30-d heart failure (HF) readmission in Black compared with White patients hospitalized for acute HF according to quartiles of neighborhood deprivation. The figure plots the absolute risk differences between Black and White individuals (reference) in 30-day HF readmission by quartile of the Social Deprivation Index, and demonstrates a higher risk of readmission for Black patients with HF at every level of socioeconomic deprivation. Q2 indicates quartile 2; and Q3, quartile 3. From Patel et al.11
Health Care System Inequalities Lead to Worse Access and Worse Quality of Care.
Long-standing systematic disinvestment in neighborhoods with greater proportions of minority residents has resulted in a deeply segregated health care system that perpetuates disparities. Health care facilities in Black and Hispanic neighborhoods are typically underresourced, with fewer clinicians, including primary care providers who may be unable to meet the needs of a very complex set of patients, and fewer specialists who can provide access to cutting-edge procedures and interventions.26,61 Black and Hispanic patients are more likely to be cared for in community settings. However, specialized devices and procedures to treat HF are typically performed at large academic or advanced HF centers, and are rarely performed at largely minority-serving or safety net hospitals (Fig. 5). For example, Black and Hispanic patients are less likely to receive transcatheter aortic and mitral valve procedures.62,63 Although race and ethnicity independently predict lower rates of transcatheter aortic valve repair, the presence of zip code–level disparities suggest that differences in referral and treatment access play an important role.
Fig. 5.
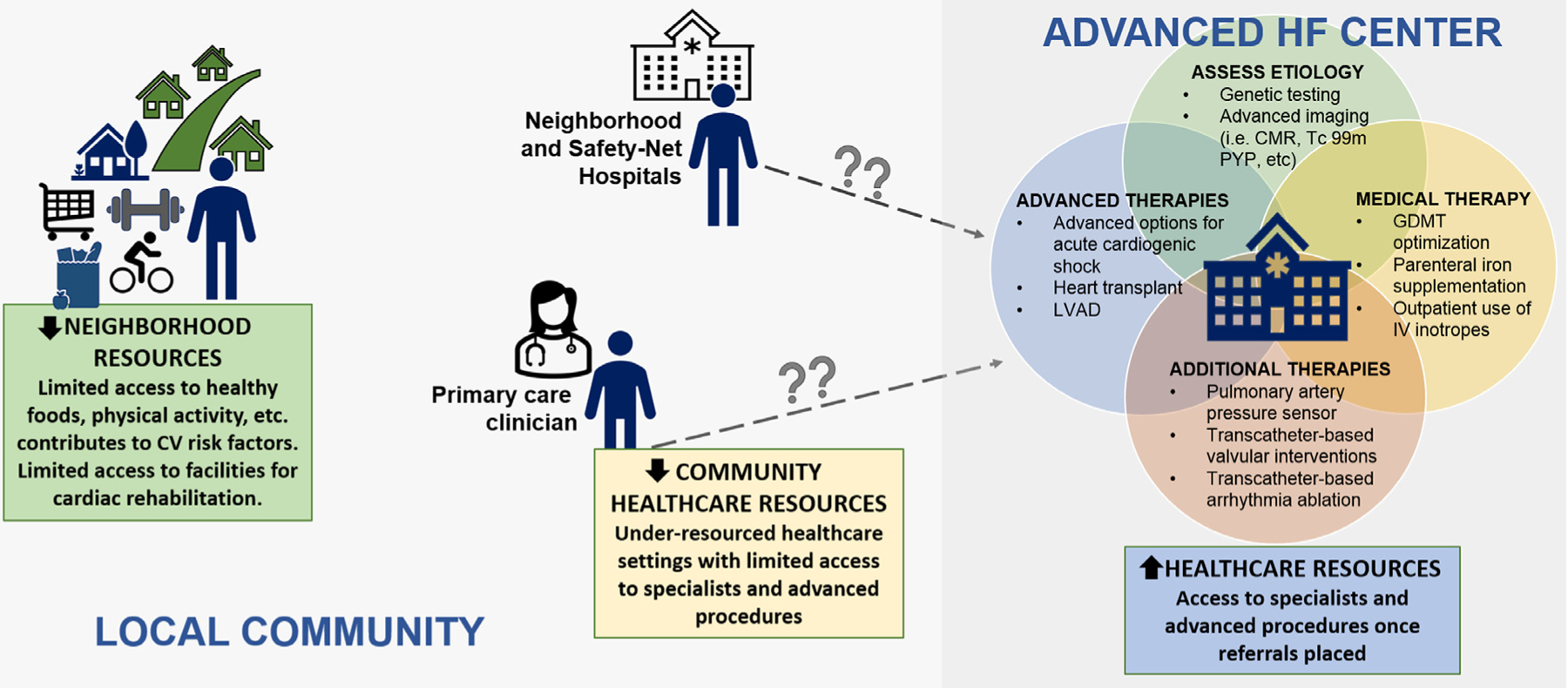
Lack of resources for heart failure care in community settings compared with advanced heart failure centers. Structural racism and residential segregation have resulted in severe economic disinvestment in neighborhoods with greater proportions of minority residents. Residential segregation has also resulted in a deeply segregated health care system that perpetuates health care disparities. Black and Hispanic patients are more likely to receive care in local community settings and safety net hospitals. Because the most specialized and comprehensive care for heart failure is often only available in advanced heart failure centers, improving access to specialty care by ensuring equity in referrals to CV specialists is critical to decreasing disparities. CMR, cardiac magnetic resonance; CV, cardiovascular; GDMT, guideline-directed medical therapy; IV, intravenous; LVAD, left ventricular assist device; PYP, pyrophosphate.
Appropriate Risk Adjustment Methodologies for HF Hospitalization.
Value-based payment programs such as the Hospital Readmissions Reduction Program may disproportionately penalize safety net hospitals that serve greater proportions of racial and ethnic minority individuals and socioeconomically disadvantaged patients.64,65 HF experts, health services researchers, clinicians, and many others rightfully recognize that systemic and structural barriers exist that make optimal HF self-care and adherence more challenging for patients from disadvantaged backgrounds or who live in low SES neighborhoods. As such, many have advocated that the Center for Medicare and Medicaid Services integrate socioeconomic and societal factors into the current risk adjustment algorithms to reverse trends that suggest race and ethnic minority-serving and safety net hospitals are incurring excess payment penalties from the Hospital Readmissions Reduction Program, which could actually worsen existing disparities.
Solutions.
Health care systems can help to decrease disparities by ensuring that patients from disadvantaged backgrounds have access to resources that promote and sustain healthy lifestyles. Health care systems can enable patients with HF and other chronic conditions to access fresh foods by including links to local voucher programs, farmers’ markets that accept supplemental nutrition assistance or other programs. Despite its association with better outcomes, access to traditional cardiac rehabilitation programs is often limited for patients with CVD in rural areas or who have limited times (younger patients who are still working, have childcare obligations, etc). The increased use of virtual cardiac rehabilitation programs can improve access and outcomes for patients with HF.66 Professional societies must also continue to advocate on behalf of patients to improve federal, state, and local policies that undermine access to care for those who are already underserved. The HFSA, for example, has taken a strong stance against the currently used Risk-Standardized Mortality Rate Following HF Hospitalization measure developed by the Center for Medicare and Medicaid Services and recently voiced concerns to the to the National Quality Forum that the measure’s risk adjustment methodology fails to incorporate social risk factors. HFSA’s advocacy consultants have also recently documented both federal legislative and administrative activity related to health inequality and will continue to update the document periodically. This type of advocacy will be required to dismantle structures that promote inequality and must be sustained by health care systems and societies until policies are in place that allow health justice to be achieved. To improve access to CV specialty services and procedures, it is important to track referral practices within health care systems to characterize how often eligible patients lack access to specialty services because they are not referred.
Health System
Scope of the Problem.
Inequities in the treatment of racial and ethnic minority patients with acute and chronic HF likely contributes to their disparate outcomes. The early recognition of HF can decrease morbidity; however, first diagnoses of HF are more likely to be missed in the outpatient setting for women and Black patients.67 Access to novel medical and device therapies is imperative for all patients with HF, particularly those at the highest risk for death and hospitalization. Novel HF therapies shown to decrease morbidity and mortality are not always affordable, even for some patients with insurance coverage. Patients face coverage gaps, and a lack of financial assistance programs may render medications inaccessible, increasing the risk for discontinuation of therapies and worsening HF. Recent qualitative analyses demonstrate that substantial out-of-pocket cost variation influences patients’ willingness to take GDMT, even with clear patient understanding of the mortality benefit, suggesting a need for further cost containment and transparency to promote shared decision-making.68,69
With regard to advanced HF therapies, Black and Hispanic patients present at a later stage of illness for advanced therapies evaluation, are sicker at the time of listing for HT or left ventricular assist device implantation, and have longer HT wait times with higher waitlist mortality.70 Although Black patients make up almost 25% of waitlist candidates for HT, there is growing concern that the number of racial and ethnic minority patients receiving advanced HF therapies remains disproportionately lower than the number of racial and ethnic minority patients who have HF. Implicit bias may contribute to differential allocation of advanced therapies for racial–ethnic minority patients and for women.71,72 Assumptions regarding patients’ ability to comply with therapies may be negatively influenced by SES, race, ethnicity, gender, marital status, and other demographic variables. Black patients, in particular, are more likely to be perceived as nonadherent by health care clinicians, as repeatedly demonstrated in studies that have used clinical vignettes to analyze the effect of implicit bias on clinical care.41
Solutions.
There are multiple opportunities to improve inequities in the treatment of racial and ethnic minority patients across the spectrum of HF care. In the electronic medical record, health systems should ensure a patient’s race or ethnicity is captured by self-report, and not assigned by clinicians or admitting staff, with enough categories to disaggregate groups. A greater use of telehealth has the potential to expand access to CV and HF specialists and should be championed by health care systems and societies. The HFSA has advocated for increased use of telehealth to improve the delivery of HF care73 and joined other stakeholders in writing to Congress in June 2020 to advance permanent telehealth reform after the coronavirus disease 2019 pandemic, prioritizing in part the removal of obsolete restrictions on the location of the patient and ensuring federally qualified health centers and rural health clinics can furnish telehealth services. However, as telehealth is more widely adopted, it is critical to ensure that care is equitable with expansion of broadband access and access to digital devices in the most vulnerable communities. To further enhance the quality of care able to be administered by telemedicine, more work is needed to provide or subsidize the cost of basic medical equipment for patients with HF (ie, scale, blood pressure cuff, pillbox). To enhance patient access to novel medical and device therapies to treat HF, corporate partners should ensure price transparency and affordability.
The composition of the multidisciplinary advanced therapies selection committee is vital and should be representative of the patient populations we serve. Implicit bias and antiracism training should be mandated for selection committee members and processes to decrease bias in patient selection should be implemented wherever possible. Examples include excluding race and ethnicity in patient presentations, using initials instead of full names that can hint to race or ethnicity, ensuring respectful and focused discussions of patients at meetings, and creating policies that apply to all patients that may decrease inequities in the allocation of advanced therapies. Centers that offer advanced HF therapies should periodically review their allocation by race or ethnicity and compare this outcome with regional demographics to ensure that patients from diverse backgrounds are not turned down for advanced therapies disproportionately. Centers that offer advanced HF therapies should also work closely with referring clinicians to ensure that all eligible patients are being referred in a manner that is consistent with their goals of care, preferably within the “golden window.”74 Financial and social support requirements often render the most vulnerable patients in our communities ineligible for advanced therapies. Steep financial requirements for HT listing may be unattainable for patients from disadvantaged backgrounds. Ambiguous definitions regarding social support can leave room for bias when assessing eligibility, particularly for female patients with HF.71,75 Because patients from racial and ethnic minority groups develop HF at younger ages than other racial and ethnic groups, for example, at ages where patients and/or care partners are still working or still have to provide care for minor children, overly stringent requirements for advanced therapies may present unique barriers in these populations. For institutions to be held accountable to best help the communities they serve, single centers should conduct ongoing annual reviews to ensure transparency and minimize bias in the selection process.
Structure and Policy
Scope of the Problem.
Structural racism refers to racial discrimination that is fostered by laws and practices, sanctioned and implemented by various levels of government, and embedded in the economic system as well as in cultural and societal norms.26 The cumulative effects of structural racism have resulted in persistent economic inequality that affects almost every facet of life for individuals from racial and ethnic minority groups, from school quality and educational attainment, to job opportunities, to the ability to acquire home loans, which ultimately affects wealth, to proximity to grocery stores, and the availability of healthy foods.76 Higher numbers of encounters with police, as well as frank police violence and mass incarceration, can lead to increased experience of anxiety and posttraumatic stress disorder for those directly impacted and other community members.77
Some component of the increased risk for HF among individuals from racial and ethnic minority groups is driven by structural racism both outside of and within the health care system that leads to later diagnoses and a worse quality of care. Access to health care is lower for individuals from racial and ethnic minority groups for multiple reasons. Workers from racial and ethnic minority groups are more likely to be paid poverty-level wages than White workers, impacting salary and wealth, but also benefits such as health insurance and subsequent access to medical care and medication coverage.78 Because the United States lacks a health care safety net for adults under the age of 65 years, adults from racial and ethnic minority groups are more likely to be affected by uninsurance and underinsurance.79,80 A lack of access to preventive care eliminates the possibility for HF prevention for patients who are at risk owing to the presence of conditions, including hypertension, obesity, and diabetes. Even after a HF diagnosis, uninsured and underinsured patients may need to be followed in federally funded clinics or indigent care clinics with fewer resources. Similarly, racial and ethnic minority patients are more likely to be cared for in community and safety net hospital settings as a result of neighborhood segregation, and thus are less likely to receive the most specialized care available for HF (including GDMT and devices).
Solutions.
Policies that improve and ensure equitable access to affordable health care and evidencebased preventive services, such as Medicaid expansion to low-income adults, have a substantial impact on decreasing health care disparities by race and ethnicity.52,81 Nationally, nearly 6 in 10 people (59%) in the coverage gap are people of color, and approximately 50% of those individuals are employed but have incomes below the poverty level because they work low-wage jobs.80 Although recent analyses document that social vulnerability is associated with an increased risk of premature CVD mortality, and premature HF mortality for Black Americans in particular, there is a striking lack of Medicaid expansion in areas of the United States where social vulnerability is associated with the greatest risk for premature CVD and HF mortality.82,83 Thus, continued efforts to prioritize universal insurance coverage, improved health care access, and appropriate referral for patients with HF who require specialized care, are viable and sustainable methods to decrease health care disparities. Moreover, ensuring equal access to the political process and protecting voting rights can also help to decrease health care disparities; those groups facing barriers to the voting process (people of color, people with disabilities, low-income individuals, and the uninsured) are also disproportionately more likely to be impacted by health disparities.84
Research Priorities
Scope of the Problem.
Despite notable differences in underlying disease pathophysiology, biomarkers (ie, natriuretic peptides) and clinical outcomes by race and ethnicity and sex, persistent underrepresentation of women and racial and ethnic minorities in HF trials has resulted in a paucity of data to determine treatment effectiveness in these populations.85–89 Poor clinical trial representation may be one reason for the significant differences between trial results and real-world clinical outcomes.90 Therefore, to improve HF care, it is necessary to improve diversity within our research cohorts, diversify our investigative teams, and expand rigorous study design that will simultaneously investigate genetic determinants that underlie heterogeneity in therapeutic response as well as SDOH that undermine the effectiveness of available therapies.
To continue to improve the field of HF, we must continue to promote diversity as a core value. Our future is shaped by science and our research cohorts are shaped by investigators who should represent the diversity of our patient population. Recruitment of racial–ethnic minorities and women in clinical trials has been more successful when led by investigators reflecting these populations, such as in A-HeFT (n= 1050 Black patients) and the Women’s Health Initiative (n = 161,856 women).21,91 Both clinician and patient attitudes can affect the quality of communication during clinical encounters with racial–ethnic minority patients, which can in turn impact the likelihood of research participation. A recent meta-analysis demonstrated that Black patients consistently experienced poorer communication quality, information giving, and participatory decision-making than White patients.92 In a single study of video-recorded interactions that examined how oncologists discussed clinical trials with Black and White patients, investigators found that interactions with Black patients were shorter in length, clinical trials were mentioned less frequently, and, when clinical trials were mentioned, less time was spent discussing them as compared with the amount of time spent with White patients.93 Moreover, studies assessing barriers to enrollment of racial–ethnic minority patients in clinical trials have found that mistrust in research and the medical system were common barriers to minority patients’ willingness to enroll in clinical trials, but other factors including provision of transportation, childcare, and flexible study design were also important factors.94,95
Solutions.
Unique recruitment strategies may be necessary to enroll patients from marginalized populations. The Women’s Health Initiative, for instance, included 10 centers capable of recruiting more than 50% racial and ethnic minority patients to enrich the cohort with non-White participants. Racial and ethnic minority recruiting centers were allowed to create research material that appealed to their population and brochures were also provided to all centers in Spanish. Prescreening visits were organized to promote interest and trust with the investigators with subsequent visits aimed at further developing this relationship. Recruitment differed by race and ethnicity, and careful documentation was collected to better understand what strategies were most effective.91 Similar strategies were successfully used in a small HF study that enrolled 406 patients (46% Black, 33% Hispanic, and 47% female) in New York City. Letters in the native language of the patient were sent discussing the study and informing patients that their medical caregiver agreed they could enroll. Financial compensation was offered for participation and travel, and bilingual recruiters were used to contact participants by phone to discuss the study, obtain consent, and help to arrange appointments.96 Therefore, successful recruitment of women and racial[C0]ethnic minorities in clinical trials is possible, but will require strategies that may be unique to each center and requires a diverse group of investigators and research staff that share language, sex, and race and ethnicity with the participants to earn trust.
Promoting diversity in HF research with the express aim of reducing health care disparities can be achieved by using various strategic initiatives. Diverse representation in the leadership of future trials (ie, steering committees, site principal investigators) is required. Steering committees can improve enrollment of racial and ethnic minority patients by compiling a list of clinics, hospitals, and regions with a high prevalence of racial and ethnic minority patients with HF. Moreover, partnering with organizations that have a strong community presence and have previously had success recruiting racial and ethnic minority patients with HF can enhance participant diversity. For example, the WomenHeart Science and Leadership Symposium for Women With Heart Disease has trained more than 900 WomenHeart Champions to be advocates, educators, and effective leaders of support groups for women with heart disease and could be a model for successful strategies to recruit women and racial[C0]ethnic minority patients.97 Consent forms, brochures, and educational material should be translated to different languages to enhance minority education and participation. Data collection for registries and trials can be improved by requesting more granular information on race and ethnicity in case report forms (ie, South Asian to refer to India, Nepal, Pakistan, Sri Lanka, or Pakistan and East Asian to refer to China, Japan, Hong Kong, Korea). In science writing and reporting, investigators should be very deliberate and sensitive in their use of terms to describe racial and ethnic minority groups. For example, the use of the term BIPOC (Black, Indigenous, and people of color) might be used in an effort to be inclusive of the oppression faced by many minority groups in the United States. However, it might also “blur the differences between groups it is meant to center,” particularly if important differences in the unique experiences of certain communities should actually be highlighted.98 Investigators should refer to many recently published documents that provide guidance on how to report race and ethnicity in scientific journals.99,100
The Role of Peer-Reviewed Journals in Promoting Diversity, Equity, and Inclusion
Scope of the Problem.
A journal’s editorial board plays a critical role in paving the trajectory of science, knowledge, and discoveries by evaluating the novelty and perceived value of their peers’ research. As such, editors are essential to structure the community of scholars contributing to the scientific dialogue in their respective field, because editorial board composition holds great influence over the types of science published in peer-reviewed journals. It is of critical importance that the editorial board reflect the principles of diversity, equity, and inclusion (DEI) by demonstrating these core principles in their roster of board members, and maintaining a balanced, diverse board with representation from distinct cultural, ethnic, and international backgrounds. Currently, the vast majority of editorial board members come from high-income countries and are predominantly male and White,101 despite data showing that editorial board diversity can increase innovation, foster creativity, enhance quality of research, and validate peers from unrepresented minority groups.102 Solutions. Scientific journals and research organizations should clearly state and demonstrate that DEI and belonging are core values.103 Journal editors should also consider requiring investigators to report the race and ethnicity of study populations in publications, particularly for clinical trials, so that generalizability of results can be appropriately assessed. Proposed strategies to account for representation and expansion of other geographical, racial, ethnic, and cultural groups (GRECO) in the peer review and manuscript submission process should include the following. (1) Internationalize the editorial board to have local editors evaluate research from nationally equivalent peers. This practice can enhance the profile and impact the articles published in the journal. (2) Provide editorial opportunities to scholars from emerging scientific regions. This step can decrease the effects of implicit bias against emerging countries. (3) Develop diverse and qualified writing/reviewer committees across the distinct career spectrum to improve the reporting of critical viewpoints to novel pieces of research. (4) Cultivate talent and promote future editors to become inclusive in the review and construct of the journal. (5) Create a DEI task force for developing future leaders and a pipeline of new CV reviewers who adhere to the guiding principles of DEI. (6) Execute benchmark data to track the diversity, inclusion, and transparency of peer reviewers and team members that conform the critical body of editors. This practice will uncover possible challenges and barriers that do not allow expanding selection of editors from unrepresented GRECO. (7) Request that all authors involved in a potential submission address DEI, language sensitivity, issues specific to marginalized groups, and that the scholar work involved collaboration with colleagues of divergent GRECO backgrounds.
Integrating representative groups from distinct backgrounds will expand collaborations with equal individuals who show interest in moving forward science and responsible to publish the highest quality of research possible. The more scholars that are embedded in a collaborative network, the greater the likelihood of having impactful research submitted.104 In academic careers, publications are crucial for career advancement and obtaining grants and promotions. To this extent, editorial board members are positioned as potential mentors to the authors whose work is being reviewed by providing constructive feedback through the reviewer comments which can serve as tool to enhance the authors writing and discussion of its work.
Conclusions
The impact of disparities in HF care in racial and ethnic minority populations cannot be understated. From CV risk factors and medical and device management, to options for advanced therapies, disparities in treatment persist across multiple domains (patient, community, and societal) in patients with HF. It remains of great importance to recognize the differences between race, ethnicity, and the influence of the various levels of racism on the SDOH, access to care, and ultimately health care disparities. Health care systems and societies are well-positioned to help decrease these disparities over time in a collaborative effort with clinicians, researchers, and patients. Ultimately, decreasing disparities and achieving health equity will require a sustained commitment to these principles with action at multiple levels of influence to help decrease risk and improve clinical outcomes in the most vulnerable populations with HF.
Supplementary Material
Footnotes
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.cardfail.2022.04.008.
References
- 1.Virani SS, Alonso A, Aparicio HJ, et al. Heartdisease and stroke statistics - 2021 update. Circulation 2021;143: e254–743.DOI:doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 2.Shah KS, Xu H, Matsouaka RA, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol 2017;70:2476–86. (In eng). DOI: 10.1016/j.jacc.2017.08.074. [DOI] [PubMed] [Google Scholar]
- 3.Morris AA, Ko YA, Hutcheson SH, Quyyumi A. Race/ethnic and sex differences in the association of atherosclerotic cardiovascular disease risk and healthy lifestyle behaviors. J Am Heart Assoc 2018;7:e008250. (In eng). DOI: 10.1161/jaha.117.008250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med 2008;168:2138–45. (In eng). DOI: 10.1001/archinte.168.19.2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawson CA, Zaccardi F, Squire I, et al. Risk factors for heart failure: 20-year population based trends by sex, socioeconomic status, and ethnicity. Circ Heart Fail 2020;13:e006472. DOI: 10.1161/CIRCHEARTFAILURE.119.006472. [DOI] [PubMed] [Google Scholar]
- 6.Vivo RP, Krim SR, Cevik C, Witteles RM. Heart failure in Hispanics. J Am Coll Cardiol 2009;53:1167–75. (In eng). DOI: 10.1016/j.jacc.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 7.Nayak A, Hicks AJ, Morris AA. Understanding the complexity of heart failure risk and treatment in Black patients. Circ Heart Fail 2020;13:e007264. (In eng). DOI: 10.1161/circheartfailure.120.007264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Healthy People. 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Accessed June 30.
- 9.Vivo RP, Krim SR, Cevik C, Witteles RM. Heart failure in Hispanics. J Am Coll Cardiol 2009;53:1167–75. DOI: 10.1016/j.jacc.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 10.Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National differences in trends for heart failure hospitalizations by sex and race/ethnicity. Circ Cardiovasc Qual Outcomes 2017;10:e003552. DOI: 10.1161/CIRCOUTCOMES.116.003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel SA, Krasnow M, Long K, Shirey T, Dickert N, Morris AA. Excess 30-day heart failure readmissions and mortality in Black patients increases with neighborhood deprivation. Circ Heart Fail 2020;13:e007947. (In eng). DOI: 10.1161/circheartfailure.120.007947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ziaeian B, Heidenreich PA, Xu H, et al. Medicare expenditures by race/ethnicity after hospitalization for heart failure with preserved ejection fraction. JACC Heart Fail 2018;6:388. DOI: 10.1016/j.jchf.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation 2021;143: e254–743. DOI: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 14.Glynn P, Lloyd-Jones DM, Feinstein MJ, Carnethon M, Khan SS. Disparities in cardiovascular mortality related to heart failure in the United States. J Am Coll Cardiol 2019;73:2354–5. (In eng). DOI: 10.1016/j.jacc.2019.02.042. [DOI] [PubMed] [Google Scholar]
- 15.Breathett K, Sims M, Gross M, et al. Cardiovascular health in American Indians and Alaska Natives: a scientific statement from the American Heart Association. Circulation 2020;141:e948–59. DOI: doi: 10.1161/CIR.0000000000000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nayak A, Cole RT, Morris AA. Race/ethnic disparities in cardiac transplantation. Curr Cardiovasc Risk Reports 2019;13:33. DOI: 10.1007/s12170-019-0629-6. [DOI] [Google Scholar]
- 17.Steinberg RS, Nayak A, Morris AA. Racial differences in outcomes after receiving advanced heart failure therapies. Curr Opin Cardiol 2021;36:352–9. (In eng). DOI: 10.1097/hco.0000000000000854. [DOI] [PubMed] [Google Scholar]
- 18.Maredia H, Bowring MG, Massie A, et al. Better understanding of the disparity associated with Black race in heart transplant outcomes: a national registry analysis. Circ Heart Fail 2021;14:e006107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wayda B, Clemons A, Givens RC, et al. Socioeconomic disparities in adherence and outcomes after heart transplant. Circ Heart Fail 2018;11:e004173. DOI: 10.1161/CIRCHEARTFAILURE.117.004173. [DOI] [PubMed] [Google Scholar]
- 20.Bonham VL, Warshauer-Baker E, Collins FS. Race and ethnicity in the genome era: the complexity of the constructs. Am Psychol 2005;60:9–15. (In eng). DOI: 10.1037/0003-066x.60.1.9. [DOI] [PubMed] [Google Scholar]
- 21.Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in Blacks with heart failure. N Engl J Med 2004;351:2049–57. DOI: 10.1056/NEJMoa042934. [DOI] [PubMed] [Google Scholar]
- 22.Jose PO, Frank AT, Kapphahn KI, et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol 2014;64:2486–94. (In eng). DOI: 10.1016/j.jacc.2014.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation 2018;138: e1–e34. (In eng). DOI: 10.1161/cir.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 24.Mehta H, Armstrong A, Swett K, et al. Burden of systolic and diastolic left ventricular dysfunction among Hispanics in the United States: insights from the Echocardiographic Study of Latinos. Circ Heart Fail 2016;9:e002733. (In eng). DOI: 10.1161/circheartfailure.115.002733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev 2011;8:115–32. (In eng). DOI: 10.1017/s1742058x11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N,Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453–63. (In eng). DOI: 10.1016/s0140673630569-x. [DOI] [PubMed] [Google Scholar]
- 27.Eberly LA, Richterman A, Beckett AG, et al. Identification of racial inequities in access to specialized inpatient heart failure care at an academic medical center. Circ Heart Fail 2019;12:e006214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breathett K, Liu WG, Allen LA, et al. African Americans are less likely to receive care by a cardiologist during an intensive care unit admission for heart failure. JACC Heart Fail 2018;6:413–20. DOI: 10.1016/j.jchf.2018.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borrell LN, Elhawary JR, Fuentes-Afflick E, et al. Race and genetic ancestry in medicine — a time for reckoning with racism. N Engl J Med 2021;384:474–80. DOI: 10.1056/NEJMms2029562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ozkor MA, Rahman AM, Murrow JR, et al. Differences in vascular nitric oxide and endothelium-derived hyperpolarizing factor bioavailability in Blacks and Whites. Arteriosclerosis, thrombosis, and vascular biology 2014;34:1320–7. (In eng). DOI: 10.1161/ATV-BAHA.113.303136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morris AA, Patel RS, Binongo JNG, et al. Racial differences in arterial stiffness and microcirculatory function between Black and White Americans. J Am Heart Assoc 2013;2:e002154. −e002154. (In eng). DOI: 10.1161/JAHA.112.002154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pratt J, Rebhun J, Zhou L, et al. Levels of mineralocorticoids in whites and blacks. Hypertension 1999; 34:315–9. [DOI] [PubMed] [Google Scholar]
- 33.Joseph JJ, Pohlman NK, Zhao S, et al. Association of serum aldosterone and plasma renin activity with ambulatory blood pressure in African Americans: the Jackson Heart Study. Circulation 2021;143:2355–66. DOI: doi: 10.1161/CIRCULATIONAHA.120.050896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morris AA, Nayak A, Ko Y-A, et al. Racial differences in diuretic efficiency, plasma renin, and rehospitalization in subjects with acute heart failure. . Circ Heart Fail 2020;13:e006827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gupta DK, de Lemos JA, Ayers CR, Berry JD, Wang TJ. Racial differences in natriuretic peptide levels: the Dallas Heart Study. JACC Heart Fail 2015;3:513–9. DOI: 10.1016/j.jchf.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patel N, Russell GK, Musunuru K, et al. Race, natriuretic peptides, and high-carbohydrate challenge: a clinical trial. Circ Res 2019;125:957–68. (In eng). DOI: 10.1161/circresaha.119.315026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quarta CC, Buxbaum JN, Shah AM, et al. The amyloidogenic v122i transthyretin variant in elderly Black Americans. N Engl J Med 2014;372:21–9. DOI: 10.1056/NEJMoa1404852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shah KB, Mankad AK, Castano A, et al. Transthyretin cardiac amyloidosis in Black Americans. Circ Heart Fail 2016;9:e002826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Powell-Wiley TM, Baumer Y, Baah FO, et al. Social determinants of cardiovascular disease. Circ Res 2022;130:782–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Golden SD, McLeroy KR, Green LW, Earp JAL, Lieberman LD. Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Health Educ Behav 2015;42(1 Suppl):8S–14S. DOI: 10.1177/1090198115575098. [DOI] [PubMed] [Google Scholar]
- 41.Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med 2018;199:219–29. (In eng). DOI: 10.1016/j.socscimed.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 42.Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health 2019;18:174. (In eng). DOI: 10.1186/s12939-019-1082-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DeVore AD, Granger BB, Fonarow GC, et al. Care optimization through patient and hospital engagement clinical trial for heart failure: rationale and design of CONNECT-HF. Am Heart J 2020;220:41–50. (In eng). DOI: 10.1016/j.ahj.2019.09.012. [DOI] [PubMed] [Google Scholar]
- 44.Allen LA, Venechuk G, McIlvennan CK, et al. An electronically delivered patient-activation tool for intensification of medications for chronic heart failure with reduced ejection fraction: the EPIC-HF Trial. Circulation 2021;143:427–37. (In eng). DOI: 10.1161/circulationaha.120.051863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies; 2003. [Google Scholar]
- 46.Churchwell K, Elkind MSV, Benjamin RM, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation 2020;142: e454–68. DOI: 10.1161/CIR.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 47.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health 2000;90:1212–5. (In eng). DOI: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lewsey SC, Breathett K. Racial and ethnic disparities in heart failure: current state and future directions. Curr Opin Cardiol 2021;36:320–8. (In eng). DOI: 10.1097/hco.0000000000000855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lo AX, Donnelly JP, Durant RW, et al. A national study of U.S. emergency departments: racial disparities in hospitalizations for heart failure. Am J Prev Med 2018;55:S31–9. DOI: 10.1016/j.amepre.2018.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cleveland Manchanda EC, Marsh RH, Osuagwu C, et al. Heart Failure Admission Service Triage (H-FAST) study: racialized differences in perceived patient self-advocacy as a driver of admission inequities. Cureus 2021;13:e13381. (In eng). DOI: 10.7759/cureus.13381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bozkurt B, Coats AJS, Tsutsui H, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail 2021;27:387–413. DOI: 10.1016/j.cardfail.2021.01.022. [DOI] [Google Scholar]
- 52.Warner JJ, Benjamin IJ, Churchwell K, et al. Advancing healthcare reform: the American Heart Association’s 2020 Statement of Principles for Adequate, Accessible, and Affordable Health Care: A Presidential Advisory From the American Heart Association. Circulation 2020;141:e601–14. DOI: doi: 10.1161/CIR.0000000000000759. [DOI] [PubMed] [Google Scholar]
- 53.Akwo EA, Kabagambe EK, Harrell FE, et al. Neighborhood deprivation predicts heart failure risk in a lowincome population of Blacks and Whites in the Southeastern United States. Circ Cardiovasc Qual Outcomes 2018;11:e004052. DOI: 10.1161/CIRCOUTCOMES.117.004052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morris AA, McAllister P, Grant A, et al. Relation of living in a food desert to recurrent hospitalizations in patients with heart failure. Am J Cardiol 2019;123:291–6. DOI: 10.1016/j.amjcard.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shirey TE, Hu Y, Ko YA, et al. Relation of neighborhood disadvantage to heart failure symptoms and hospitalizations. Am J Cardiol 2021;140:83–90. (In eng). DOI: 10.1016/j.amjcard.2020.10.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Groarke JD, Stevens SR, Mentz RJ, et al. Clinical significance of early fluid and weight change during acute heart failure hospitalization. J Card Fail 2018;24:542–9. DOI: 10.1016/j.cardfail.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 57.Whybrow S, Hollis JL, Macdiarmid JI. Social deprivation is associated with poorer adherence to healthy eating dietary goals: analysis of household food purchases. J Public Health 2017;40:e8–e15. DOI: 10.1093/pubmed/fdx007. [DOI] [PubMed] [Google Scholar]
- 58.Yancy Clyde W, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure. Circulation 2013;128:e240–327. DOI: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 59.Bower KM, Thorpe RJ Jr., Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med 2014;58:33–9. (In eng). DOI: 10.1016/j.ypmed.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bachmann JM, Huang S, Gupta DK, et al. Association of neighborhood socioeconomic context with participation in cardiac rehabilitation. J Am Heart Assoc 2022;6:e006260. DOI: 10.1161/JAHA.117.006260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bailey ZD, Feldman JM, Bassett MT. How structural racism works — racist policies as a root cause of U.S. racial health inequities. N Engl J Med 2020;384:768–73. DOI: 10.1056/NEJMms2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alkhouli M, Alqahtani F, Holmes DR, Berzingi C. Racial disparities in the utilization and outcomes of structural heart disease interventions in the United States. J Am Heart Assoc 2019;8:e012125. (In eng). DOI: 10.1161/jaha.119.012125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nathan AS, Yang L, Yang N, et al. Racial, ethnic, and socioeconomic disparities in access to transcatheter aortic valve replacement within major metropolitan areas. JAMA Cardiol 2022;7:150–7. (In eng). DOI: 10.1001/jamacardio.2021.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aggarwal R, Hammond JG, Joynt Maddox KE, Yeh RW, Wadhera RK. Association between the proportion of black patients cared for at hospitals and financial penalties under value-based payment programs. JAMA 2021;325:1219–21. DOI: 10.1001/jama.2021.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA 2013;309:342–3. DOI: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 66.Lear SA, Singer J, Banner-Lukaris D, et al. Randomized trial of a virtual cardiac rehabilitation program delivered at a distance via the internet. Circ Cardiovasc Qual Outcomes 2014;7:952–9. DOI: doi: 10.1161/CIRCOUTCOMES.114.001230. [DOI] [PubMed] [Google Scholar]
- 67.Sandhu AT, Tisdale RL, Rodriguez F, et al. Disparity in the setting of incident heart failure diagnosis. Circ Heart Fail 2021;14:e008538. Circheartfailure121008538. (In eng). DOI: 10.1161/circheartfailure.121.008538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smith GH, Shore S, Allen LA, et al. Discussing out-ofpocket costs with patients: shared decision making for sacubitril-valsartan in heart failure. J Am Heart Assoc 2019;8:e010635. DOI: 10.1161/JAHA.118.010635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rao BR, Dickert NW, Morris AA, et al. Heart failure and shared decision-making: patients open to medication-related cost discussions. Circ Heart Fail 2020;13:e007094. (In eng). DOI: 10.1161/circheartfailure.120.007094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lala A, Ferket BS, Rowland J, et al. Abstract 17340: disparities in wait times for heart transplant by racial and ethnic minorities. Circulation 2018;138(Suppl 1): A17340.–A17340. DOI: doi: 10.1161/circ.138.suppl_1.17340. [DOI] [Google Scholar]
- 71.Breathett K, Yee E, Pool N, et al. Association of gender and race with allocation of advanced heart failure therapies. JAMA Network Open 2020;3: e2011044.–e2011044. DOI: 10.1001/jamanetwor-kopen.2020.11044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Breathett K, Yee E, Pool N, et al. Does race influence decision making for advanced heart failure therapies? J Am Heart Assoc 2019;8:e013592. DOI: 10.1161/JAHA.119.013592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gorodeski EZ, Goyal P, Cox ZL, et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail 2020;26:448–56. DOI: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Morris AA, Khazanie P, Drazner MH, et al. Guidance for timely and appropriate referral of patients with advanced heart failure: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2021;144:e238–50. [DOI] [PubMed] [Google Scholar]
- 75.Steinberg RS, Nayak A, Burke MA, et al. Association of race and gender with primary caregiver relationships and eligibility for advanced heart failure therapies. Clin Transplant 2021;36:e14502. (In eng). DOI: 10.1111/ctr.14502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mitchell B, Franco JHOLC. “REDLINING” maps: the persistent structure of segregation and economic inequality. Washington, DC: National Community Reinvestment Coalition; 2018. [Google Scholar]
- 77.Sewell AA, Jefferson KA, Lee H. Living under surveillance: gender, psychological distress, and stop-question-and-frisk policing in New York City. Soc Sci Med 2016;159:1–13. DOI: 10.1016/j.socscimed.2016.04.024. [DOI] [PubMed] [Google Scholar]
- 78.Economic Policy Institute. Workers of color are far more likely to be paid poverty-level wages than white workers. 2018. Available at: https://www.epi.org/blog/workers-of-color-are-far-more-likely-to-be-paid-poverty-level-wages-than-white-workers/.
- 79.Garfield R, Orgera K, Damico A. The coverage gap: uninsured poor adults in states that do not expand Medicaid. 2022. Available at: https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/.
- 80.Garfield R, Damico A, Rudowitz R. Taking a closer look at characteristics of people in the coverage gap. Available at: https://www.kff.org/policy-watch/tak-ing-a-closer-look-at-characteristics-of-people-in-the-coverage-gap/.
- 81.Guth M, Artiga S, Pham O. Effects of the ACA Medicaid expansion on racial disparities in health and health care. Available at: https://www.kff.org/medic-aid/issue-brief/effects-of-the-aca-medicaid-expan-sion-on-racial-disparities-in-health-and-health-care/.
- 82.Khan SU, Javed Z, Lone AN, et al. Social vulnerability and premature cardiovascular mortality among US counties, 2014 to 2018. Circulation 2021;144:1272–9. (In eng). DOI: 10.1161/circulationaha.121.054516. [DOI] [PubMed] [Google Scholar]
- 83.Gangavelli A, Morris AA. Premature cardiovascular mortality in the United States: who will protect the most vulnerable among us? Circulation 2021;144:1280–3. (In eng). DOI: 10.1161/circulationaha.121.056658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yagoda N addressing health disparities through voter engagement. Ann Fam Med 2019;17:459–61. (In eng). DOI: 10.1370/afm.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hsich EM, Pina IL. Heart failure in women: a need for prospective data. J Am Coll Cardiol 2009;54:491–8. (http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19643307). [DOI] [PubMed] [Google Scholar]
- 86.Yancy CW. Heart failure in African Americans. Am J Cardiol 2005;96:3i–12i. DOI: 10.1016/j.amjcard.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 87.Sullivan K, Doumouras BS, Santema BT, et al. Sex-specific differences in heart failure: pathophysiology, risk factors, management, and outcomes. Can J Cardiol 2021;37:560–71. DOI: 10.1016/j.cjca.2020.12.025. [DOI] [PubMed] [Google Scholar]
- 88.Punnoose LR, Lindenfeld J. Sex-specific differences in access and response to medical and device therapies in heart failure: state of the art. Prog Cardiovasc Dis 2020;63:640–8. DOI: 10.1016/j.pcad.2020.09.004. [DOI] [PubMed] [Google Scholar]
- 89.Tahhan AS, Vaduganathan M, Greene SJ, et al. Enrollment of older patients, women, and racial and ethnic minorities in contemporary heart failure clinical trials: a systematic review. JAMA Cardiol 2018;3:1011–9. DOI: 10.1001/jamacardio.2018.2559. [DOI] [PubMed] [Google Scholar]
- 90.Greene SJ, DeVore AD, Sheng S, et al. Representativeness of a heart failure trial by race and sex: results from ASCEND-HF and GWTG-HF. JACC Heart Fail 2019;7:980–92. DOI: 10.1016/j.jchf.2019.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fouad MN, Corbie-Smith G, Curb D, et al. Special populations recruitment for the Women’s Health Initiative: successes and limitations. Control Clin Trials 2004;25:335–52. DOI: 10.1016/j.cct.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 92.Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Dispar 2018;5:117–40. (In eng). DOI: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Eggly S, Barton E, Winckles A, Penner LA, Albrecht TL. A disparity of words: racial differences in oncologist-patient communication about clinical trials. Health Expect 2015;18:1316–26. (In eng). DOI: 10.1111/hex.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Paskett ED, Reeves KW, McLaughlin JM, et al. Recruitment of minority and underserved populations in the United States: the Centers for Population Health and Health Disparities experience. Contemp Clin Trials 2008;29:847–61. (In eng). DOI: 10.1016/j.cct.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rivers D, August EM, Sehovic I, Lee Green B, Quinn GP. A systematic review of the factors influencing African Americans’ participation in cancer clinical trials. Contemp Clin Trials 2013;35:13–32. (In eng). DOI: 10.1016/j.cct.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 96.Sisk JE, Horowitz CR, Wang JJ, McLaughlin MA, Hebert PL, Tuzzio L. The success of recruiting minorities, women, and elderly into a randomized controlled effectiveness trial. Mt Sinai J Med 2008;75:37–43. DOI: 10.1002/msj.20014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.WomenHeart Champions. Available at: https://www.womenheart.org/about-us/become-a-womenheartchampion/. Accessed June 28, 2021.
- 98.Vox. Why the term “BIPOC” is so complicated, explained by linguists. Available at: https://www.vox.com/2020/6/30/21300294/bipoc-what-does-it-meancritical-race-linguistics-jonathan-rosa-deandra-mileshercules. Accessed April 4, 2022.
- 99.Flanagin A, Frey T, Christiansen SL, AMoS Committee. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA 2021;326:621–7. DOI: 10.1001/jama.2021.13304. [DOI] [PubMed] [Google Scholar]
- 100.Breathett K, Spatz ES, Kramer DB, et al. The groundwater of racial and ethnic disparities research. Circ Cardiovasc Qual Outcomes 2021;14:e007868. DOI: doi: 10.1161/CIRCOUTCOMES.121.007868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Espin J, Palmas S, Carrasco-Rueda F, et al. A persistent lack of international representation on editorial boards in environmental biology. PLoS Biol 2017;15: e2002760. DOI: 10.1371/journal.pbio.2002760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bhaumik S, Jagnoor J. Diversity in the editorial boards of global health journals. BMJ Glob Health 2019;4:e001909. DOI: 10.1136/bmjgh-2019-001909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mentz RJ, Lala A. Diversity, equity and inclusion at the Journal of Cardiac Failuret. J Card Fail 2021;27:263–4. DOI: 10.1016/j.cardfail.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 104.Liao CH. How to improve research quality? Examining the impacts of collaboration intensity and member diversity in collaboration networks. Scientometrics 2011;86:747–61. DOI: 10.1007/s11192-010-0309-2. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


