Abstract
Background
The COVID-19 pandemic and its impact on hospitals' activity and organization has imposed a vast change in standard neurosurgical oncology practice to accommodate for shifting resources.
Aims
This investigation aims to analyse the nationwide capability in reorganizing the surgical neuro-oncological activity during the COVID-19 pandemic to evaluate whether COVID-19-pandemic influenced the surgical management in these patients.
Method
A web-based dataset model organized by the Italian Neurosurgical Society (SINCh) was sent to all the Italian neurosurgical departments in May 2021, requesting to report the types and numbers of surgical procedures performed in the pre-pandemic period (from March 9th 2019 to March 9th 2020) compared to the pandemic period (from March 10th 2020 to March 10th 2021).
Results
This multicentre investigation included the surgical activity of 35 Italian Neurosurgical Departments in a pre-pandemic year versus a pandemic year. During the COVID period, 699 fewer neuro-oncological patients were operated on than in the pre-COVID period. We noted a slight increase in urgency and a more severe decrease in elective and benign pathology. None of these differences was statistically significant. Surgically treated patients who tested positive for SARS-CoV-2 were 36, of which 11 died. Death was found to be COVID-related only in 2 cases.
Conclusion
The reorganization of the Italian Neurosurgical Departments was able to guarantee a redistribution of the CNS tumors during the inter-pandemic periods, demonstrating that patients even in the pandemic era could be treated without compromising the efficacy and safety of the surgical procedure.
Keywords: COVID-19, Neuroncology, SINch, Survey
1. Introduction
The COVID-19 pandemic has had a distressing impact on the National Health System (NHS), causing significant organizational, processional and management struggles.1
Besides the respiratory problems,2, SARS-CoV-2 has been responsible for a decrease in the number of patients with other conditions who accessed the emergency departments,3,4, including neurosurgical conditions.
Italy was among the first countries overwhelmed by the COVID-19 pandemic in February 2020, recording an extraordinary mortality rate, mainly related to the high percentage of the elderly population.5 Considering the tremendous pressure on the healthcare system for the diagnosis and treatment of COVID-19 patients, the Government declared a national lockdown on March 9, 20206
To limit the spreading of the infection and reduce the pressure on the national health service, the Italian Government imposed a nationwide lockdown of all non-essential services between March 10, 2020, and May 3, 2020. Hospitals were forced to reduce elective activities for the more significant part of the period between March and May 2020, limiting patients' access and dedicating most resources to treating symptomatic COVID-19 patients.7
In the subsequent inter-pandemic period, from May to October 2020, following the first wave, the number of COVID-19 patients decreased, lockdown measures relaxed, and elective surgeries and clinic services started again.8 Between October and November 2020, when the number of COVID-19 patients again increased, the second wave of the COVID-19 pandemic was recorded. During this period, 30–35% capacity of hospitals was reserved for COVID-19 patients, but elective surgeries and outpatient services were ongoing.9
Hospitals quickly changed their organization, designing COVID-wards internal paths for COVID patients and specifically dedicated operating rooms.10,11
This study aimed to weigh the effect of the COVID-19 pandemic and the consequent lockdown6 on the treatment of CNS tumors, performing a multicenter analysis in 35 Italian neurosurgical centres with different geographical and structural characteristics. Similar studies have been published worldwide.12, 13, 14, 15, 16, 17
A secondary objective was to investigate how the Italian neurosurgical centres have reorganized their activities to ensure care for patients who needed it.
2. Materials and methods
2.1. Study population
Thirty-five Italian neurosurgical centres were involved in this study, listed in Table 1. A shared web-based survey organized by the Italian Society of Neurosurgery (SINch®) was submitted to two neurosurgeons in each of the centres involved.18 Respondents were asked to use data from their surgical records. Different queries investigating the COVID period, defined from March 10 2020, to March 10 2021, were analyzed, including.
-
1
the exact number of neuro-oncological surgeries, emergency or elective.
-
2
the type of tumour pathology.
-
3
the specific type of surgical procedure performed.
Table 1.
List of neurosurgical centers participating in the multicenter study with subdivision in North and Central-South groups.
| Hospital | City | Group |
|---|---|---|
| U.O. Neurochirurgia Ospedale Regionale "F.Miulli" | Acquaviva delle Fonti | Central-South |
| U.O.C. Neurochirurgia, Dipartimento di Neuroscienze, A.O.U. Friuli Centrale | Udine | North |
| U.O. Neurochirurgia, Fondazione IRCCS Policlinico San Matteo | Pavia | North |
| U.O. Neurochirurgia, A.O.U. "Federico II" | Napoli | Central-South |
| U.O.C. Neurochirurgia Policlinico Universitario di Germaneto | Catanzaro | Central-South |
| U.O.C. Neurochirurgia, Istituto Clinico Humanitas | Milano | North |
| U.O. Neurochirurgia, IRCSS Istituto Nazionale Tumori "Regina Elena" | Roma | Central-South |
| U.O.C. Neurochirurgia Ospedale "A.Perrino" | Brindisi | Central-South |
| U.O.C. Neurochirurgia A.O.U. Padova | Padova | North |
| U.O. Neurochirurgia, A.O.U. Ferrara | Ferrara | North |
| U.O. Neurochirurgia, A.O.U. Policlinico "Paolo Giaccone" | Palermo | Central-South |
| U.O Neurochirurgia, A.O.U. Maggiore della Carità | Novara | North |
| U.O. Neurochirurgia, Ospedale Vito Fazzi | Lecce | Central-South |
| U.O.C. Neurochirurgia Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico | Milano | North |
| U.OC. Neurochirurgia, Ospedale Santa Maria delle Grazie | Pozzuoli | Central-South |
| S.O.D. Neurochirurgia – A.O.U. Careggi | Firenze | Central-South |
| U.O.C. Neurochirurgia A.O.U. Sassari | Sassari | Central-South |
| U.O. Neurochirurgia 2 Fondazione IRCCS Istituto Neurologico C. Besta | Milano | North |
| U.O. Neurochirurgia, Ospedale Fabrizio Spaziani | Frosinone | Central-South |
| U.O.C. Neurochirurgia A.O. Cosenza | Cosenza | Central-South |
| U.O. Neurochirurgia, A.O.U. Sant'Andrea | Roma | Central-South |
| U.O. Neurochirurgia, ULSS2 Marca Trevigiana Ospedale Ca'Foncello | Treviso | North |
| U.O. Neurochirurgia, Ospedale Civile Santi Antonio e Biagio e Cesare Arrigo | Alessandria | North |
| U.O. Neurochirurgia, AULSS 8 - Ospedale San Bortolo | Vicenza | North |
| U.O. Neurochirurgia Ospedale dell'Angelo | Mestre | North |
| U.O Neurochirurgia, Ospedali Riuniti di Ancona | Ancona | Central-South |
| U.O. - Neurochirurgia - Ospedale "M. Bufalini" - AUSL Romagna | Cesena | Central-South |
| U.O. Neurochirurgia, Ospedale di Bolzano | Bolzano | North |
| U.O. Neurochirurgia Fondazione Policlinico Universitario Gemelli | Roma | Central-South |
| U.O. Neurochirurgia, Mater Olbia Hospital | Olbia | Central-South |
| U.O Neurochirurgia, Istituto Neuromed | Pozzilli-Isernia | Central-South |
| U.O.C. Neurochirurgia, ASST Spedali Civili di Brescia | Brescia | North |
| U.O. Neurochirurgia, University Hospital, Catania | Catania | Central-South |
| U.O. Neurochirurgia, A.O.U. Città della Salute e Della Scienza | Torino | North |
| U.O.C. Neurochirurgia AOU Policlinico “G. Martino” | Messina | Central-South |
Comparing results for each answer with the corresponding months of the years 2019–2020 (from March 9, 2019, to March 9 2020), defined as pre-COVID period and used as the control group. We also considered the exact number of COVID-19-positive patients operated on during the COVID period. We also performed a sub-analysis of the results, dividing the participating centres into two macro-categories: north and centre-south, as shown in Table 1, to highlight disparities between different Italian areas.
2.2. Statistical analysis
We used Student-tests and ANOVA for continuous variables, and chi-square or Fisher's exact test was used for categorical variables. Continuous data are reported as the mean ± standard deviation. A p < 0.05 was considered statistically significant.
Data were collected by considering the sum of single-institution surgical activity in the 12 months before the COVID-19 pandemic (from March 9 2019, to March 9 2020) and the sum of single-institution surgical activity during the first year of the COVID-19 pandemic (from March 10 2020 to March 10 2021).
Considering the geographical distribution of the participating centres (15 North, 4 Center and 16 South), we compared the surgical procedures in the north versus those in Center + South to balance the results. All statistical procedures were performed using SAS software, version 9.4 (SAS, Cary, NC, USA) and SPSS statistic software, version 26.0 (IBM®)
3. Results
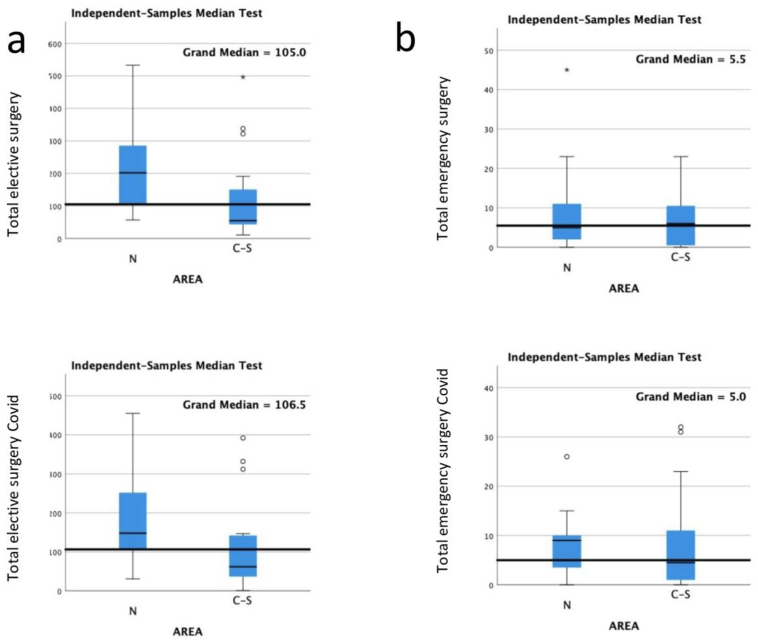
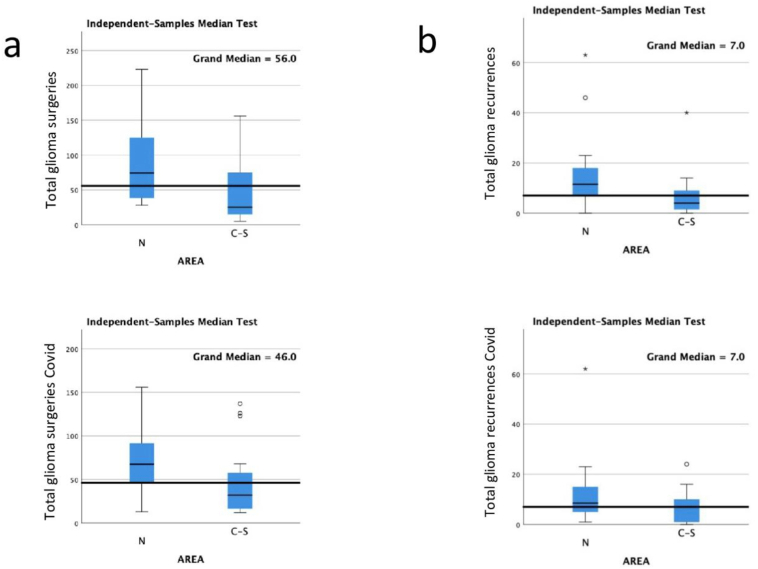
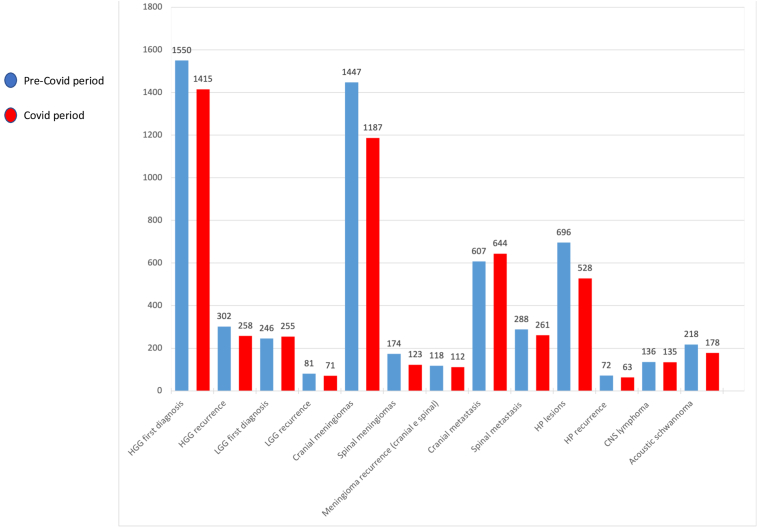
Thirty-five neurosurgical centres answered the web-based survey released by SINch; 15 were in the country's north, and 20 were in the Center-South. Table 2 shows a direct comparison in the number of patients with CNS tumors undergoing surgery. In the COVID period, we operated 5372 patients, while in the pre-COVID period we operated 6071 patients, with a difference of 699 fewer patients (p = 0.5); we carried out a total of 305 emergency neurooncological interventions compared to 244 of the same period in 2019 and 5827 elective surgeries compared to 5067 of the COVID period (p = 0.5; p = 0.73). Fig. 1 describes a statistical analysis comparing emergency and elective surgeries in the two periods of interest, obtaining no statistically significant results. Table 3 considers the various types of CNS tumors, comparing the COVID period with the pre-COVID period. We observed that first diagnoses of high-grade glioma (HGG) decreased by 135 units, while recurrences decreased by 44. Fig. 2 shows the statistical analysis for first diagnoses and recurrence (p = 0.32; p = 0.61).
Table 2.
Types of neuro-oncological surgeries performed in the COVID and pre-COVID period.
| Surgery | Patients | % |
|---|---|---|
| Emergency neuro-oncological surgeries | 244 | 4% |
| Emergency neuro-oncological surgeries COVID period | 305 | 6% |
| Elective neuro-oncological surgeries | 5827 | 96% |
| Elective neuro-oncological surgeries COVID period | 5067 | 94% |
| Neuro-oncological pathology operated | 6071 | |
| Neuro-oncological pathology operated COVID period | 5372 |
Fig. 1.
a) shows the difference of means between the total number of elective neuro oncological surgeries in the COVID period and the total number of elective neurooncological surgeries in the pre-COVID period. b) shows the difference of means between the total number of urgent neurooncological surgeries in the COVID period and the total number of urgent neurooncological surgeries in the pre-COVID period. In neither case is statistical significance reached.
Table 3.
The table shows the comparison in absolute numbers of different pathologies investigated between the pre-COVID period and the COVID period. LGG: Low-grade glioma; HP: hypothalamic-pituitary lesion.
| Pathology | Number | % |
|---|---|---|
| HGG first diagnosis | 1550 | 26% |
| HGG first diagnosis COVID period | 1415 | 27% |
| HGG recurrence | 302 | 5% |
| HGG recurrence COVID period | 258 | 5% |
| LGG first diagnosis | 246 | 4% |
| LGG first diagnosis COVID period | 255 | 5% |
| LGG recurrence | 81 | 1% |
| LGG recurrence COVID period | 71 | 1% |
| Cranial meningiomas | 1447 | 24% |
| Cranial meningiomas COVID period | 1187 | 23% |
| Spinal meningiomas | 174 | 3% |
| Spinal meningiomas COVID period | 123 | 2% |
| Meningioma recurrence (cranial e spinal) | 118 | 2% |
| Meningioma recurrence (cranial e spinal) COVID period | 112 | 2% |
| Cranial metastasis | 607 | 10% |
| Cranial metastasis COVID period | 644 | 12% |
| Spinal metastasis | 288 | 5% |
| Spinal metastasis COVID period | 261 | 5% |
| HP lesions | 696 | 12% |
| HP lesions COVID period | 528 | 10% |
| HP recurrence | 72 | 1% |
| HP recurrence COVID period | 63 | 1% |
| CNS lymphoma | 136 | 2% |
| CNS lymphoma COVID period | 135 | 3% |
| Acoustic schwannoma | 218 | 4% |
| Acoustic schwannoma COVID period | 178 | 3% |
| Total pre-COVID | 5935 | |
| Total COVID period | 5230 |
Fig. 2.
a) shows the difference of means between the total number of first diagnosis gliomas operated during the COVID period and the pre-COVID period. b) shows the difference in means between the total number of glioma recurrences operated during the COVID period and the pre-COVID period.
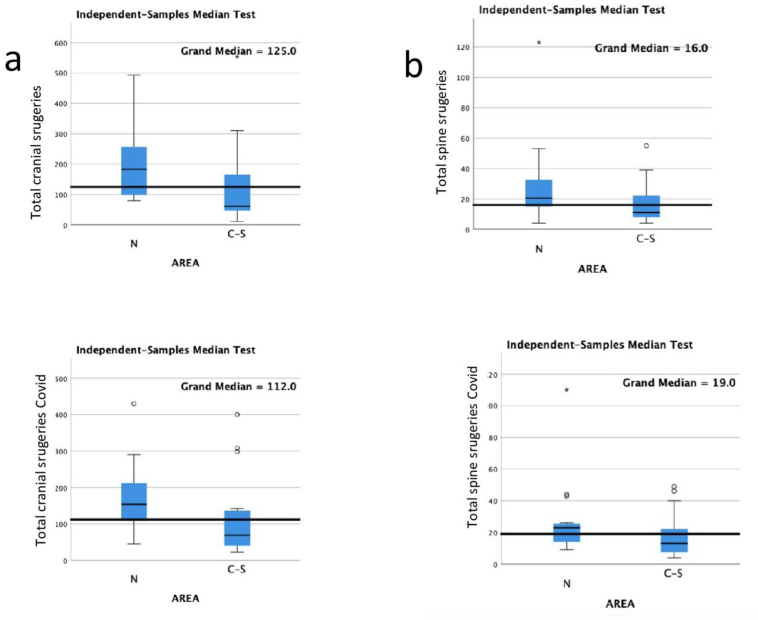
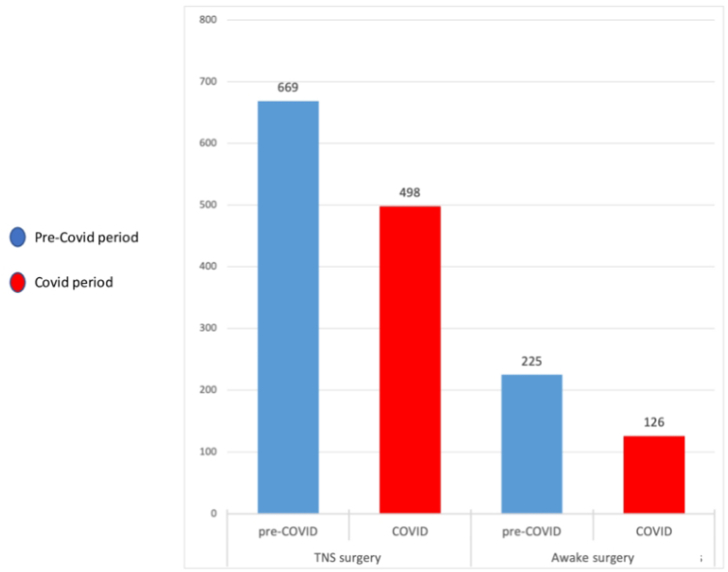
On the other hand, the diagnoses of low-grade glioma (LGG) were slightly increased by nine units (255 vs 246, p = 0.23). The number of ex novo diagnoses of cranial meningiomas in the COVID period appears to be significantly reduced compared to the pre-COVID period, with a decrease of 260 patients (1187 vs 1447, p = 0.11). In contrast, the number of meningioma recurrences remained substantially stable (112 vs 118, p = 0.51). Other pathologies that showed a significant decline in the COVID period were hypothalamic-pituitary tumors, with 168 fewer units (696 vs 528, p = 0.11) and acoustic schwannoma, with 40 fewer units (218 vs 178, p = 0.10). Instead, the number of CNS lymphomas between the two periods was substantially unchanged. Table 4 examines some specific surgical procedures, among which a significant decline can be noted for awake surgery and transsphenoidal surgery, with a decrease of 99 (225 vs 126, p = 0.17) and 171 units (669 vs 498, p = 0.12), respectively. Fig. 3 shows our analysis of cranial and spinal surgeries in the COVID and pre-COVID periods, finding no statistically significant differences in either comparison (p = 0.42; p = 0.95).
Table 4.
The table shows some types of surgeries in relation to their total number performed in the covid and pre-covid periodsCNS: Central Nervous System; ETT: Endoscopic Transnasal Transsphenoidal.
| Procedures | Patients | % |
|---|---|---|
| CNS biopsy | 380 | 6% |
| CNS biopsy COVID period | 354 | 7% |
| Awake surgery | 225 | 4% |
| Awake surgery COVID period | 126 | 2% |
| ETT surgery first diagnosis | 669 | 11% |
| ETT surgery first diagnosis COVID period | 498 | 9% |
| ETT surgery recurrence | 90 | 1% |
| ETT surgery recurrence COVID period | 70 | 1% |
| Total pre-COVID procedures | 6071 | |
| Total COVID procedures | 5372 |
Fig. 3.
a) shows the difference of means between the total number of cranial surgeries performed during the COVID period and the pre-COVID period. b) shows the same analysis on spinal surgeries.
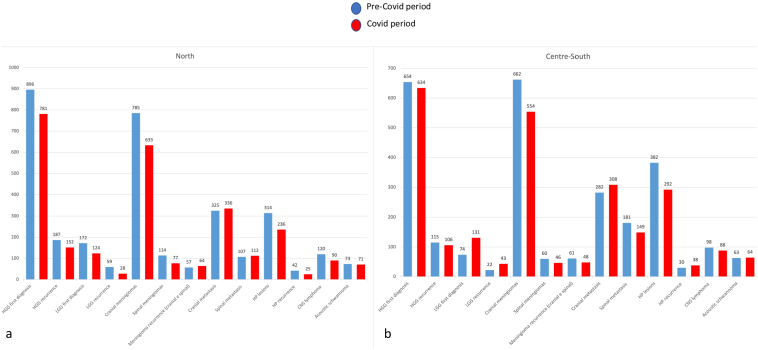
The analysis between the Northern group and the Central-Southern group essentially showed a more substantial number of interventions carried out in the North group, with the differences reduced in the number of emergency surgeries, both in the pre-COVID and in the COVID period, as shown in Fig. 4, Fig. 5. The reduction in medians during the COVID period also appears to be mirrored in the two groups, except for the total cranial surgeries, which appear to decrease more in the northern group. Fig. 6 explicitly shows the trend of the TNS and awake procedures during the two periods under comparison. The total number of positive patients operated in the COVID period was 36, of which 11 died. The postoperative death was found to be COVID-related only in 2 cases.
Fig. 4.
shows the trend of various neurooncological pathologies in Italy during the pre-COVID period (blue bar) and the COVID period (red bar).
Fig. 5.
a) and b) show the comparison between two histograms reporting the trend of different neurooncological pathologies during the pre-COVID period (blue bar) and the COVID period (red bar) in North e Central-South of Italy.
Fig. 6.
Number of TNS and awake surgery procedures during the pre-COVID (blue bar) and COVID period (red bar).
4. Discussion
From the beginning of the COVID-19 pandemic, several hospitals had to reorganize activities, managing the growing number of patients with respiratory disease, closing routine outpatient visits and postponing elective surgery.19,20 In some hospitals, surgeons also had to serve in COVID wards. This situation led to the definition of "collateral damage" due to COVID-19, with several patients no longer having access to the care they would typically need. This condition occurred in several medical fields.3,4,21 However, from a comprehensive analysis of the data collected from our web-shared survey, we can observe how the situation of the Italian neurosurgical reality was less complicated than it initially appeared. From the first days of the pandemic, the health system in various Italian regions organized a "hub & spoke" method,22, to manage and adequately move patients, guaranteeing the necessary assistance as much as possible. The great demand for anesthesiologists and intensive care operators due to the management of respiratory pathology led to the closure of most elective operating rooms. Despite this, the emergencies continued to be carried out regularly, and it is evident how the total number of emergencies during the COVID period increased compared to the previous year, although not reaching statistical significance. Our data show that in almost all centres, for nearly all neuro-oncological pathologies, there has been a reduction in the number of patients operated on, with rare exceptions. However, these reductions were not statistically significant in our analysis. To explain our results, we can assume that the COVID period in Italy is divisible into four phases: 1) first wave (from March 9 2020, to May 18 2020), when the pandemic hit the NHS hardest, leading to a national lockdown, 2) inter-pandemic period (from May 19 to October 7 2020) following the first wave, when the number of COVID-19 patients decreased, lockdown measures relaxed, elective surgeries and clinic services started again, 3) second wave (from October 8 to December 31 2021) when the number of COVID-19 patients again increased. During this period, our NHS was able to reserve 30–35% capacity of hospitals for COVID-19 patients and still keep ongoing elective surgeries and outpatient services,9, 4) post-pandemic period (from January 1 2021, to March 10 2021), where the pandemic has stabilized, until it subsides with the arrival of spring at the end of March 2021. Our NHS, during the interpandemic periods, has managed to redistribute the neuro-oncological patients who had not been treated during the pandemic's acute phases, allowing only a slight reduction in the number of interventions performed compared to the previous year.
Furthermore, the sub-analysis we conducted between the North and Central-South macro-regions showed a numerical difference in surgical interventions already present before the pandemic. This difference can be explained by the fact that several centres of the country's most populated regions (such as Lombardia, Piemonte and Veneto) participated in the proposed survey. It is interesting to note how the numbers dropped symmetrically in the north and the center-south during the COVID period. However, the northern regions, especially Lombardia, were hit the hardest in the early stages of the pandemic.
We observed how the most significant decrease occurred in benign and elective pathology, while for urgent pathology, there was a slight increase in cases (e,g. cranial meningiomas: 1447 in the pre-COVID period vs 1187 in the COVID period, with a drop of 260 units). In neither of the two comparisons, a statistically significant result was obtained. However, the analysis shows how the period of severe stress of the NHS led to a preference for acute disease over elective one and malignant disease over benign one.
A similar argument applies to CNS biopsies, which often require subsequent chemotherapy, perhaps not easily obtainable during the COVID period's maximum crisis. For this reason, they were postponed to moments of more accessible care for the patient.
Instead, a different situation was seen for cranial metastases, which appear to be slightly increased during the COVID period. This is perhaps because they often present in an acute symptomatic way, with seizures or intracerebral bleeding, leading the patient to the emergency room and treated as emergencies.
In addition, it is essential to note that the COVID-19 pandemic caused a significant decrease in surgical activity, especially during the first wave. This forced a subsequent reorganization with a rescheduled procedure, which implied a delay in other neurosurgical pathologies. This collateral damage of the COVID-19 pandemic is probably underestimated and difficult to be traced.
During the COVID-19 period, there was an essential decrease in TNS procedures and Awake surgery, as expected.
4.1. Awake surgery
In the COVID-19 pandemic year, a decrease of 2% was recorded for awake craniotomy. This data summarizes the effect of multiple reasons. There has been a growing debate about carrying out awake craniotomy surgeries during the COVID 19-pandemic, not only due to airway management but also to the close patients' proximity to the team in the operating theatre.
Awake surgery carries indeed a theoretically high risk of viral transmission, further worsened by the presence of many people in the operating theatre.
Awake craniotomy carries additional concerns, including the safety of the patient close to multiple staff members, the possibility of transmission of COVID-19 to staff where a pre-operative swab has been falsely negative, and the presence of additional staff/equipment in the theatre to perform necessary testing.
Furthermore, awake surgeries for relatively non-urgent pathologies (e.g. Low, grade gliomas) had been deferred as per SBNS/BNOS guidelines23,24
4.2. Endoscopic transnasal transsphenoidal (ETT)
In the COVID-19 pandemic year, a decrease of about 2% was recorded for ETT surgical procedures.
Scientific societies identified the transnasal skull base surgery, transoral and transfacial corridors, as the riskiest for the diffusion of COVID-1925,26 and recommended sparing the opening of paranasal cavities and mastoids during transcranial corridors. Different protocols were recommended to reduce the pooling of secretions by minimizing irrigation, utilizing an evacuation suction, and considering the placement of a throat pack.27 Some authors have also shown that electrocautery and ultrasonic devices, such as Sonopet (Stryker), led to aerosolizing viral particles. A suction evacuation was suggested if electrocautery is necessary for hemostasis.27 Given the high risk of spreading the virus with this type of surgery, many precautions have been used as scalpels affixed to long handles to avoid aerosolization associated with electrocautery and favour nonabsorbable packing, which is removed without endoscopy.27 Considering all the endorsed restrictions looks notable that the decrease was only 2%.
4.3. Study limitations
Our study was drawn from a web-based survey that did not consider the chronology of the different phases of the COVID period, so it is not possible to know precisely how the numbers varied between the first and second waves and the interpandemic periods. It is challenging to quantify the collateral damage of the COVID-19 pandemic as factors that are not easily quantifiable emerge, such as the patient's fear of going to the Emergency Department because of the contagion and a possible tendency to underestimate symptoms that in a standard period would have found a quicker outpatient response. More studies are needed in the coming years to clarify this issue. One of our study's main limitations is the lack of a shared national reorganization protocol, especially for the first wave. However, it is interesting to note that there are no significant differences between regions which were more affected than others in terms of numbers. Our data, based on an online survey, do not report the outcome of surgeries. Therefore, it is impossible to establish whether mortality from the neurosurgical disease increased during COVID.
Another potential limitation is the lack of participation of all the Italian neurosurgical centres. Although 35 responding centers represented almost 30% of the neurosurgical centers active in Italy, the remaining centers may have different perspectives and experiences that were not captured in the survey.
5. Conclusion
The Italian Neurosurgical Departments were reorganized during the COVID-19 pandemic, which allowed for the nationwide treatment of CNS tumors without compromising surgical efficacy and safety. The impact of the pandemic on Surgical Neuro-Oncology in Italy was serious, but the system was not overwhelmed. While there was a slight decrease in some departments, it was justified by the geographic redistribution of pathology management and the reduction of available resources. The decrease in the number of operated patients was not statistically significant, but further studies are needed to investigate whether it corresponds to an increase in mortality.
CRediT authorship contribution statement
Luca Zanin: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Tamara Ius: Conceptualization, Data curation, Formal analysis, Supervision, Validation, Writing – review & editing. Pier Paolo Panciani: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. Felice Esposito: Data curation, Formal analysis, Methodology, Software, Validation. Andrea Gori: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Validation. Marco Maria Fontanella: Supervision, Validation, Visualization. Maria Pia Tropeano: Data curation, Investigation, Methodology, Validation. Antonino Raco: Data curation, Supervision, Validation. Filippo Flavio Angileri: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. Giovanni Sabatino: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – review & editing. Alessandro Olivi: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Visualization. Vincenzo Esposito: Supervision, Validation, Writing – review & editing. Federico Pessina: Conceptualization, Data curation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. Edoardo Agosti: Data curation. Salvatore Aiello: Data curation. Denis Aiudi: Data curation. Danilo Aleo: Data curation. Roberto Altieri: Data curation. Rosina Amoroso: Data curation. Anna Maria Auricchio: Data curation. Giuseppe Barbagallo: Data curation. Andrea Barbanera: Data curation. Giacomo Beggio: Data curation. Andrea Bianco: Data curation. Riccardo Boccaletti: Data curation. Stefano Borsa: Data curation. Giuseppe Canova: Data curation. Paolo Cappabianca: Data curation. Manuela Caroli: Data curation. Michele Alessandro Cavallo: Data curation. Francesco Certo: Data curation. Marcella Chimenti: Data curation. Franco Chioffi: Data curation. Valentina Cioffi: Data curation. Fabio Cofano: Data curation. Christian Cossandi: Data curation. Giancarlo D’Andrea: Data curation. Raffaele De Falco: Data curation. Alessandro D'Elia: Data curation. Giuseppe Maria Della Pepa: Data curation. Alessandro Della Puppa: Data curation. Attilio Della Torre: Data curation. Paolo Ferroli: Data curation. Diego Garbossa: Data curation. Antonino Germanò: Data curation. Alessandra Giaquinta: Data curation. Franco Guida: Data curation. Maurizio Iacoangeli: Data curation. Domenico Gerardo Iacopino: Data curation. Angelo Lavano: Data curation. Giuseppe Maimone: Data curation. Vincenza Maiola: Data curation. Rosario Mauferi: Data curation. Alessandro Melatini: Data curation. Mario Moro: Data curation. Domenico Murrone: Data curation. Giovanni Muscas: Data curation. Piero Andrea Oppido: Data curation. Fabrizio Pignotti: Data curation. Domenico Policicchio: Data curation. Piermassimo Proto: Data curation. Paolo Quaglietta: Data curation. Antonino Raco: Data curation. Giulia Renisi: Data curation. Luca Ricciardi: Data curation. Francesco Romeo: Data curation. Marta Rossetto: Data curation. Alba Scerrati: Data curation. Andreas Schwarz: Data curation. Miran Skrap: Data curation. Carlo Somma: Data curation. Teresa Somma: Data curation. Giannantonio Spena: Data curation. Stefano Telera: Data curation. Luigino Tosatto: Data curation. Maria Pia Tropeano: Data curation. Francesco Volpin: Data curation. Lorenzo Volpin: Data curation. Cesare Zoia: Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Pier Paolo Panciani, Email: pierpaolo.panciani@unibs.it.
SINch NeuroOncology Study Group:
Edoardo Agosti, Salvatore Aiello, Denis Aiudi, Danilo Aleo, Roberto Altieri, Rosina Amoroso, Anna Maria Auricchio, Giuseppe Barbagallo, Andrea Barbanera, Giacomo Beggio, Andrea Bianco, Riccardo Boccaletti, Stefano Borsa, Giuseppe Canova, Paolo Cappabianca, Manuela Caroli, Michele Alessandro Cavallo, Francesco Certo, Marcella Chimenti, Franco Chioffi, Valentina Cioffi, Fabio Cofano, Christian Cossandi, Giancarlo D’Andrea, Raffaele De Falco, Alessandro D'Elia, Giuseppe Maria Della Pepa, Alessandro Della Puppa, Attilio Della Torre, Paolo Ferroli, Diego Garbossa, Antonino Germanò, Alessandra Giaquinta, Franco Guida, Maurizio Iacoangeli, Domenico Gerardo Iacopino, Angelo Lavano, Giuseppe Maimone, Vincenza Maiola, Rosario Mauferi, Alessandro Melatini, Mario Moro, Domenico Murrone, Giovanni Muscas, Piero Andrea Oppido, Fabrizio Pignotti, Domenico Policicchio, Piermassimo Proto, Paolo Quaglietta, Antonino Raco, Giulia Renisi, Luca Ricciardi, Francesco Romeo, Marta Rossetto, Alba Scerrati, Andreas Schwarz, Miran Skrap, Carlo Somma, Teresa Somma, Giannantonio Spena, Stefano Telera, Luigino Tosatto, Maria Pia Tropeano, Francesco Volpin, Lorenzo Volpin, and Cesare Zoia
References
- 1.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in lombardy, Italy: early experience and forecast during an emergency response. JAMA, J Am Med Assoc. 2020;323(16):1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 2.Grasselli G., Zangrillo A., Zanella A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region. Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masroor S. Collateral damage of COVID-19 pandemic: Delayed medical care. J Card Surg. 2020;35(6):1345–1347. doi: 10.1111/jocs.14638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahmed T., Lodhi S.H., Kapadia S., Shah G.V. Community and healthcare system-related factors feeding the phenomenon of evading medical attention for time-dependent emergencies during COVID-19 crisis. BMJ Case Rep. 2020;13(8) doi: 10.1136/bcr-2020-237817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perin A., Servadei F., DiMeco F. ‘Hub and Spoke’ Lombardy Neurosurgery Group. May we deliver neuro-oncology in difficult times (e.g. COVID-19)? J Neuro Oncol. 2020;148(1):203–205. doi: 10.1007/s11060-020-03496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gazzetta Ufficiale. Accessed March 12, 2022. https://www.gazzettaufficiale.it/eli/id/2020/03/08/20A01522/sg.
- 7.Rapporto sulla ripartenza degli screening - maggio 2020 | Osservatorio Nazionale Screening. Accessed April 3, 2022. https://www.osservatorionazionalescreening.it/content/rapporto-ripartenza-screening-maggio-2020.
- 8.Angileri F.F., Sabatino G., Cavallo L.M., et al. Natura non facit saltus: a phase 2 proposal to manage brain tumors cases from the Neuro-oncology section of the Italian Society of Neurosurgery (SINch®) J Neurosurg Sci. 2021;65(1):1–7. doi: 10.23736/S0390-5616.20.05054-7. [DOI] [PubMed] [Google Scholar]
- 9.Portale covid-19. Accessed April 3, 2022. https://www.agenas.gov.it/covid19/web/index.php?r=site%2Fheatmap.
- 10.Doglietto F., Vezzoli M., Gheza F., et al. Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID-19) in Italy. JAMA Surgery. 2020;155(8):691–702. doi: 10.1001/jamasurg.2020.2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zoia C., Bongetta D., Veiceschi P., et al. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir. 2020;162(6):1221–1222. doi: 10.1007/s00701-020-04305-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alimohammadi E., Eden S.V., Anand S.K., Ahadi P., Bostani A., Bagheri S.R. The impact of coronavirus 2019 (COVID-19) on neurosurgical practice and training: a review article. Br J Neurosurg. 2022;36(5):569–573. doi: 10.1080/02688697.2021.1888874. [DOI] [PubMed] [Google Scholar]
- 13.Nabil M., Dorrah M., Sharfeldin A., Abaza H. Impact of COVID-19 pandemic on the neurosurgical practice in Egypt. Egypt J Neurosurg. 2022;37(1):23. doi: 10.1186/s41984-022-00164-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahmud M.R., Cheserem B., Esene I.N., et al. The impact of COVID-19 on neurosurgical services in africa. World Neurosurg. 2021;146:e747–e754. doi: 10.1016/j.wneu.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lester A., Leach P., Zaben M. The impact of the COVID-19 pandemic on traumatic brain injury management: lessons learned over the first year. World Neurosurg. 2021;156:28–32. doi: 10.1016/j.wneu.2021.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh R., Sahu A., Singh K., Prasad R.S., Pandey N., Singh R.C. Impact of COVID-19 pandemic on neurosurgical practice in a tertiary care center in India. J Neurosci Rural Pract. 2021;12(1):24–32. doi: 10.1055/s-0040-1716455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raneri F., Rustemi O., Zambon G., et al. Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurg Focus. 2020;49(6):E9. doi: 10.3171/2020.9.FOCUS20691. [DOI] [PubMed] [Google Scholar]
- 18.Studio Multicentrico Sezione di Neuro-Oncologia L’IMPATTO DELLA PANDEMIA SUL TRATTAMENTO CHIRURGICO DEI PAZIENTI AFFETTI DA PATOLOGIA ONCOLOGICA. Accessed March 13, 2022. https://a2i0g8.mailupclient.com/f/rnl.aspx/?fek=ww3:0ln=t3-e.=ww1x6f0.d=&2mc7&x=pv&92gh.f9&x=pp&r3jig76me773af5.&d=twwNCLM.
- 19.Kaye K., Paprottka F., Escudero R., et al. Elective, non-urgent procedures and aesthetic surgery in the wake of SARS-COVID-19: considerations regarding safety, feasibility and impact on clinical management. Aesthetic Plast Surg. 2020;44(3):1014–1042. doi: 10.1007/s00266-020-01752-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goyal N., Venkataram T., Singh V., Chaturvedi J. Collateral damage caused by COVID-19: change in volume and spectrum of neurosurgery patients. J Clin Neurosci. 2020;80:156–161. doi: 10.1016/j.jocn.2020.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abdelaziz H.K., Abdelrahman A., Nabi A., et al. Impact of COVID-19 pandemic on patients with ST-segment elevation myocardial infarction: insights from a British cardiac center. Am Heart J. 2020;226:45–48. doi: 10.1016/j.ahj.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giunta L. DELIBERAZIONE N° XI/2906. :28.
- 23.Adult-neuro-oncology-service-provision-during-COVID-outbreak_SBNS-BNOS.pdf. Accessed April 18, 2022. https://bnos.org.uk/wp-content/uploads/2020/03/Adult-neuro-oncology-service-provision-during-COVID-outbreak_SBNS-BNOS.pdf.
- 24.Zacharia B.E., Eichberg D.G., Ivan M.E., et al. Letter: surgical management of brain tumor patients in the COVID-19 era. Neurosurgery. 2020;87(2):E197–E200. doi: 10.1093/neuros/nyaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chaves A.L.F., Castro A.F., Marta G.N., et al. Emergency changes in international guidelines on treatment for head and neck cancer patients during the COVID-19 pandemic. Oral Oncol. 2020;107 doi: 10.1016/j.oraloncology.2020.104734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel Z.M., Fernandez-Miranda J., Hwang P.H., et al. Letter: precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery. 2020;87(1):E66–E67. doi: 10.1093/neuros/nyaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spock T., Kessler R., Lerner D., et al. Endoscopic skull base surgery protocol from the frontlines: transnasal surgery during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020;163(3):482–490. doi: 10.1177/0194599820931836. [DOI] [PubMed] [Google Scholar]