Abstract
Background
There are meaningful gaps in equitable access to Primary Health Care (PHC), especially for vulnerable populations after widespread reforms in Western countries. The Innovative Models Promoting Access-to-Care Transformation (IMPACT) research program is a Canadian-Australian collaboration that aims to improve access to PHC for vulnerable populations. Relationships were developed with stakeholders in six regions across Canada and Australia where access-related needs could be identified. The most promising interventions would be implemented and tested to address the needs identified. This realist review was conducted to understand how community coalition and outreach (e.g., mobile or pop-up) services improve access for underserved vulnerable residents.
Objective
To inform the development and delivery of an innovative intervention to increase access to PHC for vulnerable populations.
Methods
A realist review was conducted in collaboration with the Local Innovative Partnership (LIP) research team and the IMPACT research members who conducted the review. We performed an initial comprehensive systematic search using MEDLINE, EMBASE, PsycINFO, and the Cochrane Library up to October 19, 2015, and updated it on August 8, 2020. Studies were included if they focused on interventions to improve access to PHC using community coalition, outreach services or mobile delivery methods. We included Randomized Controlled Trials (RCTs), and systematic reviews. Studies were screened by two independent reviewers and the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework was used for data extraction and framework analysis to obtain themes. The LIP research team was also allowed to suggest additional papers not included at screening.
Results
We included 43 records, comprising 31 RCTs, 11 systematic reviews, and 1 case control study that was added by the LIP research team. We identified three main themes of PHC interventions to promote access for vulnerable residents, including: 1) tailoring of materials and services decreases barriers to primary health care, 2) services offered where vulnerable populations gather increases the “reach” of the interventions, 3) partnerships and collaborations lead to positive health outcomes. In addition, implementation designs and reporting elements should be considered.
Conclusion
Realist reviews can help guide the development of locally adapted primary health care interventions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-023-01105-3.
Keywords: Realist Review, Vulnerable, Coalition, Mobile service, RE-AIM, Primary Health Care
Background
Health Canada defines primary health care as “an approach to health and a spectrum of services beyond the traditional health care system. It includes all services that play a part in health, such as income, housing, education, and environment” [1]. Recent and widespread reforms in Primary Health Care (PHC) in western countries reflect efforts to address the need for PHC to be more inclusive and equitable [2]. Despite these efforts, meaningful gaps in equitable access to PHC remain, especially for vulnerable populations defined as people who are unable to achieve the full potential of their lives because of social and political contextual factors [3, 4]. Poor access to PHC causes unmet healthcare needs and increases healthcare services use [3, 4].
One of the efforts made by Canada and Australia to close the equity-gap in PHC access, was to initiate a joint 5-year research program, IMPACT (Innovative Models Promoting Access-to-Care Transformation) [4]. This program was designed to increase access to PHC for vulnerable populations in three Canadian (Alberta, Ontario, Quebec) and three Australian (Victoria, New South Wales, South Australia) regions and involved stakeholders from Local Innovation Partnerships (LIP)s in the six regions. The LIPs were set up in communities where access-related needs could be identified and addressed by implementing, and testing the most promising interventions to improve PHC access for vulnerable populations [4–6].
Community-based programs have promoted community health and equity [7]. For example, community coalitions and mobile interventions have been effective in improving access to PHC for vulnerable populations [7–9] but there is evidence of poor access to PHC in some Canadian regions [5, 10]. For example, although services such as senior centres, settlement agencies (immigrant services), physician clinics, nursing, pharmacies, social work, youth-serving organizations, family services, schools, and services working with urban Aboriginal populations were available, there were high levels of social and material deprivation among vulnerable Indigenous and immigrant residents in North Lethbridge, Alberta. The IMPACT local innovation partnership (LIP) research team in Alberta, Canada, planned to implement and scale-up a community coalition and outreach health services intervention (i.e., mobile, or pop-up services) to improve access for vulnerable populations.
To inform the design of a local outreach service, we decided to conduct a realist review to understand existing global evidence on how community coalitions and outreach services work in particular contexts to improve access to PHC for vulnerable populations.
Research questions
The research question was articulated through an iterative dialogue and discussion between the LIP research team and the IMPACT review team, and is as follows: “How does establishing an outreach services program such as pop-up or mobile service interventions among community and PHC service providers lead to improved access to PHC among vulnerable populations?”.
Secondary questions were as follows:
Q2: How are community organizations working together to enhance outreach services?
Q3: What is the optimal way to implement/provide PHC using outreach services?
Q4: What forms of outreach services are the most approachable and engaging?
Q5: How are community engagement and/or participation best initiated/encouraged?
Methods
We used a realist lens approach and based our synthesis methods on two realist reviews [11, 12]. This review was conducted iteratively with the LIP research team. We chose this approach because it was essential to understand the underlying theory to design the planned intervention, by understanding the relationship between the outcomes and the underlying contexts and mechanisms of action of the interventions.
We developed a logic model (Fig. 1) in collaboration with the LIP research team, following the Levesque model of access to health care [10] and the W.K. Kellogg Foundation Logic Model Development Guide [13]. This logic model revealed the underlying program theory and assumptions about mechanisms, context, and outcomes. We used this logic model to develop the search strategy.
Fig. 1.
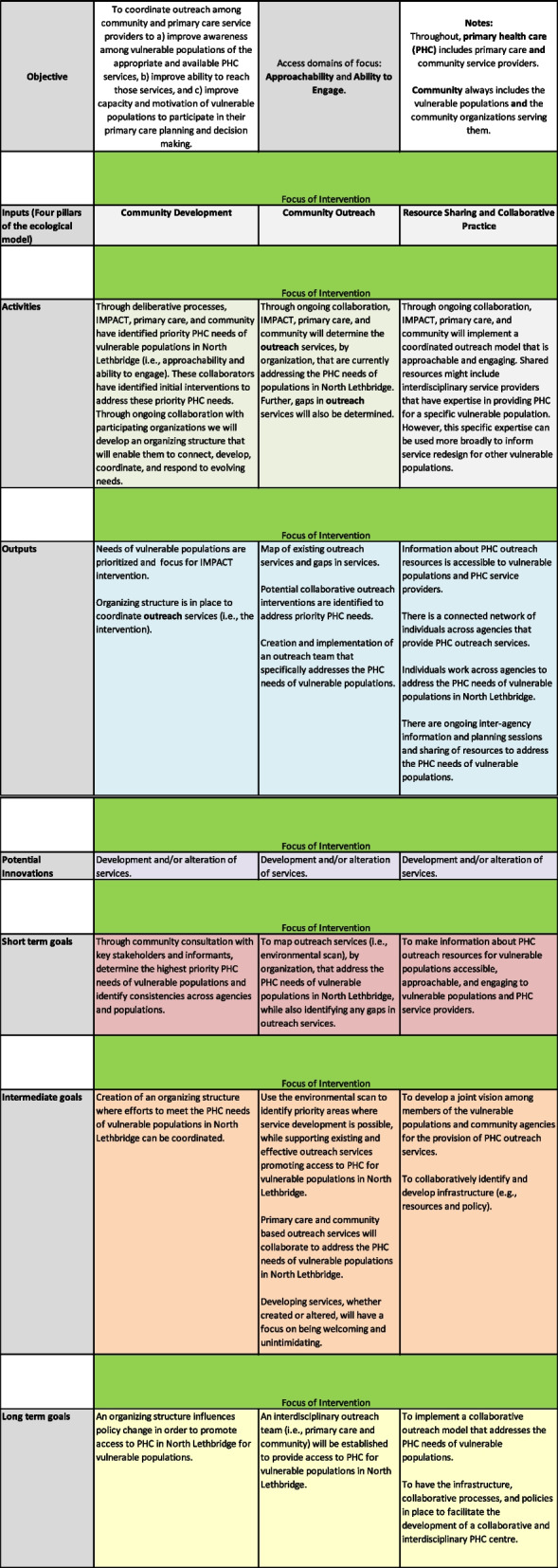
Logic model
Search strategy
The search strategy was developed and tested by an experienced medical information specialist (BS) in consultation with the IMPACT review team and the LIP research team. Using the OVID platform, we searched Ovid MEDLINE®, Ovid MEDLINE® In-Process & Other Non-Indexed Citations, EMBASE, and PsycINFO. We also searched the Cochrane Library on Wiley. Initial searches were performed on October 19th, 2015, and updated on August 8, 2020. Strategies utilized a combination of controlled vocabulary (e.g., “Mobile Health Units”, “Community Networks”, “Vulnerable Populations”) and keywords (e.g., mobile clinics, community partnerships, and at-risk people). See Additional file 1 for the full search strategies used. Vocabulary and syntax were adjusted across databases. Results were limited to the publication years 2005 to August 8, 2020. Filters for RCTs and reviews were applied.
Study inclusion and exclusion criteria
Studies were eligible if they centred on PHC in combination with at least one community health or social organization or their services. Studies were included if they featured one or a combination of the following elements to target vulnerable populations: mobile service, coalition, outreach, colocation, community development, shared care, pop-up services, resource-sharing, and cooperation. We included RCTs and systematic reviews published in either English or French and set in high-income countries. We excluded duplicates, protocols, dissertations, conference abstracts, qualitative and observational studies, literature reviews, cost-effectiveness analyses or economic evaluations, as well as protocols of studies and reviews. Further, the LIP research team advised the exclusion of studies that did not include some aspect of service provision. The LIP research team was also invited to include up to 5 contextual articles that may not necessarily fit the inclusion criteria.
Study selection, screening, and abstraction
All retrieved citations from the searches were exported to Covidence. Two independent reviewers (CG, MT, NA, AW, or EG) screened titles and abstracts for eligibility. The full texts of potentially eligible articles were retrieved and screened independently by two reviewers. Disagreements were resolved through discussions. RM and SS from the LIP research team ascertained all included studies for relevance.
A data extraction form based on the RE-AIM framework’s five dimensions (reach, efficacy, adoption, implementation, and maintenance), as well as realist contextual elements, was devised centrally and adapted to the local context in consultation with the LIP research team. The template subsequently incorporated several frameworks: the RE-AIM framework [14–16], the PROGRESS-plus framework [17], and the Template for Intervention Description and Replication (TIDieR) checklist [18]. A complete extraction using this template was done by CG, MT, NA, and AW, and a second extraction focusing on the RE-AIM abstractions was conducted by CG, MT, RM, NA, AW, and SS. When a particular program or intervention was featured in more than one paper (i.e., methodological paper and an outcomes paper), only one paper was chosen as the main publication. Additional data was abstracted from the companion papers.
Data synthesis
Data synthesis was conducted by CG, NA, AW, in conjunction with RM and SS from the LIP research team. The presence of LIP members ensured that context and local relevancy were considered.
We worked with the LIP research team to identify themes that were relevant to their planned intervention and particular context. After the data was organized and coded according to the RE-AIM framework [14–16], CG, RM, NA, AW, and SS identified patterns in process factors that enhanced or impeded the intervention (Additional file 2 Table 1), as well as patterns in information regarding the theories and mechanisms underpinning the interventions (Additional file 2 Table 2). Outliers were also noted. Finally, the review team discussed and agreed to a set of emerging themes that were then mapped, interpreted, and presented back to the LIP research team for further review and feedback. This process resulted in three themes that are presented below.
Results
We identified 4469 records (2333 through the first search strategy with 10 included) and a total of 42 studies were included in the framework analyses. The LIP research team added one study of their choosing, which was originally excluded due to its study design (case–control), bringing the number of included studies to 43. There were also 20 companion studies, that were considered alongside the main publications. Of the 102 full-text articles assessed for eligibility, 59 were excluded – 20 were companion publications to already included studies, two were duplicates, three did not feature any results, six did not meet intervention eligibility criteria, 15 were of a study design other than review or RCT, one was an RCT protocol, five were conference abstracts and four featured ineligible populations or settings. Three studies were excluded by the LIP team for relevancy. See Fig. 2 for the PRISMA flow chart.
Fig. 2.
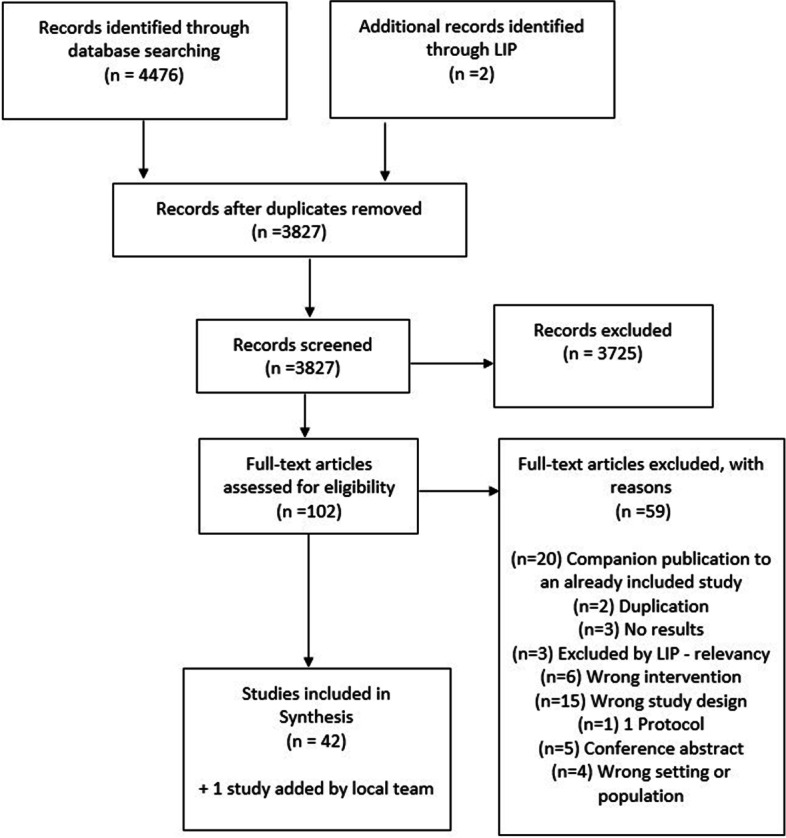
PRISMA flow diagram
Description of studies
The characteristics of the 43 included studies are described in Table 1. Additional information can be found in Tables 1 and 2 in Additional file 2, where we present the factors that enhance or impede the intervention, as well as the effects of contextual factors on the intervention. Eleven studies were reviews, 31 were trials, and one study added by the local team was a case–control study. The settings for interventions were predominantly in the community (schools, neighborhoods, homeless shelters, community clinics, mobile health clinics, PHC centres, and churches). Most of the RCTs were conducted in the United States (25 studies). Factors considered to increase vulnerability included racial, ethnic, or minority status (18 studies), low socio-economic status (8 studies), adolescents at risk for drug or alcohol abuse (2 studies), mental health issues (12 studies), elderly population (3 studies), children (5 studies) and being houseless (3 studies). Service providers featured in the studies were from a variety of backgrounds. Coalitions included various members of health and social services, as well as academia, public health, and general community members. The studies reported a range of patient-level, community-level, and service-level outcomes, including health status (22 studies), behavior change (9 studies), various psychosocial outcomes (8 studies), service usage (8 studies), various risk factors (2 studies), quality of life (1 study), community outcomes (1 study), partnership model (1 study), model of care (1 study), and clinic outcomes (1 study).
Table 1.
Study characteristics
| Study characteristics | Number of included studies | |
|---|---|---|
| Quantitative research methods | Randomized controlled trial (RCT) | 31 |
| Systematic Reviews & Meta-analysis | 11 | |
| Case–control | 1 | |
| Sample Size | RCTs | |
| Range | 4407 | |
| Median | 330 | |
| Interquartile range (IQR) | 644 | |
| Reviewsb | ||
| Range | 126 | |
| Median | 18 | |
| Interquartile range (IQR) | 48 | |
| Types of Interventiona | Mobile services | 7 |
| Coalition | 24 | |
| Outreach | 14 | |
| Duration of intervention | 1–6 months | 8 |
| 7–12 months | 10 | |
| > 1 year | 6 | |
| Variedc | 10 | |
| No information | 9 | |
| Types of providers | Community health workers (CHWs) | 5 |
| Nurses | 2 | |
| Doctors/Pharmacists | 4 | |
| Academic staff and community providers | 11 | |
| Collaboration between CHWs, nurses, doctors, community members, social worker | 18 | |
| Peer support / volunteer | 3 | |
| Most common types of outcomes | Health status | 21 |
| Behavior change | 8 | |
| Psychosocial | 8 | |
| Access to care | 4 | |
| Knowledge translation activities | 2 | |
| Countries of intervention | USA | 25 |
| United Kingdom | 4 | |
| Spain | 2 | |
| Canada | 1 | |
| Multiple countriesd | 9 | |
| No information | 2 | |
aSome reviews assessed multiple interventions
bThe sample size of reviews is based on the number of included studies
cIntervention duration varied for systematic reviews
dSome reviews included studies conducted in multiple countries
Realist analysis and synthesis
Data collection and synthesis were conducted based on the RE-AIM framework. Therefore, the relationship between the outcomes and underlying mechanisms of the included interventions were analysed within the context of the core principles of Reach, Effectiveness, Adoption, Implementation, and Maintenance. We developed themes to explain how the interventions may have improved access to PHC. The included studies in this review demonstrated an overarching emphasis on tailored outreach processes, as well as community-driven intervention designs to elicit higher levels of engagement in and efficacy of the interventions.
Themes
The three themes identified explain the mechanisms by which awareness and access to PHC services could be improved for vulnerable populations.
Tailoring materials and services decreases barriers to PHC for vulnerable populations
Although interventions tended to be complex and included many different components, authors generally endorsed that materials and services should be adapted and tailored to the local context [8, 19–31].
For instance, Hawkins et al. implemented the first community-randomized trial of the Communities that Care (CTC) program [19]. The CTC program is noted as an empowering prevention initiative that incorporates community leaders and a prevention coalition, to discern notable risk and protective factors within the community. A set of interventions designed to reduce the identified elevated risk factors and concurrently encourage the protective factors were then implemented. The authors followed a panel of 4407 students from the fifth grade to the seventh grade in selected communities in seven American states (Colorado, Illinois, Kansas, Maine, Oregon, Utah, and Washington) to explore the outcomes of a CTC program on the reduction of established risk factors, delinquent behaviour, and substance abuse. Community leaders received appropriate training and subsequently identified or established a coalition to administer the CTC process.
There were significantly lower levels of risk factors among students within CTC communities, relative to non-CTC controls 1.67 years after the implementation of the preventative interventions selected through the CTC program. Results further indicated that members of the control group displayed a significantly higher probability of engaging in delinquent behaviour during the study.
This study highlighted the promising effects of community-based partnerships and coalitions on intervention effectiveness and maintenance. The intervention demonstrated potential in the reduction of high-level risk factors within vulnerable groups by adapting the program to the local context.
Chung et al. conducted a study to assess the effects of using depression collaborative care with community engagement and planning (CEP) in minority populations [21]. Implementing the intervention involved tailoring the resources, including the provided depression toolkits to fit the needs of the participating communities. CEP councils, in fact, held bi-weekly meetings for a total of 5 months in order to develop a distinct written training and service delivery plan for each community, using a community engagement model.
Outcomes for this study were based on self-reported surveys conducted at baseline, 6 months and 12 months. Overall, implementing CEP significantly reduced the likelihood of poor-mental health-related quality of life, relative to using traditional resources for service. This study demonstrated the potential of using CEP in depression collaborative care—particularly in underserved communities—considering the limited risks associated with such a model, as well as the positive outcomes pertaining to quality of life.
Other studies, such as O’ Mara Eves et al., and Menon et al., highlight the importance of tailoring key components of interventions to the target demographics [23, 26]. For instance, O’Mara Eves et al., carried out an extensive investigation to evaluate the effectiveness of public health interventions that involve community engagement to address a multitude of health issues [23]. The authors identified that several interventions used media that was personalized to the specific needs of the participants, including newsletters and information sheets. Although there was insufficient evidence to point to one model of community engagement being favourable over the other, it was shown that the interventions had positive impacts on health behaviour outcomes.
Moreover, Menon et al. studied the effectiveness of using a community-to-clinic navigation intervention to enhance colorectal cancer screening among multicultural and underinsured individuals [26]. Participating community sites were randomized to receive group education and reminder calls, or group education and tailored navigation that fit individual concerns and behaviours. Navigators within this study were trained to deduce what may be holding participants back from completing a screening and subsequently provide a tailored message.
Menon et al. found that implementing tailored navigation intervention was associated with an increased rate of cancer screening, with the intervention group being four times more likely to complete screening relative to the control group.
Ultimately, included studies, such as Hawkins et al., Chung et al., O’Mara Eves et al., and Menon et al., highlighted the potential benefits of implementing resources and services to meet individual and/or community-specific needs.
Services offered where vulnerable populations gather increases the “reach” of the interventions
Location of services often posed barriers to accessing PHC for vulnerable populations. Two primary methods of countering these barriers are seen in the (30/43) studies included in this review: 1) Services provided in places frequented by the target population [8, 19–22, 24, 27, 30, 32–34], and 2) outreach/mobile clinics that visit where the target population is situated [9, 20, 34–37]. Areas of service provision varied across studies and included schools, social care systems, neighbourhoods, recreational parks, and community organizations. Even when services were offered in locations frequented by the target population, there were sometimes barriers to accessing services. Additional strategies were employed to ensure that the participants reached the services, such as free transportation for those who required it [20, 22, 24], utilising lay health outreach workers to provide the extra nudge to convince and help the vulnerable person seek service [8, 20, 23, 24, 28, 38] or volunteers in each neighbourhood to support the participation of the residents and help them access services [19, 22, 25, 37, 39, 40]. Services were offered at no charge, were covered by insurance or offered at nominal charge [9, 35].
Stagg et al. investigated the efficacy of a peer support intervention in encouraging participation and engagement among marginalized populations, with services targeting chronic Hepatitis C [34]. Participants were identified through outreach services for point-of-care testing for clients with problematic drug use and experiencing houselessness. They were matched with peer advocates who had personally experienced chronic Hepatitis C, allowing them to effectively support others encountering similar challenges. Through peer support, the absolute likelihood of successfully engaging with designated healthcare systems increased by 18.1%, illustrating the positive impact of services through outreach on intervention efficacy.
The MOMmobile was defined as a medical van that provides a range of pre and post pregnancy care at four scheduled locations in urban and rural areas of the Miami-Dade County, South-East Florida, USA [35]. This program resulted in users being significantly more likely to access prenatal care in the first trimester and obtain adequate prenatal care. Services included a wide range of medical and social services, health education, and additional community referral as needed. The MOMmobile services were free for qualified patients, and Medicaid and insurance were accepted for those who were covered.
Partnerships and collaborations lead to positive health outcomes for vulnerable populations
Many of the included articles (24/43) had some form of coalition as part of the intervention and their findings were conflicting. Some reviews and RCTs showed that interventions featuring aspects of collaboration, partnership, or community engagement were generally associated with positive outcomes [8, 9, 19–23, 26–28, 32, 34, 41–49], while others showed no difference between interventions and control [25, 50, 51].
Diverse types of partnerships and collaborations included academic-community coalitions, public health – public agency coalitions, and coalitions based on community agency partnerships. The lead sector was most often a university followed by health agency/healthcare provider, not-for-profit community-based organization, community members, and government human service or social welfare agencies. In one systematic review with 58 included studies [8], core group/shared leadership was reported as the predominant coalition leadership type (13/58), followed by steering committee leadership (12/58), single person co-ordinator (3/58), and principal investigator (2/58). Another review [9] reported that the lead academic partner was more often a nursing school than a medical school.
A recurring theme was that coalitions and partnerships required long-term commitment from their members. In Hawkins et al., community leaders were trained for 6–12 months before the implementation of the program, with results that took between 2 to 10 years to be observed [19]. In Redmond et al. article, the delivery of the intervention lasted over four years [32]. In Anderson et al., the average duration of interventions across various types of interventions implemented by coalitions ranged from 20 to 50 months [8].
In the article by Chung some positive outcomes observed at 6 months were not sustained at 12 months, potentially explained by reduced intervention support offered after the first 6 months of implementation [21]. According to Redmond et al., ongoing technical assistance provided by the partnership can result in long-term, high-quality implementation of interventions in the community, which in turn leads to community-level effects [32].
Implementation design and reporting elements to consider for improving the quality of evidence
Several included studies postulated methods to improve design and reporting of these community-based PHC interventions.
Complex versus simple interventions
Most of the interventions tended to be complex in terms of processes, intervention components, as well as partnerships. One systematic review [20] reported that because of the complexity of the interventions, it was unclear which components contributed to the effect of the interventions. The authors proposed that a combination of multiple strategies was more likely to be successful.
Theory
All except two of the included studies and reviews [20, 35] disclosed the use of theory for at least some components of the intervention. Various theories were applied in the included studies. The predominant ones included social-ecologic theory, community coalition action theory, community engagement and collaborative care model. Health belief model and social cognitive theory were also seen recurringly. However, theory was generally not discussed at length when presenting and interpreting findings.
Adverse outcomes, resource use and costs
In the 43 articles included in this review, adverse outcomes and costs were generally not reported, and when mentioned, were not described in detail. The lack of reporting on adverse outcomes, resource use and costs was also found in one included systematic review [8].
Rigorous evaluation
According to Anderson et al., there is a dearth of "rigorous systematic reviews on effectiveness of community coalition models in reducing racial and ethnic disparities in health and well-being.” Evidence is lacking on coalition structures, critical processes, benefits, costs, adverse effects, as well as community contextual factors [8].
Feedback from local PHC team
The preliminary results of the present review were presented to the LIP research team, as well as to other stakeholders in the design and implementation of the intervention. Feedback was positive, and the themes were all deemed relevant and helpful for improving access to PHC for the vulnerable population in a rural/remote setting in North Lethbridge.
The local team is aiming to achieve themes 1 and 2 by aligning with existing well-attended programs in the community and tailoring the services offered at each pop-up to the local setting, while maintaining a core set of services offered at every pop-up event. For example, when a pop-up service is offered at a seniors’ center, there are regular “core” services offered, such as physician consults, foot care, healthy living programming, dental services, community recreation services, financial planning and supports, and mental health counselling. Tailored services like seniors’ subsidies and benefits counseling, geriatric mental health outreach services, and home care supports are also offered. Tailoring the services, as well as offering the services where the people gather, ensures that services are acceptable and approachable.
Theme 3, “Partnerships and collaborations lead to positive health outcomes for vulnerable populations” is also very relevant and is helpful in guiding the partnerships formed for this project. Unfortunately, within the included studies, we found scant information on the evaluation of partnerships.
Implementation design and reporting elements provided information to keep in mind for successful development and reporting of the intervention. Another important element that was lacking in the literature was whether vulnerable individuals were better connected to family physicians and PHC providers after participating in mobile or pop-up services.
Discussion
We found that tailoring materials and services, offering the services in regions where vulnerable populations gather, as well as establishing partnerships that include community members and academic partners all contribute to increased access to PHC for vulnerable populations. We also found that studies with multiple strategies led to better outcomes. These strategies should be considered when designing an intervention to improve access for vulnerable populations.
Most interventions were designed based on established theories and the most common was the socio-ecologic theory. The studies do not describe the mechanisms to achieve outcomes, for example, specifics regarding the forms of outreach and optimal ways to provide services.
Nevertheless, the results of this commissioned review were used to design and implement an intervention in North Lethbridge, Alberta. The program evaluation will be published at a later date [6]. This should provide the reader with further information on the utility of a commissioned rapid review in designing and implementing an intervention to increase access to PHC for vulnerable populations.
Strengths
We followed double, independent selection and extraction processes for all steps of the review to minimize bias in selection of studies. We had a strong partnership with the LIP research team, which informed the logic model and research question as well as interpretation of results.
Limitations
We modelled our methods based on two previously published rapid realist reviews [11, 12]. In order to limit the scope of the review, we decided to include only systematic reviews and randomized controlled trials. Other types of study designs were included in two different cases: 1) on the recommendation of the LIP research team, and/or 2) if the study was related to a previously accepted randomized controlled trial (companion study). Further expanding the scope to include other study designs, such as qualitative studies, as well as grey literature might identify additional processes to consider and enrich the examples provided here. However, since we included 11 systematic reviews with a total of 348 primary studies, we do have a rich data source for relevant studies.
Another important limitation is the paucity of information available on both mobile clinics and interventions in local settings that offer PHC services tailored to community needs in high-income countries. There is evidence available mainly on low to middle-income countries. Also, we did not search grey literature and websites, thus we may have missed studies and reviews, particularly those led by community partners who may be less likely to publish and those that did not demonstrate effectiveness.
Generalizability to our local setting and other settings
The results of this realist review have been useful in the efforts to implement a “pop-up” health and social services event in North Lethbridge. Early results demonstrate that this is a promising community-based approach for those who experience barriers to accessing traditional PHC services in North Lethbridge.
There is a need for robust evaluation of mobile and outreach interventions, as well as community coalition service delivery models that focus on health and social services [52]. Luque et al. noted the lack of systematic and rigorous evaluation of mobile clinics, even when mobile clinics obviously lower access barriers [9]. They also cited a lack of generalizability of included studies due to methodological issues. They argued that mobile clinic evaluation reports should include longitudinal data on patient outcomes [9]. There is also a dearth of systematic reviews on effectiveness of community coalitions, as well as insufficient evidence regarding the comparative efficacy of various models of community engagement [8, 23]. In fact, the underlying mechanisms of how these collaborations have a positive effect on outcomes are unclear, with studies generally reporting few details on the structures and processes of these coalitions [8]. One possibility is that coalition-based interventions, particularly when an academic group is involved, are more likely to be evidence-based. Redmond et al. explained that the control group was less likely to use evidence-based interventions, even if they were free to choose from any prevention interventions available [32]. Luque et al. suggested that the addition of partners skilled in program evaluation and research would be beneficial to the coalitions [9].
Conclusion
This review with a realist lens provides preliminary explanations on the mechanisms involved in mobile and outreach services and collaborative interventions to increase access to PHC for vulnerable populations. Tailoring materials and services, offering the services where citizens experiencing many sources of vulnerability gather, as well as establishing partnerships that include community members and academic partners, all contribute to increased access to PHC for vulnerable populations. The findings of this review support the development, implementation, and evaluation of a “pop up” outreach intervention that is taking place in North Lethbridge, Alberta, which will in turn further inform PHC practice and policy.
Supplementary Information
Additional file 1: Full search strategies.
Additional file 2: Table 1. Summary of process factors that enhance or resist the intervention. Table 2. Summary of the effects of contextual factors on the intervention.
Acknowledgements
Becky Skidmore, Information Specialist.
Abbreviations
- CHW
Community health worker
- CTC program
Communities that Care program
- IMPACT
Innovative Models Promoting Access-to-Care Transformation
- LIP
Local innovation partnership
- PHC
Primary health care
- PROGRESS
Place of residence (urban/rural), Race/ethnicity/culture and language, Occupation, Gender or sex, Religion, Education, Socioeconomic status, Social capital
- RCT
Randomized controlled trial
- RE-AIM framework
Reach, Effectiveness, Adoption, Implementation, and Maintenance framework
- TIDieR checklist
Template for Intervention Description and Replication checklist
Authors’ contributions
VW, KP, SD, CS, CG, MT, and the LIP research team designed the question and methods. CG, MT, NA, AW, and EG screened articles for inclusion. CG, MT, RM, NA, AW, and SS extracted data. CG, MT, NA, AW, RM, and SS contributed to data synthesis CG, MT, NA, AW, EG wrote the draft manuscript. All authors reviewed, provided comments on the draft, and approved the final version.
Funding
The Innovative Models Promoting Access-to-Care Transformation (IMPACT) is a five-year research program funded by the Canadian Institutes for Health Research (CIHR) and the former Australian Primary Health Care Research Institute, which is supported by a grant from the Australian Government Department of Health under the Primary Health Care Research, Evaluation and Development Strategy.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Vivian Welch, Email: vwelch@bruyere.org.
Kevin Pottie, Email: kpottie@uwo.ca.
Caroline Gaudet, Email: caroline.gaudet1@gmail.com.
Micere Thuku, Email: micerethukus@gmail.com.
Ryan Mallard, Email: rwmallard@gmail.com.
Shannon Spenceley, Email: s.spenceley@uleth.ca.
Nida Amjed, Email: namjed@lakeheadu.ca.
Arpana Wadhwani, Email: awadh095@uottawa.ca.
Elizabeth Ghogomu, Email: etanjongghogomu@bruyere.org.
Cathie Scott, Email: cathie@k2aconsulting.ca.
Simone Dahrouge, Email: sdahrouge@bruyere.org.
References
- 1.Canada H. About primary health care. 2005. Available from: https://www.canada.ca/en/health-canada/services/primary-health-care/about-primary-health-care.html [Cited 2022 Jun 24]
- 2.Gauld R, Blank R, Burgers J, Cohen AB, Dobrow M, Ikegami N, et al. The World Health Report 2008 – Primary Healthcare: How Wide Is the Gap between Its Agenda and Implementation in 12 High-Income Health Systems? Healthc Policy. 2012;7(3):38–58. [PMC free article] [PubMed] [Google Scholar]
- 3.Corscadden L, Levesque JF, Lewis V, Strumpf E, Breton M, Russell G. Factors associated with multiple barriers to access to primary care: an international analysis. Int J Equity Health. 2018;17(1):1–10. doi: 10.1186/s12939-018-0740-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richard L, Furler J, Densley K, Haggerty J, Russell G, Levesque JF, et al. Equity of access to primary healthcare for vulnerable populations: the IMPACT international online survey of innovations. Int J Equity Health. 2016;15(1):1–20. doi: 10.1186/s12939-016-0351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haggerty J, Levesque JF, Harris M, Scott C, Dahrouge S, Lewis V, et al. Does healthcare inequity reflect variations in peoples’ abilities to access healthcare? Results from a multi-jurisdictional interventional study in two high-income countries. Int J Equity Health. 2020;19(1):167. doi: 10.1186/s12939-020-01281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell G, Kunin M, Harris M, Levesque JF, Descôteaux S, Scott C, et al. Improving access to primary healthcare for vulnerable populations in Australia and Canada: protocol for a mixed-method evaluation of six complex interventions. BMJ Open. 2019;9(7):e027869. doi: 10.1136/bmjopen-2018-027869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reid A, Abraczinskas M, Scott V, Stanzler M, Parry G, Scaccia J, et al. Using Collaborative Coalition Processes to Advance Community Health, Well-Being, and Equity: A Multiple-Case Study Analysis From a National Community Transformation Initiative. Health Educ Behav. 2019;46(1 suppl):100S–109S. doi: 10.1177/1090198119838833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner-Brown J, Krause LK. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev. 2015;(6). Art. No.: CD009905. 10.1002/14651858.CD009905.pub2. [DOI] [PMC free article] [PubMed]
- 9.Luque JS, Castañeda H. Delivery of mobile clinic services to migrant and seasonal farmworkers: a review of practice models for community-academic partnerships. J Community Health. 2013;38(2):397–407. doi: 10.1007/s10900-012-9622-4. [DOI] [PubMed] [Google Scholar]
- 10.Levesque JF, Pineault R, Hamel M, Roberge D, Kapetanakis C, Simard B, et al. Emerging organisational models of primary healthcare and unmet needs for care: insights from a population-based survey in Quebec province. BMC Fam Pract. 2012;13(1):1–11. doi: 10.1186/1471-2296-13-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenhalgh T, Kristjansson E, Robinson V. Realist review to understand the efficacy of school feeding programmes. BMJ. 2007;335(7625):858–861. doi: 10.1136/bmj.39359.525174.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pottie K, Hadi A, Chen J, Welch V, Hawthorne K. Realist review to understand the efficacy of culturally appropriate diabetes education programmes. Diabet Med. 2013;30(9):1017–1025. doi: 10.1111/dme.12188. [DOI] [PubMed] [Google Scholar]
- 13.Kellogg WK. WK Kellogg foundation logic model development guide. Battle Creek MI WK Kellogg Found. 2004. [Google Scholar]
- 14.Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, Vogt TM. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. 2006;21(5):688–694. doi: 10.1093/her/cyl081. [DOI] [PubMed] [Google Scholar]
- 15.Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001;44(2):119–127. doi: 10.1016/S0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- 16.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol. 2014;67(1):56–64. doi: 10.1016/j.jclinepi.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Bmj. 2014;348:g1687. [DOI] [PubMed]
- 19.Hawkins JD, Brown EC, Oesterle S, Arthur MW, Abbott RD, Catalano RF. Early effects of Communities That Care on targeted risks and initiation of delinquent behavior and substance use. J Adolesc Health. 2008;43(1):15–22. doi: 10.1016/j.jadohealth.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu M, Moritz S, Lorenzetti D, Sykes L, Straus S, Quan H. A systematic review of interventions to increase breast and cervical cancer screening uptake among Asian women. BMC Public Health. 2012;12(1):1–16. doi: 10.1186/1471-2458-12-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung B, Ong M, Ettner SL, Jones F, Gilmore J, McCreary M, et al. 12-month outcomes of community engagement versus technical assistance to implement depression collaborative care: a partnered, cluster, randomized, comparative effectiveness trial. Ann Intern Med. 2014;161(10 Supplement):S23–34. doi: 10.7326/M13-3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joshi C, Russell G, Cheng IH, Kay M, Pottie K, Alston M, et al. A narrative synthesis of the impact of primary health care delivery models for refugees in resettlement countries on access, quality and coordination. Int J Equity Health. 2013;12(1):1–14. doi: 10.1186/1475-9276-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta-analysis. BMC Public Health. 2015;15(1):1–23. doi: 10.1186/s12889-015-1352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Toole TP, Johnson EE, Borgia ML, Rose J. Tailoring outreach efforts to increase primary care use among homeless veterans: Results of a randomized controlled trial. J Gen Intern Med. 2015;30(7):886–898. doi: 10.1007/s11606-015-3193-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Yu G, et al. Measures of exposure to the Well London Phase-1 intervention and their association with health well-being and social outcomes. J Epidemiol Community Health. 2014;68(7):597–605. doi: 10.1136/jech-2013-202507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menon U, Szalacha LA, Kue J, Herman PM, Bucho-Gonzalez J, Lance P, et al. Effects of a community-to-clinic navigation intervention on colorectal cancer screening among underserved people. Ann Behav Med. 2020;54(5):308–19. doi: 10.1093/abm/kaz049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ursua RA, Aguilar DE, Wyatt LC, Trinh-Shevrin C, Gamboa L, Valdellon P, et al. A community health worker intervention to improve blood pressure among Filipino Americans with hypertension: A randomized controlled trial. Prev Med Rep. 2018;11:42–48. doi: 10.1016/j.pmedr.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berkley-Patton J, Bowe TC, Bauer AG, Berman M, Bradley-Ewing A, Goggin K, et al. A multilevel diabetes and CVD risk reduction intervention in African American churches: project Faith Influencing Transformation (FIT) feasibility and outcomes. J Racial Ethn Health Disparities. 2020;7(6):1160–171. doi: 10.1007/s40615-020-00740-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim MT, Kim KB, Huh B, Nguyen T, Han HR, Bone LR, et al. The Effect of a Community-Based Self-Help Intervention: korean Americans With Type 2 Diabetes. Am J Prev Med. 2015;49(5):726–737. doi: 10.1016/j.amepre.2015.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abbott L, Williams C, Slate E, Gropper S. Promoting Heart Health Among Rural African Americans. J Cardiovasc Nurs. 2018;33(1):E8–14. doi: 10.1097/JCN.0000000000000410. [DOI] [PubMed] [Google Scholar]
- 31.Diez E, Lopez MJ, Mari-Dell’Olmo M, Nebot L, Perez G, Villalbi JR, et al. Effects of a counselling intervention to improve contraception in deprived neighbourhoods: a randomized controlled trial. Eur J Public Health. 2018;28(1):10–5. doi: 10.1093/eurpub/ckx046. [DOI] [PubMed] [Google Scholar]
- 32.Redmond C, Spoth RL, Shin C, Schainker LM, Greenberg MT, Feinberg M. Long-term protective factor outcomes of evidence-based interventions implemented by community teams through a community–university partnership. J Prim Prev. 2009;30(5):513–530. doi: 10.1007/s10935-009-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Yu G, et al. Well London Phase-1: results among adults of a cluster-randomised trial of a community engagement approach to improving health behaviours and mental well-being in deprived inner-city neighbourhoods. J Epidemiol Community Health. 2014;68(7):606–614. doi: 10.1136/jech-2013-202505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stagg HR, Surey J, Francis M, MacLellan J, Foster GR, Charlett A, et al. Improving engagement with healthcare in hepatitis C: a randomised controlled trial of a peer support intervention. BMC Med. 2019;17(1):71. doi: 10.1186/s12916-019-1300-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Connell E, Zhang G, Leguen F, Prince J. Impact of a mobile van on prenatal care utilization and birth outcomes in Miami-Dade County. Matern Child Health J. 2010;14(4):528–534. doi: 10.1007/s10995-009-0496-8. [DOI] [PubMed] [Google Scholar]
- 36.Pati S, Ladowski KL, Wong AT, Huang J, Yang J. An enriched medical home intervention using community health workers improves adherence to immunization schedules. Vaccine. 2015;33(46):6257–6263. doi: 10.1016/j.vaccine.2015.09.070. [DOI] [PubMed] [Google Scholar]
- 37.Aldridge RW, Hayward AC, Hemming S, Possas L, Ferenando G, Garber E, et al. Effectiveness of peer educators on the uptake of mobile X-ray tuberculosis screening at homeless hostels: a cluster randomised controlled trial. BMJ Open. 2015;5(9):e008050. doi: 10.1136/bmjopen-2015-008050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Han HR, Kim K, Murphy J, Cudjoe J, Wilson P, Sharps P, et al. Community health worker interventions to promote psychosocial outcomes among people living with HIV-A systematic review. PLoS One. 2018;13(4):e0194928, 2018. doi: 10.1371/journal.pone.0194928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fang CY, Lee M, Feng Z, Tan Y, Levine F, Nguyen C, et al. Community-Based Cervical Cancer Education: Changes in Knowledge and Beliefs Among Vietnamese American Women. J Community Health. 2019;44(3):525–533. doi: 10.1007/s10900-019-00645-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vaughan EM, Johnston CA, Cardenas VJ, Moreno JP, Foreyt JP. Integrating CHWs as part of the team leading diabetes group visits: A randomized controlled feasibility study. Diabetes Educ. 2017;43(6):589–599. doi: 10.1177/0145721717737742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rodriguez-Romero R, Herranz-Rodriguez C, Kostov B, Gene-Badia J, Siso-Almirall A. Intervention to reduce perceived loneliness in community-dwelling older people. Scand J Caring Sci. 2021;35(2):366–74. doi: 10.1111/scs.12852. [DOI] [PubMed] [Google Scholar]
- 42.Reininger BM, Lee M, Hessabi M, Mitchell-Bennett LA, Sifuentes MR, Guerra JA, et al. Improved diabetes control among low-income Mexican Americans through community-clinical interventions: results of an RCT. BMJ Open Diabetes Res Care. 2020;8(1):e000867. [DOI] [PMC free article] [PubMed]
- 43.Preston MA, Glover-Collins K, Ross L, Porter A, Bursac Z, Woods D, et al. Colorectal cancer screening in rural and poor-resourced communities. Am J Surg. 2018;216(2):245–250. doi: 10.1016/j.amjsurg.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lewis ME, Myhra LL. Integrated care with indigenous populations: A systematic review of the literature. Am Indian Alsk Native Ment Health Res. 2017;24(3):88–110. doi: 10.5820/aian.2403.2017.88. [DOI] [PubMed] [Google Scholar]
- 45.Tsuyuki RT, Al Hamarneh YN, Jones CA, Hemmelgarn BR. The Effectiveness of Pharmacist Interventions on Cardiovascular Risk: the Multicenter Randomized Controlled RxEACH Trial. J Am Coll Cardiol. 2016;67(24):2846–2854. doi: 10.1016/j.jacc.2016.03.528. [DOI] [PubMed] [Google Scholar]
- 46.Stanley MA, Wilson N, Shrestha S, Amspoker AB, Armento M, Cummings JP, et al. Calmer Life: A Culturally Tailored Intervention for Anxiety in Underserved Older Adults. Am J Geriatr Psychiatry. 2016;24(8):648–658. doi: 10.1016/j.jagp.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 47.Barry M, Pappano C, Corveleyn A, Callaway C, Park ER, Irwin K. The impact of the bridge intervention on community mental health clinicians: Personcentered care for patients with serious mental illness and cancer. Psychooncology. 2020;Conference:(Supplement 1):70.
- 48.Hoffman J, Frerichs L, Story M, Jones J, Gaskin K, Apple A, et al. An integrated clinic-community partnership for child obesity treatment: a randomized pilot trial. Pediatrics. 2018;141(1):e20171444. [DOI] [PubMed]
- 49.Schroeder K, McCormick R, Perez A, Lipman TH. The role and impact of community health workers in childhood obesity interventions: a systematic review and meta-analysis. Obes Rev. 2018;19(10):1371–1384. doi: 10.1111/obr.12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Petts RA, Shahidullah JD. Engagement interventions delivered in primary care to improve off-site pediatric mental health service initiation: a systematic review. Fam Syst Health. 2020;38(3):310–22. doi: 10.1037/fsh0000521. [DOI] [PubMed] [Google Scholar]
- 51.Druss BG, von Esenwein SA, Glick GE, Deubler E, Lally C, Ward MC, et al. Randomized Trial of an Integrated Behavioral Health Home: The Health Outcomes Management and Evaluation (HOME) Study. Am J Psychiatry. 2017;174(3):246–255. doi: 10.1176/appi.ajp.2016.16050507. [DOI] [PubMed] [Google Scholar]
- 52.Dodge KA, Goodman WB, Bai Y, O’Donnell K, Murphy RA. Effect of a Community Agency-Administered Nurse Home Visitation Program on Program Use and Maternal and Infant Health Outcomes: A Randomized Clinical Trial. Jama Netw open. 2019;2(11):e1914522. doi: 10.1001/jamanetworkopen.2019.14522. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Full search strategies.
Additional file 2: Table 1. Summary of process factors that enhance or resist the intervention. Table 2. Summary of the effects of contextual factors on the intervention.
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].


