Abstract
Asteroid hyalosis (AH) is a benign clinical entity characterized by the presence of multiple refractile spherical calcium and phospholipids within the vitreous body. First described by Benson in 1894, this entity has been well documented in the clinical literature and is named due to the resemblance of asteroid bodies on clinical examination to a starry night sky. Today, a growing body of epidemiologic data estimates the global prevalence of asteroid hyalosis to be around 1%, and there is a strong established association between AH and older age. While pathophysiology remains unclear, a variety of systemic and ocular risk factors for AH have recently been suggested in the literature and may provide insight into possible mechanisms for asteroid body (AB) development. As vision is rarely affected, clinical management is focused on differentiation of asteroid hyalosis from mimicking conditions, evaluation of the underlying retina for other pathology and consideration of vitrectomy in rare cases with visual impairment. Taking into account the recent technologic advances in large-scale medical databases, improving imaging modalities, and the popularity of telemedicine, this review summarizes the growing body of literature of AH epidemiology and pathophysiology and provides updates on the clinical diagnosis and management of AH.
Keywords: asteroid hyalosis, epidemiology, risk factors, imaging, management, posterior lens calcification, telemedicine
Introduction
In 1894, Alfred Hugh Benson described a condition of multiple spherical particles within the vitreous that were sensitive to eye movements as a distinct entity from synchysis scintillans referred to Scintillatio Albescens or Benson’s Disease.1–3 The condition was later called Asteroid Hyalitis in the late 20th century given the appearance of the vitreous body resembling a starry night sky and eventually renamed asteroid hyalosis years later to denote the absence of an inflammatory component.4
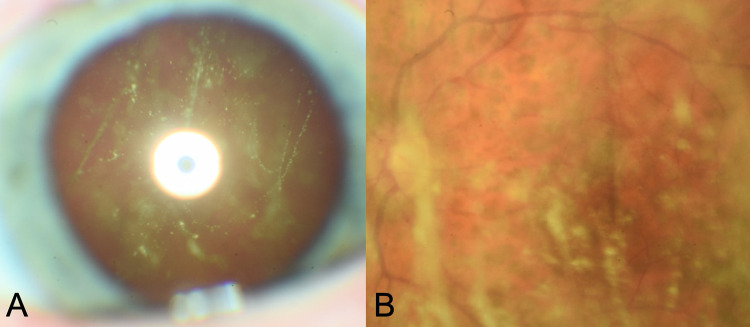
Today, asteroid hyalosis (AH) is defined as an idiopathic condition in which multiple yellow-white particles or asteroid bodies are found within the vitreous cavity4 (Figure 1). Histologically, asteroid bodies (ABs) have been characterized as primarily composed of calcium and complex phospholipids within the otherwise homogenous and proteinaceous vitreous.5 Clinically, this condition rarely affects vision despite ABs diffusely filling the vitreous and treatment with vitrectomy is seldom required.2
Figure 1.
(A) Slit-lamp and (B) fundus photography of asteroid hyalosis.
The purpose of this review is to summarize the clinical literature describing epidemiology, potential pathophysiology, clinical diagnosis, and management of AH, while also providing insight into areas of further research and evolving clinical relevance of this well-known entity.
Epidemiology of Asteroid Hyalosis
The worldwide prevalence rates of asteroid hyalosis have been reported to be between 0.3–2.0%.6–12 Largest existing epidemiologic studies on AH differ with respect to the diagnostic methodology, the ethnic makeup of the study population, and the study period and duration (Table 1).
Table 1.
Epidemiologic Literature of Asteroid Hyalosis
| Study | Location | Study Period | Ethnic Makeup of Study Population | Diagnosis | Sample Size | Prevalence | Significant Risk Factors |
|---|---|---|---|---|---|---|---|
| Bergren et al6 | Philadelphia, PA | 1989–1990 | White 56.4%a Black 43.6% |
Clinical exam | 12,205 | 0.83% (n=101) | Diabetes, hypertension, atherosclerosis, hyperopia |
| Beaver Dam Study13 | Beaver Dam, WI | 1988–1990 | White 99.4% | Fundus photos | 4,926 | 1.2% (n=57) | Age, male sex, BMI, alcohol consumption |
| Blue Mountain State8 | Blue Mountains Region, Australia | 1997–1999 | Primarily whiteb | Fundus photos and clinical exam | 3,654 | 1.0% (n=36) | Age, male sex |
| UCLA Eye Study12 | Los Angeles, CA | 1965–2000 | White 75% Black 13% Asian 2% Other 10% |
Autopsy specimen | 10,801 | 1.99% (n=212) | Age, male sex, hypertension, atherosclerosis, posterior vitreous detachment, age-related macular degeneration |
| Yonsei Eye Study7 | Seoul, Korea | 2006 | Asian 100% | Fundus photos | 9,050 | 0.36% (n=33) | Age, stroke, hypertension, hypertriglyceridemia |
| Gutenberg health survey9 | Rhine-Main Region, Germany | 2007–2012 | Primarily whiteb | Fundus photos | 12,779 | 0.46% (n=61) | Age, diabetes |
| Duong et al10 | United States | 2005–2008 | White 54.03% Black 20.33% Hispanic 22.39% Other 3.24% |
Fundus photos | 5,578 | 0.86% (n=48) | Age, BMI, prior myocardial infarction |
| Beijing Eye Study11 | Beijing | 2011 | Asian 100% | Fundus photos and clinical exam | 3,419 | 1.6% (n=53) | Age, thicker lens, hyperopia |
Notes: aOnly ethnic makeup of the asteroid patients reported. bSpecific makeup not reported. Commonly observed associations in ≥3 studies are bolded.
In contrast to clinical practice, the majority of epidemiologic studies have relied on fundus photography data alone for diagnosis of AH. The Beaver Dam Eye Study reported a regional prevalence rate of 1.2% by examining fundus photos from a primarily White population in Beaver Dam, WI from 1988–1990.13 The Gutenberg Health Study demonstrated a lower prevalence of 0.46% based on fundus imaging within the Rhine-Main Region of Germany in a similarly mostly White population from 2007–2012.9 Kim et al7 reported an even lower prevalence rate of 0.36% in imaging analysis of the Asian population of Seoul Korea in 2006. Our group has conducted an epidemiologic study of AH using fundus photography data from the United States NHANES database in a more demographically diverse population (54% White, 20% Black, 22% Hispanic) and reported an overall prevalence of 0.86%.10
Expanding methodology to include a combination of clinical exam and fundus photography to diagnose AH, the Blue Mountain Eye Study and the Beijing Eye Study reported similar higher rates despite significantly different patient populations studied with 1.0% prevalence in the Australian population in 1997–1999 and 0.9% in the Chinese population in 2011, respectively.8,11 Clinical exam alone was used to diagnose AH in the commonly cited Bergren et al study which evaluated a total of 12,205 patients (56% White, 43% Black) presenting for routine eye exams at Wills Eye Hospital between 1989–1990 and found a AH prevalence rate of 0.83% (n=101).6 A unique approach was utilized in the UCLA study, which used clinical autopsy data from 10,801 eyes to diagnose AH, observing a significantly higher rate of 2% within the Los Angeles population comprising 75% White, 13% Black, and 2% Asian groups. No specific data was reported with respect to the severity of AH noted in this autopsy study.12
While there does not appear to be a major discrepancy in prevalence rates with a diagnosis of AH based on clinical exam versus fundus photography, future population-based studies and meta-analyses may explore potential biases or overdiagnosis of AH via photography alone, paying specific attention to potential mimickers of asteroid hyalosis such as synchysis scintillans or uveitis which may not be as easily distinguishable with only a single fundus view.
The variability in AH prevalence rates over time appears to reflect differences in the geographic distribution and demographics of the study populations as well as diagnostic approaches. It is difficult to determine whether prevalence rates have changed since the 1980s given such regional and ethnic variations. Of the previous literature, six of seven large studies are limited to a single center, city, or region. White and Asian ethnic groups remain relatively over-sampled with respect to the global population at-large. Hispanic and Black patients have been under-represented overall, but their distribution within existing literature appears to reflect the regional ethnic distribution of the overall population at the time of study.
While there is ongoing debate10 regarding increased prevalence of AH within specific ethnic groups, presently, there is a lack of epidemiologic studies comparing regional and ethnic prevalence rates. Only one prior large scale study has attempted to examine AH at a national level with a demographically diverse study population.10 This US study found no significant difference in AH prevalence with respect to ethnicity groups but reported an ethnicity-specific prevalence of 0.86% in Caucasians, 0.79% in African-Americans, and 0.88% in Hispanics.10 Interestingly, Malerbi et al14 described a much smaller study of 82 individuals within the closed Brazilian Xavante Indian tribe and found an astonishingly high prevalence rate of 10.7% with potentially familial cases of AH. The ethnic distribution of AH may be an area for future epidemiologic surveys as rising popularity of insurance-based databases and central registries allows for larger scale studies and potential uncovering of regional versus demographic differences that may speak of the potential etiology of AH or risk factors.15
Bilateral asteroid hyalosis is an interesting and rare sub-group of AH that deserves special attention. Within the current literature, bilateral AH appears to be present in roughly 9–21% of AH cases.9,11,13 No specific risk factors have been identified for development of bilateral AH, and it remains unclear why bilateral cases are present in only a minority of patients. This prevalence is specifically important to consider when considering potential mimickers of AH such as vitreous amyloidosis or ocular lymphoma which have a higher rate of bilateral involvement. The presence of bilateral cases supports at least some systemic pathophysiology or predisposition, although no familial cases of AH have been reported. Previous literature has suggested a younger age of AH onset may be seen in bilateral cases, although this has yet to be validated or studied in sufficient detail.6
Systemic Risk Factors
A variety of systemic risk factors have been proposed for AH, with age being the best established. Nearly all the population-based surveys in Table 1 described a population of patients age 50 or older. Considering that there are over 46 million United States citizens over the age of 65 currently and that this number is expected to nearly double by 206016 with a correlated increase in AH prevalence to 91.2 million by the year 2100,17 a greater understanding of AH pathology, the disease process, and its clinical impact is necessary. Older age as a risk factor may imply an underlying degenerative causality.
In addition to age, numerous other systemic risk factors have been proposed for AH, including male sex,8,12,13 hypertension,6,7 stroke,7 elevated serum triglyceride,7 elevated serum low-density lipoprotein (LDL),7 hypercalcemia,18 atherosclerotic vessel disease,6 diabetes,6,19 high body mass,13 and alcohol consumption13 (Table 1). Unfortunately, these risk factors have been inconsistently explored within the existing epidemiologic literature which may contribute to the observed differences in AH prevalence. Notably, smoking has never been found to be associated with AH, despite its strong correlation with these systemic factors, and age may be a potential confounder as not all previous epidemiologic studies adjusted for age in their analysis.
Taken collectively, these risk factors may imply an underlying relationship with metabolic dysfunction or coronary disease. Our analysis of the US population discovered an additional association with greater body weight (BMI) and prior myocardial infarction.10 The predominantly unilateral nature of AH remains difficult to reconcile with systemic risk factors such as age, metabolic dysfunction, or coronary disease, and there does not appear to be a right vs left predominance despite potential implications and atherosclerotic differences between an aortic-derived versus subclavian-derived carotid artery.
Ocular Risk Factors
Ocular-level risk factors and associations with AH have similarly been inconclusively addressed in the literature. Bergren et al first identified a relationship between AH and refractive error with a mean refractive error of +1.10 D in AH compared to +0.193 in the control arm. Hyperopia along with a thicker lens were found as ocular risk factors for AH in the Beijing Eye Study.11 However, the Beaver Dam Study and our own recent national survey of United States adults did not find any significant relationship between AH and ocular conditions studied, including refractive error, glaucoma, intraocular pressure, diabetic retinopathy, or cataract.
Interestingly, recently several reports have pointed out a higher prevalence of AH in younger patients with rare retinal dystrophies which deserves further study. Ikeda et al20 reported a higher than average prevalence of AH (3.1%, n=10) within the Asian retinitis pigmentosa population. There is also a report of high AH prevalence within a specific subtype of Leber congenital amaurosis patients with discovered LRAT (lecithin retinol acyltransferase) gene mutation (n=3, 37.5%).21 Fantin et al22 reported a case of a 4-week infant with Down syndrome and bilateral cataracts. The association between AH and these dystrophic cases may further support the degenerative mechanism of AB formation discussed earlier.
Histopathology and Possible Pathophysiology
A variety of suggested mechanisms for AH have been described in the literature. Early theories were formed on the bases of biochemical and histological discoveries of asteroid body structure and arrangement. In the 1920s Verhoef23 characterized the histologic structure of a human AH sample and identified the presence of calcium bound to fatty acids. This composition, distinct from the surrounding vitreous, led Verhoef to postulate angiosclerosis of intraocular vessels as a potential route for AB formation. Forty years later, Rodman et al24 continued to describe the arrangement of AB’s in relation to the vitreous and identified two different arrangements. In Type I, ABs were suspended in normal vitreous fibrils, whereas ABs appeared surrounded by vitreous tissues in a milieu of macrophages and inflammatory cells in Type II. This led Rodman et al to suggest the potential presence of two pathophysiologic mechanisms. Interestingly, both types of ABs have been identified in a single eye25 and there remains no association with AH and clinical uveitis.2
In the 1970s, electron microscopy technology allowed March and Shoch26 to characterize numerous AB “satellites” equal in size and arrangement within the surrounding vitreous, and they postulated AB formation to be related to a shift in the physiochemical properties of a hyper-saturated vitreous to form solid satellite calcium crystals which coalesce into larger, visible ABs. However, Streeten27 opposed this hypothesis, pointing out that large quantities of complex lipids do not usually present in normal vitreous, and suggested AB derivation from a source exogenous to the eye. Thirty years later, in 2003, Komatsu et al28 conducted a biochemical analysis using electron microscopy and focused ion-beam technology, simulating analogous ex vivo lipid arrangements of asteroid bodies. Based on these findings, they inferred that production of AB occurs in response to changes in ionic tension and the extracellular matrix of the vitreous, as can be seen with aging or disease and coined the term “a condition of lithiasis in the body” to describe AH pathogenesis.
To date, these pathogenic hypotheses have yet to be studied in sufficient detail and the exact pathophysiology remains unclear. More precise characterization of the composition and structure of ABs within the vitreous remains limited due to their small size and high rate of contamination with surrounding vitreous matrix.29 Further, the conversation regarding potential AH pathophysiology has shifted towards attempting to reconcile previously established significant risk factors for AH. There is on-going debate whether AH shares similar degenerative and microvascular mechanisms with metabolic dysfunction and coronary artery disease given commonly identified shared risk factors of age, hypertension, diabetes, and male sex.6,9,12,13 In addition, the recently identified findings of higher AH prevalence within retinitis pigmentosa and Leber congenital amaurosis patients have also led to the theory that intraocular cellular degradation (either with age in these cases photoreceptor death) leads to cellular remains and deposition of waste products in the vitreous.20,21
Future approaches to understanding AH pathophysiologic should utilize a multimodal approach, reconciling epidemiologic findings with histologic and biochemical data. One consideration may be to explore calcium dysregulation as a mechanism for AB formation given the known presence of calcium within the AB bodies along with several shared risk factors between AH and coronary disease, in which aberrant calcification is a known part of disease pathogenesis and progression. Only one study has demonstrated a relationship between AH and hypercalcemia to date, so further work is needed to explore the potential association between AH and systemic calcium dysregulation including variables such as renal disease, parathyroid dysfunction, or Vitamin D. It is also reasonable to explore the cellular waste product theory by observing vitreous changes in response to cellular degradation in vitro or in animal models. In the same manner, future epidemiologic studies should continue to evaluate suspected risk factors and comorbidities to validate pathophysiologic hypotheses, including looking into prior trauma as a risk factor for AH, exploring the degenerative and cell death theory of AH pathology. AH may in fact represent a final common pathway for multiple clinical conditions and risk factors.
Presentation
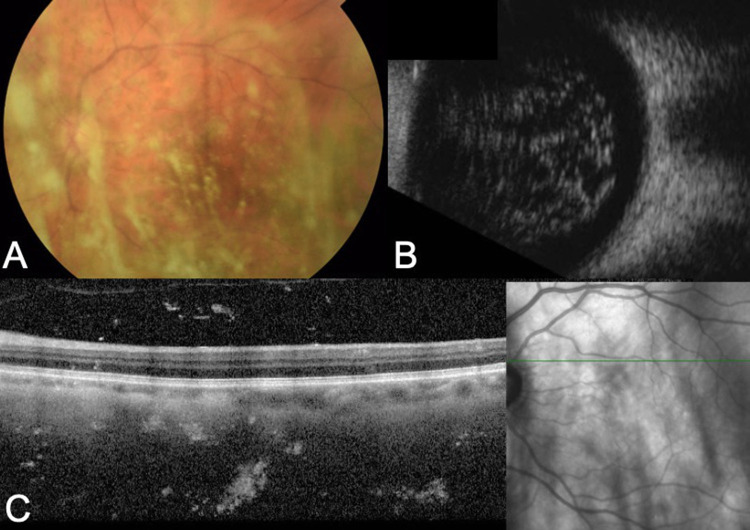
Typical presentation is of gradual onset, unilateral involvement in an asymptomatic older patient without pain, history of trauma, or recent surgery. Diagnosis is usually made on fundoscopic examination by observation of numerous diffuse yellow-white spherical opacities of varying size and density within the otherwise clear intervening vitreous (Figure 1). There is typically no evidence of anterior segment inflammation, absence of retinal vessel dilation, no vascular exudates, and lack of optic nerve swelling or pallor. The asteroid bodies undulate with the vitreous during eye movement but do not settle inferiorly at rest.2 They are often directly visible with dilation on slit lamp exam with a fundus lens or fundus photography. On optical coherence tomography (OCT), ABs appear as multiple hyperreflective foci and they are hyperechogenic on B-scan ultrasonography (Figure 2). To our knowledge, there is only one previously published grading system to characterize AH based on visibility of fundus features. Rani and Prajapati30 described AH as Grade 1 if the optic disc and second-order vessels were visible, Grade 2 if the optic disc and first order vessels were visible, Grade 3 if the optic was disc hazy, or Grade 4 if there was no view of the fundus. However, in clinical practice there is no widely utilized grading system for AH severity, and AH is typically only described based on the AB density (mild-to-severe). Given the rarity of cases, a rate for symptomatic AH has not yet been reported.
Figure 2.
(A) Fundus photography, (B) B-scan, and (C) OCT imaging of asteroid bodies in an eye with asteroid hyalosis.
Differential Diagnosis
While AH is classically recognizable on exam, it is important to consider potential, more ominous, mimickers of AH, as described in Table 2. Any deviation from the typical AH presentation and exam such as new onset of symptoms, pain, extra-vitreal involvement/findings, or vitreous stranding/haze warrant further exploration of alternative diagnosis.
Table 2.
Differential Diagnosis of Asteroid Hyalosis
| Diagnosis | Vitreous Deposits | Typical Presentation | Common Exam Findings | Relevant Imaging | Associations and Relevant History |
|---|---|---|---|---|---|
| Asteroid Hyalosis | Calcium and phospholipids (hydroxyapatite) | Slow onset, asymptomatic | Multiple yellow-white well demarcated spherical vitreous bodies. Otherwise clear vitreous, No ocular inflammation or retinal findings |
Yellow-white vitreous deposits on fundus photography. Multiple hyperreflective foci on OCT B-Scan with multiple hyperechoic foci |
Older age, possibly male sex, hypertension, elevated BMI, etc. |
| Synchysis Scintillans | Cholesterol deposits | Slow onset, asymptomatic | Gold colored vitreous opacities that settle inferiorly at rest | Similar to AH with hyperreflective foci on OCT and hyperechoic bodies on b-scan. A-mode images display characteristic flickering spikes from the reflections of these crystals. | Younger age of onset than AH (Typically 3rd decade) Chronic vitreous hemorrhage, Diabetic retinopathy, chronic uveitis, detachment Bilateral predominance |
| Posterior Vitreous Detachment | Posterior hyaloid membrane | Acute onset floater, flashing lights | Single or small cluster vitreous opacities or Weiss ring with or without pre-retinal hemorrhage | OCT and B-scan showing separation of posterior hyaloid with otherwise normal retina | Older age, trauma |
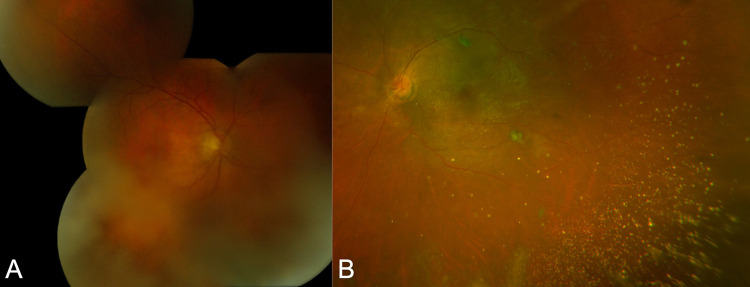
| Chronic Vitreous Hemorrhage (Figure 3B) | Dehemoglobinzed red blood cells | Gradual and acute onset of blurry vision | White or white-yellow intra-vitreal blood obscuring view of fundus | B-scan showing dot like echoes form a highly reflective membrane over a period of time, denser inferiorly. | Diabetes, trauma, prior surgery |
| Uveitis (Intermediate/Posterior) | Inflammatory cells | Acute onset pain, blurry vision, photophobia | Vitreous Cell/Flare, Haze, Stranding, or Snowballs. Less distinct borders of vitreous debris. Potential anterior chamber and retinal changes. |
Varied but can see underlying retinal pathology and OCT on fundus photography, including snowbanking, retinoschisis, epiretinal membrane (ERM), Cystoid macular edema (CME), retinitis, choroiditis |
|
| Siderosis | Metallic iron deposition from intraocular foreign body (IOFB) | Early acute mydriasis and iris heterochromia followed by progressive vision loss | Variable but can see iron deposition within cornea, iris, lens, or retina. | Variable but CT may localize IOFB (MRI not recommended due to potential electromagnetic reaction). Possible CME and evidence of retinal necrosis on OCT | Male, younger age, History of activity activities that may predispose to metallic IOFB injury |
| Amyloidosis (Figure 3A) | Hyaline fibrils | Gradual onset blurred vision, photophobia, diplopia | Grannular vitreous opacities that coalesce into a glass wool- appearance. Coating of vitreous strands. |
Varied findings but can see extension to retina on OCT or adnexal involvement on head CT | Bilateral predominance. Vitreous opacities are common in familial amyloidosis and can deposit along blood vessels May have history of arrhythmia, cardiac dysfunction, pulmonary disease, or peripheral neuropathy |
| Indolent Endophthalmitis | Inflammatory and bacterial or fungal cells | Progressive decline in visual activity. Pain atypical in indolent cases |
Anterior segment reaction, possible small hypopyon (less common in indolent cases). Vitreous haze. Possible retinal or subretinal inflammatory deposits |
Hazy media on fundus photography and OCT. B-scan with dispersed vitreous opacities, vitritis, chorioretinal thickening Diffuse vitreous haze, Less distinct borders of vitreous deposit |
|
| Malignancy & Lymphoma | Malignant lymphoid cells | Gradual onset floaters, blurred vision | Anterior white vitreous cells often with a dense posterior vitreous membrane | Varied findings but can see chorioretinal involvement on OCT with subretinal infiltrates. CME is less common than with posterior uveitis |
Female predominance 4th to 6th decade of life |
Posterior vitreous detachment (PVD) is a far more common entity to consider for older patients presenting with floaters and vitreous debris. It is usually easily distinguished from AH by only a single Weiss ring or a small cluster of vitreous opacities. However, dual pathology is plausible and development of a PVD in an eye with asteroid hyalosis has been reported to induce acute symptoms by potentially concentrating the AB towards the anterior vitreous or allowing sub-hyaloidal re-distribution and loculation of ABs closer to the retina.31
The presence of vitreous cells (neoplastic, inflammatory, pigmentary, or hematogenous) must be distinguished from the larger sharply defined creamy-white asteroid bodies. Careful evaluation of the anterior segment and underlying retina for absence of concurrent pathology signs is crucial to rule out conditions such as uveitis, endophthalmitis, retinal tear/detachment, or dehemoglobinized vitreous hemorrhage (Table 2). Specifically, the presence of ocular inflammation, vascular dilation, vitreous haze or stranding, retinal, subretinal, or retinovascular deposits, retinal tear or scars, and optic nerve swelling or pallor are concerning for alternative pathology. A multimodal evaluation or imaging approach is recommended as dense AH may mimic other conditions when evaluated by a single imaging modality. For example, severe AH may appear similar to snowballs observed in intermediate uveitis in a single fundus image, and asteroid bodies can appear more confluent on B-scan mimicking vitreous hemorrhage, although calcium within ABs causes a typical hyperechoic signal on US.
There are three very rare conditions where clinical differentiation from AH may be especially difficult. Synchysis scintillans, or cholesterosis bulbi, is a benign condition characterized by cholesterol deposits within the vitreous that freely move in a gravity-dependent manner. This condition is often found incidentally and described by the presence of yellow highly refractive flat crystals within the vitreous humor. The pathophysiology of synchysis scintillans remains largely unknown, although is postulated to be related to degeneration of blood products within the vitreous given known associations of this condition with history of chronic ocular conditions such as vitreous hemorrhage, hyphema, retinal detachment, chronic uveitis, and Coats’ disease.1,32,33 This entity can be distinguished from AH by observing the vitreous bodies settle inferiorly when the eye is not in movement providing a “snow-globe” effect.34 Additionally, synchysis scintillans typically has a younger age of onset, around the third decade of life, compared to AH, and has a bilateral predominance.
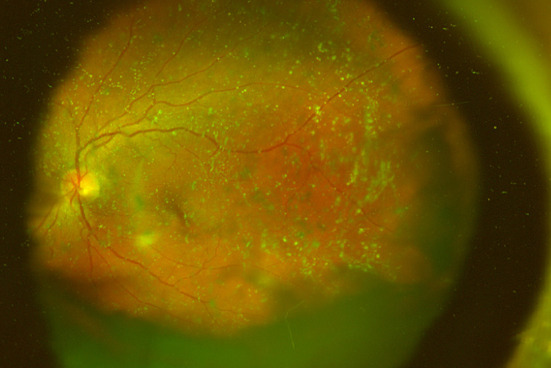
Amyloidosis is a heterogenous group of disorders characterized by deposition of hyaline extracellular material throughout the organs in the body and can involve the eyes. Ocular amyloidosis often presents bilaterally, although the presentation can be asynchronous, and can involve all structures within the eye with perivascular deposits and periocular tissues in the orbital compartment35 and conjunctiva. Vitreous amyloid deposits are specifically common in transthyretin-related amyloidosis36 and appear as “initially granular with wispy fringes” which grow and aggregate into a “glass-wool appearance”37 (Figure 3). These deposits frequently impact vision in contrast to AH and can often be distinguished by the presence of extravitreal involvement. Finally, malignancy such as primary vitreoretinal lymphoma can present with a posterior/intermediate uveitis and white anterior vitreous cells with less defined borders compared to AH. Chorioretinal lesions can sometimes be concurrently present but may be challenging to assess in the setting of dense anterior deposits.38
Figure 3.
Mimickers of asteroid hyalosis – (A) montage fundus photography of ocular amyloidosis and (B) Optos imaging of de-hemoglobinzed vitreous hemorrhage resembling AH.
Further diagnostic workup is rarely needed for AH or synchysis scintillans but can be pursued in cases where clinical examination and imaging alone are insufficient to differentiate or rule out other conditions. Vitreous sampling and cytopathology should be reserved for cases where clinical suspicion of more aggressive conditions remains high. Cytopathology can be both diagnostic and prognostic in conditions such as amyloidosis or lymphoma and carries significant implications for management of extra-ocular aspects of the disease.
Clinical Management
Patients with AH are typically asymptomatic and treatment with vitrectomy is rarely considered. Indications for surgery in symptomatic AH include extensive floaters, glare, and visual obscurations, as can be seen with PVD shifting ABs anteriorly.31,39,40 Surgery can also be considered when AH impairs visualization of the fundus thereby limiting adequate evaluation of posterior pathology or when treatment with focal laser or pan-retinal photocoagulation (PRP) requires better visualization.39,41 Higher order aberrations can be a source of visually symptomatic AH and use of an aberrometer to quantify these aberrations in correlation with patient-reported symptoms can provide an objective data point to assist with the decision to pursue surgery for symptomatic AH.42,43
Specific outcomes data for surgical treatment of AH are limited due to the rarity of these cases. To our knowledge, the only case series of patients undergoing vitrectomy for visually symptomatic AH, without additional retinal pathology, was reported in 1998 by Parnes et al,44 who found at least neline of Snellen visual acuity improvement in nine of ten total eyes. The remainder of the literature describing surgical outcomes in AH come from a case series of patients with incidental AH undergoing vitrectomy for other indications such as retinal detachments, macular hole, or epiretinal membranes.45–47 While this limits interpretation of visual outcomes for primary treatment of symptomatic AH, specific surgical challenges with AH have been described such as increased vitreomacular adhesions and vitreoretinoschisis.45–47 Because of this, careful discussion of the risks and benefits is necessary prior to pursuing vitrectomy in patients with AH.
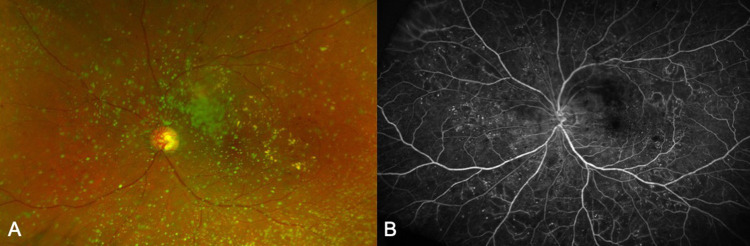
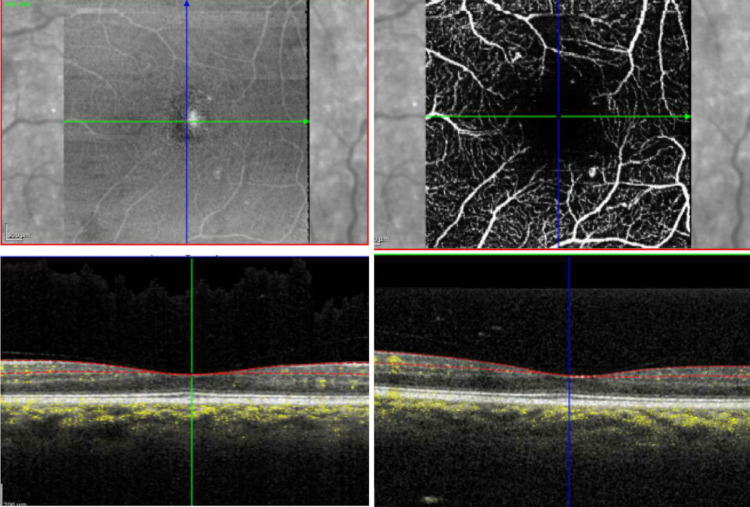
The need for vitrectomy to better visualize the posterior pole in dense AH may likely decrease moving forward given advances in ocular imaging techniques. In the past, fluorescein angiography was the only imaging modality that could minimize the blue light scatter effect of ABs via the built in barrier function48 and has been a useful tool to monitor underlying retinal disease in AH (Figure 4). Newer advances in non-invasive imaging are allowing for better visualization of the underlying retina and assessment of pathologies such as diabetic retinopathy, age-related macular degeneration (AMD), retinal vascular occlusion, or retinal tears in even dense AH.30 Since the early 2000s, OCT technology has drastically improved assessment of the underlying retina, and a recent study has confirmed the ability of this modality to minimize AB artifactual distortion with use of patient positioning, corneal lubrication, and adjusting the focus knob to the most highly saturated diopter.34 OCT Angiography (OCT-A) has been demonstrated to provide adequate assessment of the underlying retinal and choroidal vasculature with minimal induced AB artifacts30,49 (Figure 5). For example, a single case study by Belenje and Rani49 demonstrated the effectiveness of OCT-A to detect new vessel growth in proliferative diabetic retinopathy with dense AH. Ultra-wide field imaging has also recently become an additional helpful tool to evaluate disease peripheral to central ABs (Figure 6) with a recent case reporting successfully imaging and diagnosing choroidal melanoma in an eye with dense AH.50
Figure 4.
(A) Pseudo-color photo versus (B) fluorescein angiography of an eye with asteroid hyalosis and severe non-proliferative diabetic retinopathy.
Figure 5.
OCTA imaging of asteroid hyalosis depicted.
Figure 6.
Ultra-wide view imaging of asteroid hyalosis.
Necessity of vitrectomy to allow visualization for laser ablative treatment of proliferative vascular diseases in eyes with AH may be supplanted by the use of intravitreal injections that are not affected by visual obscuration of AH and appear to be effective in recent trials compared to PRP for treating proliferative diabetic retinopathy (PDR) with reduced need for laser (and therefore vitrectomy) in AH eyes with PDR.51,52
Cataract Surgery
Implications of AH in cataract surgery are well documented in the literature. Pre-operatively, clinical refraction and retinoscopy is always recommended in patients with AH as ABs can create a falsely hyperopic results on auto-refraction by creating a reference point within the vitreous rather than the retina.53 Wang et al demonstrated a false automated refraction of +13D in a patient with AH that correlated with clinical retinoscopy finding of +1.0D. Likewise A-scan ultrasound of eyes with AH tend to create falsely low estimates via similar mechanisms.54–56 Allison et al54 reported a case series of 20 patients in 1991 with unilateral AH in which five eyes (25%) had falsely low biometry of roughly 1 mm estimated by A-scan which corresponds greater than 2.5 D of error in implanted intraocular lens (IOLs). Previously, tactics to address this problem included use of the fellow eye to calculate intraocular lens power prior to surgery,57 but fortunately modern optical biometry limits the need for A-scan to estimate axial length to only eyes with severe dense cataracts.
It is unclear to what extent asteroid bodies affect modern biometry techniques, so a multi-modal approach, utilizing multiple methodologies and measurements is recommended for IOL calculation and selection for patients with AH.39 Monofocal lenses are typically preferred for AH given potential concerns for worsening glare or dysphotopsia with multi-focal IOL.39 The newer light-adjustable IOLs may be considered in AH patients given concerns with unpredictability of pre-operative measurements.58
During the cataract surgery itself, AB bodies may affect visualization of the posterior capsule.2 As intra-operative and early post-operative complications are rare, there is limited literature describing cataract surgery outcomes and early complications in eyes with AH. One case report described an eye with severe visual acuity loss due to an induced PVD during cataract that required vitrectomy.59 A second report described a case of vitreous wicking syndrome post-cataract surgery complicated by ABs prolapsing into the anterior chamber and causing incarceration in the inner lip of the superotemporal limbal incisional scar.60 This case resolved with Nd:YAG vitreolysis, and the authors postulated that, much like the anomalous vitreoretinal adhesions described in the vitrectomy case series with AH,45–47 there may be increased risk of vitreoretinal interface disorders in eyes with AH and vitreous wicking.
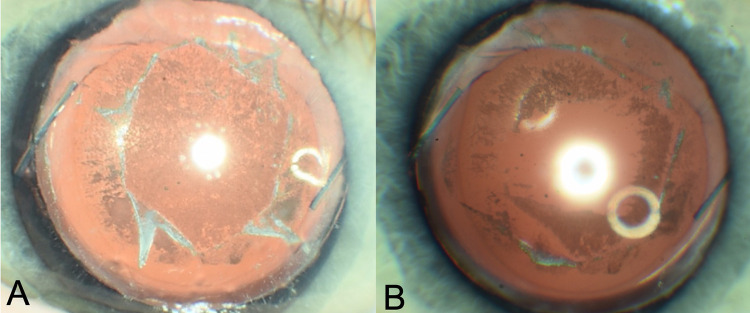
Recently, a novel condition has been described in patients with AH involving posterior calcification of silicone IOL implants. It is a rare but well documented late complication in eyes with AH which can occur years after surgery.2,4,39,61 Interestingly, this process appears to be exclusive to silicone-containing IOLs, and management is traditionally IOL exchange with a hydrophobic acrylic lens.4,39,62 For patients with open posterior capsules, the new IOL may be placed in the sulcus, although this may be associated with complications including corneal decompensation, loss of zonular stability, and change in post-operative refractive error. Additionally, anterior vitrectomy during IOL exchange is frequently required in patients with a prior posterior capsulotomy.63
Alternative approaches have recently been attempted to avoid IOL exchange in patients with dystrophic IOL calcification from AH and a posterior capsulotomy. Lee and Han64 described successful use of a Nd:YAG laser to clear calcifications in an eye that previously had undergone laser capsulotomy treatment for posterior capsular opacification (PCO) 3 years prior. Mehta et al65 used a 23-g vitrector to scrape calcium deposits without intra-operative complication. Ullman and Gupta66,67 and Rainsbury nd Lochhead also attempted a similar debridement using 23 and 25-g vitrectors but were unsuccessful, pointing out a smearing effect with the vitrectors due to the “putty-like” consistency of the lens calcifications. Platt et al68 attempted the scraping technique using a variety of tools ndhad most success with the lighted pick. Most recently, our group reported a successful AH-associated silicone IOL debridement in an eye with prior capsulotomy using a 27-g shielded light pipe, followed by vitrectomy to prevent further calcifications (Figure 7).69 We felt that use of the shielded light pipe was a safer alternative to 23-g and 25-g vitrectors and provided a broader beveled tip and wider area of illumination, which may make silicone IOL scraping more efficient compared to the lighted pick without damaging the lens. Further research and surgical outcomes work may continue to explore IOL debridement and laser as an alternative treatment to IOL exchange for silicone IOL calcifications in AH.
Figure 7.
Silicone lens calcification in an eye with asteroid hyalosis before (A) and after (B) lens-debridement and vitrectomy.
Evolving Areas of Clinical Relevance
The evolution of big data and machine learning algorithms as well as rapidly developing ophthalmic imaging technology bring into question potential impacts and interaction with AH. It remains uncertain how newer developments in AI, telemedicine, and home imaging will affect patients with AH, where fundus evaluation is inherently difficult. Future work should pay specific attention to this growing sub-population.
AI-based fundus photography evaluation is perhaps the largest growing area of clinical interest with relevance to AH.70 To date, several artificial intelligence (AI)-based algorithms have been developed to interpret fundus photography. Specifically, automation of diabetic retinopathy screening has been a target goal for software companies in recent years,71 but the impact of AH and AB artifacts on the screening algorithms remains unclear. A recent multicenter cross-sectional diagnostic study demonstrated the use of an EyeArt algorithm in screening diabetic retinopathy with a sensitivity of 96% and specificity of 88% for more than moderate diabetic retinopathy in primarily non-mydriatic eyes.72 However, as with many studies evaluating AI-based fundus interpretation software, photos with ABs were either never included in the training/testing datasets or were screened out due to poor image quality.71,73
Compared with clinician review, a computer-based algorithm may be more at risk for falsely misinterpreting an AB-induced scatter artifact as, for example, a media opacity or vitreous hemorrhage. Interestingly, when AH images were included in the test set for evaluation of an offline AI-based screening algorithm, they were misinterpreted as diabetic retinopathy and made up roughly 2% of the total false positives within the study.74 This emphasizes the importance to address the presence of refractory ABs in future software development. One solution may be to include a spectrum of AH fundus imaging within the training dataset of AI-algorithms, but this may be challenging due to the low overall prevalence, wide range of AB densities and morphologies, and ongoing big data issues with patient data protection and confidentiality.15 Another solution could be to develop ancillary technology to “clean up” induced artifacts, as demonstrated by Yoo et al75 in an analysis of the CycleGAN model which was able to at least reduce some amount of media haze induced by mild AH.
Telemedicine is another developing area of interest that may have bearing on patients with AH. Currently there are on-going efforts to develop technologies and modalities for monitoring and even treating retinal conditions remotely.76 It will be interesting to evaluate whether remote imaging is feasible and able to perform comparably to in-office fundus evaluation for patients with conditions such as AH, where imaging is inherently prone to artifactual distortion. Specifically, home OCT is one of the promising technologies that may ultimately allow for overall less in in-person office visits,77 even in the presence of AH. As prior studies have shown that artifactual distortion of ABs can be minimized with in-office OCT,34 the potential to produce similar high quality images at home is promising. It remains unclear whether this can be done without the help of a trained technician. To our knowledge, there have been no studies specifically including AH eyes in evaluation of home OCT technologies, so further evaluation is needed to assess the varying image quality in this group with potential areas for technological improvements including a built in “auto-adjust” feature which can autonomously modify saturation settings in order to minimize artifacts, as previously described in the office setting.
It will also be interesting to observe changes in practice patterns for the management of AH as remote technologies become available. We suspect the trend thus far has been less frequent vitrectomy for monitoring and treating posterior pathology in eyes with AH, favoring improved in-office imaging techniques and intravitreal injections. However, there may reasonably be a shift back to vitrectomy in AH patients who are geographically remote or otherwise unable to be seen regularly in a clinic setting. In these scenarios, an initial vitrectomy could open the door for telemedicine by augmenting the ability of home imaging modalities to remotely monitor conditions such as diabetic retinopathy and potentially even provide an opportunity to perform tele-photocoagulation78 if needed.
Conclusions
In conclusion, asteroid hyalosis is a benign clinical entity characterized by multiple refractile spherical calcium and phospholipids within the vitreous. Prevalence rates are around 1% (ranging from 0.3–2.0%) and there is a strong association with older age. While the etiology remains unclear, there is growing evidence pointing towards a degenerative component to the pathogenesis of AH based on histopathologic data as well as multiple suggested systemic risk factors associated with metabolic and coronary dysfunction.
Clinical management of AH begins with careful evaluation and exclusion of more ominous conditions such as ocular lymphoma or amyloidosis. Vitrectomy is rarely required, typically in cases of symptomatic visual disturbance or when there is a limited view of the fundus and the need to perform PRP. Modern multi-modal imaging approaches and treatment options of retinal pathology have decreased the need for vitrectomy in patients with asymptomatic AH. Specific considerations should be made in planning cataract surgery in the setting of AH due to potential inaccurate calculations and post-operative calcification in silicone IOLs. Silicone lenses should be avoided in patients with AH due to the risk of post-operative calcification which may require further surgeries. As AI-based image analysis, remote imaging, and telemedicine practices continue to grow, further research is needed to consider potential impacts and limitations of these technologies in AH eyes.
Disclosure
Dr Yevgeniy Shildkrot was previously employed by Genetech/Roche (this research was done outside of that role) and reports no conflicts of interest presented in this work. The authors report no other conflicts of interest in this work.
References
- 1.Wand M, Smith TR, Cogan DG. Cholesterosis bulbi: the ocular abnormality known as synchysis scintillans. Am J Ophthalmol. 1975;80(2):177–183. doi: 10.1016/0002-9394(75)90129-4 [DOI] [PubMed] [Google Scholar]
- 2.Mishra C, Tripathy K. Asteroid Hyalosis. StatPearls; 2022. [PubMed] [Google Scholar]
- 3.Benson A. Diseases of the vitreous: a case of monocular asteroid hyalitis. Ophthalmol Soc. 1976;14(416):101–104. [Google Scholar]
- 4.Khoshnevis M, Rosen S, Sebag J. Asteroid hyalosis-a comprehensive review. Surv Ophthalmol. 2019;64(4):452–462. doi: 10.1016/j.survophthal.2019.01.008 [DOI] [PubMed] [Google Scholar]
- 5.Winkler J, Lünsdorf H. Ultrastructure and composition of asteroid bodies. Invest Ophthalmol Vis Sci. 2001;42(5):902–907. [PubMed] [Google Scholar]
- 6.Bergren RL, Brown GC, Duker JS. Prevalence and association of asteroid hyalosis with systemic diseases. Am J Ophthalmol. 1991;111(3):289–293. doi: 10.1016/s0002-9394(14)72311-6 [DOI] [PubMed] [Google Scholar]
- 7.Kim JH, Roh MI, Byeon SH, Koh HJ, Lee SC, Kwon OW. Prevalence of and risk factors for asteroid hyalosis in Seoul, Korea. Retina. 2008;28(10):1515–1521. doi: 10.1097/iae.0b013e318185ea3c [DOI] [PubMed] [Google Scholar]
- 8.Mitchell P, Wang MY, Wang JJ. Asteroid hyalosis in an older population: the Blue Mountains Eye Study. Ophthalmic Epidemiol. 2003;10(5):331–335. doi: 10.1076/opep.10.5.331.17324 [DOI] [PubMed] [Google Scholar]
- 9.Elbaz H, Schuster AK, Nickels S, et al. Epidemiologic analysis of asteroid hyalosis and associations: the Gutenberg Health Study. Ophthalmology. 2021;128(2):328–330. doi: 10.1016/j.ophtha.2020.07.008 [DOI] [PubMed] [Google Scholar]
- 10.Duong R, Cai X, Ambati N, Shildkrot Y, Sieburth R. Prevalence of asteroid hyalosis and systemic risk factors in United States adults. Eye. 2022. doi: 10.1038/s41433-022-02214-z 37 1678–1682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang C, Shao L, Dong L, Da Zhou W, Zhang RH, Wei W. Prevalence and associations of asteroid hyalosis: the Beijing Eye Study. BMC Ophthalmol. 2022;22(1):360. doi: 10.1186/s12886-022-02586-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fawzi AA, Vo B, Kriwanek R, et al. Asteroid hyalosis in an autopsy population: the University of California at Los Angeles (UCLA) experience. Arch Ophthalmol. 2005;123(4):486–490. doi: 10.1001/archopht.123.4.486 [DOI] [PubMed] [Google Scholar]
- 13.Moss SE, Klein R, Klein BE. Asteroid hyalosis in a population: the Beaver Dam eye study. Am J Ophthalmol. 2001;132(1):70–75. doi: 10.1016/s0002-9394(01)00936-9 [DOI] [PubMed] [Google Scholar]
- 14.Malerbi FK, Dal Fabbro AL, Moises RCS, Vieira Filho JPB, Franco LJ. High frequency of asteroid hyalosis precludes diabetic retinopathy screening with smartphone-based retinal camera in Brazilian Xavante Indians. J Diabetes Sci Technol. 2020;14(5):974–975. doi: 10.1177/1932296820929673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng C-Y, Da Soh Z, Majithia S, et al. Big data in ophthalmology. Asia-Pacific J Ophthalmol. 2020;9(4):291–298. doi: 10.1097/APO.0000000000000304 [DOI] [PubMed] [Google Scholar]
- 16.Mather M, Jacobsen L, Pollard M. Aging in the United States. Popul Bull. 2015;70(2):245. [Google Scholar]
- 17.Møller-Lorentzen TB, Eckmann-Hansen C, Faber C, Larsen M, Subhi Y. Global prevalence of asteroid hyalosis and projection of its future burden: a systematic review and meta-analysis. Acta Ophthalmol. 2020;98(8):755–762. doi: 10.1111/aos.14465 [DOI] [PubMed] [Google Scholar]
- 18.Anderson WBJ, Anderson WB. Asteroid hyalitis: a study of serum calcium levels in affected patients. South Med J. 1965;58:191–194. doi: 10.1097/00007611-196502000-00010 [DOI] [PubMed] [Google Scholar]
- 19.Hatfield RE, Gastineau CF, Rucker CW. Asteroid bodies in the vitreous: relationship to diabetes and hypercholesterolemia. Proc Staff Meet Mayo Clin. 1962;37:513–514. [PubMed] [Google Scholar]
- 20.Ikeda Y, Hisatomi T, Murakami Y, et al. Retinitis pigmentosa associated with asteroid hyalosis. Retina. 2010;30(8):1278–1281. doi: 10.1097/IAE.0b013e3181dcfc0a [DOI] [PubMed] [Google Scholar]
- 21.Dev Borman A, Ocaka LA, Mackay DS, et al. Early onset retinal dystrophy due to mutations in LRAT: molecular analysis and detailed phenotypic study. Invest Ophthalmol Vis Sci. 2012;53(7):3927–3938. doi: 10.1167/iovs.12-9548 [DOI] [PubMed] [Google Scholar]
- 22.Fantin A, Summers CG, Cameron JD. Neonatal asteroid hyalosis. J AAPOS. 1998;2(4):253–254. doi: 10.1016/s1091-8531(98)90061-1 [DOI] [PubMed] [Google Scholar]
- 23.Verhoeff FH. Microscopic findings in a case of asteroid hyalitis. Am J Ophthalmol. 1921;4(3):155–160. doi: 10.5555/uri:pii:S0002939421911279 [DOI] [Google Scholar]
- 24.Rodman HI, Johnson FB, Zimmerman LE. New histopathological and histochemical observations concerning asteroid hyalitis. Arch Ophthalmol. 1961;66(4):552–563. doi: 10.1001/archopht.1961.00960010554019 [DOI] [PubMed] [Google Scholar]
- 25.Topilow HW, Kenyon KR, Takahashi M, Freeman HM, Tolentino FI, Hanninen LA. Asteroid hyalosis. Biomicroscopy, ultrastructure, and composition. Arch Ophthalmol. 1982;100(6):964–968. doi: 10.1001/archopht.1982.01030030972015 [DOI] [PubMed] [Google Scholar]
- 26.March WF, Shoch D. Electron diffraction study of asteroid bodies. Invest Ophthalmol. 1975;14(5):399–400. [PubMed] [Google Scholar]
- 27.Streeten BW. Vitreous asteroid bodies. Ultrastructural characteristics and composition. Arch Ophthalmol. 1982;100(6):969–975. doi: 10.1001/archopht.1982.01030030977016 [DOI] [PubMed] [Google Scholar]
- 28.Komatsu H, Kamura Y, Ishi K, Kashima Y. Fine structure and morphogenesis of asteroid hyalosis. Med electron Microsc. 2003;36(2):112–119. doi: 10.1007/s00795-002-0211-y [DOI] [PubMed] [Google Scholar]
- 29.Kador PF, Wyman M. Asteroid hyalosis: pathogenesis and prospects for prevention. Eye. 2008;22(10):1278–1285. doi: 10.1038/eye.2008.35 [DOI] [PubMed] [Google Scholar]
- 30.Rani PK, Prajapati RC. Role of OCT angiography in the detection of retinal vascular and macular abnormalities in subjects with asteroid hyalosis. Semin Ophthalmol. 2018:1–5. doi: 10.1080/08820538.2018.1551497 [DOI] [PubMed] [Google Scholar]
- 31.Marlow E, Mikhail M, Faia L, Garretson B. Acute decreased vision in asteroid hyalosis due to posterior vitreous separation. Invest Ophthalmol Vis Sci. 2019;60(9):5782. [Google Scholar]
- 32.Kumar S. Cholesterol crystals in the anterior chamber. Br J Ophthalmol. 1963;47(5):295–299. doi: 10.1136/bjo.47.5.295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brodsky MC. Synchysis scintillans in a child. JAMA Ophthalmol. 2015;133(7):e150793–e150793. doi: 10.1001/jamaophthalmol.2015.0793 [DOI] [PubMed] [Google Scholar]
- 34.Hwang JC, Barile GR, Schiff WM, et al. Optical coherence tomography in asteroid hyalosis. Retina. 2006;26(6):661–665. doi: 10.1097/01.iae.0000224502.33905.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dammacco R, Merlini G, Lisch W, et al. Amyloidosis and ocular involvement: an overview. Semin Ophthalmol. 2020;35(1):7–26. doi: 10.1080/08820538.2019.1687738 [DOI] [PubMed] [Google Scholar]
- 36.Kawaji T, Ando Y, Hara R, Tanihara H. Novel therapy for transthyretin-related ocular amyloidosis: a pilot study of retinal laser photocoagulation. Ophthalmology. 2010;117(3):552–555. doi: 10.1016/j.ophtha.2009.07.042 [DOI] [PubMed] [Google Scholar]
- 37.AAO. Retina and vitreous. In: Basic and Clinical Science Course. AAO; 2022. [Google Scholar]
- 38.Coupland SE, Damato B. Understanding intraocular lymphomas. Clin Experiment Ophthalmol. 2008;36(6):564–578. doi: 10.1111/j.1442-9071.2008.01843.x [DOI] [PubMed] [Google Scholar]
- 39.Scott DAR, Møller-Lorentzen TB, Faber C, Wied J, Grauslund J, Subhi Y. Spotlight on asteroid hyalosis: a clinical perspective. Clin Ophthalmol. 2021;15:2537–2544. doi: 10.2147/OPTH.S272333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noda S, Hayasaka S, Setogawa T. Patients with asteroid hyalosis and visible floaters. Jpn J Ophthalmol. 1993;37(4):452–455. [PubMed] [Google Scholar]
- 41.Lambrou FHJ, Sternberg PJ, Meredith TA, Mines J, Fine SL. Vitrectomy when asteroid hyalosis prevents laser photocoagulation. Ophthalmic Surg. 1989;20(2):100–102. [PubMed] [Google Scholar]
- 42.Yokoyama S, Kojima T, Kaga T, Ichikawa K. Increased internal higher-order aberrations as a useful parameter for indication of vitrectomy in three asteroid hyalosis cases. BMJ Case Rep. 2015; 2015:bcr2015211704. doi: 10.1136/bcr-2015-211704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sato T, Koh S, Mori R, Korehisa H, Hayashi K. Impact of asteroid hyalosis on internal higher-order aberrations in eyes with cataract accompanied by acoustic shadows on swept-source optical coherence tomography examination. J Cataract Refract Surg. 2020;46(12):e1–e4. doi: 10.1097/j.jcrs.0000000000000303 [DOI] [PubMed] [Google Scholar]
- 44.Parnes RE, Zakov ZN, Novak MA, Rice TA. Vitrectomy in patients with decreased visual acuity secondary to asteroid hyalosis. Am J Ophthalmol. 1998;125(5):703–704. doi: 10.1016/s0002-9394(98)00031-2 [DOI] [PubMed] [Google Scholar]
- 45.Yamaguchi T, Inoue M, Ishida S, Shinoda K. Detecting vitreomacular adhesions in eyes with asteroid hyalosis with triamcinolone acetonide. Graefes Arch Clin Exp Ophthalmol. 2007;245(2):305–308. doi: 10.1007/s00417-005-0236-8 [DOI] [PubMed] [Google Scholar]
- 46.Ikeda T, Sawa H, Koizumi K, Yasuhara T, Kinoshita S, Tano Y. Vitrectomy for proliferative diabetic retinopathy with asteroid hyalosis. Retina. 1998;18(5):410–414. doi: 10.1097/00006982-199805000-00004 [DOI] [PubMed] [Google Scholar]
- 47.Mochizuki Y, Hata Y, Kita T, et al. Anatomical findings of vitreoretinal interface in eyes with asteroid hyalosis. Graefes Arch Clin Exp Ophthalmol. 2009;247(9):1173–1177. doi: 10.1007/s00417-009-1095-5 [DOI] [PubMed] [Google Scholar]
- 48.Hampton GR, Nelsen PT, Hay PB. Viewing through the asteroids. Ophthalmology. 1981;88(7):669–672. doi: 10.1016/s0161-6420(81)34969-0 [DOI] [PubMed] [Google Scholar]
- 49.Belenje A, Rani PK. Role of wide-angle optical coherence tomography angiography in detection of proliferative diabetic retinopathy in a patient with dense asteroid hyalosis. BMJ Case Rep. 2020;13(9). doi: 10.1136/bcr-2020-237248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Motiani MV, McCannel CA, Almanzor R, McCannel TA. Diagnosis of choroidal melanoma in dense asteroid hyalosis. Semin Ophthalmol. 2017;32(2):257–259. doi: 10.3109/08820538.2015.1053627 [DOI] [PubMed] [Google Scholar]
- 51.Gross JG, Glassman AR, Liu D, et al. Five-year outcomes of panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136(10):1138–1148. doi: 10.1001/jamaophthalmol.2018.3255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Azad AD, Chen EM, Hinkle J, et al. Anti-vascular endothelial growth factor and panretinal photocoagulation use after protocol S for proliferative diabetic retinopathy. Ophthalmol Retin. 2021;5(2):151–159. doi: 10.1016/j.oret.2020.07.018 [DOI] [PubMed] [Google Scholar]
- 53.Wong SCK, Sampath R. Erroneous automated refraction in a case of asteroid hyalosis. J Cataract Refract Surg. 2002;28(9):1707–1708. doi: 10.1016/s0886-3350(01)01224-x [DOI] [PubMed] [Google Scholar]
- 54.Allison KL, Price J, Odin L. Asteroid hyalosis and axial length measurement using automated biometry. J Cataract Refract Surg. 1991;17(2):181–186. doi: 10.1016/s0886-3350(13)80248-9 [DOI] [PubMed] [Google Scholar]
- 55.Martin RG, Safir A. Asteroid hyalosis affecting the choice of intraocular lens implant. J Cataract Refract Surg. 1987;13(1):62–65. doi: 10.1016/s0886-3350(87)80014-7 [DOI] [PubMed] [Google Scholar]
- 56.Hartstein I, Barke RM. Axial length measurement discrepancies in asteroid hyalosis. Br J Ophthalmol. 1991;75(3):191. doi: 10.1136/bjo.75.3.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Erkin EF, Tarhan S, Oztürk F. Axial length measurement and asteroid hyalosis. J Cataract Refract Surg. 1999;25(10):1400–1403. doi: 10.1016/S0886-3350(99)00214-X [DOI] [PubMed] [Google Scholar]
- 58.Moshirfar M, Martin DJ, Jensen JL, Payne CJ. Light adjustable intraocular lenses: an updated platform for cataract surgery. Curr Opin Ophthalmol. 2023;34(1):78–83. doi: 10.1097/ICU.0000000000000911 [DOI] [PubMed] [Google Scholar]
- 59.Ochi R, Sato B, Morishita S, et al. Case of asteroid hyalosis that developed severely reduced vision after cataract surgery. BMC Ophthalmol. 2017;17(1):68. doi: 10.1186/s12886-017-0467-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Doshi S, Pathengay A, Sane S, Saldanha M. Asteroid hyalosis prolapse in the anterior chamber after cataract surgery. BMJ Case Rep. 2019;12(4). doi: 10.1136/bcr-2019-230076 e230076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stringham J, Werner L, Monson B, Theodosis R, Mamalis N. Calcification of different designs of silicone intraocular lenses in eyes with asteroid hyalosis. Ophthalmology. 2010;117(8):1486–1492. doi: 10.1016/j.ophtha.2009.12.032 [DOI] [PubMed] [Google Scholar]
- 62.Espandar L, Mukherjee N, Werner L, Mamalis N, Kim T. Diagnosis and management of opacified silicone intraocular lenses in patients with asteroid hyalosis. J Cataract Refract Surg. 2015;41(1). 222–225 doi: 10.1016/j.jcrs.2014.11.009 [DOI] [PubMed] [Google Scholar]
- 63.Leysen I, Bartholomeeusen E, Coeckelbergh T, Tassignon M. Surgical outcomes of intraocular lens exchange: five-year study. J Cataract Refract Surg. 2009;35(6). 1013–1018 doi: 10.1016/j.jcrs.2009.01.024 [DOI] [PubMed] [Google Scholar]
- 64.Lee YJ, Han SB. Laser treatment of silicone intraocular lens opacification associated with asteroid hyalosis. Taiwan J Ophthalmol. 2019;9(1):49–52. doi: 10.4103/tjo.tjo_65_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mehta N, Goldberg RA, Shah CP. Treatment of dystrophic calcification on a silicone intraocular lens with pars plana vitrectomy. Clin Ophthalmol. 2014;8:1291–1293. doi: 10.2147/OPTH.S62108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ullman DI, Gupta S. Pars plana vitrectomy for dystrophic calcification of a silicone intraocular lens in association with asteroid hyalosis. J Cataract Refract Surg. 2014;40(7):1228–1231. doi: 10.1016/j.jcrs.2014.04.022 [DOI] [PubMed] [Google Scholar]
- 67.Rainsbury PG, Lochhead J. Pars plana vitrectomy for posterior surface calcification in a silicone intraocular lens in asteroid hyalosis - a report of mistaken identity? Clin Ophthalmol. 2014;8:2239–2241. doi: 10.2147/OPTH.S74532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Platt SM, Iezzi R, Mahr MA, Erie JC. Surgical removal of dystrophic calcification on a silicone intraocular lens in association with asteroid hyalosis. J Cataract Refract Surg. 2017;43(12). 1608–1610 doi: 10.1016/j.jcrs.2017.09.026 [DOI] [PubMed] [Google Scholar]
- 69.Ambati NR, Duong RT, Zhang A, Shildkrot Y. Mechanical removal of calcifications on a silicone intraocular lens with a shielded light pipe in asteroid hyalosis. J Ophthalmic Surg. 2022;5(1):82–84. doi: 10.36959/587/607 [DOI] [Google Scholar]
- 70.Zapata MA, Royo-Fibla D, Font O, et al. Artificial intelligence to identify retinal fundus images, quality validation, laterality evaluation, macular degeneration, and suspected glaucoma. Clin Ophthalmol. 2020;14:419–429. doi: 10.2147/OPTH.S235751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Grzybowski A, Brona P, Lim G, et al. Artificial intelligence for diabetic retinopathy screening: a review. Eye. 2020;34(3):451–460. doi: 10.1038/s41433-019-0566-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ipp E, Liljenquist D, Bode B, et al. Pivotal evaluation of an artificial intelligence system for autonomous detection of referrable and vision-threatening diabetic retinopathy. JAMA Netw Open. 2021;4(11):e2134254–e2134254. doi: 10.1001/jamanetworkopen.2021.34254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shi C, Lee J, Wang G, Dou X, Yuan F, Zee B. Assessment of image quality on color fundus retinal images using the automatic retinal image analysis. Sci Rep. 2022;12(1):10455. doi: 10.1038/s41598-022-13919-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jain A, Krishnan R, Rogye A, Natarajan S. Use of offline artificial intelligence in a smartphone-based fundus camera for community screening of diabetic retinopathy. Indian J Ophthalmol. 2021;69(11):3150–3154. doi: 10.4103/ijo.IJO_3808_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yoo TK, Choi JY, Kim HK. CycleGAN-based deep learning technique for artifact reduction in fundus photography. Graefes Arch Clin Exp Ophthalmol. 2020;258(8):1631–1637. doi: 10.1007/s00417-020-04709-5 [DOI] [PubMed] [Google Scholar]
- 76.Chee R-I, Darwish D, Fernandez-Vega A, et al. Retinal telemedicine. Curr Ophthalmol Rep. 2018;6(1):36–45. doi: 10.1007/s40135-018-0161-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim JE, Tomkins-Netzer O, Elman MJ, et al. Evaluation of a self-imaging SD-OCT system designed for remote home monitoring. BMC Ophthalmol. 2022;22(1):261. doi: 10.1186/s12886-022-02458-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen H, Pan X, Yang J, et al. Application of 5G technology to conduct real-time teleretinal laser photocoagulation for the treatment of diabetic retinopathy. JAMA Ophthalmol. 2021;139(9):975–982. doi: 10.1001/jamaophthalmol.2021.2312 [DOI] [PMC free article] [PubMed] [Google Scholar]