Abstract
Objective
Electronic health records (EHRs) within the United States increasingly include sexual orientation and gender identity (SOGI) fields. We assess how well SOGI fields, along with International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) codes and medication records, identify gender-expansive patients.
Materials and Methods
The study used a data set of all patients that had in-person inpatient or outpatient encounters at an academic medical center in a rural state between December 1, 2018 and February 17, 2022. Chart review was performed for all patients meeting at least one of the following criteria: differences between legal sex, sex assigned at birth, and gender identity (excluding blank fields) in the EHR SOGI fields; ICD-10 codes related to gender dysphoria or unspecified endocrine disorder; prescription for estradiol or testosterone suggesting use of gender-affirming hormones.
Results
Out of 123 441 total unique patients with in-person encounters, we identified a total of 2236 patients identifying as gender-expansive, with 1506 taking gender-affirming hormones. SOGI field differences or ICD-10 codes related to gender dysphoria or both were found in 2219 of 2236 (99.2%) patients who identify as gender-expansive, and 1500 of 1506 (99.6%) taking gender-affirming hormones. For the gender-expansive population, assigned female at birth was more common in the 12–29 year age range, while assigned male at birth was more common for those 40 years and older.
Conclusions
SOGI fields and ICD-10 codes identify a high percentage of gender-expansive patients at an academic medical center.
Keywords: gender identity, medical informatics, pathology, population health, sex, transgender
BACKGROUND AND SIGNIFICANCE
Achieving health equity requires information systems that document and identify marginalized groups. In recent years, sexual orientation and gender identity (SOGI) demographic fields have been integrated into major electronic health record (EHR) packages in the United States.1–4 This integration allows for providers, receptionists, and/or patients to list sexual orientation, legal sex, sex assigned at birth (SAAB), and gender identity (GI) within individual patient charts. Access to this information empowers providers to tailor their clinical care as applicable to sexual and gender minority groups. Additionally, it allows providers to have access to preferred pronouns and name, which is a baseline requirement in developing a respectful patient/provider relationship. Other functionality can include anatomical/organ inventory and presence of intersex/differences in sexual differentiation.5–7
There are, however, potential risks to patients to providing SOGI information that will be recorded in the EHR and thus potentially viewed by anyone who accesses the patient record.8–10 Common negative experiences cited by patients include bias, discrimination, and disparaging comments from healthcare providers.8,9,11 Privacy of adolescents represents an additional concern in terms of parent/guardian access to the child’s medical information when parents/guardians do not support the child’s GI or sexual orientation.11,12
GI is an internal sense of being a man, woman, or somewhere between.13 Gender expression is how a person chooses to use their outward appearances to convey their gender. In contrast, SAAB is chromosomally defined and directly related to the external genitalia and/or reproductive organs a person was born with. In the United States, SOGI information is often missing in population surveys and identity documents.14,15 For example, sexual orientation, SAAB, and GI information are not currently collected in the American Community Survey used to define the US Census.15 Motor vehicle bureaus in some states in the United States have added an additional option such as “X” for sex but nothing else specific for SAAB and GI.16 The process for and ability to officially change sex on identity documents varies among US states, with some states not allowing this and others requiring gender-affirming treatment such as hormones and/or sex reassignment surgery.16 Not surprisingly, prevalence estimates of gender-expansive people vary by more than 10-fold between studies, and the most comprehensive studies to date have significant limitations.3,17–26
The introduction of SOGI fields in health records is a pivotal step toward normalizing gender diversity and promoting inclusivity in clinical care.2,27–29 Additionally, SOGI fields offer a tool for researchers to retrospectively identify cohorts for population studies, public health initiatives, and predictive analytics. To appropriately analyze the retrieved data, the SOGI tools should be validated to understand their specific limitations including overall compliance and error rate.10,23,30
The primary objective of this study was to validate SOGI data for GI and SAAB at a large academic medical center using extensive chart review. A secondary objective was to approximate the prevalence of gender-expansive people who seek healthcare (including gender-affirming hormones and surgery) in a midwestern city.
MATERIALS AND METHODS
The study was conducted at the University of Iowa Hospitals and Clinics (UIHC), an 860-bed tertiary/quaternary care academic medical center that includes inpatient, emergency department, and outpatient services, as well as inpatient and outpatient services at the 190-bed University of Iowa Stead Family Children’s Hospital. UIHC has pediatric and adult Lesbian, Gay, Bisexual, Transgender, Queer, and Questioning (LGBTQ) clinics. The EHR for UIHC has been Epic (Epic Systems, Inc., Madison, WI, USA) since 2009. The institution adopted the tethered patient portal (Epic MyChart) in 2010.31 Patients can obtain their own MyChart account at age 12, with restricted parent/guardian access starting at age 14. Functionality for SOGI fields in the UIHC EHR became available in December 2018.
Study design and data retrieval
The data in this study were collected as part of a retrospective study approved by the University of Iowa Institutional Review Board (protocol #202202388) covering the timeframe from December 1, 2018 to February 17, 2022. During the retrospective analysis timeframe, the EHR allowed for 3 options for Legal Sex (Male, Female, Unknown) as a mandatory field. Patients could voluntarily select from 6 options for SAAB and 7 options for GI or leave either or both of these fields blank (Table 1). The total number of possible combinations for Legal Sex, SAAB, and GI (including SAAB and/or GI being left blank) is 168.
Table 1.
Choices available for gender and sex in the sexual orientation/gender identity (SOGI) data fields
| Legal sex | Sex assigned at birth | Gender identity |
|---|---|---|
| Female | Female | Female |
| Male | Male | Male |
| Unknown | Choose not to disclose | Nonbinary |
| Not recorded on birth certificate | Other | |
| Uncertain | Transgender female/male to female | |
| Unknown | Transgender male/female to male | |
| [Blank] | Choose not to disclose | |
| [Blank] |
Note: Legal sex cannot be selected directly by patient; any changes in legal sex required documentation and review under hospital policy. Sex assigned at birth and gender identity can be left blank, whereas legal sex must be 1 of the 3 options. There is option to auto-fill sex assigned at birth and gender identity by selecting either cisgender female or cisgender male. This option will match sex assigned at birth and gender identity to the legal sex currently in the system for the patient.
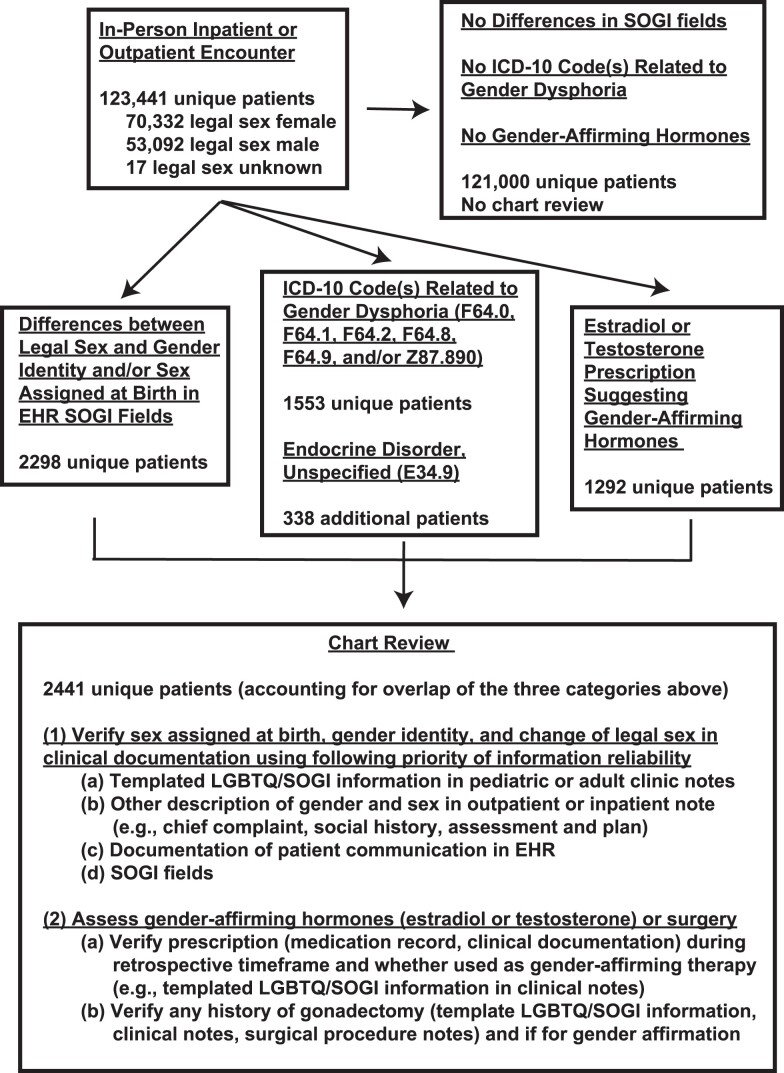
The flow diagram for data retrieval and analysis is shown in Figure 1. The data set for SOGI field analysis was an export of all patients with a completed in-person inpatient or outpatient encounter within the UIHC system between December 18, 2018 and February 17, 2022. This consisted of 123 441 unique patients (70 332 with legal sex of female, 53 092 male, 17 unknown; mean age 48.2 years, standard deviation 22.0 years; 116 897 were 12 years or older). Data retrieval was performed by the UIHC Health Care Information Systems Reporting and Analytics team. This retrieved data on Legal Sex, SAAB, and GI for patients who met the inclusion criteria as of February 17, 2022. Within this total data set, 2298 patients had nonblank response(s) for SAAB and/or GI in the SOGI fields that were different from Legal Sex (eg, Legal Sex of “Male” and Gender Identity of “Transgender female” or Legal Sex of “Female” and SAAB of “Male”). This group of 2298 patients was considered as having “SOGI field differences” for the purposes of the study (Figure 1). Blank responses were ignored in identifying SOGI field differences (eg, Legal Sex of “Male,” SAAB left blank, and GI of “Male” would be considered as having no field differences).
Figure 1.
Flow diagram of data sources and analysis. A total of 123 441 unique patients had in-person encounters within the retrospective timeframe of the study: 2298 had differences in the EHR SOGI fields; 1891 had one or more encounters associated with an ICD-10 code related to gender dysphoria or unspecified endocrine disorder; and 1292 had estradiol or testosterone prescription suggesting gender-affirming hormones. All these data sources were obtained using EHR reporting tools. Chart review using the information described was performed on the 2441 unique patients resulting from overlap of the 3 broad data sources (SOGI fields, ICD-10 codes, prescriptions). Chart review was not performed for the remaining 121 000 unique patients who did not meet any of the categories above. EHR: electronic health record; LGBTQ: lesbian, gay, bisexual, transgender, queer, and questioning; SOGI: sexual orientation/gender identity.
We performed 2 additional searches to identify gender-expansive patients. An Epic Reporting Workbench search31 retrieved patients with specific International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) codes32 assigned for a clinical encounter during the retrospective timeframe of the study: F64.0 (GI disorder in adolescence and adulthood), F64.1 (dual-role transvestism), F64.2 (GI disorder of childhood), F64.8 (other GI disorders), F64.9 (GI disorder, unspecified), and Z87.890 (personal history of sex reassignment). For simplicity, we refer to these 6 codes (F64.0, F64.1, F64.2, F64.8, F64.9, and Z87.890) as “ICD-10 codes related to gender dysphoria.” The data retrieval identified 1553 patients (934 with legal sex of female, 616 male, 3 unknown; mean age 25.8 years, standard deviation 11.5 years), of which 1429 had SOGI field differences (ie, 124 had presumptively cisgender SOGI profiles, including those who did not provide response for GI or SAAB) (Figure 1). We also searched for the ICD-10 code E34.9 (endocrine disorder, unspecified), as this code was sometimes instead of ICD-10 codes related to gender dysphoria. ICD-10 code E34.9 was used in 1480 patients in our data set, although 1407 of these had either SOGI field differences in the EHR or ICD-10 codes related to gender dysphoria or both.
We also performed a search for patients that were potentially prescribed gender-affirming (estradiol or testosterone) hormones based on legal sex (ie, estradiol for Legal Sex of “Male”; testosterone for Legal Sex of “Female”). These included all formulations of estradiol and testosterone used in our system’s medication database for gender-affirming therapy. The estradiol search identified 483 patients, while the testosterone search identified 809 patients. Overlap of the 3 searches (SOGI field differences, ICD-10 codes, prescription for estradiol or testosterone suggesting use of gender-affirming hormones) yielded 2441 unique patients whose charts were reviewed (Figure 1).
Chart review
Detailed chart review included assessment for gender-affirming therapy within or prior to the retrospective analysis timeframe that would impact hormonal levels (eg, estradiol, testosterone, puberty blockers, bilateral gonadectomy) and for documentation within the EHR indicating that the patient identified broadly within the gender-expansive umbrella. Chart review involved 2 reviewers, with an additional reviewer used for rare cases with uncertain information.
Figure 1 illustrates the hierarchical preference of the information used in chart review to verify SAAB, GI, and gender-affirming care. Our institution has developed and promoted LGBTQ and SOGI information templates in the EHR for use in pediatric and adult clinical notes. These are widely used for those seeking gender-affirming care at our institution. These templates include fields that provider can fill in for SAAB, current legal sex, GI, sexual orientation, preferred name, and preferred pronouns. More detailed templates for transgender/nonbinary-identifying patients include fields for gender-affirming hormones (type and date started), transition-related surgeries/procedures, and goals of transitions. In cases where these templates were not available in the charts for those reviewed, additional documentation in the EHR was reviewed including outpatient or inpatient notes, documentation of patient communications logged into the EHR, prescription medical records (medical administration record, documentation of prescription medications in clinical notes, medication information from EHR reporting tools). We also reviewed free text responses by patients who selected “Other” in the EHR SOGI field for GI (which allowed for additional detail). Free text responses by patients indicative of gender-expansive identity included the following along with any easily interpreted spelling variants: “agender,” “demiboy,” “demigirl,” “fluid,” “gender atypical,” “gender fluid,” “gender nonconforming,” “gender queer,” “questioning,” “they/them” (or preferences for other pronouns different from he/him or she/hers that would be associated with their SAAB), “transfeminine,” and “transmasculine.”
RESULTS
Overall use of SOGI fields
We utilized a data set consisting of 123 441 unique patients with 1 or more in-person clinical encounter(s) within the UIHC system between December, 18, 2018 and February 17, 2022. In this data set, 35.3% of patients provided a response for SAAB and 37.3% for GI, with lower response rates at younger ages (Table 2). SOGI field response rates were higher for the 1553 patients with ICD-10 codes related to gender dysphoria (89.1% for SAAB, 93.6% for GI; Table 2).
Table 2.
Usage of sex assigned at birth and gender identity fields by age category
| SOGI field use, n (%) | Legal sex | Sex assigned at birth | Gender identity |
|---|---|---|---|
| In-person outpatient or inpatient encounter(s) December 2018–February 2022 (N = 123 441) | |||
| All ages | 123 441 (100%) | 43 607 (35.3%) | 46 103 (37.3%) |
| 12+ years old | 116 984 (100%) | 43 538 (37.2%) | 45 996 (39.3%) |
| <12 years old | 6547 (100%) | 69 (1.1%) | 107 (1.6%) |
| 12–17 years old | 6177 (100%) | 1732 (28.0%) | 1631 (26.4%) |
| ICD-10CM diagnosis codes related to gender dysphoria (N = 1553) | |||
| All ages | 1553 (100%) | 1384 (89.1%) | 1454 (93.6%) |
| 12+ years old | 1522 (100%) | 1366 (89.8%) | 1435 (94.3%) |
| <12 years old | 31 (100%) | 18 (58.1%) | 19 (61.3%) |
| 12–17 years old | 349 (100%) | 268 (76.8%) | 301 (86.2%) |
Note: Sex assigned at birth and gender identity can be left blank, whereas legal sex must be female, male, or unknown. The ICD-10CM codes related to gender dysphoria are: F64.0, F64.1, F64.2, F64.8, F64.9, and Z87.890.
Abbreviations: ICD-10CM: International Statistical Classification of Diseases and Related Health Problems, 10th Revision codes and medication; SOGI: sexual orientation/gender identity.
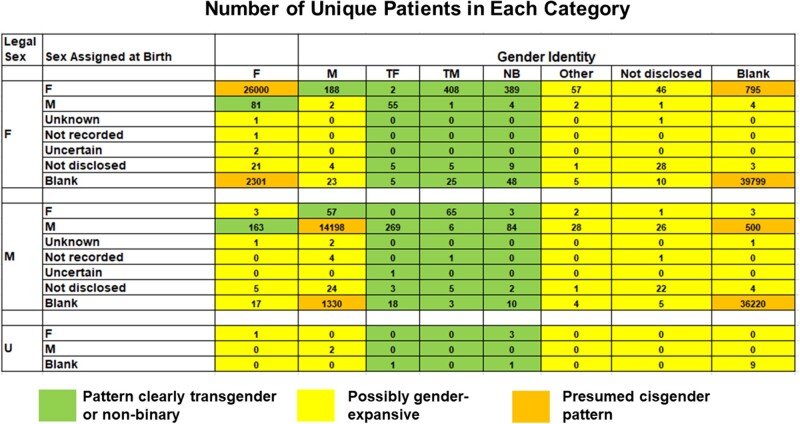
Figure 2 shows the distribution of the number of patients for all the possible combinations of Legal Sex, SAAB, and GI (including SAAB and/or GI left blank) in the data set of 123 441 patients (note that some rows are not included as no patients were found in any categories within those rows). Figure 2 is color-coded to show combinations that are presumed cisgender in the absence of other evidence (orange), high likelihood of being gender-expansive (green; includes GI of “Transgender Female,” “Transgender Male,” or “Nonbinary,” as well as combinations of “Male” and “Female” that differed between the SOGI fields), and possibly gender-expansive (yellow; includes responses such as “Choose Not to Disclose” or “Other” for GI). Out of 168 possible combinations (including SAAB and/or GI being blank), 88 combinations were not seen in the data. For infrequent combinations, 60 combinations were only seen in 5 or fewer unique patients each. The 2 most common combinations were those in which both SAAB and GI were left blank (N = 39 799 with Legal Sex of “Female”; N = 36 220 with Legal Sex of “Male”).
Figure 2.
Distribution of numbers of unique patients (out of 123 441 total) who selected various combinations for Legal Sex, Sex Assigned at Birth, and Gender Identity. Out of 168 possible combinations, 88 combinations did not occur in the data set. Four of the possibilities for Sex Assigned at Birth were not seen for any patients with Legal Sex of “Unknown”; thus, those rows are not shown. The colored boxes indicate categories that were predicted to be high likelihood of being gender-expansive (green), possibly gender-expansive (yellow), or likely >95% cisgender (orange). “Blank” indicates that the patient did not select an option. Abbreviations (all apply to SOGI fields): Not recorded, “Not recorded on birth certificate”; Not disclosed, “Choose not to disclose”; M, “Male”; F, “Female”; TM, “Transgender male”; TF, “Transgender female”; NB, “Nonbinary.”
Chart review findings for patients with SOGI field differences
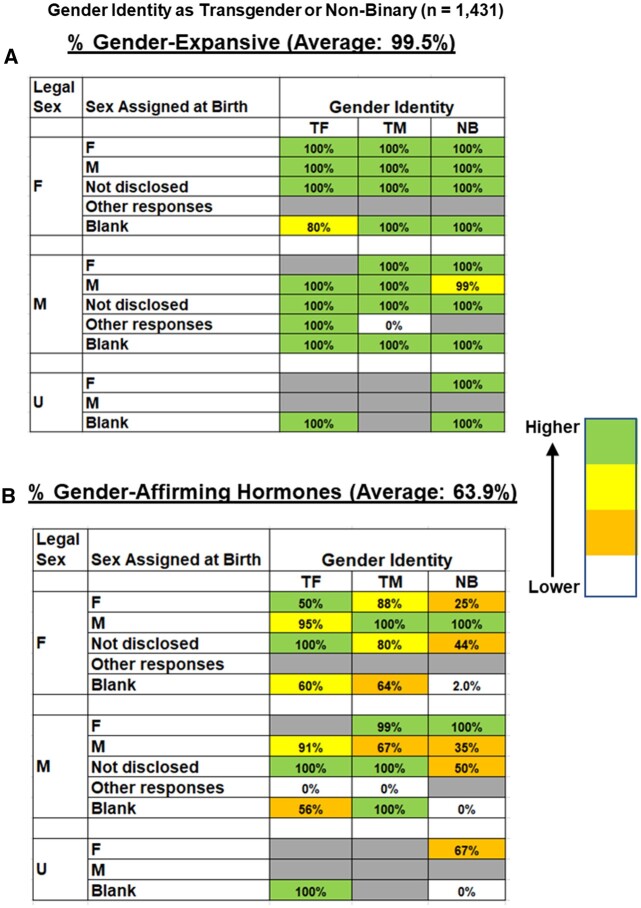
Starting with chart review for those with SOGI field differences (N = 2298), the combinations where patients selected “Transgender Female,” “Transgender Male,” or “Nonbinary” for GI (N = 1431) were 99.5% gender-expansive (Figure 3A), with 63.9% receiving gender-affirming hormones (Figure 3B). Use of gender-affirming hormones was higher in those who selected “Transgender Female” or “Transgender Male” compared to “Nonbinary” (Figure 3B and Table 3). Within the subset of patients selecting “Transgender Female,” “Transgender Male,” or “Nonbinary” for GI, 138 of the 1430 patients (9.7%) selected “Choose not to disclose” for SAAB or left this field blank. We detected a small number of responses that were illogical such as GI of “Transgender Female” but with Legal Sex and SAAB both selected as “Female.”
Figure 3.
Percent of patients who identified as gender-expansive (verified by chart review) and who were taking gender-affirming hormones from those who selected “Transgender Male,” “Transgender Female,” or “Nonbinary” for Gender Identity in the electronic health record SOGI fields (1431 unique patients). (A) Percentage of patients in each category that were determined to be gender-expansive by chart review (average of 99.5%). (B) Percentage of patients in each category that were determined to be actively using gender-affirming hormones (average of 63.9%). The color coding indicates frequency of gender-expansive identity or use of gender-affirming hormones (see index on right side of figure). Not disclosed: “Choose not to disclose”; Other responses: includes “Not recorded on birth certificate,” “Uncertain”: or “Unknown for Sex Assigned at Birth”; M: “Male”; F: “Female”; TM: “Transgender male”; TF: “Transgender female”; NB: “Nonbinary.”
Table 3.
Gender-expansive and gender-affirming therapy percentages
| Gender-expansive | Gender-affirming therapy | |
|---|---|---|
| Sexual orientation/gender identity (SOGI) field pattern, n (%) | ||
| Gender identity: transgender female (N = 359) | 358 (99.7%) | 321 (89.4%) |
| Gender identity: transgender male (N = 519) | 517 (99.6%) | 454 (87.5%) |
| Gender identity: nonbinary (N = 553) | 552 (99.8%) | 142 (25.7%) |
| Gender identity: female, different from other fields (N = 296) | 273 (92.2%) | 246 (83.1%) |
| Gender identity: male, different from other fields (N = 306) | 284 (92.8%) | 246 (80.4%) |
| Gender identity: other (N = 100) | 79 (79.0%) | 28 (28.0%) |
| Gender identity: choose not to disclose (N = 141) | 28 (19.9%) | 18 (12.8%) |
| All other SOGI field differences (N = 24) | 6 (25.0%) | 6 (25.0%) |
| All patients with SOGI field differences (N = 2298) | 2097 (91.3%) | 1461 (63.6%) |
| Diagnostic code search, n (%) | ||
| ICD-10 codes related to gender dysphoria (N = 1553) | 1550 (99.8%) | 1217 (78.4%) |
| ICD-10 code E34.9 (N = 1480) | 1408 (95.1%) | 1295 (87.5%) |
| Any of the above ICD-10 codes (N = 1891) | 1817 (96.1%) | 1455 (76.9%) |
| SOGI field difference and/or ICD-10 codes related to gender dysphoria (N = 2422) | 2219 (91.6%) | 1500 (61.9%) |
| Prescription for estradiol or testosterone suggesting use of gender-affirming hormones, n (%) (N = 1292) | 1171 (90.6%) | 1155 (89.4%) |
| Estradiol medication with legal sex of male (N = 483) | 482 (99.8%) | 479 (99.2%) |
| Testosterone medication with legal sex of female (N = 809) | 689 (85.2%) | 676 (83.6%) |
| Estradiol medication with cisgender male SOGI pattern (N = 16) | 14 (87.5%) | 14 (87.5%) |
| Testosterone medication with cisgender female SOGI pattern (N = 137) | 17 (12.4%) | 17 (12.5%) |
Abbreviation: ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th Revision codes and medication
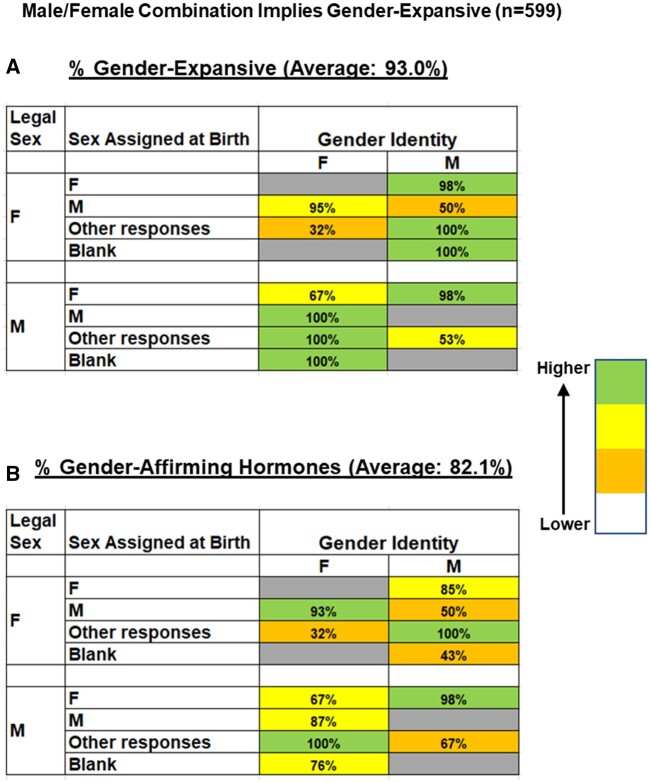
We next examined combinations where GI was selected as either “Female” or “Male” but with some discordance between GI, Legal Sex, or SAAB (N = 599). This population was 93.0% gender-expansive (Figure 4A), with 82.1% receiving gender-affirming hormones (Figure 4B). Some of the combinations implied a change of legal sex, with SAAB and Legal Sex SOGI fields now different in the EHR. Within the 588 patients, there were 9 patients (1.5%) who selected “Choose not to disclose” for SAAB.
Figure 4.
Percent of patients who identified as gender-expansive (verified by chart review) and who were taking gender-affirming hormones from those who selected either “Male” or “Female” for Legal Sex and Gender Identity but with discordance in Male/Female selections across the SOGI fields and/or a nonblank Sex Assigned at Birth selection other than “Male” or “Female” (599 unique patients). (A) Percentage of patients in each category that were determined to be gender-expansive by chart review (average of 93.0%). (B) Percentage of patients in each category that were determined to be actively using gender-affirming hormones (average of 82.1%). The color coding indicates frequency of gender-expansive identity or use of gender-affirming hormones (see index on right side of figure). M: “Male”; F: “Female.”
The remaining patients with SOGI field differences (other than a small group of those with Legal Sex of “Unknown” described separately below) comprised a heterogeneous group, including combinations where GI was selected as “Other” or “Choose not to disclose” or where GI was left blank but with SAAB provided and different from Legal Sex (N = 256). Using chart review, this group was 44.1% gender-expansive (Supplementary Figure S1A), with 20.3% receiving gender-affirming hormones (Supplementary Figure S1B). The choice of “Other” for GI also included a wide range of free text additional responses provided by patients in the SOGI data fields including “agender” (N = 5), “demiboy” (N = 3), “gender atypical” (N = 3), “gender fluid” (N = 23), “gender nonconforming” (N = 16), “gender queer” (N = 4), “gender questioning” (N = 1), “they/them” (N = 5), “transfeminine” (N = 1), and “transmasculine” (N = 11), as well as recognizable spelling variants of these.
There were 17 unique patients who had a Legal Sex of “Unknown” at time of data review, including 5 gender-expansive patients with GI either as “Nonbinary” (N = 4; all with SAAB as “Female”; 2 taking testosterone as gender-affirming hormones) or “Transgender Female” (N = 1; taking estradiol as gender-affirming hormone). These patients had utilized a formal process through the Health Information Management department to change Legal Sex in their medical records to “Unknown” to reflect a change in state identification documents for their gender. The remaining 12 patients with Legal Sex of “Unknown” appeared unrelated to gender-expansive identity and instead resulted from rapid patient registration during emergency trauma (N = 7) or as registration for public health-related laboratory testing using specimens lacking a sex identifier (N = 5).
Supplementary Figures S2 and S3 summarize the overall percentages of gender-expansive identity and use of gender-affirming hormones for the 2298 unique patients with 1 or more SOGI field differences. Supplementary Figures S4A (Legal Sex = “Female”) and S4B (Legal Sex = “Male” or “Unknown”) provide more detailed summaries of the underlying patterns determined through chart review for each combination. Within Supplementary Figures S4A and B, there are examples of infrequent combinations that likely had some element of selection error or terminology confusion. For example, there were 2 unique patients with Legal Sex of “Female” who selected “Transgender Female” for GI but also “Female” for SAAB (Supplementary Figure S4A). In both cases, the patients were transgender female based on chart review but did not select “Male” for SAAB. There were also examples of those who appeared to be cisgender from chart review but selected options for SAAB or GI that were discordant from Legal Sex, likely due to selection error or terminology confusion.
Within the total data set that was chart reviewed (N = 2441), we identified a total of 345 patients who officially changed legal sex. Of these 345 patients, 170 (49.3%) selected “Female” or “Male” for the GI field in the EHR (which now matched Legal Sex). These were detected in our study as changes in legal sex due to 1 or more factors that led to chart review (eg, SAAB also provided and different from Legal Sex or ICD-10 code for gender dysphoria present). However, if using SOGI field information alone, change of legal sex in this situation would be evident only if SAAB were also disclosed. From chart review, the GIs of those who officially changed legal sex were transgender female (N = 367), transgender male (N = 159), nonbinary (N = 16), gender fluid (N = 1), and transfeminine (N = 1).
Review of patients with ICD-10 diagnosis codes related to gender dysphoria or unspecified endocrine disorder
There were a total of 1553 patients who had at least 1 in-person clinical encounter that used 1 or more of the following 6 diagnosis codes related to gender dysphoria and its management: F64.0 (N = 341), F64.1 (N = 1), F64.2 (N = 176), F64.8 (N = 0), F64.9 (N = 1408), and Z87.890 (N = 9). A total of 1550 of 1553 patients (99.8%) were gender-expansive, 1217 (78.3%) were taking gender-affirming hormones, and 1429 (92.0%) also had SOGI field differences. The 3 out of 1553 (0.2%) patients who were not gender-expansive by chart review appeared to result from erroneous selection of one of the ICD-10 codes related to gender dysphoria for a single visit. A combined set of patients with SOGI field differences and/or ICD-10 codes related to gender dysphoria comprised 2422 unique patients, of which 2219 (91.6%) were gender-expansive and 1500 (61.9%) receiving gender-affirming hormones.
ICD-10 code E34.9 (endocrine disorder, unspecified) was used in nearly as many patients (N = 1480) as the 6 ICD-10 codes related to gender dysphoria. However, there was substantial overlap of use of these codes, leading to a total of 1891 patients that had any of 6 ICD-10 codes related to dysphoria and/or ICD-10 code E34.9, of which 1817 (96.0%) were gender-expansive and 1455 (76.9%) were receiving gender-affirming hormones. The inclusion of ICD-10 code E34.9 identified 73 patients that did not have any SOGI field differences in the EHR or any of the 6 ICD-10 codes related to gender dysphoria. From chart review, only 2 of these 73 (2.7%) patients were gender-expansive and receiving gender-affirming hormones. The remaining 71 patients were cisgender, with the E34.9 code documenting an endocrine condition unrelated to gender dysphoria.
Review of patients potentially prescribed gender-affirming hormones using legal sex as reference
We identified 483 patients with Legal Sex of “Male” who were prescribed estradiol during the retrospective timeframe, of which 482 (99.8%) were gender-expansive and 479 (99.2%) were receiving estradiol as part of gender-affirming care. A total of 467 of these 483 patients had SOGI field differences in the EHR. The remaining 16 patients had presumptively cisgender male SOGI field profiles, 14 of whom were gender-expansive and receiving gender-affirming estradiol.
We also identified 809 patients with Legal Sex of “Female” who were prescribed testosterone during the retrospective timeframe, of which 689 (85.2%) were gender-expansive and 676 (83.6%) receiving testosterone as part of gender-affirming care. A total of 672 of the 809 patients had SOGI field differences in the EHR. The remaining 137 patients had presumptively cisgender female SOGI field profiles; however, using chart review, only 17 of these 137 (12.4%) were gender-expansive and receiving testosterone for gender-affirming hormone. A high percentage of the remainder were prescribed testosterone as part of hormonal medication treatment for menopausal symptoms.
The various approaches to identify gender-expansive patients (SOGI field differences in the EHR, ICD-10 codes related to gender dysphoria, and potential gender-affirming hormone use based on legal sex) identified a total of 2236 patients identifying as gender-expansive and 1506 taking gender-affirming hormones. Figure 5 shows how well the various approaches did with identifying the total population at UIHC determined by chart review to be gender-expansive and taking gender-affirming hormones. Supplementary Figure S5 shows a diagram breaking down the different subpopulations analyzed in the study. Combining SOGI field differences in the EHR with the ICD-10 codes related to gender dysphoria captures 2219 of 2236 (99.2%) patients who identify as gender-expansive and 1500 of 1506 (99.6%) taking gender-affirming hormones. This approach identifies 203 patients who do not identify as gender-expansive, at least as evidenced through chart review. Supplementary Figure S6 has a Venn diagram of how the 3 main approaches overlap with one another.
Figure 5.
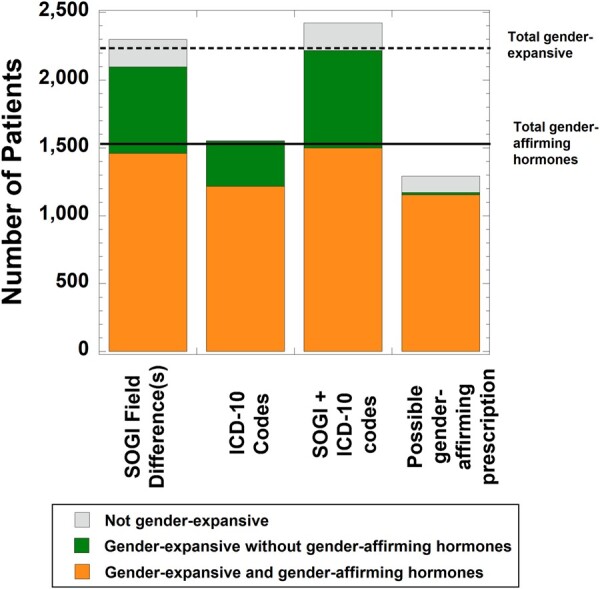
Relation of variables analyzed in the study relative to the total identified population of gender-expansive patients (dashed line; N = 2236) and those taking gender-affirming hormones (solid line; N = 1506). The bars depict the breakdown of how many patients were determined by chart review to be not gender-expansive, gender-expansive but not taking gender-affirming hormones, or gender-expansive and actively taking gender-affirming hormones. The individual bars include those with one or more SOGI field differences (excluding blank responses; N = 2298), those with at least 1 of 6 ICD-10 codes related to gender dysphoria for a clinical encounter (N = 1553), combination of SOGI field differences and/or ICD-10 codes related to gender dysphoria (N = 2422), and prescription for estradiol or testosterone suggesting use of gender-affirming hormones (eg, estradiol in someone with Legal Sex of “Male”; N = 1292).
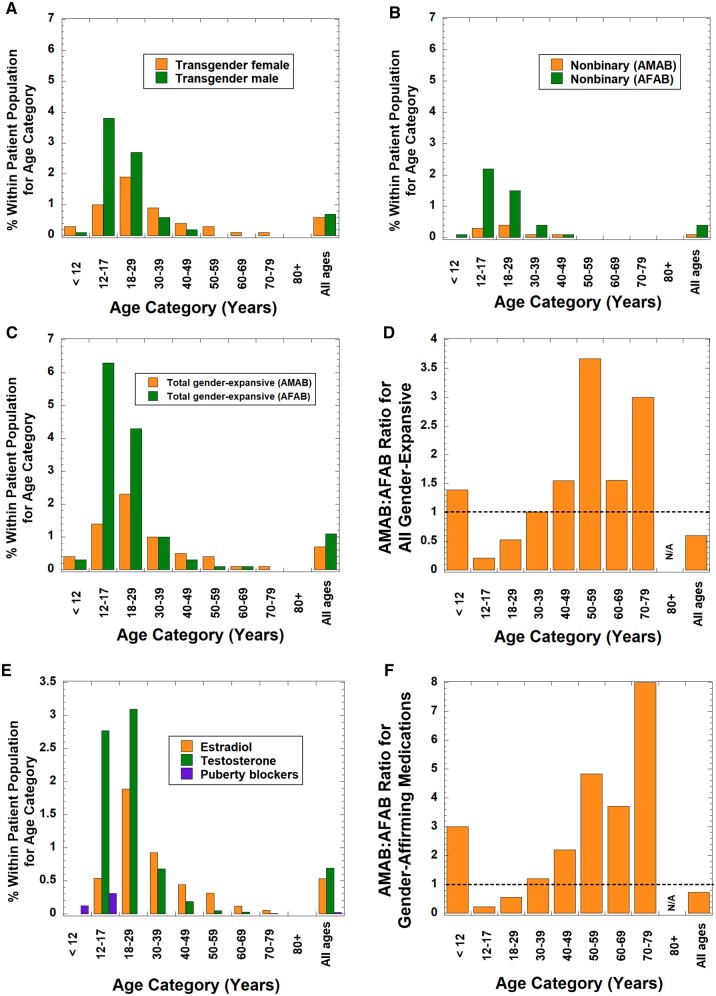
Differences in SAAB for the gender-expansive population
We analyzed differences in SAAB for the population identifying as gender-expansive. Assuming correct input into the SOGI fields in the EHR, transgender males by definition are assigned female at birth (AFAB) and transgender females are assigned male at birth (AMAB). Based on GI alone, SAAB would not be obvious for other GIs such as nonbinary, gender queer, or gender nonconforming. Figure 6A shows the distribution of transgender male and transgender female within age categories. Transgender males are relatively more common in the 12–17 and 18–29 year age groups, while transgender females are relatively more common in age groups of 30–39 years or higher. In contrast, those identifying as nonbinary who are AFAB are more common across all age categories, although uncommon overall in the total patient population 40 years and older (Figure 6B).
Figure 6.
Ratios of assigned male at birth (AMAB) compared to assigned female at birth (AFAB) for gender-expansive identity and use of gender-affirming therapy in different age categories. (A) Breakdown of transgender male patients compared to transgender female as a percentage of total patients within specific age distributions. (B) Breakdown of AMAB nonbinary patients compared to AFAB nonbinary patients as a percentage of total patients within specific age distributions. (C) Breakdown of all gender-expansive patients (including transgender, nonbinary and other gender-expansive identities) into those who are AMAB compared to AFAB as a percentage of total patients within specific age distributions. (D) Ratio of AMAB to AFAB for all gender-expansive patients within specific age distributions. The dashed line represents a ratio of 1.0. (E) Breakdown of gender-affirming medications within specific age distributions. (F) Ratio of AMAB to AFAB for patients who were receiving gender-affirming medications within specific age distributions. Total patient population is 123 441 (<12 years, N = 6547; 12–17 years, N = 6177; 18–29 years, N = 17 123; 30–39 years, N = 15 452; 40–49 years, N = 14 963; 50–59 years, N = 18 508; 60–69 years, N = 22 692; 12–17 years, N = 15 515; 80 years or older, N = 6464).
There were also a total of 73 gender-expansive individuals (53 AFAB, 20 AMAB) who did not identify as transgender or nonbinary from chart review but instead selected another identity with the broader gender-expansive umbrella. These include the following GIs (number of those who are AFAB: number of AMAB): agender (5:0), demiboy (3:0), exploring/indifferent (0:1), gender atypical (3:0), gender-expansive (5:0), gender fluid (15:8), gender nonconforming (7:9), gender queer (3:1), gender questioning (1:0), transfeminine (0:1), and transmasculine (11:0). Figure 6C shows the distribution of all gender-expansive patients within age categories. Figure 6D shows how the AMAB: AFAB ratio of the gender-expansive population at UIHC varies within age categories. The ratio was skewed toward AFAB in the 12–17 and 18–29 year age categories but skewed toward AMAB in other age categories. The highest age for anyone with a gender-expansive identification was 78.2 years.
We also examined the distribution of gender-affirming hormones and puberty blockers within age categories (Figure 6E). Testosterone prescriptions as gender-affirming hormones were more common than estradiol in the 12–17 and 18–29 year categories, while estradiol predominated in the 30 year and older categories. There were 26 patients taking puberty blockers, with 15 AMAB patients (N = 13 identifying as transgender female, N = 2 nonbinary) and 11 AFAB (all identifying as transgender male). The overall pattern of AMAB : AFAB ratios for those prescribed gender-affirming medications (including puberty blockers) was similar to that for gender-expansive identities (Figure 6F).
Lastly, by chart review, we identified a total of 188 patients who were gender-expansive and had bilateral gonadectomy. This group was comprised of 69 AFAB patients who had bilateral ovariectomy (N = 63 identifying as transgender male, N = 5 nonbinary, and N = 1 agender) and 119 AMAB patients who had bilateral orchiectomy (N = 115 identifying as transgender female, N = 4 nonbinary). In 184 of the 188 patients, the bilateral gonadectomy was done for gender affirmation in someone also prescribed gender-affirming hormones. In 3 of the AFAB patients, hysterectomy and bilateral ovariectomy were performed for the primary indication of dysmenorrhea or menorrhagia; none of these 3 patients were taking gender-affirming hormones. There was 1 AFAB patient who had bilateral ovariectomy for gender affirmation who had taken testosterone previously but discontinued while being treated for a myeloproliferative neoplasm.
DISCUSSION
SOGI demographic fields are a relatively new functionality for EHRs in the United States.1–4,10 Here, we used chart review to validate how well SOGI fields, pharmacy records, and ICD-10 codes related to gender dysphoria identify the gender-expansive population at an academic medical center in Iowa. A combination of SOGI field differences and ICD-10 codes identified over 99% of the total gender-expansive population, including those using gender-affirming hormones.
ICD-10 codes, SOGI field differences, and pharmacy search have contrasting strengths and weaknesses for identifying the gender-expansive population. ICD-10 codes alone will not detect patients who identify as gender-expansive but have not yet had a diagnosis code related to gender dysphoria. This may include the gender-expansive population that is not seeking gender-affirming hormones or surgery. SOGI field differences capture a wider group then ICD-10 codes but include some cisgender patients who select choices such as “Choose not to disclose,” “Uncertain,” or “Unknown” for GI and SAAB for a variety of reasons. While there was an option to specify “Other” for GI in our institutional EHR SOGI fields, this was not a commonly selected choice. Information volunteered by the patient will be influenced by the options offered that may exclude other possibilities that may fit the GI better (eg, 2-spirit for GI). A pharmacy search for prescriptions for estradiol in those with legal sex of male or for testosterone in those with legal sex of female has some limitations including therapeutic use of these hormones for reasons unrelated to gender-expansive identity (eg, testosterone prescribed for menopausal symptoms in cisgender women) and cases where patients have changed legal sex in their health record. In addition, ICD-10 codes for gender dysphoria will often be needed as documentation for prescriptions for gender-affirming hormones and thus already identify many of the same patients.
There have been efforts to employ phenotyping algorithms, using natural language processing or other methods, to identify transgender and other gender diverse individuals within EHRs.33–36 This approach is especially useful for larger scale studies that identify healthcare disparities and formulate strategies for improving healthcare to the gender diverse population. Our results indicate that variables such as SOGI field differences and ICD-10 codes will be useful in such approaches, and can help in reducing time-intensive chart review.
Prevalence estimates for the gender-expansive population vary widely across published studies.3,17–26 Some of this variation relates to differing definitions and intent of studies, which may focus more narrowly on the transgender population or a broader gender-expansive population. In the total patient population analyzed in our study, 1.8% identify broadly as gender-expansive (1.3% transgender, 0.5% nonbinary and <0.1% other gender-expansive identity). The rates of gender-expansive identity are highest in the 12–17 year (7.4%) and 18–29 year (6.6%) age ranges compared to older ages. The corresponding total rates of gender-affirming hormone prescriptions (estradiol, testosterone, or puberty blockers) at our institution in these age ranges are 3.8% for the 12–17 year and 5.3% in the 18–29 year ranges. As a frame of reference to hormone prescriptions used for other clinical applications, data from the 2011–2015 United States National Survey of Family Growth showed 13.3% of females aged 15–19 years used contraceptive hormonal pills and 5.3% used other hormonal contraception methods. These data are similar to previous surveys dating back to 2002.37
We observed a bias toward AFAB in the gender-expansive population between 12 and 29 years old, especially in the nonbinary population, a trend noted in other published studies in clinical settings.23,38–40 Interestingly, survey data with larger sample sizes have not shown this bias.11,40 There are a number of potential factors that may influence disclosure of gender-expansive identity by adolescents and young adults in a clinical setting including referral bias, social and peer acceptance, and concerns with medical privacy (especially for adolescent patients related to parent/guardian access to medical information).11,38,39,41 In contrast, adolescents and young adults may report GIs more openly in surveys that preserve anonymity.11 The adolescent and young adult populations at our institution also account for nearly all gender-expansive identities not included in the SOGI field choices within the EHR (eg, agender, demiboy, gender queer, transfeminine), illustrating age-related variation in adoption of specific terms other than transgender or nonbinary to identify GI. A higher ratio of AMAB relative to AFAB was noted in the gender-expansive population in our institution for those 30 years and older, consistent with earlier data for these age ranges.42
As mentioned in the “Introduction” section, there are risks to patients disclosing SOGI information that will be accessible in the EHR.8–10 These include negative treatment by healthcare professionals,8,9,11 as well as privacy concerns for others (including parents/guardians of adolescent patients) to access this information in the health record.11,12 There are also significant differences in inclusivity for gender diverse people across different locations within the United States, such as a recent trend toward legislation banning gender-affirming care in minors in some states.43,44 In addition to impacting mental health and gender-affirming care, such legislation may also make individuals less comfortable with disclosing SOGI information. However, the goal is to increase awareness and access to healthcare for gender-expansive people to avoid the alternative of erasure of noncisgender identities.45
Limitations to our study include analysis at a single academic medical center that serves as a regional center for specialized gender-affirming care. The efficacy of SOGI fields at our institution was likely strongly influenced by workflows that encourage use of the SOGI fields in the LGBTQ clinics, along with training for inclusive practices such as use of preferred name.7 Institutions with low rates of SOGI field adoption will likely find less benefit for research purposes. In addition, extensive use of templated clinical notes for the LGBTQ patient population at our institution provided more consistency for information in clinical notes related to gender-expansive identity and use of gender-affirming therapy. Future studies should examine how SOGI profiles can enhance clinical care.
CONCLUSIONS
We validated 3 different methods for identifying gender-expansive people using EHR information and show that a combination of SOGI indicators and ICD-10 codes are especially effective identifiers.
Supplementary Material
ACKNOWLEDGEMENTS
The introduction of SOGI fields into the EHR patient is a major undertaking and requires the combined effort of many people from different teams. The authors would like to thank all the individuals involved in implementation, validation, policy revisions, help support, training, and other key tasks in this project. The authors would particularly like to thank Nick Dreyer, Dean Aman, and Linda Kleinmeyer from the University of Iowa Health Care Information Systems for answering specific questions and assistance with retrieving data from the institutional data warehouse.
Contributor Information
Nicole G Hines, Carver College of Medicine, University of Iowa, Iowa City, Iowa, USA.
Dina N Greene, Department of Laboratory Medicine, University of Washington, Seattle, Washington, USA; LetsGetChecked Laboratories, Monrovia, California, USA.
Katherine L Imborek, Department of Family Medicine, University of Iowa, Iowa City, Iowa, USA.
Matthew D Krasowski, Department of Pathology, University of Iowa Hospitals and Clinics, Iowa City, Iowa, USA.
AUTHOR CONTRIBUTIONS
NGH and MDK extracted data and carried out the data analysis. NGH and MDK conceived the original idea with subsequent input from DNG and KLI. MDK supervised the project. NGH and MDK produced the original draft. All authors revised and approved the final manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at JAMIA Open online.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data are not publicly available as the data were derived from electronic health records and include sensitive individual-level information that could compromise research participant privacy.
REFERENCES
- 1. Cahill S, Makadon HJ.. Sexual orientation and gender identity data collection update: U.S. government takes steps to promote sexual orientation and gender identity data collection through meaningful use guidelines. LGBT Health 2014; 1 (3): 157–60. [DOI] [PubMed] [Google Scholar]
- 2. Cahill SR, Baker K, Deutsch MB, Keatley J, Makadon HJ.. Inclusion of sexual orientation and gender identity in Stage 3 Meaningful Use Guidelines: a huge step forward for LGBT health. LGBT Health 2016; 3 (2): 100–2. [DOI] [PubMed] [Google Scholar]
- 3. Grasso C, Goldhammer H, Brown RJ, Furness BW.. Using sexual orientation and gender identity data in electronic health records to assess for disparities in preventive health screening services. Int J Med Inform 2020; 142: 104245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marney HL, Vawdrey DK, Warsame L, et al. Overcoming technical and cultural challenges to delivering equitable care for LGBTQ+ individuals in a rural, underserved area. J Am Med Inform Assoc 2022; 29 (2): 372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Deutsch MB, Buchholz D.. Electronic health records and transgender patients–practical recommendations for the collection of gender identity data. J Gen Intern Med 2015; 30 (6): 843–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Donald C, Ehrenfeld JM.. The opportunity for medical systems to reduce health disparities among lesbian, gay, bisexual, transgender and intersex patients. J Med Syst 2015; 39 (11): 178. [DOI] [PubMed] [Google Scholar]
- 7. Imborek KL, Nisly NL, Hesseltine MJ, et al. Preferred names, preferred pronouns, and gender identity in the electronic medical record and laboratory information system: is pathology ready? J Pathol Inform 2017; 8: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maragh-Bass AC, Torain M, Adler R, et al. Risks, benefits, and importance of collecting sexual orientation and gender identity data in healthcare settings: a multi-method analysis of patient and provider perspectives. LGBT Health 2017; 4 (2): 141–52. [DOI] [PubMed] [Google Scholar]
- 9. Thompson HM. Stakeholder experiences with gender identity data capture in electronic health records: implementation effectiveness and a visibility paradox. Health Educ Behav 2021; 48 (1): 93–101. [DOI] [PubMed] [Google Scholar]
- 10. Thompson HM, Kronk CA, Feasley K, Pachwicewicz P, Karnik NS.. Implementation of gender identity and assigned sex at birth data collection in electronic health records: where are we now? Int J Environ Res Public Health 2021; 18 (12): 6599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goldhammer H, Grasso C, Katz-Wise SL, Thomson K, Gordon AR, Keuroghlian AS.. Pediatric sexual orientation and gender identity data collection in the electronic health record. J Am Med Inform Assoc 2022; 29 (7): 1303–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kraschel KL, Chen A, Turban JL, Cohen IG.. Legislation restricting gender-affirming care for transgender youth: politics eclipse healthcare. Cell Rep Med 2022; 3 (8): 100719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goldstein Z, Corneil TA, Greene DN.. When gender identity doesn't equal sex recorded at birth: the role of the laboratory in providing effective healthcare to the transgender community. Clin Chem 2017; 63 (8): 1342–52. [DOI] [PubMed] [Google Scholar]
- 14. LeBron AMW, Cowan K, Lopez WD, Novak NL, Ibarra-Frayre M, Delva J.. The Washtenaw ID Project: a government-issued ID coalition working toward social, economic, and racial justice and health equity. Health Educ Behav 2019; 46 (1 suppl): 53S–61S. [DOI] [PubMed] [Google Scholar]
- 15. Topaz CM, Higdon J, Epps-Darling A, et al. Race- and gender-based under-representation of creative contributors: art, fashion, film, and music. Humanit Soc Sci Commun 2022; 9 (1): 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Movement Advancement Project. Identity Document Laws and Policies. Secondary Identity Document Laws and Policies, 2023. https://www.lgbtmap.org/equality-maps/identity_document_laws Accessed June 2, 2023.
- 17. Deutsch MB. Making it count: improving estimates of the size of transgender and gender nonconforming populations. LGBT Health 2016; 3 (3): 181–5. [DOI] [PubMed] [Google Scholar]
- 18. Meerwijk EL, Sevelius JM.. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health 2017; 107 (2): e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nik-Ahd F, Waller J, De Hoedt AM, et al. Seeing the unseen: how can we best identify transgender women within the Veterans Affairs healthcare system's electronic medical record? J Sex Med 2023; 20 (4): 559–67. [DOI] [PubMed] [Google Scholar]
- 20. Blosnich JR, Cashy J, Gordon AJ, et al. Using clinician text notes in electronic medical record data to validate transgender-related diagnosis codes. J Am Med Inform Assoc 2018; 25 (7): 905–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Collin L, Reisner SL, Tangpricha V, Goodman M.. Prevalence of transgender depends on the “Case” definition: a systematic review. J Sex Med 2016; 13 (4): 613–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dubin S, Cook TE, Radix A, Greene RE.. Sexual orientation demographic data in a clinical cohort of transgender patients. Appl Clin Inform 2021; 12 (2): 222–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dubin S, Cook T, Liss A, et al. Comparing electronic health record domains' utility to identify transgender patients. Transgend Health 2022; 7 (1): 78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Feldman JL, Luhur WE, Herman JL, Poteat T, Meyer IH.. Health and health care access in the US transgender population health (TransPop) survey. Andrology 2021; 9 (6): 1707–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McFarland W, Wilson E, Fisher Raymond H.. How many transgender men are there in San Francisco? J Urban Health 2018; 95 (1): 129–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Roblin D, Barzilay J, Tolsma D, et al. A novel method for estimating transgender status using electronic medical records. Ann Epidemiol 2016; 26 (3): 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Deutsch MB, Green J, Keatley J, et al. , World Professional Association for Transgender Health EMR Working Group. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J Am Med Inform Assoc 2013; 20 (4): 700–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moorthie S, Peacey V, Evans S, et al. A scoping review of approaches to improving quality of data relating to health inequalities. Int J Environ Res Public Health 2022; 19 (23): 5874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Staggs S, Sewell R, Buchanan C, et al. Instituting sexual orientation and gender identity training and documentation to increase inclusivity at a pediatric health system. Transgend Health 2022; 7 (5): 461–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kronk CA, Everhart AR, Ashley F, et al. Transgender data collection in the electronic health record: current concepts and issues. J Am Med Inform Assoc 2022; 29 (2): 271–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Krasowski MD, Grieme CV, Cassady B, et al. Variation in results release and patient portal access to diagnostic test results at an academic medical center. J Pathol Inform 2017; 8: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. World Health Organisation. ICD-10: international Statistical Classification of Diseases and Related Health Problems. 10th Revision, 4th edn. Geneva, Switzerland: World Health Organization, 2010. [Google Scholar]
- 33. Ehrenfeld JM, Gottlieb KG, Beach LB, Monahan SE, Fabbri D.. Development of a natural language processing algorithm to identify and evaluate transgender patients in electronic health record systems. Ethn Dis 2019; 29 (suppl 2): 441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Guo Y, He X, Lyu T, et al. Developing and validating a computable phenotype for the identification of transgender and gender nonconforming individuals and subgroups. AMIA Annu Symp Proc 2020; 2020: 514–23. [PMC free article] [PubMed] [Google Scholar]
- 35. Rich AJ, Poteat T, Koehoorn M, et al. Development of a computable phenotype to identify a transgender sample for health research purposes: a feasibility study in a large linked provincial healthcare administrative cohort in British Columbia, Canada. BMJ Open 2021; 11 (3): e040928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xie F, Getahun D, Quinn VP, et al. An automated algorithm using free-text clinical notes to improve identification of transgender people. Inform Health Soc Care 2021; 46 (1): 18–28. [DOI] [PubMed] [Google Scholar]
- 37. Abma JC, Martinez GM.. Sexual activity and contraceptive use among teenagers in the United States, 2011–2015. Natl Health Stat Rep 2017; (104): 1–23. [PubMed] [Google Scholar]
- 38. Exposito-Campos P, Gomez-Balaguer M, Hurtado-Murillo F, Morillas-Arino C.. Evolution and trends in referrals to a specialist gender identity unit in Spain over 10 years (2012-2021). J Sex Med 2023; 20 (3): 377–87. [DOI] [PubMed] [Google Scholar]
- 39. Kearns S, O’Shea D, Neff K.. Transgender and non-binary demographics, referrals, and comorbidities among young Irish adults (2014–2020). Ir J Med Sci 2022. 10.1007/s11845-022-03163-y. [DOI] [PubMed] [Google Scholar]
- 40. Turban JL, Dolotina B, King D, Keuroghlian AS.. Sex assigned at birth ratio among transgender and gender diverse adolescents in the United States. Pediatrics 2022; 150 (3): e2022056567. [DOI] [PubMed] [Google Scholar]
- 41. Ashley F. Shifts in assigned sex ratios at gender identity clinics likely reflect changes in referral patterns. J Sex Med 2019; 16 (6): 948–9. [DOI] [PubMed] [Google Scholar]
- 42. Wiepjes CM, Nota NM, de Blok CJM, et al. The Amsterdam Cohort of Gender Dysphoria Study (1972–2015): trends in prevalence, treatment, and regrets. J Sex Med 2018; 15 (4): 582–90. [DOI] [PubMed] [Google Scholar]
- 43. Barbee H, Deal C, Gonzales G.. Anti-transgender legislation – a public health concern for transgender youth. JAMA Pediatr 2022; 176 (2): 125–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kline NS, Webb NJ, Johnson KC, Yording HD, Griner SB, Brunell DJ.. Mapping transgender policies in the US 2017–2021: the role of geography and implications for health equity. Health Place 2023; 80: 102985. [DOI] [PubMed] [Google Scholar]
- 45. Bauer GR, Hammond R, Travers R, Kaay M, Hohenadel KM, Boyce M.. I don't think this is theoretical; this is our lives”: how erasure impacts health care for transgender people. J Assoc Nurses AIDS Care 2009; 20 (5): 348–61. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are not publicly available as the data were derived from electronic health records and include sensitive individual-level information that could compromise research participant privacy.