Abstract
Neuropsychiatric diseases (NPD) represent a significant global disease burden necessitating innovative approaches to pathogenic understanding, biomarker identification and therapeutic strategy. Emerging evidence implicates heart/brain axis malfunction in NPD etiology, particularly via the autonomic nervous system (ANS) and brain central autonomic network (CAN) interaction. This heart/brain inter-relationship harbors potentially novel NPD diagnosis and treatment avenues. Nevertheless, the lack of multidisciplinary clinical approaches as well as a limited appreciation of molecular underpinnings has stymied progress. Large-scale preclinical multi-systemic functional data can therefore provide supplementary insight into CAN and ANS interaction. We here present an overview of the heart/brain axis in NPD and establish a unique rationale for utilizing a preclinical cardiovascular disease risk gene set to glean insights into heart/brain axis control in NPD. With a top-down approach focusing on genes influencing electrocardiogram ANS function, we combined hierarchical clustering of corresponding regional CAN expression data and functional enrichment analysis to reveal known and novel molecular insights into CAN and NPD. Through ‘support vector machine’ inquiries for classification and literature validation, we further pinpointed the top 32 genes highly expressed in CAN brain structures altering both heart rate/heart rate variability (HRV) and behavior. Our observations underscore the potential of HRV/hyperactivity behavior as endophenotypes for multimodal disease biomarker identification to index aberrant executive brain functioning with relevance for NPD. This work heralds the potential of large-scale preclinical functional genetic data for understanding CAN/ANS control and introduces a stepwise design leveraging preclinical data to unearth novel heart/brain axis control genes in NPD.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00335-022-09974-9.
Introduction
Neuropsychiatric diseases (NPD) are clinically heterogeneous and comprise 7% of the global disease burden (Rehm and Shield 2019; Yang et al. 2021). Cardiovascular disease (CVD) is similarly prevalent (Roth et al. 2020) and a significant cause of premature death in NPD (Correll et al. 2017) inferring pathogenic overlap. Poor lifestyle leading to obesity and diabetes as well as medication use partially underlie CVD/NPD comorbidity (Correll et al. 2015; Hamer et al. 2008; Penninx and Lange 2018; Rosengren et al. 2004). Nevertheless, heart and brain miscommunication through the heart/brain axis likely contributes to pathogenesis. Particularly the NPD implications of autonomic nervous system (ANS) dysfunction attracted some attention (Mulkey and du Plessis 2019; Perrone and Valente 2021). The brain’s central autonomic network (CAN), via the ANS, transduces emotional and psychological experience effects on heart activity with abnormalities therein increasing NPD and comorbid CVD risk (Mulkey and du Plessis 2019). The prevalence and therapeutic shortcomings highlight the need for more innovative approaches to tackling NPDs. Thus, a deeper understanding of this bidirectional brain/heart relationship, including the trans-diagnostic potential of heart rate variability (HRV), will evince potentially unexplored NPD biomarkers, endophenotypes (genetic dysfunction traits), and risk gene variants for precision psychiatry approaches (Beauchaine and Thayer 2015).
An impediment to heart/brain axis understanding in NPD and neurocardiology is the dearth of holistic approaches to patient treatment and the current emphasis on specialization in one medical field (Valenza et al. 2016). The availability of large-scale preclinical multi-systemic data is thus a valuable resource to gain insights into the molecular mechanism of heart/brain interaction for patient translation. In this report, we provide, therefore, an introduction to heart/brain axis and CAN/ANS communication in NPD. Moreover, we outline a unique rationale and stepwise refinement incorporating brain expression data of a previously identified CVD risk gene set from the International Mouse Phenotyping Consortium (IMPC) data (Spielmann et al. 2022). By addressing NPD understanding from a CVD risk perspective, we introduce a novel means of exploiting preclinical multi-disciplinary data to prioritize NPD candidate genes and unearth unrealized molecular foundations of heart/brain and CAN/ANS abnormality as a blueprint for innovative NPD therapies.
Heart/brain abnormality in NPD—the evidence from CVD and NPD comorbidity data
Epidemiological studies indicate an upsurge in NPD prevalence in the last 20 years, particularly in early-onset diseases such as autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) (Atladottir et al. 2015, 2007; Kim et al. 2011; Maenner et al. 2021). The increase likely relates to non-etiological features (e.g. broadened diagnostic criteria) and additional factors (parental lifestyle, advancing age at conception) increasing abnormal genetic neurodevelopmental risk. NPDs exhibit moderate to high heritability particularly ASD, schizophrenia (SCZ) and bipolar disorder (BD), and major depressive disorder (MDD) to a lesser extent (Faa et al. 2016; Sandin et al. 2017). In ASD, much of the genetic risk originates from common variants, as well as rare and de novo variants with gene x environment (GxE) interactions and epigenetics accounting for missing heritability. Such elements are critical during intrauterine and postnatal neurodevelopment when there is greater vulnerability to adverse early life events and developmental influences (Faa et al. 2016).
While neurocardiology is still a burgeoning field, there is evidence connecting NPD and CVD pathogenesis that reflects the so far established bidirectional heart/brain interaction. Depression symptoms, for example, are frequent in coronary artery disease patients [particularly in young and female patients (Shah et al. 2014)]. In addition, heart failure can impair cerebral perfusion, leading to stroke, cognitive obstruction and mood disorder [reviewed by (Doehner et al. 2018)]. Among NPDs, MDD, anxiety disorders, SCZ and ASD are comorbid with cardiovascular dysfunction (Kawachi et al. 1994; Lett et al. 2004; Tyler et al. 2011; Westman et al. 2018). For example, both MDD and SCZ patients are at increased coronary heart disease risk while SCZ patients are also vulnerable to cerebrovascular disease and congestive heart failure (Correll et al. 2017; Rugulies 2002). Furthermore, severe anxiety and stress experience are associated with sudden cardiac death and Takotsubo (“broken heart”) cardiomyopathy related to sympathomimetic overflow (Doehner et al. 2018; Watkins et al. 2006). Congenital heart disease (CHD) is also a risk factor for neurodevelopmental disorders such as ASD (Wernovsky and Licht 2016) potentially related to shared genetic origins and/or vulnerability to environmental challenges during development.
Additional, likely overlapping, bidirectional brain/heart communication channels underlying CVD and NPD risk include the hypothalamic–pituitary–adrenal (HPA) axis, inflammatory signaling and ANS dysfunction (De Hert et al. 2018). HPA-induced cortisol hyperactivity in MDD augments coronary artery atherosclerosis and cardiovascular death risk (Jokinen and Nordstrom 2009; Lichtman et al. 2008; Vale 2005). Furthermore, inflammation and increased cytokine levels [interleukin (IL)-6, IL-1β, tumor necrosis factor (TNF)-α] are etiological in both NPD and CVD (Empana et al. 2005). Disrupted CAN and ANS development impair stress resilience increasing NPD vulnerability (Homsy et al. 2015). Thus, understanding the genetic underpinnings of heart/brain axis interaction, particularly via the ANS and CAN, has the potential to provide so far unexploited disease and patient stratification biomarkers as well as NPD therapeutic avenues. As the Research Domain Criteria (RDoC) initiative seeks objective NPD markers (Insel et al. 2010), such novel endophenotype identification is welcome.
An overview of heart/brain communication via CAN—feedforward and feedback ANS control
The complex nature of CAN and ANS interaction and function warrants an overview to understand NPD-related dysfunction. The ANS modulates the intrinsic cardiac nervous system, sinoatrial and atrioventricular node activity, transducing peripheral signals (autonomic afference) into physiological responses (autonomic efference). The efferent system dichotomizes into sympathetic (SNS) and parasympathetic (PNS) branches (Fig. 1) (Karemaker 2017). SNS preganglionic neurons from the thoracic spinal cord synapse with neurons in cervical and thoracic ganglia and postganglionic fibers innervate the cardiac conduction system (Silvani et al. 2016). Preganglionic PNS neurons originate from the nucleus ambiguous and dorsal motor nucleus of the vagus in the medulla oblongata. Via the vagus nerve, these neurons extend to the cardiac nervous system and postganglionic PNS fibers innervate the cardiac conduction system (Silvani et al. 2016). “Fight or flight” emergency responses to stress and danger, including increased heart rate (HR), are mediated by the SNS and the PNS underlies “rest and digest” restorative functions. Preganglionic SNS and postganglionic PNS nerve endings release acetylcholine while postganglionic SNS terminals release predominantly noradrenaline (Waxenbaum et al. 2022). Autonomic imbalance occurs with hyper-activation of one ANS branch, usually the SNS, at the expense of the other (PNS) augmenting pathological risk and even death (arrhythmias, sudden cardiac death). Low HRV signifies decreased vagal tone and is a non-invasive disease marker in this case (Cerritelli et al. 2021).
Fig. 1.
A highly schematized representation of the complex central autonomic network (CAN) organization in the brain involved in both feedforward [FF-ANS (red shading)] and feedback [FB-ANS (blue shading)] control of autonomic nervous system (ANS) function and the neuroanatomical correlate of heart/brain axis communication. The most important CAN brain structures include the prefrontal cortex (PFC), anterior cingulate cortex (ACC), insular cortex (IC), hippocampus (HIP), amygdala (AMYG), thalamus (TH), hypothalamus (HYP) as well as periaqueductal gray (PAG) in the midbrain, parabrachial nucleus (PBN) of the pons and the following medulla oblongata nuclei: dorsal motor vagus (DMV), solitary tract (NTS) and ambiguous (NA). This network of brain regions interconnects as depicted and, via sympathetic (SNS) and parasympathetic (PNS) connections, influence heart function. Parasympathetic output extends from the DMV to NA projecting through the vagus nerve to the heart sino-atrial node (Created with Biorender.com)
The CAN encompasses brain cortical and subcortical mood and memory influences on ANS cardiovascular activity, dividing into ‘feedforward’ (FF-ANS) and ‘feedback’ (FB-ANS) brain regions (Fig. 1) (Dampney 2016). The former includes the insular and anterior cingulate (ACC) cortices, amygdala, hypothalamus and the periaqueductal gray (PAG) region (Scheitz et al. 2020; Silvani et al. 2016). These brain regions alter ANS (both SNS and PNS) and HPA axis activity to regulate cardiovascular function (e.g. HR) (Dampney 2016). The insular cortex is a viscerosensory and -motor brain area (Nagai et al. 2010), highly connected to the cortex, thalamus, amygdala and hippocampus. External somatosensory information transmits to the agranular insula integrating with cardiac afferent input received by the posterior granular and mid-dysgranular insular cortex (Ceunen et al. 2016; Nieuwenhuys 2012). Along with ACC and amygdala, the insula mediates interoception i.e. the awareness of internal bodily states such as cardiac palpitations in panic disorder (Craske et al. 2010; Khoury et al. 2018). The ACC (Gillies et al. 2019) connects to the hypothalamus and PAG and associates with sympathetic modulation of HR (Critchley et al. 2003). The PAG itself encapsulates the midbrain cerebral aqueduct connecting descending and ascending projections concerning emotion-related and motor information (Vianna and Brandao 2003). The hippocampus and amygdala connect to the hypothalamic paraventricular nucleus (PVN) of the HPA axis and respond to cortisol through glucocorticoid receptors. Both regions are involved in memory and mood, the former particularly in fear memory. The thalamus and cortex connect to the central amygdala in response to stressful experiences and the parvocellular PVN neurons adjust the SNS outflow to the heart facilitating a “fight or flight” response, (Ferguson et al. 2008).
Feedback control involves brainstem ANS nuclei mediating reflex effects in response to peripheral receptor input (Fig. 1). The medullary nucleus of the solitary tract (NTS) receives baroreflex information concerning cardiovascular feedback regulation controlling arterial pressure. NTS activation decreases blood pressure and HR. It is highly connected to the pons parabrachial nucleus that transmits cardiovascular information to forebrain regions increasing SNS activity and tachycardia (Davern 2014). Feedback control includes also the aforementioned nucleus ambiguous from where PNS vagal cardiac outflow stems (Dampney 2016).
Evidence implicating abnormal CAN and ANS in NPD
The neuroanatomical organization of the CAN permits psychological states to influence cardiovascular ANS control via or even bypassing the brainstem homeostatic nuclei. Thus, HRV, the HR beat-to-beat variability measured in an electrocardiogram (ECG), is a valuable non-invasive ANS index in humans and animal models (Laborde et al. 2017; Thayer and Lane 2000; Thireau et al. 2008). Given this and the high heritability of this trait, it has potential as an NPD endophenotype (Golosheykin et al. 2017). Thus, we here describe several, albeit at times controversial, lines of evidence connecting HRV and hence abnormal ANS in anxiety/post-traumatic stress disorder (PTSD), MDD and SCZ.
In terms of anxiety, laboratory stressors increase SNS and decrease PNS cardiovascular control with fight-or-flight activation (Berntson et al. 1994; Pagani et al. 1991; Sloan et al. 1996). This state manifests as increased low frequency (LF)-HRV (reflecting baroreceptor reflex modulation and both SNS and PNS activity) and decreased high frequency (HF)-HRV (reflecting PNS activity) power or an increased LF/HF ratio (Goldstein et al. 2011; Reyes del Paso et al. 2013). Consistent with autonomic inflexibility, evidence indicates decreased HF-HRV across several anxiety disorders including panic disorder (PD), generalized anxiety disorder (GAD), social anxiety and obsessive–compulsive disorder (OCD) (Chalmers et al. 2014; Pittig et al. 2013). The findings for PTSD have been less consistent however, limited by small sample sizes with diverse individual patient experience (Dennis et al. 2014; Ge et al. 2020). Abnormal function of CAN brain regions mediating executive function likely underlies the associated aberrant HRV (Lee et al. 2022). While the amygdala activates in fear conditioning (LaBar et al. 1998) transmitting brief exposure information, the more general anxiety states require the medial PFC input to maintain protracted attentional focus on threat-related cues (Eippert et al. 2007).
MDD is generally associated with decreased HF-HRV (Jangpangi et al. 2016; Koch et al. 2019; Moretta and Messerotti Benvenuti 2022) yet the relationship between ANS function and disease severity is complex (Sarlon et al. 2021). A deeper understanding of this connection is particularly germane given that MDD is a risk for CVD (Correll et al. 2017). The pathological origin of altered HRV in MDD is not clear although comorbid anxiety disorder may be partially responsible. Depressive states are associated with obstructed communication between ACC and brainstem ANS nuclei (Critchley et al. 2005; Makovac et al. 2015; Ruiz-Padial et al. 2011). In addition, depression severity correlates with vagal tone loss highlighting the value of HRV as an MDD metric for which vagal nerve stimulation is a proposed treatment (O'Reardon et al. 2006). Takotsubo cardiomyopathy further implicates severe anxiety and depressive states and is associated with reduced thickness of the insula and ACC (Hiestand et al. 2018).
The data available for HRV in SCZ is less consistent although of immense potential. Thayer and Lane (Thayer and Lane 2000) proposed a so-called Neurovisceral Integration Model to denote the utility of HRV as a proxy index of PFC function and cognitive ability. The PFC inhibits SNS activation thereby augmenting vagal tone and altered PFC function directly reflects in HRV measures. Specifically, HF-HRV aligns with increased blood flow to the PFC and ACC (Thayer et al. 2012). These brain regions mediate working memory, executive control of attentional shifting, decision-making and sociability that are impaired in SCZ (Morris et al. 2013). In general, high HRV is associated with improved executive functioning (Hansen et al. 2004) as well as superior stress resilience with low HRV, the opposite (Pulopulos et al. 2018). HRV decreased in SCZ patients correlating with symptom severity thereby emphasizing the benefit as a dependent variable in cognitive analysis (Morris et al. 2013). In general, despite this available information, supporting evidence is limited and gaps remain in understanding the genetic underpinnings of CAN-based ANS and HRV control and disease risk.
Leveraging large-scale preclinical functional genetic data to gain insight into CAN/ANS in NPD
A promising approach to identify new disease biomarkers and therapeutic targets is to pin-point novel candidate genes that, when mutated, cause abnormal CAN and ANS activity augmenting NPD risk. While the lack of holistic clinical interdisciplinary data impedes heart/brain axis understanding (Valenza et al. 2016), the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) nonetheless advocates for integrated psychiatric patient care considering medical and mental conditions in parallel (American Psychiatric Association 2022). As a move in this direction, the IMPC resource (Brown and Moore 2012) provides open access to large-scale multi-systemic experimental data from single knockout mouse lines generated for each protein-coding gene in the genome [see www.mousephenotype.org, 8916 genes annotated to date, Data Release (DR) Version 17.0, (Brown and Moore 2012)]. Utilizing data contained therein can reveal molecular mechanisms not easily detectable in a clinical setting, especially in the case of brain disease. It is thus a valuable tool to understand heart/brain interaction in NPD.
We introduce here a rationale for distillation of this large-scale data to prioritize candidate genes involved in heart/brain axis control. Recently, Spielmann et al. (2022) exploited IMPC cardiovascular data (3894 single-gene null deletion alleles) to establish 705 CVD risk genes, associated with ECG and/or trans-thoracic echocardiography (TTE) phenotypes in young adult mice (12-weeks of age). This included 486 genes with no former cardiac dysfunction association causing cardiac rhythm disorder, cardiomyopathies, or structural heart defects. Given that ECG parameters (HR/HRV) potentially index CAN and PFC function, and that a similar parameter and diagnostic can be applied to humans and mice, we implemented a unique stepwise refinement of this ECG gene set. The goal was to derive novel NPD insight from an initial CVD risk starting point. To this end, we capitalized on the assertion that analysis of gene expression can infer function for a range of tissues (Hume et al. 2010; Mabbott et al. 2013). Thus, combining hierarchical clustering of the corresponding ECG gene CAN regional brain expression data with functional enrichment analysis, we gathered and characterized candidate genes likely involved in modulating cardiovascular activity via the CAN. Furthermore, with subsequent ‘support vector machine’ inquiries and literature validation, we deduced 32 CAN-expressed genes altering HR/HRV for future NPD empirical validation.
Stepwise design and methods applied
A summary of our stepwise analysis design appears in Fig. 2. Spielmann et al. (2022) also detailed the 705 cardiovascular dysfunction genes identified (from IMPC DR10.1), the mouse lines used and the analyses performed. We focused on the ECG gene set and implemented mouse-brain in situ hybridization (ISH) raw values i.e. expression energies and corresponding brain tissues from the mouse Allen Brain Atlas (ABA) (Lein et al. 2007) that yielded this information for 2426 defined brain areas focusing on data from sagittal sections. Of the 462 genes associated with an ECG phenotype, we could obtain unique expression data for 418. Gene expression energy data of the whole mouse brain were downloaded via the Allen Brain Atlas application programming interface (API) (brain-map.org/api/index.html, following “Example Queries for Experiment Metadata”, database update March 04, 2021) by using custom-written bash scripts. We then performed a global unsupervised hierarchical clustering analysis, first focusing on all brain areas with all genes for each phenotype (Fig. S1) and then with CAN brain regions (Fig. 3A) as described previously [Feedforward (FF-ANS) and feedback (FB-ANS) control, (Dampney 2016)].
Fig. 2.
Shows the workflow and stepwise design used for characterization of the ECG gene set identified by (Spielmann et al. 2022). We first performed an unsupervised hierarchical clustering analysis of brain regions and gene expression data from 418 ECG genes, using all brain regions and then with 47 central autonomic network (CAN) relevant brain regions obtained from the Allen Brain Atlas. We then implemented Enrichr to perform gene set enrichment analysis on the two clusters of genes identified for functional annotation purposes. The two clusters were designated “FF-ANS” for feedforward and “FB-ANS” for feedback control to denote genes involved in either form of cardiovascular function in the CAN. We focused on human disease and Mammalian Phenotype annotations from the MGI database for validating our clustering algorithm. We used the mSVM-RFE method to identify the top 99 hub genes from all 418 genes. Using manual curation, we then focused on FF genes that caused heart rate (HR) or heart rate variability (HRV) phenotypes in mice to identify genes that influence ECG activity via the CAN and we earmarked poorly annotated genes as those potentially novel heart/brain axis genes in neuropsychiatric disease (Created with Biorender.com)
Fig. 3.
A Dendrogram and heat map of the unsupervised hierarchical clustering analysis of 47 central and brainstem autonomic nervous system (ANS) relevant brain regions and gene expression data from 418 electrocardiogram (ECG) genes. The columns each represent individual brain areas and the rows represent each gene (z-scores calculated across rows). There were 7 brain region clusters (C1-7) and 2 ECG gene clusters designated “FF-ANS” for feedforward and “FB-ANS” for feedback control of cardiovascular ANS function. Red and blue reflect up and downregulated expression levels, respectively, within each brain structure relative to all the other brain structures. B-D Bar charts of top enriched terms from the MGI Mammalian Phenotype terms level 4 2021, Jensen diseases and Enrichr submissions TF-gene co-occurrence gene set libraries respectively for feedforward (FF-ANS) and feedback (FB-ANS) control clusters. The top 10 enriched terms for the input gene set are displayed based on the -log10(p-value), with the actual p-value shown next to each term. The asterisk indicates significance related to the adjusted p-value. The term at the top has the most significant overlap with the input query gene set. The graphs were generated using the Enrichr interface: https://maayanlab.cloud/Enrichr/
The clustering algorithm grouped the ECG genes into discrete clusters with similar brain region expression. For the generation of the heat maps, we used the R package ComplexHeatmap. Agglomerative hierarchical clustering by the Heatmap function (clustering_method_columns = “ward.D2” and clustering_method_rows = “ward.D2”) was applied to group mouse brain regions (columns) as well as expression energies of genes (rows) for the heat map. The genes with the most similar expression patterns are closest in proximity in the heat map with rows scaled and represented as a z-score. The red color denoted higher expression levels and the blue had lower expression levels. We included the dendrogram for the columns, where we highlighted the subtrees with numbers (C1 and 2 for Fig. S1 and C1-7 for Fig. 3A). In addition, in Fig. 3A, we annotated the x-axis with the brain regions relevant for CAN feedforward and feedback regulation of cardiovascular function. We used the silhouette method by the function fviz_nbclust from the R package factoextra to determine this optimal number of clusters.
For gene set enrichment analysis of the clusters, we used the Enrichr web server that encompasses a broad set of libraries for analysis including information from MGI Mammalian Phenotype Level 4 2021 (that incorporated IMPC multi-systemic phenotypic data from the corresponding null mouse lines), Jensen Diseases and Enrichr Submissions TF [transcription factor]-gene co-occurrence (Chen et al. 2013; Kuleshov et al. 2016). To validate the results of our clustering algorithm, we used also a multiclass support vector machine with recursive feature elimination (mSVM-RFE) to identify the top genes defining the clusters of adult brain structures (Augustin et al. 2011). This method works through R package e1071 and assesses how often the expression pattern of a respective gene correctly classifies specified brain tissues (7 classes in this case) from randomly drawn subsets of the original dataset. First, expression energies of 7 clusters C1-7 resulting from hierarchical clustering were randomly grouped into stratified four folds by using all combinations of three folds, which results in four combinations for mSVM-RFE. This grouping was completed fifty times arising in a total of 200 mSVM-RFE runs or 200 different gene selections in the end. mSVM-RFE starts with all 418 gene expression profiles (i.e. features) and ends up with 15 representing the stop condition for iterations. In each run, mSVM-RFE recursively eliminates 10% of the remaining expression values, which are not good enough for classification according to the cost function of the SVM classifier. The SVM function in R was used with default settings except the parameters type = “C-Classification”, kernel = “linear” and cost = 0.01.
Results—clustering based on brain expression and enrichment analysis of ECG-related genes
We clustered 418 ECG genes focusing on 47 predefined brain regions recruited for feedforward or feedback CAN control responses as summarized in see “An overview of heart/brain communication via CAN—feedforward and feedback ANS control” section (Fig. 3A, clustering based on all brain areas shown in Fig. S1) (Dampney 2016). We identified two main ECG gene clusters (designated “FF-ANS” [feedforward] and “FB-ANS” [feedback]) based on relative expression within seven CAN-relevant brain structure clusters (C1-7, See Supplementary information for gene list). FF-ANS consisted of 212 ECG genes with the highest expression in mainly the amygdaloid and hippocampal subfields as well as the insular and cingulate cortical areas (highest in clusters C1, C3 and C4 with relatively lower expression in C2). The FB-ANS cluster comprised 206 genes with the highest expression in brainstem nuclei (cluster C5), more variable in feedforward brain areas (C1-4 and C6-7 hypothalamic and thalamic subnuclei).
We hypothesized that the FF-ANS expressed genes influence ECG activity by mediating effects of cognitive and emotion-related higher brain function. The FB-ANS genes, on the other hand, were potentially active in response to cardiovascular baroreflex information. Consistent with our hypothesis, the top enriched mammalian phenotype (MP) terms associated with FF-ANS genes related to behavioral brain function. These included hyperactivity, abnormal sleep behavior, decreased exploration of a new environment, decreased startle reflex and impaired sensorimotor gating [decreased prepulse inhibition] (Fig. 3B, tables of genes in Supplementary information). Preweaning lethality complete and incomplete penetrance also enriched within the FF-ANS gene set suggesting a strong essential developmental role for a subset. Confirming our initial gene selection based on ECG phenotypes, increased heart rate, shortened ST segment and shortened RR interval were also among the top enriched MP terms (Fig. 3B). The top enriched related disease within the FF-ANS gene set was “Mental Depression” (Fig. 3C) and the most significant transcription factor-gene co-occurrence were POGZ and ASH1L (Fig. 3D). Pogo transposable element derived with ZNF domain (POGZ) is the most frequently de novo mutated gene in neurodevelopmental disorder patients including ASD (De Rubeis et al. 2014; Matsumura et al. 2020; Sanders et al. 2015; Ye et al. 2015). ASH1-Like Histone Lysine Methyltransferase (ASH1L) is also a major ASD risk factor with decreased PFC levels evident in post-mortem ASD patients (Qin et al. 2021). The FF-ANS cluster is comprised therefore of cognitive and emotion-related behavior and disease genes indicating that our algorithm has gathered a gene set with potential NPD relevance.
Conversely, the FB-ANS gene set did not enrich for behavior but rather ECG-related phenotypes such as shortened RR interval, increased HR and abnormal sinus arrhythmia (Fig. 3B). Pre-weaning lethality complete penetrance was overrepresented albeit concerning fewer genes than in FF-ANS (38 genes in the case of FB-ANS while 50 genes in the corresponding FF-ANS category). There were no strong disease or transcription factor-gene co-occurrence associations (i.e. significant with adjusted P value [Padj], Fig. 3C and D). Nevertheless, “coronary artery disease” and “reflex sympathetic dystrophy” featured among the top enriched disease terms with unadjusted significance that were not significantly enriched in FF-ANS disease terms (Fig. 3C). This profile indicates that FB-ANS genes are involved in cardiovascular reflex responses. Overall, our combined hierarchical cluster and enrichment analysis identified two gene sets based on brain-region expression profiles with distinct functional and disease enrichments.
Support vector machine inquiry and literature classification of top CAN expressed ECG genes
To validate our clustering approach, we used a support vector machine (mSVM-RFE) to pinpoint the top expressed genes defining the clusters (Augustin et al. 2011). We extracted 99 in total across both clusters, FF-ANS (55 genes) and FB-ANS (44 genes, Full list of genes in Supplementary information). We then used existing mouse and human data and literature concerning the top 5 cluster discriminating genes to confirm that the analysis gathered genes with similar functions and NPD relevance. The top FF-ANS genes were Satb2, Stx1a, Adnp2, Ust and Acap2. Both Satb2 and Stx1a are highly expressed in the adult mouse ACC and insular cortices (Fig. 4A and B). The former encodes SATB homeobox 2 (SATB2) protein and the latter, syntaxin 1A. SATB2 functions during mouse brain development (Britanova et al. 2008) and both SATB2 and STX1A function in the adult brain and are associated with SCZ (Jaitner et al. 2016; Whitton et al. 2018; Wong et al. 2004). The genes Adnp2, Ust and Acap2 are highly expressed in the hippocampus and Adnp2 also in the amygdala (Fig. 4A and B). Adnp2 encodes the activity-dependent neuroprotective protein (ADNP2), expressed during development and associated with ASD and SCZ (Dresner et al. 2011; Helsmoortel et al. 2014; Van Dijck et al. 2019). Ust encodes the protein uronyl 2-sulfotransferase (UST) (Nikolovska et al. 2015), which is downregulated in MDD (Oommen et al. 2021). Acap2 encodes ArfGAP with coiled-coil, ankyrin repeat and PH domains 2 (ACAP2) protein with no prior NPD annotations. Thus, four of the top five ECG genes within CAN brain structures (FF-ANS) have previous NPD associations.
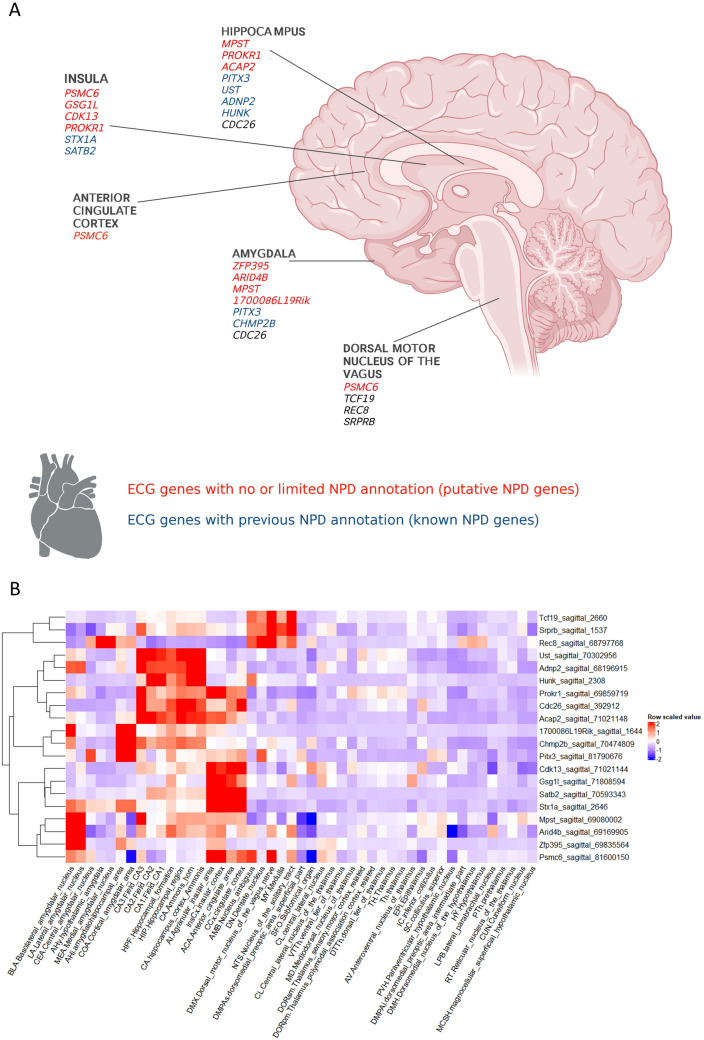
Fig. 4.
Schematized overview of established and putative neuropsychiatric disease (NPD) genes identified based on brain central autonomic network (CAN) expression clustering of cardiovascular disease risk electrocardiogram genes. A Depicts the established (blue text) and putative (red text) NPD genes and the CAN brain regions with the highest expression. B Shows a dendrogram and heat map of the top FF-ANS and FB-ANS cluster expressed ECG genes. The columns each represent an individual brain area and the rows represent each gene (z-scores calculated across rows). Red and blue reflect up and downregulated expression levels, respectively, within each brain structure relative to all the other brain structures (A was created with Biorender.com)
The top FB-ANS cluster genes were Rec8, Cdk13, Srprb, Hunk and Tcf19. All three of the genes Rec8 (encoding REC8 meiotic recombination (REC8) protein), Srprb (encoding signal recognition particle receptor subunit beta (SRPRB) protein) and Tcf19 (encoding Transcription Factor 19 protein) while exhibiting relatively higher brain expression in the brainstem nuclei (Fig. 4A and B) are higher expressed in other tissues (Rec8: testis, Srprb: pancreas, bones, Tcf19: immune cells, oesophagus, see www.proteinatlas.org). Figure 4B illustrates the distinct mouse expression pattern where the left Y-axis dendrogram shows a clear separation of these three genes from the remainder. Moreover, they do not have previous CNS disease implications and ablation did not alter behavior. The remaining two genes, Cdk13 (encodes cyclin-dependent kinase 13 (CDK13) enzyme) and Hunk (encodes Hormonally Up-Regulated Neu-Associated Kinase (HUNK) protein) express in adult mouse insular/cingulate cortices and hippocampus respectively (Fig. 4A and B) as well as in other adult tissues (Cdk13: gastrointestinal tract, kidney, Hunk: multiple tissues, www.proteinatlas.org). Nevertheless, at least one of these genes plays a developmental disorder role (Hamilton and Suri 2019). In summary, the top FB-ANS cluster ECG genes do not have strong previous CNS disease associations with exceptions related to aberrant development. Furthermore, the higher relative expression of these genes outside the adult brain is consistent with the lack of brain disease connections and indicates that the clustering analysis has grouped genes with more limited adult brain expression and function and/or confined to a feedback regulatory role in cardiovascular function. This information concerning the FF-ANS and FB-ANS clusters further confirms the validity of our clustering approach to identifying potentially novel NPD-relevant genes associated with abnormal cardiovascular/autonomic function.
Novel insights from altered HR/HRV with hyperactivity to index CAN dysregulation
Given the HR/HRV and CAN/ANS connection, we manually identified the top CAN-expressed ECG genes associated with abnormal HR/HRV (32 genes, Table 1, see Supplementary information for gene lists and 23 genes associated with altered heart rhythm QRS and QTc parameters). These enriched for the mouse phenotype “hyperactivity”, which is of interest in terms of implementing HRV as a proxy for PFC function as proposed by the Neurovisceral Integration Model (Thayer and Lane 2000). Hyperactivity is at least partially emblematic of impaired inhibitory PFC influence on inappropriate behavior and attention (Ma et al. 2005) as well as impaired parasympathetic vagal tone and sympathetic overdrive. Decision-making and impulse control ability rely on maintaining a balance between movement initiation and inhibition in response to extraneous stimuli necessitating intact PFC activity (Hardung et al. 2017). Eleven of the 32 CAN expressed genes increased HR, eight of which exhibit no or limited previous NPD annotation (Table 1). This highlights how our clustering of the HR-altering ECG genes based on CAN brain expression successfully identified known and potentially novel NPD-related genes of which we will now focus on specific examples.
Table 1.
Top feedforward (FF) ANS expressed genes affecting electrocardiogram (ECG) activity
| Gene identifier | Mouse ECG phenotype | Mouse behavioral phenotype | Human neuropsychiatric disease (NPD) association from GWAS catalog 2019 and MGI enriched terms |
|---|---|---|---|
| Psmc6 | HR ↑ HRV↓ | Hyperactivity, decreased thigmotaxis | Limited or no NPD annotations |
| 1700086L19Rik | rMSSD, HRV↓ | Hyperactivity | Limited or no NPD annotations |
| Mpst | PQ ↓,HR ↑,PR ↓ | Decreased exploration of a novel environment, increased latency to center entry, hypoactivity | Limited or no NPD annotations |
| Mdp1 | HR ↑ | Increased latency to the first transition into the dark in light/dark box, decreased % prepulse inhibition | Bipolar disorder, mood disorder |
| Gsg1l | HR ↓ (F),HR ↑ (M),RR ↑ (F),RR ↓ (M) | Hyperactivity, decreased startle response | Limited or no NPD annotations |
| Cdc26 | HR ↑ | Increased prepulse inhibition | Limited or no NPD annotations |
| Chmp2b | HR, RR ↑ | Abnormal freezing behavior in fear conditioning | Tourette's syndrome or obsessive–compulsive disorder, frontotemporal dementia |
| Pitx3 | HR ↑,ST, RR, QTc ↓ | Hyperactivity, Increased coping response, decreased vertical activity, decreased exploration of a novel environment | Cognitive ability, Parkinson’s disease |
| Prokr1 | HR ↑,RR ↓, rMSSD ↑ | No | Limited or no NPD annotations |
| Arid4b | HR,QRS ↑ | Decreased centre time | Limited or no NPD annotations |
| Zfp395 | HR ↑ST,RR ↓ | Hyperactivity | Limited or no NPD annotations |
| Stx1a | PQ↑,HR↓,ST,rMSSD,RR ↑HR_TTE ↓ | No | Disease of mental health |
| Hipk3 | HR ↓,RR, HRV ↑ | Decreased startle, hypoactivity, decreased prepulse inhibition, increased acoustic brainstem response thresholds | Limited or no NPD annotations |
| Srsf11 | HRV ↑ | Decreased prepulse inhibition | Limited or no NPD annotations |
| Tnnc1 | HRV ↑ | No | Feeling worry, Bipolar disorder, Autism spectrum disorder or schizophrenia |
| Kbtbd7 | HR ↓,RR ↑ | Hyperactivity, decreased thigmotaxis | Limited or no NPD annotations |
| Rasgef1a | HR ↓, RR↑ | Increased vertical activity | Recurrent major depressive disorder |
| Cap2 | HR↓,ST, rMSSD, RR, QTc ↑ | No | Limited or no NPD annotations |
| Bclaf1 | rMSSD ↑ | Hyperactivity | Limited or no NPD annotations |
| Entpd1 | rMSSD ↑ | No | Limited or no NPD annotations |
| 4931406C07Rik | HR ↓ rMSSD, HRV ↑ | No | Limited or no NPD annotations |
| Fbxl16 | ST, RR, QTc, HR_TTE ↑ HR_TTE ↓, HRV ↑ | Unresponsive to tactile stimuli | Attention deficit hyperactivity disorder |
| Atn1 | rMSSD, HRV ↑ | Limb grasping, decreased exploration of novelty | Limited or no NPD annotations |
| Lpin3 | HR ↓,RR ↑ | No | Limited or no NPD annotations |
| Dnase1l2 | HR ↓,RR ↑,LVIDd, LVIDs ↓ | Abnormal vocalisation, decreased grip strength, abnormal motor capabilities/coordination/movement, hypoactivity, small superior vagus ganglion | Limited or no NPD annotations |
| Spred3 | HRV ↑ | Increased freezing behavior, decreased prepulse inhibition | Limited or no NPD annotations |
| Grm7 | HR ↓,RR ↑ | Hyperactivity, increased grip, decreased anxiety-related behavior, limb grasping | Recurrent major depressive disorder, Clozapine-induced agranulocytosis/granulocytopenia in treatment-resistant schizophrenia, Personality traits in bipolar disorder, Major depressive disorder (broad), Panic disorder, Neurodevelopmental disorder with seizures, hypotonia, and brain abnormalities |
| Cyp27a1 | HR,QRS↓,RR ↑ | No | Limited or no NPD annotations |
| Agpat1 | HR ↓,rMSSD, RR, HRV ↑ | No | Clozapine-induced agranulocytosis/granulocytopenia in treatment-resistant schizophrenia, Autism spectrum disorder or schizophrenia |
| Ctsd | ST,RR ↑ | No | neuronal ceroid lipofuscinosis |
| P3h1 | HR ↓,RR ↑ | Decreased grip strength | Limited or no NPD annotations |
| Pnmt | QTc Dispersion, rMSSD ↑ | Increased startle response, decreased exploration of novel environment, decreased breath rate during sleep | Limited or no NPD annotations |
Table shows the top ECG genes with the highest expression in the cluster FF-ANS representing feedforward central autonomic network (CAN) brain structures from Allen Brain Atlas. Also shown are the ECG and behavioral phenotypes associated with the mouse knockout (KO) lines for each gene as well as the human neuropsychiatric disease annotations
HR heart rate, HRV heart rate variability, RR R-R interval, ST, QTc, QRS ST, QTc, QRS intervals in electrocardiogram (ECG), TTE transthoracic echocardiography, rMSSD root mean square of successive differences between heart beats, shaded indicates increased HR and/or decreased HRV phenotypes in the corresponding knockout mouse line in IMPC. Neuropsychiatric disease associations are italicised
Of the HR-altering CAN genes, two also decreased HRV, Psmc6 and 1700086L19Rik. Psmc6 encodes the 26S protease regulatory subunit S10B protein, a part of the 19S proteasome complex involved in cellular proteome homeostasis. It is highest expressed in the mouse adult insula and ACC as well as the dorsal motor nucleus of the vagus nerve (Fig. 4A and B). While there are limited established NPD associations, there is a link, albeit not widely researched, between PSMC6 and the pre-symptomatic stage of Huntington’s neurodegenerative disease [HD (Xiang et al. 2020)]. This phenotypic pattern, therefore, indicates that hyperactivity and reduced HRV due to mouse Psmc6 KO could translate as an early harbinger of impaired PFC activity in HD patients with PSMC6 mutation. Behavioral alterations including decreased concentration and decision-making ability with mood disorder characterize the pre-symptomatic stage of HD (Kirkwood et al. 2001) consistent with the mouse hyperactivity phenotype with gene ablation. A similar hyperactivity/decreased HRV pattern was evident with KO of 1700086L19Rik. This gene has no or minimal functional or NPD annotation to date however the decreased HRV/hyperactivity phenotypes seen with loss-of-function again suggest altered sympathetic/parasympathetic balance and potentially impaired PFC and CAN function (highest expression in the mouse basolateral and cortical amygdala, Fig. 4A and B). Based on phenotype similarity, IMPC predicted psychiatric disease associations including ADHD, SCZ and neurodevelopmental disorder (https://www.mousephenotype.org/data/genes/MGI:1921534). Thus, 1700086L19Rik is a potential novel NPD-risk gene predicted by our clustering algorithm, related to CAN and autonomic dysfunction that is of interest for future detailed investigation.
Three additional CAN/FF-ANS genes revealed through our clustering analysis increased HR and caused hyperactivity on ablation in mice: Pitx3 (Pituitary homeobox 3), Gsg1l (Germ Cell-Specific Gene 1-Like Protein) and Zfp395 (zinc finger protein 395). Pitx3 expresses in midbrain dopaminergic neurons (highest adult CAN expression in the central and cortical amygdala, Fig. 4A and B) and is involved in Parkinson’s disease pathogenesis (Le et al. 2011; Li et al. 2009). Predictions indicate that GSG1L plays a role in AMPA receptor activity regulation in the hippocampus with the highest CAN expression in the insula and ACC (Fig. 4A and B) (Gu et al. 2016). Abnormal dopaminergic and glutamatergic activity leads to CAN dysregulation and thus the associated phenotype pattern described here emphasizes the value of HR measurement as an early index of aberrant CAN activity. ZFP395 (also known as HD Gene Regulatory Region-Binding Protein 2) is located in the HD gene promotor region (Tanaka et al. 2004). There is some scant empirical data implicating this gene in HD however this phenotypic pattern of increased HR/hyperactivity and the highest expression in the basolateral and lateral amygdala (Fig. 4A and B) again suggests CAN dysregulation for further investigation related to this disease. These examples illustrate how likely dysregulation of the CAN in parallel disinhibits sympathetic drive and impairs parasympathetic vagal tonic control of HR. Thus, the combination of mouse hyperactivity and HR/HRV signifies likely CAN disruption including PFC and hippocampal impairments. The remaining CAN-expressed genes gathered by our clustering algorithm with increased HR (Mpst, Arid4b, Mdp1, Cdc26 and Chmp2b), high amygdala and hippocampal expression (Fig. 4A and B) and mouse behavior phenotypes (abnormal sensorimotor gating, emotionality, Table 1) are therefore additional genes where HR likely signifies aberrant CAN function and are a mixture of known and possibly novel NPD genes of interest.
The picture for increased mouse HRV and altered behavior associated with CAN-expressed gene clustering is less clear (Table 1). Nevertheless, these cases likely involve brainstem abnormality rather than higher CAN dysfunction. For example, Hipk3 [Homeodomain Interacting Protein Kinase 3 (HIPK3) protein] is highly expressed in the heart and the IMPC predicts a role for this gene in the ANS disease Neuropathy, Hereditary Sensory and Autonomic, Type Vi (https://www.mousephenotype.org/data/genes/MGI:1314882). Moreover, loss of the mouse genes Spred3 [Sprouty Related EVH1 Domain Containing 3 (SPRED3) protein] and Fbxl1 (F-box/LRR-repeat protein) increase HRV and alter emotionality requiring further investigation to determine the disease relevance.
Summary and conclusion
Evidence implicates heart/brain axis and CAN/ANS dysfunction in NPD yet there remain gaps in understanding the genetic underpinnings as well as in delineating potential therapeutic targets. Moreover, HRV, as an index of intact CAN-ANS interaction, is a highly heritable trait and putative non-invasive proxy of higher brain function and NPD endophenotype (Golosheykin et al. 2017). Mouse multi-systemic data has the potential to yield relevant and innovative NPD therapeutic insights not feasible yet in a clinical setting. Therefore, we provided here a rationale for tackling large-scale mouse genetic data in the public domain to gain insights into heart/brain axis control in NPD. As a unique approach, our initial gene set concerned abnormal ECG and CVD risk to distinguish potential NPD genes related to abnormal CAN/ANS. To that end, we introduced a stepwise refinement of the extensive aberrant ECG gene set. Combining hierarchical clustering of regional brain expression levels and enrichment analysis of these genes, as well as support vector machine and literature classification, we determined CAN-associated genes with NPD relevance. Furthermore, we isolated a candidate gene set highly expressed in CAN brain areas that also alter HR and/or HRV (32 of the top 99 expressed genes) and a combination of known and putative NPD genes. Our in silico validation showed that the clustering algorithm has reliably predicted established NPD genes and thus application of this well-defined pipeline to new ECG gene sets will reveal potentially novel NPD-related genes. In addition, the association of specific genes with a combination of HR/HRV alterations and novelty-induced hyperactivity represents a multimodal biomarker relevant for executive brain function and NPD, useful for isolating CAN genes of interest from the large-scale mouse data.
While this was a first step and an introductory prediction based on a limited set of ECG genes, we did uncover a poorly annotated gene 1700086L19Rik underlying a hyperactivity/decreased HRV combined phenotype with relatively high amygdala expression. The likely influence of the encoded protein on CAN amygdala activation in response to stress exposure indicates a potential NPD pathogenic role for further deep investigation. A more in-depth analysis, applicable to any elucidated genes of interest, will necessarily entail preclinical experimental validation incorporating additional genetically engineered mouse models and more targeted technologies. As a whole body gene KO yielded this initial insight, follow up studies will require more spatially- and temporally-controlled gene KO (or knock-in) in CAN brain regions using, for example, the conditional Cre/LoxP system. In this case, a brain-specific (particularly forebrain) transgenic Cre line, e.g. calcium/calmodulin-dependent protein kinase II alpha subunit (CaMKIIα)-Cre, can be implemented in concert with functional assays to ascertain whether HRV abnormality associated with specific genes is secondary to CAN dysfunction. Alternatively, viral vector approaches such as the AAV vector-based RNA interference systems can be applied to similar effect (Kim et al. 2022). Given the therapeutic potential of sympatho-vagal balance restoration, it will be advantageous to assess the efficacy of vagal nerve stimulation as well as that of other pharmacological ANS modulatory agents and exercise on behavioral and cardiovascular abnormality in these models (van Bilsen et al. 2017).
The question then is how best to translate the validated preclinical heart/brain axis genetic control findings to human NPD patients. Our analysis confirms the importance of holistic multi-systemic analysis both for NPD and CVD patients, considering the neuropsychiatric etiology of altered HR/HRV (Shivkumar et al. 2016). Should HRV be linked to NPD genetic modifications it then represents a powerful trans-diagnostic and stratification tool as well as a treatment response metric. Effective application of this knowledge to patients therefore requires availability of genomic screening and ECG data and consideration of medical and mental conditions in parallel as advocated by DSM-5 (American Psychiatric Association 2022). Preclinical precision genetic models, generated for NPD patient-specific variants, can be analysed to determine the likely efficacy of ANS interventions.
The volume of IMPC mouse gene KO data will continue to expand to encompass all protein-coding genes in the genome. One limitation of this resource is that HRV analysis is not mandatory and so not available for all genes. Moreover, this mouse high-throughput measurement provides a first indication that will be confirmed with more robust techniques such as telemetry. These limitations aside, we expect additional CAN target elucidation for which this stepwise design will identify relevant NPD genes. Moreover, similar analyses of the associated cardiac rhythmic disorder and TTE gene sets identified previously (Spielmann et al. 2022) will provide complementary information. The role of the insular cortex and heartbeat-evoked potentials is also of interest for future investigation. Heartbeats can modulate conscious perception by augmenting heartbeat-evoked neural activity and this aligns with impaired somatosensory perception related to interoception (Al et al. 2020). Consonant genetic target identification will yield anxiety and mood disorder information. Overall, the potential insights garnered from the preclinical data will include prioritization of GWAS loci as well as application to digital phenotyping, NPD diagnosis and risk stratification for precision psychiatry approaches.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
L.G. and D.T. wrote the main manuscript text and prepared the figures. D.T. performed the bioinformatic analysis. All authors reviewed the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. German Federal Ministry of Education and Research (Infrafrontier grant 01KX1012 to MHdA); German Center for Diabetes Research (DZD) (MHdA).
Declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lillian Garrett and Dietrich Trümbach have contributed equally.
References
- Al E, Iliopoulos F, Forschack N, Nierhaus T, Grund M, Motyka P, Gaebler M, Nikulin VV, Villringer A. Heart-brain interactions shape somatosensory perception and evoked potentials. Proc Natl Acad Sci USA. 2020;117:10575–10584. doi: 10.1073/pnas.1915629117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2022) Diagnostic and statistical manual of mental disorders (5th ed., text rev.). 10.1176/appi.books.9780890425787
- Atladottir HO, Parner ET, Schendel D, Dalsgaard S, Thomsen PH, Thorsen P. Time trends in reported diagnoses of childhood neuropsychiatric disorders: a danish cohort study. Arch Pediatr Adolesc Med. 2007;161:193–198. doi: 10.1001/archpedi.161.2.193. [DOI] [PubMed] [Google Scholar]
- Atladottir HO, Gyllenberg D, Langridge A, Sandin S, Hansen SN, Leonard H, Gissler M, Reichenberg A, Schendel DE, Bourke J, Hultman CM, Grice DE, Buxbaum JD, Parner ET. The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. Eur Child Adolesc Psychiatry. 2015;24:173–183. doi: 10.1007/s00787-014-0553-8. [DOI] [PubMed] [Google Scholar]
- Augustin R, Lichtenthaler SF, Greeff M, Hansen J, Wurst W, Trumbach D. Bioinformatics identification of modules of transcription factor binding sites in Alzheimer's disease-related genes by in silico promoter analysis and microarrays. Int J Alzheimers Dis. 2011;2011:154325. doi: 10.4061/2011/154325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Thayer JF. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int J Psychophysiol. 2015;98:338–350. doi: 10.1016/j.ijpsycho.2015.08.004. [DOI] [PubMed] [Google Scholar]
- Berntson GG, Cacioppo JT, Binkley PF, Uchino BN, Quigley KS, Fieldstone A. Autonomic cardiac control. III. Psychological stress and cardiac response in autonomic space as revealed by pharmacological blockades. Psychophysiology. 1994;31:599–608. doi: 10.1111/j.1469-8986.1994.tb02352.x. [DOI] [PubMed] [Google Scholar]
- Britanova O, de Juan RC, Cheung A, Kwan KY, Schwark M, Gyorgy A, Vogel T, Akopov S, Mitkovski M, Agoston D, Sestan N, Molnar Z, Tarabykin V. Satb2 is a postmitotic determinant for upper-layer neuron specification in the neocortex. Neuron. 2008;57:378–392. doi: 10.1016/j.neuron.2007.12.028. [DOI] [PubMed] [Google Scholar]
- Brown SD, Moore MW. The international mouse phenotyping consortium: past and future perspectives on mouse phenotyping. Mamm Genome. 2012;23:632–640. doi: 10.1007/s00335-012-9427-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerritelli F, Frasch MG, Antonelli MC, Viglione C, Vecchi S, Chiera M, Manzotti A. A Review on the vagus nerve and autonomic nervous system during fetal development: searching for critical windows. Front Neurosci. 2021;15:721605. doi: 10.3389/fnins.2021.721605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceunen E, Vlaeyen JW, van Diest I. On the origin of interoception. Front Psychol. 2016;7:743. doi: 10.3389/fpsyg.2016.00743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psych. 2014;5:80. doi: 10.3389/fpsyt.2014.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen EY, Tan CM, Kou Y, Duan Q, Wang Z, Meirelles GV, Clark NR, Ma'ayan A. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics. 2013;14:128. doi: 10.1186/1471-2105-14-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correll CU, Joffe BI, Rosen LM, Sullivan TB, Joffe RT. Cardiovascular and cerebrovascular risk factors and events associated with second-generation antipsychotic compared to antidepressant use in a non-elderly adult sample: results from a claims-based inception cohort study. World Psychiatr. 2015;14:56–63. doi: 10.1002/wps.20187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, Thapa-Chhetri N, Fornaro M, Gallicchio D, Collantoni E, Pigato G, Favaro A, Monaco F, Kohler C, Vancampfort D, Ward PB, Gaughran F, Carvalho AF, Stubbs B. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatr. 2017;16:163–180. doi: 10.1002/wps.20420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Epstein A, Wittchen HU, Pine DS, Lewis-Fernandez R, Hinton D, Anxiety DV, Spectrum OC, Posttraumatic DD, Work G. Panic disorder: a review of DSM-IV panic disorder and proposals for DSM-V. Depress Anxiety. 2010;27:93–112. doi: 10.1002/da.20654. [DOI] [PubMed] [Google Scholar]
- Critchley HD, Mathias CJ, Josephs O, O'Doherty J, Zanini S, Dewar BK, Cipolotti L, Shallice T, Dolan RJ. Human cingulate cortex and autonomic control: converging neuroimaging and clinical evidence. Brain. 2003;126:2139–2152. doi: 10.1093/brain/awg216. [DOI] [PubMed] [Google Scholar]
- Critchley HD, Tang J, Glaser D, Butterworth B, Dolan RJ. Anterior cingulate activity during error and autonomic response. Neuroimage. 2005;27:885–895. doi: 10.1016/j.neuroimage.2005.05.047. [DOI] [PubMed] [Google Scholar]
- Dampney RA. Central neural control of the cardiovascular system: current perspectives. Adv Physiol Educ. 2016;40:283–296. doi: 10.1152/advan.00027.2016. [DOI] [PubMed] [Google Scholar]
- Davern PJ. A role for the lateral parabrachial nucleus in cardiovascular function and fluid homeostasis. Front Physiol. 2014;5:436. doi: 10.3389/fphys.2014.00436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Hert M, Detraux J, Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin Neurosci. 2018;20:31–40. doi: 10.31887/DCNS.2018.20.1/mdehert. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Rubeis S, He X, Goldberg AP, Poultney CS, Samocha K, Cicek AE, Kou Y, Liu L, Fromer M, Walker S, Singh T, Klei L, Kosmicki J, Shih-Chen F, Aleksic B, Biscaldi M, Bolton PF, Brownfeld JM, Cai J, Campbell NG, Carracedo A, Chahrour MH, Chiocchetti AG, Coon H, Crawford EL, Curran SR, Dawson G, Duketis E, Fernandez BA, Gallagher L, Geller E, Guter SJ, Hill RS, Ionita-Laza J, Jimenz Gonzalez P, Kilpinen H, Klauck SM, Kolevzon A, Lee I, Lei I, Lei J, Lehtimaki T, Lin CF, Ma'ayan A, Marshall CR, McInnes AL, Neale B, Owen MJ, Ozaki N, Parellada M, Parr JR, Purcell S, Puura K, Rajagopalan D, Rehnstrom K, Reichenberg A, Sabo A, Sachse M, Sanders SJ, Schafer C, Schulte-Ruther M, Skuse D, Stevens C, Szatmari P, Tammimies K, Valladares O, Voran A, Li-San W, Weiss LA, Willsey AJ, Yu TW, Yuen RK, Study DDD. Homozygosity Mapping Collaborative for A. Consortium UK. Cook EH, Freitag CM, Gill M, Hultman CM, Lehner T, Palotie A, Schellenberg GD, Sklar P, State MW, Sutcliffe JS, Walsh CA, Scherer SW, Zwick ME, Barett JC, Cutler DJ, Roeder K, Devlin B, Daly MJ, Buxbaum JD. Synaptic, transcriptional and chromatin genes disrupted in autism. Nature. 2014;515:209–215. doi: 10.1038/nature13772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis PA, Watkins LL, Calhoun PS, Oddone A, Sherwood A, Dennis MF, Rissling MB, Beckham JC. Posttraumatic stress, heart rate variability, and the mediating role of behavioral health risks. Psychosom Med. 2014;76:629–637. doi: 10.1097/PSY.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doehner W, Ural D, Haeusler KG, Celutkiene J, Bestetti R, Cavusoglu Y, Pena-Duque MA, Glavas D, Iacoviello M, Laufs U, Alvear RM, Mbakwem A, Piepoli MF, Rosen SD, Tsivgoulis G, Vitale C, Yilmaz MB, Anker SD, Filippatos G, Seferovic P, Coats AJS, Ruschitzka F. Heart and brain interaction in patients with heart failure: overview and proposal for a taxonomy. A position paper from the study group on heart and brain interaction of the heart failure association. Eur J Heart Fail. 2018;20:199–215. doi: 10.1002/ejhf.1100. [DOI] [PubMed] [Google Scholar]
- Dresner E, Agam G, Gozes I. Activity-dependent neuroprotective protein (ADNP) expression level is correlated with the expression of the sister protein ADNP2: deregulation in schizophrenia. Eur Neuropsychopharmacol. 2011;21:355–361. doi: 10.1016/j.euroneuro.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Eippert F, Veit R, Weiskopf N, Erb M, Birbaumer N, Anders S. Regulation of emotional responses elicited by threat-related stimuli. Hum Brain Mapp. 2007;28:409–423. doi: 10.1002/hbm.20291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Empana JP, Sykes DH, Luc G, Juhan-Vague I, Arveiler D, Ferrieres J, Amouyel P, Bingham A, Montaye M, Ruidavets JB, Haas B, Evans A, Jouven X, Ducimetiere P. Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men: the prospective epidemiological study of myocardial infarction (PRIME) Circulation. 2005;111:2299–2305. doi: 10.1161/01.CIR.0000164203.54111.AE. [DOI] [PubMed] [Google Scholar]
- Faa G, Manchia M, Pintus R, Gerosa C, Marcialis MA, Fanos V. Fetal programming of neuropsychiatric disorders. Birth Defects Res C Embryo Today. 2016;108:207–223. doi: 10.1002/bdrc.21139. [DOI] [PubMed] [Google Scholar]
- Ferguson AV, Latchford KJ, Samson WK. The paraventricular nucleus of the hypothalamus - a potential target for integrative treatment of autonomic dysfunction. Expert Opin Ther Targets. 2008;12:717–727. doi: 10.1517/14728222.12.6.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge F, Yuan M, Li Y, Zhang W. Posttraumatic stress disorder and alterations in resting heart rate variability: a systematic review and meta-analysis. Psychiatr Investig. 2020;17:9–20. doi: 10.30773/pi.2019.0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies MJ, Huang Y, Hyam JA, Aziz TZ, Green AL. Direct neurophysiological evidence for a role of the human anterior cingulate cortex in central command. Auton Neurosci. 2019;216:51–58. doi: 10.1016/j.autneu.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein DS, Bentho O, Park MY, Sharabi Y. Low-frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Exp Physiol. 2011;96:1255–1261. doi: 10.1113/expphysiol.2010.056259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golosheykin S, Grant JD, Novak OV, Heath AC, Anokhin AP. Genetic influences on heart rate variability. Int J Psychophysiol. 2017;115:65–73. doi: 10.1016/j.ijpsycho.2016.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu X, Mao X, Lussier MP, Hutchison MA, Zhou L, Hamra FK, Roche KW, Lu W. GSG1L suppresses AMPA receptor-mediated synaptic transmission and uniquely modulates AMPA receptor kinetics in hippocampal neurons. Nat Commun. 2016;7:10873. doi: 10.1038/ncomms10873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52:2156–2162. doi: 10.1016/j.jacc.2008.08.057. [DOI] [PubMed] [Google Scholar]
- Hamilton MJ, Suri M. CDK13-related disorder. Adv Genet. 2019;103:163–182. doi: 10.1016/bs.adgen.2018.11.001. [DOI] [PubMed] [Google Scholar]
- Hansen AL, Johnsen BH, Sollers JJ, 3rd, Stenvik K, Thayer JF. Heart rate variability and its relation to prefrontal cognitive function: the effects of training and detraining. Eur J Appl Physiol. 2004;93:263–272. doi: 10.1007/s00421-004-1208-0. [DOI] [PubMed] [Google Scholar]
- Hardung S, Epple R, Jackel Z, Eriksson D, Uran C, Senn V, Gibor L, Yizhar O, Diester I. A functional gradient in the rodent prefrontal cortex supports behavioral inhibition. Curr Biol. 2017;27:549–555. doi: 10.1016/j.cub.2016.12.052. [DOI] [PubMed] [Google Scholar]
- Helsmoortel C, Vulto-van Silfhout AT, Coe BP, Vandeweyer G, Rooms L, van den Ende J, Schuurs-Hoeijmakers JH, Marcelis CL, Willemsen MH, Vissers LE, Yntema HG, Bakshi M, Wilson M, Witherspoon KT, Malmgren H, Nordgren A, Anneren G, Fichera M, Bosco P, Romano C, de Vries BB, Kleefstra T, Kooy RF, Eichler EE, van der Aa N. A SWI/SNF-related autism syndrome caused by de novo mutations in ADNP. Nat Genet. 2014;46:380–384. doi: 10.1038/ng.2899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiestand T, Hanggi J, Klein C, Topka MS, Jaguszewski M, Ghadri JR, Luscher TF, Jancke L, Templin C. Takotsubo syndrome associated with structural brain alterations of the limbic system. J Am Coll Cardiol. 2018;71:809–811. doi: 10.1016/j.jacc.2017.12.022. [DOI] [PubMed] [Google Scholar]
- Homsy J, Zaidi S, Shen Y, Ware JS, Samocha KE, Karczewski KJ, DePalma SR, McKean D, Wakimoto H, Gorham J, Jin SC, Deanfield J, Giardini A, Porter GA, Jr, Kim R, Bilguvar K, Lopez-Giraldez F, Tikhonova I, Mane S, Romano-Adesman A, Qi H, Vardarajan B, Ma L, Daly M, Roberts AE, Russell MW, Mital S, Newburger JW, Gaynor JW, Breitbart RE, Iossifov I, Ronemus M, Sanders SJ, Kaltman JR, Seidman JG, Brueckner M, Gelb BD, Goldmuntz E, Lifton RP, Seidman CE, Chung WK. De novo mutations in congenital heart disease with neurodevelopmental and other congenital anomalies. Science. 2015;350:1262–1266. doi: 10.1126/science.aac9396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hume DA, Summers KM, Raza S, Baillie JK, Freeman TC. Functional clustering and lineage markers: insights into cellular differentiation and gene function from large-scale microarray studies of purified primary cell populations. Genomics. 2010;95:328–338. doi: 10.1016/j.ygeno.2010.03.002. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatr. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jaitner C, Reddy C, Abentung A, Whittle N, Rieder D, Delekate A, Korte M, Jain G, Fischer A, Sananbenesi F, Cera I, Singewald N, Dechant G, Apostolova G. Satb2 determines miRNA expression and long-term memory in the adult central nervous system. Elife. 2016;5:e17361. doi: 10.7554/eLife.17361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jangpangi D, Mondal S, Bandhu R, Kataria D, Gandhi A. Alteration of heart rate variability in patients of depression. J Clin Diagn Res. 2016;10:CM04–CM06. doi: 10.7860/JCDR/2016/22882.9063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokinen J, Nordstrom P. HPA axis hyperactivity and cardiovascular mortality in mood disorder inpatients. J Affect Disord. 2009;116:88–92. doi: 10.1016/j.jad.2008.10.025. [DOI] [PubMed] [Google Scholar]
- Karemaker JM. An introduction into autonomic nervous function. Physiol Meas. 2017;38:R89–R118. doi: 10.1088/1361-6579/aa6782. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Sparrow D, Vokonas PS, Weiss ST. Symptoms of anxiety and risk of coronary heart disease. Norm Aging Study Circ. 1994;90:2225–2229. doi: 10.1161/01.cir.90.5.2225. [DOI] [PubMed] [Google Scholar]
- Khoury NM, Lutz J, Schuman-Olivier Z. Interoception in psychiatric disorders: a review of randomized, controlled trials with interoception-based interventions. Harv Rev Psychiatr. 2018;26:250–263. doi: 10.1097/HRP.0000000000000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YS, Leventhal BL, Koh YJ, Fombonne E, Laska E, Lim EC, Cheon KA, Kim SJ, Kim YK, Lee H, Song DH, Grinker RR. Prevalence of autism spectrum disorders in a total population sample. Am J Psychiatry. 2011;168:904–912. doi: 10.1176/appi.ajp.2011.10101532. [DOI] [PubMed] [Google Scholar]
- Kim SC, Kim A, Park JY, Hwang EM. Improved AAV vector system for cell-type-specific RNA interference. J Neurosci Methods. 2022;368:109452. doi: 10.1016/j.jneumeth.2021.109452. [DOI] [PubMed] [Google Scholar]
- Kirkwood SC, Su JL, Conneally P, Foroud T. Progression of symptoms in the early and middle stages of Huntington disease. Arch Neurol. 2001;58:273–278. doi: 10.1001/archneur.58.2.273. [DOI] [PubMed] [Google Scholar]
- Koch C, Wilhelm M, Salzmann S, Rief W, Euteneuer F. A meta-analysis of heart rate variability in major depression. Psychol Med. 2019;49:1948–1957. doi: 10.1017/S0033291719001351. [DOI] [PubMed] [Google Scholar]
- Kuleshov MV, Jones MR, Rouillard AD, Fernandez NF, Duan Q, Wang Z, Koplev S, Jenkins SL, Jagodnik KM, Lachmann A, McDermott MG, Monteiro CD, Gundersen GW, Ma'ayan A. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016;44:W90–97. doi: 10.1093/nar/gkw377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBar KS, Gatenby JC, Gore JC, LeDoux JE, Phelps EA. Human amygdala activation during conditioned fear acquisition and extinction: a mixed-trial fMRI study. Neuron. 1998;20:937–945. doi: 10.1016/S0896-6273(00)80475-4. [DOI] [PubMed] [Google Scholar]
- Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research - recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017;8:213. doi: 10.3389/fpsyg.2017.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le W, Nguyen D, Lin XW, Rawal P, Huang M, Ding Y, Xie W, Deng H, Jankovic J. Transcription factor PITX3 gene in Parkinson's disease. Neurobiol Aging. 2011;32:750–753. doi: 10.1016/j.neurobiolaging.2009.03.015. [DOI] [PubMed] [Google Scholar]
- Lee D, Kwon W, Heo J, Park JY. Associations between heart rate variability and brain activity during a working memory task: a preliminary electroencephalogram study on depression and anxiety disorder. Brain Sci. 2022;12:172. doi: 10.3390/brainsci12020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lein ES, Hawrylycz MJ, Ao N, Ayres M, Bensinger A, Bernard A, Boe AF, Boguski MS, Brockway KS, Byrnes EJ, Chen L, Chen L, Chen TM, Chin MC, Chong J, Crook BE, Czaplinska A, Dang CN, Datta S, Dee NR, Desaki AL, Desta T, Diep E, Dolbeare TA, Donelan MJ, Dong HW, Dougherty JG, Duncan BJ, Ebbert AJ, Eichele G, Estin LK, Faber C, Facer BA, Fields R, Fischer SR, Fliss TP, Frensley C, Gates SN, Glattfelder KJ, Halverson KR, Hart MR, Hohmann JG, Howell MP, Jeung DP, Johnson RA, Karr PT, Kawal R, Kidney JM, Knapik RH, Kuan CL, Lake JH, Laramee AR, Larsen KD, Lau C, Lemon TA, Liang AJ, Liu Y, Luong LT, Michaels J, Morgan JJ, Morgan RJ, Mortrud MT, Mosqueda NF, Ng LL, Ng R, Orta GJ, Overly CC, Pak TH, Parry SE, Pathak SD, Pearson OC, Puchalski RB, Riley ZL, Rockett HR, Rowland SA, Royall JJ, Ruiz MJ, Sarno NR, Schaffnit K, Shapovalova NV, Sivisay T, Slaughterbeck CR, Smith SC, Smith KA, Smith BI, Sodt AJ, Stewart NN, Stumpf KR, Sunkin SM, Sutram M, Tam A, Teemer CD, Thaller C, Thompson CL, Varnam LR, Visel A, Whitlock RM, Wohnoutka PE, Wolkey CK, Wong VY, Wood M, Yaylaoglu MB, Young RC, Youngstrom BL, Yuan XF, Zhang B, Zwingman TA, Jones AR. Genome-wide atlas of gene expression in the adult mouse brain. Nature. 2007;445:168–176. doi: 10.1038/nature05453. [DOI] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66:305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- Li J, Dani JA, Le W. The role of transcription factor Pitx3 in dopamine neuron development and Parkinson's disease. Curr Top Med Chem. 2009;9:855–859. [PMC free article] [PubMed] [Google Scholar]
- Lichtman JH, Bigger JT, Jr., Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES, American Heart Association Prevention Committee of the Council on Cardiovascular N, American Heart Association Council on Clinical C, American Heart Association Council on E, Prevention, American Heart Association Interdisciplinary Council on Quality of C, Outcomes R, American Psychiatric A (2008) Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 118:1768–1775 [DOI] [PubMed]
- Ma CL, Arnsten AF, Li BM. Locomotor hyperactivity induced by blockade of prefrontal cortical alpha2-adrenoceptors in monkeys. Biol Psychiat. 2005;57:192–195. doi: 10.1016/j.biopsych.2004.11.004. [DOI] [PubMed] [Google Scholar]
- Mabbott NA, Baillie JK, Brown H, Freeman TC, Hume DA. An expression atlas of human primary cells: inference of gene function from coexpression networks. BMC Genomics. 2013;14:632. doi: 10.1186/1471-2164-14-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A, Furnier SM, Hallas L, Hall-Lande J, Hudson A, Hughes MM, Patrick M, Pierce K, Poynter JN, Salinas A, Shenouda J, Vehorn A, Warren Z, Constantino JN, DiRienzo M, Fitzgerald RT, Grzybowski A, Spivey MH, Pettygrove S, Zahorodny W, Ali A, Andrews JG, Baroud T, Gutierrez J, Hewitt A, Lee LC, Lopez M, Mancilla KC, McArthur D, Schwenk YD, Washington A, Williams S, Cogswell ME. Prevalence and characteristics of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveill Summ. 2021;70:1–16. doi: 10.15585/mmwr.ss7011a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makovac E, Garfinkel SN, Bassi A, Basile B, Macaluso E, Cercignani M, Calcagnini G, Mattei E, Agalliu D, Cortelli P, Caltagirone C, Bozzali M, Critchley H. Effect of parasympathetic stimulation on brain activity during appraisal of fearful expressions. Neuropsychopharmacology. 2015;40:1649–1658. doi: 10.1038/npp.2015.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumura K, Seiriki K, Okada S, Nagase M, Ayabe S, Yamada I, Furuse T, Shibuya H, Yasuda Y, Yamamori H, Fujimoto M, Nagayasu K, Yamamoto K, Kitagawa K, Miura H, Gotoda-Nishimura N, Igarashi H, Hayashida M, Baba M, Kondo M, Hasebe S, Ueshima K, Kasai A, Ago Y, Hayata-Takano A, Shintani N, Iguchi T, Sato M, Yamaguchi S, Tamura M, Wakana S, Yoshiki A, Watabe AM, Okano H, Takuma K, Hashimoto R, Hashimoto H, Nakazawa T. Pathogenic POGZ mutation causes impaired cortical development and reversible autism-like phenotypes. Nat Commun. 2020;11:859. doi: 10.1038/s41467-020-14697-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moretta T, Messerotti Benvenuti S. Early indicators of vulnerability to depression: the role of rumination and heart rate variability. J Affect Disord. 2022;312:217–224. doi: 10.1016/j.jad.2022.06.049. [DOI] [PubMed] [Google Scholar]
- Morris R, Griffiths O, Le Pelley ME, Weickert TW. Attention to irrelevant cues is related to positive symptoms in schizophrenia. Schizophr Bull. 2013;39:575–582. doi: 10.1093/schbul/sbr192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulkey SB, du Plessis AJ. Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatr Res. 2019;85:120–126. doi: 10.1038/s41390-018-0155-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagai M, Hoshide S, Kario K. The insular cortex and cardiovascular system: a new insight into the brain-heart axis. J Am Soc Hypertens. 2010;4:174–182. doi: 10.1016/j.jash.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuys R. The insular cortex: a review. Prog Brain Res. 2012;195:123–163. doi: 10.1016/B978-0-444-53860-4.00007-6. [DOI] [PubMed] [Google Scholar]
- Nikolovska K, Spillmann D, Seidler DG. Uronyl 2-O sulfotransferase potentiates Fgf2-induced cell migration. J Cell Sci. 2015;128:460–471. doi: 10.1242/jcs.152660. [DOI] [PubMed] [Google Scholar]
- Oommen AM, Cunningham S, O'Suilleabhain PS, Hughes BM, Joshi L. An integrative network analysis framework for identifying molecular functions in complex disorders examining major depressive disorder as a test case. Sci Rep. 2021;11:9645. doi: 10.1038/s41598-021-89040-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reardon JP, Cristancho P, Peshek AD. Vagus nerve stimulation (vns) and treatment of depression: to the brainstem and beyond. Psychiatry (edgmont) 2006;3:54–63. [PMC free article] [PubMed] [Google Scholar]
- Pagani M, Mazzuero G, Ferrari A, Liberati D, Cerutti S, Vaitl D, Tavazzi L, Malliani A. Sympathovagal interaction during mental stress. A study using spectral analysis of heart rate variability in healthy control subjects and patients with a prior myocardial infarction. Circulation. 1991;83:II43–51. [PubMed] [Google Scholar]
- Penninx B, Lange SMM. Metabolic syndrome in psychiatric patients: overview, mechanisms, and implications. Dialogues Clin Neurosci. 2018;20:63–73. doi: 10.31887/DCNS.2018.20.1/bpenninx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrone L, Valente M. The emerging role of metabolism in brain-heart axis: new challenge for the therapy and prevention of Alzheimer disease. May thioredoxin interacting protein (TXNIP) play a role? Biomolecules. 2021;11:1652. doi: 10.3390/biom11111652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittig A, Arch JJ, Lam CW, Craske MG. Heart rate and heart rate variability in panic, social anxiety, obsessive-compulsive, and generalized anxiety disorders at baseline and in response to relaxation and hyperventilation. Int J Psychophysiol. 2013;87:19–27. doi: 10.1016/j.ijpsycho.2012.10.012. [DOI] [PubMed] [Google Scholar]
- Pulopulos MM, Vanderhasselt MA, de Raedt R. Association between changes in heart rate variability during the anticipation of a stressful situation and the stress-induced cortisol response. Psychoneuroendocrinology. 2018;94:63–71. doi: 10.1016/j.psyneuen.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin L, Williams JB, Tan T, Liu T, Cao Q, Ma K, Yan Z. Deficiency of autism risk factor ASH1L in prefrontal cortex induces epigenetic aberrations and seizures. Nat Commun. 2021;12:6589. doi: 10.1038/s41467-021-26972-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21:10. doi: 10.1007/s11920-019-0997-0. [DOI] [PubMed] [Google Scholar]
- Reyes del Paso GA, Langewitz W, Mulder LJ, van Roon A, Duschek S. The utility of low frequency heart rate variability as an index of sympathetic cardiac tone: a review with emphasis on a reanalysis of previous studies. Psychophysiology. 2013;50:477–487. doi: 10.1111/psyp.12027. [DOI] [PubMed] [Google Scholar]
- Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi-amorn C, Sato H, Yusuf S. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernandez-Sola J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundstrom J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V, Group G-N-JGBoCDW (2020) Global burden of cardiovascular diseases and risk factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol 76:2982–3021
- Rugulies R. Depression as a predictor for coronary heart disease. a review and meta-analysis. Am J Prev Med. 2002;23:51–61. doi: 10.1016/S0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- Ruiz-Padial E, Vila J, Thayer JF. The effect of conscious and non-conscious presentation of biologically relevant emotion pictures on emotion modulated startle and phasic heart rate. Int J Psychophysiol. 2011;79:341–346. doi: 10.1016/j.ijpsycho.2010.12.001. [DOI] [PubMed] [Google Scholar]
- Sanders SJ, He X, Willsey AJ, Ercan-Sencicek AG, Samocha KE, Cicek AE, Murtha MT, Bal VH, Bishop SL, Dong S, Goldberg AP, Jinlu C, Keaney JF, 3rd, Klei L, Mandell JD, Moreno-De-Luca D, Poultney CS, Robinson EB, Smith L, Solli-Nowlan T, Su MY, Teran NA, Walker MF, Werling DM, Beaudet AL, Cantor RM, Fombonne E, Geschwind DH, Grice DE, Lord C, Lowe JK, Mane SM, Martin DM, Morrow EM, Talkowski ME, Sutcliffe JS, Walsh CA, Yu TW, Autism Sequencing C, Ledbetter DH, Martin CL, Cook EH, Buxbaum JD, Daly MJ, Devlin B, Roeder K, State MW. Insights into autism spectrum disorder genomic architecture and biology from 71 risk loci. Neuron. 2015;87:1215–1233. doi: 10.1016/j.neuron.2015.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandin S, Lichtenstein P, Kuja-Halkola R, Hultman C, Larsson H, Reichenberg A. The heritability of autism spectrum disorder. JAMA. 2017;318:1182–1184. doi: 10.1001/jama.2017.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarlon J, Staniloiu A, Kordon A. Heart rate variability changes in patients with major depressive disorder: related to confounding factors, not to symptom severity? Front Neurosci. 2021;15:675624. doi: 10.3389/fnins.2021.675624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheitz JF, Ghadri JR, Templin C. Brain-heart interaction revisited: Takotsubo syndrome secondary to seizures. Int J Cardiol. 2020;299:71–72. doi: 10.1016/j.ijcard.2019.08.036. [DOI] [PubMed] [Google Scholar]
- Shah AJ, Ghasemzadeh N, Zaragoza-Macias E, Patel R, Eapen DJ, Neeland IJ, Pimple PM, Zafari AM, Quyyumi AA, Vaccarino V. Sex and age differences in the association of depression with obstructive coronary artery disease and adverse cardiovascular events. J Am Heart Assoc. 2014;3:e000741. doi: 10.1161/JAHA.113.000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shivkumar K, Ajijola OA, Anand I, Armour JA, Chen PS, Esler M, de Ferrari GM, Fishbein MC, Goldberger JJ, Harper RM, Joyner MJ, Khalsa SS, Kumar R, Lane R, Mahajan A, Po S, Schwartz PJ, Somers VK, Valderrabano M, Vaseghi M, Zipes DP. Clinical neurocardiology defining the value of neuroscience-based cardiovascular therapeutics. J Physiol. 2016;594:3911–3954. doi: 10.1113/JP271870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvani A, Calandra-Buonaura G, Dampney RA, Cortelli P. Brain-heart interactions: physiology and clinical implications. Philos Trans A Math Phys Eng Sci. 2016;374:20150181. doi: 10.1098/rsta.2015.0181. [DOI] [PubMed] [Google Scholar]
- Sloan RP, Shapiro PA, Bagiella E, Bigger JT, Jr, Lo ES, Gorman JM. Relationships between circulating catecholamines and low frequency heart period variability as indices of cardiac sympathetic activity during mental stress. Psychosom Med. 1996;58:25–31. doi: 10.1097/00006842-199601000-00005. [DOI] [PubMed] [Google Scholar]
- Spielmann N, Miller G, Oprea TI, Hsu C-W, Fobo G, Frishman G, Montrone C, Haseli Mashhadi H, Mason J, Munoz Fuentes V, Leuchtenberger S, Ruepp A, Wagner M, Westphal DS, Wolf C, Görlach A, Sanz-Moreno A, Cho Y-L, Teperino R, Brandmaier S, Sharma S, Galter IR, Östereicher MA, Zapf L, Mayer-Kuckuk P, Rozman J, Teboul L, Bunton-Stasyshyn RKA, Cater H, Stewart M, Christou S, Westerberg H, Willett AM, Wotton JM, Roper WB, Christiansen AE, Ward CS, Heaney JD, Reynolds CL, Prochazka J, Bower L, Clary D, Selloum M, Bou About G, Wendling O, Jacobs H, Leblanc S, Meziane H, Sorg T, Audain E, Gilly A, Rayner NW, Aguilar-Pimentel JA, Becker L, Garrett L, Hölter SM, Amarie OV, Calzada-Wack J, Klein-Rodewald T, da Silva-Buttkus P, Lengger C, Stoeger C, Gerlini R, Rathkolb B, Mayr D, Seavitt J, Gaspero A, Green JR, Garza A, Bohat R, Wong L, McElwee ML, Kalaga S, Rasmussen TL, Lorenzo I, Lanza DG, Samaco RC, Veeraragaven S, Gallegos JJ, Kašpárek P, Petrezsélyová S, King R, Johnson S, Cleak J, Szkoe-Kovacs Z, Codner G, Mackenzie M, Caulder A, Kenyon J, Gardiner W, Phelps H, Hancock R, Norris C, Moore MA, Seluke AM, Urban R, Kane C, Goodwin LO, Peterson KA, McKay M, Cook JJ, Lowy JP, McFarland M, Wood JA, Willis BJ, Tolentino H, Tolentino T, Schuchbauer M, Salazar J, Johnson J, Munson R, Ayadi A, Pavlovic G, Birling M-C, Jacquot S, Ali-Hadji D, Charles P, Andre P, Champy M-F, Riet F, Vukobradovic I, Berberovic Z, Qu D, Guo R, D’Souza A, Huang Z, Camilleri S, Ganguly M, Adissu H, Eskandarian M, Shang X, Duffin K, Xu C, Roberton K, Laurin V, Lan Q, Sleep G, Creighton A, Lintott L, Gertsenstein M, Pereira M, Tondat S, Patel A, Cruz M, Bezginov A, Miller D, Hy W, Yoshiki A, Tanaka N, Tamura M, Liu Z, Ermakova O, Ferrara A, Fruscoloni P, Seisenberger C, Bürger A, Giesert F, Ambrose JC, Arumu gam P, Bevers R, Bleda M, Boardman-Pretty F, Boustred CR, Brittain H, Caulfield MJ, Chan GC, Fowler T, Giess A, Hamblin A, Henderson S, Hubbard TJP, Jackson R, Jones LJ, Kasperaviciute D, Kayikci M, Kousathanas A, Lahnstein L, Leigh SEA, Leong IUS, Lopez FJ, Maleady-Crowe F, McEntagart M, Minneci F, Moutsianas L, Mueller M, Murugaesu N, Need AC, O‘Donovan P, Odhams CA, Patch C, Perez-Gil D, Pereira MB, Pullinger J, Rahim T, Rendon A, Rogers T, Savage K, Sawant K, Scott RH, Siddiq A, Sieghart A, Smith SC, Sosinsky A, Stuckey A, Tanguy M, Taylor-Tavares AL, Thomas ERA, Thompson SR, Tucci A, Welland MJ, Williams E, Witkowska K, Wood SM, Hitz M-P, Zeggini E, Wolf E, Sedlacek R, Murray SA, Svenson KL, Braun RE, White JK, Kelsey L, Gao X, Shiroishi T, Xu Y, Seong JK, Mammano F, Tocchini-Valentini GP, Beaudet AL, Meehan TF, Parkinson H, Smedley D, Mallon A-M, Wells SE, Grallert H, Wurst W, Marschall S, Fuchs H, Brown SDM, Flenniken AM, Nutter LMJ, McKerlie C, Herault Y, Lloyd KCK, Dickinson ME, Gailus-Durner V, Hrabe de Angelis M, consortium I, Genomics England Research C (2022) Extensive identification of genes involved in congenital and structural heart disorders and cardiomyopathy. Nat Cardiovasc Res 1:157–173 [DOI] [PMC free article] [PubMed]
- Tanaka K, Shouguchi-Miyata J, Miyamoto N, Ikeda JE. Novel nuclear shuttle proteins, HDBP1 and HDBP2, bind to neuronal cell-specific cis-regulatory element in the promoter for the human Huntington's disease gene. J Biol Chem. 2004;279:7275–7286. doi: 10.1074/jbc.M310726200. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61:201–216. doi: 10.1016/S0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Ahs F, Fredrikson M, Sollers JJ, 3rd, Wager TD. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. 2012;36:747–756. doi: 10.1016/j.neubiorev.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Thireau J, Zhang BL, Poisson D, Babuty D. Heart rate variability in mice: a theoretical and practical guide. Exp Physiol. 2008;93:83–94. doi: 10.1113/expphysiol.2007.040733. [DOI] [PubMed] [Google Scholar]
- Tyler CV, Schramm SC, Karafa M, Tang AS, Jain AK. Chronic disease risks in young adults with autism spectrum disorder: forewarned is forearmed. Am J Intellect Dev Disabil. 2011;116:371–380. doi: 10.1352/1944-7558-116.5.371. [DOI] [PubMed] [Google Scholar]
- Vale S. Psychosocial stress and cardiovascular diseases. Postgrad Med J. 2005;81:429–435. doi: 10.1136/pgmj.2004.028977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenza G, Toschi N, Barbieri R. Uncovering brain-heart information through advanced signal and image processing. Philos Trans A Math Phys Eng Sci. 2016;374:20160020. doi: 10.1098/rsta.2016.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Bilsen M, Patel HC, Bauersachs J, Bohm M, Borggrefe M, Brutsaert D, Coats AJS, de Boer RA, de Keulenaer GW, Filippatos GS, Floras J, Grassi G, Jankowska EA, Kornet L, Lunde IG, Maack C, Mahfoud F, Pollesello P, Ponikowski P, Ruschitzka F, Sabbah HN, Schultz HD, Seferovic P, Slart R, Taggart P, Tocchetti CG, van Laake LW, Zannad F, Heymans S, Lyon AR. The autonomic nervous system as a therapeutic target in heart failure: a scientific position statement from the translational research committee of the heart failure association of the European society of cardiology. Eur J Heart Fail. 2017;19:1361–1378. doi: 10.1002/ejhf.921. [DOI] [PubMed] [Google Scholar]
- van Dijck A, Vulto-van Silfhout AT, Cappuyns E, van der Werf IM, Mancini GM, Tzschach A, Bernier R, Gozes I, Eichler EE, Romano C, Lindstrand A, Nordgren A, Consortium A, Kvarnung M, Kleefstra T, de Vries BBA, Kury S, Rosenfeld JA, Meuwissen ME, Vandeweyer G, Kooy RF. Clinical presentation of a complex neurodevelopmental disorder caused by mutations in ADNP. Biol Psychiatr. 2019;85:287–297. doi: 10.1016/j.biopsych.2018.02.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vianna DM, Brandao ML. Anatomical connections of the periaqueductal gray: specific neural substrates for different kinds of fear. Braz J Med Biol Res. 2003;36:557–566. doi: 10.1590/S0100-879X2003000500002. [DOI] [PubMed] [Google Scholar]
- Watkins LL, Blumenthal JA, Davidson JR, Babyak MA, McCants CB, Jr, Sketch MH., Jr Phobic anxiety, depression, and risk of ventricular arrhythmias in patients with coronary heart disease. Psychosom Med. 2006;68:651–656. doi: 10.1097/01.psy.0000228342.53606.b3. [DOI] [PubMed] [Google Scholar]
- Waxenbaum JA, Reddy V, Varacallo M. Anatomy, autonomic Nervous system. United States: StatPearls Treasure Island (FL); 2022. [PubMed] [Google Scholar]
- Wernovsky G, Licht DJ. Neurodevelopmental outcomes in children with congenital heart disease-what can we impact? Pediatr Crit Care Med. 2016;17:S232–242. doi: 10.1097/PCC.0000000000000800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westman J, Eriksson SV, Gissler M, Hallgren J, Prieto ML, Bobo WV, Frye MA, Erlinge D, Alfredsson L, Osby U. Increased cardiovascular mortality in people with schizophrenia: a 24-year national register study. Epidemiol Psychiatr Sci. 2018;27:519–527. doi: 10.1017/S2045796017000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitton L, Apostolova G, Rieder D, Dechant G, Rea S, Donohoe G, Morris DW. Genes regulated by SATB2 during neurodevelopment contribute to schizophrenia and educational attainment. PLoS Genet. 2018;14:e1007515. doi: 10.1371/journal.pgen.1007515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong AH, Trakalo J, Likhodi O, Yusuf M, Macedo A, Azevedo MH, Klempan T, Pato MT, Honer WG, Pato CN, van Tol HH, Kennedy JL. Association between schizophrenia and the syntaxin 1A gene. Biol Psychiat. 2004;56:24–29. doi: 10.1016/j.biopsych.2004.03.008. [DOI] [PubMed] [Google Scholar]
- Xiang C, Cong S, Liang B, Cong S. Bioinformatic gene analysis for potential therapeutic targets of Huntington's disease in pre-symptomatic and symptomatic stage. J Transl Med. 2020;18:388. doi: 10.1186/s12967-020-02549-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X, Fang Y, Chen H, Zhang T, Yin X, Man J, Yang L, Lu M. Global, regional and national burden of anxiety disorders from 1990 to 2019: results from the global burden of disease study 2019. Epidemiol Psychiatr Sci. 2021;30:e36. doi: 10.1017/S2045796021000275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Y, Cho MT, Retterer K, Alexander N, Ben-Omran T, Al-Mureikhi M, Cristian I, Wheeler PG, Crain C, Zand D, Weinstein V, Vernon HJ, McClellan R, Krishnamurthy V, Vitazka P, Millan F, Chung WK. De novo POGZ mutations are associated with neurodevelopmental disorders and microcephaly. Cold Spring Harb Mol Case Stud. 2015;1:a000455. doi: 10.1101/mcs.a000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.