Abstract
Background
The COVID-19 pandemic accelerated adoption of telemedicine in cardiology clinics. Early in the pandemic, there were sociodemographic disparities in telemedicine use. It is unknown if these disparities persisted and whether they were associated with changes in the population of patients accessing care.
Methods
We examined all adult cardiology visits at an academic and an affiliated community practice in Northern California from March 2019 to February 2020 (pre-COVID) and March 2020 to February 2021 (COVID). We compared patient sociodemographic characteristics between these periods. We used logistic regression to assess the association of patient/visit characteristics with visit modality (in-person vs telemedicine and video- vs phone-based telemedicine) during the COVID period.
Results
There were 54,948 pre-COVID and 58,940 COVID visits. Telemedicine use increased from <1% to 70.7% of visits (49.7% video, 21.0% phone) during the COVID period. Patient sociodemographic characteristics were similar during both periods. In adjusted analyses, visits for patients from some sociodemographic groups were less likely to be delivered by telemedicine, and when delivered by telemedicine, were less likely to be delivered by video versus phone. The observed disparities in the use of video-based telemedicine were greatest for patients aged ≥80 years (vs age <60, OR 0.24, 95% CI 0.21, 0.28), Black patients (vs non-Hispanic White, OR 0.64, 95% CI 0.56, 0.74), patients with limited English proficiency (vs English proficient, OR 0.52, 95% CI 0.46-0.59), and those on Medicaid (vs privately insured, OR 0.47, 95% CI 0.41-0.54).
Conclusions
During the first year of the pandemic, the sociodemographic characteristics of patients receiving cardiovascular care remained stable, but the modality of care diverged across groups. There were differences in the use of telemedicine vs in-person care and most notably in the use of video- vs phone-based telemedicine. Future studies should examine barriers and outcomes in digital healthcare access across diverse patient groups.
Keywords: telemedicine, cardiology, healthcare disparities, COVID-19, age, racial, ethnic, language, socioeconomic
Introduction
The COVID-19 pandemic disrupted the delivery of routine healthcare.1 Early in the pandemic, clinics across the world rapidly deployed telemedicine to maintain access to ambulatory care while minimizing risks to patients and providers.2, 3, 4 This expansion of virtual care was facilitated by changes in telecommunications infrastructure, reimbursement models, and licensure requirements.5 , 6
The pandemic disproportionately impacted individuals from historically marginalized groups, who experienced both higher rates of infection and a greater burden of disease.7 , 8 It also exacerbated existing disparities in access to healthcare, including ambulatory care.9 , 10 Studies evaluating the utilization of outpatient cardiovascular care and telemedicine across sociodemographic groups are particularly important because telemedicine will likely play a lasting role in outpatient management.11 Research is needed to inform policymakers as they re-evaluate and modify the emergency measures that facilitated telemedicine expansion.12 In addition, healthcare systems should examine their own care delivery patterns as new technologies, such as telemedicine, are introduced, so that they can identify and address disparities in access.
Previous analyses of academic cardiology practices in the first several weeks of the pandemic highlighted disparities in the use of telemedicine based on sociodemographic characteristics, most notably in the use of audiovisual versus audio-only telemedicine.13, 14, 15, 16, 17 Telemedicine use continued at high rates during the first year of the pandemic and allowed health systems to provide similar numbers of visits to patients with cardiovascular disease as compared to before the pandemic.4 , 18 It is unclear if disparities in telemedicine use persisted during this period and if so, whether they were associated with changes in the overall population of patients accessing outpatient cardiovascular care. Furthermore, analyses are needed evaluating disparities across different cardiology practice settings, including community-based practices, since most patients access cardiovascular care outside of academic centers.
To identify disparities in access to cardiovascular care and telemedicine at our health system, we examined the sociodemographic characteristics of patients who received ambulatory care at two large cardiology practices, one academic and one community-based, before and during the COVID-19 pandemic. The results were used to improve care delivery at our institution and are informative for health system leaders and policymakers seeking to improve access to telemedicine.
Materials and Methods
Study Design and Setting
This quality improvement study focused on two outpatient cardiology practices, one academic and one community-based, owned by Stanford Health Care (SHC), which is located in Northern California. The academic practice serves patients at two clinics in Santa Clara County, and the community-based practice serves patients at clinics in Alameda and Contra Costa Counties. This project was supported by the SHC Digital Health Care Integration team to understand the current use of telemedicine in SHC outpatient cardiology clinics, assess its impact on access to care, and identify opportunities to improve care delivery. Data were only collected that were required for this purpose.
All adults (≥18 years) with an outpatient physician visit between March 2019 and February 2021 were included. We investigated associations between patient and visit characteristics and the mode of care delivery. Telemedicine visits were conducted via audio-only (phone-based telemedicine) or via audiovisual teleconferencing (video-based telemedicine). We applied an equity-focused social determinants of health framework, examining factors including social and structural barriers due to race/ethnicity, socioeconomic status, and neighborhood environment, which may have influenced access to cardiovascular ambulatory care and telemedicine during the pandemic.19
This project was funded by a quality improvement grant from the Division of Cardiovascular Medicine at Stanford University School of Medicine. This study was deemed to be non-research by the Stanford Institutional Review Board. The study adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper, and its final contents.
Data
Patient sociodemographic and visit characteristics were extracted using automated queries from the SHC Enterprise Data Warehouse, which imports data directly from the SHC EHR. The SHC information technology team conducts regular quality assurance checks to ensure that data is correctly extracted from the EHR and loaded into the Enterprise Data Warehouse. Visits were defined as unique outpatient encounters, and visit modality was determined based on how visits were scheduled in the EHR and delivered by physicians. In-person, phone, and video visits each had a different visit type, which was included in the database. We categorized visits by subspecialty using the primary affiliation of the treating physician. Supporting data for this study are available from the corresponding author upon request.
Study period
The pre-COVID period was defined as March 4, 2019, to February 29, 2020, and the COVID period was defined as March 4, 2020, to February 28, 2021. On March 4, 2020, the governor of California declared a state of emergency due to rising COVID-19 cases in the state.
Outcomes
Outcomes consisted of the proportion of visits provided to patients with specific sociodemographic characteristics during the pre-COVID and COVID periods and the adjusted odds ratios for a visit being delivered by telemedicine versus in-person and for a telemedicine visit being delivered by video versus phone during the COVID period.
Covariates
Patient sociodemographic characteristics included age, gender, self-identified race/ethnicity, insurance status, and English proficiency. Categories for self-identified race/ethnicity were Asian, Black, Hispanic, non-Hispanic White, and other. Other includes patients self-identifying as American Indian or Alaska Native, Native American, Native Hawaiian or other Pacific Islander, other, and unknown. Residential ZIP codes were used to determine median household income and educational attainment from the American Community Survey. We also calculated the linear distance between residential ZIP codes and the site of care. Gender, self-identified race/ethnicity, and ZIP code were missing for a small number of patients. The remaining covariates were the half of the COVID period when the visit occurred (March-August 2020 versus September 2020-February 2021), the practice site, and the visit subspecialty.
Analysis
We used logistic regression models to assess the associations between visit and patient characteristics and the likelihood of a visit being delivered by telemedicine versus in-person and of a telemedicine visit being delivered by video versus phone. For the telemedicine versus in-person model, the dependent variable was a binary variable indicating whether a visit occurred via telemedicine (1) or in-person (0). For the video- versus phone-based telemedicine model, the dependent variable indicated whether a visit occurred by video (1) or phone (0). Analyses were conducted at the visit level rather than the patient level because the focus of this project was to determine the relationships between patient sociodemographic characteristics and visit modality assignment rather than to understand how individual patient care utilization changed during the pandemic. The modality of each visit was treated as an independent event.
Our strategy for variable selection included a careful consideration of factors that could be associated with visit modality. This was based on literature review and discussion with clinical experts. Covariates with a significant univariate association (p < 0.1) were included in the final multivariable model. For pairs of highly correlated continuous variables (Pearson correlation > 0.5 or < -0.5), we retained the variable that was most highly associated with the dependent variable. The final multivariable logistic regression models comparing care modality between groups included the following covariates: period of visit [ref. March-August]; type of visit [ref. new visit]; age category [ref. <60yo]; gender [ref. female]; race/ethnicity [ref. non-Hispanic White]; English proficiency [ref. proficient]; insurance coverage [ref. private]; median household income [ref. <$50 000]; distance to clinic [ref. <20 miles]; provider subspecialty [ref. general cardiology]; and practice site [ref. academic]. As a sensitivity analysis, we repeated the analysis including all covariates. We reported missing data and assumed that missingness occurred at random. Observations with missing data were excluded from the logistic regression models.
Analyses and data visualizations were performed using Tableau Desktop (Version 2020.1.8, Tableau Software, LLC) and R (Version 4.0.3, The R Foundation for Statistical Computing).
Results
There were 54,948 outpatient visits during the pre-COVID period and 58,940 visits during the COVID period. Telemedicine use increased from <1% of visits to 70.7% of visits (49.7% video, 21.0% phone) during the pandemic. Of the visits during this period, 21.0% were for patients >80 years old, 44.4% were for women, 6.0% were for Black patients, 8.0% were for Hispanic patients, 10.0% were for patients on Medicaid, and 55.9% were for patients on Medicare (Table 1 ). The proportions of visits for patients from these groups stayed the same or increased as compared to the pre-COVID period.
Table 1.
Patient visit characteristics in the Pre-COVID and COVID periods.
| Characteristic | Pre-COVID, N = 54,948 N (%) |
COVID, N = 58,940 N (%) |
|---|---|---|
| Care modality | ||
|
In-person Phone Video |
54,660 (99.5%) 77 (0.1%) 211 (0.4%) |
17,283 (29.3%) 12,364 (21.0%) 29,293 (49.7%) |
| Type of visit | ||
| New visit | 11,025 (20.1%) | 10,956 (18.6%) |
| Return visit | 43,923 (79.9%) | 47,984 (81.4%) |
| Age | ||
| <60 | 15,841 (28.8%) | 16,276 (27.6%) |
| 60-79 | 27,773 (50.5%) | 30,262 (51.3%) |
| ≥80 | 11,334 (20.6%) | 12,402 (21.0%) |
| Gender | ||
| Female | 24,390 (44.4%) | 26,178 (44.4%) |
| Male | 30,553 (55.6%) | 32,753 (55.6%) |
| Missing | 5 | 9 |
| Race/Ethnicity | ||
| Non-Hispanic White | 30,172 (54.9%) | 32,834 (55.7%) |
| Asian | 10,201 (18.6%) | 10,109 (17.2%) |
| Black | 2,925 (5.3%) | 3,533 (6.0%) |
| Hispanic, all races | 4,380 (8.0%) | 4,695 (8.0%) |
| Othera | 4,623 (8.4%) | 4,941 (8.4%) |
| Missing | 2,647 | 2,828 |
| English proficiency | ||
| Proficient | 47,633 (86.7%) | 51,427 (87.3%) |
| Limited English proficiency | 7,153 (13.0%) | 7,261 (12.3%) |
| Missing | 162 | 252 |
| Insurance coverage | ||
| Private | 16,940 (30.8%) | 18,594 (31.5%) |
| Medicaid | 5,248 (9.6%) | 5,902 (10.0%) |
| Medicare | 30,665 (55.8%) | 32,921 (55.9%) |
| Other | 2,095 (3.8%) | 1,523 (2.6%) |
| Median household income, $ | ||
| <50 000 | 1,266 (2.3%) | 1,316 (2.2%) |
| 50 000-100 000 | 22,569 (41.1%) | 24,269 (41.2%) |
| >100 000 | 30,568 (55.6%) | 32,865 (55.8%) |
| Missing | 545 | 490 |
| % with a bachelor's degree or higher | ||
| <50% | 23,835 (43.4%) | 25,611 (43.5%) |
| 50-75% | 24,895 (45.3%) | 26,805 (45.5%) |
| >75% | 6,145 (11.2%) | 6,507 (11.0%) |
| Missing | 73 | 17 |
| Distance to clinic, miles | ||
| <20 | 41,004 (74.6%) | 44,137 (74.9%) |
| 20-100 | 9,755 (17.8%) | 10,854 (18.4%) |
| >100 | 3,918 (7.1%) | 3,699 (6.3%) |
| Missing | 271 | 250 |
| Subspecialty | ||
| General cardiology | 19,218 (35.0%) | 20,515 (34.8%) |
| Adult congenital heart disease | 1,609 (2.9%) | 1,392 (2.4%) |
| Electrophysiology | 8,291 (15.1%) | 9,513 (16.1%) |
| Heart failure | 4,655 (8.5%) | 4,860 (8.2%) |
| Interventional cardiology | 18,954 (34.5%) | 20,631 (35.0%) |
| Transplant | 1,250 (2.3%) | 1,146 (1.9%) |
| Vascular medicine | 971 (1.8%) | 883 (1.5%) |
| Practice type | ||
| Academic | 23,479 (42.7%) | 23,564 (40.0%) |
| Community-based | 31,469 (57.3%) | 35,376 (60.0%) |
Includes patients self-identifying as American Indian or Alaska Native, Native American, Native Hawaiian or other Pacific Islander, other, and unknown.
In adjusted analyses, use of telemedicine versus in-person care varied significantly across sociodemographic groups during the COVID period. Visits for older patients, men, patients with LEP, and those on Medicaid and Medicare were less likely to be delivered by telemedicine versus in-person (Table 2 ).
Table 2.
Adjusted odds ratios for a visit occurring by telemedicine (vs in-person) and for a telemedicine visit occurring by video (vs phone) during the COVID period.
| Characteristic | Telemedicine vs In-Person Visit OR (95% CI) (n=58,940) | Video vs Phone Telemedicine Visit OR (95% CI) (n=41,657) |
|---|---|---|
| Period | ||
| COVID - Mar-Aug 2020 | — | — |
| COVID - Sept 2020-Feb 2021 | 0.47 (0.44, 0.50) | 0.96 (0.90, 1.03) |
| Type of visit | ||
| New visit | — | — |
| Return visit | 1.51 (1.40, 1.62) | 0.11 (0.09, 0.13) |
| Age | ||
| <60 | — | — |
| 60-79 | 0.83 (0.77, 0.91) | 0.55 (0.49, 0.62) |
| ≥80 | 0.80 (0.72, 0.89) | 0.24 (0.21, 0.28) |
| Gender | ||
| Female | — | — |
| Male | 0.88 (0.83, 0.93) | 1.09 (1.02, 1.17) |
| Race/Ethnicity | ||
| Non-Hispanic White | — | — |
| Asian | 1.02 (0.94, 1.12) | 1.05 (0.94, 1.17) |
| Black | 1.01 (0.89, 1.14) | 0.64 (0.56, 0.74) |
| Hispanic, all races | 0.90 (0.81, 1.01) | 0.86 (0.75, 1.00) |
| Othera | 0.98 (0.89, 1.09) | 1.01 (0.88, 1.16) |
| English proficiency | ||
| Proficient | — | — |
| Limited English proficiency | 0.80 (0.72, 0.88) | 0.52 (0.46, 0.59) |
| Insurance coverage | ||
| Private | — | — |
| Medicaid | 0.89 (0.80, 0.99) | 0.47 (0.41, 0.54) |
| Medicare | 0.91 (0.84, 0.98) | 0.58 (0.52, 0.64) |
| Other | 0.92 (0.77, 1.11) | 0.73 (0.57, 0.93) |
| Median household income, $ | ||
| <50 000 | — | — |
| 50 000-100 000 | 0.92 (0.76, 1.11) | 1.17 (0.87, 1.56) |
| >100 000 | 0.97 (0.80, 1.18) | 1.68 (1.25, 2.24) |
| Distance to clinic, miles | ||
| <20 | — | — |
| 20-100 | 1.11 (1.02, 1.20) | 1.23 (1.10, 1.38) |
| >100 | 1.19 (1.04, 1.36) | 1.44 (1.17, 1.79) |
| Subspecialty | ||
| General cardiology | — | — |
| Adult Congenital Heart Disease | 0.31 (0.26, 0.36) | 1.90 (1.24, 3.02) |
| Electrophysiology | 1.57 (1.44, 1.73) | 1.00 (0.91, 1.11) |
| Heart failure | 0.31 (0.28, 0.34) | 1.33 (1.09, 1.64) |
| Interventional cardiology | 0.95 (0.88, 1.02) | 1.22 (1.12, 1.33) |
| Transplant | 0.13 (0.11, 0.16) | 0.45 (0.31, 0.66) |
| Vascular medicine | 0.05 (0.03, 0.07) | 8.81 (1.86, 158) |
| Site | ||
| Academic | — | — |
| Community-based | 1.65 (1.52, 1.79) | 0.44 (0.39, 0.49) |
OR = adjusted odds ratios
Includes patients self-identifying as American Indian or Alaska Native, Native American, Native Hawaiian or other Pacific Islander, other, and unknown.
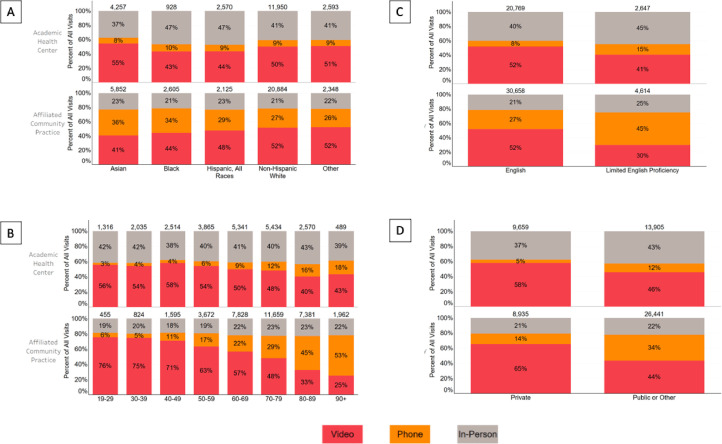
Among telemedicine visits during the COVID period (n=41,657), visits for older patients, women, Black and Hispanic patients, patients with LEP, those on Medicaid and Medicare, and those from lower income ZIP codes were less likely to be delivered by video versus phone. The observed disparities in the use of video-based telemedicine were greatest for patients aged ≥80 years (vs age <60, OR 0.24, 95% CI 0.21, 0.28), Black patients (vs non-Hispanic White, OR 0.64, 95% CI 0.56, 0.74), those with LEP (vs English proficient, OR 0.52, 95% CI 0.46-0.59), and those on Medicaid (vs privately insured, OR 0.47, 95% CI 0.41-0.54) (Table 2). A sensitivity analysis including all prespecified covariates in the models yielded similar results (Tables S1 and S2). At the community-based practice, phone visits were the most common mode of care delivery during the COVID period for patients aged ≥80 years and those with LEP (Figure 1 ).
Figure 1.
Unadjusted visits by mode of care delivery in the COVID period, stratified by practice site, across four sociodemographic characteristics: A) self-identified race/ethnicity, B) age, C) English proficiency and D) insurance coverage.
Other race/ethnicity includes patients self-identifying as American Indian or Alaska Native, Native American, Native Hawaiian or other Pacific Islander, other, and unknown.
Discussion
In this analysis of two large cardiology practices in Northern California, we found significant disparities in the modality of care delivery across sociodemographic groups during the first year of the COVID-19 pandemic. There were differences in the use of telemedicine versus in-person care, and even more strikingly, in the use of video- versus phone-based telemedicine visits, especially for patients who were 80 years and older, self-identified as Black, with non-English language preference, and publicly insured.
These practices capture the transformation in care delivery that occurred during the first year of the pandemic. Telemedicine use for cardiology visits increased from <1% to over 70% during the COVID period, with the greatest number of visits delivered by video. Despite this significant change in the modality of care, the sociodemographic characteristics of patients receiving visits remained remarkably consistent. At these practices, telemedicine thus served its intended purpose to maintain access to care during a year of COVID-19 surges, shelter-in-place orders, and business closures.
Though patients 80 years and older continued to access cardiovascular care at these practices during the pandemic, older age was associated with lower likelihood of telemedicine use and substantially decreased use of video-based telemedicine. There is a high prevalence of telemedicine unreadiness in elderly Americans, exceeding 70% in those aged 85 years or older.20 Phone-based telemedicine constituted an important mode of cardiovascular care delivery for these patients during the pandemic, particularly at the community-based practice, where it represented over 45% of all visits for patients older than 80 years.
Visits for female patients were more likely to occur by telemedicine than visits for male patients. Women took on a greater share of caregiving responsibilities during the pandemic, and thus may have relied more on telemedicine to access healthcare.21 When completing visits by telemedicine, however, women were more likely to receive phone- versus video-based visits as compared to men. It is possible that caregiving responsibilities also made it more difficult for female patients to find the private time and space required to complete video visits.
The proportion of visits for Black and Hispanic patients at these practices did not decrease during the pandemic, but these patient groups were significantly less likely to participate in video-based telemedicine as compared to non-Hispanic White patients. These finding are consistent with prior studies on disparities in digital healthcare access among Black and Hispanic patients.16 , 22 Structural social, economic and political barriers may limit access to video-based telemedicine for these patients.23 , 24 For example, as compared to White Americans, Black and Hispanic Americans have disproportionately lower access to home broadband.25 , 26 Alternatively, these differences may reflect implicit bias in the assignment of patients to care modalities or distinct patient preferences on care delivery.
Patients with non-English language preference face unique barriers in the use of telemedicine due to the challenge of adequately incorporating interpreters into virtual visits and because English proficiency may be required to navigate EHR video telemedicine patient portals.27 We found that patients with LEP were less likely to have telemedicine versus in-person visits and when receiving telemedicine visits, were more likely to have phone- versus video-based visits. At the community-based practice, 45% of visits for these patients during the COVID period were delivered by phone. As health systems move toward integrated virtual care models for chronic disease management, patients with language barriers may be left behind without further support. Clinics should develop inclusive practices to ensure seamless integration of translation services into telemedicine visits and invest in simplified video-visit on-boarding for non-English speaking patients.
The observed differences in the use of video- versus phone-based telemedicine merit further scrutiny. For some patients, phone-based visits may be sufficient for certain clinical scenarios and may be preferred as they allow for connection with clinicians through a medium that is more familiar.28 Video visits, however, offer specific benefits over phone visits, including the ability for clinicians to conduct a visual physical exam, to see a patient's home environment, and to use non-verbal communication to build rapport. Some recent evidence also suggests that outcomes from phone visits may be inferior to those from video or in-person visits for some cardiovascular conditions.29 Further research is needed comparing outcomes across care modalities for common cardiovascular diagnoses. In addition, the reliance on phone visits by some groups, highlighted in this study and others, has important policy implications as regulators consider reducing or eliminating reimbursements for this care modality.30
Patient-centered telemedicine care models hold particular promise in the management of cardiovascular disease. Recent evidence suggests that access to telemedicine may improve outcomes for ambulatory care-sensitive chronic conditions, including heart failure.4 Inequitable access to video-based telemedicine, however, may prevent certain groups from fully engaging in and reaping the benefits of integrated virtual care.31 While phone-based telemedicine continues to partially bridge the digital divide, the structural barriers driving the disparities demonstrated in this study and others must be diligently addressed.24 , 32 These barriers include insufficient broadband and technology access, implicit bias, and inadequate clinical workflows.
Healthcare organizations can promote digital inclusion by examining their own care patterns to identify and address access gaps in the populations they serve. Efforts should be made to select the most bandwidth-efficient and device-compatible technologies, develop inclusive workflows (e.g., on-boarding assistance), advocate for equitable broadband deployment, and work with community partners like libraries and schools to promote digital health literacy. These initiatives must be enabled through government regulation and legislation.33
At our own institution, the findings of this study motivated a focused effort to reduce barriers to video-visit use for patients with non-English language preference. At the time of our study, clinicians could request an interpreter if needed after joining a video visit, but this often delayed the start of the visit and interpreters could only join by audio. To address these limitations, clinical workflows were changed to notify interpreters as soon as patients joined the video-visit platform before the clinician's arrival. In addition, multiparty video conferencing was implemented to allow interpreters to join by video, so they could fully participate in the visits. Further evaluation will be needed to determine the success of interventions like these in reducing disparities in access to telemedicine.34 , 35
Our study should be interpreted in the context of some limitations. First, we retrospectively evaluated a cohort of patients who had successfully reached specialized care at one of two large cardiology practices. Therefore, this study does not capture disparities in utilization of ambulatory cardiovascular care that pre-dated the COVID-19 pandemic. Though we included two distinct cardiology practice settings, one academic and one community-based, the findings may not be generalizable to cardiology practices with different patient populations. The observational nature of this study limited our ability to determine the etiologies of the observed differences in care modality and whether they were due to disparities in access or distinct patient preferences on care delivery. We also could not evaluate the impact of patient comorbidities on the mode of care delivery as this data was not available. Finally, data on income and educational attainment were obtained at the ZIP code rather than individual patient level.
Conclusions
At two large cardiology practices, one academic and one community-based, significant sociodemographic disparities were observed in the modality of care delivery during the first 12 months of the COVID-19 pandemic. Though the patient population remained similar as compared to before the pandemic, several groups were less likely to receive telemedicine versus in-person care. Sociodemographic disparities were most notable in the use of video- versus phone-based telemedicine visits. Future studies should address barriers in telemedicine access for patients based on sociodemographic characteristics and compare outcomes across modalities of care.
Disclosures
NK reports stock options from Gordy Health outside the submitted work. FR reports consulting fees from Novartis, Janssen, NovoNordisk, and HealthPals outside the submitted work. RD reports research funding from Bayer AG and consulting fees from HealthPals outside the submitted work. The remaining authors have nothing to disclose.
Acknowledgments
Acknowledgements
The authors would like to thank the Stanford Health Care Digital Health Care Integration team for their support of this project.
Sources of Funding
This project was funded by a quality improvement grant from the Division of Cardiovascular Medicine at Stanford University School of Medicine. The investigators were also supported by funding from the United States Agency for Healthcare Research and Quality [NMK; T32 HS026128], the United States National Heart, Lung, and Blood Institute [FR; K01 HL144607 01], the American Heart Association/Robert Wood Johnson Foundation [FR], and the Kothari Family Fund [RD] not directly related to this project.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ahj.2023.06.011.
Appendix. Supplementary materials
References
- 1.Mehrotra A, Bhatia RS, Snoswell CL. Paying for Telemedicine After the Pandemic. JAMA. 2021;325(5):431–432. doi: 10.1001/jama.2020.25706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Internal Medicine. 2021;181(3):388–391. doi: 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lau J, Knudsen J, Jackson H, Wallach AB, Bouton M, Natsui S, et al. Staying Connected In The COVID-19 Pandemic: Telehealth At The Largest Safety-Net System In The United States. Health Aff (Millwood) 2020;39(8):1437–1442. doi: 10.1377/hlthaff.2020.00903. [DOI] [PubMed] [Google Scholar]
- 4.McAlister FA, Hsu Z, Dong Y, Tsuyuki RT, van Walraven C, Bakal JA. Frequency and Type of Outpatient Visits for Patients With Cardiovascular Ambulatory-Care Sensitive Conditions During the COVID-19 Pandemic and Subsequent Outcomes: A Retrospective Cohort Study. J Am Heart Assoc. 2023;12(3) doi: 10.1161/JAHA.122.027922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. The New England journal of medicine. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 6.Zulman DM, Verghese A. Virtual Care, Telemedicine Visits, and Real Connection in the Era of COVID-19: Unforeseen Opportunity in the Face of Adversity. JAMA. 2021;325(5):437–438. doi: 10.1001/jama.2020.27304. [DOI] [PubMed] [Google Scholar]
- 7.Yehia BR, Winegar A, Fogel R, Fakih M, Ottenbacher A, Jesser C, et al. Association of Race With Mortality Among Patients Hospitalized With Coronavirus Disease 2019 (COVID-19) at 92 US Hospitals. JAMA Netw Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.18039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alsan M, Stantcheva S, Yang D, Cutler D. Disparities in Coronavirus 2019 Reported Incidence, Knowledge, and Behavior Among US Adults. JAMA Netw Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME, et al. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic Bridging or Opening the Digital Divide? Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sachs JW, Graven P, Gold JA, Kassakian SZ. Disparities in telephone and video telehealth engagement during the COVID-19 pandemic. JAMIA Open. 2021;4(3) doi: 10.1093/jamiaopen/ooab056. ooab056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Totten AM, Womack DM, Eden KB, McDonagh MS, Griffin JC, Grusing S, et al. Telehealth: Mapping the Evidence for Patient Outcomes From Systematic Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016. AHRQ Comparative Effectiveness Technical Briefs. [PubMed] [Google Scholar]
- 12.Verma S. Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19. In: Blog HA, editor.; 2020.
- 13.Brown KJ, Mathenge N, Crousillat D, Pagliaro J, Grady C, Katz N, et al. Social determinants of telemedicine utilization in ambulatory cardiovascular patients during the COVID-19 pandemic. European Heart Journal - Digital Health. 2021;2(2):244–253. doi: 10.1093/ehjdh/ztab039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang X, Hidrue MK, Del Carmen MG, Weiner RB, Wasfy JH. Sociodemographic Disparities in Outpatient Cardiology Telemedicine During the COVID-19 Pandemic. Circ Cardiovasc Qual Outcomes. 2021;14(8) doi: 10.1161/CIRCOUTCOMES.121.007813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME, et al. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic. Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tam S, Wu VF, Williams AM, Girgis M, Sheqwara JZ, Siddiqui F, et al. Disparities in the Uptake of Telemedicine During the COVID-19 Surge in a Multidisciplinary Head and Neck Cancer Population by Patient Demographic Characteristics and Socioeconomic Status. JAMA Otolaryngology–Head & Neck Surgery. 2021;147(2):209–211. doi: 10.1001/jamaoto.2020.3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hollander JE. Maturation from Adoption-Based to Quality-Based Telehealth Metrics. NEJM Catalyst. 2020 [Google Scholar]
- 18.Kalwani NM, Osmanlliu E, Parameswaran V, Qureshi L, Dash R, Heidenreich PA, et al. Changes in telemedicine use and ambulatory visit volumes at a multispecialty cardiovascular center during the COVID-19 pandemic. J Telemed Telecare. 2022 doi: 10.1177/1357633X211073428. 1357633X211073428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell-Wiley TM, Baumer Y, Baah FO, Baez AS, Farmer N, Mahlobo CT, et al. Social Determinants of Cardiovascular Disease. Circ Res. 2022;130(5):782–799. doi: 10.1161/CIRCRESAHA.121.319811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lam K, Lu AD, Shi Y, Covinsky KE. Assessing Telemedicine Unreadiness Among Older Adults in the United States During the COVID-19 Pandemic. JAMA Internal Medicine. 2020;180(10):1389–1391. doi: 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ranji U, Frederiksen B, Salganicoff A, Long M. Women's Health Policy: Kaiser Family Foundation; 2021. Women, Work, and Family During COVID-19: Findings from the KFF Women's Health Survey. [Google Scholar]
- 22.Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, et al. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Network Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31640. -e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thronson LR, Jackson SL, Chew LD. The Pandemic of Health Care Inequity. JAMA Network Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.21767. -e2021767. [DOI] [PubMed] [Google Scholar]
- 24.Neff J, Holmes SM, Knight KR, Strong S, Thompson-Lastad A, McGuinness C, et al. Structural Competency: Curriculum for Medical Students, Residents, and Interprofessional Teams on the Structural Factors That Produce Health Disparities. MedEdPORTAL. 2020;16:10888. doi: 10.15766/mep_2374-8265.10888. -10888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Planet Digital. The Fletcher School; 2021. Digital Injustice: Disparities in Digital Access across the US and How they Disproportionately Hurt the Black and Latinx Communities. editor. [Google Scholar]
- 26.Marshall B, Ruane K. Union ACL; 2021. How Broadband Access Advances Systemic Equality. editor. [Google Scholar]
- 27.Payán DD, Frehn JL, Garcia L, Tierney AA, Rodriguez HP. Telemedicine implementation and use in community health centers during COVID-19: Clinic personnel and patient perspectives. SSM Qual Res Health. 2022;2 doi: 10.1016/j.ssmqr.2022.100054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baras Shreibati J. When Low Tech Wins. N Engl J Med. 2021;385(7):581–583. doi: 10.1056/NEJMp2104234. [DOI] [PubMed] [Google Scholar]
- 29.Yuan N, Botting PG, Elad Y, Miller SJ, Cheng S, Ebinger JE, et al. Practice Patterns and Patient Outcomes After Widespread Adoption of Remote Heart Failure Care. Circ Heart Fail. 2021;14(10) doi: 10.1161/CIRCHEARTFAILURE.121.008573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kleinman RA, Sanches M. Impacts of Eliminating Audio-Only Care on Disparities in Telehealth Accessibility. J Gen Intern Med. 2022;37(15):4021–4023. doi: 10.1007/s11606-022-07570-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.2019. American Hospital Association. Telehealth: A Path to Virtual Integrated Care. [Google Scholar]
- 32.Khoong E, Nouri S, Lyles C, Karliner L. Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. 2020.
- 33.Rodriguez JA, Shachar C, Bates DW. Digital Inclusion as Health Care - Supporting Health Care Equity with Digital-Infrastructure Initiatives. N Engl J Med. 2022;386(12):1101–1103. doi: 10.1056/NEJMp2115646. [DOI] [PubMed] [Google Scholar]
- 34.Khoong E, Nouri S, Lyles C, Karliner L. Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. NEJM Catal Innov Care Deliv. 2020 [Google Scholar]
- 35.Curfman AL, Hackell JM, Herendeen NE, Alexander JJ, Marcin JP, Moskowitz WB, et al. Telehealth: Improving Access to and Quality of Pediatric Health Care. Pediatrics. 2021;148(3) doi: 10.1542/peds.2021-053129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.