Abstract
In India, expenditure incurred to access mental health services often drives families to economic crisis. Families of Persons with mental illness (PMI) incur ‘out-of-pocket’ (OOP) expenditure for medicines, psychiatrist fee and travel in addition to losing wages on the day of visiting psychiatrist.
Aim:
To describe impact of Community Based Rehabilitation (CBR) on OOP expenditure incurred by families of persons with severe mental illness (PSMI).
Methods:
The sample comprised 95 PSMI who switched from treatment from other mental health facilities to CBR at Jagaluru, India.
Results:
The PSMI were predominantly male (52%) with mean age 41 years and diagnosed with psychosis (75%). Most of them (84%) were earlier taking treatment from private sector and spent on an average Rs. 15,074 (US $ 215) per PSMI per annum in availing treatment. After availing CBR, the annual expenditure reduced to Rs 492 (US $ 7) on an average per PSMI. OOP expenditure on medicines (largest head of expenditure) and psychiatrist consultation fee dropped to zero.
Discussion:
After excluding costs incurred to run the CBR, the net savings for the system for 95 PSMI included in study alone was Rs 3,83,755 (US $ 5,482) per annum. The amount would be much higher on including savings for PSMI initiated on treatment for the first time and PMI on regular follow-up in CBR.
Conclusions:
Provision of CBR in partnership with public health system and NGO’s leads to dramatic fall in OOP health expenditure of families of PSMI. It is also cost-effective to the system.
Keywords: Out-of-pocket expenditure, Community based rehabilitation, Mental illness, Public health
1. Introduction
The National Mental health Survey of India (2015–16) reported that the treatment gap is as high as 83% for mental health problems (Gururaj et al., 2016). 85% of persons with mental illness (PMI) seek treatment from private sector (Gururaj et al., 2016). Expenditure incurred to access care (about Rs 1000–1500 per month for treatment and travel) often drove families to economic crisis (Gururaj et al., 2016).
India is heavily dependent on out-of-pocket (OOP) expenditure and private health care (Reddy et al., 2011) for her health care needs. OOP expenditure includes direct costs incurred for travel, lodging, food, drugs bought, investigations made, money spent on paper work or other treatments (Grover et al., 2005). Health spending is considered catastrophic when a household must reduce its basic expenditure over a period of time to cope with health costs (Xu et al., 2003). Catastrophic expenditure is incurred by poorest people in hospitalization for cancers (85%), psychiatric and neurological disorders (63%) and injuries (63%) (Tripathy et al., 2016). 3.25–4% of the Indian population gets impoverished due to healthcare payments (Chowdhury et al., 2018). Substantial proportion of healthcare related impoverishment in India has been attributed to people’s preference for private hospitals (Kastor and Mohanty, 2018).
Dispensing free psychotropic medicines is an acceptable cost-effective intervention to reduce direct OOP expenditure which benefits families from lower socioeconomic status (Yan et al., 2019). In Indian government health facilities, PMI can avail free or subsidized consultation and may also get free psychotropic medicines (Grover et al., 2005; Sarkar et al., 2017; Sharma et al., 2006). The Government of India has recently passed Mental Heath care act (2017) which specifies that essential list of psychotropic medicines be made available free of cost at community health centres (Mental Health care Act, 2017). In private sector, OOP expenditure is incurred for consultation and medicines. Irrespective of government or private facility, family incurs expenditure on travel, food and accommodation for follow-up consultation with psychiatrist. Frequently, a caregiver also accompanies with the patient for consultation and this doubles the cost of travel, food and accommodation.
Our team has been running a community-based rehabilitation (CBR) program for PMI in a rural taluk (a local administrative block) of Karnataka state. A CBR program deals with health, education, livelihood, social and empowerment domains. In the current paper, we are presenting data pertaining to health component of our CBR program. This report describes the reduction of OOP expenditure incurred by persons with severe mental illness/families after availing community based mental health services.
2. Methods
2.1. Setting
Jagaluru taluk in Davangere district (Karnataka, India) has a population of about 171,000, more than 90% live in villages. Agriculture is the predominant source of livelihood and more than 90% area is rain dependent. The taluk is regularly declared as drought hit by Government of Karnataka and is economically backward. The taluk has ten primary health centres (PHCs) and one Taluk hospital. There are no psychiatrists at the Jagaluru Taluk. Davanagere, the district headquarters town, has a government district hospital with psychiatrists working full time and 2 private medical colleges with departments of psychiatry and a few private psychiatrists.
As part of CBR program, since August 2015, mental health camps are being conducted on 1st and 3rd Tuesday of every month at the ten PHCs & taluk hospital. The psychiatrists from our team (one consultant psychiatrist and one junior/senior resident) visit the taluk twice in a month during camps and attend to persons with mental illness. Two social workers liaise with stakeholders, coordinate the camps, do periodic home visits and remind families for camps. When there are patients who are unable to come to the PHC, home visits are done to assess the patient at their home and start treatment. Patients are given medicines for up to 3 months along with next follow-up date. The program involves grass-root workers including Accredited Social Health Activists (ASHA), Village health nurse, Anganwadi workers, Village rehabilitation workers, Auxiliary nurses and midwives. Psychotropic medicines are dispensed free of cost.
So far, the program has catered to 778 persons with mental health issues. About 275 PMI are on regular follow-up (have not missed the follow-up consultations) over last 1 year and avail free services close to their residence under the program. Among those on regular follow-up, many beneficiaries were initiated on treatment for the first time ever by active outreach.
2.2. Aim
To describe impact of Community Based Rehabilitation (CBR) on OOP expenditure incurred by families of persons with severe mental illness (PSMI)
2.3. Sample
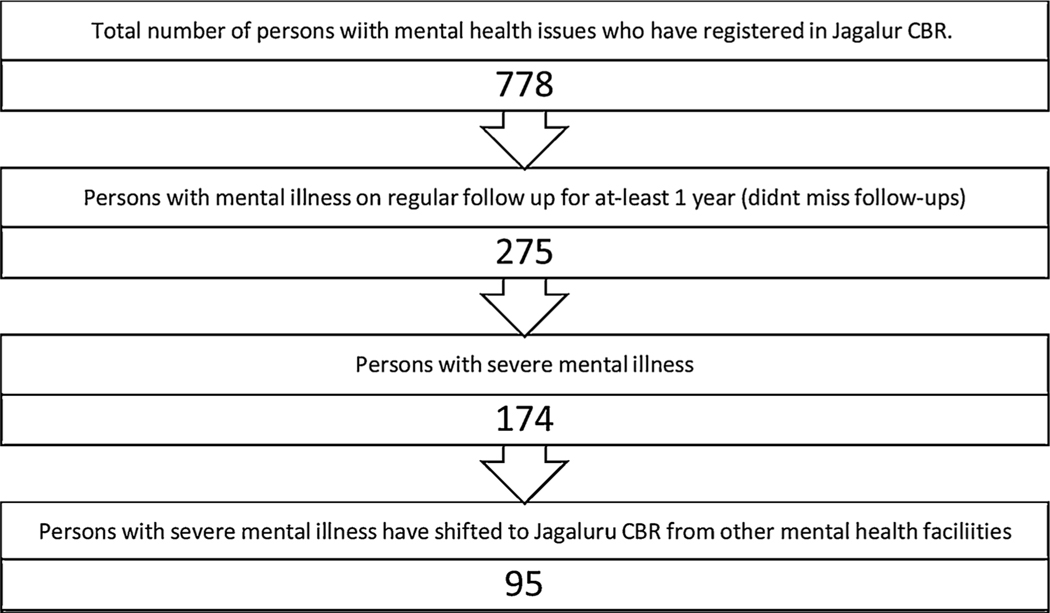
95 PSMI who were on treatment from other mental health facilities (private & Government), switched to Jagaluru CBR and are on regular follow-up for > 1 year comprised study sample (Flowchart 1).
Flowchart 1.
Flowchart depicting participant recruitment.
PSMI/ families were enquired about
Mental health facility where treatment was sought earlier
Number of people who travelled for follow-up with psychiatrist (PMI with family caregiver or PMI alone or family caregiver alone for a proxy consultation)
Frequency of visit
Expenses incurred per person for round trip to mental health facility from home
Psychiatrist consultation fee per visit
Expenses incurred for medicines per visit
Source of money
Wherever available, the receipt for medicines purchased from earlier health facility was checked.
Most people in Jagaluru are engaged in casual labour and agriculture related work. Work is not available daily. If rains are timely, work is available around sowing and harvesting crops. Based on average wages per person, loss of wage of Rupees 200 (US $ 3 at US $ Indian Rupee exchange rate of 1 US $ = 70 Rupees) per day was assumed per person while travelling to seek psychiatrist consultation.
Institutional ethics committee clearance has been taken for the Jagaluru CBR study.
2.4. Statistics used
Descriptive statistics are used for socio-demographic profile and clinical profile of the patients. Paired t-test (2-tailed, with confidence interval (CI) 0.99) is used for OOP expenditure.
GNU pspp 1.2.0-g0fb4db is used for analyses of the data (Free Software Foundation, Inc. 2013. https://www.gnu.org/software/pspp/)
3. Results
The socio-demographic, clinical variables, mental healthcare facility accessed before availing CBR and annual OOP expenditures are provided in Tables 1–3. Before shifting to Jagaluru CBR, 84% of study sample was availing treatment from private facilities despite availability of government facilities at district headquarters.
Table 1.
Socio-demographic and Clinical profile of persons with mental illness (n = 95).
| Socio-demographic & clinical variables | N (%)/ Mean (SD) |
|---|---|
|
| |
| Age | 40.70 (12.12) |
| Gender | |
| Male | 49 (.51.6%) |
| Female | 46 (48.4%) |
| Education (in years) | 4.44 (4.78) |
| Duration of illness (in years) | 11.16 (5.95) |
| Diagnosis | |
| Psychosis (including Schizophrenia) | 71 (74.7) |
| Bipolar affective disorder | 24 (25.3) |
Table 3.
Annual Out of pocket expenditure per PSMI per year (in Rupees).
| Expenditure Head | Mean (SD) In Rupees | T (df) | Significance (2-tailed) CI 0.99 | |
|---|---|---|---|---|
|
|
||||
| Before CBR | After CBR | |||
|
| ||||
| Travel | 2780 (3022) | 53 (86) | 8.77(94) | < 0.001 |
| Psychiatrist fee | 619 (402) | 0 | 14.91 (94) | < 0.001 |
| Medicines | 9911(10562) | 0 | 9.15 (94) | < 0.001 |
| Loss of wage | 1469 (2933) | 413 (419) | 3.43 (94) | < 0.001 |
| Total Expenditure | 15074(15333) | 492 (511) | 9.24 (94) | < 0.001 |
After switching to Jagaluru CBR, PSMI being accompanied by a family member for follow-up with the psychiatrist reduced from 99% to 68% & PSMI visiting psychiatrist alone increased from 1% to 32%. It is important to note that the study sample included those who were on regular follow-up and were maintaining well on medicines. They were also followed up periodically by staff in home visits where medication adherence checked and family psycho-educated. Consequently, indirect cost to family on account of ‘loss of wages’ came down.
Jagaluru CBR has significantly brought down OOP expenditure incurred by PSMI and their families. For those availing our services, annual expenses incurred on medicines (which were the largest head of expenditure) and psychiatrist consultation fee has come down to zero. The cost per annum incurred in travel to avail Jagaluru CBR is 2% of what the families spent earlier. Total OOP annual expenditure incurred by 95 families of PSMI cost before shifting to Jagaluru CBR was Rs 14,04,020 (US $ 20,057) and it reduced to Rs 44,240 (US $ 632) after shifting to Jagalur CBR. After switching to Jagaluru CBR, 95 families of PSMI saved Rs 13,59,780 (US $ 19,425) per annum.
4. Discussion
In India, fiscal constraints are not the biggest barrier to offer mental health services. Money allotted by Government for mental health remains unspent (Goel, 2011). In this context, it is unfortunate that poor people forego treatment due to financial constraints (Balarajan et al., 2011). For healthcare system, community based care for mental health services is more cost effective than hospital based care, improves quality of life for patients and also expands access to care for the needy (Chatterjee et al., 2009, 2003a; Collins et al., 2011; Goel, 2011; Puspitosari et al., 2019).
At national and international level, economic data is needed to influence mental health policy and resource allocation (Chisholm et al., 2000). Demonstration of financial savings to the system and patients by managing mental illness in community will help policymakers scale up such initiatives (Jacob, 2001). The present study shows that the when services are made available near to the homes of PMI, OOP expenditure came down dramatically. The effect could be long standing in terms of preventing families from getting impoverished due to health expenditure and drifting down the social ladder. This is of importance for policy discussion and service development.
In line with other studies (Bhojani et al., 2012; Tripathy et al., 2016), medicines accounted for the largest chunk of OOP expenditure. Though the same medicines were available free of cost at Government hospital at district headquarters, many were availing it from private sector. The authors have come across families save money over several months/ years so that they can afford to take the PMI for treatment in towns where popular private psychiatric centers are available. In our experience, this preference of health care utilization from private sector is due to a range of factors:
Lack of awareness that treatment for mental illness is available in government hospital.
PMI approach healthcare facility at times when patient is unmanageable at home. The private sector offers them admission immediately which alleviates the distress of family. The same may not be availed in as easily in public facilities, where there is competition for limited beds. When the PMI improves with treatment at a facility, the family trusts the facility and prefers to continue at the same facility.
Personal negative experience of unsatisfactory care (including absence or interruption in continuous availability of medicines (Murthy et al., 2005), lack of continuity of care) adversely impacts the reputation of the health care facility in the community making others wary of that facility.
In government hospital, it cannot be guaranteed that patient can seek consultation from the same doctor(s) of their choice with whom they have gained trust (Russell, 2005)
Except 5 families, the rest families of PSMI reported having borrowed for treatment in addition to selling assets or spending from savings and income. People take loans for health care depending on timing of the payment and cash-flow problems. Most rural poor households in India have income from work as agricultural labourers around sowing/ harvest season and while selling the crop during harvest (Binnendijk et al., 2012). At other times of the year, they are left with no other option but to spend from savings or sell assets or borrow.
In India, the role of family is ‘all-pervasive’ influencing decision to seek treatment, mental health facility to be consulted, need to continue treatment and issues pertaining to marriage, employment and other rehabilitation issues (Thara et al., 2004). While consulting a psychiatrist, a family member is required to corroborate history. In an underprivileged area, people feel overwhelmed to travel alone to nearby city and prefer to have company of another person (who may also be a family member) who is well versed with travel. Most PMI in the study sample were accompanied by a family member for follow-up consultations. Only one person from the study sample reported of having travelled alone for consultation to the city. When services are provided at the nearest PHC/ Taluk hospital and PSMI was maintaining well on regular medicines, PSMI could come alone for a proportion of visits. In such instances, the family caregiver who used to accompany for follow-up consultations is free to use the time for other purposes. As psychiatrist can corroborate information from fellow villagers or PHC staff or ASHA worker who lives in the same village & from staff who does home visits, there is no difficulty in providing care.
Jagaluru CBR lead to a savings of Rs 13,59,780 (US $ 19,425) per annum to 95 families of PSMI who had switched to our services. PSMI have shifted to our services over a period of time by ‘word of mouth’ publicity that quality mental health care services were being provided free of cost near their home periodically and beneficiaries were doing well. In our experience, people also express preference to see the same doctor (TS) during camps and feel reassured after being told that the other doctor (resident who accompanies for camp and changes every time) has prescribed the appropriate medicine. At the same time, there are several families who are comfortable with continuing treatment at the private facility and do not want to take ‘risk’ of Jagaluru camp medicine ‘not suiting’ their family member with mental illness.
On analyzing expenditure incurred in running Jagaluru CBR (Table 4), the largest component of expenditure was human resource costs: monthly salary of staff, salary of consultant psychiatrist and resident for time spent at mental health camps. We did not include the costs of providing services at PHC/ Taluk hospital and utilizing their resources (including infrastructure, consultation room, services of staff in camps, injections administered etc). The annual expenditure to run Jagaluru CBR (for 778 registered Persons with mental health challenges) is Rs 8,76,000 (US $ 12,514).
Table 4.
Annual expenses to run Jagaluru CBR (in Rupees).
| Expenditure Head | PMI (n) | In Rupees |
|---|---|---|
|
| ||
| 2 staff: 1 from Association of People with disability (NGO) & 1 project staff | 778 | 4,50,000 |
| Travel expenses for camps (Round trip from Bengaluru to Jagaluru & Local travel) | 778 | 1,40,000 |
| Miscellaneous (Food, stationery, postal expenses) | 778 | 70,000 |
| 1 Consultant psychiatrist + 1 Resident (24 days salary) | 778 | 2,16,000 |
| Expenses related to medication (dispensed from Government of Karnataka supply (DMHP/PHC) Chittasanjeevini charitable trust/ project funds) | 95 | 1,00,025 |
| Total expenditure | 9,76,025 | |
For 95 PSMI, expenses incurred for purchasing medicines which were dispensed free of cost for calendar year 2018 is as follows
Government of Karnataka (medicines indented through PHC or Taluk Hospital or District Mental Health Program (DMHP)) : Rs 30,301 (US $ 433)
Chittasanjeevini charitable trust : Rs 62,014 (US $ 886)
Project funds: Rs 7,710 (US $ 110) for clozapine, penfluridol and propranolol tablets.
Before shifting to Jagaluru CBR, 95 families of PSMI incurred OOP annual expenditure of Rs 941,560 (US $ 13,450) on medicines earlier. The annual expenses incurred to give free medicines to them was only Rs 1,00,025 (US $ 1,429) which is a little above 10% of money which they were spending earlier. The dramatic fall is mainly attributable to the cheap prices at which organizations procure medicines while ordering in bulk and rationalization of pharmacotherapy in Jagaluru CBR.
The annual expenditure to run Jagaluru CBR (including costs to provide services for 778 registered persons with mental health issues; and medicines for 95 PSMI included in study sample) is Rs 9,76,025 (US $ 13943). After availing Jagaluru CBR, 95 families of PSMI saved Rs 13,59,780 (US $ 19,425) per annum as OOP. The net annual savings to the system for 95 PSMI alone is Rs 3,83,755 (US $ 5,482). This amount will be much higher if remaining PSMI who were initiated on treatment for the first time and those with diagnosis other than severe mental illness are also accounted for.
4.1. Implications
‘Providing effective and affordable community-based care and rehabilitation’ (Collins et al., 2011) expands accessibility of services to needy, brings down OOP health expenditure for family and is cost-effective for the healthcare system. Investing in community based mental health services to provide free psychotropic medicines near homes of PMI yields tangible macro-level economic benefits and increased productivity (Goel, 2011). In addition to public health facilities, mental health professionals need to partner with non-governmental organizations (NGO’s) working in disability sector, build their capacity in mental health, draw upon their knowledge of community resources in running a CBR program for PMI (Chatterjee et al., 2003b; Sivakumar et al., 2015; WHO/UNESCO/ILO/IDDC, 2010).
4.2. Limitations
As PSMI / family were interviewed about expenditure incurred in taking treatment before availing Jagaluru CBR, the estimates are subject to recall bias. We tried to minimize it by cross checking the receipts where available.
The mental health camps were conducted in PHC and taluk hospital. The services of the PHC/ Taluk hospital staff were used during the mental health camps. The costing for using PHC/ Taluk hospital infrastructure and utilizing services of the hospital staff wasn’t calculated.
Sometimes, family clubs the visit to mental health facility with other work (like purchasing items for household consumption, for agriculture etc) or social obligations. In a retrospective study, it is difficult to account for it. We assumed that travel expenditure was only for mental health consultation.
5. Conclusions
Provision of CBR in partnership with public health system and NGO’s leads to a dramatic fall in OOP health expenditure of families of PSMI. The effect could be long standing in terms of preventing families from getting impoverished due to health expenditure and drifting down the social ladder. It is also cost-effective to the system.
Table 2.
Mental Health facility accessed before availing CBR.
| Location of mental health facility | Distance from Jagaluru (in km) | N (%) N = 95 |
|---|---|---|
|
| ||
| Shivamogga (Private) | 120–160 | 61 (64.2) |
| Davangere (Private) | 30–70 | 17 (17.9) |
| Davangere (Public) | 30–70 | 6 (6.3) |
| Dharwad (Public) | 200–240 | 5 (5.3) |
| Bengaluru (Public) | 220–260 | 3 (3.2) |
| Chitradurga (Public) | 20–60 | 1(1) |
| Chitradurga (Private) | 20–60 | 2(2.1) |
Acknowledgements
The authors would like to place on record their appreciation of the support provided by Department of Psychiatry, NIMHANS, Bengaluru, District Health Officer (Davangere), District Leprosy officer (Davangere), District Mental health program (Davangere), Taluk health Officer (Jagaluru) and all the heath staff in Jagaluru taluk.
The work would not have been possible without support of Association of People with disability: [Mr Janardhana AL (Assistant Director: Inclusive education & Community mental health program), Mr Santosha S (Executive, Community mental health program, Davangere) and Mr Rajappa T (staff, Community mental health program, Davangere)], Chittasanjeevini charitable trust, Mr Dundappa Doddur (project staff) and officials/ key community members at Jagaluru.
Financial disclosure
This work was supported by research grants to Dr Thanapal Sivakumar from NIMHANS intramural research grant, The Live Love laugh Foundation and Indian Council of Medical Research.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Balarajan Y, Selvaraj S, Subramanian SV, 2011. Health care and equity in India. Lancet 377, 505–515. 10.1016/S0140-6736(10)61894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhojani U, Thriveni B, Devadasan R, Munegowda C, Devadasan N, Kolsteren P, Criel B, 2012. Out-of-pocket healthcare payments on chronic conditions impoverish urban poor in Bangalore, India. BMC Public Health 12, 990. 10.1186/1471-2458-12-990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binnendijk E, Koren R, Dror DM, 2012. Hardship financing of healthcare among rural poor in Orissa, India. BMC Health Serv. Res 12, 23. 10.1186/1472-6963-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee S, Patel V, Chatterjee A, Weiss HA, 2003a. Evaluation of a community-based rehabilitation model for chronic schizophrenia in rural India. BJP 182, 57–62. 10.1192/bjp.182.1.57. [DOI] [PubMed] [Google Scholar]
- Chatterjee S, Patel V, Chatterjee A, Weiss HA, 2003b. Evaluation of a community-based rehabilitation model for chronic schizophrenia in rural India. Br. J. Psychiatry 182, 57–62. [DOI] [PubMed] [Google Scholar]
- Chatterjee S, Pillai A, Jain S, Cohen A, Patel V, 2009. Outcomes of people with psychotic disorders in a community-based rehabilitation programme in rural India. BJP 195, 433–439. 10.1192/bjp.bp.108.057596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisholm D, James S, Sekar K, Kumar KK, Murthy RS, Saeed K, Mubbashar M, 2000. Integration of mental health care into primary care Demonstration cost-outcome study in India and Pakistan. BJP 176, 581–588. 10.1192/bjp.176.6.581. [DOI] [PubMed] [Google Scholar]
- Chowdhury S, Gupta I, Trivedi M, Prinja S, 2018. Inequity & burden of out-of-pocket health spending: district level evidences from India. Indian J. Med. Res 148, 180–189. 10.4103/ijmr.IJMR_90_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, 2011. Grand challenges in global mental health. Nature 475, 27–30. 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel D, 2011. Why mental health services in low- and middle-income countries are under-resourced, underperforming: an Indian perspective. Natl. Med. J. India 24, 94–97. [PubMed] [Google Scholar]
- Grover S, Avasthi A, Chakrabarti S, Bhansali A, Kulhara P, 2005. Cost of care of schizophrenia: a study of Indian out-patient attenders. Acta Psychiatr. Scand 112, 54–63. 10.1111/j.1600-0447.2005.00512.x. [DOI] [PubMed] [Google Scholar]
- Gururaj G, Varghese M, Benegal V, Rao G, Pathak K, Singh L, Mehta R, Ram D, Shibhukumar T, Kokane A, Lenin Singh R, Chavan B, Sharma P, Ramasubramanian C, Dalal P, Saha P, Deuri S, Giri A, Kavishvar A, Sinha VK, Thavody J, Chatterji R, Akoijam B, Das S, Kashyap A, Raghavan V, Singh S, Misra R, NMHS collaborators group, 2016. National Mental Health Survey of India. Prevalence, Patterns and Outcomes, pp. 2015–2016. [Google Scholar]
- Jacob K, 2001. Community care for people with mental disorders in developing countries: problems and possible solutions. Br. J. Psychiatry 178, 296–298. [DOI] [PubMed] [Google Scholar]
- Kastor A, Mohanty SK, 2018. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: Do Indian households face distress health financing? PLoS One 13, e0196106. 10.1371/journal.pone.0196106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy RS, Kumar KVK, Chisholm D, Thomas T, Sekar K, Chandrashekar CR, 2005. Community outreach for untreated schizophrenia in rural India: a follow-up study of symptoms, disability, family burden and costs. Psychol. Med 35, 341–351. 10.1017/S0033291704003551. [DOI] [PubMed] [Google Scholar]
- Puspitosari WA, Wardaningsih S, Nanwani S, 2019. Improving the quality of life of people with schizophrenia through community based rehabilitation in Yogyakarta Province, Indonesia: a quasi experimental study. Asian J. Psychiatry 42, 67–73. [DOI] [PubMed] [Google Scholar]
- Reddy KS, Patel V, Jha P, Paul VK, Kumar AS, Dandona L, 2011. Towards achievement of universal health care in India by 2020: a call to action. Lancet 377, 760–768. 10.1016/S0140-6736(10)61960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell S, 2005. Treatment-seeking behaviour in urban Sri Lanka: trusting the state, trusting private providers. Soc. Sci. Med 61, 1396–1407. 10.1016/j.socscimed.2004.11.077. [DOI] [PubMed] [Google Scholar]
- Sarkar S, Mathan K, Sakey S, Shaik S, Subramanian K, Kattimani S, 2017. Cost-oftreatment of clinically stable severe mental illnesses in India. Indian J. Soc. Psychiatry 33, 262–268. 10.4103/0971-9962.214600. [DOI] [Google Scholar]
- Sharma P, Das SK, Deshpande SN, 2006. An estimate of the monthly cost of two major mental disorders in an Indian metropolis. Indian J. Psychiatry 48, 143–148. 10.4103/0019-5545.31576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivakumar T, Sathish Kumar SV, Arun G, 2015. Partnership with non-governmental organizations working for persons with physical disability: need of the hour for psychiatric rehabilitation. J. Psychosoc. Rehabil. Ment. Health 2, 153–154. 10.1007/s40737-015-0040-7. [DOI] [Google Scholar]
- Thara R, Padmavati R, Srinivasan TN, 2004. Focus on psychiatry in India. Br. J. Psychiatry 184, 366–373. [DOI] [PubMed] [Google Scholar]
- Mental Health care Act, 2017. Available from https://indiacode.nic.in/handle/123456789/2249?view_type=search&sam_handle=123456789/1362. Last accessed on 3rd March 2019.
- Tripathy JP, Prasad BM, Shewade HD, Kumar AMV, Zachariah R, Chadha S, Tonsing J, Harries AD, 2016. Cost of hospitalisation for non-communicable diseases in India: are we pro-poor? Trop. Med. Int. Health 21, 1019–1028. 10.1111/tmi.12732. [DOI] [PubMed] [Google Scholar]
- WHO/UNESCO/ILO/IDDC, 2010. Community Based Rehabilitation: CBR Guidelines. World Health Organization, Geneva. [PubMed] [Google Scholar]
- Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL, 2003. Household catastrophic health expenditure: a multicountry analysis. Lancet 362, 111–117. 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- Yan F, Yang Y, Huang Q, Chen Y, Jia P, Chen W, Ma X, 2019. Cost-effectiveness of a free drug program for schizophrenia in Beijing, China. Int. J. Soc. Psychiatry 65, 28–37. 10.1177/0020764018815200. [DOI] [PubMed] [Google Scholar]