Abstract
Although partner alcohol use and acceptance of intimate partner violence against women (IPVAW) are critical determinants of IPVAW, little is known about their interaction. We explored how partner alcohol use and attitudes toward IPVAW act independently and jointly at the individual and community levels to influence women’s reports of experiencing IPVAW across low- and middle-income countries. We conducted secondary analyses using a pooled sample of reproductive-aged women (n = 166,621) from 19 Demographic and Health Survey datasets. We fit a series of a priori-defined mixed-effects logistic regression models of the total effects, within- and between-community effects, and contextual effects of past-year IPVAW on partner alcohol use, acceptance of IPVAW, and their multiplicative interaction. We then fit a series of models stratified by community alcohol use and acceptance of IPVAW. Partner alcohol use (odds ratio [OR] = 3.20; 95% confidence interval [CI]: [3.07, 3.33]) and women’s acceptance of IPVAW (OR = 1.83; 95% CI: [1.76, 1.89]) were consistently associated with increased odds of experiencing IPVAW. Sub-multiplicative interactions were present for within-community effects (ratio of OR = 0.86; 95% CI: [0.79, 0.94]), whereas supra-multiplicative interactions were present for between-community effects (ratio of OR = 1.002; 95% CI: [1.0002, 1.005]) and contextual effects (ratio of OR = 1.003; 95% CI: [1.0007, 1.005]). The odds of IPVAW associated with partner alcohol use was greatet in communities with lower partner alcohol prevalence and lower acceptance of IPVAW. It is important to consider norms and attitudes toward IPVAW alongside alcohol use when understanding epidemiological patterns of IPVAW and potential opportunities for preventive programs and policymaking. Future studies should focus on the complex interactions, at multiple social levels, between interacting risk factors for IPVAW.
Keywords: intimate partner violence, alcohol, attitudes toward intimate partner violence, low- and middle-income country
Intimate partner violence against women (IPVAW), defined as behavior within an intimate relationship that threatens or causes physical, psychological, or sexual harm, is a leading risk factor for poor health outcomes among women globally (World Health Organization, 2022). Although IPV affects all genders, male perpetrated IPVAW especially is prevalent globally and often is associated with more serious consequences (Caldwell et al., 2012). More than one quarter of ever-partnered women aged 15 to 49 years old experience physical or sexual violence perpetrated by an intimate partner during their lifetime (Sardinha et al., 2022). Consequences of IPVAW include physical and mental health problems, functional impairment, social exclusion and stigma, economic impacts, and mortality (Bacchus et al., 2018; Kennedy et al., 2018; Krug et al., 2002). Furthermore, IPVAW presents risks for children exposed to violence (McTavish et al., 2016) and economic and social costs to society (Krug et al., 2002).
Multiple risk factors have shown consistent associations with IPVAW. These include diverse factors related to women (e.g., age, witnessing IPV in childhood, and polygyny), partners (e.g., current alcohol use), and households (e.g., wealth) (Coll et al., 2021). In a recent analysis, fifteen risk factors were evaluated using a decision tree analysis. Witnessing IPV during childhood, partner alcohol use, and empowerment (of which attitudes toward IPVAW is one component) emerged as the three most important risk factors (Coll et al., 2021). Partner alcohol use and attitudes toward IPVAW have overlapping risk factors and pathways occurring at multiple levels of the social ecology; yet, they historically have been addressed by different investigators, disciplines, and interventions, and therefore, their intersections are underexplored.
Alcohol use is a well-established modifiable risk factor for IPVAW perpetration (Abbey et al., 2014; Durevall & Lindskog, 2015; Ezard, 2014; Foran & O’Leary, 2008; Wagman et al., 2016). Alcohol use is believed to directly increase risk for IPVAW perpetration via the psychophysiological effects of alcohol (Pihl et al., 2002). It also shares common risk factors with IPVAW, such as inequitable gender attitudes, that vary across cultures and contexts. Research on the relationship between alcohol use and IPVAW from low- and middle-income countries (LMICs) has identified that in addition to shared individual-level risk factors, contextual factors may also modify the association between alcohol use and IPVAW (Greene et al., 2017). For example, in communities where alcohol use is more normative and acceptable, there may be fewer social consequences related to alcohol use. Improved understanding of the multilevel conditions that strengthen the pathways from alcohol use to IPVAW is critical for the design of effective prevention and early intervention strategies.
Attitudes toward IPVAW are another critical link in the complex causal chain toward IPVAW. Attitudes toward IPVAW concern stances about what is and what is not acceptable regarding the use of violence in intimate relationships. They are shaped by cultural and contextual factors, and in turn, shape the environment in which IPVAW occurs (Gracia et al., 2020). Like alcohol use, attitudes toward IPVAW have been shown to be a risk factor for IPVAW, and attitudes to IPVAW themselves are determined through predictors at multiple levels. Attitudes toward IPVAW measured among women and/or men have been associated with the perpetration of IPVAW (McCarthy et al., 2018), survivors’ responses to IPVAW victimization, societal and institutional responses to IPVAW, and differences in IPVAW prevalence across communities and countries (Heise & Kotsadam, 2015). Attitudes that accept or condone male-perpetrated IPVAW may represent a manifestation of broader gender inequity and social and cultural norms that favor men: that is, patriarchal values (Flood & Pease, 2009; Herrero et al., 2017; Tran et al., 2016). They also may reflect broader cultural norms that sanction violence to discipline transgressions against norms and values (Lawoko, 2008). However, multiple interpersonal, situational, and contextual factors shape how gender inequity and likely attitudes toward IPVAW are associated with IPVAW (Weber et al., 2019). Whereas changing IPVAW attitudes has been identified as a primary focus for prevention and early intervention (Ellsberg et al., 2015; Jewkes et al., 2015), limited attention has been granted to characterizing how attitudes toward IPVAW interact with other risk factors to influence IPVAW, which is critical for describing how and at what level to address attitudes to reduce IPVAW. For example, should programs work to change attitudes of individuals or reduce acceptance of violence at the community level? To what extent do such interventions need to address other independent or synergistic risk factors for IPVAW?
As described above, both partner alcohol use and attitudes to IPVAW are well-established risk factors for IPVAW. Both these risk factors interact with IPVAW in complex, multilevel pathways. Understanding these complex interactions is essential for the design of preventive interventions. Using the socioecological model, we therefore seek to explore how partner alcohol use and attitudes toward IPVAW act independently and jointly at the individual and community level to influence IPVAW across LMICs (Figure 1). Established theoretical frameworks acknowledge that multiple factors interact across the social ecology to confer risk for experiencing IPVAW. As articulated by Heise (1998, 2011), a woman’s characteristics interact with the characteristics of her male partner, relationship, community, and macrosocial context to increase risk for IPVAW. Research investigating potential synergies at different ecological levels is emerging, yet we are unaware of any epidemiological investigations of these two important risk factors, across ecological levels. Understanding the independent and synergistic roles of alcohol use and attitudes toward IPVAW in context is essential to improving IPVAW prevention and response efforts globally.
Figure 1.
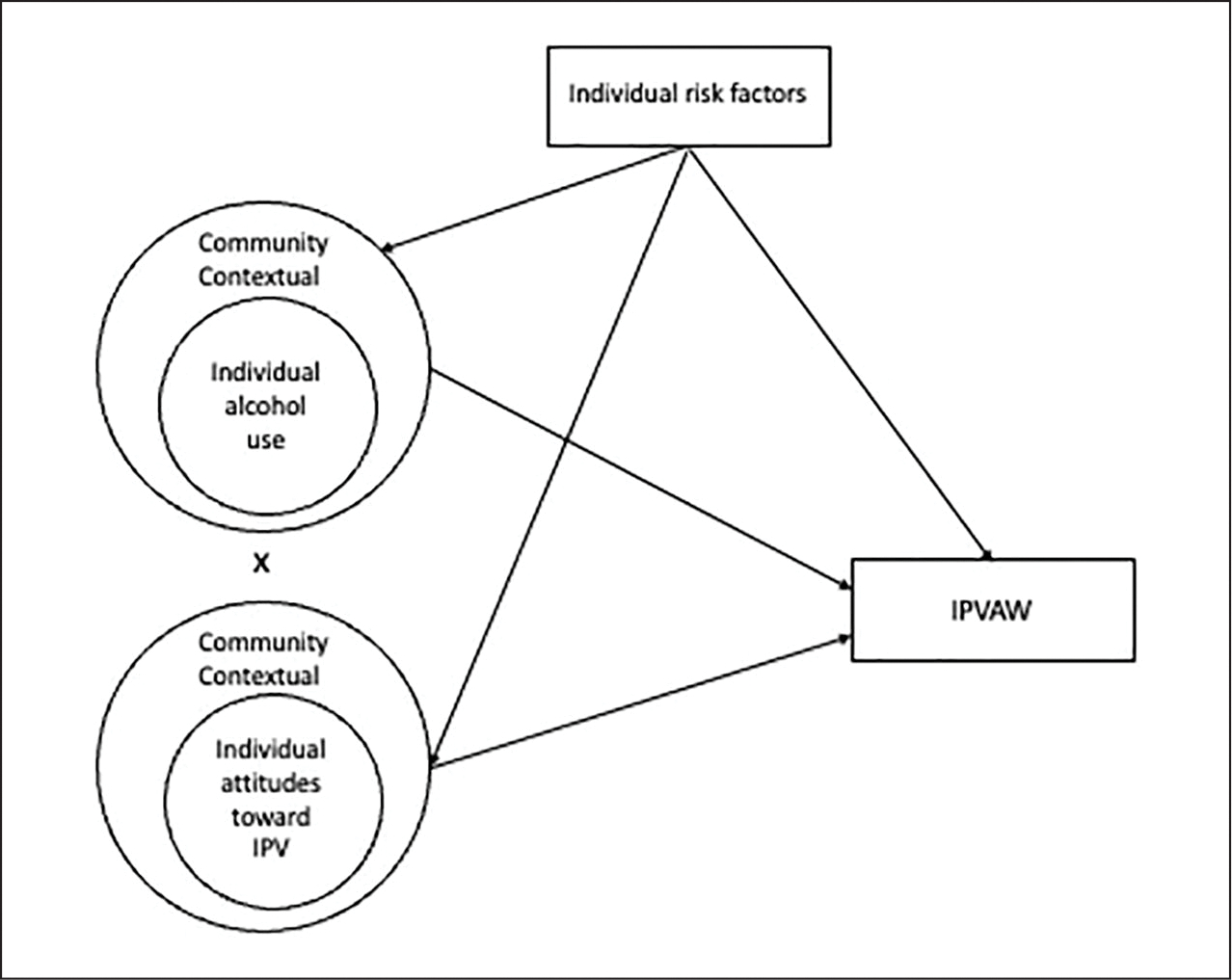
Model of relationships among partner alcohol use, attitudes toward IPVAW, and IPVAW.
Note. IPVAW = intimate partner violence against women.
Method
Participants and Procedures
Data for this study come from the Demographic and Health Surveys (DHSs), which are publicly available nationally representative surveys conducted in LMICs (The DHS Program, 2017). In each country, 5,000 to 30,000 households were selected using a probability sample from a census frame or complete list of villages/communities (ICF International, 2012). The target population was women aged 15 to 49 years old and children under the age of five. Interviewers were sex-matched, fluent in the local language, typically had a secondary education, and underwent intensive training and supervision (ICF International, 2012).
This analysis was restricted to women (defined by self-reported sex) who reported being currently married or partnered and who completed the domestic violence module. Domestic violence questions were administered privately to one randomly selected ever-partnered woman in every second sampled household (ICF International, 2012). We included data from 166,621 women living 19 countries that collected data about IPVAW, partner alcohol use, and attitudes toward IPVAW between 2010 and 2017.
Measures
The outcome in this study, past-year IPVAW victimization, was assessed using a modified version of the Conflict Tactics Scale, which has shown good internal consistency across psychological (α = 0.79), physical (α = 0.86), and sexual (α = 0.87) IPVAW subscales in high-income countries (Straus et al., 1996). In this survey, women were asked to report whether they experienced specific types of IPV in their lifetime and in the past 12 months. Psychological IPVAW included being humiliated, insulted, or threatened by her partner. Physical IPVAW included being slapped, pushed, shaken, having something thrown at her, having her hair pulled, having her arm twisted, being kicked, dragged, beat up, choked, burned, or threatened/attacked with a weapon by her partner. Sexual IPVAW included having been forced by her partner to have sex or perform another sexual act when it was not wanted. In this analysis, we defined IPVAW as any psychological, physical, or sexual IPVAW victimization occurring within the last 12 months.
Partner alcohol use, one of the primary exposures of interest, was assessed by asking the woman whether her male partner drinks alcohol (yes/no). The other primary exposure of interest, acceptance of IPVAW, was a dichotomous indicator generated as the endorsement by the respondent of one or more of the attitudes toward IPVAW indicators. These indicators asked whether a husband is justified in hitting or beating his wife if the woman: (a) argues with him, (b) burns food, (c) goes out without telling him, or (d) neglects the children. At the individual-level, both partner alcohol use and attitudes toward IPVAW were dichotomous indicators (yes/no). We also constructed community-level variables for the prevalence of male partner alcohol use and prevalence of endorsing one or more acceptance of IPVAW indicators. The community-level was defined based on the primary sampling unit, which are groups of households defined by census enumeration areas, electoral zones, or villages (ICF International, 2012). We scaled the community-level variables by multiplying each prevalence estimate by 10. Each unit increase, therefore, reflects a 10% increase in the community prevalence of partner alcohol use and acceptance of IPVAW.
Other variables included in the analysis as covariates included the woman’s age, education level, whether the head of household was female, wealth, and urbanicity. Among potential covariates documented in the literature, these were available in the DHSs. Age was a continuous variable. Education was measured by level: no education, primary education, secondary education, and higher education. Wealth was a composite relative wealth index based on assets, housing, water access, and sanitation facilities and categorized respondents into quintiles. Urbanicity was a dichotomous variable determined by whether the woman resided in a rural or urban setting.
Statistical Analysis
We estimated the distribution of the sociodemographic covariates, partner alcohol use, and acceptance of IPVAW by past-year IPV in the analytic sample. We then constructed a series of mixed-effect regression models with random intercepts for country and primary sampling unit. In each model, we estimated the independent effects of partner alcohol use and acceptance of IPVAW from which we then computed the joint effect of these two exposures. The joint effect was estimated using the linear combination of main effects and the interaction term at the individual and, separately, at the community level. For each model, we estimated the unadjusted model including only main effects and interaction terms for the individual- and/or community-level exposures of interest as well as an adjusted model controlling for age, education level, sex of the head of household, wealth, and urbanicity.
Model 1 estimated the total effect of partner alcohol use, acceptance of IPVAW, and their interaction on IPVAW victimization (Table 1). As parameter estimates in this model combine individual- (Level 1) and community-level (Level 2) effects, we estimated the within- and between-community effects in Model 2. We included the cluster-mean-centered individual-level effects of partner alcohol use, acceptance of IPVAW, and their interaction at the individual level (Level 1; within-community effect) and the prevalence of male partner alcohol use, the prevalence of acceptance of IPVAW, and their interaction at the community level (Level 2; between-community effect). The within-community effects estimate the association between individual differences and past-year individual odds of IPVAW within a given community and country. The between-community effects capture the association between community risk factor prevalence and past-year individual odds of IPVAW. Model 3 included partner alcohol use, acceptance of IPVAW, and their interaction and the prevalence of male partner alcohol use, the prevalence of acceptance of IPVAW, and their interaction at the community level (Level 2). Contextual effects were estimated from this model using the community-level (Level 2) coefficients. Results from this model effectively compare two women with similar partner alcohol use and attitudes accepting IPVAW, but who live in separate communities with a 10% difference in risk factor prevalence. Models 4a to 4d examined the within-community effect of partner alcohol use and acceptance of IPVAW stratified across the following types of communities:
Table 1.
Models of Past-Year IPVAW on Independent and Joint Effects of Partner Alcohol Use and Acceptance of IPVAW in 19 Low- and Middle-Income Countries (n = 166,621), 2010 to 2017.
| Total effect | Effect of partner alcohol use, acceptance of IPVAW, and their interaction on IPVAW (across individual and community levels) |
| Individual effect | Effect of individual partner alcohol use, acceptance of IPVAW, and their interaction on IPVAW within a given community |
| Community effect | Effect of community prevalence of partner alcohol use, acceptance of IPVAW, and their interaction on IPVAW |
| Contextual effect | Effectively compares two women with similar partner alcohol use and attitudes accepting IPVAW, but who live in separate communities with a 10% difference in risk factor prevalence |
Note. IPVAW = intimate partner violence against women.
communities with a low prevalence of partner alcohol use and low justification of IPVAW,
communities with a low prevalence of partner alcohol use and a high prevalence of favorable attitudes toward IPVAW,
communities with a high prevalence of partner alcohol use and a low prevalence of justification of IPVAW, and
communities with a high prevalence of partner alcohol use and strong endorsement of IPVAW.
Communities were classified as low versus high by whether they were below versus equal to or above the median prevalence of these exposures across the communities included in this analysis (median prevalence of partner alcohol use = 25%; median prevalence of attitudes accepting of IPVAW = 40%). Within each of these community types, we estimated the cluster-mean-centered individual-level effects of partner alcohol use, acceptance of IPVAW, and their interaction. These models investigate whether the association between individual risk factors and IPVAW differ based on community characteristics.
Results
We included data from 166,621 women living in the 19 countries that collected data about IPVAW, partner alcohol use, and attitudes toward IPVAW. The countries included in the analysis were Afghanistan (n = 17,573), Angola (n = 6,498), Myanmar (n = 2,877), Burundi (n = 6,391), Democratic Republic of the Congo (n = 4,898), Ethiopia (n = 4,102), India (n = 61,795), Kenya (n = 3,712), Malawi (n = 4,593), Mali (n = 2,930), Mozambique (n = 4,616), Namibia (n = 1,220), Nepal (n = 3,698), Nigeria (n = 20,224), Rwanda (n = 1,601), Senegal (n = 2,486), Zimbabwe (n = 4,867), Egypt (n = 6,186), and Tanzania (n = 6,354).
Table 2 shows proportions and univariable associations for the pooled sample. Of the 166,621 women included in the analysis, the average age was 31.7 years. The majority had primary school education or less (62.6%), resided in male-headed households (87.1%), and lived in rural settings (68.4%). More than one quarter (27.9%) reported partner alcohol use. Regarding attitudes toward IPVAW, nearly half (45.8%) endorsed IPVAW as justified for at least one specified reason. In simple logistic regression models, the odds of past-year IPVAW was slightly lower among women with increasing age, education, and wealth. Having a female head of household and urban residence also were associated with lower odds of IPVAW. By contrast, partner alcohol use was associated with a 2.3-fold higher odds of past-year IPVAW (odds ratio [OR] = 2.29; 95% confidence interval [CI]: [2.24, 2.34]), and any attitudes accepting of IPVAW was associated with a 2.2-fold higher odds of past-year IPVAW (OR = 2.19; 95% CI: [2.14, 2.24]).
Table 2.
Descriptive Statistics and Univariable Logistic Regression Models for Past-Year IPVAW in 19 Low- and Middle-Income Countries (n = 166,621), 2010 to 2017.
| Sample Proportions |
Univariable
Analysis |
|||
|---|---|---|---|---|
|
n = 166,621 % (n) |
No Past-Year
IPVAW n = 119,077 %(n) |
Past-Year IPVAW n = 47,544 %(n) |
Odds Ratio [95% CI]a |
|
|
| ||||
| Woman’s age, M (SD) | 31.71 (8.24) | 31.82 (8.32) | 31.41 (8.03) | 0.994 [0.993, 0.995] |
| Woman’s education | ||||
| No education | 38.43 (64,039) | 36.05 (42,930) | 44.40 (21,109) | ref. |
| Primary education | 24.18 (40,287) | 22.97 (27,356) | 27.20 (12,931) | 0.96 [0.94, 0.99] |
| Secondary education | 30.75 (51,229) | 32.90 (39,180) | 25.34 (12,049) | 0.63 [0.61, 0.64] |
| Higher education | 6.64 (11,066) | 8.07 (9,611) | 3.06 (1,455) | 0.31 [0.29, 0.33] |
| Female head of household | 12.86 (21,426) | 13.33 (15,869) | 11.69 (5,557) | 0.86 [0.83, 0.89] |
| Relative wealth index | ||||
| Poorest | 20.22 (33,698) | 18.98 (22,601) | 23.34 (11,097) | ref. |
| Poorer | 20.94 (34,890) | 20.18 (24,034) | 22.83 (10,856) | 0.92 [0.89, 0.95] |
| Middle | 20.23 (33,715) | 19.83 (23,614) | 21.25 (10,101) | 0.87 [0.84, 0.90] |
| Richer | 19.83 (33,045) | 20.21 (24,063) | 18.89 (8,982) | 0.76 [0.74, 0.79] |
| Richest | 18.77 (31,273) | 20.80 (24,765) | 13.69 (6,508) | 0.54 [0.52, 0.55] |
| Urban residence | 31.61 (52,661) | 32.99 (39,288) | 28.13 (13,373) | 0.79 [0.78, 0.81] |
| Partner alcohol use | 27.92 (46,526) | 22.90 (27,273) | 40.50 (19,253) | 2.29 [2.24, 2.34] |
| Any acceptance of IPVAW | 45.76 (76,248) | 40.24 (47,911) | 59.60 (28,337) | 2.19 [2.14, 2.24] |
Note. IPVAW = intimate partner violence against women; CI = confidence interval.
Odds ratios from univariable logistic regression models on past-year IPVAW.
Mixed-effects regression models, with random intercepts for community and country, are summarized in Table 3 and Figure 2. Model 1 captured the main effects of partner alcohol use, attitudes accepting of IPVAW, and their multiplicative interaction for past-year IPVAW. The adjusted model shows deleterious associations for partner alcohol use (OR = 3.20; 95% CI: [3.07, 3.33]), acceptance of IPVAW (OR = 1.83; 95% CI: [1.76, 1.89]), and the combination (OR = 5.65; 95% CI: [5.41, 5.90]). These results suggest that partner alcohol use and attitudes have sub-multiplicative effects on IPVAW (i.e., the combined effects are less than if the individual effects were multiplied together). However, the ability to interpret these associations is limited in this model because the effects of individual- and community-level risk factors are mixed.
Table 3.
Mixed-Effect Logistic Regression Models of Past-Year IPVAW on Independent and Joint Effects of Partner Alcohol Use and Acceptance of IPVAW in 19 Low- and Middle-Income Countries (n = 166,621), 2010 to 2019.
| Partner Alcohol Use | Acceptance of IPVAW | Unadjusted OR [95% CI] |
Adjustedd OR [95% CI] |
|
|---|---|---|---|---|
|
| ||||
| Model 1: Total effects | ||||
| Reference | No alcohol use | No acceptance | ref | ref |
| Partner alcohol usea | No alcohol use | Any acceptance | 3.27 [3.14, 3.41] | 3.20 [3.07, 3.33] |
| Justification of IPVAWa | Any alcohol use | No acceptance | 1.94 [1.87, 2.01] | 1.83 [1.76, 1.89] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 0.97 [0.91, 1.02] | 0.97 [0.91, 1.02] |
| Joint effect c | Any alcohol use | Any acceptance | 6.12 [5.86, 6.39] | 5.65 [5.41, 5.90] |
| Model 2: Within- and between-community effects | ||||
| Within-community effects | ||||
| Reference | Community-mean alcohol use | Community-mean acceptance | ref | ref |
| Partner alcohol usea | Community-mean alcohol use | Higher vs. lower acceptance | 3.06 [2.96, 3.17] | 2.98 [2.88, 3.08] |
| Justification of IPVAWa | Higher vs. lower alcohol use | Community-mean acceptance | 1.66 [1.61, 1.71] | 1.60 [1.55, 1.65] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 0.87 [0.80, 0.94] | 0.86 [0.79, 0.94] |
| Joint effect c | Higher vs. lower alcohol use | Higher vs. lower acceptance | 4.40 [4.02, 4.83] | 4.1 1 [3.75, 4.50] |
| Between-community effects | ||||
| Partner alcohol usea | No community alcohol use | 10% increase in community acceptance | 1.15 [1.13, 1.16] | 1.15 [1.13, 1.16] |
| Justification of IPVAWa | 10% increase in community alcohol use | No community acceptance | 1.14 [1.12, 1.15] | 1.12 [l.l 1, 1.13] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 1.002 [0.99988, 1.004] | 1.002 [1.0002, 1.005] |
| Joint effect c | 10% increase in community alcohol use | 10% increase in community acceptance | 1.31 [1.28, 1.33] | 1.29 [1.26, 1.31] |
| Model 3: Contextual effects | ||||
| Reference | No community alcohol use | No community acceptance | ref | ref |
| Contextual effect of partner alcohol usea | No community alcohol use | 10% increase in community acceptance | 1.02 [1.01, 1.04] | 1.03 [1.01, 1.04] |
| Contextual effect of justification of IPVAWa | 10% increase in community alcohol use | No community acceptance | 1.08 [1.07, 1.09] | 1.07 [1.06, 1.08] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 1.003 [1.0005, 1.005] | 1.003 [1.0007, 1.005] |
| Joint effect c | 10% increase in community alcohol use | 10% increase in community acceptance | 1.11 [1.08, 1.13] | 1.10 [1.08, 1.12] |
| STRATIFIED MODELS | ||||
| Model 4a: Within-community effects in communities with lower partner alcohol use and lower IPVAW acceptance | ||||
| Reference | Community-mean alcohol use | Community-mean acceptance | ref | ref |
| Partner alcohol usea | Community-mean alcohol use | Higher vs. lower acceptance | 4.37 [3.91, 4.89] | 4.29 [3.83, 4.80] |
| Justification of IPVAWa | Higher vs. lower alcohol use | Community-mean acceptance | 1.73 [1.59, 1.89] | 1.65 [1.52, 1.80] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 0.70 [0.52, 0.96] | 0.72 [0.53, 0.98] |
| Joint effect c | Higher vs. lower alcohol use | Higher vs. lower acceptance | 5.32 [3.86, 7.32] | 5.10 [3.70, 7.03] |
| Model 4b: Within-community effects in communities with lower partner alcohol use and higher IPVAW acceptance | ||||
| Reference | Community-mean alcohol use | Community-mean acceptance | ref | ref |
| Partner alcohol usea | Community-mean alcohol use | Higher vs. lower acceptance | 3.94 [3.52, 4.41] | 3.84 [3.43, 4.30] |
| Justification of IPVAWa | Higher vs. lower alcohol use | Community-mean acceptance | 1.57 [1.49, 1.67] | 1.52 [1.44, 1.61] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 0.996 [0.76, 1.30] | 0.98 [0.75, 1.29] |
| Joint effect c | Higher vs. lower alcohol use | Higher vs. lower acceptance | 6.17 [4.62, 8.24] | 5.75 [4.31, 7.68] |
| Model 4c: Within-community effects in communities with higher partner alcohol use and lower IPVAW acceptance | ||||
| Reference | Community-mean alcohol use | Community-mean acceptance | ref | ref |
| Partner alcohol usea | Community-mean alcohol use | Higher vs. lower acceptance | 2.78 [2.63, 2.93] | 2.68 [2.54, 2.83] |
| Justification of IPVAWa | Higher vs. lower alcohol use | Community-mean acceptance | 1.73 [1.62, 1.85] | 1.64 [1.53, 1.76] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 0.83 [0.72, 0.97] | 0.83 [0.71, 0.96] |
| Joint effect c | Higher vs. lower alcohol use | Higher vs. lower acceptance | 4.01 [3.42, 4.70] | 3.62 [3.09, 4.25] |
| Model 4d: Within-community effects in communities with higher partner alcohol use and higher IPVAW acceptance | ||||
| Reference | Community-mean alcohol use | Community-mean acceptance | ref | ref |
| Partner alcohol usea | Community-mean alcohol use | Higher vs. lower acceptance | 2.82 [2.68, 2.96] | 2.72 [2.59, 2.86] |
| Justification of IPVAWa | Higher vs. lower alcohol use | Community-mean acceptance | 1.67 [1.58, 1.76] | 1.59 [1.51, 1.68] |
| Partner Alcohol Use × Justification of IPVAWb | — | — | 0.87 [0.77, 0.98] | 0.87 [0.77, 0.98] |
| Joint effect c | Higher vs. lower alcohol use | Higher vs. lower acceptance | 4.08 [3.58, 4.65] | 3.77 [3.31, 4.30] |
Note. IPVAW = intimate partner violence against women; CI = confidence interval.
Main effect of partner alcohol use/acceptance of IPVAW (i.e., independent effect).
Interaction between partner alcohol use and attitudes toward IPVAW.
Joint effect represents the linear combination of partner alcohol use (main effect), acceptance of IPVAW (main effect), and their multiplicative interaction.
Models adjusted for woman’s age, woman’s education, sex of the household head, relative wealth index, and urban vs. rural residence.
Figure 2.
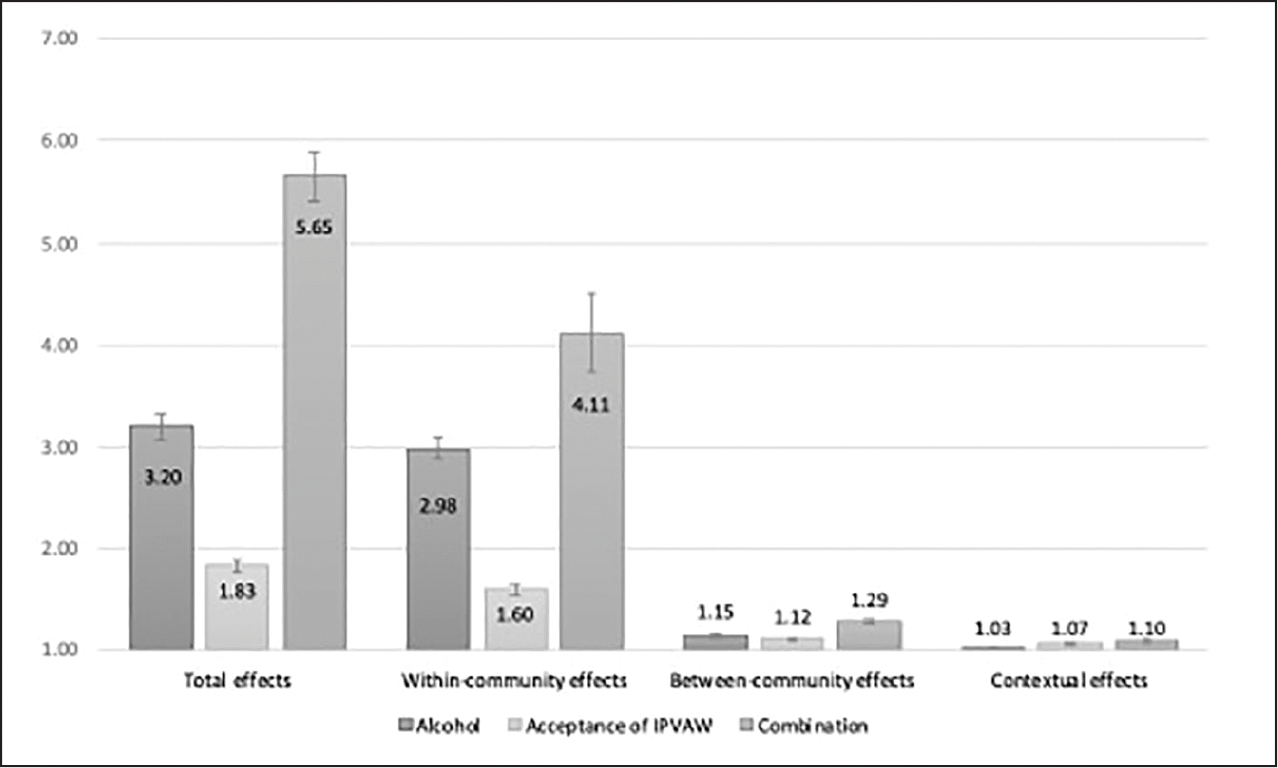
Odds ratios from mixed-effect logistic regression models of past-year IPVAW on partner alcohol use and acceptance of IPVAW (n = 166,621; Models 1–3).
Note. IPVAW = intimate partner violence against women.
To disentangle these associations, Model 2 separated the total effects into within-community and between-community effects. The within-community effects estimate the association between individual differences and past-year IPVAW within a given community. Among women with attitudes at the community mean, those who report partner alcohol use have nearly 300% higher odds of IPVAW than women who do not report partner alcohol use (OR = 2.98; 95% CI: [2.88, 3.08]). Among women with partner alcohol use at the community mean, the corresponding increase in odds among women who agree versus do not agree with any reasons accepting of IPVAW is 60% (OR = 1.60; 95% CI: [1.55, 1.65]). The combination of risk factors operating together is associated with higher odds than either individual exposure (OR = 4.11; 95% CI: [3.75, 4.50]) but lower odds than if they combined multiplicatively (ratio of OR = 0.86; 95% CI: [0.79, 0.94]).
The between-community effects capture the association between community risk factor prevalence and past-year IPVAW. Among communities where women do not report attitudes justifying IPVAW, each 10% increase in the community prevalence of partner alcohol use is associated with a 15% increase in the odds of IPVAW (OR = 1.15; 95% CI: [1.13, 1.16]). The same 10% increase in community acceptance of violence is associated with a 12% increase in the odds of IPVAW (OR = 1.12; 95% CI: [1.11, 1.13]). At the community level, this combination of risk factors is associated with excess odds of IPVAW. Each combined 10% increase in the prevalence of alcohol use and accepting attitudes is associated with a 29% increase in IPVAW odds (OR 1.29; 95% CI: [1.26, 1.31]): a small increase above what the independent effects predict (ratio of OR = 1.002; 95% CI: [1.0002, 1.005]) suggesting a synergistic interaction.
Contextual effects in Model 3 estimated the effect of community risk factors among women with comparable individual risk factors. Results effectively compare two women who report similar individual attitudes accepting of IPVAW and partner alcohol use, but who live in separate communities with a 10% difference in risk factor prevalence. In the case where the prevalence of attitudes is the same, but partner alcohol use differs, the woman from the community with a 10% higher prevalence of partner alcohol use has 3% greater odds of IPV (OR = 1.03; 95% CI: [1.01, 1.04]). Where the communities have equal prevalence of partner alcohol use, but acceptance of IPVAW differs, the woman from the community with a higher prevalence of women who accept IPVAW has 7% greater odds of IPVAW (OR = 1.07; 95% CI: [1.06, 1.08]). Again, the combination of alcohol use and attitudes is associated with a small excess odds of IPV (ratio of OR = 1.003; 95% CI: [1.0007, 1.005]).
Model 4a to 4d explored potential cross-level interactions through stratification by community characteristics (Table 3, Figure 3). Variations in effect estimates across 4a to 4d suggest that the association between individual risk factors and IPVAW differ based on community characteristics. These models reveal that the odds of IPVAW associated with partner alcohol use is greater in communities with lower partner alcohol prevalence (lower acceptance of IPVAW: OR = 4.29; 95% CI: [3.83, 4.80]; higher acceptance of IPVAW: OR = 3.84; 95% CI: [3.43, 4.30]) and lower acceptance of IPVAW (lower alcohol: OR = 1.65; 95% CI: [1.52, 1.80]; higher alcohol: OR = 1.64; 95% CI: [1.53, 1.76]). When both individual risk factors are present, there is a sub-multiplicative interaction in communities with lower alcohol-lower acceptance (ratio of OR = 0.72; 95% CI: [0.53, 0.98]), higher alcohol-lower acceptance (ratio of OR = 0.83; 95% CI: [0.71, 0.96]), and higher alcohol-higher acceptance (ratio or OR = 0.87; 95% CI: [0.77, 0.98]).
Figure 3.
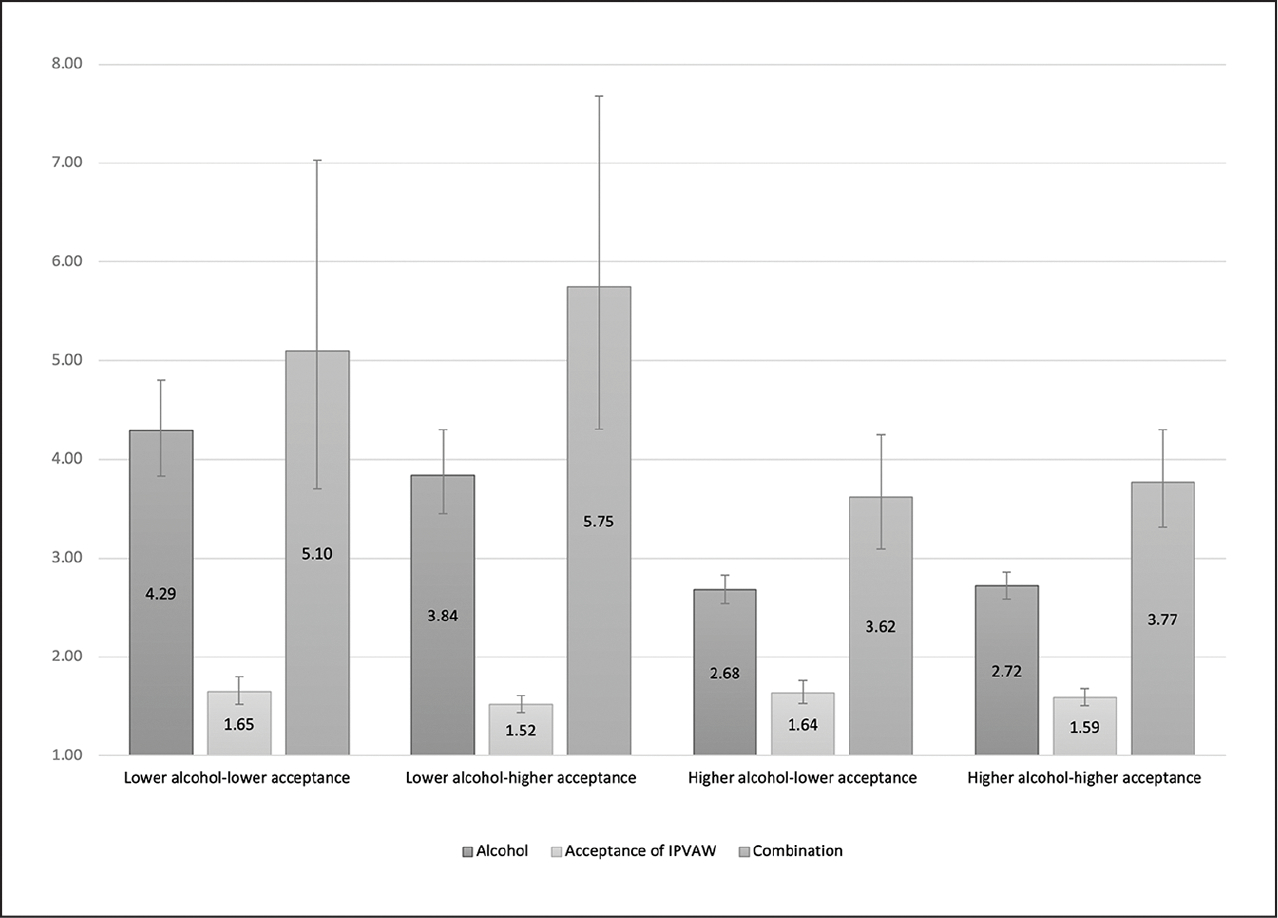
Odds ratios from mixed-effect logistic regression models of past-year IPVAW on partner alcohol use and acceptance of IPVAW, stratified by community alcohol and acceptance of IPVAW (n = 166,621; Models 4a–4d).
Note. IPVAW = intimate partner violence against women.
Discussion
In this analysis, we sought to jointly analyze two well-known risk factors for IPVAW: partner alcohol use and attitudes toward IPVAW (Coll et al., 2021). We aimed to examine these risk factors’ independent and joint influence on IPVAW across levels of the social ecology.
Our results suggest that, firstly, partner alcohol use and attitudes toward IPVAW are strongly associated with IPVAW at the individual, community, and contextual levels—both independently and in combination. At the individual and community levels, both were associated with large independent effects, yet the OR for the impact of alcohol use on IPVAW was more than 1.5 times greater than the OR for acceptance of IPVAW in adjusted models. Given their similar ORs in univariable analyses, multiple explanations are possible. For example, alcohol use may be a more proximal risk factor, therefore explaining more variance (Crane et al., 2016). A more complex explanation may be that attitudes toward IPVAW mediate the association between partner alcohol use and IPVAW (i.e., partner alcohol use may fuel the manifestation of male justificatory attitudes that mirror respondents’ attitudes, resulting in IPVAW). Finally, alcohol use may serve as closer proxy variable than IPVAW attitudes for a construct that is shared with IPVAW (e.g., masculinity norms that encourage both drinking and IPVAW, broader demoralization, or level of social vulnerability), thereby explaining the stronger relation with IPVAW. The latter explanation may align with findings about the interaction between reporting partner alcohol use and justificatory attitudes toward IPVAW. At the individual level, the combination was associated with lower odds of IPVAW than what would be expected if the results combined multiplicatively or synergistically. However, the combination of risk factors contrastingly resulted in a small excess odds of IPVAW at both the community and contextual levels. This underscores the potential for complex interactions that vary across the social ecology.
In the stratified analyses, we found that the association between partner alcohol use and IPVAW was largest in communities where the prevalence of alcohol use among male partners is low. This suggests that in contexts where drinking is less normative, alcohol use may confer stronger alcohol related IPVAW risk, a finding that is consistent with prior research (Bye & Rossow, 2008; Coleman & Straus, 1983; Greene et al., 2021). This contrasted with the association between acceptance of IPVAW and IPVAW, which remained relatively consistent across varied levels of community attitudes and alcohol use prevalence. Therefore, acceptance of IPVAW within communities appears to be similarly associated with risk of IPVAW regardless of community norms or alcohol use prevalence. In contrast, partner alcohol use may be a particularly salient risk factor for IPVAW in communities where alcohol use is less normative.
Our results have important implications for practice and policy. First, the emergent focus on gender norms for IPVAW intervention, while important, may neglect a critical correlate of IPVAW with a large magnitude of association. There is need for interdisciplinary conversations that bring mental health/substance use researchers into conversation with feminist scholars focusing on norms surrounding acceptance of IPVAW. These findings reveal that it is important to consider norms and attitudes alongside alcohol use when understanding epidemiological patterns of IPVAW and potential opportunities for preventive programs and policymaking. Further research unpacking the joint effects between alcohol use and attitudes toward IPVAW (e.g., whether they share an underlying trait, such as masculinity norms) could further guide the choice of preventive interventions. Another important consideration for policy and practice that emerged from this study relates to the relatively consistent association between individual-level acceptance of IPVAW across communities with varying community attitudes toward IPVAW or alcohol use prevalence. Further research on how individual-level attitudes toward IPVAW are shaped, including the role of community norms, is needed to identify whether focusing on altering community norms is the most efficient way to mitigate the proximal effect of individual acceptance of IPVAW. To the extent that these questions measure a combination of personal attitudes and community norms (Schuler & Islam, 2008), it is possible that couples- and individual-level preventive interventions focused on attitudes toward IPVAW are needed to complement community-level interventions to reduce risk of IPVAW.
These results should be evaluated considering several limitations. Among these, we utilized cross-sectional data, which precludes the ability to make causal inferences. Partner alcohol use was measured imprecisely, as no recall period or severity level was specified. This may introduce temporal biases and recall bias, if women who experience IPV are differentially likely to report partner alcohol use. It is also possible that recall bias may be greater in communities where alcohol use is less normative, thus introducing bias into the stratified analyses. Moreover, attitudes toward IPVAW were measured by self-report; they may be underreported or overreported due to social desirability bias. There may be potential endogeneity between acceptance of IPVAW and IPVAW, such that accepting attitudes emerge as a coping mechanism or response to experienced violence. For these reasons, we conservatively interpret our findings as associations, although we recognize both partner alcohol use (Choenni et al., 2017) and acceptance of IPVAW (Raj et al., 2018) are established risk factors, also found in longitudinal studies. Additionally, we developed a composite measure of IPVAW inclusive of any past-year psychological, physical, and/or sexual violence. Some scholars now advocate that only high-intensity psychological violence be included (Heise et al., 2019). In this analysis, we retain any psychological violence to remain consistent with the extant literature on partner alcohol use and attitudes toward IPVAW.
We also acknowledge several limitations related to how we have framed this work. First, we acknowledge that this work is more salient to LMICs. This focus was selected given the preponderance of evidence historically has been generated in high-income countries. Within LMICs, however, we have grouped diverse countries. This is both a strength, to the extent that the data are more generalizable, and limitation, to the extent that we have not captured the unique cultures and sub-cultures present within these countries. We recognize that the etiology of IPVAW is complex, and its presence or absence is related both to the risk factors on which we have focused this work and risk and protective factors across the social ecology, which include the unique strengths of diverse communities and cultures. Similarly, we acknowledge that this work focuses on male perpetrated IPVAW, drawing on an historical literature that largely presupposes cisgender status and heterosexual relationships (Henry et al., 2021). Although it is critical to grow our understanding of male perpetrated IPVAW, building theory and empirical findings that advance understanding of IPV in transgender/gender nonconforming persons and diverse relationships likewise is essential, especially in LMIC contexts.
In summary, these analyses revealed the importance of evaluating risk factors for IPVAW in context. First, risk factors for IPVAW should be considered together to understand their interconnected roles in conferring risk for IPVAW. Second, individual-level risk factors must also be considered within the community context. Understanding community norms and how they modify individual-level risk factors for IPVAW, as was the case for alcohol use in this study, can inform tailored preventive intervention approaches. Third, focusing on gender norms alone may be insufficient to effectively reduce the risk of IPVAW for women in LMICs. Alcohol use and acceptance of IPVAW were consistently associated with increased odds of IPV. We identified notable and nuanced interactions between individual- and community-level risk factors for IPVAW as well as moderation of the association between risk factors and IPVAW based on community-level characteristics. Future studies should focus on the complex interactions, at multiple social levels, between interacting risk factors for IPVAW—to pave the way for the design of optimally effective IPVAW-focused interventions that have the smallest risk of doing harm.
Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article:
Christine Bourey was supported by training grant T32MH103210 from the National Institute of Mental Health.
Biographies
Christine Bourey, MPH, MSN, is a psychiatric nurse practitioner, certified nurse midwife, and doctoral candidate at the Johns Hopkins Bloomberg School of Public Health, Department of Mental Health. Her research focuses on mental health and well-being in the context of intimate partner and collective violence.
Lori Heise, PhD, is the Founder and Technical Director of the Prevention Collaborative, a global organization dedicated to reducing violence against women and children, using research-based evidence, practice-based knowledge, and feminist principles. She previously served as a Professor of Social Epidemiology at the Johns Hopkins Bloomberg School of Public Health and the London School of Hygiene and Tropical Medicine.
Wietse Tol, PhD, is Professor of Global Mental Health at the Section of Global Health, Department of Public Health at the University of Copenhagen; Extraordinary Professor of Global Mental Health and Social Justice at the Athena Institute, Vrije Universiteit Amsterdam; Adjunct Professor at the Department of Mental Health, Johns Hopkins Bloomberg School of Public Health and Senior Advisor at HealthRight International.
M. Claire Greene, PhD MPH, is an Assistant Professor in the Program on Forced Migration and Health at the Columbia University Mailman School of Public Health. Her research focuses on improving the effectiveness and implementation of interventions to improve mental health and reduce substance use-related harm among displaced populations in humanitarian settings.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
References
- Abbey A, Wegner R, Woerner J, Pegram SE, & Pierce J (2014). Review of survey and experimental research that examines the relationship between alcohol consumption and men’s sexual aggression perpetration. Trauma, Violence, & Abuse, 15(4), 265–282. 10.1177/1524838014521031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacchus LJ, Ranganathan M, Watts C, & Devries K (2018). Recent intimate partner violence against women and health: A systematic review and meta-analysis of cohort studies. BMJ Open, 8, 1–20. 10.1136/bmjopen-2017-019995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bye EK, & Rossow I (2008). Is the impact of alcohol consumption on violence relative to the level of consumption?. Journal of Scandinavian Studies in Criminology and Crime Prevention, 9(1), 31–46. 10.1080/14043850801896729 [DOI] [Google Scholar]
- Caldwell JE, Swan SC, & Woodbrown VD (2012). Gender differences in intimate partner violence outcomes. Psychology of Violence, 2(1), 42–57. 10.1037/a0026296 [DOI] [Google Scholar]
- Choenni V, Hammink A, & van de Mheen D (2017). Association between substance use and the perpetration of family violence in industrialized countries: A systematic review. Trauma, Violence, & Abuse, 18(1), 37–50. 10.1177/1524838015589253 [DOI] [PubMed] [Google Scholar]
- Coleman DH, & Straus MA (1983). Alcohol abuse and family violence. In Gottheil E, Druley KA, Skoloda TE, & Waxman HM (Eds.), Alcohol, Drug Abuse, and Aggression (pp. 104–124). Charles C. Thomas. [Google Scholar]
- Coll CVN, Santos TM, Devries KM, Knual F, Bustreo F, Gatuguta A, Houvessou GM, & Barros AJD (2021). Identifying the women most vulnerable to intimate partner violence: A decision tree analysis from 48 low and middle-income countries. EClinicalMedicine, 42, 1–10. 10.1016/j.eclinm.2021.101214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane CA, Godleski SA, Przybyla SM, Schlauch RC, & Testa M (2016). The proximal effects of acute alcohol consumption on male-to-female aggression: A meta-analytic review of the experimental literature. Trauma, Violence, & Abuse, 17(5), 520–531. 10.1177/1524838015584374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durevall D, & Lindskog A (2015). Intimate partner violence and HIV in ten sub-Saharan African countries: What do the Demographic and Health Surveys tell us? Lancet Global Health, 3(1), e34–43. 10.1016/S2214-109X(14)70343-2 [DOI] [PubMed] [Google Scholar]
- Ellsberg M, Arango DJ, Morton M, Gennari F, Kiplesund S, Contreras M, & Watts C (2015). Prevention of violence against women and girls: What does the evidence say?. Lancet, 385(9977), 1555–1566. 10.1016/S0140-6736(14)61703-7 [DOI] [PubMed] [Google Scholar]
- Ezard N (2014). It’s not just the alcohol: Gender, alcohol use, and intimate partner violence in Mae La refugee camp, Thailand, 2009. Substance Use & Misuse, 49(6), 684–693. 10.3109/10826084.2013.863343 [DOI] [PubMed] [Google Scholar]
- Flood M, & Pease B (2009). Factors influencing attitudes to violence against women. Trauma, Violence, & Abuse, 10(2), 125–142. 10.1177/1524838009334131 [DOI] [PubMed] [Google Scholar]
- Foran HM, & O’Leary KD (2008). Alcohol and intimate partner violence: A meta-analytic review. Clinical Psychology Review, 28(7), 1222–1234. 10.1016/j.cpr.2008.05.001 [DOI] [PubMed] [Google Scholar]
- Gracia E, Rodriguez CM, Martín-Fernández M, & Lila M (2020). Acceptability of family violence: Underlying ties between intimate partner violence and child abuse. Journal of Interpersonal Violence, 35(17–18), 3217–3236. 10.1177/0886260517707310 [DOI] [PubMed] [Google Scholar]
- Greene MC, Heise L, Musci RJ, Wirtz AL, Johnson R, Leoutsakos J-M., Wainberg ML., & Tol WA. (2021). Improving estimation of the association between alcohol use and intimate partner violence in low-income and middle-income countries. Injury Prevention, 27(3), 2212–2226. 10.1136/injuryprev-2019-043433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene MC, Kane JC, & Tol WA (2017). Alcohol use and intimate partner violence among women and their partners in sub-Saharan Africa. Global Mental Health, 4, 1–11. 10.1017/gmh.2017.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heise L (2011). What works to prevent partner violence? An evidence overview. https://www.oecd.org/derec/49872444.pdf
- Heise LL (1998). Violence against women: An integrated, ecological framework. Violence Against Women, 4(3), 262–290. 10.1177/1077801298004003002 [DOI] [PubMed] [Google Scholar]
- Heise LL, & Kotsadam A (2015). Cross-national and multilevel correlates of partner violence: An analysis of data form population-based surveys. Lancet Global Health, 3(6), e332–340. 10.1016/S2214-109X(15)00013-3 [DOI] [PubMed] [Google Scholar]
- Heise L, Pallitto C, García-Moreno C, & Clark CJ (2019). Measuring psychological abuse by intimate partners: Constructing a cross-cultural indicator for the Sustainable Development Goals. SSM Population Health, 9, 1–6. 10.1016/j.ssmph.2019.100377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry RS, Perrin PB, Coston BM, & Calton JM (2021). Intimate partner violence and mental health among transgender/gender nonconforming adults. Journal of Interpersonal Violence, 36(7–8), 3374–3399. 10.1177/0886260518775148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrero J, Rodríguez FJ, & Torres A (2017). Acceptability of partner violence in 51 societies: The role of sexism and attitudes toward violence in social relationships. Violence Against Women, 23(3), 351–367. 10.1177/1077801216642870 [DOI] [PubMed] [Google Scholar]
- ICF International. (2012). Demographic and Health Survey sampling and household listing manual. ICF International. https://dhsprogram.com/pubs/pdf/DHSM4/DHS6_Sampling_Manual_Sept2012_DHSM4.pdf [Google Scholar]
- Jewkes R, Flood M, & Lang J (2015). From work with men and boys to changes of social norms and reduction of inequities in gender relations: A conceptual shift in prevention of violence against women and girls. Lancet, 385(9977), 1580–1590. 10.1016/S0140-6736(14)61683-4 [DOI] [PubMed] [Google Scholar]
- Kennedy AC, & Prock KA (2018). “I still feel like I am not normal:” A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma, Violence, & Abuse, 19(5), 512–527. 10.1177/1524838016673601 [DOI] [PubMed] [Google Scholar]
- Krug EG, Dahlberg LL, Mercy JA, Zwi AB, & Lozano R (2002). World report on violence and health. World Health Organization. [Google Scholar]
- Lawoko S (2008). Predictors of attitudes toward intimate partner violence: A comparative study of men in Zambia and Kenya. Journal of Interpersonal Violence, 23(8), 1056–1074. 10.1177/0886260507313972 [DOI] [PubMed] [Google Scholar]
- McCarthy KJ, Mehta R, & Haberland NA (2018). Gender, power, and violence: A systematic review of measures and their association with male perpetration of IPV. PloS One, 13(11), 1–27. 10.1371/journal.pone.0207091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTavish JR, MacGregor JCD, Wathen CN, & MacMillan HL (2016). Children’s exposure to intimate partner violence: An overview. International Review of Psychiatry, 28(5), 504–518. 10.1080/09540261.2016.1205001 [DOI] [PubMed] [Google Scholar]
- Pihl R, Hoaken P, Werkele C, & Wall A (2002). Biological bases to addiction and aggression in close relationships. In Brunner PA (Ed.), The violence and addiction equation: Theoretical and clinical issues in substance abuse and relationship violence. Mazel. [Google Scholar]
- Raj A, Silverman JG, Klugman J, Saggurti N, Donta B, & Shakya HB (2018). Longitudinal analysis of the impact of economic empowerment on risk for intimate partner violence among married women in rural Maharashtra, India. Social Science & Medicine, 196, 197–203. 10.1016/j.soc-scimed.2017.11.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardinha L, Maheu-Giroux M, Stöckl H, Meyer SR, & García-Moreno C (2022). Global, regional, and national prevalence estimates of physical or sexual, or both, intimate partner violence against women in 2018. The Lancet, 399(10327), 803–813. 10.1016/S0140-6736(21)02664-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler SR, & Islam F (2008). Women’s acceptance of intimate partner violence within marriage in rural Bangladesh. Studies in Family Planning, 39(1), 49–58. 10.1111/j.1728-4465.2008.00150.x [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2): Development and preliminary psycho metric data. Journal of Family Issues, 17, 283–316. 10.1177/019251396017003001 [DOI] [Google Scholar]
- The DHS Program. (2017). DHS overview The DHS Program. https://dhsprogram.com/methodology/survey-Types/dhs.cfm [Google Scholar]
- Tran TD, Nguyen H, & Fisher J (2016). Attitudes toward intimate partner violence against women among women and men in 39 low- and middle-income countries. PloS One, 11(11), 1–14. 10.1371/journal.pone.0167438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagman JA, Donta B, Ritter J, Naik DD, Nair S, Saggurti N, Raj A, & Silverman JG (2016). Husband’s alcohol use, intimate partner violence, and family maltreatment of low-income postpartum women in Mumbai, India. Journal of Interpersonal Violence, 33(14), 2241–2267. 10.1177/0886260515624235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber AM, Cislaghi B, Meausoone V, Abdalla S, Mejia-Guevara I, Loftus P, Hallgren E, SEff I, Stark L, Victoria CG, Buffarini R, Barros AJD, Domingue BW, Bhushan D, Gupta R, Nagata JM, Shakya HB, Richter LM, Norris SA, . . .Gupta GR. (2019). Gender norms and health: Insights from global survey data. The Lancet, 393(10189), 2455–2468. 10.1016/S0140-6736(19)30765-2 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2022). Intimate partner violence. World Health Organization. https://apps.who.int/violence-info/intimate-partner-violence/ [Google Scholar]


