Graphical Abstract
Graphical Abstract.
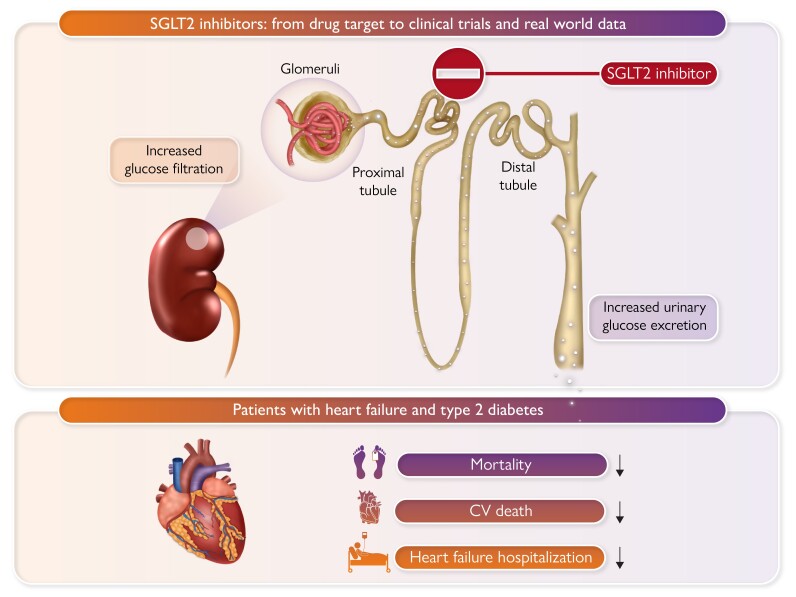
Effect of SGLT2 inhibitors in patients with heart failure and type 2 diabetes. CV, cardiovascular; HF, heart failure.
This editorial refers to ‘Sodium–glucose cotransporter 2 inhibitors vs. sitagliptin in heart failure and type 2 diabetes: an observational cohort study’, by E.L. Fu et al., https://doi.org/10.1093/eurheartj/ehad273.
Randomized, placebo-controlled trials (RCTs) are the gold standard to assess efficacy and safety of a given treatment in cardiovascular medicine and the cornerstone of evidence-based guideline recommendations. In addition, RCTs have a low potential for bias and are usually required for regulatory approval. Still, these trials have limitations including selected patient populations, a defined and controlled treatment environment, specified duration of follow-up, as well as monitored and ‘supported’ adherence to medication.1 Therefore, RCTs may have a limited generalizability to wider populations. Meta-analyses of RCTs may overcome some of these limitations by integrating results from multiple individual studies with similar but different patient populations, thus ideally increasing the precision in estimating treatment effects and providing detailed analyses for subgroups and secondary endpoints.2 However, publication and search bias as well as the heterogeneity of results between individual studies may influence the treatment benefit seen. Still, one must go from treatment efficacy in a controlled study to analyses of effectiveness of treatment in routine clinical practice. Therefore, real-world data may complement and support the evidence from RCTs and allow the analysis of treatment effects in populations not represented in RCTs or in an uncontrolled clinical environment. In this respect, real-world evidence studies are confronted with potential confounders and often employ complex analysis methods such as propensity score matching to minimize bias. In addition, other limitations include immortal time bias as well as less restrictive inclusion criteria which may dilute the treatment effects seen in RCTs.3 Overall, each type of study has strengths and limitations, but the combination of RCTs, meta-analyses, and real-world data can provide the most comprehensive understanding of the clinical value of a given treatment in a broad group of patients. The available evidence for the treatment of patients with heart failure (HF) and type 2 diabetes must be seen in this light.
First data from a RCT with a sodium-dependent glucose co-transporter 2 (SGLT2) inhibitor on HF-related endpoint in patients with type 2 diabetes were published in 2015 when in the EMAP-REG Outcome trial empagliflozin showed significant reduction in the combined primary endpoint (3-MACE), and—somewhat unexpected—a highly significant early reduction of HF hospitalization (HHF) compared with placebo.4 This finding has been principally confirmed with other SGLT2 inhibitors in the diabetes cardiovascular outcome trials (CVOTs) DECLARE,5 CANVAS,6 and VERTIS-CV,7 and analysed in a meta-analysis.8 Based on these early data, dedicated trials in patients with HF with reduced ejection fraction (HFrEF) or preserved ejection fraction (HFpEF) with and without diabetes have been performed (EMPEROR-REDUCED, DAPA-HF, EMPEROR-PRESERVED, DELIVER, and SOLOIST-HF). The data from these trials have led to a paradigm shift, making SGLT2 inhibitors nowadays an integral part of the foundational therapy in HF patients independent of left ventricular ejection fraction. A recent meta-analysis of all five randomized, placebo-controlled HF trials with SGLT2 inhibitors showed a very robust 23% relative risk reduction of the combined endpoint of cardiovascular death and HHF in patients with diabetes, thus underscoring the effectiveness of these drugs on HF-related endpoints in patients with diabetes.9
How does this clinical trial evidence translate into effectiveness in routine clinical care?
In this issue of the European Heart Journal, Fu et al. report a study in which they evaluated the effect of SGLT2 inhibitors in patients with HF and type 2 diabetes in routine clinical practice using claims data.10 They enrolled 59 605 patients with HF and type 2 diabetes from Medicare claim data from April 2013 to December 2019. The study compared the effectiveness of SGLT2 inhibitors vs. the dipeptidyl peptidase-4 (DPP4) inhibitor sitagliptin (which has been shown to be non-inferior to placebo in the previously published TECOS trial11) and investigated differences between agents within the SGLT2 inhibitor class and for HFrEF or HFpEF. The analysis included 16 253 SGLT2 inhibitor initiators vs. 43 352 initiators of sitagliptin (adjusted for 100 confounders with propensity score rating), and the primary endpoint was a composite of all-cause mortality and worsening HF over a 365-day intention-to-treat follow-up. In this study, initiation of SGLT 2 inhibitors vs. sitagliptin was associated with a lower risk for the primary composite endpoint [hazard ratio (HR) 0.72; 95% confidence interval (CI) 0.67–0.77]. The adjusted relative risk reduction for all-cause mortality was 30% (HR 0.70; 95% CI 0.63–0.71), 36% for HF hospitalization (HR 0.64 95% CI 0.58–0.7), and 23% (HR 0.77 95% CI 0.69–0.86) for urgent visit requiring i.v. diuretics. No difference was seen between the three different agents within the SGLT2 inhibitor class (empagliflozin, dapagliflozin, or canagliflozin), nor for HF with reduced or preserved ejection fraction. Interestingly, the authors also found a significant reduction of HF hospitalization in SGLT2 inhibitor-treated patients as early as at day 5 of follow-up, a finding in line with the early benefit seen in the RCTs. Interestingly, the population was ∼10 years older than in the respective CVOTs. This new evidence is important since the prevalence of type 2 diabetes in individuals aged 70 years and above is > 20% and this population is underrepresented in most CVOTs.12
The authors should be congratulated for providing such a valuable real-world study on the effectiveness of SGLT2 inhibitors in patients with HF and type 2 diabetes. The data complement the results from RCTs and meta-analyses with comparable point estimates, e.g. for HF hospitalization, thus underscoring the robustness of the benefit of SGLT2 inhibitors in this high-risk population (Graphical Abstract). The real-world evidence study by Fu and colleagues thus provides additional strong confidence that patients with type 2 diabetes and HF—irrespective of the ejection fraction—should be treated with SGLT2 inhibitors to reduce HF-related endpoints.
In addition to this clinically highly relevant aspect, the authors deserve credit for conducting such a thoroughly planned real-world analysis which aimed to minimize the usual shortcomings of real-world data evidence. The design and the approach chosen by the authors in this analysis include very important aspects: the choice of a 365-day intention-to-treat follow-up rather than an indefinite follow-up accounts for the high discontinuation rate in clinical practice, which might bias potential beneficial effects towards the null. In addition, they adjusted for 100 covariants of clinical interests, e.g. vascular complications, comorbidities, and recent hospitalizations, and performed propensity score-based defined risk stratification to adjust for these confounders. Finally, they conducted three bias calibration analyses in which they leveraged two negative control outcomes and one positive control outcome to adjust the HRs for residual bias due to unmeasured confounding or measurement errors. This carefully conducted approach providing comparable HRs for HF-related endpoints as seen in RCTs and meta-analyses could act as a blueprint for future analyses of data from routine clinical care.
The present study provides another piece in completing the spectrum of data derived from RCTs, meta-analyses, registries,13 and now health claims data. Given the available totality of evidence for the beneficial effects of SGLT2 inhibitor treatment on HF-related endpoints in HF patients with type 2 diabetes, we should now aim to implement this therapy in clinical practice and overcome clinical inertia to reduce morbidity and mortality in this high-risk population.
Contributor Information
Nikolaus Marx, Department of Internal Medicine I, RWTH Aachen University Hospital, Pauwelsstraße 30, D-52074 Aachen, Germany.
Dirk Müller-Wieland, Department of Internal Medicine I, RWTH Aachen University Hospital, Pauwelsstraße 30, D-52074 Aachen, Germany.
Funding
This work is supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) TRR 219; Project-ID 322900939 (M03, M05).
Data availability
No new data were generated or analysed in support of this research.
References
- 1. Saturni S, Bellini F, Braido F, Paggiaro P, Sanduzzi A, Scichilone N, et al. Randomized controlled trials and real life studies. Approaches and methodologies: a clinical point of view. Pulm Pharmacol Ther 2014;27:129–138. 10.1016/j.pupt.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 2. Walker E, Hernandez AV, Kattan MW. Meta-analysis: its strengths and limitations. Cleve Clin J Med 2008;75:431–439. 10.3949/ccjm.75.6.431 [DOI] [PubMed] [Google Scholar]
- 3. Schilsky RL. Finding the evidence in real-world evidence: moving from data to information to knowledge. J Am Coll Surg 2017;224:1–7. 10.1016/j.jamcollsurg.2016.10.025 [DOI] [PubMed] [Google Scholar]
- 4. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–2128. 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 5. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019;380:347–357. 10.1056/NEJMoa1812389 [DOI] [PubMed] [Google Scholar]
- 6. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 2017;377:644–657. 10.1056/NEJMoa1611925 [DOI] [PubMed] [Google Scholar]
- 7. Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med 2020;383:1425–1435. 10.1056/NEJMoa2004967 [DOI] [PubMed] [Google Scholar]
- 8. McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, et al. Association of SGLT2 inhibitors with cardiovascular and kidney outcomes in patients with type 2 diabetes: a meta-analysis. JAMA Cardiol 2021;6:148–158. 10.1001/jamacardio.2020.4511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vaduganathan M, Docherty KF, Claggett BL, Jhund PS, de Boer RA, Hernandez AF, et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet 2022;400:757–767. 10.1016/S0140-6736(22)01429-5 [DOI] [PubMed] [Google Scholar]
- 10.Fu EL, Patorno E, Everett BM, Vaduganathan M, Solomon SD, Levin R, et al. Sodium–glucose cotransporter 2 inhibitors vs. sitagliptin in heart failure and type 2 diabetes: an observational cohort study. Eur Heart J 2023;44:2216–2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;373:232–242. 10.1056/NEJMoa1501352 [DOI] [PubMed] [Google Scholar]
- 12. Otto T, Diesing J, Borchert J, Heitmann E NCS, Lebrec J, Müller-Wieland D, et al. Age-dependent prevalence of type 2 diabetes, cardiovascular risk profiles and use of diabetes drugs in Germany using health claims data. Diabetes Obes Metab 2023;25:767–775. 10.1111/dom.14924 [DOI] [PubMed] [Google Scholar]
- 13. Lam CSP, Karasik A, Melzer-Cohen C, Cavender MA, Kohsaka S, Norhammar A, et al. Association of sodium–glucose cotransporter-2 inhibitors with outcomes in type 2 diabetes with reduced and preserved left ventricular ejection fraction: analysis from the CVD-REAL 2 study. Diabetes Obes Metab 2021;23:1431–1435. 10.1111/dom.14356 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research.