Abstract
Objective
To investigate the effects of multidirectional elastic tape on pain and function in individuals with lateral elbow tendinopathy.
Study Design
Randomised crossover trial.
Setting
Biomechanics laboratory.
Subjects
27 participants (11 females, mean (SD) age: 48.6 (11.9) years) with clinically diagnosed lateral elbow tendinopathy of at least six weeks’ duration.
Interventions
Tensioned multidirectional elastic tape applied over the wrist, compared to control tape (untensioned), and no tape conditions.
Main measures
Pain-free grip strength and pressure pain threshold were recorded at three timepoints for each condition: baseline, post-application, and following an exercise circuit. Change scores were calculated as the post-application or post-exercise value minus baseline. Repeated-measure analyses of variance were used to examine differences between conditions.
Results
There were no statistically significant differences in pain-free grip strength between conditions (flexed position: F2,52 = 0.02, p = 0.98; extended position: F2,52 = 2.26, p = 0.12) or across timepoints (post-application vs post-exercise) (flexed position: F1,26 = 0.94, p = 0.34; extended position: F1,26 = 0.79, p = 0.38). Seven participants (26%) increased pain-free grip strength above the minimal detectable change following application of multidirectional elastic tape. There were no statistically significant differences in pressure pain threshold between conditions (affected lateral epicondyle: F1.51,39.17 = 0.54, p = 0.54) or across timepoints (affected lateral epicondyle: F1,26 = 0.94, p = 0.34).
Conclusion
Tensioned multidirectional elastic tape may not immediately improve pain-free grip strength or pressure pain threshold in our lateral elbow tendinopathy population; however, individual variation may exist.
Keywords: Biomechanical tape, hand grip strength, lateral epicondylalgia, pain threshold, tennis elbow
Introduction
Lateral elbow tendinopathy is a common musculoskeletal condition associated with lateral elbow pain during gripping. 1 Evidence suggests individuals with lateral elbow tendinopathy have motor system impairments, including reduced pain-free grip strength compared to healthy controls.1, 2 Additionally, pain system changes can lead to decreased pressure pain thresholds at the affected lateral epicondyle 3 and at distal anatomic sites. 4 Multimodal treatment approaches involving pain reduction, load optimisation, and forearm strengthening are recommended.5, 6
One approach commonly used to reduce pain in individuals with lateral elbow tendinopathy is therapeutic tape. 7 A recent systematic review identified that rigid tape applied using a diamond deloading technique improves pain-free grip strength immediately following application, while conflicting evidence exists for kinesiotape. 8 The diamond deloading technique is applied to traction the underlying tissue towards the site of pain. 9 Despite the possible benefit, lengthy application times or movement restrictions may limit use. 7 Recently, advances in tape technology have led to the development of multidirectional elastic tape, also called ‘biomechanical tape®’. 10 Multidirectional elastic tape is a synthetic based tape that stretches up to 200% in both the longitudinal and transverse directions without a rigid endpoint 10 ; and is applied with tension over a shortened musculotendinous unit. 10 The proposed deloading effect is thought to occur during muscle contraction 10 via a mechanical effect on underlying skin, muscle and sensory receptors; or by altering load distribution among synergistic muscles (e.g. wrist extensors during gripping). 11 While multidirectional elastic tape seems like a promising treatment for musculoskeletal conditions, no studies have investigated the immediate effects in an upper limb pain population. 8
Two studies have examined multidirectional elastic tape in the lower limb.12, 13 After applying tensioned and untensioned tape over the gluteus medius muscle in healthy women, one study found no significant between- or within-group differences in hopping performance (distance or time), or gluteus medius muscle activity during functional tasks. 12 Conversely, Robinson et al. 13 reported significantly lower pain following application of tensioned and untensioned tape, compared to baseline measures in women with greater trochanteric pain syndrome. In addition, tensioned tape elicited small, significant reductions in hip adduction and internal rotation during walking compared to baseline (no tape) and untensioned tape. 13 Changes in pain and function were attributed to a deloading effect. 13 Thus, we hypothesised that the application of multidirectional elastic tape to the wrist extensors could improve two clinically relevant outcome measures, pain-free grip strength and pressure pain threshold.
Methods
This randomised crossover trial compared the immediate and post-exercise effects of tensioned multidirectional elastic tape, control (untensioned) tape, and no tape in individuals with clinically diagnosed lateral elbow tendinopathy, and is reported according to the Consolidated Standards of Reporting Trials (CONSORT) checklist for crossover trials. 14 This study was approved by an institutional Human Research Ethics Committee and was prospectively registered with the Australian New Zealand Clinical Trials Registry. All data collection was completed between August 2019 and January 2021.
Participants
Potential participants were recruited from regional Australia via social media and word-of-mouth. Potential participants completed an online screening questionnaire, followed by a clinical interview and physical examination, conducted by an experienced registered physiotherapist (CH). Eligible participants were ≥18 years old; with unilateral lateral elbow pain of at least six weeks’ duration; had a pain-free grip strength of ≤70% of their unaffected side 15 ; and experienced pain during at least two of the following pain provocation tests: (1) palpation of the lateral epicondyle, (2) Cozen's resisted wrist extension test, or (3) Maudsley's resisted third finger extension test. 16 Individuals were excluded if they reported a condition that could affect pain or grip strength (e.g. fibromyalgia, Parkinson's disease); received treatment for their affected elbow within the previous three months, or a corticosteroid injection within the previous six months; had treatment from a health professional for spinal, arm, or leg pain other than their affected elbow within the previous six months; were severely allergic to tape or silver; had a cardiac pacemaker; were pregnant; or were <6 months post-partum.
All participants provided written informed consent before enrolment and were familiarised with data collection procedures during the physical assessment. Participants provided details about condition history (affected side, symptom duration) and demographic information was obtained (age, sex, height, body mass). Patient pain and functional disability were quantified using the patient-rated tennis elbow evaluation, a valid and reliable 15-item questionnaire. 17 The pain subscale includes five questions related to the average pain over the past week and a higher score represents greater pain. The function subscale includes 10 questions relating to difficulty completing tasks over the past week, and a higher score represents greater disability. 17 To reduce fluctuations in pain due to unusual activity, participants were asked to maintain normal activities and avoid changes in medication for 24 h preceding data collection.
Randomisation, allocation and blinding
Each participant underwent three experimental conditions: tensioned tape, control tape and no tape, in a randomised order. An independent research assistant used simple randomisation (www.randomizer.org) to allocate condition sequence a priori into sequentially numbered opaque envelopes. Participants were informed that the study purpose was to test two different tape application methods; thus, were blinded to the manufacturer-recommended taping method. It was not possible to blind participants to the no tape condition. At the end of the final data collection session, participants were asked which tape condition they thought was applied as per manufacturer instructions, and were informed of the control condition. 18 The number of correct responses was used to assess blinding success.
Data collection procedure
Data collection sessions lasted approximately 150 min and were conducted at least two days apart to ensure adequate washout, 9 and no more than 28 days apart to minimise changes in pain and function. 19 Data were recorded at three timepoints within each data collection session, (1) at baseline, (2) immediately after tape application (or 5 min quiet sitting for no tape) and (3) immediately after a 20 min exercise circuit. Baseline measures (i.e. timepoint 1) were recorded prior to the application of each condition, while timepoints 2 and 3 were recorded as per the condition being tested. The circuit involved tasks (i.e. bag carry, lifting, stapling and hole-punching, wrist extension gripping a Flexbar®, and pronation/supination with a hammer; more details are provided in Supplemental Materials) designed to replicate the musculotendinous loads of ADLs on the wrist extensors, due to their role in stabilising the wrist and counteracting the forces produced by the wrist and finger flexors. 20 The circuit was included to observe whether biomechanical tape could mitigate the potentially painful or fatiguing effects of wrist extensor muscle contractions; and to replicate musculotendinous loads encountered during ADLs, which allows for interpretation of the results in a clinically meaningful context. Exercise order was set a priori and remained the same at subsequent sessions.
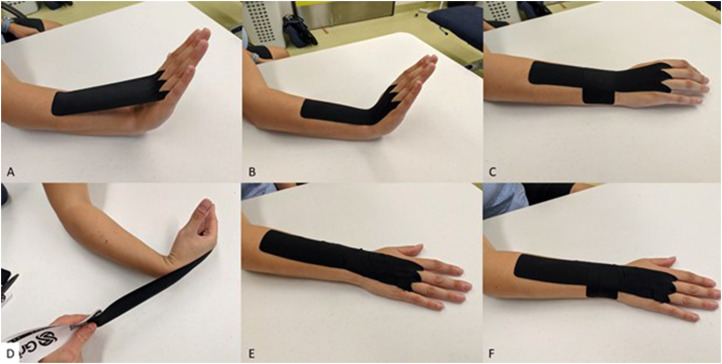
Intervention
A registered physiotherapist (CH) with 10 years of clinical practice experience, trained in using multidirectional elastic tape, applied a single layer of ActiveTape® V2 (Strapit Medical & Sports Supplies Pty. Ltd, Melbourne, Australia) for both tape conditions. The tensioned tape and control tape were anchored (i.e. applied without stretch) at both ends to reduce the risk of skin irritation. The distal anchor traversed the mid-palm to the dorsal 3rd metacarpal head, with holes cut for the third and fourth fingers (Figure 1). The forearm anchor (2 cm length) extended proximally from the mid-forearm. To determine the length of the tensioned tape midsection, the participant extended the wrist, and the distance from the 3rd metacarpal head to 2 cm distally of the mid forearm point was measured. This length was divided by 1.4, so that the midsection was stretched to 140% of its original length, and the tape was applied to the extended wrist and forearm (Figure 1(a) to (c)). The midsection length of the control condition was measured using the same points as the tensioned tape, except the participant actively flexed their wrist. The control tape was applied to a fully flexed wrist without stretch, to control for the sensation of tape on the skin (Figure 1(d) to (f)). Both tape conditions required a transverse section, applied without stretch at the radiocarpal joint, to prevent bowstringing (Figure 1(c) to (f)). All tape was removed following each session.
Figure 1.
Tensioned tape and control tape application. (a) Tensioned tape applied with the wrist extended, (b) at 140% of its original length, and (c) with transverse section in situ. (d) Control tape applied with the wrist flexed, (e) with no stretch, and (f) with transverse section in situ.
Outcome measures
Pain-free grip strength
Pain-free grip strength was measured with the participant seated, back supported, hips and knees at 90°, and feet flat on the floor. Testing was conducted with the arm in two positions: (1) shoulder neutral, elbow flexed to 90°, forearm pronated (flexed); and (2) shoulder flexed to 90°, elbow fully extended, forearm pronated (extended). 21 These positions were chosen due to changes in muscle length of the forearm extensor muscles which may affect pain-free grip strength measures and alter the outcomes of the tape application. The order of grip testing positions was randomised a priori and remained the same at subsequent sessions. Grip force was sampled at 2000 Hz using a calibrated electronic grip force transducer (Model MLT004/ST, ADInstruments, Dunedin, NZ), connected to a PowerLab data acquisition system (ADInstruments, Dunedin, New Zealand) and recorded using LabChart software (Version 8.1.13, ADInstruments, Dunedin, New Zealand).
For each testing position, participants were instructed to ‘slowly increase your grip until you first feel pain’. If participants experienced resting pain (Verbal Numerical Rating Scale ≥1) they were instructed to ‘slowly increase your grip until you first feel the pain increase’. Three trials were completed in each position with 30 s rest between trials. If participants reported failure to cease gripping at the first change in pain, the trial was repeated. Peak force (Newtons, N) was recorded for each trial, with the mean of three trials used for analysis. Pain-free grip strength is valid 22 and has excellent within-session reliability for the mean of three trials in an lateral elbow tendinopathy population (Intraclass correlation coefficient [ICC]2,3 = 0.96 [flexed] and 0.92 [extended]), with minimum detectable changes of 49.3 and 63.8 N for the flexed and extended positions, respectively. 23
Pressure pain threshold
Pressure pain threshold was measured at the affected and unaffected lateral epicondyle, and the mid-tibia on the unaffected side. The participant was positioned supine, elbow supported at 90° and hand resting on their abdomen. Increasing perpendicular pressure was applied with a digital pressure algometer (AlgoMed, Medoc Ltd, Ramat Yishai, Israel) at a rate of 40 kPa/s, with visual feedback on a computer monitor to guide the assessor's rate of force application. Data were recorded using Medoc software (Version 6.3.7.24, Medoc Ltd, Ramat Yishai, Israel). The participant was instructed to press a button, held in the opposite hand, as soon as the sensation of pressure changed to pain. Three trials were conducted at each site, separated by 30 s rest. Pressure pain threshold is a valid measure of mechanical hyperalgesia in lateral elbow tendinopathy. 24 The within-session reliability of the mean of three trials is excellent for the affected and unaffected lateral epicondyle and the tibia (ICC2,3 = 0.93, 0.97 and 0.99, respectively), with minimum detectable changes of 161.3, 154.1 and 199.3 kPa, respectively. 25
Sample size
Sample size calculation were performed using GLIMMPSE Guided Study Design (version 2.2.8) using a 3 × 2 (condition by time) repeated-measure ANOVA for the primary outcome of pain-free grip strength. Based on change in pain-free grip strength data (mean [SD]) following diamond deloading tape application, 9 an error probability of 0.05, and correlation among repeated measures of r = 0.80 between conditions and r = 0.90 within session, we determined that 27 participants were required to detect a condition by time interaction with a power of 0.80.
Statistical analysis
Pain-free grip strength and pressure pain threshold change scores were calculated as the immediate or post-exercise value minus the baseline value. A series of two-way 3 × 2 (condition by time) repeated-measure ANOVAs were used to examine differences in pain-free grip strength and pressure pain threshold change scores, with an alpha of 0.05. If Mauchley's test of sphericity indicated unequal variance (p < 0.05), a Huynh-Feldt correction was applied. 26 Planned pairwise comparisons were performed on the change from baseline to immediate and baseline to post-exercise between each condition. 27 A Bonferroni correction was applied to account for multiple comparisons, with an adjusted alpha of 0.006 (i.e. 0.05/9 comparisons). Results are reported as mean difference with 95% CIs between immediate and post-exercise timepoints and between conditions. In addition to examining statistical significance, the immediate and post-exercise differences in pain-free grip strength and pressure pain threshold for each participant were compared to the minimum detectable change (i.e. the minimum value to be 95% confident of true change). A chi-squared test of independence was used to assess whether participants were aware of which tape condition was applied as per the manufacturer's instructions. Blinding was considered successful if the p-value of a chi-squared test was ≥0.05. All statistical analyses were completed using SPSS Version 26 (IBM Corp., NY, USA).
Results
Participants
Data were collected for 27 participants with no missing data and no adverse events. The flow of participants is presented in Figure 2. Most participants were male (n = 16), right arm dominant (n= 23) with right-sided symptoms (n = 17). Mean (SD) time between data collection sessions was 9.9 (7.1) days. Participant demographics and injury details are reported in Table 1. Participants responded correctly to the blinding question 67% of the time. Chi-square test revealed no difference between the observed and expected distribution of responses (p = 0.08), indicating successful blinding as to the tensioned or untensioned condition.
Figure 2.
Flow of participants through study.
PFGS: pain-free grip strength; PPT: pressure pain threshold.
Table 1.
Participant (N = 27) characteristics and injury details.
| Characteristics | Mean (SD) or n (%) |
|---|---|
| Age, year | 48.6 (11.9) |
| Female, n (%) | 11 (40.7) |
| Height, m | 1.7 (0.1) |
| Mass, kg | 85.2 (16.4) |
| BMI, kg/m2 | 28.1 (4.9) |
| Repetitive/manual tasks at work, n (%) | 14 (51.9) |
| Computer work, n (%) | 13 (48.1) |
| Dominant side affected, n (%) | 19 (70.4) |
| Duration of symptoms, median (IQR), week | 10.0 (8.0–39.0) |
| Had ≥1 previous episode, n (%) | 12 (44.4) |
| Patient-rated Tennis Elbow Evaluation a | |
| Total, 0–100 | 34.3 (10.3) |
| Pain subscale, 0–50 | 18.4 (5.3) |
| Function subscale, 0–50 | 15.9 (7.6) |
| Maximum grip strength, unaffected side, flexed, N | 341.2 (106.6) |
| Maximum grip strength, unaffected side, extended, N | 353.4 (122.8) |
Values are expressed as mean ± SD unless stated otherwise.
BMI: body mass index; IQR: interquartile range.
aHigher values indicate greater levels of pain and disability.
Pain-free grip strength
For the flexed position, there was no significant main effect for time (F1,26 = 0.94, p = 0.34), or condition (F2,52 = 0.02, p = 0.98), or condition by time interaction (F2,52 = 0.46, p = 0.64). There were also no significant main effects for time (F1,26 = 0.79, p = 0.38), condition (F2,52 = 2.26, p = 0.12), or condition by time (F2,52 = 0.74, p = 0.48) for the extended position. Table 2 presents change scores and mean differences (95% CI) between timepoints and between conditions. On inspection of the individual data, seven of the 27 participants (26%) showed an increase in pain-free grip strength in the extended position above minimum detectable change (63.8 N) following tensioned tape application, compared to only one participant (4%) for each the control tape and no tape conditions. Group means (SD) for timepoints and conditions are presented in the Supplemental Material.
Table 2.
Change scores and mean differences between conditions and between timepoints.
| Multidirectional elastic tape (T) | Control tape (CT) | No tape (NT) | MD (95% CI) T−CT | MD (95% CI) T−NT | MD (95% CI) CT−NT | |
|---|---|---|---|---|---|---|
| Pain-free grip strength, flexed, N | ||||||
| Δ Immediate−baseline | 8.7 (−8.0–25.5) | 2.5 (−14.0–19.0) | 4.2 (−5.6–14.0) | 6.2 (−17.9–30.4) | 4.6 (−15.6–24.7) | −1.7 (−23.0–19.7) |
| Δ Post-exercise−baseline | 0.6 (−14.1–15.2) | 3.1 (−19.0–25.2) | 2.5 (−10.8–15.7) | −2.5 (−28.2–23.2) | −1.9 (−22.4–18.6) | 0.6 (−23.3–24.6) |
| MD (95% CI) IMM−PEX | 8.1 (−1.5–17.8) | −0.6 (−16.9–15.7) | 1.7 (−10.5–13.9) | |||
| Pain-free grip strength, extended, N | ||||||
| Δ Immediate−baseline | 21.8 (3.0–40.7) | −5.0 (−20.9–11.0) | 5.8 (−6.9–18.5) | 26.8 (−0.2–53.8) | 16.1 (−4.1–36.2) | −10.7 (−31.6–10.1) |
| Δ Post-exercise−baseline | 19.2 (1.3–37.0) | 2.9 (−16.7–22.5) | 12.4 (−0.5–25.4) | 16.3 (−9.6–42.1) | 6.7 (−16.1–29.6) | −9.5 (−29.9–10.9) |
| MD (95% CI) IMM−PEX | 2.7 (−8.8–14.1) | −7.9 (−25.8–10.1) | −6.7 (−19.9–6.6) | |||
| Pressure pain threshold, affected lateral epicondyle, kPa | ||||||
| Δ Immediate−baseline | 3.0 (−20.2–26.3) | −16.3 (−44.5–11.9) | −5.4 (−37.3–26.5) | 19.3 (−7.1–45.6) | 8.4 (−38.2–55.1) | −10.9 (−63.2–41.5) |
| Δ Post-exercise−baseline | 3.5 (−31.8–38.8) | −15.9 (−45.5–13.7) | −21.5 (−46.8–3.9) | 19.4 (−11.8–50.7) | 25.0 (−23.0–72.9) | 5.5 (−41.6–52.7) |
| MD (95% CI) IMM−PEX | −0.5 (−19.2–18.2) | −0.4 (−16.3–15.6) | 16.0 (−0.9–33.0) | |||
| Pressure pain threshold, unaffected lateral epicondyle, kPa | ||||||
| Δ Immediate−baseline | −23.9 (−48.2–0.5) | −37.3 (−68.1–−6.4) | −13.1 (−43.9–17.6) | 13.4 (−24.4–51.2) | −10.7 (−52.3–30.8) | −24.1 (−77.3–29.1) |
| Δ Post-exercise−baseline | −48.7 (−75.4–−22.0) | −59.6 (−86.7–−2.5) | −42.3 (−77.5–−7.2) | 10.9 (−25.6–47.4) | −6.4 (−53.7–41.0) | −17.3 (−66.9–32.3) |
| MD (95% CI) IMM−PEX | 24.9 (3.9–45.8) | 22.3 (0.7–44.0) | 29.2 (−0.5–58.9) | |||
| Pressure pain threshold, tibia, kPa | ||||||
| Δ Immediate−baseline | 2.0 (−22.7–26.7) | −110.8 (−172.8–−48.8) | 0.2 (−39.9–40.3) | 112.8 (35.4–190.3) | 1.9 (−45.1–48.8) | −111.0 (−190.7–−31.3) |
| Δ Post-exercise−baseline | −17.5 (−57.6–22.7) | −4.5 (−43.0–34.1) | −11.8 (−44.3–20.7) | −13.0 (−67.6–41.6) | −5.7 (−51.6–40.2) | 7.3 (−42.1–56.8) |
| MD (95% CI) IMM−PEX | 19.5 (−14.4–53.4) | −106.4 (−154.5–−58.3) | 12.0 (−9.6–33.5) | |||
Change scores (Δ) are the mean of immediate or post-exercise values minus baseline values (95% CI) of each participant.
IMM: immediate; MD: mean difference; PEX: post-exercise.
Pressure pain threshold
For the affected lateral epicondyle, there was no significant main effect for time (F1,26 = 0.94, p = 0.34), condition (F1.51,39.17 = 0.54, p = 0.54), or condition by time interaction (F2,52 = 1.40, p = 0.26). For the unaffected lateral epicondyle, there was a significant main effect for time (F1,26 = 11.97, p = 0.002), with no significant main effect for condition (F2,52 = 0.53, p = 0.59), or condition by time interaction (F2,52 = 0.09, p = 0.91). Pairwise comparisons of the main effect for time failed to show statistical significance at the corrected alpha level of 0.006. For the tibia, there was a significant main effect for time (F1,26 = 6.99, p = 0.01), no significant main effect for condition (F2,52 = 2.45 p = 0.10) and a significant effect for condition by time interaction (F2,52 = 15.04, p < 0.001). Pairwise comparisons of the main effect for condition or condition by time interactions failed to show statistical significance at the corrected alpha level of 0.006. Table 2 presents change scores and mean differences (95% CI) between timepoints and between conditions. On inspection of individual data only one participant showed an increase in pressure pain threshold at the affected lateral epicondyle above the minimum detectable change (161.3 kPa) following tensioned tape application, as did one participant following control tape application. Group means (SD) for timepoints and conditions are presented in the Supplemental Material.
Discussion
The present study examined the effects of tensioned multidirectional elastic tape on pain-free grip strength and pressure pain threshold immediately following application and post-exercise, compared to control tape and no tape conditions. There were no statistically significant changes in pain-free grip strength or pressure pain threshold after tensioned tape application, compared to control tape or no tape; however, comparison of individual pain-free grip strength data to the minimum detectable change suggests that there may be some minor benefit of tensioned tape for a subset of participants.
The present results differ from previous work reporting that diamond deloading tape elicits significant improvements in pain-free grip strength and pressure pain thresholds in individuals with lateral elbow tendinopathy immediately and 30 min after application, compared to baseline and control conditions. 8 The diamond deloading technique appears to alter load at the common extensor origin sufficiently to improve pain and function. 8 However, it requires eight strips of rigid tape, applied while the skin and underlying tissue is tractioned towards the lateral epicondyle, 9 which is more time-consuming than the technique used in the present study (i.e. one strip over the posterior wrist and one transverse strip). In comparison, the tape applied in our study is tensioned over a shortened musculotendinous unit, creating elastic recoil and potentially deloading, 10 via a mechanical effect on underlying skin, muscle, and joint or via a sensory effect on receptors. 11 The longitudinal direction of tape application used in the present study is more similar to kinesiotape techniques, which were also found to have no consistent effect on pain and function. 8 Unlike kinesiotape, which does not adhere to itself, a second layer of multidirectional elastic tape could be applied over the first to potentially increase the elastic recoil and improve the deloading capacity. 10 Alternatively, given that the diamond deloading tape is applied directly around the lateral epicondyle, future research should investigate whether applying deloading tape to the entire musculotendinous unit (i.e. across the common extensor origin) can improve the deloading capacity in individuals with lateral elbow tendinopathy.
The present study reported no significant effect of multidirectional elastic tape on pain-free grip strength or pressure pain threshold in individuals with lateral elbow tendinopathy. In contrast, Robinson et al. 13 reported significant improvements in gait following multidirectional elastic tape application in women with greater trochanteric pain syndrome. However, the magnitude of these findings was small, for example, changes of only 0.8° to 1.5° were recorded for hip adduction angle. 13 Longer, wider strips of tape, in a double layer, and directly overlaying the painful tissue were potentially sufficient to achieve the suggested deloading effect during walking, 13 which were possibly more effective than a single layer of tape, adjacent to the affected area, used in the present study.
Inspection of individual data revealed substantial variation in the pain-free grip strength response of individual participants following application of all three conditions. For example, immediately after tensioned tape application, seven participants (26%) had an improvement in pain-free grip strength in the extended position that was greater than the minimum detectable change (63.8 N). Varied individual response to treatment is a well-known phenomenon in research and clinical practice, 28 and previous work in lateral elbow tendinopathy has demonstrated variability in change scores similar to the present study.29, 30 This individual variability suggests there could be subgroups of responders within lateral elbow tendinopathy populations; thus, future studies adequately powered to examine responder characteristics would benefit clinicians in identifying patients who may benefit from multidirectional elastic tape.
The use of a randomised crossover trial design, with each participant acting as their own control, is ideal for testing the acute effects of an intervention in stable musculoskeletal conditions. 14 Even stable conditions will have minor daily fluctuations in pain and function, thus the inclusion of a baseline for each condition is important. Additionally, the no tape condition controlled any potential effects of the outcome measurement and exercise tasks. Another methodological consideration is blinding. Although participants were blinded as to which condition was the recommended application method by being informed that the study was testing two different application techniques, they could not be blinded to the no tape condition. Further, due to the nature of the tape application, the assessor could not be blinded to either tape condition. This lack of assessor and participant blinding for certain conditions may have impacted on the results; however, outcome measures were reliant on participants’ judgement based on the sensory feeling of pain (i.e. ceasing grip in pain-free grip strength; pressing the button to indicate pressure pain threshold). Participant instructions were controlled, therefore, assessor influence on outcomes is thought to be minimal. Furthermore, this study only examined the immediate effects of tape and the time period for which tape was applied may not have been sufficient for a consistent and detectable change in PFGS or PPT to occur. Longer term studies where participants are undertaking their usual ADLs will provide ecologically valid data to assess the effects of the biomechanical tape intervention.
Clinical messages.
Multidirectional elastic tape did not elicit immediate statistically significant improvements in pain or function in our sample of individuals with lateral elbow tendinopathy.
Improvements in pain-free grip strength for some study participants may indicate potential individual benefit.
Long-term treatment studies will provide information regarding real-world effects.
Supplemental Material
Supplemental material, sj-docx-1-cre-10.1177_02692155231152817 for Effects of multidirectional elastic tape on pain and function in individuals with lateral elbow tendinopathy: A randomised crossover trial by Caitlin E Hill, Luke J Heales, Robert Stanton and Crystal O Kean in Clinical Rehabilitation
Footnotes
Author contributions: All authors met the ICMJE recommendations for authorship including substantial contributions to the design of the work; contributions to the acquisition, analysis or interpretation of data; drafting and revision of the paper; final approval of the version to be published; and agreement to be accountable for the work. Dr Crystal Kean is the guarantor for the work.
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: A Sports Medicine Australia Research Foundation Grant was received to fund advertising and participant re-imbursement. CH was supported by an Australian Commonwealth Government Research Training Program Stipend. Tape used for the intervention was supplied by Strapit Medical & Sports Supplies Pty. Ltd. The funders played no role in data collection, analysis or interpretation, and impose no restrictions on publication of the study findings.
Institutional review board approval: This study was approved by the Central Queensland University Human Research Ethics Committee (HREC #0000021221).
Registration: This study was prospectively registered with the Australian New Zealand Clinical Trials Registry (ACTRN 12619000790145).
ORCID iD: Caitlin E Hill https://orcid.org/0000-0002-5566-9305
Supplemental material: Supplemental material for this article is available online.
References
- 1.Bisset LM, Russell T, Bradley S, et al. Bilateral sensorimotor abnormalities in unilateral lateral epicondylalgia. Arch Phys Med Rehabil 2006; 87: 490–495. [DOI] [PubMed] [Google Scholar]
- 2.Coombes BK, Bisset L, Vicenzino B. Thermal hyperalgesia distinguishes those with severe pain and disability in unilateral lateral epicondylalgia. Clin J Pain 2012; 28: 595–601. [DOI] [PubMed] [Google Scholar]
- 3.Ruiz-Ruiz B, Fernandez-de-Las-Penas C, Ortega-Santiago R, et al. Topographical pressure and thermal pain sensitivity mapping in patients with unilateral lateral epicondylalgia. J Pain 2011; 12: 1040–1048. [DOI] [PubMed] [Google Scholar]
- 4.Heales L, Lim E, Hodges P, et al. Sensory and motor deficits exist on the non-injured side of patients with unilateral tendon pain and disability — implications for central nervous system involvement: a systematic review with meta-analysis. Br J Sports Med 2014; 48: 1400–1406. [DOI] [PubMed] [Google Scholar]
- 5.Coombes BK, Bisset L, Vicenzino B. Management of lateral elbow tendinopathy: one size does not fit all. J Orthop Sports Phys Ther 2015; 45: 938–949. [DOI] [PubMed] [Google Scholar]
- 6.Bisset LM, Vicenzino B. Physiotherapy management of lateral epicondylalgia. J Physiother 2015; 61: 174–181. [DOI] [PubMed] [Google Scholar]
- 7.Hill CE, Stanton R, Heales LJ, et al. Therapeutic tape use for lateral elbow tendinopathy: a survey of Australian healthcare practitioners. Musc Sci Prac 2020; 48: 102160. [DOI] [PubMed] [Google Scholar]
- 8.George CE, Heales LJ, Stanton R, et al. Sticking to the facts: a systematic review of the effects of therapeutic tape in lateral epicondylalgia. Phys Ther Sport 2019; 40: 117–127. [DOI] [PubMed] [Google Scholar]
- 9.Vicenzino B, Brooksbank J, Minto J, et al. Initial effects of elbow taping on pain-free grip strength and pressure pain threshold. J Orthop Sports Phys Ther 2003; 33: 400–407. [DOI] [PubMed] [Google Scholar]
- 10.McNeill W, Pedersen C. Dynamic Tape. Is it all about controlling load? J Bodyw Mov Ther 2016; 20: 179–188. [DOI] [PubMed] [Google Scholar]
- 11.Hug F, Ouellette A, Vicenzino B, et al. Deloading tape reduces muscle stress at rest and during contraction. Med Sci Sports Exerc 2014; 46: 2317–2325. [DOI] [PubMed] [Google Scholar]
- 12.Silva RO, Carlos FR, Morales MC, et al. Effect of two Dynamic Tape™ applications on the electromyographic activity of the gluteus medius and functional performance in women: a randomized, controlled, clinical trial. J Bodyw Mov Ther 2020. DOI: 10.1016/j.jbmt.2020.11.0181360-8592. [DOI] [PubMed] [Google Scholar]
- 13.Robinson NA, Spratford W, Welvaert M, et al. Does Dynamic Tape change the walking biomechanics of women with greater trochanteric pain syndrome? A blinded randomised controlled crossover trial. Gait Posture 2019; 70: 275–283. [DOI] [PubMed] [Google Scholar]
- 14.Dwan K, Li T, Altman DG, et al. CONSORT 2010 Statement: extension to randomised crossover trials. Br Med J 2019; 366: l4378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coombes BK, Bisset L, Brooks P, et al. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. J Am Med Assoc 2013; 309: 461–469. [DOI] [PubMed] [Google Scholar]
- 16.Saroja G, Aseer ALP, Sai VPM. Diagnostic accuracy of provocative tests in lateral epicondylitis. Int J Physiotherap Res 2014; 2: 815–823. [Google Scholar]
- 17.Rompe JD, Overend TJ, MacDermid JC. Validation of the patient-rated tennis elbow evaluation questionnaire. J Hand Ther 2007; 20: 3–11. [DOI] [PubMed] [Google Scholar]
- 18.Bello S, Moustgaard H, Hrobjartsson A. Unreported formal assessment of unblinding occurred in 4 of 10 randomized clinical trials, unreported loss of blinding in 1 of 10 trials. J Clin Epidemiol 2017; 81: 42–50. [DOI] [PubMed] [Google Scholar]
- 19.Bisset LM, Beller E, Jull G, et al. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. Br Med J 2006; 333: 939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takala EP, Toivonen R. Placement of forearm surface EMG electrodes in the assessment of hand loading in manual tasks. Ergonomics 2013; 56: 1159–1166. [DOI] [PubMed] [Google Scholar]
- 21.Heales LJ, Hug F, MacDonald DA, et al. Is synergistic organisation of muscle coordination altered in people with lateral epicondylalgia? A case-control study. Clin Biomech 2016; 35: 124–131. [DOI] [PubMed] [Google Scholar]
- 22.Stratford PW, Levy DR.Assessing valid change over time in patients with lateral epicondylitis at the elbow. Clin J Sport Med 1994; 4: 88–91. [Google Scholar]
- 23.Hill CE, Heales LJ, Stanton R, et al. Pain-free grip strength in individuals with lateral elbow tendinopathy: between- and within-session reliability of one versus three trials. Physiother Theory Pract 2022: 1–9. DOI: 10.1080/09593985.2022.2030445. [DOI] [PubMed] [Google Scholar]
- 24.Slater H, Arendt-Nielsen L, Wright A, et al. Sensory and motor effects of experimental muscle pain in patients with lateral epicondylalgia and controls with delayed onset muscle soreness. Pain 2005; 114: 118–130. [DOI] [PubMed] [Google Scholar]
- 25.Hill CE. Understanding the effects of therapeutic tape in individuals with lateral elbow tendinopathy . Doctoral Thesis, CQUniversity, 2021. [Google Scholar]
- 26.Haverkamp N, Beauducel A. Violation of the sphericity assumption and its effect on type-I error rates in repeated measures ANOVA and multi-level linear models (MLM). Front Psychol 2017; 8: 1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruxton GD, Beauchamp G. Time for some a priori thinking about post hoc testing. Behav Ecol 2008; 19: 690–693. [Google Scholar]
- 28.Edwards RR, Dworkin RH, Turk DC, et al. Patient phenotyping in clinical trials of chronic pain treatments: IMMPACT recommendations. Pain 2016; 157: 1851–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho Y-T, Hsu W-Y, Lin L-F, et al. Kinesio taping reduces elbow pain during resisted wrist extension in patients with chronic lateral epicondylitis: a randomized, double-blinded, cross-over study. BMC Musculoskelet Disord 2018; 19: 193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bisset LM, Collins NJ, Offord SS. Immediate effects of 2 types of braces on pain and grip strength in people with lateral epicondylalgia: a randomized controlled trial. J Orthop Sports Phys Ther 2014; 44: 120–128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cre-10.1177_02692155231152817 for Effects of multidirectional elastic tape on pain and function in individuals with lateral elbow tendinopathy: A randomised crossover trial by Caitlin E Hill, Luke J Heales, Robert Stanton and Crystal O Kean in Clinical Rehabilitation