Abstract
Lower limb sensory disturbance can be a false localizing sign of cervical spondylotic myelopathy. It may lead to delayed or missed diagnosis, resulting in an inappropriate management plan, especially in the presence of concurrent lumbar lesions. Three Asian patients with lower limb sensory disturbance were ineffectively treated in the lumbar region. Magnetic resonance imaging showed cervical disc herniation and cervical spinal cord compression. The patients underwent anterior cervical discectomy and interbody fusion using a stand-alone cervical interbody fusion cage. Postoperative imaging showed that the spinal cord compression was relieved. On the first postoperative day, the lower limb sensory disturbance was also relieved. The patients showed good recovery at the 3-month postoperative follow-up. These three cases of cervical cord compression with lower limb sensory disturbance were easily misdiagnosed as lumbar spondylosis. Anterior cervical discectomy and fusion had a good therapeutic effect. Therefore, the presence of lower limb sensory disturbance in a non-radicular classic pattern should always raise suspicion of a possible cord compression at a higher level.
Keywords: Cervical spine, cervical spondylotic myelopathy, false localizing, tract pain, lower limb sensory disturbance, magnetic resonance imaging
Introduction
Cervical spondylotic myelopathy (CSM) is characterized by spinal cord compression or ischemia, followed by dysfunction due to narrowing of the sagittal diameter of the spinal canal.1,2 The typical symptoms of CSM are neck and shoulder pain, arm numbness or paresthesia, and gait disorders. 3 However, some patients have atypical symptoms, especially when the presentation involves the lower limbs, resulting in difficult diagnosis.4–7 Such presentations are considered false localizing signs of CSM because there are discrepancies between the neurological signs and the expected anatomical location of the lesion. 8
We herein present three rare cases of lower limb sensory disturbance and cervical disc herniation that were successfully managed by anterior cervical surgery. All patients provided written informed consent. The reporting of this study conforms to the CARE guidelines. 9
Case Reports
Case 1
Clinical presentation
The first patient was a 61-year-old Asian man who presented with a 5-year history of a burning sensation in the left lower limb. He also felt neck pain, upper limb numbness, and girdle sensation in his chest. He had no history of hypertension, diabetes, or nephropathy. Additionally, he had no history of hepatitis, tuberculosis, trauma, blood transfusion, poisoning, or penicillin anaphylaxis.
On examination, the patient was able to walk on his own, but with staggering. His cervical spine range of motion was normal, but his neck and shoulder muscles were tense. He also exhibited hypoesthesia of the left side of his body below the nipple. The strength of the main left limb muscles was slightly decreased, whereas the strength of the right ones was normal (left biceps brachii 4/5, triceps brachii 4/5, dorsal forearm 4/5, volar forearm 4/5, hand grasp 4/5) (right biceps brachii 5/5, triceps brachii 5/5, dorsal forearm 5/5, volar forearm 5/5, hand grasp 5/5) (left quadriceps femoris 4/5, tibialis anterior 4/5, gastrocsoleus 4/5, flexor longus 4/5) (right quadriceps femoris 5/5, tibialis anterior 5/5, gastrocsoleus 5/5, flexor longus 5/5). Bilateral reflex testing produced the following results: Eaten sign (−), Spurling sign (+), Hoffman sign (+), Babinski sign (+), patellar clonus (+++), ankle clonus (+++), patellar tendon reflex (++), and Achilles tendon reflex (++).
Radiologic evaluation
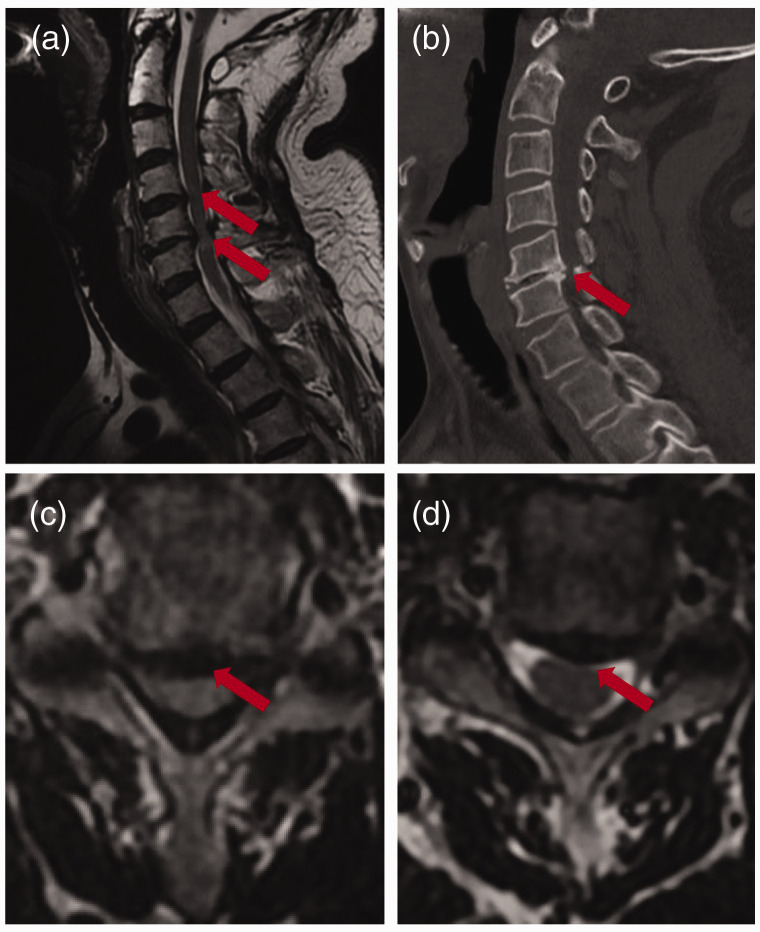
Magnetic resonance imaging (MRI) and coronal and sagittal computed tomography (CT) showed disc herniation and spinal cord compression at levels C4/5 and C5/6 (Figure 1(a)–(d)).
Figure 1.
Preoperative imaging of the cervical spine. (a, c, d) Magnetic resonance imaging showed C4/5 and C5/6 level spinal cord compression and (b) Computed tomography showed intervertebral space narrowing, osteophyte formation, and osteosclerosis.
Treatment
The patient was treated by anterior cervical surgery involving C4/5 and C5/6 discectomy and interbody fusion using a stand-alone cervical interbody fusion cage (ZERO-P; DePuy Synthes, Raynham, MA, USA).
Outcome and follow-up
The day after surgery, CT showed that the herniated discs at C4/5 and C5/6 had been removed and that the fusion cage was in a good position (Figure 2(a)–(c)). Additionally, the left lower limb burning was relieved and the upper limb numbness had almost disappeared. One month later, the patient had no complaints regarding left lower limb burning or upper limb numbness via telephone follow-up.
Figure 2.
Postoperative imaging of the cervical spine. (a) X-ray after C4/5 and C5/6 anterior cervical surgery, discectomy, and interbody fusion. (b, c) Computed tomography showed that the herniated discs at C4/5 and C5/6 had been removed.
Case 2
Clinical presentation
The second patient was a 40-year-old Asian woman who presented to our hospital because of a 6-month history of left lower leg and foot numbness and pain. She had also experienced headache, dizziness, right ring finger numbness, and right heel pain. She had a 6-year history of diabetes, which was well-controlled. She had no history of hypertension, nephropathy, hepatitis, tuberculosis, trauma, blood transfusion, poisoning, or penicillin anaphylaxis. She did not regularly drink alcohol and never smoked. On examination, the patient was able to walk normally without assistance. Her cervical spine range of motion was normal, but her neck and shoulder muscles were tense. She also had lumbar percussion pain. Her left thigh circumference was about 1.5 cm smaller than her right thigh circumference. Her left thigh sensation was decreased in the front and back, and her left leg and sole sensation were also decreased, especially the sole. The muscle strength of her left limb main muscles was slightly decreased. Additionally, her right heel exhibited tenderness. All pathological and physiological reflexes were normal.
Radiologic evaluation
MRI showed disc herniation at C4/5 and C5/6 and left spinal cord compression at C5/6 (Figure 3(a)–(c)). A vertebral hemangioma was present at C5, and left ligamentum flavum thickening was present at T2/3.
Figure 3.
Preoperative imaging of the cervical spine. (a, b, c) Magnetic resonance imaging showed C4/5 and C5/6 level spinal cord compression.
Treatment
The patient was treated by anterior cervical surgery involving C4/5 and C5/6 discectomy, interbody fusion (ZERO-P; DePuy Synthes), and C5 cement filling.
Outcome and follow-up
The day after surgery, CT showed that the C4/5 and C5/6 spinal cord compression was relieved (Figure 4(a)–(c)). Additionally, the left lower leg and foot numbness and pain were relieved, and the right heel pain had disappeared. The strength of the main left limb muscles had recovered. The headache, dizziness, and right ring finger numbness were slightly relieved. One month later, the patient had no complaints regarding lower limb numbness and pain via telephone follow-up.
Figure 4.
Postoperative imaging of the cervical spine. (a) X-ray after C4/5 and C5/6 anterior cervical surgery, discectomy, and interbody fusion and (b, c) Computed tomography showed that the C4/5 and C5/6 spinal cord compression was relieved after surgery.
Case 3
Clinical presentation
The third patient was a 34-year-old Asian man who presented to our hospital because of a 3-month history of right lower limb numbness and pain. He had no history of hypertension, diabetes, nephropathy, hepatitis, tuberculosis, trauma, blood transfusion, poisoning, or penicillin anaphylaxis. He did not drink alcohol regularly and never smoked.
On examination, the patient was able to walk normally without assistance. He had hypoesthesia of the right side of his body below the nipple and a decline in temperature sensation of the right lower leg. His limb muscle tension was normal, and he showed no obvious atrophy or fine motor disorder. His cervical spine range of motion was normal. Although is cervical spine curvature was straight, his neck and shoulder muscles were tense. The strength of the main limb muscles was normal. All pathological and physiological reflexes were also normal.
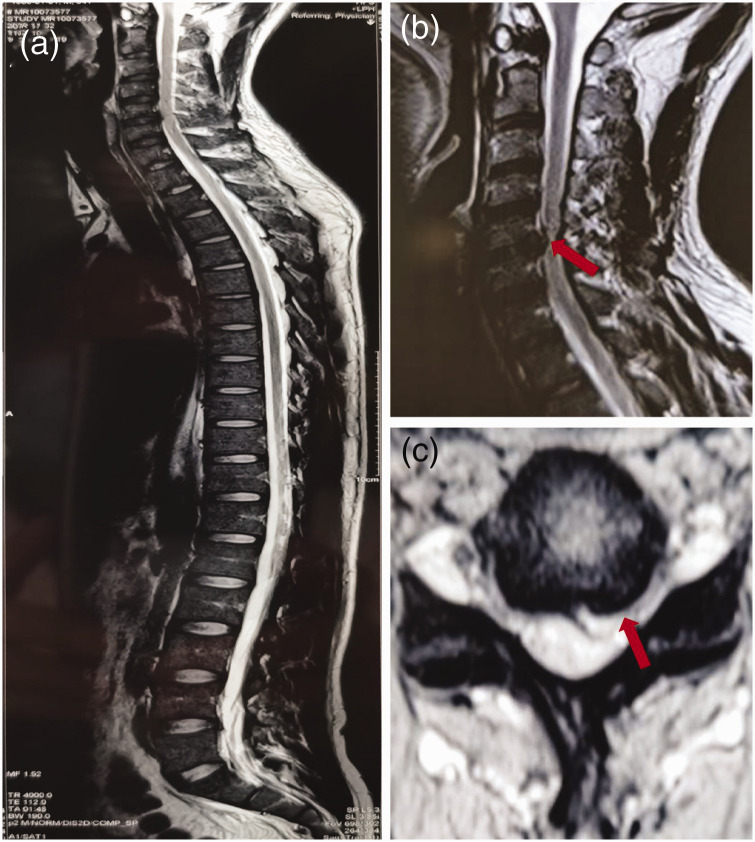
Radiologic evaluation
MRI showed disc herniation at C5/6 and left spinal cord compression and degeneration at C5/6 (Figure 5(b), (c)). Whole-spine MRI showed no thoracic or lumbar abnormalities (Figure 5(a)).
Figure 5.
Preoperative and postoperative cervical spine imaging. (a) Whole-spine magnetic resonance imaging showed normal lumbar and thoracic anatomy and (b, c) Magnetic resonance imaging showed left spinal cord compression at the C5/6 level.
Treatment
The patient was treated by anterior cervical surgery involving C5/6 discectomy and interbody fusion (ZERO-P; DePuy Synthes).
Outcome and follow-up
The day after the operation, the right body numbness and pain below the nipple had resolved, and the right lower limb numbness and pain were relieved. Additionally, MRI showed that the left spinal cord C5/6 compression was relieved (Figure 6(a), (b)). Three months later, MRI showed that the spinal cord degeneration had recovered and that the right lower limb numbness and pain were almost relieved.
Figure 6.
Postoperative cervical spine imaging. (a, b) Magnetic resonance imaging showed that the left spinal cord compression at C5/6 was relieved after surgery.
Discussion
In the three patients described herein, the primary symptoms did not take the form of typical neck pain and upper limb numbness; instead, the patients presented with lower limb sensory disturbance. This presentation is considered a false localizing sign of cervical cord compression because of the discrepancies between the neurological signs and the expected anatomical location of the lesion. 8 Collier 10 found discrepancies between antemortem clinical features and expected postmortem anatomical findings and first established the term “false localizing signs” in 1904. The correct diagnosis in our patients was markedly delayed because of the false localizing signs.
In Case 3, the patient had a 3-month history of right lower limb numbness and pain. He was young and had visited many orthopedic doctors. Most doctors believed that his symptoms were caused by pathology affecting the lumbar vertebrae, although MRI did not show lumbar abnormalities and conservative lumbar treatments were ineffective. The hypoesthesia of the right body below the nipple alerted us to the possibility of cervical cord involvement. In Case 1, the patient had a 5-year history of a burning sensation in the left lower limb as well as neck pain, upper limb numbness, and a girdle sensation in the chest. Although his main symptoms were not located in the cervical spine, we considered his secondary symptoms and realized that the cervical cord compression was the main cause. In Case 2 the patient presented to the hospital because of left lower leg and foot numbness and pain as well as headache, dizziness, right ring finger numbness, and right heel pain. Her symptoms were complicated and accompanied by lumbar disc herniation as shown by MRI. These three patients had similarities: lower limb sensory disturbance, cervical cord compression, and improvement of symptoms after cervical spine surgery. In Cases 2 and 3, the patients’ girdle sensation in the chest disappeared after surgery. However, the patient in Case 1 had no girdle sensation but exhibited right heel pain that we misdiagnosed as a calcaneal spur. Immediately after surgery, the right heel pain disappeared.
The precise mechanism of lower limb sensory disturbance caused by cervical cord compression is not clearly understood. The pain in the lower body parts caused by different spinal cord pathological conditions is called “tract pain,” and the precise mechanism responsible for such pain is unclear. In most reported cases, tract pain was the main symptom and was usually described as a burning, boring, or aching sensation. 11 The spinal tract disorder was regarded as the main reason for the tract pain in previous reports.12,13 From outside to inside, the spinothalamic tract fibers are the sacral, lumbar, thoracic, and cervical tract fibers. The cervical segment fibers are the most medial and are located in scattered positions. A compression lesion finally affects the cervical segment fibers and the segments lower than the lesion plane. The spinal cord blood supply should also be considered, especially in patients with a girdle sensation. The area surrounding the spinal cord T4 level is a watershed zone of the anterior spinal artery (ASA). The thoracic cord around the T4 level will become ischemic if the ASA is compressed by a lower cervical lesion. 14 Additionally, interruption of pain modulation pathways is considered an important cause of this tract pain. In the presumed pathomechanism, interruptions of descending antinociceptive projections from the rostral ventral medulla play a critical role in modulation and maintenance of the pain threshold. 15
The above pathological mechanisms are only speculations; the only confirmed point is that cervical surgery can eliminate the sensory disturbance of the lower limb. The disease diagnosis is very important, especially for patients with concurrent lumbar spinal lesions. The condition is often confused as a lumbar problem, leading to lumbar treatment or even unnecessary lumbar surgery. A careful physical examination based on a more comprehensive inspection should be performed to avoid this misdiagnosis. Although the main symptoms are in the lower limbs, CSM should be considered when the accompanying symptoms appear above the lumbar level. The patients in Cases 1 and 3 presented with a girdle sensation, and the patient in Case 2 presented with headache, dizziness, and right ring finger numbness. Additionally, for patients with both lumbar and cervical lesions on MRI, a cervical epidural steroid block given by either a foraminal or interlaminar approach would be helpful to differentiate compressive cervical and lumbar stenotic lesions. 6
In summary, we have described three cases of cervical cord compression presenting as lower limb sensory disturbance. These symptoms were probably caused by spinothalamic tract disorder, interruptions of descending antinociceptive projections from the rostral ventral medulla, or compression of the ASA. They were easily misdiagnosed as lumbar spondylosis. Anterior cervical discectomy and fusion had a good therapeutic effect. Thus, lower limb sensory disturbance that presents in a non-radicular classical pattern should always raise suspicion for possible cord compression at a higher level. These case studies will help clinicians to better manage CSM presenting as lower limb sensory disturbance.
Acknowledgements
We are grateful to the patients and all the researchers, including the physicians, nurses, and technicians, who participated in this study.
The authors declare that there is no conflict of interest.
Funding: This work was supported by the Shenzhen Science and Technology Program (No. JCYJ20210324111205015), the Traditional Chinese Medicine Bureau of Guangdong Province (No. 20221355), and the Sanming Project of Medicine in Shenzhen (No. SZSM201812066).
ORCID iDs: Kun Gao https://orcid.org/0000-0003-0323-4219
Yafei Cao https://orcid.org/0000-0001-9193-376X
Author contributions statement
Each of the authors significantly contributed to this manuscript. All authors are responsible for the content and have read and approved the manuscript for submission. Kun Gao: Data curation, Writing-Original draft preparation. Shufen Sun and Weidong Liu: Writing-Reviewing and editing. Weiji Yu and Yihong Wu: Visualization, Resource, Data curation. Yafei Cao: Supervision, Project administration.
Ethics and consent
Our institution does not require ethics approval for case reports. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The rights of the patients were protected. Written informed consent for treatment and publication of this case report were obtained from the patient and Shenzhen Traditional Chinese Medicine Hospital.
References
- 1.Gorter K.Influence of laminectomy on the course of cervical myelopathy. Acta Neurochir (Wien) 1976; 33: 265–281. [DOI] [PubMed] [Google Scholar]
- 2.Gross J, Benzel E.Dorsal surgical approach for cervical spondylotic myelopathy. In: Camins MB. (ed). Techniques in neurosurgery. Philadelphia: Lippincott Williams & Wilkins, 1999, pp.162–176. [Google Scholar]
- 3.Montgomery DM, Brower RS.Cervical spondylotic myelopathy. Clinical syndrome and natural history. Orthop Clin North Am 1992; 23: 487–493. [PubMed] [Google Scholar]
- 4.Ross MD, Elliott R.Cervical cord compressive myelopathy in a man with a primary complaint of knee pain. J Spinal Cord Med 2010; 33: 431–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akhavan-Sigari R, Rohde V, Alaid A.Cervical spinal canal stenosis and central disc herniation c3/4 in a man with primary complaint of thigh pain. J Neurol Surg Rep 2013; 74: 101–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan CK, Lee HY, Choi WC, et al. Cervical cord compression presenting with sciatica-like leg pain. Eur Spine J 2011; 20: S217–S221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kozaki T, Minamide A, Iwasaki H, et al. Funicular pain: a case report of intermittent claudication induced by cervical cord compression. BMC Musculoskelet Disord 2020; 21: 302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kobayashi S.“Tract pain syndrome” associated with chronic cervical disc herniation. Hawaii Med J 1974; 33: 376–381. [PubMed] [Google Scholar]
- 9.Gagnier JJ, Kienle G, Altman DG, et al. ; CARE Group. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 10.Collier J.The false localizing signs of intracranial tumour. Brain 1904; 27: 490–508. [Google Scholar]
- 11.Neo M, Ido K, Sakamoto T, et al. Cervical disc herniation causing localized ipsilateral popliteal pain. J Orthop Sci 2002; 7: 147–150. [DOI] [PubMed] [Google Scholar]
- 12.Scott M.Lower extremity pain simulating sciatica: tumors of the high thoracic and cervical cord as causes. J Am Med Assoc 1956; 160: 528–534. [DOI] [PubMed] [Google Scholar]
- 13.Pego-Reigosa R, Trobajo de las Matas JE, Branas F, et al. Dorsal sensory level as a false localizing sign in cervical myelopathy [in Spanish]. Rev Neurol 1998; 27: 86–88. [PubMed] [Google Scholar]
- 14.Ochiai H, Yamakawa Y, Minato S, et al. Clinical features of the localized girdle sensation of mid-trunk (false localizing sign) appeared in cervical compressive myelopathy patients. J Neurol 2002; 249: 549–553. [DOI] [PubMed] [Google Scholar]
- 15.Thimineur M, Kitaj M, Kravitz E, et al. Functional abnormalities of the cervical cord and lower medulla and their effect on pain: observations in chronic pain patients with incidental mild Chiari I malformation and moderate to severe cervical cord compression. Clin J Pain 2002; 18: 171–179. [DOI] [PubMed] [Google Scholar]