Abstract
Background:
Acute tibiofemoral knee dislocations (KDs) with a single cruciate ligament remaining intact are rare and can be classified as Schenck KD I. The inclusion of multiligament knee injuries (MLKIs) has contributed to a recent surge in Schenck KD I prevalence and has convoluted the original definition of the classification.
Purpose:
To (1) report on a series of true Schenck KD I injuries with radiologically confirmed tibiofemoral dislocation and (2) introduce suffix modifications to further subclassify these injuries based on the reported cases.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective chart review identified all Schenck KD I MLKIs at 2 separate institutions between January 2001 and June 2022. Single-cruciate tears were included if a concomitant complete disruption of a collateral injury was present or injuries to the posterolateral corner, posteromedial corner, or extensor mechanism. All knee radiographs and magnetic resonance imaging scans were retrospectively reviewed by 2 board-certified orthopaedic sports medicine fellowship-trained surgeons. Only documented cases consistent with a complete tibiofemoral dislocation were included.
Results:
Of the 227 MLKIs, 63 (27.8%) were classified as KD I, and 12 (19.0%) of the 63 KD I injuries had a radiologically confirmed tibiofemoral dislocation. These 12 injuries were subclassified based on the following proposed suffix modifications: KD I-DA (anterior cruciate ligament [ACL] only; n = 3), KD I-DAM (ACL + medial collateral ligament [MCL]; n = 3), KD I-DPM (posterior cruciate ligament [PCL] + MCL; n = 2), KD I-DAL (ACL + lateral collateral ligament [LCL]; n = 1), and KD I-DPL (PCL + LCL; n = 3).
Conclusion:
The Schenck classification system should only be used to describe dislocations with bicruciate injuries or with single-cruciate injuries that have clinical and/or radiological evidence of tibiofemoral dislocation. Based on the presented cases, the authors recommend the suffix modifications for subclassifying Schenck KD I injuries with the goal of improving communication, surgical management, and the design of future outcome studies.
Keywords: knee dislocation, multiligament knee injury, Schenck classification, KD I
Acute tibiofemoral knee dislocations (KDs) are devastating limb-threatening injuries that require emergent assessment of the neurovascular status. Once the knee is reduced and stabilized, determination of the numerous injury patterns and/or associated injuries is undertaken to formulate a proper treatment algorithm. Classification systems designed for KDs can facilitate communication and organization of injuries for proper treatment planning and inform research-based decision-making. Several KD classification systems have been created based on either the energy mechanism, the direction of tibial displacement with respect to the femur, the pathophysiology, or the combination of injuries to the ligaments.2,15,26,31,32,37 The anatomic classification system described by Schenck 26 is the most widely recognized in the literature (Table 1). By definition, a KD I injury involves complete disruption of a single cruciate ligament with a variable partial injury to the other cruciate ligament and complete or partial disruption of the collateral ligaments.11,26
Table 1.
| Classification | Description |
|---|---|
| KD I | Disruption of 1 cruciate (ACL or PCL) |
| KD II | Disruption of both cruciates (ACL + PCL) |
| KD III | Disruption of both cruciates (ACL + PCL) and either collateral (MCL or LCL) |
| KD IIIM | Disruption of both cruciates (ACL + PCL) and MCL |
| KD IIIL | Disruption of both cruciates (ACL + PCL) and LCL |
| KD IV | Disruption of both cruciates (ACL + PCL) and both collaterals (MCL + LCL) |
| KD V | Fracture-dislocation |
ACL, anterior cruciate ligament; KD, knee dislocation; LCL, lateral cruciate ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
KDs most commonly result in complete disruption of both cruciate ligaments with variable injury to the collateral ligaments and surrounding structures. 23 Complete tearing of only a single cruciate ligament and clinical and/or radiological evidence of tibiofemoral dislocation (Schenck KD I) is a particularly rare anatomic injury pattern, with only 14 well-characterized instances and only 1 instance involving the posterior cruciate ligament (PCL) (Table 2).4,6,9,10,33,35 Additional studies have reported cases of Schenck KD I that may have a clinically and/or radiologically confirmed tibiofemoral dislocation.16,34,36
Table 2.
Prior Studies With Detailed Instances of Schenck KD I Injury in Patients With Documented KD a
| Lead Author (Year) | Schenck KD I Injury, n | Ligament Tear Pattern |
|---|---|---|
| Cooper (1992) 6 | 4 | 3 isolated ACL, 1 ACL/LCL |
| Shelbourne (1992) 33 | 3 | 1 isolated ACL, 2 ACL/MCL |
| Bratt (1993) 4 | 4 | 2 ACL/LCL, 1 ACL/MCL, 1 PCL/LCL |
| Toritsuka (1999) 35 | 1 | 1 isolated ACL |
| Flowers (2003) 10 | 1 | 1 ACL/MCL |
| Figueroa (2021) 9 | 1 | 1 ACL/MCL |
ACL, anterior cruciate ligament; KD, knee dislocation; LCL, lateral cruciate ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
In the recent literature, there has been a noticeable rise in the reported incidence of multiligament knee injuries (MLKIs) that are classified as Schenck KD I because of the lack of a designated MLKI classification system for non-dislocated MLKIs.3,18,20,22,28,30 Such classifications blur the distinction between dislocated and non-dislocated knees that sustain the same ligamentous injuries. A recent study demonstrated an increased risk of neurovascular injury in patients with KDs that were confirmed on radiographs compared with patients with MLKIs who had no radiological evidence of a dislocation. 14 This finding directly challenges the notion that patients with a non-dislocated knee injury should be grouped into the same classification scheme as patients with a KD. 12 It is necessary to properly stratify distinct knee injuries to optimize the utility of classification systems in the clinic and research settings. There is likely an associated increased capsular injury with a true tibiofemoral KD that may contribute to a potentially higher risk of residual instability, arthrofibrosis, or heterotopic ossification, but this needs further study.
There is currently a diverse spectrum of injury presentations that fall under the same classification of a Schenck KD I injury. Consequently, the current KD I category of the Schenck classification may present with shortcomings in predicting surgery timing, staging, and overall management strategy by not indicating which specific ligaments are torn. 20 Furthermore, this overgeneralization of KD I injuries may be limiting future clinical outcome research when comparing dislocated versus non-dislocated knees with the same ligamentous injuries.
The aim of this study is to report the injury patterns of the largest known case series on true Schenck KD I injuries with radiologically confirmed KDs. Illustration of the various presentations of documented tibiofemoral KDs involving a single cruciate disruption may act as the first step toward potential modifications to the Schenck anatomic classification system to categorize these respective injury patterns more accurately as distinct knee pathologies.
Methods
The protocol for this multicenter study received institutional review board approval. A retrospective chart review was conducted at 2 separate institutions (Yale School of Medicine and NYU Langone Orthopaedic Center) to identify the patients treated for an MLKI between January 2001 and June 2022. Specific Current Procedural Terminology (CPT) and International Classification of Disease (ICD) codes were used to determine if patients were treated for an MLKI or KD.
In this study, MLKIs were defined as a complete tear of 2 or more of the following ligamentous structures of the knee: anterior cruciate ligament (ACL), PCL, superficial medial collateral ligament (sMCL), and lateral collateral ligament (LCL). Additional injuries to the supporting structures of the knee including the posterolateral corner (PLC), posteromedial corner (PMC), or extensor mechanism were included. Injuries to the PLC were defined as complete disruption of the LCL in addition to any combination of complete tears to the biceps femoris tendon (BFT), popliteal fibular ligament (PFL), or popliteus tendon (PLT). 13 A PMC injury constituted complete disruption to a combination of the sMCL, deep MCL, posterior oblique ligament (POL), oblique popliteal ligament, and/or posteromedial joint capsule.5,7 A ruptured patellar tendon (PT) represented an extensor mechanism injury. Between both institutional databases, 227 patients with MLKI were identified.
All ligament and myotendinous injuries from each patient were initially diagnosed on 1.5-T or 3.0-T magnetic resonance imaging (MRI) and were confirmed by examination under anesthesia (EUA) or operative reports. At each institution, a board-certified musculoskeletal fellowship-trained radiologist completed the initial radiology report. Patients with MRI scans performed and interpreted by radiologists at outside hospitals were reevaluated by a board-certified musculoskeletal fellowship-trained radiologist at each institution before to inclusion in the initial MLKI cohort. Board-certified orthopaedic sports medicine fellowship-trained surgeons (M.J.M. and M.J.A.) retrospectively reviewed the same MRI scans and compared them with the initial MRI assessment and their own EUA and/or operative findings. No cases were included if the initial radiographs and MRI scans were unavailable for retrospective review. Any discrepancies between the initial MRI report, retrospective review of the MRI, or the original operative findings were resolved by having the surgeon’s final postoperative diagnosis serve as the definitive diagnosis.13,14 MLKIs were subsequently categorized according to Schenck classification.11,26
Of the 227 MLKIs in the shared multicenter database, 63 patients were identified as having only a single cruciate ligament with or without collateral ligament involvement and were classified as KD I based on the ligament tear pattern. Knee radiographs and MRI scans of the 63 patients with KD I injuries were retrospectively re-reviewed by the board-certified orthopaedic sports medicine fellowship-trained surgeons (M.J.M. and M.J.A.) for the presence of a KD. In this study, a KD was defined as complete disruption of the normal tibiofemoral articulation with radiographic evidence at the time of presentation (Figure 1).
Figure 1.

Schenck knee dislocation (KD) I injury with radiologically confirmed tibiofemoral dislocation of the right knee and complete tear of the anterior cruciate ligament (ACL), intact posterior cruciate ligament (PCL), and lateral meniscus root tear. (A) Sagittal view radiograph shows a nondisplaced nonarticular impaction fracture at the posterior aspect of the proximal tibia and an anterior KD. (B) Sagittal T1-weighted magnetic resonance imaging (MRI) scan shows disruption of ACL at the midsubstance (yellow arrow). (C and D) Sequential sagittal T1-weighted MRI scans demonstrating continuity of the proximal, midsubstance, and distal PCL (yellow arrows).
There was no evidence of a tibiofemoral dislocation on the initial radiographs in 51 of the 63 patients. Therefore, these patients were subsequently classified as “non-dislocated KD I” and excluded from the study. The remaining 12 patients with confirmed tibiofemoral KD on radiographic imaging were considered as true Schenck KD I and were included in the case series for further descriptive analysis (Figure 2).
Figure 2.

Strobe diagram of patients with Schenck knee dislocation (KD) I in the multicenter multiligament knee injury (MLKI) database with radiographically documented tibiofemoral dislocation.
Results
Twelve patients met the inclusion criteria of disruption to a single cruciate ligament with a radiologically confirmed complete tibiofemoral dislocation (Schenck KD I). Seven of the 12 patients sustained traumatic high-velocity injuries. Of these 7 cases, 6 were patients with polytrauma who were involved in motor vehicle accidents and 1 was a patient with polytrauma who was struck by a vehicle and left in critical condition. The patient data of all 12 included cases are summarized in Table 3.
Table 3.
Characteristics of Patients With Schenck KD I Injury (n = 12) a
| Characteristic | Value |
|---|---|
| Age, y | 34.4 ± 12.8 |
| Sex, male/female, n | 8/4 |
| BMI | 27.7 ± 7.6 |
| Injury mechanism | |
| MVA | 6 (50) |
| Pedestrian struck by vehicle | 1 (8.3) |
| Sports-related | 2 (16.7) |
| Fall (<3 m) | 3 (25) |
| High-velocity mechanism b | 7 (58.3) |
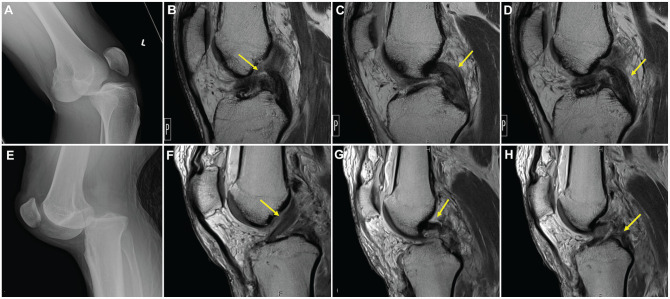
The Kennedy classification system describes the direction of tibial displacement with respect to the femur in the setting of tibiofemoral dislocation. 15 According to the Kennedy classification, 5 patients had anterior dislocations, 5 had posterior dislocations, 1 patient had an anteromedial dislocation, and 1 patient had a lateral dislocation (Figure 3).
Figure 3.
Schenck knee dislocation (KD) I injuries illustrating variable imaging presentation of tibiofemoral dislocations according to the Kennedy classification. (A) Lateral radiograph of a left knee demonstrating anterior tibiofemoral dislocation. (B) Sagittal T1-weighted magnetic resonance imaging (MRI) scan demonstrating anterior cruciate ligament (ACL) torn at midsubstance (yellow arrow). (C and D) Sequential sagittal T1-weighted MRI scans demonstrating thickening but continuity of the proximal, midsubstance, and distal posterior cruciate ligament (PCL) (yellow arrows). (E) Lateral radiograph of a left knee demonstrating posterior tibiofemoral dislocation. (F) Sagittal T1-weighted MRI scan demonstrating intact ACL (yellow arrow). (G) Sagittal T1-weighted MRI scan of intact proximal PCL femoral attachment (yellow arrow). (H) Sagittal T1-weighted MRI scan showing PCL torn at midsubstance (yellow arrow).
Nine of the 12 cases demonstrated variable tear patterns to either the medial, lateral, or both menisci. 13 Two patients had concomitant extensor mechanism injuries (PT rupture), and 2 had concomitant common peroneal nerve (CPN) palsies (2/12; 16.7%). One pregnant patient sustained a complete popliteal artery occlusion with compensatory collateral flow and elected nonsurgical treatment of her vascular injury (1/12; 8.3%). 29 In comparison, in the non-dislocated Schenck KD I group, a CPN injury occurred in 3 of 51 patients (5.9%), and no patients sustained a vascular injury. Statistical significance could not be reached when comparing neurovascular injury between the dislocated and non-dislocated KD I groups. A summary of the findings from the 12 confirmed cases of Schenck KD I, including injuries to additional cartilaginous, myotendinous, and ligamentous structures, is shown in Table 4.
Table 4.
Characteristics of the Schenck KD I Patients a
| Patient | Side | Dislocation | Injured Ligaments |
Medial Meniscus |
Lateral Meniscus |
Additional Injuries |
KD I Class b | Neurovascular Injury |
|---|---|---|---|---|---|---|---|---|
| 1 | R | Anterior | Isolated ACL | — | Posterior root | — | KD I-DA | — |
| 2 | R | Anterior | Isolated ACL | Oblique | Radial | PT | KD I-DA | — |
| 3 | R | Anterior | Isolated ACL | — | — | — | KD I-DA | — |
| 4 | R | Anterior | ACL + MCL | — | — | POL, MPFL | KD I-DAM | — |
| 5 | L | Anterior | ACL + MCL | Posterior horn | — | POL, MPFL | KD I-DAM | — |
| 6 | L | Lateral | ACL + MCL | Longitudinal | — | MPFL | KD I-DAM | — |
| 7 | R | Anteromedial | ACL + LCL | — | — | BFT, popliteus | KD I-DNAL | CPN |
| 8 | R | Posterior | PCL + MCL | Anterior horn | Complex | PT, ITB | KD I-DPM | — |
| 9 | R | Posterior | PCL + MCL | Radial | — | Popliteus | KD I-DCPM | Popliteal artery |
| 10 | R | Posterior | PCL + LCL | Posterior horn | — | BFT, PFL | KD I-DNPL | CPN |
| 11 | L | Posterior | PCL + LCL | Posterior root | — | BFT, PLT, PFL | KD I-DPL | — |
| 12 | L | Posterior | PCL + LCL | Posterior horn | — | — | KD I-DPL | — |
Dashes indicate areas not applicable. ACL, anterior cruciate ligament; BFT, biceps femoris tendon; CPN, common peroneal nerve injury; ITB, iliotibial band; KD I, Schenck knee dislocation I; L, left; LCL, lateral cruciate ligament; LTP, lateral tibial plateau; MCL, medial collateral ligament; MPFL, medial patellofemoral ligament; PCL, posterior cruciate ligament; PFL, popliteal fibular ligament; POL, posterior oblique ligament; PT, patellar tendon; R, right.
KD I subclass: A, anterior cruciate ligament; C, vascular injury; D, documented dislocation; L, lateral-sided; M, medial-sided; N, neurologic injury; P, posterior cruciate ligament.
All included Schenck KD I instances with radiologically confirmed dislocations were divided into subclassifications based on the proposed suffix modifications outlined in Table 5. The modified subclassifications were as follows: 3 KD I-DA (ACL only), 3 KD I-DAM (3 ACL + MCL), 2 KD I-DPM (PCL + MCL), 1 KD I-DAL (1 ACL + LCL), and 3 KD I-DPL (PCL + LCL).
Table 5.
Proposed KD I Subclassification Scheme a
| Suffix b | KD I Subclassification | Ligaments Torn |
|---|---|---|
| DA | KD I-DA | ACL |
| DAM | KD I-DAM | ACL/MCL |
| DAL | KD I-DAL | ACL/LCL |
| DALM | KD I-DALM | ACL/LCL/MCL |
| DP | KD I-DP | PCL |
| DPM | KD I-DPM | PCL/MCL |
| DPL | KD I-DPL | PCL/LCL |
| DPLM | KD I-DPLM | PCL/LCL/MCL |
ACL, anterior cruciate ligament; KD, knee dislocation; LCL, lateral cruciate ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
Suffix “D” designates radiologically documented tibiofemoral dislocation. Suffix “A” or “P” designates a torn cruciate ligament (ACL or PCL). Suffix “M” or “L” designates a torn collateral ligament (MCL or LCL).
Discussion
In this study, we present the largest known collection of radiologically confirmed true Schenck KD I injuries. Through the 12 case examples, 5 distinct ligament tear patterns with tibiofemoral dislocations could be identified as Schenck KD I: ACL only, ACL and MCL, ACL and LCL, PCL and MCL, and PCL and LCL. In theory, 3 additional variations of Schenck KD I would be a tibiofemoral dislocation with disruption of the PCL only and a single cruciate disruption with both collateral ligaments torn. In our multicenter MLKI database and in the literature, only non-dislocated injuries involving a single cruciate ligament (either the ACL or PCL) and both collaterals could be identified. 17
To our knowledge, there are only 14 cases of radiologically confirmed tibiofemoral Schenck KD I that have been well described in the current orthopaedic literature (Table 2).4,6,9,10,33,35 Cooper et al 6 first described 4 cases of anterior KDs with either an isolated ACL disruption or an ACL disruption with an additional PLC injury. Bratt and Newman 4 presented a separate series that included KD cases with injury to either the ACL or PCL and a concomitant complete tear of the MCL. Additional examples of Schenck KD I with similar injury patterns were presented in 2 separate case series by Shelbourne 33 and Toritsuka. 35 Most recently, Figueroa et al 9 acknowledged the rarity of these Schenck KD I injuries and presented a case of a posterior KD with an ACL avulsion, intact PCL, and PMC involvement. Collectively, these documented cases provide evidence of there being several unique injury patterns of KDs that involve a single cruciate, yet they all currently fall under the same anatomic classification of a Schenck KD I.
The terms “KD” and “MLKI” have often been used synonymously throughout the orthopaedic literature, and it has become common practice to apply the Schenck KD classification system to MLKIs without a documented KD. As a result, several studies have expanded the definition of Schenck KD I to include MLKIs with a single cruciate remaining intact, which has resulted in a sudden and dramatic increase in the reported prevalence of these injuries.12,20,24 In 2021, Maxwell et al 20 published a study with a reported 121 Schenck KD I injuries, which constituted 42.2% of the entire MLKI cohort. However, it is important to note that this study included high-grade partial ligamentous injuries, which are not usually considered under the Schenck classification system. Meanwhile, Patel et al 24 and Hughes et al 12 reported that 56 of 108 patients (52%) and 83 of 136 patients (61%) had Schenck KD I injuries in their respective studies on MLKIs that were published during the past year. In our multicenter database, only 63 of 227 MLKIs (27.8%) could be considered as Schenck KD I based on the ligament tear pattern alone, and only 12 of 227 patients (5.3%) were classified as true Schenck KD I with radiologically confirmed KD. As a result, Schenck KD I injuries appear to be much rarer entities than the reporting trends in the literature.
The surge in reported Schenck KD I injuries is believed to represent a misnomer in the current literature since not all MLKIs are KDs. 38 Therefore, there is a need to emphasize the importance of distinguishing between KDs and MLKIs and to standardize the definition of the Schenck KD I classification as a single cruciate ligament injury with a radiologically and/or clinically confirmed tibiofemoral dislocation. The Schenck classification system should be used strictly for KDs with clinical and/or radiological evidence of tibiofemoral dislocation and all bicruciate injuries. There is an opportunity to develop a separate stratified MLKI classification system, which would be beneficial for communication and research purposes and could lead to a more focused evaluation of our outcome assessments.
The patients included in this case series illustrate a variety of anatomic injury patterns with differing injury mechanisms, operative planning, and clinical outcomes. Of the 63 MLKIs initially classified as KD I in our combined cohort, 51 did not fit the criteria of a radiologically confirmed KD. Despite growing evidence that dislocated and non-dislocated MLKIs represent distinct knee pathologies, they remain under the KD I category since there is no other suitable classification system in which to include these MLKIs. A recent study by Kahan et al 14 determined that MLKIs with a radiologically confirmed tibiofemoral dislocation have significantly higher rates of neurovascular injury when compared with non-dislocated MLKIs. It is quite rare to have an injury to the popliteal artery or peroneal nerve when only a single cruciate ligament is involved.14,34,38 In our MLKI cohort, there were no concomitant popliteal artery injuries among the patients with non-dislocated single-cruciate injuries. Additionally, the risk of CPN injury has been shown to be higher in KDs and MLKIs that involve the PLC or ACL, suggesting that neurological injury may be more attributed to the ligament structures involved.1,8,13,19 In the current case series, 1 of 12 patients (8.33%) had an arterial injury and 2 of the 12 patients (16.67%) were evaluated with injuries to the CPN. As such, true Schenck KD I with tibiofemoral KD carries a degree of neurovascular injury risk. Nevertheless, there should remain a high index of clinical suspicion of neurovascular injuries in non-dislocated MLKIs, and these injuries still need to be acutely assessed as closely as a dislocated knee.12,29,32
The current findings suggest that modification to the current Schenck KD I classification schema should incorporate more descriptive subclassifications to further clarify the distinct pathoanatomy of these injuries. Until a comprehensive classification is established specifically for MLKIs, we propose using the suffix “D” to signify that the injury entails a documented tibiofemoral KD. This would represent an additional specifier to implement into the KD nomenclature for all Schenck classes, along with the previously described labels of “C” for vascular injury and “N” for neurologic injury. 27 Regarding the KD I class, the addition of the suffix “A” for ACL or “P” for PCL would specify which cruciate ligament is torn and would be analogous to the “M” or “L” suffixes used in Schenck KD III and KD IV injuries, which indicate medial and lateral-sided injuries.25,39 The permutations generated by these suffixes comprise new Schenck KD I subclasses that distinguish the presence of tibiofemoral dislocation and more accurately pinpoint the unique ligament tear patterns as represented by the 12 cases presented in this series. Increased recognition of these proposed Schenck KD I subclassifications may be beneficial for clarifying the communication of these injuries and guiding operative approaches for surgeons to provide optimal care for these patients.
The primary goal of this case series was simply to demonstrate that the current Schenck KD I classification resembles an umbrella term composed of several variations of ligament tear patterns that should each be recognized as distinct entities. The addition of the suggested subclassifications may lead to more precise stratification of these injuries, which may improve prediction of clinical management and the methodology of comparative outcome studies. Although it is implied that the presence of a tibiofemoral dislocation may make Schenck KD I injuries unique when compared with non-dislocated counterparts, further study must be conducted to establish significant and clinically relevant differences between them.
Limitations
The main limitation of this study is that it is a descriptive case series of a retrospective cohort. As such, the small sample size and absence of a control group means that the ability to make significant claims is limited by study design and insufficient statistical power. Given the rarity of the injury, large enough numbers to prove the relative increased neurovascular morbidity in Schenck KD I injuries with documented KDs may be challenging to generate.
Conclusion
The number of Schenck KD I injuries described in the literature has been escalating. However, the incidence of a true tibiofemoral KD in the reported “KD I” injuries is expected to be scarce and is likely <20%. The Schenck classification system should only be used to describe KDs with bicruciate injuries or with single-cruciate injuries that have radiological evidence of tibiofemoral dislocation. Based on the presented cases, we recommend the suffix modifications for subclassifying Schenck KD I injuries with the goal of improving communication, surgical management, and the design of future outcome studies.
Footnotes
Final revision submitted January 23, 2023; accepted February 6, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.A. has received research support from Arthrex and Orcosa; education payments from Arthrex; consulting fees from Arthrex, JRF Ortho, and DePuy; and nonconsulting fees from Arthrex. M.J.M. has received consulting and nonconsulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Yale University (reference No. 2000028912).
References
- 1.Bloom DA, Essilfie AA, Lott A, et al. Distal biceps femoris avulsions: associated injuries and neurological sequelae. Knee. 2020;27(6):1874-1880. [DOI] [PubMed] [Google Scholar]
- 2.Boisgard S, Versier G, Descamps S, et al. Bicruciate ligament lesions and dislocation of the knee: mechanisms and classification. Orthop Traumatol Surg Res. 2009;95(8):627-631. [DOI] [PubMed] [Google Scholar]
- 3.Borque KA, Jones M, Balendra G, et al. High return to play rate following treatment of multiple-ligament knee injuries in 136 elite athletes. Knee Surg Sports Traumatol Arthrosc. 2022;30(10):3393-3401. [DOI] [PubMed] [Google Scholar]
- 4.Bratt HD, Newman AP. Complete dislocation of the knee without disruption of both cruciate ligaments. J Trauma. 1993;34(3):383-389. [DOI] [PubMed] [Google Scholar]
- 5.Cinque ME, Chahla J, Kruckeberg BM, et al. Posteromedial corner knee injuries: diagnosis, management, and outcomes: a critical analysis review. JBJS Rev. 2017;5(11):e4. [DOI] [PubMed] [Google Scholar]
- 6.Cooper DE, Speer KP, Wickiewicz TL, et al. Complete knee dislocation without posterior cruciate ligament disruption. A report of four cases and review of the literature. Clin Orthop Relat Res. 1992;284:228-233. [PubMed] [Google Scholar]
- 7.Dold AP, Swensen S, Strauss E, et al. The posteromedial corner of the knee: anatomy, pathology, and management strategies. J Am Acad Orthop Surg. 2017;25(11):752-761. [DOI] [PubMed] [Google Scholar]
- 8.Essilfie AA, Alaia EF, Bloom DA, et al. Distal posterolateral corner injury in the setting of multiligament knee injury increases risk of common peroneal palsy. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):239-245. [DOI] [PubMed] [Google Scholar]
- 9.Figueroa F, Sandoval A, Figueroa D. Schenck’s knee dislocation (KD) I injury: an uncommon pattern. J Clin Orthop Trauma. 2021;16:230-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flowers A, Copley LAB. High-energy knee dislocation without anterior cruciate ligament disruption in a skeletally immature adolescent. Arthroscopy. 2003;19(7):782-786. [DOI] [PubMed] [Google Scholar]
- 11.Goebel CP, Domes C. Classifications in brief: the Schenck classification of knee dislocations. Clin Orthop Relat Res. 2020;478(6):1368-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hughes JD, Lynch AD, Smith CN, et al. External fixation increases complications following surgical treatment of multiple ligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):161-166. [DOI] [PubMed] [Google Scholar]
- 13.Kahan JB, Li D, Schneble CA, et al. The pathoanatomy of posterolateral corner ligamentous disruption in multiligament knee injuries is predictive of peroneal nerve injury. Am J Sports Med. 2020;48(14):3541-3548. [DOI] [PubMed] [Google Scholar]
- 14.Kahan JB, Schneble CA, Li D, et al. Increased neurovascular morbidity is seen in documented knee dislocation versus multiligamentous knee injury. J Bone Joint Surg Am. 2021;103(10):921-930. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg Am. 1963;45:889-904. [PubMed] [Google Scholar]
- 16.Kilicoglu OI, Pehlivanoglu T, Demirel M, et al. The impact of the ligamentous injury pattern and associated neurovascular injury on ultimate knee function in patients with traumatic knee dislocations. J Knee Surg. 2021;34(14):1495-1502. [DOI] [PubMed] [Google Scholar]
- 17.Krych AJ, Sousa PL, King AH, et al. Meniscal tears and articular cartilage damage in the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3019-3025. [DOI] [PubMed] [Google Scholar]
- 18.Labarre C, Kim SH, Pujol N. Incidence and type of meniscal tears in multiligament injured knees. Knee Surg Sports Traumatol Arthrosc. 2023;31(2):465-474. [DOI] [PubMed] [Google Scholar]
- 19.Markus DH, Mojica ES, Bi A, et al. Relationship between peroneal nerve and anterior cruciate ligament involvement in multiligamentous knee injury: a multicenter study. J Am Acad Orthop Surg. 2022;30(22):e1461-e1466. [DOI] [PubMed] [Google Scholar]
- 20.Maxwell GT, Warth RJ, Amin A, et al. Multiple ligament knee injuries: does the knee dislocation classification predict the type of surgical management? J Knee Surg. 2021;34(3):273-279. [DOI] [PubMed] [Google Scholar]
- 21.Moran J, Schneble CA, Katz LD, et al. Examining the bone bruise patterns in multiligament knee injuries with peroneal nerve injury. Am J Sports Med. 2022;50(6):1618-1626. [DOI] [PubMed] [Google Scholar]
- 22.Nielsen TG, Sørensen OG, Lind M. A comparison of multi-ligament reconstruction and isolated anterior cruciate ligament reconstruction at one year follow-up: results from the Danish Knee Ligament Reconstruction Registry. J Exp Orthop. 2022;9(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ockuly AC, Imada AO, Richter DL, et al. Initial evaluation and classification of knee dislocations. Sports Med Arthrosc Rev. 2020;28(3):87-93. [DOI] [PubMed] [Google Scholar]
- 24.Patel NK, Lian J, Nickoli M, et al. Risk factors associated with complications after operative treatment of multiligament knee injury. Orthop J Sports Med. 2021;9(3):2325967121994203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Richter D, Wascher DC, Schenck RC., Jr.A novel posteromedial approach for tibial inlay PCL reconstruction in KDIIIM injuries: avoiding prone patient positioning. Clin Orthop Relat Res. 2014;472(9):2680-2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schenck RC. The dislocated knee. Instr Course Lect. 1994;43:127-136. [PubMed] [Google Scholar]
- 27.Schenck RC, Jr, Richter DL, Wascher DC. Knee dislocations: lessons learned from 20-year follow-up. Orthop J Sports Med. 2014;2(5):2325967114534387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schlumberger M, Schuster P, Eichinger M, et al. Posterior cruciate ligament lesions are mainly present as combined lesions even in sports injuries. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2091-2098. [DOI] [PubMed] [Google Scholar]
- 29.Schneble CA, Kahan JB, Burroughs PJ, et al. Popliteal artery occlusion with collateral blood flow in a reducible knee dislocation during pregnancy: a case report. JBJS Case Connect. 2021;11(2). doi:10.2106/JBJS.CC.20.00516 [DOI] [PubMed] [Google Scholar]
- 30.Shamrock AG, Hall JR, Hajewski CJ, et al. Cartilage and meniscus injuries are more common in patients undergoing delayed multiligament reconstruction. J Knee Surg. 2022;35(5):560-565. [DOI] [PubMed] [Google Scholar]
- 31.Shelbourne KD, Klootwyk TE. Low-velocity knee dislocation with sports injuries. Treatment principles. Clin Sports Med. 2000;19(3):443-456. [DOI] [PubMed] [Google Scholar]
- 32.Shelbourne KD, Porter DA, Clingman JA, et al. Low-velocity knee dislocation. Orthop Rev. 1991;20(11):995-1004. [PubMed] [Google Scholar]
- 33.Shelbourne KD, Pritchard J, Rettig AC, et al. Knee dislocations with intact PCL. Orthop Rev. 1992;21(5):607-611. [PubMed] [Google Scholar]
- 34.Stannard JP, Sheils TM, Lopez-Ben RR, et al. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86(5):910-915. [PubMed] [Google Scholar]
- 35.Toritsuka Y, Horibe S, Hiro-oka A. Knee dislocation following anterior cruciate ligament disruption without any other ligament tears. Arthroscopy. 1999;15(5):522-526. [DOI] [PubMed] [Google Scholar]
- 36.Twaddle BC, Bidwell TA, Chapman JR. Knee dislocations: where are the lesions? A prospective evaluation of surgical findings in 63 cases. J Orthop Trauma. 2003;17(3):198-202. [DOI] [PubMed] [Google Scholar]
- 37.Wascher DC. High-velocity knee dislocation with vascular injury. Treatment principles. Clin Sports Med. 2000;19(3):457-477. [DOI] [PubMed] [Google Scholar]
- 38.Wascher DC, Schenck RC, Treme GP, et al. The knee dislocation classification system is simple, reproducible, and allows communication among surgeons. J Knee Surg. 2022;35(9):1044-1045. [DOI] [PubMed] [Google Scholar]
- 39.Werner BC, Hadeed MM, Gwathmey FW, Jr, et al. Medial injury in knee dislocations: what are the common injury patterns and surgical outcomes? Clin Orthop Relat Res. 2014;472(9):2658-2666. [DOI] [PMC free article] [PubMed] [Google Scholar]